Abstract
Objective
Japanese Orthopaedic Association (JOA) scoring systems were developed to evaluate the neurological function of patients with cervical or lumbar degeneration. As patient‐based and multi‐dimensional clinical evaluation tools, these systems should be capable of reflecting the walking disability of patients. The association between JOA scores and gait parameters, however, are not well characterized. The purpose of this study was to determine the correlations between JOA scores and gait parameters of patients with cervical spondylotic myelopathy (CSM) and lumbar intervertebral disc herniation (LDH).
Methods
A total of 32 CSM and 30 LDH patients with gait dysfunction were recruited for the present study. All patients were diagnosed by two senior orthopaedic doctors and evaluated with JOA scoring systems. A body‐mounted motion analyzer, the Intelligent Device for Energy Expenditure and Activity (IDEEA), was applied to measure gait parameters of patients across 30 m of flat floor in an orthopaedic ward. A linear regression model was used to determine the correlations between JOA scores and gait parameters. Multiple linear regressions were used to identify the relationships between subsections of the JOA systems and gait parameters.
Results
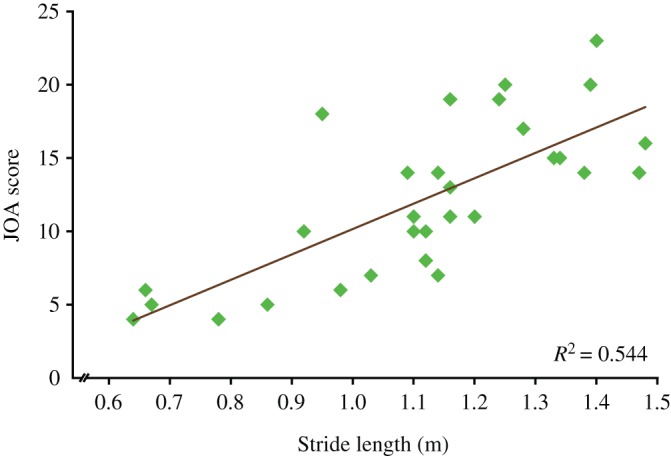
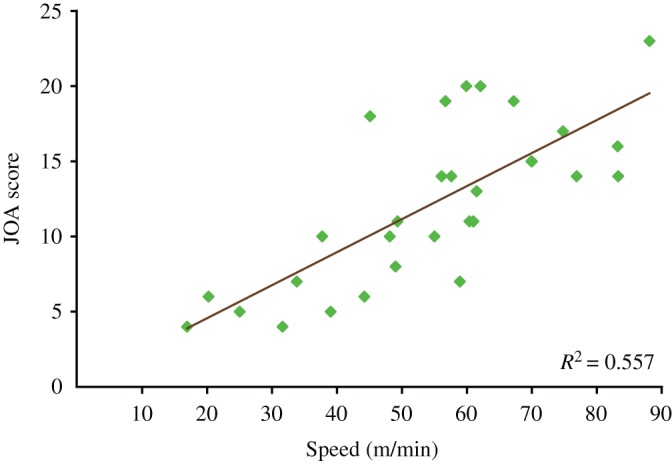
Japanese Orthopaedic Association scores of LDH patients from the JOA lumbar scoring system are significantly correlated with gait speed (R 2 = 0.557, P < 0.001) and stride length (R 2 = 0.544, P < 0.001). JOA scores are also correlated with double support duration, step duration, cycle duration and cadence, and weakly correlated with single support duration. For the four subsections of the JOA lumbar scoring system, “restriction of activities of daily living” is the significant predictor of all gait parameters, especially gait speed (R 2 = 0.573, P < 0.001) and stride length (R 2 = 0.553, P < 0.001). However, JOA scores of CSM patients from the JOA cervical scoring system are only weakly correlated with these measures (all R 2 < 0.3). For the four subsections of the JOA cervical scoring system, “motor function of the lower extremity” is a weak predictor of gait parameters (all R 2 < 0.3).
