Abstract
Objective:
To assess the impact of baseline dietary self-efficacy on the effect of a dietary intervention to reduce sodium intake in hemodialysis (HD) patients, and identify determinants of low dietary self-efficacy.
Design:
Post-hoc analysis of the BalanceWise study, a randomized controlled trial that aimed to reduce dietary sodium intake in HD patients
Setting:
17 dialysis centers in Pennsylvania
Subjects:
151 HD patients
Main Outcome Measures:
Dietary self-efficacy and reported dietary sodium density
Analysis:
ANOVA with post-hoc group-wise comparison was used to examine the effect of baseline dietary self-efficacy on changes in reported sodium density in the intervention and control groups at 8- and 16-weeks. Chi square or independent t-tests or Wilcoxon rank sum tests were used to identify determinants of low dietary self-efficacy.
Results:
The interaction between dietary self-efficacy and impact of the intervention on changes in reported dietary sodium density approached significance at 8- and 16-weeks (p-int = 0.051 and 0.06, respectively). Younger age and perceived income inadequacy were significantly associated with low self-efficacy in HD patients.
Conclusion:
The benefits of dietary interventions designed to improve self-efficacy may differ by baseline self-efficacy status. This may be particularly important for HD patients that are younger and report inadequate income, as they had lower dietary self-efficacy.
Keywords: hemodialysis, self-efficacy, social cognitive theory, dietary sodium intake, behavioral intervention
INTRODUCTION
Adherence to dietary recommendations is a key component of preventing and managing most chronic diseases.1 The hemodialysis (HD) diet is arguably one of the most complex and difficult to follow medically prescribed diets,2,3 making it an excellent model for studying behavioral approaches to improve dietary adherence. Indeed, HD patients need to balance the requirements of the conditions that led to kidney disease (usually hypertension and/or diabetes) with the high-protein, low-fluid, low-sodium, low-phosphorus and low-potassium dietary requirements of renal replacement therapy, all while dealing with complicated medication regimens, dialysis treatments, unpleasant symptoms (e.g., fatigue, pruritis, constipation, anorexia, pain),4 and a potential myriad of psychosocial issues (e.g., depression, anxiety, and impaired cognition).2,4 Consequently, it is no surprise that the majority of HD patients report some difficulty following the recommended diet and motivating themselves to eat right.2–7
In circumstances such as these, education alone is unlikely to achieve lasting behavior change.8 Social cognitive theory (SCT) posits that behavioral change is affected by a complex interaction between the person, environment and nature of the required behavior.9,10 This theory has been widely used as a treatment model for numerous behavioral interventions, including dietary interventions.11–15 According to SCT, self-efficacy, defined as one’s confidence in performing a behavior, is an important determinant of initiating and maintaining certain behaviors. 9,10 SCT-based interventions attempt to promote behavior change, in part, by enhancing self-efficacy for behavior change by building mastery experiences, emphasizing past successes, social modeling, highlighting the benefits of new behaviors, and verbal persuasion. 9,10
Behavioral interventions generally enroll participants on the basis of whether improvements in the primary outcomes of interest are likely, rather than the appropriateness of the intervention’s theoretical underpinnings. Given the resources required to design and implement effective dietary interventions, strategies to identify patients that are likely to respond to treatment are critically important for research and clinical practice. Although higher self-efficacy has been shown to be associated with better adherence to dietary recommendations6,16–20, to the best of our knowledge, no study has examined the role of baseline self-efficacy on the efficacy of dietary interventions. The BalanceWise study was a 16-week, technology-supported, SCT-based randomized controlled trial designed to reduce dietary sodium intake in HD patients. One hundred and seventy-nine participants were randomized. A significant differential change in dietary sodium intake observed at 8 weeks (−372 mg/day; p=0.05) but was not sustained at 16 weeks (−191 mg/day; p=0.32).21,22 In this secondary data analysis, we evaluated the impact of baseline dietary self-efficacy on treatment efficacy. We additionally examined whether low dietary self-efficacy was associated with sociodemographic and clinical variables to identify at-risk groups.
METHODS
DESIGN AND SETTING
Participants in BalanceWise were recruited from 17 dialysis units in Western Pennsylvania_and randomized to an attention control group or a 16-week technology-supported SCT-based behavioral intervention designed to reduce dietary sodium intake. Measurements were obtained at baseline, 8 weeks, and 16 weeks. Recruitment occurred from September 2009 to September 2012 and the final data collection was completed around March 2013. The study was reviewed and approved by the Institutional Review Board of the University of Pittsburgh. Signed informed consent was obtained from all participants.
