Abstract
Background:
Uncontrolled hypertension constitutes a significant challenge throughout the world. Blood pressure measurement by patients is informative for both patients and providers, but is rarely performed systematically, thereby reducing its utility. Mobile phones can be used to efficiently prompt individuals to measure blood pressure and automate data management while avoiding technology barriers to widespread adoption. Presented is the design and pilot test results of MyBP, an automated texting intervention to support blood pressure self-monitoring and patient self-management.
Methods:
Three sequential phases are described: 1) stakeholders’ needs assessment, 2) preliminary design pilot (n=10), and 3) a six-week pilot of the re-designed comprehensive program with hypertensive patients (n=43) recruited from three clinical sites (Emergency Department, Primary Care, Hypertension Center). Outcomes of interest included, participant adherence, perceived importance of blood pressure monitoring and healthy behavior change.
Results:
Median adherence to MyBP prompts over six weeks was 79% (72% Emergency Department, 84% Primary Care and 96% Hypertension Center, H(2)=5.56, p=0.06). Adherence did not vary by age, gender, education or baseline use of texting, but was lowest among patients recruited from the Emergency Department (χ(2)2=6.66, p=0.04). In the exit survey, MyBP was associated with increased importance of blood pressure self-monitoring and particularly motivated primary care and emergency department groups to improve dietary habits, increase daily physical activity and focus on stress reduction. The majority of participants (88%) indicated interest in using the program for 6 months.
Conclusions:
Automated mobile-phone based blood pressure self-monitoring using MyBP is feasible, acceptable and scalable, and may improve self-management and support clinical care.
Keywords: hypertension, home blood pressure measurement, self-management, text messaging, eHealth
Graphical Abstract:
Hypertension affects an estimated 30% of the world’s adult population1 and is a primary source of all-cause death as well as stroke, heart disease and kidney failure. Despite significant improvements in hypertension diagnosis and treatment, over half of US adults with hypertension have uncontrolled blood pressure2. Due to the recent changes to the ACC/AHA hypertension guidelines, specifically redefining stage 1 hypertension from 140–159/90–99 to 130–139/80–89 mm Hg and setting a goal of <130/80 mm Hg for all patients3, healthcare systems face an even bigger challenge with hypertension management.
Hypertension diagnosis and medical management are traditionally based on office blood measurements. However, office measurements are highly variable, potentially unreliable and influenced by the “white coat” effect (the increase of blood pressure that occurs in the medical care environment)4. Often, clinicians find these isolated readings insufficient to guide hypertension care including initiating or intensifying therapy5,6. Sparse, periodic BP readings can also leave patients feeling confused, making it difficult for them to understand if and when they need to alter blood pressure-related health behaviors (e.g. medication adherence, DASH diet, daily exercise, and stress reduction)7.
Evidence indicates measuring blood pressure outside the traditional clinical setting (i.e., blood pressure self-monitoring) is feasible and informative for both patients and providers8–11. However, patients lack guidance in performing reliable and systematic measurement and documentation. A range of communication technologies to better leverage blood pressure self-monitoring for hypertension management have been tested12. Despite promising results, broad implementation has not occurred. Limitations of existing programs include: 1) use of blood pressure self-monitoring solely for clinical decision-making (i.e., “telemonitoring”), which neglects patient engagement and inadvertently perpetuates provider-centered care8,13,14); 2) utilization of clinical personnel (e.g. pharmacists, nurses, etc.) for recurring communication via secure websites, email, text or telephone9,15, resources that most general practices cannot provide; and 3) deployment of specialized equipment (e.g. Bluetooth enabled blood pressure devices), assumption of facile use of a smartphone with Wi-Fi service 24/7, or both16,17, thereby creating financial and/or technology literacy access barriers. Therefore, we sought to design a mobile phone-based intervention that assists blood pressure self-monitoring and self-care while minimizing cost and technology barriers.