Conclusions
There is a significant correlation between gait parameters and functional disability as measured by the JOA lumbar scoring system, which indicates that the JOA lumbar scoring system can reflect gait impairment. The JOA cervical scoring system, however, may need to be improved for efficiently evaluating the walking ability of CSM patients in the assessment of motor function of the lower extremity.
Keywords: Cervical spondylotic myelopathy, Gait, JOA scores, Lumbar intervertebral disc herniation
Introduction
Cervical spondylotic myelopathy (CSM) is a degenerative disorder of the cervical spine characterized by narrowing of the cervical spinal canal and compression of the spinal cord1, 2, 3. Clinical manifestations of CSM may include symptoms such as paresthesia in the upper limbs, spastic paraparesis, impaired sensation, and gait disturbance4. When cervical medullary are compressed to a certain degree, gait abnormalities such as unsteady walking and impaired balance may be observed; such abnormalities are a strong indication for surgical intervention and can be used as an index to assess postoperative recovery.
Lumbar intervertebral disc herniation (LDH) is a localized displacement of disc material beyond the normal margins of the lumbar intervertebral disc space resulting in lumbar nerve roots irritation, which is a common generic of lumbar spinal degeneration5. The clinical presentation may include lower back pain, sciatica, radicular leg pain, changes in sensation, and weakness in the muscles of the hips or legs6, 7, which leads to walking disability and physical restrictions in daily life.
Self‐report measures are essential in the management of patients with degenerative spine disease, and are usually classified as generic or disease‐specific. There are several common generic self‐report measures, including the Medical Outcomes Survey Short‐Form 36 (SF‐36)8, the Oswestry Disability Index (ODI)9, the Visual Analogue Scale (VAS)10, and the Japanese Orthopaedic Association (JOA) scoring systems. Among these self‐report measures, the JOA scoring systems, which were released by the Clinical Outcome Committee of the JOA, are among the most common and widely used evaluation systems in Asia11, 12, 13. The JOA scoring systems are meant to capture data related to function, perceived disability, and symptoms, including gait disturbance of patients with spinal degeneration. There are two types of JOA scoring systems to evaluate spinal degeneration in patients: the JOA cervical scoring system for clinical evaluation of patients with cervical myelopathy and the JOA lumbar scoring system for evaluating lumbar spinal degeneration14, 15.
As gait abnormalities comprise an important indication for surgical intervention of CSM and LDH patients and an index by which postoperative recovery can be assessed, it is necessary for orthopaedists to evaluate the walking disability of patients during routine clinical visits. Orthopaedists commonly use self‐report measures such as the JOA scoring systems to evaluate gait deviations before and after surgery16, 17, which, however, are somewhat subjective and qualitative18, 19, 20. The associations between the JOA systems and objective measures of gait in patients with spinal degeneration are not well characterized. In addition, it is still unknown whether the JOA cervical and lumbar scoring systems are able to reflect the walking disability of patients. The purpose of this study was to determine the correlation between JOA scores and patients’ gait parameters, and to evaluate the effectiveness of functional assessments of the JOA cervical and lumbar scoring systems.
Patients and Methods
Inclusion Criteria and Exclusion Criteria
The following inclusion criteria were applied: (i) ability to complete basic activities of daily living; (ii) ability to mobilize at least 30 m without assistance of another person; and (iii) clinical and radiological evidence of CSM or LDH diagnosed by two senior orthopaedic physicians.
Patients were excluded from the study if they: (i) were affected by severe respiratory or cardiac disease that hindered safe mobilization; (ii) were affected by other neurological or orthopaedic disorders that affect gait; (iii) previously underwent any orthopaedic surgery; or (iv) were pregnant.
Patient Data
From September 2013 to March 2015, 32 CSM patients with gait dysfunction and 30 LDH patients with unilateral leg pain (Table 1) were consecutively recruited from Tianjin Hospital, Tianjin, China. The durations of gait dysfunction in CSM patients were from 2 months to 3 years, and from 3 weeks to 8 months in LDH patients.
Table 1.
