Abstract
Objective
Although there is evidence that Attention Deficit Hyperactivity Disorder (ADHD) symptoms are positively related to alcohol use and related problems among young adults, little research has examined the mechanisms that might explain this association. In response, this study examined the mediating effects of coping and enhancement drinking motives on the prospective associations between ADHD symptoms and alcohol outcomes.
Method
Participants (N = 4,536) were young men from the Cohort Study on Substance Use Risk Factors. Measures of ADHD symptoms and those of drinking motives, heavy episodic drinking (HED) and alcohol use disorder symptoms were used from the baseline and 15-month follow-up assessments.
Results
Findings indicated that the associations of ADHD-inattention symptoms with alcohol use disorder (AUD) symptoms and with HED were partially and completely mediated through drinking motives, respectively, whereas drinking motives did not mediate the ADHD-hyperactivity/impulsivity-symptoms-alcohol outcomes associations.
Conclusion
Results indicated that coping and enhancement motives partially explained the ADHD-inattention symptoms—subsequent alcohol outcomes association. These findings suggest that interventions targeting enhancement and coping motives may help prevent problematic drinking among young men with elevated ADHD-inattention symptoms.
Introduction
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by inattentive (e.g., often distracted by extraneous stimuli) and/or hyperactive-impulsive symptoms (e.g., excessive talking) affecting 5–10% of school-age children [1, 2]. Contrary to the widespread belief that ADHD outgrows as children mature, longitudinal studies have shown that ADHD symptoms persist into adulthood in up to 65% of cases [3]. Accordingly, epidemiological studies indicate that adult ADHD prevalence is between 1.0–7.5% worldwide, [4–8], with prevalence rates being higher in young males (5.4%) than in young females (3.2%) [4]. Alarmingly, adult ADHD has been consistently related to social (e.g., high prevalence of adult ADHD in incarcerated populations) and professional functional impairments (e.g., unemployment), thereby producing costly societal burden [4, 9–12]. Furthermore, psychological comorbidities (e.g., depression, antisocial personality disorder) are common among adults with ADHD, potentially leading to further functional impairments [5, 8, 13].
There is also evidence that ADHD is a correlate of problematic drinking in adults [14, 15]. Notably, besides often co-occurring, there is evidence that ADHD and alcohol use disorder (AUD) share similar signs and symptoms [16]. Specifically, both ADHD and AUD have been associated with neuropsychological impairments in diverse domains, including executive functioning and working memory [1, 17, 18]. Given their similarities and their co-occurrence, research has started to examine both ADHD and AUD together. A line of this research has focused on the mechanisms through which ADHD may promote alcohol outcomes. This study aims to contribute to this field of research by examining whether coping and enhancement drinking motives—drinking to attenuate negative affects and to enhance positive mood or well-being, respectively—mediate the prospective association between ADHD symptoms and alcohol outcomes among young men. Examining this question may be especially relevant in young males considering their elevated rates of both ADHD prevalence and risky drinking behaviors. Indeed, as mentioned earlier, prevalence rate of ADHD is higher among young than among young females [4]. Furthermore, among young adults, males have been consistently identified as being at greater risk regarding unhealthy drinking behaviors than females [19, 20]. Epidemiological research indicates for instance that prevalence rates of heavy episode drinking (HED, reporting > 60gr of pure alcohol on a single occasion) in the past 30 days are twice as high among young males compared with young females (i.e., ages 15–24; [21]).
Increasing evidence suggests that ADHD stands at the end of a continuum and that ADHD symptoms may occur in the absence of the full disorder [22, 23]. Accordingly, recent research has started to examine manifestations of ADHD symptoms even if they do not meet diagnostic threshold (e.g., [13, 24, 25]). Such examination allows capturing subclinical variations along the ADHD continuum, thereby providing valuable information for prevention. There is evidence that ADHD symptomatology is positively related to alcohol outcomes in nonclinical samples of youths and adults [14], even though some findings have been inconsistent across studies regarding inattention and hyperactivity/impulsivity dimensions [26, 27]. For instance, studies in youths (i.e., adolescents) found ADHD symptoms to be positively related to drinking frequency [14]. Hyperactivity/impulsivity (hereafter referred as ADHD-HI) symptoms have been positively related to alcohol use and related problems in adults and college students [13, 27], yet they were not significantly related to alcohol use and related-problems in two other studies among college students [24, 26]. Finally, some previous findings in the same populations have documented inattention symptoms (hereafter referred as ADHD-I) to be positively associated with alcohol use [24, 27], whereas others found opposite results [26]. Similarly, ADHD-I symptoms were found to be associated with alcohol-related problems in one research [27], whereas another study found this association to be significant among females, yet not among males [13].
Recent research has started to examine the mechanisms through which ADHD may promote alcohol outcomes. That said most studies examining this line of research has focused on the associations between childhood ADHD and subsequent AUD. For instance, a study conducted in the general adult population found that the positive association between childhood ADHD and future AUD was mediated by conduct disorders [28]. In another study, moderated-mediation analyses indicated that social impairment, delinquency and grade points significantly mediated the association between childhood ADHD and subsequent alcohol use among youths with lower parental knowledge of their child friendships, activities and whereabouts [29]. Some of these findings were corroborated by another study that found social impairment and delinquency as significant mediators of the association between childhood ADHD and future HED [30].
To the best of the authors’ knowledge, only three studies to date have attempted to identify factors that may explain the associations between ADHD symptoms and alcohol outcomes in samples of non-clinical adults. The two first studies were conducted among college students and identified disinhibition, difficulty stopping drinking, lack of premeditation and sensation seeking as significant mediators of the positive association between ADHD (diagnoses, symptoms) and current alcohol use and/or related consequences [27, 31]. The third study was conducted among college students in China [32]. The authors found that anxiety significantly mediated the association between ADHD-HI symptoms and alcohol behaviors (i.e., alcohol use, HED, intoxication), whereas depression mediated both the associations between ADHD-HI and alcohol behaviors, and the one between ADHD-IN and alcohol behaviors.
Other correlates of drinking that may play a role in the ADHD symptoms-alcohol outcomes association include drinking motives, which are considered among the most proximal factors for engaging in drinking behaviors [33, 34]. According to the motivational model of alcohol use, some individuals drink alcohol to enhance positive mood or well-being (i.e., enhancement drinking motives), and others to attenuate negative affects (i.e., coping drinking motives; [33, 35]). Given that ADHD is related to functional impairments and psychiatric problems, it is likely that individuals with elevated symptoms are motivated to use alcohol to seek relief from psychological distress and thus to endorse high coping drinking motives. In fact, coping with stressful events may be particularly challenging for individuals with ADHD because of executive functioning impairments, including inattention and distractibility [36, 37]; specifically, attention deficits may impede them to cognitively reappraising stressful situations and using adaptive strategies. Accordingly, a study conducted among adults with ADHD showed maladaptive coping strategies (e.g., escape-avoidance, less problem solving) to be the most endorsed in this population [38]
Similarly, it is likely that individuals with elevated ADHD symptoms endorse high enhancement drinking motives; indeed, considering that two core ADHD symptoms include being easily bored and having aversion of delayed reward, alcohol use may represent a means of reducing boredom feelings by providing immediate stimulation [39]. Echoing this hypothesis, past research has found significantly higher levels of sensation seeking (i.e., tendency to seek stimulation, novelty and risk; [40]) among individuals with ADHD than among controls [41, 42], with sensation seeking being mostly related to the hyperactivity/impulsivity dimension rather than to the inattention one [43].