METHODS
The study had three phases: 1) needs assessment and conceptual modeling, 2) preliminary design and alpha testing, and 3) program redesign and pilot testing in patients with hypertension in varied clinical settings: primary care, emergency medicine, and specialty care. Methods and results of each phase are presented sequentially. The following procedures were approved by the University of Pittsburgh’s Institutional Review Board. For more methodological detail of each phase refer to the online supplement.
Phase 1: Needs Assessment and Conceptual Modeling Methods
A team of representative clinical investigators ascertained the needs of stakeholders (patients with hypertension, primary care providers and health system administrators) through a series of meetings and focus groups.
Results
Input from investigators and stakeholders led to assembly of core constructs (online supplement Table I) and generated a general strategy and conceptual model to support hypertension self-management. Because hypertension is largely asymptomatic, individuals living with elevated blood pressure are often unaware of their condition and whether or not their blood pressure is controlled. Therefore, we identified hypertension health-literacy and blood pressure self-monitoring with timely feedback as key intervention elements. Frequently, patients are unsuccessful in self-management due to inadequate or inaccurate understanding of hypertension, its health risks and proper measurement, and the various health behaviors that raise or lower blood pressure. Also, patients struggle to understand quantification of blood pressure and its inherent variability. While knowledge of one’s blood pressure is considered to be crucial information, patients find it difficult to measure their blood pressure systematically and calculate averages, which would determine hypertension control. This constrains patients from developing accurate health beliefs and adequate self-efficacy related to hypertension self-management.
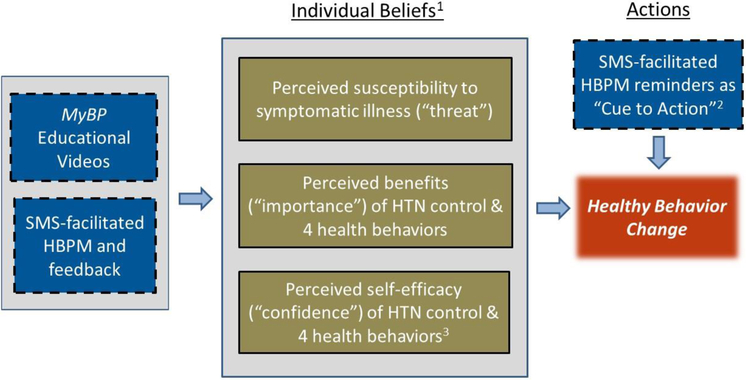
The conceptual model (Figure I) for MyBP illustrates how hypertension education coupled with assistance in systematic blood pressure self-monitoring and feedback may improve relevant health behaviors. We concluded this conceptualization phase with primary objectives and design components including: 1) education delivered at patients’ convenience using high-quality, web-accessed videos supplemented by periodic health tip messages, 2) proactive and personalized messaging to aid patients in systematic blood pressure self-monitoring, 3) automated, bidirectional messaging to efficiently provide timely reinforcement and feedback, 4) blood pressure data management with automated summaries, and 5) time delimited averaging to generate reliable estimates and permit detection of change in blood pressure over time. The system requests a blood pressure reading on two mornings and two evenings each week. This provides a sufficient number of readings to calculate an updated blood pressure average every 2 weeks18 without over-burdening patients during long-term self-monitoring.
Figure 1: Conceptual Model for the Design of MyBP in Hypertension Self-Management.
Adapted from Health Belief and other health behavior models. Intervention components are noted in blue boxes.
(1) Individuals beliefs are also influenced by a variety of fixed factors, such as age, gender, culture, and education.
(2) SMS reminders directly cue BP self-measurement and indirectly nudge thinking and action of related health behaviors.
(3) Although not illustrated, feedback loops exist through which behavior change, BP change, or both may increase self-efficacy.
Phase 2: Preliminary Design and Feasibility Testing
Methods
Phase 2 aims were to: a) program the alpha version of an automated SMS system to guide blood pressure self-monitoring with feedback, and b) conduct a 4-week feasibility study to assess response rates to prompted blood pressure self-measurement and collect qualitative feedback in a semi-structured phone interview.