SAMPLE
To be eligible for the study, participants had to be: 1) over 18 years of age; and 2) receiving in-center HD for at least 3 months. Individuals were excluded if they: 1) were unable to read, write, or speak English; 2) could not see personal digital assistant (PDA) or use a stylus to choose menus on PDA screen; 3) had dementia; 4) planned to change dialysis center or move out of the area within the next 16 weeks; 5) had a life expectancy of less than 12 months (per the dialysis center dietitian or social worker); 6) lived in an institutional setting where they had no control over their diet; 7) were unwilling to speak with a study dietitian 1-2 times/week or document their dietary intake for 16 weeks using the PDA; or 8) were scheduled to undergo a transplant during the study period. In our analysis, we included data from 151 (84.4%) participants who had complete baseline data on self-reported dietary sodium intake and dietary self-efficacy.
MEASURES
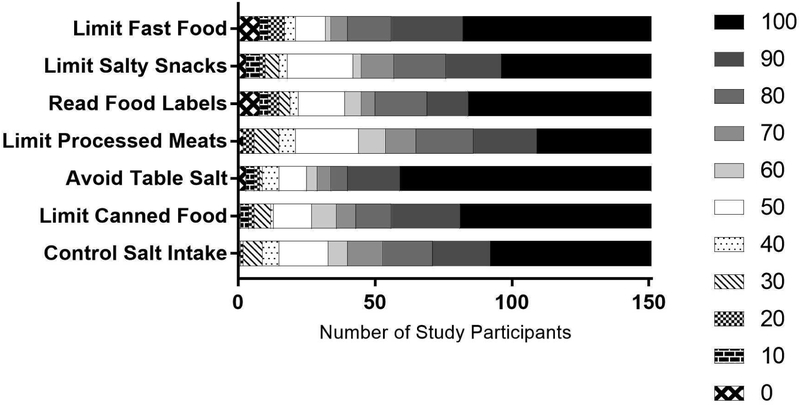
Dietary self-efficacy was analyzed at baseline using an investigator-developed 15-item survey.23 For this report, dietary self-efficacy was calculated as the unweighted sum of 7 items regarding confidence to follow dietary sodium restriction. Using an 11-point Visual Numeric Scale with responses ranging from 0 (not confident at all) to 100 (very confident), participants were asked to indicate their level of confidence that, in the next month, they would be able to limit sodium intake, avoid canned food, avoid table salt, limit processed meat, read food labels for sodium information, limit salty food, and limit fast food. The reliability of this scale (Cronbach α = 0.93) has been reported elsewhere.23 Participants were classified as high or low self-efficacy using the baseline sample median score as the cut point.
Dietary intakes were estimated at baseline (i.e. pre-intervention), 8-weeks and 16-weeks using three, unscheduled 24-hour dietary recalls, including 1 dialysis and 1 non-dialysis weekday, and 1 non-dialysis weekend day. The first two recalls were conducted in person, and provided portion-size guidance to estimate dietary intake. To minimize participant’s burden, the third recall was conducted over the phone. Dietary data were analyzed for nutrient composition using the Nutrition Data System for Research (NDSR) software.24,25 Daily reported sodium intakes were converted into nutrient densities (mg/1,000 kcal) for all analyses.
Sociodemographic and clinical characteristics were collected at baseline by questionnaires, and included age, gender, race, education, duration of dialysis, marital status, employment status, and whether income met basic living needs.
Statistical Analysis
Responses to the items in the self-efficacy questionnaire were plotted in a column graph. Participant characteristics were summarized overall, and by self-efficacy status as mean ± standard deviation (SD) for normally distributed continuous variables, median (interquartile range, IQR) for non-normally distributed continuous variables, and frequency (percent) for categorical variables. Differences between participants in the low and high self-efficacy groups were assessed using independent two-sample t-tests, Wilcoxon rank sum tests and Chi-square tests, as appropriate.
