Key Points
Question
Is childbirth delivery mode associated with risk of pelvic floor disorders over time?
Findings
In this cohort study of 1528 women, compared with spontaneous vaginal delivery, cesarean delivery was associated with a significantly lower risk of stress urinary incontinence (adjusted hazard ratio [aHR], 0.46), overactive bladder (aHR, 0.51), and pelvic organ prolapse (aHR, 0.28); operative vaginal delivery was associated with a significantly higher risk of anal incontinence (aHR, 1.75) and pelvic organ prolapse (aHR, 1.88).
Meaning
After childbirth, the risk of pelvic floor disorders varied by delivery mode.
Abstract
Importance
Pelvic floor disorders (eg, urinary incontinence), which affect approximately 25% of women in the United States, are associated with childbirth. However, little is known about the course and progression of pelvic floor disorders over time.
Objective
To describe the incidence of pelvic floor disorders after childbirth and identify maternal and obstetrical characteristics associated with patterns of incidence 1 to 2 decades after delivery.
Design, Setting, and Participants
Women were recruited from a community hospital for this cohort study 5 to 10 years after their first delivery and followed up annually for up to 9 years. Recruitment was based on mode of delivery; delivery groups were matched for age and years since first delivery. Of 4072 eligible women, 1528 enrolled between October 2008 and December 2013. Annual follow-up continued through April 2017.
Exposures
Participants were categorized into the following mode of delivery groups: cesarean birth (cesarean deliveries only), spontaneous vaginal birth (≥1 spontaneous vaginal delivery and no operative vaginal deliveries), or operative vaginal birth (≥1 operative vaginal delivery).
Main Outcomes and Measures
Stress urinary incontinence (SUI), overactive bladder (OAB), and anal incontinence (AI), defined using validated threshold scores from the Epidemiology of Prolapse and Incontinence Questionnaire, and pelvic organ prolapse (POP), measured using the Pelvic Organ Prolapse Quantification Examination. Cumulative incidences, by delivery group, were estimated using parametric methods. Hazard ratios, by exposure, were estimated using semiparametric models.
Results
Among 1528 women (778 in the cesarean birth group, 565 in the spontaneous vaginal birth group, and 185 in the operative vaginal birth group), the median age at first delivery was 30.6 years, 1092 women (72%) were multiparous at enrollment (2887 total deliveries), and the median age at enrollment was 38.3 years. During a median follow-up of 5.1 years (7804 person-visits), there were 138 cases of SUI, 117 cases of OAB, 168 cases of AI, and 153 cases of POP. For spontaneous vaginal delivery (reference), the 15-year cumulative incidences of pelvic floor disorders after first delivery were as follows: SUI, 34.3% (95% CI, 29.9%-38.6%); OAB, 21.8% (95% CI, 17.8%-25.7%); AI, 30.6% (95% CI, 26.4%-34.9%), and POP, 30.0% (95% CI, 25.1%-34.9%). Compared with spontaneous vaginal delivery, cesarean delivery was associated with significantly lower hazard of SUI (adjusted hazard ratio [aHR], 0.46 [95% CI, 0.32-0.67]), OAB (aHR, 0.51 [95% CI, 0.34-0.76]), and POP (aHR, 0.28 [95% CI, 0.19-0.42]), while operative vaginal delivery was associated with significantly higher hazard of AI (aHR, 1.75 [95% CI, 1.14-2.68]) and POP (aHR, 1.88 [95% CI, 1.28-2.78]). Stratifying by delivery mode, the hazard ratios for POP, relative to a genital hiatus size less than or equal to 2.5 cm, were 3.0 (95% CI, 1.7-5.3) for a genital hiatus size of 3 cm and 9.0 (95% CI, 5.5-14.8) for a genital hiatus size greater than or equal to 3.5 cm.
Conclusions and Relevance
Compared with spontaneous vaginal delivery, cesarean delivery was associated with significantly lower hazard for stress urinary incontinence, overactive bladder, and pelvic organ prolapse, while operative vaginal delivery was associated with significantly higher hazard of anal incontinence and pelvic organ prolapse. A larger genital hiatus was associated with increased risk of pelvic organ prolapse independent of delivery mode.
This cohort study describes the incidence of urinary incontinence, organ prolapse, and other pelvic floor disorders among women who gave birth via cesarean, spontaneous vaginal, or operative vaginal delivery.
Introduction
Pelvic floor disorders, including urinary incontinence, anal incontinence (AI), and pelvic organ prolapse (POP), are common in women worldwide. Nygaard et al1 found that approximately 25% of women in the United States from 2005 to 2006 had at least 1 pelvic floor disorder, with the rate more than doubled for women older than 80 years. A woman’s lifetime risk of surgery for POP or stress urinary incontinence (SUI) was estimated to be 20%2 in 2014, and, in 2008, the 10-year reoperation rate was estimated to be 17%.3 The US population aged 65 years and older is expected to double between 2010 and 2050,4 further increasing the burden and costs of pelvic floor disorders on the health care system.
Despite recent advances, the biological mechanisms underlying pelvic floor disorders remain uncertain. Epidemiologic studies suggest that pelvic floor disorders are associated with childbirth, because these conditions are strongly associated with parity5 and are more common after vaginal birth vs cesarean birth.6 Little is known, however, about the association of various obstetrical exposures with the course and progression of pelvic floor disorders during a woman's life. The goals of this study were to describe the incidence of pelvic floor disorders after childbirth and to identify maternal and obstetrical characteristics associated with patterns of incidence in the first 1 to 2 decades after childbirth.