Results
Ten patients with hypertension submitted blood pressure readings in response to 84% of prompts after a mean delay of 18 minutes. In an exit phone interview, most participants stated that using MyBP was a positive experience, found the program easy to use, and felt it was akin to using a journal to keep themselves accountable.
Phase 3: Program Re-Design and Pilot Testing in Varied Clinical Settings
Methods
Phase 3 aims were to revise and expand the features of MyBP, and conduct more in-depth pilot testing in several clinical settings. The pilot study aims were to: 1) examine operational fidelity, 2) quantify participant utilization, 3) assess any impact on patients’ beliefs and behaviors related to hypertension and hypertension self-management, and 4) determine whether usage and responses varied as a function of clinical setting, age, gender, race, education or baseline use of texting.
Blood pressure self-monitoring was scheduled for self-selected times on two mornings and two evenings each week and demarcated into two-week recording periods. Receipt of an automated text message prompted participants to take a blood pressure reading with their own blood pressure cuff and text back reading. Every two weeks, participants received a text report containing adherence to blood pressure self-monitoring and, if at least four readings were submitted, the average blood pressure in comparison with their previous two-week average.
Participant samples
Patients diagnosed with hypertension and able to text were recruited by a research staff member at an urban emergency room, a general internal medicine clinic, and a hypertension referral center. Participants who did not own an automated blood pressure cuff were given a validated device (A&D Medical UA−-767FAC), and participants received $30 at study completion.
Measures
Sample characteristics.
Medical information (current BP, prescription medications, body mass index and medical history) was abstracted from the medical record and patient sociodemographic characteristics were self-reported. At baseline, current blood pressure self-monitoring and use of texting was provided by self-report.
The messaging system database contained all outgoing (computer generated) and incoming messages (participant generated), and was used to examine operational fidelity, participant adherence and reported BP values. Adherence was calculated as the proportion of blood pressure prompts to which patients replied with blood pressure readings divided by the total of prompts in each two-week monitoring period and across all monitoring periods. At study completion, a survey about MyBP acceptance and impact on health behaviors was administered (online supplement Table II).
Statistical Analysis
Descriptive statistical analyses of variables of interest (demographics, health characteristics, participant engagement, texting experience, and adherence) were organized by site. Group differences were determined using chi-square or Fisher’s exact for nominal and ordinal variables, and analysis of variance (ANOVA) for continuous variables. Median adherence for each group was calculated and compared across groups using the Kruskal-Wallis H test. Quartile rank of adherence to blood pressure prompts was calculated, with the low adherence quartile contrasted with the upper 3 quartiles using analyses analogous to those described above, with the addition of Spearman’s correlation with ordinal variables and point-biserial correlation with continuous variables. A repeated-measures ANOVA was conducted to determine whether there was a statistically significant difference in mean blood pressure over the course of the three two-week periods. Post hoc testing with Bonferroni corrections were performed using standardized adjusted Pearson residuals to determine the source of any significant chi-square or Fisher’s exact result with a threshold of ±219 and Tukey post hoc comparisons with significant ANOVA results. SPSS version 24.0 software (SPSS Inc.) was used for all analyses.
Results
A six-week pilot test of the re-designed MyBP program was conducted with 43 patients enrolled from three clinical settings. Table I provides participant characteristics by recruitment site. Fourteen additional patients signed consent forms but did not enroll. Compared to those enrolled, these 14 individuals were somewhat younger and less educated but similar in race, gender, average BMI and average blood pressure (online supplement Table III).
Table I.