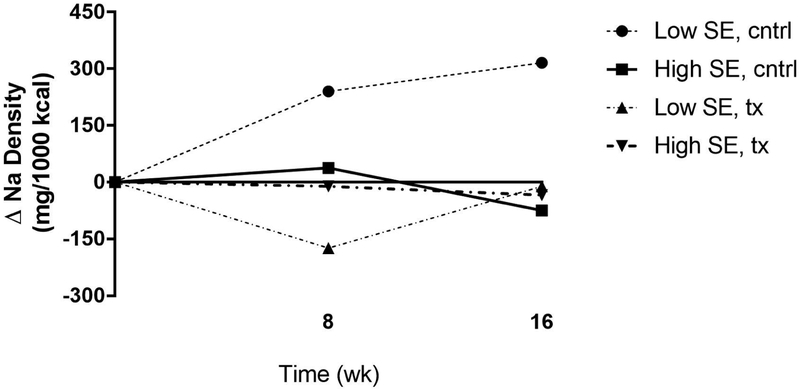
Changes in self-reported dietary sodium density by baseline self-efficacy and treatment group were plotted in a line graph as means ± standard errors, and compared across groups using one-way analysis of variance with post-hoc Tukey HSD test. The multiplicative interactions between baseline self-efficacy status (low vs high) and treatment group allocation (control vs treatment) at 8-weeks and 16-weeks were assessed using multivariable analysis of variance. Changes in reported self-efficacy among participants in the low self-efficacy group at baseline were assessed at 8-weeks and 16-weeks, and compared across treatment groups using Wilcoxon rank sum tests. Of note, few participants were missing follow up data for self-efficacy in the treatment group at 8-weeks (n=1) and 16-weeks (n=2).
Statistical tests were performed using Statistical Analysis Software (SAS©) 9.3 for Windows (Cary NC, USA), and graphs were created using GraphPad Prism (GraphPad Software, La Jolla, CA, USA). The significance level was set as p < .05 for two-tailed hypothesis testing.
RESULTS
Characteristics of participants overall and by self-efficacy status at baseline are depicted in Table 1. Briefly, the majority of participants were male (57%), white (65%) and approximately 60 years of age (SD=13) with a median dialysis vintage of 33 months (IQR: 15-66). Most reported having no post-secondary education (58%), being unemployed (85%) and unmarried (58%), and having adequate income to meet their basic needs (69%).
Table 1.
Characteristics of Study Participants
| Variables | n | Values |
|---|---|---|
| Age, years: mean±SD | 151 | 60 ± 13 |
| Dialysis vintage, months: median (IQR) | 137 | 33 (15-66) |
| Male gender: n(%) | 151 | 86 (57%) |
| Currently married: n (%) | 151 | 63 (42%) |
| African American race: n(%) | 150 | 53 (35%) |
| More than high school education: n(%) | 151 | 63 (42%) |
| Income meets needs: n(%) | 144 | 100 (69%) |
| Currently employed: n(%) | 151 | 22 (15%) |
SD: standard deviation; IQR: interquartile range
The median (IQR) of the baseline self-efficacy scores was 580 (480-660) out of a possible 700 (Figure 1). The majority of participants reported greater than 50% confidence for all of the items included in the self-efficacy questionnaire, ranging from 107/151 (71%) for limiting processed meats to 126/151 (83%) for avoiding table salt. There was a strong positive correlation between self-efficacy scores of the individual items (Spearman’s rho range 0.38-0.70, p<0.0001).
Figure 1.
Self-Efficacy for Each Survey Item based on an 11-point Likert Scale Ranging from Not Confident At All (0) to Completely Confident (100)
As shown in Figure 2, among participants having high baseline self-efficacy, little change in dietary sodium density was observed regardless of randomization assignment. Larger changes were observed in those with low baseline self-efficacy, with increases in sodium density observed at both time points in the control group, and transient reductions in sodium density observed in the intervention group. The difference between randomization groups having low baseline self-efficacy was statistically significant (p<0.05) at 8 weeks. The multiplicative interaction of baseline self-efficacy status and treatment group allocation on changes in reported dietary sodium density tended towards significance at 8-weeks (p-int. = 0.051) and 16-weeks (p-int. = 0.06).
Figure 2.
Changes in Reported Dietary Sodium Density by Baseline Dietary Self-Efficacy and Treatment Group
Note: SE: self-efficacy;cntrl: control;tx: treatment
Compared to participants with low self-efficacy scores at baseline (≤580), those with high self-efficacy scores (>580) were older (63 vs 57 years old, p=0.008), more likely to be African American (43% vs 28%, p=0.046), and reported that their income was sufficient to meet their needs (78% vs 61%, p=0.02) (Table 2). When age, race and income adequacy were analyzed in a multivariable model, age and income adequacy, but not race, remained significantly associated with self-efficacy status (p <0.05).