General characteristics of patients
| Variables | CSM | LDH | P‐value |
|---|---|---|---|
| Age (years) | 56.1 ± 9.9 | 38.7 ± 12.8 | <0.001* |
| Gender (male: female) | 23:9 | 23:7 | — |
| Height (cm) | 169.0 ± 9.3 | 173.0 ± 6.4 | 0.057 |
| Weight (kg) | 75.3 ± 15.3 | 75.2 ± 10.6 | 0.967 |
indicates significant difference between the CSM group and the LDH group.
Values of age, height and weight are mean ± standard deviation.
CSM, cervical spondylotic myelopathy; LDH, lumbar intervertebral disc herniation
—, none.
The study was approved by the Institutional Review Board at Tianjin Hospital, Tianjin, China and the Capital Medical University, Beijing, China. All subjects provided informed consent before participation.
Japanese Orthopaedic Association Scoring Systems
Since 1975, the Japanese Orthopaedic Association has advocated the use of a more sophisticated system for evaluating cervical myelopathy21. The JOA cervical scoring system consists of four subsections, including six categories: motor function of the upper and lower extremities, sensory function of the upper and lower extremities, and trunk and bladder function. The highest possible total score from the six categories for a normal person is 17 points. The JOA cervical scoring system has been shown to have excellent intra‐observer and inter‐observer reliability for patients with CSM21. In this study, the JOA cervical scoring system was used to evaluate the neurological function of patients with CSM.
Selected members of the Japanese Orthopaedic Association developed the JOA lumbar scoring system in 198622. The system consists of four subsections, including 14 categories with overall headings of subjective symptoms, clinical signs, restriction of activities of daily living, and bladder function. The highest possible total score from categories for a normal person is 29 points. The JOA lumbar scoring system has demonstrated high validity and reliability in populations with degenerative lumbar spinal disorders. In this study, the JOA lumbar scoring system was used to evaluate the neurological function of patients with LDH.
Gait Analysis
A body‐mounted motion analyzer, the Intelligent Device for Energy Expenditure and Activity (IDEEA [Minisun, Fresno, CA, USA]), was used to capture gait parameters (sampling frequency 64 Hz). The IDEEA consists of a data recorder (a 32‐bit microprocessor that enables real‐time acquisition) and seven body‐mounted motion sensors that detect acceleration and displacement in three dimensions (Fig. 1). The initial preparation of each participant was to tape the seven motion sensors onto the skin surface. The sensor on the chest and the sensors on the thighs were connected to the recorder by cables. The sensors on the ankle and feet communicated with the recorder wirelessly. This type of portable body‐mounted monitor is well accepted by patients, and is useful for clinical assessments. Previous studies have shown that the IDEEA is highly accurate in both healthy adults and in patients23, 24, 25.
Figure 1.

Intelligent Device for Energy Expenditure and Activity (IDEEA) system: (A) composition of IDEEA; (B) the sensor on chest; (C) the sensors on thighs; (D) the sensors on ankles; and (E) the sensors on the bottom of feet.
For consistency of the measurement, one trained researcher placed the sensors for all of the trials. Each participant was asked to sit in an upright position with their thighs parallel to the floor and their hips, knees, and ankles flexed to 90° while the system performed a baseline calibration. Once the calibration was completed, the system immediately began recording.
Patients were asked to walk at a self‐selected comfortable pace for 30 m while gait parameters were collected by the IDEEA. Acquired data were subsequently transferred to a personal computer for data analysis. For the middle 20 strides, spatiotemporal parameters, including single support duration, double support duration, step duration, cycle duration, gait speed, cadence, and stride length, were analyzed using the IDEEA software (GaitView software, Version 3.7 [Minisun]26).
Statistical Analysis
The SPSS Version 12.0 (SPSS, Chicago, IL, USA) statistical package was used for statistical analysis. General characteristics were compared between the CSM group and the LDH group using Student's t‐test. To analyze the correlation between JOA scores evaluated by physicians and parameters of gait provided by IDEEA, a linear regression model was fitted between each gait parameter and JOA score. The F‐test was used to analyze the significance of the relation between two variables. Multiple linear regression was applied to assess which subsections of the JOA cervical scoring system (motor functions of the upper and lower extremities, sensory function, and bladder function) and the JOA lumbar scoring system (subjective symptoms, clinical signs, restriction of activities of daily living, and bladder function) were strong predictors of gait parameters. The level of statistical significance was set at P < 0.05.