As far as we are aware of, the mediating effect of coping and enhancement drinking motives on the association between ADHD symptoms and alcohol outcomes in adults has not been tested yet. As outlined below, very little research to date has explored mediators of the association between ADHD symptoms and alcohol outcomes in adults. Answering a call to conduct more research examining potential explanatory factors of this association in large samples [26], this study aimed at examining the mediating effect of enhancement and coping drinking motives on the ADHD symptoms-alcohol outcomes association in a large sample of young men in Switzerland. Gaining a better knowledge of the mechanisms explaining the association between ADHD symptoms and alcohol outcomes is important to tailor interventions aiming to decrease problematic drinking to young adults with ADHD symptoms. Specifically, this study aimed at evaluating the mediating effect of coping and enhancement drinking motives on the prospective associations of ADHD symptoms (ADHD-total symptoms [ADHD-I and ADHD-HI symptoms]; ADHD-I symptoms and ADHD-HI symptoms separately) with HED and AUD symptoms in a representative sample of young men in Switzerland.
Based on previous research, we expected that ADHD symptoms would be positively related to subsequent alcohol outcomes. We also expected that these associations would be partially mediated by both drinking motives with models testing ADHD-HI symptoms being mediated by enhancement drinking motives and those testing ADHD-I by coping drinking motives.
Methods
Procedure and participants
This study used data from the Cohort Study on Substance Use Risk Factors designed to examine substance-use trajectories among young Swiss men. Recruitment took place between August 2010 and July 2011 in three of a total of six recruitment centers covering 21 of the 26 Swiss cantons (including French and German-speaking cantons). In Switzerland, all Swiss men aged approximately 19 must undergo a recruitment process to determine their eligibility for military service. All young men were eligible for inclusion, independently of whether they were deemed eligible or not to serve in the army. Thus, virtually all men aged 19–20 in the 21 covered cantons were eligible for inclusion in the study. Participants completed questionnaires outside of the army environment. At baseline, conscripts who gave consent to participate were invited by email (or by mail if they asked so) within two weeks to complete a paper pencil questionnaire or an online questionnaire. Then, they received an email (or a mail if they preferred) to complete the follow-up assessment using an online questionnaire (or a paper-pencil questionnaire if they preferred; 45–60 minutes duration on average). Participants received a voucher after completion of each survey (i.e., CHF 30—around $30 for the baseline and for the follow-up 1 and CHF 50—around $50 for the follow-up 2 assessment). More details regarding the parent study procedures are provided elsewhere [44]. In the current study, we used data from the baseline and 15-month follow-up assessments. All procedures were approved by the institutional review board (ethic committee of the Canton de Vaud, research protocol number 15/07).
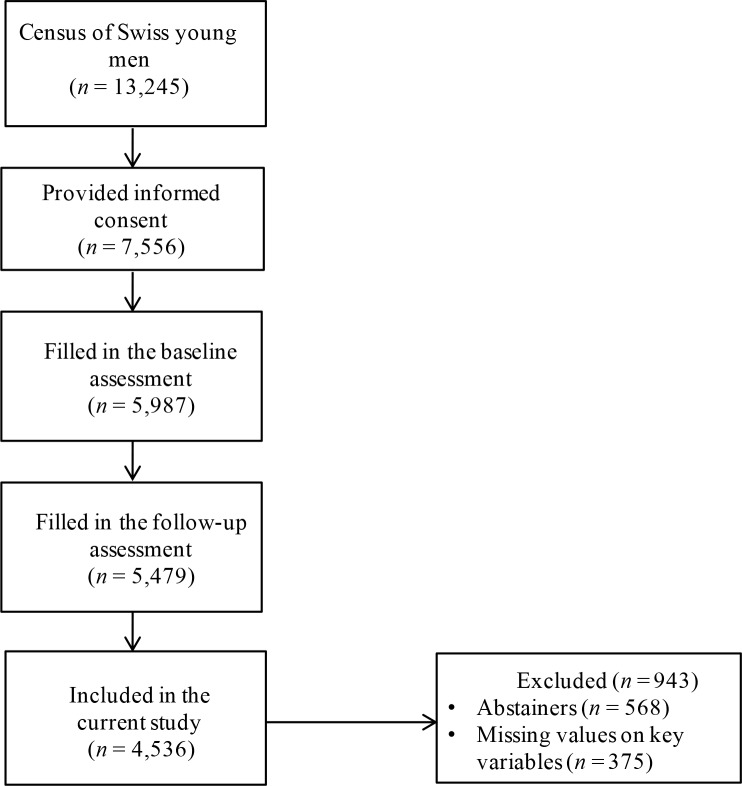
A total of 7,556 conscripts provided written informed consent to participate in the study. Of those, 5,987 (79.2%) completed the baseline assessment between September 2010 and March 2012, and among them 5,479 (91.5% of the baseline sample) completed the follow-up assessment between March 2012 and January 2014. Non-response analysis indicated that non-respondents reported more alcohol use than respondents. The magnitude of these differences was, however, small, indicating a small non-response bias [45]. For instance, non-respondents (9.5%) were more often abstainers than respondents (9.2%) but the difference was not significant (OR = 1.04, 95% CI 0.91, 1.17), whereas non-respondents reported HED at least monthly significantly more often than respondents (49.4% vs 45.1%, OR = 1.19, 95% CI 1.10, 1.28). Abstainers (n = 568, 10.4%) were not included in the current study because the questionnaire assessing drinking motives was administrated among 12-month drinkers only. Missing values (n = 375, 6.8%) on key variables were listwise deleted, resulting in a final sample of 4,536 participants (see Fig 1). At baseline, the mean age of participants was 19.94 (SD = 1.19). More than half of the sample was French-speaking (54.30%). Primary school was the most commonly reported highest level of education completed (48.80%), followed by secondary school (28.30%) and tertiary school (22.80%).
Fig 1. Flow diagram documenting participants’ progression from recruitment to participation in the current study.
Measures
Socio-demographic variables
Age, linguistic region (i.e., German and French-speaking) and highest achieved education were assessed at baseline and served to describe the sample and as covariates in the analyses.