Methods
This study was approved by the Johns Hopkins and Greater Baltimore Medical Center institutional review boards. All enrolled participants provided written informed consent. Data were derived from the Mother’s Outcome after Delivery (MOAD) study,6 a longitudinal cohort study of parous women. From October 2008 to December 2013, participants were recruited from a community hospital 5 to 10 years after their first delivery (index birth) and followed up annually for up to 9 years. Follow-up ended in April 2017. Participants were identified based on hospital discharge diagnoses, and eligibility was confirmed by medical record review and telephone interview. Each eligible delivery was classified as either a vaginal birth or cesarean birth. Each delivery was also classified by the woman’s age at delivery (organized into 5-year strata) and the number of years from first delivery to recruitment (organized into one-fourth–year strata). The recruitment strategy was to match women who delivered by cesarean and vaginal births for age at first delivery and years since first delivery. Eligible women were randomly selected for recruitment until the desired sample size was achieved. Detailed recruitment methods have been published.6 Exclusion criteria (applied to the index birth) included maternal age younger than 15 or older than 50 years, delivery at less than 37 weeks’ gestation, placenta previa, multiple gestation, known fetal congenital anomaly, stillbirth, prior myomectomy, and abruption. Women who developed these events during subsequent pregnancies were not excluded.
Exposures
Medical records were reviewed for maternal and obstetrical characteristics. To explore the potential association between pelvic floor disorders and operative vaginal delivery,6 each delivery was classified as a cesarean birth, a spontaneous vaginal birth, or an operative vaginal birth (eg, delivery with the use of forceps, vacuum-assisted vaginal delivery). Each participant was classified according to all routes of delivery at the time of study entry. Specifically, the cesarean birth group included women who delivered only by cesarean birth, the spontaneous vaginal birth group was composed of women who experienced at least 1 spontaneous vaginal birth but no operative vaginal deliveries, and the operative vaginal birth group included women who had at least 1 operative vaginal delivery. For multiparous women, if the medical record of a subsequent delivery was not available (eg, for <5% of deliveries that occurred at nonaffiliated hospitals), the woman’s description of her birth was used to classify her obstetrical exposure, because it has been demonstrated that the agreement between maternal recall and obstetrical medical record information for birth mode is excellent.7
Outcomes
Primary outcomes included the incidence of 4 pelvic floor disorders: SUI, overactive bladder (OAB), AI, and POP. These outcomes were assessed annually via the Epidemiology of Prolapse and Incontinence Questionnaire (EPIQ)8 and a physical examination (gynecologic, height, and weight information). The EPIQ was included as a component of the online study questionnaire that was accessed via a link sent to participants by the research team. The EPIQ was used to identify the presence of SUI, defined as leakage of urine with activities that increase intra-abdominal pressure; OAB, defined as urinary urgency and frequency, often with urgency incontinence; and AI, defined as involuntary loss of solid stool, liquid stool, or gas.8 The EPIQ uses a scale of 0 to 100, with 100 representing the worst symptoms. Higher scores than previously validated thresholds have been shown to correspond to clinically significant disorders: SUI, 47.3; OAB, 59.6; AI, 22.8.8 Women with scores exceeding these thresholds were considered to have the corresponding condition. POP was assessed via physical examination using the Pelvic Organ Prolapse Quantification System (POP-Q),9 and was defined as descent of the vaginal walls or cervix beyond the hymen during the Valsalva maneuver (ie, bearing down as if having a bowel movement).10 In addition, the study questionnaire asked participants to report past treatment for pelvic floor disorders, including surgical procedures, supervised pelvic muscle exercises, pessary use, and use of medication to improve bladder control. Women who reported receiving therapy for a specific pelvic floor disorder were considered to have that condition, regardless of current symptoms. Women who reported pessary use were only classified as having POP if they also met the criteria after a physical examination (eg, protrusion beyond the hymen). During annual follow-up visits, study personnel were blinded to the participants’ obstetrical history and to current symptoms.
Additional Covariates
Other covariates were assessed at baseline and at annual follow-up visits. Parity was self-reported. Age at first delivery was categorized by the following approximate tertiles: younger than 30 years, 30 to 34 years, and 35 years or older. Body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) was measured at each annual follow-up visit and categorized for analyses as less than 25 (normal weight or reference), 25 to 29 (overweight), or greater than or equal to 30 (obese). Race was also assessed, because studies have suggested an association between pelvic floor disorders and race.11,12 Participants’ race/ethnicity (categorized as American Indian or Alaska Native, Asian, black or African American, Native Hawaiian or other Pacific Islander, white, or other) was self-reported. For analysis, race/ethnicity was dichotomized as black vs nonblack; Asian women and women who indicated “other” accounted for only 5.2% of the study population and were therefore included with the largest racial category to minimize misclassification in statistical inferences.
An additional covariate of interest was genital hiatus size, which has been associated with POP progression over time.13 Genital hiatus size was measured annually during the POP-Q9 assessment and is defined as the distance (in centimeters) from the middle of the external urethral meatus to the posterior midline hymen measured during the maximal Valsalva maneuver. For this analysis, genital hiatus size was classified by approximate tertiles of the overall population based on the distribution of values measured to the nearest half-centimeter at enrollment (≤2.5 cm, 3 cm, or ≥3.5 cm).
Data Analysis
In describing the incidence of pelvic floor disorders, each woman’s first delivery was considered as the time origin, with the aim to describe the cumulative incidence of each pelvic floor disorder from that origin. Some participants had already developed a pelvic floor disorder before enrollment (left censored), others developed pelvic floor disorders during study observation (uncensored), and the remainder of women had no pelvic floor disorders at the end of follow-up (right censored). Conventional lognormal models were used to estimate and compare, by delivery mode, the cumulative incidences of each pelvic floor disorder over time. In addition, the log-normal model yields estimates of time ratios,14 which reflect the relative time to event for each pelvic floor disorder by delivery mode (ie, the extent by which a delivery group either contracts or expands the time to event relative to the reference group).