Results
Correlations between Japanese Orthopaedic Association Cervical Scores and Gait Parameters
Correlations between JOA scores of CSM and LDH patients and all gait parameters are summarized in Table 2. The JOA scores for CSM are only weakly correlated with double support time, step duration, cycle duration, gait speed, cadence, and stride length. They are not correlated with single support duration.
Table 2.
Correlations between Japanese Orthopaedic Association scores and gait parameters
| Parameter | CSM | LDH | ||
|---|---|---|---|---|
| R 2 | P value | R 2 | P value | |
| Single support duration (ms) | 0.003 | 0.763 | 0.349 | 0.001 |
| Double support duration (ms) | 0.251 | 0.004 | 0.456 | <0.001 |
| Step duration (ms) | 0.205 | 0.009 | 0.466 | <0.001 |
| Cycle duration (s) | 0.194 | 0.012 | 0.459 | <0.001 |
| Gait speed (m/min) | 0.171 | 0.019 | 0.557 | <0.001 |
| Cadence (steps/min) | 0.178 | 0.016 | 0.477 | <0.001 |
| Stride length (m) | 0.171 | 0.019 | 0.544 | <0.001 |
R 2 refers to the coefficient of determination of the linear regression
P is the level of significance.
CSM, cervical spondylotic myelopathy; LDH, lumbar intervertebral disc herniation.
Correlations between Japanese Orthopaedic Association Lumbar Scores and Gait Parameters
The JOA scores for LDH are significantly correlated with gait speed (R 2 = 0.557, P < 0.001) (Fig. 2) and stride length (R 2 = 0.544, P < 0.001) (Fig. 3). They also correlate with double support duration, step duration, cycle duration, and cadence, and are weakly correlated with single support duration.
Figure 2.
Correlation between the Japanese Orthopaedic Association (JOA) lumbar score and gait speed.
Figure 3.
Correlation between the Japanese Orthopaedic Association (JOA) lumbar score and stride length.
Multiple Linear Regression Analyses for Subsections of the Japanese Orthopaedic Association Cervical Scoring System and Gait Parameters
Multiple linear regression analyses for subsections of the JOA cervical scoring system and gait parameters are summarized in Table 3. Among the four sections of the JOA cervical scoring system, “motor function of lower extremity” could be the predictor of most of the gait parameters, but it does not provide unique significant prediction of the gait parameters (R 2 < 0.3 in all regression models for subsections of the JOA cervical scoring system and gait parameters).
Table 3.
Multiple linear regression analyses for subsections of the Japanese Orthopaedic Association cervical scoring system and gait parameters
| Dependent variable | Predictors | R 2 | P value |
|---|---|---|---|
| Single support duration (ms) | None | — | — |
| Double support duration (ms) | Motor function of lower extremity | 0.240 | 0.004 |
| Step duration (ms) | Motor function of lower extremity | 0.258 | 0.003 |
| Cycle duration (s) | Motor function of lower extremity | 0.252 | 0.003 |
| Gait speed (m/min) | Motor function of lower extremity | 0.283 | 0.002 |
| Cadence (steps/min) | Motor function of lower extremity | 0.246 | 0.004 |
| Stride length (m) | Motor function of lower extremity | 0.271 | 0.002 |
—, none.
Multiple Linear Regression Analyses for Subsections of the Japanese Orthopaedic Association Lumbar Scoring System and Gait Parameters
Multiple linear regression analyses for subsections of the JOA lumbar scoring system and gait parameters are summarized in Table 4. Among the four sections of the JOA lumbar scoring system, “restriction of activities of daily living” could be the predictor of gait parameters. It contributes significantly to gait parameters (R 2 > 0.4 in most of the regression models for subsections of the JOA lumbar scoring system and gait parameters), especially gait speed (R 2 = 0.573) and stride length (R 2 = 0.553).