Adult ADHD symptoms
Adult ADHD symptoms over the past 12 months were assessed at baseline with the Adult ADHD Self-Report Scale Screener (ASRS-v1; [46]). The ASRS-v1.1 is a six-item scale that measures six ADHD symptoms based on DSM-IV diagnostic criteria for ADHD [47]. Participants indicated how often they experienced each symptom over the past 12 months with a Likert-scale ranging from 0 to 4. The ASRS-v1.1 includes a 4-item inattention subscale (e.g., How often do you have problems remembering appointments or obligations) and a 2-item hyperactivity/impulsivity subscale (e.g., How often do you feel overly active and compelled to do things, like you were driven by a motor; [48]). ADHD-total symptoms (α = 0.80) and ADHD-I symptoms (α = 0.80) showed adequate internal consistency, unlike ADHD-HI symptoms (α = 0.66), which was not unexpected given that this subscale comprised only two items. ADHD symptoms were treated as latent variables for ordinal data in the main analyses. Specifically, each item was constrained to load on its respective factor. These measures served as independent variables in the analyses.
Drinking motives
Coping and enhancement drinking motives were measured at 15 months with two 3-item subscales of the Drinking Motives Questionnaire Revised Short Form (DMQ-R SF; [49]). Participants were asked to consider all the time they had consumed alcohol in the past year and indicate how often they did so for coping (e.g., to forget about your problems) or enhancement (e.g., to get high) motives, using a 5-point Likert scale. Coping (α = 0.84) and enhancement (α = 0.82) drinking motives subscales showed adequate consistency. Both drinking motives were treated as latent variables for ordinal data in the analyses and served as mediators in the analyses.
Alcohol outcomes
AUD symptoms following DSM-5 diagnostic criteria were measured with 11 items adapted from the Semi-Structured Assessment for the Genetics of Alcoholism (SAAGA; [50, 51]). Participants were asked to indicate whether they had experienced any of 11 situations corresponding to AUD symptoms over the past 12 months (e.g., you often found yourself drinking more and for longer periods of time than you intended). Reliability and validity of this measure have been supported in previous research [50, 51]. In this study, internal consistency was adequate (α = 0.70). AUD symptoms were treated as a latent variable for ordinal data in the analyses. Participants were also asked to indicate how often they drank six or more alcoholic beverages (≥ 60gr of pure alcohol) on one occasion in the past 12 months with a Likert scale ranging from 0 to 5. Answers were dichotomized to yield a report of monthly HED, where 0 = reporting less than 1 HED per month and, 1 = reporting one or more HED per month. AUD symptoms and HED at 15 months and baseline served as dependent variables and covariates, respectively.
Depression symptoms
Depression symptoms were assessed at baseline with the Major Depression Inventory (MDI; [52]), which is a 10-item scale covering the ICD-10 symptoms of depression such as feeling lacking in energy and strength [53]. Participants were asked to indicate how often they had experienced each symptom over the past 2 weeks using a 6-point Likert scale ranging from 0 to 5. Answers were summed up to yield a total score (depression symptoms), which served as covariate in the analyses. Internal consistency was good (α = 0.89).
Anti-social personality disorder symptoms
The Mini International Neuropsychiatric interview (MINI plus; [54]) was used to assess anti-social personality disorder (ASPD) symptoms. Participants were required to indicate how often they had engaged in 12 behaviors—six before they were 15 years old (e.g., Before you were 15 years old, how often did you start fights or bully, threaten, or intimidate others?) and in six others since they were 15 (e.g., Since you were 15 years old, how often have you exposed others to danger without caring?)—using a 6-point Likert-scale ranging from 1 to 6. Answers were summed up to yield a total score (ASPD symptoms), which served as covariate in the analyses. Internal consistency was adequate (α = 0.83).
Statistical analyses
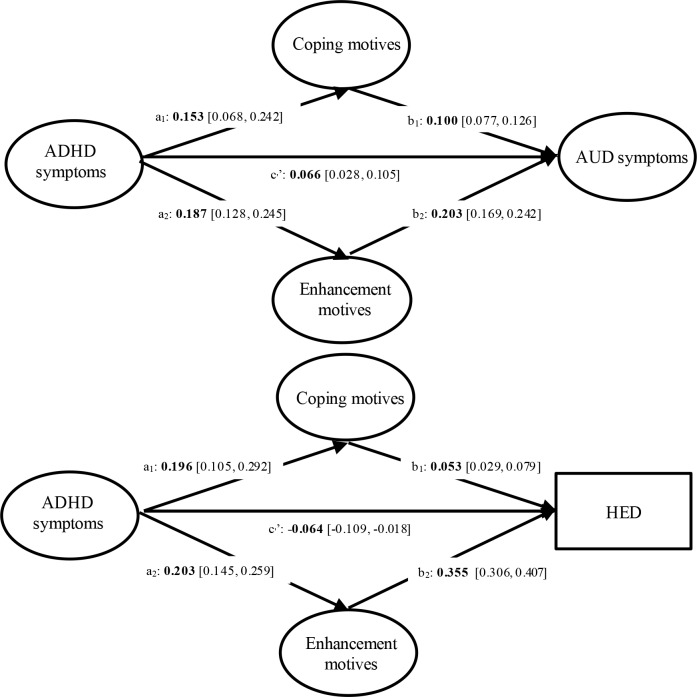
Four structural equation models (SEMs) were conducted to examine the path from ADHD symptoms to alcohol outcomes through coping and enhancement drinking motives. Two SEMs examined the mediating effects of drinking motives on the associations between ADHD-total symptoms at baseline and a) AUD symptoms and b) HED at 15 months; two other SEMs tested the mediating effects of drinking motives on the associations of ADHD-I and ADHD-HI symptoms at baseline with c) AUD symptoms and d) HED at 15 months. To test mediation (see Fig 2 for illustrative purposes), SEMs estimate the path (c’) between the predictor (e.g., ADHD symptoms) and the outcome (i.e., alcohol outcomes), the paths (a) between the predictor and the mediators (e.g., coping and enhancement drinking motives) and the paths (b) between the mediators and the outcome. Specific indirect associations of the predictor on the outcome through a specific mediator is the product of the paths linking the predictor to the given mediator (a) and the one linking that moderator to the outcome b); the total indirect associations of a predictor is the sum of all specific indirect associations, whereas the total association is the sum of the direct association (c’) and the total indirect association. SEMs show partial mediation when both indirect and direct associations are significant and full mediation when the indirect association is significant, whereas the direct association is not.
Fig 2. Results of the structural equation model of ADHD-total symptoms.
Covariates were omitted from the figure for ease of presentation. For ease of reading, significant parameters are shown in bold.
All models were adjusted for demographic variables. Furthermore, given that comorbidities with depression and ASPD are common in adult ADHD [8, 55, 56] and that they are related to problematic alcohol use [57–59], all models were adjusted for depression and ASPD symptoms at baseline. Finally, the AUD and HED SEMs were adjusted for AUD and HED at baseline, respectively. Parameter estimates were based on the weighted least squares mean-variance adjusted estimator, which was developed to handle ordinal indicators [60]. We tested for mediation using the 95% bias-corrected bootstrap confidence intervals based on 5,000 bootstrap samples, to account for potential nonnormality of the indirect effect [61, 62]. All analyses were conducted with and without adjustment. Model fit was examined using the comparative fit index (CFI) and the root mean square error of approximation (RMSEA). A CFI higher than 0.95 and a RMSEA close to 0.06 or lower indicate a good fit [63]. Descriptive analyses and the SEMs were conducted on SPSS 23 and on Mplus 7, respectively.