Characteristics of Enrolled Participants by Recruitment Site
| Total n=43 |
Emergency Department n=22 |
Primary Care Office n=10 |
Hypertension Referral Center n=11 |
Group Differences |
|
|---|---|---|---|---|---|
| Age, mean (range) | 54 (34–70) | 53 (34–70) | 59 (49–67) | 54 (38–66) | p= 0.11 |
| Sex, n (% female) | 25 (58%) | 10 (46%) | 8 (80%) | 7 (64%) | p= 0.19 |
| Race, n (% black) | 26 (61%) | 15 (68%) | 8 (80%) | 3 (27%) | p= 0.03 |
| Education, n (%) | |||||
| High school only | 17 (40%) | 11 (50%) | 3 (30%) | 3 (27%) | p= 0.06 |
| Some college/tech | 12 (28%) | 8 (36%) | 3 (30%) | 1 (9%) | |
| training | 14 (33%) | 3 (15%) | 4 (40%) | 7 (64%) | |
| Bachelors or higher | |||||
| Body mass index (kg/m2) | 34 (22–47) | 33 (22–43) | 36 (30–41) | 33 (23–47) | p= 0.44 |
| Systolic BP, mean (range) | 157 (110–250) | 169 (140–250) | 156 (129193) | 136 (110–160) | p<0.001 |
| Diastolic BP, mean (range) | 94 (70–130) | 98 (72–130) | 96 (74–124) | 83 (70–100) | p= 0.01 |
| Number of Antihypertensive medications, mean (range) | 2.1 (0–5) | 1.6 (0–5) | 2.1 (0–4) | 3.1 (1–5) | p= 0.02 |
| Owned a BP cuff, n (%) | 12 (28%)a | 2 (9%)c | 0 (0%) | 11 (100%) | p<.001 |
| Checked own BP in past month, n (%) | 18 (42%)b | 7 (32%)d | 0 (0%) | 11 (100%) | p<.001 |
| Average number of texts sent per day, n (%) | |||||
| 0 | 2 (5%) | 1 (5%) | 1 (10%) | 0 (0%) | p=0.76 |
| 1–2 | 10 (23%) | 5 (23%) | 3 (30%) | 2 (18%) | |
| 3 or more | 31 (72%) | 16 (72%) | 6 (60%) | 9 (82%) |
n=40,
n=42,
n=19,
n=21
There were no statistically significant differences among participants across the three recruitment sites in terms of age, sex, and BMI. Compared to the other two groups, the Hypertension Center group had more white participants, lower blood pressure, had received a greater number of prescribed antihypertensive medications, and more often owned a blood pressure cuff and performed blood pressure self-monitoring at baseline. Emergency Department participants tended to have the lowest level of completed education.
Program fidelity
During the first two months of enrollment at the Hypertension Center and Emergency Department, through participant feedback and manual inventory of the SMS database we found that: 1) the program was failing to send about 25% of blood pressure reminders, 2) the two-week reports occasionally omitted the two-week blood pressure average, and 3) and the two-week reports sometimes miscalculated adherence with blood pressure self- monitoring. These issues were addressed by our programmer within two weeks and before enrollment of Primary Care patients. Subsequent manual auditing of the messaging database revealed high operational fidelity.
Blood Pressure Readings
Thirty-three participants submitted blood pressure readings sufficient to calculate an average blood pressure over each of the three successive two-week blood pressure monitoring periods. The average blood pressure for periods 1, 2 and 3 were 144/89, 140/87, and 142/88 mmHg, respectively. There was not a statistically significant change in mean systolic or diastolic blood pressure over the three two-week periods (systolic (F (1.6, 49.7) =.88, p=.39), diastolic (F (2,64) = 1.37, p=.26)).