Table 4.
Multiple linear regression analyses for subsections of the Japanese Orthopaedic Association lumbar scoring system and gait parameters
| Dependent variable | Predictors | R 2 | P value |
|---|---|---|---|
| Single support duration (ms) | Restriction of activities of daily living | 0.332 | 0.001 |
| Double support duration (ms) | Restriction of activities of daily living | 0.458 | <0.001 |
| Step duration (ms) | Restriction of activities of daily living | 0.471 | <0.001 |
| Cycle duration (s) | Restriction of activities of daily living | 0.462 | <0.001 |
| Gait speed (m/min) | Restriction of activities of daily living | 0.573 | <0.001 |
| Cadence (steps/min) | Restriction of activities of daily living | 0.480 | <0.001 |
| Stride length (m) | Restriction of activities of daily living | 0.553 | <0.001 |
Discussion
Comparison of Gait Assessments between Japanese Orthopaedic Association Cervical and Lumbar Scoring Systems
For CSM patients, gait disturbance is the main reason for surgical intervention. Approximately 80% of patients with CSM have preoperative gait dysfunction27. Alteration in gait can contribute to the surgeon's decision to recommend operative intervention28. Okada et al. reported on 37 patients with cervical spondylotic myelopathy or cervical spinal stenosis that had hyperreflexia and impaired sensation; however, walking disability was considered as the primary indication for operative treatment and for evaluating the effect of the surgery29. There is evidence that individuals with CSM have a slower gait speed, prolonged double support duration, and reduced stride length30. We found, however, that the JOA scores of the CSM patients were only weakly correlated with these gait parameters (all R 2 < 0.3), suggesting that the JOA cervical scoring system does not adequately reflect the gait impairment of these patients. Kuhtz‐Buschbeck et al. found that gait analysis was more reliable and sensitive than the JOA scoring system in detecting improved walking after surgical decompression of the cervical spinal cord31.
Compared with the JOA cervical scoring system, the JOA lumbar scoring system is more reliable for evaluating the walking ability of patients: The JOA scores of LDH patients are significantly correlated with gait speed (R 2 = 0.557) and stride length (R 2 = 0.544). They are also correlated with double support duration, step duration, cycle duration, and cadence, although R 2 are not as high as gait speed and stride length. It has been noted clinically that walking disability and muscle weakness are among the several functional deficits associated with LDH32. Reduced velocity, stride length, cadence, and increased double support duration in patients with LDH have also been reported in previous studies33. Our study results have shown a significant correlation between JOA scores for LDH and gait parameters, which indicates that the JOA lumbar scoring system is more efficient for evaluating the walking ability of patients compared to the JOA cervical scoring system.
Predictors of Gait Parameters in Japanese Orthopaedic Association Cervical and Lumbar Scoring Systems
The association between JOA scores of CSM and gait parameters is weaker than the JOA scores for LDH and gait parameters. The weak association may be due to the fewer questions in the score system about the functions of the lower extremities. Among the four sections of the JOA cervical scoring system, “motor function of the lower extremity” is the predictor of most of the gait parameters in this study. However, “motor function of the lower extremity” could not provide unique significant prediction for gait parameters (R 2 < 0.3 in all regression models for subsections of the JOA cervical scoring system and gait parameters). Among these four sections of the JOA cervical scoring system (total six categories), only one category (“motor function of lower extremity”) is related to motor function of the lower extremity, which only counts for 4 of the total 17 points (approximately one‐quarter of the total). Meanwhile, 6 of 14 categories of the JOA lumbar scoring systems (i.e. leg pain and/or tingling, gait, motor disturbance, straight‐leg‐raising test, standing, and walking) are related to function of the lower extremity, which counts for 14 of the total 29 points (approximately half of the total). In addition, other than the lack of assessment of motor function in the JOA cervical scoring system, another possible reason is that the symptoms in cervical spinal stenosis are mainly neuron symptoms with dyscoordination, which may be insufficiently detected by the questionnaire and/or the gait measurement device. The cardinal symptoms of patients with LDH are described as muscle weakness, leg pain, and/or numbness and lower back pain, and such symptoms can directly affect the gait. As a primary indication for operative treatment and an index for assessing the effect of an operation for spinal degeneration patients, the JOA scores should truly reflect gait impairment. Therefore, we believe that the JOA cervical scoring system should add more questions about motor function of the lower extremity so that the JOA cervical scoring system can be more effective for evaluating patients’ walking ability.