Results
Descriptive statistics and correlations among key variables are presented in Table 1. Fit indices indicated that the SEMs achieved a good fit (all CFIs > 0.95; all RMSEAs < 0.05). Unadjusted models showed the same general pattern than adjusted ones. We thus present below results yielded in the adjusted models only.
Table 1. Descriptive statistics and bivariate correlations among key variables (N = 4,536).
| Variable | Correlationsa | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M/% | SD | Skewness | Kurtosis | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
| ADHD symptoms baseline | |||||||||||
| 1. ADHD-total | 5.69 | 4.24 | 0.47 | -0.25 | - | ||||||
| 2. ADHD-I | 3.39 | 2.94 | 0.81 | 0.42 | 0.91*** | - | |||||
| 3. ADHD-HI | 2.29 | 1.97 | 0.56 | -0.42 | 0.82*** | 0.53*** | - | ||||
| Drinking motives 15-months | |||||||||||
| 4. Coping motives | 1.63 | 0.78 | 1.28 | 1.08 | 0.13*** | 0.14*** | 0.08*** | - | |||
| 5. Enhancement motives | 2.63 | 1.10 | 0.05 | -0.99 | 0.19*** | 0.20*** | 0.11*** | 0.37*** | - | ||
| Alcohol outcomes 15 months | |||||||||||
| 6. HED at least 1/month | 51.8% | 0.07*** | 0.07*** | 0.04*** | 0.27*** | 0.46*** | - | ||||
| 7. AUD symptoms | 1.32 | 1.64 | 1.72 | 3.87 | 0.21*** | 0.22*** | 0.15*** | 0.35*** | 0.46*** | 0.44*** | - |
aSpearman rank-order correlations. ADHD-total, ADHD-I and ADHD-hyperactivity symptoms scores ranged from 0 to 24, 0 to 16 and 0 to 8, respectively. Coping and enhancement drinking motives scores ranged from 1 to 5. AUD symptoms scores ranged from 0 to 11.
*** p < .001.
Coping and enhancement drinking motives as mediators of the association between ADHD-total symptoms and alcohol outcomes
AUD symptoms
As shown in Table 2 and Fig 2, the total and direct (c1’ on Fig 2) associations between ADHD-total symptoms and AUD symptoms and the specific indirect associations through coping and enhancement motives were significant. These findings indicated that the positive association between ADHD-total symptoms and AUD symptoms was partially mediated through coping and enhancement motives, such that ADHD-total symptoms at baseline were positively related to drinking motives at 15 months, which in turn were positively related to AUD symptoms.
Table 2. Structural equation models examining the mediating effects of coping and enhancement drinking motives on the association between ADHD-total, I and HI symptoms and AUD symptoms and HED (N = 4,536).
| AUD symptoms | HED | |||||
|---|---|---|---|---|---|---|
| B | SE | [95%CI] | B | SE | [95%CI] | |
| ADHD-total symptoms models1 | ||||||
| Total association | 0.119 | 0.021 | [0.078, 0.163] | 0.019 | 0.024 | [-0.028, 0.067] |
| Total indirect association | 0.053 | 0.009 | [0.036, 0.071] | 0.082 | 0.012 | [0.059, 0.106] |
| Specific indirect associations | ||||||
| Through coping (a1 x b1) | 0.015 | 0.005 | [0.007, 0.025] | 0.010 | 0.004 | [0.005, 0.019] |
| Through enhancement (a2 x b2) | 0.038 | 0.007 | [0.026, 0.052] | 0.072 | 0.011 | [0.050, 0.094] |
|
ADHD-I and -HI symptoms models2 ADHD-I symptoms |
||||||
| Total association | 0.134 | 0.030 | [0.078, 0.197] | 0.037 | 0.037 | [-0.033, 0.111] |
| Total indirect association | 0.073 | 0.014 | [0.048, 0.101] | 0.103 | 0.018 | [0.069, 0.140] |
| Specific indirect associations | ||||||
| Through coping (a1 x b1) | 0.023 | 0.007 | [0.010, 0.039] | 0.015 | 0.005 | [0.006, 0.027] |
| Through enhancement (a2 x b2) | 0.050 | 0.010 | [0.033, 0.071] | 0.089 | 0.016 | [0.058, 0.122] |
| ADHD-HI symptoms2 | ||||||
| Total association | -0.013 | 0.020 | [-0.053, 0.025] | -0.015 | 0.027 | [-0.073, 0.035] |
| Total indirect association | -0.017 | 0.009 | [-0.036, 0.001] | -0.017 | 0.012 | [-0.042, 0.006] |
| Specific indirect associations Through coping (a3 x b1) |
-0.007 | 0.005 | [-0.018, 0.002] | -0.003 | 0.003 | [-0.010, 0.001] |
| Through enhancement (a4 x b2) | -0.010 | 0.007 | [-0.024, 0.002] | -0.014 | 0.011 | [-0.036, 0.007] |
Note. B, unstandardized slopes; SE, standard error of B. The confidence interval reflects the 95% bias-corrected bootstrap confidence interval based on 5,000 bootstrapped samples. The models were adjusted for demographic variables, depression, ASPD and alcohol outcome at baseline.
For ease of reading significant parameters are shown in bold.
1The letters refer to Fig 1.
2The letters refer to Fig 2.
HED
Findings showed a significant direct (c1’ on Fig 2) association, such that ADHD-total symptoms were negatively related to HED. The total association between ADHD-total symptoms and HED was not significant. However, it is possible to have significant mediation (indirect effects) in the absence of a total effect [64]. The indirect associations through both motives did reach significance, indicating that ADHD-total symptoms were positively associated with drinking motives at 15 months, which were in turn positively related to HED (see Table 2, Fig 2).