Table 2.
Comparison of Participant Characteristics by Baseline Self-Efficacy Status
| Variables* | Low Self-Efficacy (n=76) |
High Self-Efficacy (n=75) |
p-value |
|---|---|---|---|
| Age, years | 57 ± 13 | 63 ± 13 | .008 |
| Dialysis vintage, months | 39 (15-71) | 31 (15-63) | .68 |
| Male gender | 43 (57%) | 43 (57%) | .93 |
| Currently married | 33 (43%) | 30 (40%) | .67 |
| African American race | 55 (72%) | 42 (57%) | .046 |
| More than high school education | 31 (41%) | 32 (43%) | .82 |
| Income meets needs | 43 (61%) | 57 (78%) | .02 |
| Currently employed | 13 (17%) | 9 (12%) | .37 |
Values are presented as mean ± standard deviation or median (interquartile range) or n (%).
DISCUSSION
In this report, we examined the impact of baseline dietary self-efficacy on the intervention outcome (self-reported dietary sodium density) and its association with sociodemographic and clinical characteristics in HD patients. Our findings suggest that those with low self-efficacy may benefit the most from an SCT-based intervention to reduce dietary sodium, which, if confirmed, could have important implication for research and clinical practice. At present, most clinical trials and practices identify potential participants based upon the outcome of interest (e.g., high blood pressure), with little emphasis on the underlying behavioral constructs (e.g., self-efficacy) that the intervention targets. Given the large amount of resources required to plan and deliver efficacious dietary interventions in chronic disease populations, any strategy that can help to identify patients that are likely to respond to treatment are crucially important.
Overall, HD patients enrolled in the BalanceWise study reported a high level of self-efficacy to restrict sodium intake, with a median score of 580 out of possible 700. These findings are consistent with those reported by Zrinyi and colleagues,18 who found among 107 HD patients in Switzerland, the mean self-efficacy level was moderately high (110 out of 150). Analyzing each item separately showed that HD patients reported least confidence in limiting processed meat, followed by limiting salty snacks, and were most confident in avoiding table salt. This suggests that interventions to restrict sodium intake in HD patients may want to focus on strategies to enhance confidence for limiting processed meat and salty snacks.
Among the sociodemographic variables collected in the BalanceWise study, younger age and perceived income inadequacy were associated with low dietary self-efficacy level in HD patients. Park et al.26 also found significantly lower confidence to follow dietary recommendations among younger HD patients. It is possible that younger HD patients are more likely to dine out and socialize with friends, thus have less confidence to follow their dietary recommendations. 2,5,8,26 Consistent with our findings, Chan and colleagues16 reported that low income is a significant predictor of low confidence to follow a healthy lifestyle, in general. Perceived financial hardship may exist among HD patients making it less likely for them to purchase the generally more expensive, unprocessed food products that are relatively low in sodium.
STRENGTHS AND LIMITATIONS
BalanceWise included a robust, diverse sample of patients recruited from multiple dialysis units located in Western Pennsylvania. Despite the morbidity and mortality associated with end stage kidney disease and the complex nature of the treatment regimen, there were relatively few losses to follow up. We were unable to find similar studies that examined the role of baseline self-efficacy on intervention efficacy and, thus, the findings presented here are novel.
However, the following limitations should be considered in drawing conclusions from this analysis. The current analysis is post hoc and subject to the problem of multiple testing. In addition, use of self-reported dietary intakes for analysis of dietary sodium density is subject to measurement error. Unfortunately, objective biomarkers of sodium intake, namely 24-hour urinary sodium output, are not valid in individuals with advanced renal failure who produce little or no urine. In order to minimize error and bias in dietary reporting, participants received training on portion size estimation, and recalls were unscheduled and collected across dialysis treatment and week days at each time point.
PRACTICAL APPLICATION
In this study, we found that participants with low level of self-efficacy appeared to benefit most from a behavioral intervention trial. Given the need to stretch research and healthcare resources, this finding may have far-reaching implications for planning efficacious interventions. Although evaluating patient self-efficacy may seem impractical for the busy dietitian, approaches to identify the right dietary intervention for the patient (i.e. personalized nutrition) may help to improve efficiency and effectiveness, as time is not spent delivering interventions that are unlikely to result in lasting behavior change. This is, in fact, already standard practice, as patients are typically selected for specific dietary interventions based on perceived risk, or ongoing problems with a disease outcome. We have identified two sociodemographic factors associated with low dietary self-efficacy (and perhaps more likely to respond to an SCT-based approach) in HD patients, younger age and perceived income inadequacy. Additional research in this area may help to streamline efforts to deliver tailored and patient-centered behavioral approaches for patient care, and ultimately improve health outcomes.