Among the four sections of the JOA lumbar scoring system, “restriction of activities of daily living” is the predictor of all gait parameters. “Restriction of activities of daily living” is significantly correlated to most of the gait parameters in our study (R 2 > 0.4 in most of the regression models for subsections of the JOA lumbar scoring system and gait parameters), especially gait speed (R 2 = 0.573) and stride length (R 2 = 0.553). This means that among all subsections of the JOA lumbar scoring system, “activities of daily living” adequately reflects the gait disturbance of patients. When LDH patients are evaluated using the JOA lumbar scoring system, “activities of daily living” could be a key subsection for orthopaedists and therapists to examine.
Self‐Report Measures and Instrumented Gait Analysis
Self‐report measures such as JOA scoring systems are widely used due to their convenience. The subjectivity and non‐specificity of self‐report measurements, however, can lead to uncertainty16, 34. Although the association between the JOA lumbar scoring system and gait parameters was relatively significant, the correlations observed in this study between JOA scores and gait parameters were not statistically strong. As walking disability is one of the cardinal symptoms of spinal degeneration, gait parameters of patients can be fundamental measures of physical capacity and performance. Due to recent advancement in portable technology, quantitative and portable gait analysis is possible outside the laboratory, and can be used by orthopaedists to evaluate patients during routine clinical visits.
Limitations
There are some limitations in this study. Subjects were not grouped by gender in this study due to the limited number of patients within the two groups. Studies with larger number of subjects may need to be carried out to examine whether gender would affect the correlations between the JOA scores and gait parameters. In addition, only the JOA scoring systems were used in this study. In future, different scoring systems such as SF‐36 and ODI may need to be considered for determining the correlations between scores and gait parameters.
Conclusion
There is a significant correlation between gait parameters and functional disability as measured by the JOA lumbar scoring system, which indicates that the JOA lumbar scoring system can reflect gait impairment. The JOA cervical scoring system, however, may need to be improved for efficient evaluation of the walking ability of CSM patients in the assessment of motor function of the lower extremity.
Acknowledgments
This study was partially supported by the National Natural Science Foundation of China (Grant 31170900), the Beijing Natural Science Foundation Program and Scientific Research Key Program Foundation Program and Scientific Research Key Program of the Beijing Municipal Commission of Education (Grant KZ201310025010), and the Research Fund for the Doctoral Program of Higher Education of China (Grant 20121107110018).
Disclosure: There are no conflicts of interests to declare with respect to financial or personal relationships. All authors meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors; all authors are in agreement with the content of the manuscript.
Contributor Information
Ji‐dong Zhang, Email: f175726627@sina.com, Email: kzhang@ccmu.edu.cn.
Kuan Zhang, Email: kzhang@ccmu.edu.cn, Email: f175726627@sina.com.