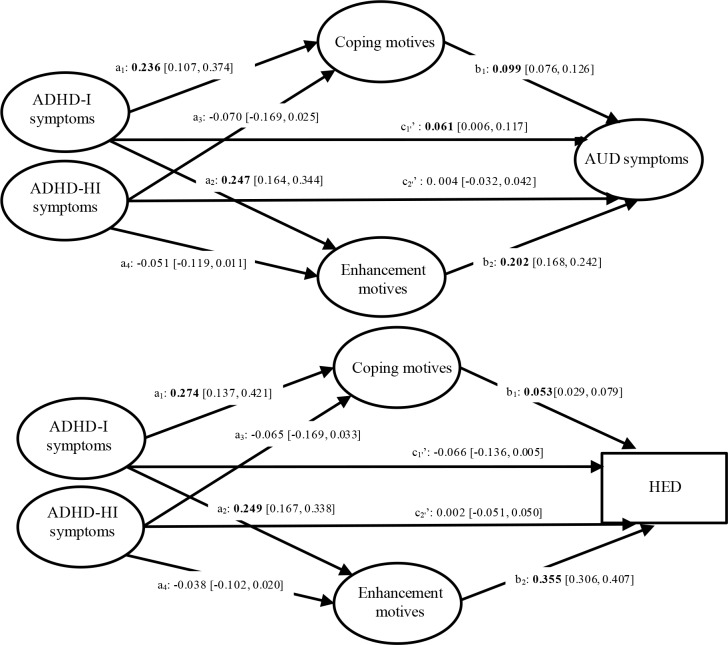
Coping and enhancement drinking motives as mediators of the association between ADHD-I and ADHD-HI symptoms and alcohol outcomes
AUD symptoms
The total and direct (c1’ on Fig 3) associations between ADHD-I symptoms and AUD symptoms were significant, so were the specific indirect associations through coping and enhancement motives (see Table 2 and Fig 3). These findings revealed that the positive association between ADHD-I symptoms and AUD symptoms was partially mediated by drinking motives, such that ADHD-I symptoms at baseline were positively related to drinking motives at 15 months, which were in turn positively related to AUD symptoms. Regarding ADHD-HI-symptoms, the total and the direct (c2’ on Fig 3) associations between ADHD symptoms and AUD symptoms did not reach significance. Similarly, the specific indirect associations through drinking motives were not significant (see Table 2 and Fig 3).
Fig 3. Results of the structural equation model of ADHD-I and HI symptoms.
Covariates were omitted from the figure for ease of presentation. For ease of reading, significant parameters are shown in bold.
HED
The total association between ADHD-I symptoms and HED was not significant, neither was the direct association (c1’ on Fig 3). Next, the specific indirect associations through coping and enhancement motives were significant, such that ADHD-I symptoms were positively associated with drinking motives at 15-months, which were in turn positively related to HED. Finally, neither the total association between ADHD-HI symptoms and HED, nor the direct (c2’ on Fig 3) and indirect associations through drinking motives did reach significance.
Discussion
This study aimed to examine the mediating effects of coping and enhancement drinking motives on the prospective associations of ADHD-total, ADHD-I and ADHD-HI symptoms with HED and AUD symptoms among young males. As expected, findings indicated that enhancement and coping drinking motives significantly mediated the associations between ADHD-total symptoms and subsequent HED and AUD symptoms. Findings also revealed indirect effects of drinking motives on the association between ADHD-I symptoms and subsequent alcohol outcomes. By contrast, findings showed that neither enhancement nor coping drinking motives significantly mediated the association of ADHD-HI symptoms with subsequent alcohol outcomes.
Unexpectedly the SEMs yielded a significant negative direct association between ADHD-total symptoms and future HED. These findings are inconsistent with past research that revealed significant positive associations between ADHD symptoms and alcohol use beyond the effects of depression and antiestablishment attitudes [14]. Notably though, the latter study focused on adolescents, whereas the current study included young men. It is possible that the association between ADHD symptoms and alcohol use changes over time. In fact, another study conducted among college students found ADHD symptoms to be not significantly related to alcohol use [26], whereas another study documented that college students with ADHD reported lower rates of alcohol use than their non-ADHD peers [65]. Our findings that ADHD-total symptoms were negatively related to HED may also pertain to an inconsistent mediation representing the variance left over after taking coping and enhancement drinking motives into account. Accordingly, bivariate analyses documented significant positive associations between ADHD symptoms and subsequent HED, although coefficients were small. Given the significant indirect associations through coping and enhancement drinking motives, these findings may indicate that young adults with elevated ADHD symptoms are not likely to engage in HED if they are not seeking coping and enhancement from this behavior. Furthermore, in line with past research [15], findings indicated that ADHD symptoms were positively associated with subsequent AUD symptoms. Taken together, these findings suggest that endorsing ADHD symptoms may increase risks of engaging in problematic drinking in youths (i.e., endorsing AUD symptoms); young adults with elevated ADHD symptoms may therefore benefit from alcohol-related harm reduction interventions (e.g., personalized normative feedbacks, protective behavior strategies use promotion; [66, 67]).
Interestingly, findings did not support a significant association between ADHD-HI symptoms and alcohol outcomes (i.e., HED; AUD symptoms), whereas ADHD-I symptoms were significantly related to more AUD symptoms but not to HED. These results are incongruent with some of previous research conducted in young adults that revealed ADHD-HI symptoms to be significantly related to alcohol use [27, 32] and problematic alcohol use [13, 32], and ADHD-I symptoms associated with alcohol use [27, 32]. Notably though, both Tong and colleagues and Roberts and colleagues focused on ADHD-HI diagnostic thresholds rather than ADHD-HI symptoms, which may help explain these differences. That said our findings are consistent with another study conducted among college students that found ADHD-HI symptoms to be unrelated to alcohol use and related problems and ADHD-I symptoms to be significantly associated with alcohol-related problems, yet not alcohol use [26]. Our findings may pertain to the fact that ADHD-HI symptoms were measured with a 2-item subscale [48], although the ASRS-v1.1 has been found to have good psychometric properties [46, 68] and Glass and colleagues found similar findings while using a scale measuring ADHD-HI that included more items. It may also be that ADHD-I symptoms carry more importance than ADHD-HI symptoms among young adults. In fact, literature indicates that ADHD-I symptoms are more persistent than ADHD-HI symptoms over time [69, 70]. Importantly, given the inconsistent findings yielded in both past research and the current study, future research is needed to clarify the associations between ADHD-HI and ADHD-I symptoms and alcohol outcomes among young adults.
Our findings notably add to the existing literature by providing initial evidence that the association between ADHD symptoms and subsequent alcohol outcomes may be partially explained by coping and enhancement drinking motives. As expected, findings revealed indirect effects of enhancement and coping drinking motives on the associations between ADHD-total symptoms and subsequent HED and AUD symptoms. Further, findings revealed indirect effects through coping drinking motives on the association between ADHD-I symptoms and subsequent alcohol outcomes. Unexpectedly, findings also revealed significant indirect effects through enhancement drinking motives on the longitudinal association between ADHD-I symptoms and alcohol outcomes. It may be that impairments of executive functioning, such as inattention and distractibility, lead to poor risk perception and impaired ability to deploy appropriate judgment, which may in turn increase the likelihood of engaging in risky behaviors aiming to seek sensation (e.g., fast driving). Past research has documented that adults with ADHD are prone to risky decision making [71] and, relatedly, to engage in risky behaviors. In fact, a recent review of the literature on ADHD and driving risks concluded that deficits in cognitive abilities such as inattentiveness may be the mechanism through which ADHD affects driving risks [72].
Taken together, the findings of this study suggest that young adults with elevated ADHD-I symptoms may be more at risk from engaging in problematic drinking because they use alcohol for enhancement and/or coping motives. If replicated by future research, these findings provide important insight regarding the development of alcohol-related interventions tailored to young men endorsing elevated ADHD-I symptoms. Specifically, they suggest that alcohol-related cognitive behavioral interventions targeting both enhancement and coping drinking motives may be a promising way to prevent problematic drinking among young adults with elevated ADHD-I symptoms [73]. Such interventions might aim to increase awareness of coping and enhancement drinking motives as well as to reduce alcohol use as a coping mechanism by means of a coping skill training program (e.g., relaxation methods). Furthermore, they might target enhancement drinking motives by helping at-risk young men consider alternative ways to enhance their well-being and positive mood (e.g., sport practicing, mind-fullness meditating; [73]).