Adherence
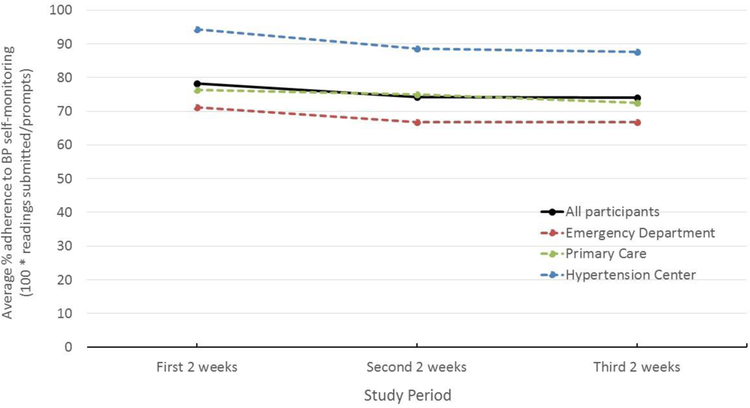
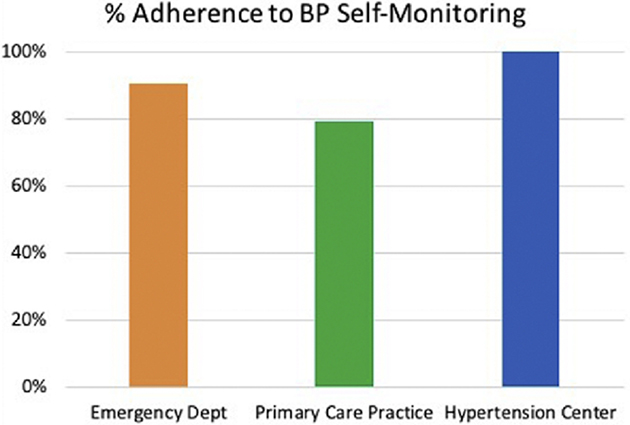
Of the 43 participants, all but two (both from the Emergency Department) began sending blood pressure readings in response to message prompts. Three other patients (all from the Emergency Department) opted out of blood pressure monitoring for the third two- week monitoring period. Figure II displays the average adherence across the 6 weeks according to recruitment site. Overall, the median blood pressure self-monitoring adherence across the 6 weeks was 79% (72% Emergency Department, 84% Primary Care and 96% Hypertension Center, H(2)=5.56, p=0.06). The frequency distribution is available in online supplement Figure I.
Figure II.
Average adherence to home BP monitoring in response to MyBP prompts by recruitment site.
Characteristics associated with adherence
In the low quartile, the median adherence to blood pressure prompts was 48%, as compared to 92% among remaining patients. Table II compares characteristics of low and high adhering patients. Of the low adherers, 41% were Emergency Department participants (χ(2)2=6.66,` p=0.04) and black race trended toward significance (p=0.09). Otherwise, adherence to blood pressure self-monitoring with MyBP did not vary notably by age, gender, education or baseline use of texting.
Table II.
Characteristics of Low and Adequately Adherent Participants
| Low Adherers n=11 |
Adequate Adherers n=32 |
Group Differences |
|
|---|---|---|---|
| Mean percent Adherence to blood pressure self-monitoring (range) | 38% (0–68%) | 88% (69–100%) | P<0.001c |
| Recruitment site | |||
| Emergency Department | 9 (82%) | 13 (40%) | |
| Primary Care | 2 (18%) | 8 (25%) | p=0.04d |
| Hypertension Center | 0 | 11 (24%) | |
| Age, mean (range) | 54 (43–67) | 55 (34–70) | p=0.81 |
| Sex, n (% female) | 6 (54%) | 19 (59%) | p=0.78 |
| Race, n (% black) | 9 (82%) | 17 (53%) | p=0.09 |
| Education, n (%) | |||
| High school only | 5 (46%) | 12 (38%) | p= 0.38 |
| Some college/tech training | 4 (36%) | 8 (25%) | |
| Bachelors or higher | 2 (18%) | 12 (38%) | |
| Body mass index (kg/m2) | 34 (25–42) | 33 (22–47) | p=0.74 |
| Systolic BP, mean (range) | 157 (129–187) | 157 (110–250) | p=0.99 |
| Diastolic BP, mean (range) | 97 (72–130) | 93 (70–130) | p=0.44 |
| Number of Antihypertensive | |||
| medications | 2.5 (1–5) | 2(0–5) | p=0.26 |
| mean (range) | |||
| Owned a BP cuff, n (%) | 1 (9%)a | 11 (34%)b | p=0.36 |
| Checked own BP in past month, n (%) | 3 (27%)a | 15 (46.9%) | p= 0.47 |
| Self-reported text messages sent per day, n (%) | 0 | 2 (6%) | |
| 0 | 4 (36%) | 6 (19%) | p=0.55 |
| 1–2 | 7 (64%) | 24 (75%) | |
| 3 or more |
n=10,
n=30,
rpb(41)=0.8,
χ2(2)=6.66
Effects on patients’ beliefs and behaviors related to hypertension and hypertension self-management
An exit survey was completed by telephone in 40 of the 43 participants. The three not completing the survey (all from the Emergency Department group) had withdrawn from the program and multiple attempts to reach them by phone were unsuccessful.