Acknowledgments:
This research was supported in part by funding from NIH grants NINR/R01-NR010135 (PI: Mary Ann Sevick, ScD), NINR/NIDDK/NHLBI/NIA-K24-NR012226 (PI: Mary Ann Sevick, ScD), and NIMHD/K99 MD012811 (PI: Lu Hu, PhD). Portions of this research were presented at the 37th Annual Meeting of the Society of Behavioral Medicine (SBM) in April 2016, Washington DC.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:None
Contributor Information
Lu Hu, New York University School of Medicine, Center for Healthful Behavior Change.
David E. St-Jules, New York University School of Medicine, Center for Healthful Behavior Change.
Collin J. Popp, New York University School of Medicine, Center for Healthful Behavior Change.
Mary Ann Sevick, New York University School of Medicine, Center for Healthful Behavior Change.
REFERENCES
- 1.Desroches S, Lapointe A, Ratté S, Gravel K, Légaré F, Turcotte S. Interventions to enhance adherence to dietary advice for preventing and managing chronic diseases in adults. Cochrane Database Syst Rev. 2013;(2):CD008722. doi: 10.1002/14651858.CD008722.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.St-Jules DE, Woolf K, Pompeii M Lou, Sevick MA. Exploring problems in following the hemodialysis diet and their relation to energy and nutrient intakes: The BalanceWise Study. J Ren Nutr. 2016;26(2):118–124. doi: 10.1053/j.jrn.2015.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kugler C, Vlaminck H, Haverich A, Maes B. Nonadherence with diet and fluid restrictions among adults having hemodialysis. J Nurs Scholarsh. 2005;37(1):25–29. [DOI] [PubMed] [Google Scholar]
- 4.Murtagh FE, Addington-Hall J, Higginson IJ. The prevalence of symptoms in end-stage renal disease: A systematic review. Adv Chronic Kidney Dis. 2007;14(1):82–99. doi: 10.1053/j.ackd.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Kugler C, Maeding I, Russell CL. Non-adherence in patients on chronic hemodialysis: An international comparison study. J Nephrol. 2011;24(3):366–375. doi: 10.5301/JN.2010.5823. [DOI] [PubMed] [Google Scholar]
- 6.Clark-Cutaia MN, Ren D, Hoffman LA, Burke LE, Sevick MA. Adherence to hemodialysis dietary sodium recommendations: Influence of patient characteristics, self-efficacy, and perceived barriers. J Ren Nutr. 2014;24(2):92–99. doi: 10.1053/j.jrn.2013.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saran R, Bragg-Gresham JL, Rayner HC, et al. Nonadherence in hemodialysis: Associations with mortality, hospitalization, and practice patterns in the DOPPS. Kidney Int. 2003;64(1):254–262. doi: 10.1046/j.1523-1755.2003.00064.x. [DOI] [PubMed] [Google Scholar]
- 8.Meuleman Y, Hoekstra T, Dekker FW, et al. Perceived Sodium Reduction Barriers Among Patients with Chronic Kidney Disease: Which Barriers Are Important and Which Patients Experience Barriers? Int J BehavMed. 2018;25(1):93–102. doi: 10.1007/s12529-017-9668-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bandura A. Social cognitive theory: An agentic perspective. Annu Rev Psychol.2001. ;52:1–26. https://www.uky.edu/~eushe2/Bandura/Bandura2001ARPr.pdf. Accessed May 30, 2017. [DOI] [PubMed] [Google Scholar]
- 10.Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13(4):623–649. doi: 10.1080/08870449808407422. [DOI] [Google Scholar]
- 11.Sevick MA, Stone RA, Novak M, et al. A PDA-based dietary self-monitoring intervention to reduce sodium intake in an in-center hemodialysis patient. Patient Prefer Adherence. 2008;2:177–184. http://www.ncbi.nlm.nih.gov/pubmed/19920960. Accessed March 12, 2018. [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson ES, Winett RA, Wojcik JR. Self-regulation, self-efficacy, outcome expectations, and social support: Social cognitive theory and nutrition behavior. Ann Behav Med. 2007;34(3):304–312. doi: 10.1007/BF02874555. [DOI] [PubMed] [Google Scholar]