Although the major strengths of this study include its longitudinal design and its large sample size, findings should be interpreted in the light of several limitations. First, the sample was limited to young males, which precludes generalizability of findings to young females or to other age groups. Second, the study relied on responses to self-reported questionnaires and their validity may be a concern, although participants were assured confidentiality. Third, as mentioned earlier, ADHD-HI symptoms were measured with a 2-item subscale. Although the ASRS-v1.1 has been found to have good psychometric properties [46, 68], future research using additional scales is needed to further confirm these findings. Fourth, the association between mediators and outcome variables were measured at the same time point, which precludes drawing inferences regarding the temporal associations between these variables. Future research using additional follow-up measurements is thus necessary. Fifth, it is important to highlight that coefficients of the indirect effect through coping and enhancement drinking motives on the association between ADHD-total/ADHD-I and alcohol outcomes were rather small, suggesting small effect sizes. It may be that our models were inclusive of a wide range of measures, which may have diluted the overall effect sizes. That said, our results are supported by the fact that these indirect effects were consistently significant across both models. Future research further testing these indirect effects are yet needed to confirm these findings.
Despite these limitations, this study makes an interesting contribution to the literature by providing initial evidence that the association between ADHD-I symptoms and future alcohol outcomes is partially mediated by coping and enhancement drinking motives. Although future research is needed to confirm these findings and ensure their generalizability, they suggest that cognitive-behavioral interventions targeting enhancement and coping drinking motives may represent a promising way to decrease alcohol-related harm among at-risk young adults with elevated ADHD-I symptoms.
Data Availability
The data are in a public repository: DOI: 10.16909/DATASET/16.
Funding Statement
This study was funded by the Swiss National Science Foundation (FN 33CSC0-122679 and FN 33CS30-139467, both awarded to GG). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author; 2013.
- 2.Faraone SV, Sergeant J, Gillberg C, Biederman J. The worldwide prevalence of ADHD: is it an American condition? World Psychiatry. 2003;2(2):104–13. Epub 2006/09/02. [PMC free article] [PubMed] [Google Scholar]
- 3.Biederman J, Faraone SV, Spencer T, Wilens T, Norman D, Lapey KA, et al. Patterns of psychiatric comorbidity, cognition, and psychosocial functioning in adults with attention deficit hyperactivity disorder. Am J Psychiatry. 1993;150(12):1792–8. Epub 1993/12/01. 10.1176/ajp.150.12.1792 . [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716–23. Epub 2006/04/06. 10.1176/appi.ajp.163.4.716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Estevez N, Eich-Hochli D, Dey M, Gmel G, Studer J, Mohler-Kuo M. Prevalence of and associated factors for adult attention deficit hyperactivity disorder in young Swiss men. PLoS One. 2014;9(2):e89298 Epub 2014/03/04. 10.1371/journal.pone.0089298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9(3):490–9. Epub 2012/09/15. 10.1007/s13311-012-0135-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simon V, Czobor P, Balint S, Meszaros A, Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194(3):204–11. Epub 2009/03/03. 10.1192/bjp.bp.107.048827 . [DOI] [PubMed] [Google Scholar]
- 8.Fayyad J, De Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry. 2007;190:402–9. Epub 2007/05/02. 10.1192/bjp.bp.106.034389 . [DOI] [PubMed] [Google Scholar]
- 9.Doshi JA, Hodgkins P, Kahle J, Sikirica V, Cangelosi MJ, Setyawan J, et al. Economic impact of childhood and adult attention-deficit/hyperactivity disorder in the United States. J Am Acad Child Adolesc Psychiatry. 2012;51(10):990–1002 e2. Epub 2012/10/02. 10.1016/j.jaac.2012.07.008 . [DOI] [PubMed] [Google Scholar]
- 10.Das D, Cherbuin N, Butterworth P, Anstey KJ, Easteal S. A population-based study of attention deficit/hyperactivity disorder symptoms and associated impairment in middle-aged adults. PLoS One. 2012;7(2):e31500 Epub 2012/02/22. 10.1371/journal.pone.0031500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biederman J, Faraone SV. The effects of attention-deficit/hyperactivity disorder on employment and household income. MedGenMed. 2006;8(3):12 Epub 2007/04/05. [PMC free article] [PubMed] [Google Scholar]
- 12.Young S, Moss D, Sedgwick O, Fridman M, Hodgkins P. A meta-analysis of the prevalence of attention deficit hyperactivity disorder in incarcerated populations. Psycholical Medicine. 2015;45(2):247–58. 10.1017/S0033291714000762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kolla NJ, van der Maas M, Toplak ME, Erickson PG, Mann RE, Seeley J, et al. Adult attention deficit hyperactivity disorder symptom profiles and concurrent problems with alcohol and cannabis: sex differences in a representative, population survey. BMC Psychiatry. 2016;16:50 Epub 2016/02/28. 10.1186/s12888-016-0746-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gudjonsson GH, Sigurdsson JF, Sigfusdottir ID, Young S. An epidemiological study of ADHD symptoms among young persons and the relationship with cigarette smoking, alcohol consumption and illicit drug use. J Child Psychol Psychiatry. 2012;53(3):304–12. Epub 2011/11/10. 10.1111/j.1469-7610.2011.02489.x . [DOI] [PubMed] [Google Scholar]
- 15.Estevez N, Dey M, Eich-Hochli D, Foster S, Gmel G, Mohler-Kuo M. Adult attention-deficit/hyperactivity disorder and its association with substance use and substance use disorders in young men. Epidemiology and Psychiatric Sciences. 2016;25(3):255–66. 10.1017/S2045796015000360 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arcos-Burgos M, Velez JI, Solomon BD, Muenke M. A common genetic network underlies substance use disorders and disruptive or externalizing disorders. Human Genetics. 2012;131(6):917–29. 10.1007/s00439-012-1164-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pitel AL, Zahr NM, Jackson K, Sassoon SA, Rosenbloom MJ, Pfefferbaum A, et al. Signs of preclinical Wernicke's encephalopathy and thiamine levels as predictors of neuropsychological deficits in alcoholism without Korsakoff's syndrome. Neuropsychopharmacology. 2011;36(3):580–8. 10.1038/npp.2010.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ihara H, Berrios GE, London M. Group and case study of the dysexecutive syndrome in alcoholism without amnesia. Journal of Neurology, Neurosurgery, and Psychiatry. 2000;68(6):731–7. 10.1136/jnnp.68.6.731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future national survey results on drug use, 1975–2013: Volume I, Secondary school students. Ann Arbor: Institute for Social Research, the University of Michigan.; 2014. [Google Scholar]