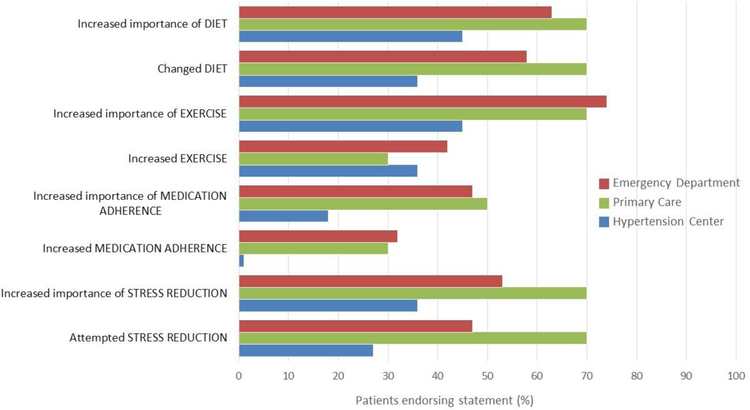
Most respondents indicated that use of MyBP increased their sense of the importance of blood pressure self-monitoring. In addition, over 75% of patients indicated an interest in using the program for substantially longer (i.e., 6 months). Overall, participants reported that the MyBP program increased the sense of the importance of medication adherence, a healthy diet, regular exercise and stress management (Figure III). In addition, most patients reported changing one or more health behaviors in response to use of the MyBP program. Behavioral changes were largest in the Primary Care and Emergency Department groups.
Figure III.
Survey results -- Patient-reported changes in cognitions and health behaviors after using MyBP
DISCUSSION
This multi-phase study aimed to develop and pilot test MyBP, an automated, bidirectional, text-based monitoring system to support patients in hypertension self- management. Findings from the first two phases assisted in the development of a set of key design constructs and a theoretically supported conceptual model and confirmed that SMS was a viable digital communication platform. Feasibility testing of the re-designed MyBP program in patients from three distinct clinical sites again revealed high rates of blood pressure reporting overall (79%), but a somewhat lower rate in participants from the urban ED. Using a minimum of four readings (50% adherence) every two weeks in order to provide a reliable average, the large majority of our participants submitted a sufficient number of readings to reasonably estimate and track readings over successive two-week monitoring periods.
Exit survey results showed the majority of participants liked using the MyBP program, were willing to use it for an extended period of time and reported changing at least one health- related behavior in response to MyBP. Primary Care and Emergency Department patients were especially motivated to increase medication adherence, improve their diet, increase physical activity or engage in stress reduction. This may be attributable to the effects of the program’s video education and regular BP self-monitoring on the salience and importance of blood pressure control and behaviors affecting blood pressure.
Meta-analyses of randomized clinical trials indicate that having patients conduct blood pressure self-monitoring leads to a fall in blood pressure20,21. Blood pressure self-monitoring may increase patient’s daily awareness of his or her BP and provide feedback that improves adherence to BP-lowering health behaviors and overall hypertension management9,22,23. Current trials using web/mobile technologies to support blood pressure self-monitoring are identifying design features that may increase blood pressure reduction achieved by blood pressure self-monitoring24.