References
- 1. Garza‐Ramos R, Nicholas B, Kerezoudis P, et al. Deep‐wound and organ‐space infection after surgery for degenerative spine disease: an analysis from 2006 to 2012. Neurol Res, 2016: 117–123. [DOI] [PubMed] [Google Scholar]
- 2. Sasiadek MJ, Bladowska J. Imaging of degenerative spine disease‐‐the state of the art. Adv Clin Exp Med, 2012, 21: 133–142. [PubMed] [Google Scholar]
- 3. Montgomery DM, Brower RS. Cervical spondylotic myelopathy. Clinical syndrome and natural history. Orthop Clin North Am, 1992, 23: 487–493. [PubMed] [Google Scholar]
- 4. Liu B, Ma W, Zhu F, Guo CH, Yang WL. Comparison between anterior and posterior decompression for cervical spondylotic myelopathy: subjective evaluation and cost analysis. Orthop Surg, 2012, 4: 47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fardon DF, Milette PC. Nomenclature and classification of lumbar disc pathology. Recommendations of the combined task forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976), 2001, 26: E93–E113. [DOI] [PubMed] [Google Scholar]
- 6. Rissanen A, Kalimo H, Alaranta H. Effect of intensive training on the isokinetic strength and structure of lumbar muscles in patients with chronic low back pain. Spine (Phila Pa 1976), 1995, 20: 333–340. [DOI] [PubMed] [Google Scholar]
- 7. Takada E, Takahashi M, Shimada K. Natural history of lumbar disc hernia with radicular leg pain: spontaneous MRI changes of the herniated mass and correlation with clinical outcome. J Orthop Surg (Hong Kong), 2001, 9: 1–7. [DOI] [PubMed] [Google Scholar]
- 8. King JJ, McGinnis KA, Roberts MS. Quality of life assessment with the medical outcomes study short form‐36 among patients with cervical spondylotic myelopathy. Neurosurgery, 2003, 52: 113–120. discussion 121 [DOI] [PubMed] [Google Scholar]
- 9. Fairbank JC, Pynsent PB. The Oswestry disability index. Spine (Phila Pa 1976), 2000, 25: 2940–2952. [DOI] [PubMed] [Google Scholar]
- 10. Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health, 1990, 13: 227–236. [DOI] [PubMed] [Google Scholar]
- 11. Kimura I, Shingu H, Murata M, Hashiguchi H. Lumbar posterolateral fusion alone or with transpedicular instrumentation in L4‐‐L5 degenerative spondylolisthesis. J Spinal Disord, 2001, 14: 301–310. [DOI] [PubMed] [Google Scholar]
- 12. Zhang JD, Xia Q. Role of intraoperative disc contrast injection in determining the segment responsible for cervical spinal cord injury without radiographic abnormalities. Orthop Surg, 2015, 7: 239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yu PF, Jiang H, Liu JT, et al. Traditional Chinese medicine treatment for ruptured lumbar disc herniation: clinical observations in 102 cases. Orthop Surg, 2014, 6: 229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Edwards CN, Riew KD, Anderson PA, Hilibrand AS, Vaccaro AF. Cervical myelopathy. Current diagnostic and treatment strategies. Spine J, 2003, 3: 68–81. [DOI] [PubMed] [Google Scholar]
- 15. Osawa T, Ogura T, Hayashida T, Mori M, Hase H. Evaluation of lumbosacral nerve root lesions using evoked potentials recorded by a surface electrode technique. Spine (Phila Pa 1976), 2003, 28: 496–501. [DOI] [PubMed] [Google Scholar]
- 16. Conrad BP, Shokat MS, Abbasi AZ, Vincent HK, Seay A, Kennedy DJ. Associations of self‐report measures with gait, range of motion and proprioception in patients with lumbar spinal stenosis. Gait Posture, 2013, 38: 987–992. [DOI] [PubMed] [Google Scholar]
- 17. Park SJ, Kim SB, Kim MK, Lee SH, Oh IH. Clinical features and surgical results of cervical myelopathy caused by soft disc herniation. Korean J Spine, 2013, 10: 138–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kim CR, Yoo JY, Lee SH, Lee DH, Rhim SC. Gait analysis for evaluating the relationship between increased signal intensity on t2‐weighted magnetic resonance imaging and gait function in cervical spondylotic myelopathy. Arch Phys Med Rehabil, 2010, 91: 1587–1592. [DOI] [PubMed] [Google Scholar]