- 20.Schulenberg JE, Johnston LD, O'Malley PM, Bachman JG, Miech RA, Patrick ME. Monitoring the Future national survey results on drug use, 1975–2016: Volume II, College students and adults ages 19–55. Ann Arbor: Institute for Social Research, The University of Michigan; 2017. [Google Scholar]
- 21.Delgrande Jordan M, Notari L. Consommation d'alcool en Suisse une analyse des données de l'Enquête suisse sur la santé 2007. Lausanne: Addiction Info Suisse; 2011. [Google Scholar]
- 22.Frazier TW, Youngstrom EA, Naugle RI. The latent structure of attention-deficit/hyperactivity disorder in a clinic-referred sample. Neuropsychology. 2007;21(1):45–64. Epub 2007/01/05. 10.1037/0894-4105.21.1.45 . [DOI] [PubMed] [Google Scholar]
- 23.McLennan JD. Understanding attention deficit hyperactivity disorder as a continuum. Canadian Family Physician. 2016;62(12):979–82. [PMC free article] [PubMed] [Google Scholar]
- 24.Bidwell LC, Henry EA, Willcutt EG, Kinnear MK, Ito TA. Childhood and current ADHD symptom dimensions are associated with more severe cannabis outcomes in college students. Drug Alcohol Depend. 2014;135:88–94. Epub 2013/12/18. 10.1016/j.drugalcdep.2013.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.De Alwis D, Lynskey MT, Reiersen AM, Agrawal A. Attention-deficit/hyperactivity disorder subtypes and substance use and use disorders in NESARC. Addictive Behaviors. 2014;39(8):1278–85. Epub 2014/05/14. 10.1016/j.addbeh.2014.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glass K, Flory K. Are symptoms of ADHD related to substance use among college students? Psychology of Addictive Behaviors 2012;26(1):124–32. Epub 2011/06/08. 10.1037/a0024215 . [DOI] [PubMed] [Google Scholar]
- 27.Roberts W, Peters JR, Adams ZW, Lynam DR, Milich R. Identifying the facets of impulsivity that explain the relation between ADHD symptoms and substance use in a nonclinical sample. Addictive Behaviors. 2014;39(8):1272–7. Epub 2014/05/13. 10.1016/j.addbeh.2014.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tuithof M, ten Have M, van den Brink W, Vollebergh W, de Graaf R. The role of conduct disorder in the association between ADHD and alcohol use (disorder). Results from the Netherlands Mental Health Survey and Incidence Study-2. Drug Alcohol Depend. 2012;123(1–3):115–21. Epub 2011/11/29. 10.1016/j.drugalcdep.2011.10.030 . [DOI] [PubMed] [Google Scholar]
- 29.Molina BS, Pelham WE, Cheong J, Marshal MP, Gnagy EM, Curran PJ. Childhood attention-deficit/hyperactivity disorder (ADHD) and growth in adolescent alcohol use: the roles of functional impairments, ADHD symptom persistence, and parental knowledge. J Abnorm Psychol. 2012;121(4):922–35. Epub 2012/08/01. 10.1037/a0028260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molina BS, Walther CA, Cheong J, Pedersen SL, Gnagy EM, Pelham WE. Heavy alcohol use in early adulthood as a function of childhood ADHD: developmentally specific mediation by social impairment and delinquency. Exp Clin Psychopharmacol. 2014;22(2):110–21. Epub 2014/03/13. 10.1037/a0035656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rooney M, Chronis-Tuscano AM, Huggins S. Disinhibition mediates the relationship between ADHD and problematic alcohol use in college students. J Atten Disord. 2012;19(4):313–27. Epub 2012/11/03. 10.1177/1087054712459885 . [DOI] [PubMed] [Google Scholar]
- 32.Tong L, Shi HJ, Zhang Z, Yuan Y, Xia ZJ, Jiang XX, et al. Mediating effect of anxiety and depression on the relationship between attention-deficit/hyperactivity disorder symptoms and smoking/drinking. Sci Rep. 2016;6 10.1038/srep21609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: a motivational model of alcohol use. J Pers Soc Psychol. 1995;69(5):990–1005. Epub 1995/11/01. . [DOI] [PubMed] [Google Scholar]
- 34.Kuntsche E, Von Fischer M, Gmel C. Personality factors and alcohol use: A mediator analysis of drinking motives. Personality and Individual Differences. 2008;45:796–800. [Google Scholar]
- 35.Kuntsche E, Knibbe R, Gmel G, Engels R. Who drinks and why? A review of socio-demographic, personality, and contextual issues behind the drinking motives in young people. Addictive Behaviors. 2006;31(10):1844–57. Epub 2006/02/08. 10.1016/j.addbeh.2005.12.028 . [DOI] [PubMed] [Google Scholar]
- 36.Nigg JT. Is ADHD a disinhibitory disorder? Psycholical Bulletin. 2001;127(5):571–98. . [DOI] [PubMed] [Google Scholar]
- 37.Nigg JT, Stavro G, Ettenhofer M, Hambrick DZ, Miller T, Henderson JM. Executive functions and ADHD in adults: evidence for selective effects on ADHD symptom domains. J Abnorm Psychol. 2005;114(4):706–17. 10.1037/0021-843X.114.3.706 . [DOI] [PubMed] [Google Scholar]
- 38.Young S. Coping strategies used by adults with ADHD. Personality and Individual Differences. 2005;38:809–16. [Google Scholar]
- 39.Kronenberg LM, Goossens PJ, van Busschbach J, van Achterberg T, van den Brink W. Coping styles in substance use disorder (SUD) patients with and without co-occurring attention deficit/hyperactivity disorder (ADHD) or autism spectrum disorder (ASD). BMC Psychiatry. 2015;15:159 Epub 2015/07/15. 10.1186/s12888-015-0530-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zuckerman M. The sensation seeking scale V (SSS-V): Still reliable and valid. Personality and Individual Differences. 2007;43:1303–5. [Google Scholar]
- 41.Ballon N, Brunault P, Cortese S. Sensation seeking and cocaine dependence in adults with reported childhood ADHD. J Atten Disord. 2015;19(4):335–42. 10.1177/1087054714543651 . [DOI] [PubMed] [Google Scholar]
- 42.Cho SC, Hwang JW, Lyoo IK, Yoo HJ, Kin BN, Kim JW. Patterns of temperament and character in a clinical sample of Korean children with attention-deficit hyperactivity disorder. Psychiatry Clinical Neurosciences. 2008;62(2):160–6. 10.1111/j.1440-1819.2008.01749.x . [DOI] [PubMed] [Google Scholar]
- 43.Purper-Ouakil D, Cortese S, Wohl M, Aubron V, Orejarena S, Michel G, et al. Temperament and character dimensions associated with clinical characteristics and treatment outcome in attention-deficit/hyperactivity disorder boys. Comprehensive Psychiatry. 2010;51(3):286–92. 10.1016/j.comppsych.2009.08.004 . [DOI] [PubMed] [Google Scholar]