The contribution of the left-censored data provided by women with pelvic floor disorders at enrollment permitted the estimation of the cumulative incidence less than 5 years after the first delivery. Cumulative incidence estimates for that period were obtained using maximum likelihood methods,14 concatenating the information provided by the full data (prevalent as left censored, incident as uncensored, and event-free as right censored). The use of a parametric survival model (eg, log-normal) allows estimates of the cumulative incidence over the entire period, starting at first delivery. Additional details about the statistical methods are provided in the eMethods in the Supplement.
The second goal of this study was to identify maternal and obstetrical characteristics associated with incidence of pelvic floor disorders. As previously noted, some participants developed a pelvic floor disorder before enrollment (left censored or prevalent at enrollment). The study, by design, collected prospective data only as recent as 5 years after a woman’s first delivery (ie, no women were enrolled before that milestone). Although data from the women prevalent at enrollment were used in the descriptions of the incidence of pelvic floor disorders during the 5 years after first delivery, these cases occurred before study observation and therefore these events could not be used to model the relative hazard of exposures of interest. Hence, in the analysis of relative hazard, the origin was defined at 5 years from first delivery, and cases of women prevalent at enrollment were excluded.
Methods appropriate for staggered entries14 (ie, staggered by the number of years past 5 years after first delivery when the participant was recruited) were used to appropriately account for participants surviving disorder-free until entry into the study. The inclusion of staggered entries not only controlled for survival bias, but also compensated for the truncation of participants who developed pelvic floor disorders before enrollment. To characterize the association with fixed (race, delivery group) and time-varying (BMI, parity, genital hiatus size) exposures, classic semiparametric proportional hazards models were used. The summary measures of these associations were the hazard ratios (HRs) of the hazard rate of the exposure of interest relative to the hazard rate of the reference group. To facilitate the interpretation of the putative protective association with cesarean delivery and the deleterious association with operative vaginal delivery relative to spontaneous vaginal delivery, spontaneous vaginal delivery was used as the reference category. To check the proportionality assumption, the HRs of delivery groups were allowed to vary over time, which was accomplished by including interactions between time, where the origin is 5 years after first delivery, and delivery group in the model. These interaction terms between time and delivery group were tested for significance in the final multivariable models.
Studies have suggested that genital hiatus size may be affected by the mode of delivery (ie, vaginal delivery may result in a wider genital hiatus than cesarean delivery).13 Thus, genital hiatus size may be part of a causal pathway between delivery mode and the incidence of pelvic floor disorders. Therefore, this variable was not considered a possible confounder of delivery mode in the multivariable analysis. Instead, to characterize the association of genital hiatus size with the 4 pelvic floor disorders in women with the same delivery mode, the analysis was stratified by delivery mode.
Although data were complete for all variables at study entry, not all the participants provided time-varying exposures (eg, BMI, genital hiatus size) at all follow-up visits. Missing data for these exposures were imputed with a 1-visit carry-forward method (ie, if a value was missing from a visit, the value from the previous visit was used, but only once). This occurred in only 306 of 7804 person-visits (3.9%).
For all measures of association, the corresponding 2-sided 95% CIs are reported and statistical significance is attached to intervals not containing the null value of 1. Analyses were conducted using SAS version 9.4 (SAS Institute) and Stata version 15 (StataCorp), and graphics were created using R version 3.4.3 (R Foundation).
Results
Based on medical record review, 12 691 eligible women were identified, of whom 7948 were approached for recruitment. Study personnel were able to contact and confirm eligibility for 4072 women (51%). Of these 4072 women, 1528 (38%) enrolled. Participation did not differ by delivery mode.6 Median age at first delivery differed minimally between women who enrolled and women who declined (30.6 years vs 31.6 years).
Among the 1528 study participants, 778 women were in the cesarean birth group, 565 women were in the vaginal birth group, and 185 women were in the operative vaginal birth group. The total number of deliveries was 2887; 436 women (28%) had 1 delivery, 851 (56%) had 2, and 241 (16%) had at least 3. Among multiparous (ie, more than 1 birth) women, the transition between cesarean and vaginal delivery mode was infrequent. In particular, of 511 women whose first delivery was cesarean and had a subsequent birth, only 24 had a subsequent vaginal birth (21 spontaneous vaginal deliveries and 3 operative vaginal deliveries).
Table 1 describes the study population characteristics at enrollment and follow-up information. Women in the cesarean birth group made 4039 person-visits, the spontaneous vaginal birth group made 2817 person-visits, and the operative vaginal delivery birth group made 948 person-visits. Loss to follow-up (defined as no follow-up visits 2 years before the conclusion of follow-up in April 2017) was similar in the 3 delivery groups (37%, 34%, and 36% for cesarean birth, spontaneous vaginal birth, and operative vaginal birth groups, respectively) and the data from these women were considered right-censored in the analysis. Overall, the median age at enrollment was 38.3 years. The youngest woman in the study at enrollment was aged 22.7 years and the oldest woman at the end of the study was aged 61.7 years. The longest time after first delivery when a participant was seen in the study was 18.7 years. As previously noted for this cohort,13,15 delivery type was associated with BMI and genital hiatus size, with major differences between cesarean delivery and vaginal delivery (spontaneous vaginal and operative vaginal delivery were not significantly different from each other).