- 19. Deie M, Hoso T, Shimada N, et al. Differences between opening versus closing high tibial osteotomy on clinical outcomes and gait analysis. Knee, 2014, 21: 1046–1051. [DOI] [PubMed] [Google Scholar]
- 20. Zeifang F, Schiltenwolf M, Abel R, Moradi B. Gait analysis does not correlate with clinical and MR imaging parameters in patients with symptomatic lumbar spinal stenosis. BMC Musculoskelet Disord, 2008, 9: 89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K. Interobserver and intraobserver reliability of the japanese orthopaedic association scoring system for evaluation of cervical compression myelopathy. Spine (Phila Pa 1976), 2001, 26: 1890–1895. [DOI] [PubMed] [Google Scholar]
- 22. Fujiwara A, Kobayashi N, Saiki K, Kitagawa T, Tamai K, Saotome K. Association of the Japanese Orthopaedic Association score with the Oswestry Disability Index, Roland‐Morris Disability Questionnaire, and short‐form 36. Spine (Phila Pa 1976), 2003, 28: 1601–1607. [PubMed] [Google Scholar]
- 23. Zhang K, Werner P, Sun M, Pi‐Sunyer FX, Boozer CN. Measurement of human daily physical activity. Obes Res, 2003, 11: 33–40. [DOI] [PubMed] [Google Scholar]
- 24. Saremi K, Marehbian J, Yan X, et al. Reliability and validity of bilateral thigh and foot accelerometry measures of walking in healthy and hemiparetic subjects. Neurorehabil Neural Repair, 2006, 20: 297–305. [DOI] [PubMed] [Google Scholar]
- 25. Kwon S, Jamal M, Zamba GK, Stumbo P, Samuel I. Validation of a novel physical activity assessment device in morbidly obese females. J Obes, 2010, 2010, doi: 10.1155/2010/856376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gorelick ML, Bizzini M, Maffiuletti NA, Munzinger JP, Munzinger U. Test–retest reliability of the IDEEA system in the quantification of step parameters during walking and stair climbing. Clin Physiol Funct Imaging, 2009, 29: 271–276. [DOI] [PubMed] [Google Scholar]
- 27. Emery SE, Bohlman HH, Bolesta MJ, Jones PK. Anterior cervical decompression and arthrodesis for the treatment of cervical spondylotic myelopathy. Two to seventeen‐year follow‐up. J Bone Joint Surg Am, 1998, 80: 941–951. [DOI] [PubMed] [Google Scholar]
- 28. Rao RD, Gourab K, David KS. Operative treatment of cervical spondylotic myelopathy. J Bone Joint Surg Am, 2006, 88: 1619–1640. [DOI] [PubMed] [Google Scholar]
- 29. Okada K, Shirasaki N, Hayashi H, Oka S, Hosoya T. Treatment of cervical spondylotic myelopathy by enlargement of the spinal canal anteriorly, followed by arthrodesis. J Bone Joint Surg Am, 1991, 73: 352–364. [PubMed] [Google Scholar]
- 30. Malone A, Meldrum D, Bolger C. Gait impairment in cervical spondylotic myelopathy: comparison with age‐ and gender‐matched healthy controls. Eur Spine J, 2012, 21: 2456–2466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kuhtz‐Buschbeck JP, Johnk K, Mader S, Stolze H, Mehdorn M. Analysis of gait in cervical myelopathy. Gait Posture, 1999, 9: 184–189. [DOI] [PubMed] [Google Scholar]
- 32. Morag E, Hurwitz DE, Andriacchi TP, Hickey M, Andersson GB. Abnormalities in muscle function during gait in relation to the level of lumbar disc herniation. Spine (Phila Pa 1976), 2000, 25: 829–833. [DOI] [PubMed] [Google Scholar]
- 33. Lee JH, An JH, Lee SH, Seo IS. Three‐dimensional gait analysis of patients with weakness of ankle dorsiflexor as a result of unilateral L5 radiculopathy. J Back Musculoskelet Rehabil, 2010, 23: 49–54. [DOI] [PubMed] [Google Scholar]
- 34. Rainville J, Childs LA, Pena EB, et al. Quantification of walking ability in subjects with neurogenic claudication from lumbar spinal stenosis‐‐a comparative study. Spine J, 2012, 12: 101–109. [DOI] [PMC free article] [PubMed] [Google Scholar]