- 44.Gmel G, Akre C, Astudillo M, Bähler C, Baggio S, Bertholet N, et al. The Swiss cohort study on substance use risk factors—Findings of two waves. Sucht. 2015;61(4):251–62. 10.1024/0939-5911.a00380 [DOI] [Google Scholar]
- 45.Studer J, Baggio S, Mohler-Kuo M, Dermota P, Gaume J, Bertholet N, et al. Examining non-response bias in substance use research—are late respondents proxies for non-respondents? Drug Alcohol Depend. 2013;132(1–2):316–23. Epub 2013/03/29. 10.1016/j.drugalcdep.2013.02.029 . [DOI] [PubMed] [Google Scholar]
- 46.Kessler RC, Adler LA, Gruber MJ, Sarawate CA, Spencer T, Van Brunt DL. Validity of the World Health Organization Adult ADHD Self-Report Scale (ASRS) Screener in a representative sample of health plan members. Int J Methods Psychiatr Res. 2007;16(2):52–65. Epub 2007/07/12. 10.1002/mpr.208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th edition, text revision (DSM-IV-TR). 4th ed Washington, DC: Author; 2000. [Google Scholar]
- 48.Hesse M. The ASRS-6 has two latent factors: attention deficit and hyperactivity. Journal of Attenion Disorders. 2013;17(3):203–7. 10.1177/1087054711430330 . [DOI] [PubMed] [Google Scholar]
- 49.Kuntsche E, Kuntsche S. Development and validation of the Drinking Motive Questionnaire Revised Short Form (DMQ-R SF). J Clin Child Adolesc Psychol. 2009;38(6):899–908. Epub 2010/02/26. 10.1080/15374410903258967 . [DOI] [PubMed] [Google Scholar]
- 50.Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI Jr., et al. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol. 1994;55(2):149–58. Epub 1994/03/01. . [DOI] [PubMed] [Google Scholar]
- 51.Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V. A validity study of the SSAGA—a comparison with the SCAN. Addiction. 1999;94(9):1361–70. Epub 2000/01/01. . [DOI] [PubMed] [Google Scholar]
- 52.Bech P, Rasmussen NA, Olsen LR, Noerholm V, Abildgaard W. The sensitivity and specificity of the Major Depression Inventory, using the Present State Examination as the index of diagnostic validity. J Affect Disord. 2001;66(2–3):159–64. Epub 2001/10/02. . [DOI] [PubMed] [Google Scholar]
- 53.World Health Organization. The ICD-10 classification of mental and behavioural disorders: Clinical and diagnodtic guidelines (10th ed.). Geneva: World Health Organization; 1994. [Google Scholar]
- 54.Lecrubier Y, Weiller E, Hergueta T, Amorim P, Bonora LI, Lépine P, et al. MINI Mini International Neuropsychiatric Interview French Version 5.00. Paris: Hôpital de la Pitié Sapétierre, INSERM; 1998. [Google Scholar]
- 55.de Zwaan M, Gruss B, Muller A, Graap H, Martin A, Glaesmer H, et al. The estimated prevalence and correlates of adult ADHD in a German community sample. Eur Arch Psychiatry Clin Neurosci. 2012;262(1):79–86. Epub 2011/04/19. 10.1007/s00406-011-0211-9 . [DOI] [PubMed] [Google Scholar]
- 56.Moss SB, Nair R, Vallarino A, Wang S. Attention deficit/hyperactivity disorder in adults. Prim Care. 2007;34(3):445–73, v. Epub 2007/09/18. 10.1016/j.pop.2007.05.005 . [DOI] [PubMed] [Google Scholar]
- 57.Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA Psychiatry. 1990;264(19):2511–8. Epub 1990/11/21. . [PubMed] [Google Scholar]
- 58.Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(4):361–8. Epub 2004/04/07. 10.1001/archpsyc.61.4.361 . [DOI] [PubMed] [Google Scholar]
- 59.Weitzman ER. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. J Nerv Ment Dis. 2004;192(4):269–77. Epub 2004/04/03. . [DOI] [PubMed] [Google Scholar]
- 60.Muthén L, Muthén BO. Mplus: The Comprehensive Modeling Program for Applied Researchers: User's Guide. Los Angeles: Author; 1998. [Google Scholar]
- 61.Fritz MS, Mackinnon DP. Required sample size to detect the mediated effect. Psychol Sci. 2007;18(3):233–9. Epub 2007/04/21. 10.1111/j.1467-9280.2007.01882.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–31. Epub 2005/01/12. . [DOI] [PubMed] [Google Scholar]
- 63.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- 64.O'Rourke HP, MacKinnon DP. When the test of mediation is more powerful than the test of the total effect. Behavioral Research Methods. 2015;47(2):424–42. 10.3758/s13428-014-0481-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Janusis GM, Weyandt LL. An exploratory study of substance use and misuse among college students with and without ADHD and other disabilities. Journal of Attenion Disorders. 2010;14:205–15. [DOI] [PubMed] [Google Scholar]
- 66.Kenney SR, Napper LE, LaBrie JW, Martens MP. Examining the efficacy of a brief group protective behavioral strategies skills training alcohol intervention with college women. Psychology of Addictive Behaviors 2014;28(4):1041–51. Epub 2014/10/28. 10.1037/a0038173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Larimer ME, Lee CM, Kilmer JR, Fabiano PM, Stark CB, Geisner IM, et al. Personalized mailed feedback for college drinking prevention: a randomized clinical trial. J Consult Clin Psychol. 2007;75(2):285–93. Epub 2007/05/02. 10.1037/0022-006X.75.2.285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35(2):245–56. Epub 2005/04/22. . [DOI] [PubMed] [Google Scholar]
- 69.Gentile JP, Atiq R, Gillig PM. Adult ADHD: Diagnosis, Differential Diagnosis, and Medication Management. Psychiatry (Edgmont). 2006;3(8):25–30. [PMC free article] [PubMed] [Google Scholar]
- 70.Wilens TE, Biederman J, Faraone SV, Martelon M, Westerberg D, Spencer TJ. Presenting ADHD symptoms, subtypes, and comorbid disorders in clinically referred adults with ADHD. Journal of Clinical Psychiatry. 2009;70(11):1557–62. 10.4088/JCP.08m04785pur [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Matthies S, Philipsen A, Svaldi J. Risky decision making in adults with ADHD. Journal of Behavior Therapy and Experimental Psychiatry. 2012;43(3):938–46. 10.1016/j.jbtep.2012.02.002 . [DOI] [PubMed] [Google Scholar]
- 72.Jerome L, Habinski L, Segal A. Attention-deficit/hyperactivity disorder (ADHD) and driving risk: a review of the literature and a methodological critique. Current Psychiatry Reports. 2006;8(5):416–26. . [DOI] [PubMed] [Google Scholar]
- 73.Wurdak M, Wolstein J, Kuntsche E. Effectiveness of a drinking-motive-tailored emergency-room intervention among adolescents admitted to hospital due to acute alcohol intoxication—A randomized controlled trial. Preventive Medicine Reports. 2016;3:83–9. 10.1016/j.pmedr.2015.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are in a public repository: DOI: 10.16909/DATASET/16.