Table 1. Characteristics of Women Enrolled in a Study Examining the Association of Delivery Mode With Pelvic Floor Disorders .
| Group, No. (%) | |||
|---|---|---|---|
| Cesarean Birth (n = 778) | Spontaneous Vaginal Birth (n = 565) | Operative Vaginal Birth (n = 185) | |
| Age at first delivery, y | |||
| <30 | 296 (38.1) | 237 (42.0) | 60 (32.4) |
| 30-34 | 263 (33.8) | 185 (32.7) | 79 (42.7) |
| ≥35 | 219 (28.2) | 143 (25.3) | 46 (24.9) |
| Primary race/ethnicity | |||
| White | 596 (76.6) | 462 (81.8) | 157 (84.9) |
| Black | 139 (17.9) | 77 (13.6) | 18 (9.7) |
| Asian | 15 (1.9) | 15 (2.7) | 8 (4.3) |
| Other | 28 (3.6) | 11 (2.0) | 2 (1.1) |
| Deliveries at enrollment | |||
| 1 | 252 (32.4) | 137 (24.3) | 47 (25.4) |
| 2 | 423 (54.4) | 324 (57.4) | 104 (56.2) |
| ≥3 | 103 (13.2) | 104 (18.4) | 34 (18.4) |
| BMI at enrollment | |||
| <25 | 303 (39.0) | 283 (50.1) | 110 (59.5) |
| 26-29 | 206 (26.5) | 176 (31.1) | 51 (27.6) |
| ≥30 | 269 (34.6) | 106 (18.7) | 24 (13.0) |
| Genital hiatus size at enrollment, cma | |||
| ≤2.5 | 624 (80.2) | 216 (38.2) | 69 (37.3) |
| 3 | 114 (14.7) | 132 (23.4) | 37 (20.0) |
| ≥3.5 | 40 (5.1) | 217 (38.4) | 79 (42.7) |
| No. of follow-up visitsb | |||
| 1-3 | 247 (31.8) | 164 (29.0) | 58 (31.4) |
| 4-6 | 222 (28.5) | 224 (39.7) | 58 (31.4) |
| 7-9 | 309 (39.7) | 177 (31.3) | 69 (37.3) |
| Stress urinary incontinence | 101 (13.0) | 149 (26.4) | 56 (30.3) |
| Overactive bladder | 81 (10.4) | 89 (15.8) | 45 (24.3) |
| Anal incontinence | 148 (19.0) | 129 (22.8) | 58 (31.4) |
| Pelvic organ prolapse | 39 (5.0) | 94 (16.7) | 56 (30.3) |
| Time from first delivery to study entry, median (IQR), y | 6.5 (5.6-8.2) | 6.2 (5.5-7.8) | 6.7 (5.6-8.5) |
| Time from first delivery to last follow-up, median (IQR), y | 11.4 (9.2-14.3) | 10.7 (9.1-13.4) | 11.4 (9.3-14.5) |
| Time from study entry to last follow up, median (IQR), y | 5.1 (2.1-7.0) | 5.0 (2.5-6.3) | 5.1 (2.1-7.1) |
| Follow-up visitsb | 4039 | 2817 | 948 |
| Person-years of follow-up | 3512 | 2440 | 829 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); IQR, interquartile range.
The genital hiatus size is the distance from the middle of the external urethral meatus to the posterior midline hymen, measured during the Valsalva maneuver.
Follow-up visits included 7804 annual participant assessments, of which 364 (4.7%) did not include a physical examination.
Of the 1528 women enrolled, the number of pelvic floor disorders prevalent at enrollment (ie, occurring between first delivery and the date of enrollment) and cases of pelvic floor disorders during follow-up in the study were as follows: 168 (11.0%) and 138 (9.0%), respectively, for SUI; 98 (6.4%) and 117 (7.7%), respectively, for OAB; 167 (10.8%) and 168 (11.0%), respectively, for AI; and 36 (2.4%) and 153 (10.0%), respectively, for POP. The total number of pelvic floor disorders and when they occurred informed the models to estimate the cumulative incidences (described in the eTable in the Supplement).
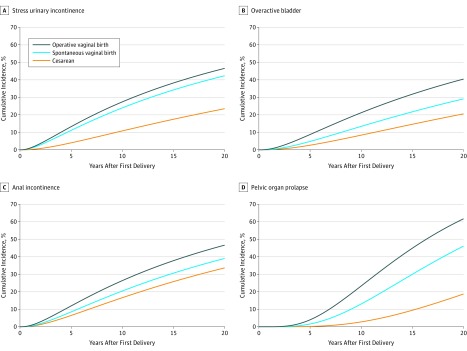
Figure 1 shows the cumulative incidence of each pelvic floor disorder over time, by delivery mode, based on log-normal models described in detail in the eTable in the Supplement. Time ratios are shown by delivery mode, with spontaneous vaginal birth as the reference category, in Table 2. Compared with spontaneous vaginal delivery, the time ratios associated with cesarean delivery were significantly higher (indicating the magnitude by which times to event were longer) for SUI (time ratio, 2.04 [95% CI, 1.63-2.56]), OAB (time ratio, 1.40 [95% CI, 1.13-1.73]), and POP (time ratio, 1.70 [95% CI, 1.48-1.95]). In contrast, the time ratios associated with operative vaginal delivery were significantly lower (indicating the magnitude by which times to event were shorter) than time ratios associated with spontaneous vaginal delivery for OAB (time ratio, 0.68 [95% CI, 0.51-0.91]) and POP (time ratio, 0.76 [95% CI, 0.66-0.89]).
Figure 1. Cumulative Incidence of Pelvic Floor Disorders by Delivery Mode.
Based on log-normal models (see the eTable in the Supplement). The number of events according to the delivery modes and type of pelvic floor disorder are included in Table 1.
Table 2. Time Ratios for Pelvic Floor Disordersa.
| Delivery Mode Group | Time Ratio (95% CI) | |||
|---|---|---|---|---|
| Stress Urinary Incontinence (n = 1360) | Overactive Bladder (n = 1430) | Anal Incontinence (n = 1361) | Pelvic Organ Prolapse (n = 1492) | |
| Cesarean | 2.04 (1.63-2.56) | 1.40 (1.13-1.73) | 1.20 (0.99-1.45) | 1.70 (1.48-1.95) |
| Spontaneous vaginal | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Operative vaginal | 0.87 (0.65-1.15) | 0.68 (0.51-0.91) | 0.78 (0.59-1.03) | 0.76 (0.66-0.89) |
Time ratios reflect the relative time to event for each pelvic floor disorder by delivery mode using spontaneous delivery as the reference group.