- 13.Burke LE, Ewing LJ, Ye L, et al. The SELF trial: A self-efficacy-based behavioral intervention trial for weight loss maintenance. Obesity. 2015;23(11):2175–2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sevick MA, Korytkowski M, Stone RA, et al. Biophysiologic Outcomes of the Enhancing Adherence in Type 2 Diabetes (ENHANCE) Trial. J Acad Nutr Diet. 2012;112(8): 1147–1157. doi: 10.1016/j.jand.2012.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stacey FG, James EL, Chapman K, Courneya KS, Lubans DR. A systematic review and meta-analysis of social cognitive theory-based physical activity and/or nutrition behavior change interventions for cancer survivors. J Cancer Surviv. 2015;9(2):305–338. doi: 10.1007/s11764-014-0413-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chan YM, Zalilah MS, Hii SZ. Determinants of compliance behaviours among patients undergoing hemodialysis in malaysia. PLoS One. 2012;7(8):e41362.doi: 10.1371/journal.pone.0041362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsay S-L, Healstead M. Self-care self-efficacy, depression, and quality of life among patients receiving hemodialysis in Taiwan. Int J Nurs Stud. 2002;39(3):245–251. doi: 10.1016/S0020-7489(01)00030-X. [DOI] [PubMed] [Google Scholar]
- 18.Zrinyi M, Juhasz M, Balla J, et al. Dietary self-efficacy: Determinant of compliance behaviours and biochemical outcomes in haemodialysis patients. Nephrol Dial Transplant. 2003; 18(9): 1869–1873. doi: 10.1093/ndt/gfg307. [DOI] [PubMed] [Google Scholar]
- 19.Oka M, Chaboyer W. Influence of self-efficacy and other factors on dietary behaviours in japanese haemodialysis patients. Int J Nurs Pract. 2001;7(6):431–439. doi: 10.1046/j.1440-172X.2001.00334.x. [DOI] [PubMed] [Google Scholar]
- 20.Jafari M, Mannani R, Zarea K. The association between self-concept and self-efficacy in patients under treatment by hemodialysis. Jundishapur J Chronic Dis Care.2015;4(3): e27222. doi: 10.5812/jjcdc.27222v2. [DOI] [Google Scholar]
- 21.Sevick MA, Piraino BM, St-jules DE, et al. No difference in average interdialytic weight gain observed in a randomized trial with a technology-supported behavioral intervention to reduce dietary sodium intake in adults undergoing maintenance hemodialysis in the United States : Primary outcomes of. J Ren Nutr. 2016;26(3): 149–158. doi: 10.1053/j.jrn.2015.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sevick MA, Zickmund S, Korytkowski M, et al. Design, feasibility, and acceptability of an intervention using personal digital assistant-based self-monitoring in managing type 2 diabetes. Contemp Clin Trials. 2009;29(3):396–409. doi: 10.1016/j.cct.2007.09.004.Design. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clark-Cutaia MN, Ren D, Hoffman LA, Snetselaar LG, Sevick MA. Psychometric validation of the self-efficacy for restricting dietary salt in hemodialysis scale. Top Clin Nutr. 2013;28(4):384–391. doi: 10.1530/ERC-14-0411.Persistent [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schakel SF. Maintaining a Nutrient Database in a Changing Marketplace: Keeping Pace with Changing Food Products—A Research Perspective. J Food Compos Anal. 2001;14(3):315–322. doi: 10.1006/JFCA.2001.0992. [DOI] [Google Scholar]
- 25.Schakel SF, Sievert YA, Buzzard IM. Sources of data for developing and maintaining a nutrient database. J Am Diet Assoc. 1988;88(10): 1268–1271. http://www.ncbi.nlm.nih.gov/pubmed/3171020. Accessed March 12, 2018. [PubMed] [Google Scholar]
- 26.Park KA, Choi-Kwon S, Sim YM, Kim SB. Comparison of Dietary Compliance and Dietary Knowledge Between Older and Younger Korean Hemodialysis Patients. J Ren Nutr. 2008;18(5):415–423. doi: 10.1053/j.jrn.2008.04.004. [DOI] [PubMed] [Google Scholar]