In addition, Figure 1 shows temporal distinctions among the different pelvic floor disorders. Some pelvic floor disorders, such as SUI, had a high incidence in the first few years after delivery. On the other hand, POP had a much longer latency after first delivery. Specifically, for spontaneous vaginal delivery (reference), the estimated 5-year cumulative incidences following first delivery were as follows: SUI, 11.1% (95% CI, 8.7%-13.5%); OAB, 4.8% (95% CI, 3.3%-6.3%); AI, 8.5% (95% CI, 6.4%-10.5%); and POP, 1.6% (95% CI, 0.9%-2.3%). The corresponding 15-year cumulative incidences were as follows: SUI, 34.3% (95% CI, 29.9%-38.6%); OAB, 21.8% (95% CI, 17.8%-25.7%); AI, 30.6% (95% CI, 26.4%-34.9%); and POP, 30.0% (95% CI, 25.1%-34.9%). For cesarean delivery, the estimated 5-year cumulative incidences following first delivery were the following: SUI, 4.0% (95% CI, 2.8%-5.2%); OAB, 2.6% (95% CI, 1.7%-3.6%); AI, 6.5% (95% CI, 4.9%-8.0%); and POP, 0.2% (95% CI, 0.1%-0.3%). The corresponding 15-year cumulative incidences for cesarean delivery were the following: SUI, 17.5% (95% CI, 14.5%-20.5%); OAB, 14.6% (95% CI, 11.8%-17.5%); AI, 25.8% (95% CI, 22.3%-29.3%); and POP, 9.4% (95% CI, 6.8%-12.1%). For operative vaginal delivery, the estimated 5-year cumulative incidences following first delivery were as follows: SUI, 13.3% (95% CI, 9.0%-17.5%); OAB, 8.7% (95% CI, 5.4%-12.1%); AI, 11.9% (95% CI, 8.0%-15.8%); and POP, 4.0% (95% CI, 2.0%-5.9%). The corresponding 15-year cumulative incidences for operative vaginal delivery were the following: SUI, 38.2% (95% CI, 31.0%-45.5%); OAB, 31.8% (95% CI, 24.7%-38.9%); AI, 37.8% (95% CI, 30.6%-44.9%); and POP, 44.9% (95% CI, 37.0%-52.8%).
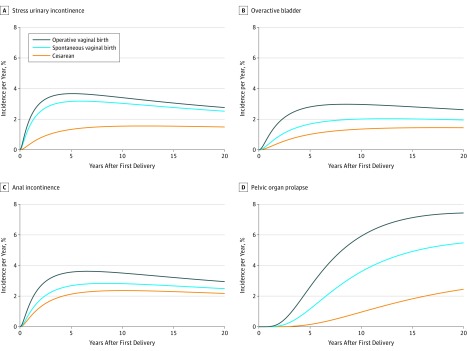
The corresponding hazard functions of each pelvic floor disorder are shown in Figure 2. Consistent with the time ratios shown in Table 2, the hazard of each pelvic floor disorder was highest among women in the operative vaginal birth group and lowest among women in the cesarean birth group. The curves for SUI demonstrate a very sharp rise in the hazard rate in the first few years following each woman’s first delivery. Specifically, the peak hazard rate was within the first 5 years of delivery, corresponding with the observed pattern of early onset for this condition. This was in contrast with POP, for which the peak hazard rate was estimated to occur more than 20 years after delivery. An additional observation was that the between-group differences for SUI were greatest in the first few years but waned thereafter. In contrast, the differences between delivery groups were sustained over time for POP.
Figure 2. Incidence Per Year of Pelvic Floor Disorders by Mode of Delivery and Years From First Delivery.
Each curve was created by dividing the rate of change of the cumulative incidence curve in Figure 1 by 1 minus the cumulative incidence.
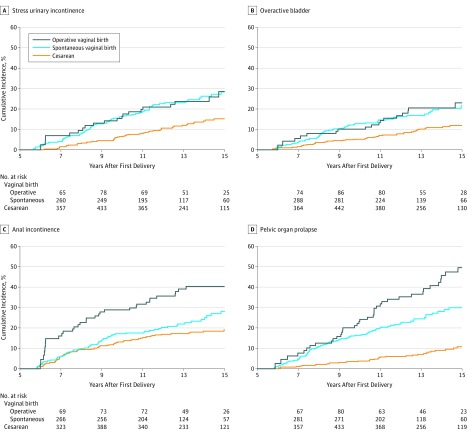
Figure 3 depicts the bivariable extended (ie, including left truncation or staggered entries) Kaplan-Meier curves of the 4 pelvic floor disorders starting 5 years after first delivery. Using these data, HRs were calculated for each pelvic floor disorder as a function of delivery mode group and the other maternal and obstetrical characteristics. Considering an interaction between delivery group and time, significant departures from proportionality were not detected. Table 3 presents the HRs and adjusted hazard ratios (aHRs) for each pelvic floor disorder, derived from bivariable and multivariable models, respectively. In both models, compared with spontaneous vaginal delivery (reference), cesarean delivery was associated with a significantly lower hazard of SUI (aHR, 0.46 [95% CI, 0.32-0.67]), OAB (aHR, 0.51 [95% CI, 0.34-0.76]), and POP (aHR, 0.28 [95% CI, 0.19-0.42]). Conversely, compared with spontaneous vaginal delivery, operative vaginal delivery had a significantly greater hazard of both AI (aHR, 1.75 [95% CI, 1.14-2.68]) and POP (aHR, 1.88 [95% CI, 1.28-2.78]).
Figure 3. Cumulative Incidence of Pelvic Floor Disorder by Mode of Delivery and Years From First Delivery.
The time scale starts at 5 years because the prevalent (left censored) cases were truncated to focus on incident cases observed in the study with concomitant annually collected longitudinal data on covariates. By delivery mode, median (IQR) years from first delivery to last follow up was 11.4 (9.2, 14.3) for cesarean birth, 10.7 (9.1, 13.4) for spontaneous vaginal birth, and 11.4 (9.3, 14.5) for operative vaginal birth.
Table 3. Hazard Ratios (HRs) for Pelvic Floor Disordersa.
| Stress Urinary Incontinence (n = 1360) | Overactive Bladder (n = 1430) | Anal Incontinence (n = 1361) | Pelvic Organ Prolapse (n = 1492) | |||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | aHR (95% CI) | HR (95% CI) | aHR (95% CI) | HR (95% CI) | aHR (95% CI) | HR (95% CI) | aHR (95% CI) | |
| Person-years | 5892 | 6383 | 5737 | 6424 | ||||
| Cases | 138 | 117 | 168 | 153 | ||||
| Delivery mode group | ||||||||
| Cesarean | 0.49 (0.34-0.71) | 0.46 (0.32-0.67) | 0.54 (0.36-0.80) | 0.51 (0.34-0.76) | 0.77 (0.55-1.08) | 0.72 (0.51-1.02) | 0.29 (0.19-0.43) | 0.28 (0.19-0.42) |
| Spontaneous vaginal | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Operative vaginal | 0.99 (0.60-1.64) | 1.07 (0.65-1.78) | 1.07 (0.63-1.83) | 1.07 (0.63-1.84) | 1.70 (1.11-2.59) | 1.75 (1.14-2.68) | 1.78 (1.21-2.60) | 1.88 (1.28-2.78) |
| Age at first delivery, y | ||||||||
| <30 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 30-34 | 0.75 (0.50-1.12) | 0.80 (0.53-1.21) | 1.11 (0.72-1.72) | 1.10 (0.70-1.73) | 1.07 (0.74-1.55) | 1.03 (0.71-1.49) | 0.89 (0.61-1.30) | 0.94 (0.64-1.37) |
| ≥35 | 0.92 (0.61-1.38) | 0.96 (0.62-1.48) | 1.26 (0.80-1.96) | 1.20 (0.74-1.94) | 1.33 (0.92-1.92) | 1.36 (0.92-2.01) | 0.98 (0.67-1.45) | 1.33 (0.88-2.01) |
| Race | ||||||||
| Nonblack | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Black | 1.02 (0.64-1.62) | 0.86 (0.52-1.42) | 1.06 (0.63-1.78) | 1.08 (0.62-1.87) | 0.46 (0.27-0.80) | 0.42 (0.24-0.73) | 0.84 (0.52-1.36) | 0.99 (0.60-1.65) |
| Parity | ||||||||
| 1 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 2 | 0.80 (0.54-1.19) | 0.82 (0.54-1.23) | 0.87 (0.58-1.30) | 0.88 (0.57-1.36) | 1.28 (0.89-1.85) | 1.37 (0.93-2.02) | 1.96 (1.25-3.06) | 2.07 (1.31-3.30) |
| ≥3 | 1.16 (0.72-1.87) | 1.13 (0.67-1.88) | 0.57 (0.31-1.06) | 0.56 (0.29-1.08) | 1.05 (0.63-1.75) | 1.12 (0.65-1.91) | 2.14 (1.26-3.64) | 2.08 (1.19-3.64) |
| BMI | ||||||||
| <25 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 25-29 | 1.25 (0.83-1.88) | 1.32 (0.87-2.00) | 0.72 (0.46-1.14) | 0.76 (0.48-1.21) | 1.21 (0.84-1.76) | 1.37 (0.94-1.99) | 0.97 (0.66-1.42) | 1.11 (0.76-1.63) |
| ≥30 | 1.62 (1.09-2.41) | 1.97 (1.29-3.01) | 1.02 (0.66-1.57) | 1.14 (0.72-1.81) | 1.59 (1.11-2.29) | 2.24 (1.53-3.20) | 0.97 (0.66-1.43) | 1.50 (0.99-2.26) |
| Genital hiatus size,b,c cm | ||||||||
| ≤2.5 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 3 | 1.84 (1.19-2.83) | 1.01 (0.59-1.73) | 1.65 (1.13-2.41) | 3.49 (2.02-6.03) | ||||
| ≥3.5 | 2.31 (1.57-3.40) | 2.09 (1.41-3.11) | 1.60 (1.12-2.27) | 11.74 (7.51-18.4) | ||||
Abbreviations: aHR, adjusted hazard ratio; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Hazard ratios were derived from bivariable analysis and adjusted hazard ratios were derived from multivariable analysis .
The genital hiatus size is the distance from the middle of the external urethral meatus to the posterior midline hymen, measured during the Valsalva maneuver.
Genital hiatus size was not included in the multivariable analysis because this variable is likely to be in causal pathway of delivery mode.
With respect to the associations of other variables in the multivariable model, Table 3 shows that black women had a reduced hazard of developing AI (aHR, 0.42 [95% CI, 0.24-0.73]) and obese women were at significantly greater hazard of developing both SUI (aHR, 1.97 [95% CI, 1.29-3.01]) and AI (aHR, 2.24 [95% CI, 1.53-3.20]). Parity of at least 3 was significantly associated with an increasing hazard of POP (aHR, 2.08 [95% CI, 1.19-3.64]). Age at first delivery was not associated with the hazard of any of these disorders.
As noted in Table 3, genital hiatus size was significantly associated with each of the 4 pelvic floor disorders. Further analyses revealed that for each mode of delivery, there were significant associations between increasing genital hiatus size and the incidence of pelvic floor disorders. This association was most notable for POP; among women with the same delivery mode (ie, stratified by delivery mode in a proportional hazards model) and relative to a genital hiatus size of 2.5 cm or less, the HRs for POP were 3.0 (95% CI, 1.7-5.3) for a genital hiatus size of 3 cm and 9.0 (95% CI, 5.5-14.8) for a genital hiatus size greater than or equal to 3.5 cm. This association was present in each of the delivery groups. The corresponding HRs for genital hiatus size of 3 cm and genital hiatus size greater than or equal to 3.5 cm were 2.7 (95% CI, 1.2-6.2) and 8.0 (95% CI, 3.7-17.2), respectively, for cesarean delivery; 3.0 (95% CI, 1.1-8.7) and 10.4 (95% CI, 4.2-25.8), respectively, for spontaneous vaginal delivery; and 4.5 (95% CI, 1.2-16.9) and 9.8 (95% CI, 3.0-32.1), respectively, for operative vaginal delivery.
Discussion
Results of this study showed a substantial difference in pelvic floor disorder incidence based on a woman’s obstetrical characteristics. The cumulative incidence of each pelvic floor disorder was significantly associated with delivery mode. Compared with spontaneous vaginal delivery, cesarean delivery was significantly associated a with lower hazard of SUI, OAB, and POP. Furthermore, operative vaginal delivery was significantly associated with a higher hazard of AI and POP. The association with delivery mode was most pronounced for POP.
Two longitudinal studies investigated the association between incontinence and delivery mode. In the first study, among 278 Danish primiparous women who completed questionnaires 2 to 5 days, 3 months, and 5 years after delivery,16 no difference was found in the incidence of SUI by mode of delivery. However, only 18% of participants in this study delivered by cesarean birth, limiting the power. In the second study,17,18,19 3763 women from the United Kingdom and New Zealand completed questionnaires 3 months, 6 years, and 12 years after delivery. Compared with spontaneous vaginal delivery, cesarean delivery was associated with a lower risk of urinary incontinence (odds ratio, 0.46 [95% CI, 0.37-0.58]). At 12 years, POP was assessed in a subset of women (n = 762) and was found to be less common in women who delivered exclusively by cesarean birth (odds ratio, 0.11 [95% CI, 0.03-0.38]).
Data from the present study build on those observations by providing a more complete picture of incidence over time. For example, this study illustrated differences in the progression over time of the 4 pelvic floor disorders. POP, for instance, had a longer latency after childbirth than SUI and AI. These temporal differences may explain the different patterns seen in surgery for POP and SUI. Wu et al2 reported that the annual risk of surgery for SUI has 2 peaks: at 46 and at 70 to 71 years of age. In contrast, the annual risk of surgery for POP increased with age, with the highest risk for women aged 71 to 73 years. The difference in latency observed in the present study may also suggest different causation of the various pelvic floor disorders. For example, there is mounting evidence that some cases of POP may be caused by trauma to the levator ani muscle.20,21 Although such injuries are not typically evident at the time of delivery, research studies using either 3-D ultrasonography or magnetic resonance imaging have detected significant levator ani trauma after 10% to 20% of vaginal deliveries.22,23 The effect of levator ani muscle injury on the pelvic floor appears to evolve over decades, resulting in a long latency for symptomatic POP. In contrast, the urethral sphincteric mechanism may be a stronger predictor of symptoms of incontinence, and injury to that mechanism with vaginal delivery may explain the relatively early onset after delivery for incontinence disorders.24
In addition, genital hiatus size was significantly associated with hazard for the 4 pelvic floor disorders analyzed, especially POP. Among women with the same mode of delivery, including women in the cesarean birth group, there was a statistically and clinically significant association between genital hiatus size and POP. A strength of the analysis was the availability of repeated assessments of genital hiatus size over time, which were included as such in the analysis. Thus, genital hiatus size is viable as a marker to monitor the risk of POP over time. Indeed, the changes in genital hiatus may actually be a mechanism for the development of POP, regardless of delivery mode.
This study had many additional strengths. The primary strength was the longitudinal design. Longitudinal studies of pelvic floor disorders are rare, particularly for POP because of the logistical burden and cost associated with repeated gynecologic examinations. Second, the cohort was large enough to examine differences by delivery mode, and the follow-up was sufficient to model changes in incidence over time. Third, the tools used to measure pelvic floor disorders were validated, including the use of a structured examination to assess pelvic organ support. Fourth, the use of models that account for time-varying measures (eg, BMI and genital hiatus) allowed the description of the relative hazard as a function of the current status of the participants, based on the BMI and genital hiatus size at each point in time. Although the primary exposure (ie, delivery mode) was considered fixed, there was little misclassification because transitions between delivery modes were infrequent. Fifth, statistical methods were implemented to maximize the information provided by the prevalent cases handling them as left censored observations for the description of the incidence of pelvic floor disorders, using years from first delivery as the time scale. In turn, the time scale changed to years after 5 years from first delivery to focus on incident cases, and staggered entries were used to examine the women who entered the study without pelvic floor disorders.
Limitations
This study had several limitations. First, although pelvic floor disorders were determined with validated research tools, some misclassification was possible. Second, the use of dichotomous definitions of pelvic floor disorders is an oversimplification because worsening of a mild pelvic floor disorder over time may also be clinically relevant. Third, although, to our knowledge, this is the longest cohort study on the epidemiology of pelvic floor disorders to date, the duration of follow-up was not adequate to look at patterns of hazard in older women. Fourth, the sample size was not sufficient to further explore some risk factors. For example, there was a limited number of women with a high parity and, therefore, the findings cannot be extrapolated to women who may have experienced 4 or more deliveries. Fifth, the data were from a single institution, so the results may not be generalizable to all populations. Sixth, because there were 4 coprimary outcomes and multiple subgroup comparisons without adjustment for multiple comparisons, it is possible that some of the statistically significant findings may reflect type I error.
Conclusions
Compared with spontaneous vaginal delivery, cesarean delivery was associated with significantly lower hazard of SUI, OAB, and POP, while operative vaginal delivery was associated with significantly higher hazard of AI and POP. A larger genital hiatus was associated with an increased risk of POP independent of delivery mode.
eMethods
eReferences
eTable 1
References
- 1.Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311-1316. doi: 10.1001/jama.300.11.1311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201-1206. doi: 10.1097/AOG.0000000000000286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Denman MA, Gregory WT, Boyles SH, Smith V, Edwards SR, Clark AL. Reoperation 10 years after surgically managed pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol. 2008;198(5):555.e1-555.e5. doi: 10.1016/j.ajog.2008.01.051 [DOI] [PubMed] [Google Scholar]
- 4.Vincent GK, Velkoff VA. The Next Four Decades–the Older Population in the United States: 2010 to 2050. Washington, DC: US Census Bureau; 2010. https://www.census.gov/prod/2010pubs/p25-1138.pdf. [Google Scholar]
- 5.Mant J, Painter R, Vessey M. Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study. Br J Obstet Gynaecol. 1997;104(5):579-585. doi: 10.1111/j.1471-0528.1997.tb11536.x [DOI] [PubMed] [Google Scholar]
- 6.Handa VL, Blomquist JL, Knoepp LR, Hoskey KA, McDermott KC, Muñoz A. Pelvic floor disorders 5-10 years after vaginal or cesarean childbirth. Obstet Gynecol. 2011;118(4):777-784. doi: 10.1097/AOG.0b013e3182267f2f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen C, Smith LJ, Pierce CB, Blomquist JL, Handa VL. Do symptoms of pelvic floor disorders bias maternal recall of obstetrical events up to 10 years after delivery? Female Pelvic Med Reconstr Surg. 2015;21(3):129-134. doi: 10.1097/SPV.0000000000000158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lukacz ES, Lawrence JM, Buckwalter JG, Burchette RJ, Nager CW, Luber KM. Epidemiology of prolapse and incontinence questionnaire: validation of a new epidemiologic survey. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(4):272-284. doi: 10.1007/s00192-005-1314-5 [DOI] [PubMed] [Google Scholar]
- 9.Bump RC, Mattiasson A, Bø K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10-17. doi: 10.1016/S0002-9378(96)70243-0 [DOI] [PubMed] [Google Scholar]
- 10.Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783-1790. doi: 10.1007/s00192-013-2169-9 [DOI] [PubMed] [Google Scholar]
- 11.Whitcomb EL, Rortveit G, Brown JS, et al. Racial differences in pelvic organ prolapse. Obstet Gynecol. 2009;114(6):1271-1277. doi: 10.1097/AOG.0b013e3181bf9cc8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thom DH, van den Eeden SK, Ragins AI, et al. Differences in prevalence of urinary incontinence by race/ethnicity. J Urol. 2006;175(1):259-264. doi: 10.1016/S0022-5347(05)00039-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Handa VL, Blomquist JL, Roem J, Muňoz A. Longitudinal study of quantitative changes in pelvic organ support among parous women. Am J Obstet Gynecol. 2018;218(3):320.e1-320.e7. doi: 10.1016/j.ajog.2017.12.214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cox C, Chu H, Schneider MF, Muñoz A. Parametric survival analysis and taxonomy of hazard functions for the generalized gamma distribution. Stat Med. 2007;26(23):4352-4374. doi: 10.1002/sim.2836 [DOI] [PubMed] [Google Scholar]
- 15.Britz SE, McDermott KC, Pierce CB, Blomquist JL, Handa VL. Changes in maternal weight 5-10 years after a first delivery. Womens Health (Lond). 2012;8(5):513-519. doi: 10.2217/WHE.12.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Viktrup L. The risk of lower urinary tract symptoms five years after the first delivery. Neurourol Urodyn. 2002;21(1):2-29. doi: 10.1002/nau.2198 [DOI] [PubMed] [Google Scholar]
- 17.MacArthur C, Glazener C, Lancashire R, Herbison P, Wilson D, ProLong study group . Exclusive caesarean section delivery and subsequent urinary and faecal incontinence: a 12-year longitudinal study. BJOG. 2011;118(8):1001-1007. doi: 10.1111/j.1471-0528.2011.02964.x [DOI] [PubMed] [Google Scholar]
- 18.MacArthur C, Glazener CM, Wilson PD, Lancashire RJ, Herbison GP, Grant AM. Persistent urinary incontinence and delivery mode history: a six-year longitudinal study. BJOG. 2006;113(2):218-224. doi: 10.1111/j.1471-0528.2005.00818.x [DOI] [PubMed] [Google Scholar]
- 19.Glazener C, Elders A, MacArthur C, et al. ; ProLong Study Group . Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. BJOG. 2013;120(2):161-168. doi: 10.1111/1471-0528.12075 [DOI] [PubMed] [Google Scholar]
- 20.DeLancey JO, Morgan DM, Fenner DE, et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109(2):295-302. doi: 10.1097/01.AOG.0000250901.57095.ba [DOI] [PubMed] [Google Scholar]
- 21.Dietz HP, Simpson JM. Levator trauma is associated with pelvic organ prolapse. BJOG. 2008;115(8):979-984. doi: 10.1111/j.1471-0528.2008.01751.x [DOI] [PubMed] [Google Scholar]
- 22.DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101(1):46-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shek KL, Dietz HP. Intrapartum risk factors for levator trauma. BJOG. 2010;117(12):1485-1492. doi: 10.1111/j.1471-0528.2010.02704.x [DOI] [PubMed] [Google Scholar]
- 24.Delancey JO. Why do women have stress urinary incontinence? Neurourol Urodyn. 2010;29(suppl 1):s13-s17. doi: 10.1002/nau.20888 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
eReferences
eTable 1