However, as mentioned in the introduction many of these innovations constitute barriers to usefulness and feasibility in routine clinical practice. For example, the trials lead by Magid and Margolis each achieved BP control 20%−30% more often in intervention patients compared to control patients, but the programs provided patients with a special BP monitor which they used to periodically download readings to a website monitored by clinical pharmacists who had recurring contact with patients via face-to-face visits, phone appointments or secure email15,25. The CAATCH trial included computerized patient education modules, a series of nurse-administered behavioral/lifestyle telephone group counseling sessions, and monthly onsite continuing education for the primary care physicians. It failed to show effectiveness due to low adherence with the multicomponent intervention26. These considerations, along with development work completed in Phase 1, drove MyBP design objectives: simplicity for the user, convenient low-cost patient education, tailoring for patient convenience, and automated, proactive communication with recurring feedback.
Several features of MyBP are worth highlighting. First, it uses a ubiquitous, inexpensive and proactive modality (i.e. SMS) to communicate with patients. The utility of SMS is particularly relevant since, due to controversial concerns about data security health systems may feel compelled to invest in alternative, “secure messaging systems”27. Second, the algorithm provides patients with running averages of their BP with a data refresh every two weeks. This served the purpose of emphasizing one’s blood pressure average, thus reducing unnecessary preoccupation with isolated readings. Third, MyBP provided summary data on blood pressure trends, empowering patients by delivering valid feedback on the blood pressure effects of their behaviors. Fourth, simple self-management strategy tips were delivered each week; these may prompt specific behaviors within the context of patients’ daily lives, thus increasing the chances of behavioral adoption.
The current feasibility data are small in number but suggest that MyBP may be acceptable to and used by the majority of patients across different clinical settings and sociodemographic characteristics. Additionally, the program generates what we believe are reliable blood pressure averages over successive two-week monitoring periods28, and favorably motivates patients as reflected in changes in perceived importance of blood pressure control and self-reported changes in health behaviors. It is unclear whether continued use of MyBP will encourage improvement in, and maintenance of healthy behavior changes via the direct feedback of acceptable blood pressure readings. Our work to date is also limited by its short duration and absence of integration with the provider or electronic health record. Our next version of MyBP will add automated reports routed to the primary care provider. Providers are often dubious regarding the reliability of patient-generated blood pressure readings29–31. Using MyBP, patients take blood pressure measurements after learning proper technique and using a systematic approach to self-monitoring which generates sequential, time-delimited blood pressure averages. These features may raise providers’ confidence in blood pressure self- monitoring data32 and permit more informed and timely medication management13,33,34.
Ultimately, the effectiveness and feasibility of MyBP as an adjunct to standard medical care depends on patient engagement but also on providers’ sense of its utility in achieving and maintaining blood pressure control in patients with hypertension. Thus, testing MyBP in randomized trials of clinical effectiveness along with implementation research35 are necessary to more fully evaluate its potential role in clinical practice.
Supplementary Material
Highlights:
Blood pressure self-monitoring is vital in patients with uncontrolled hypertension.
MyBP uses ubiquitous texting as its platform for automated communication.
Feedback consisted of blood pressure averages and trend reports every two weeks.
Initial testing in three diverse clinical settings suggested high engagement.
Use was associated with patient-initiated improvements in health behaviors.
ACKNOWLEDGEMENTS
We would like to acknowledge the assistance of the following organizations and individuals. Each was integral to the development and study of the MyBP program.
○ The UPP Academic Foundation provided seed funding.
○ Patients from the three clinical study sites served as volunteer study participants.
○ Mr. Jack Doman designed and programmed the automated SMS system.
○ Francis Solano, MD (Medical Director, Center for Quality Improvement and Innovation, UPMC Health System), Jeanette South-Paul, MD (Chair, Department of Family Medicine, University of Pittsburgh School of Medicine), Gary Fischer, MD (Medical Director, General Medicine Ambulatory Care, UPMC), Stephen Perkins, MD (Vice President, Medical Affairs, UPMC Health Plan) are each clinical administrators who provided insight regarding hypertension management within health care systems and insurance plans, and offered recommendations and feedback regarding MyBP.
○ Emmi Solutions, Inc. created the hypertension education videos which were used through a lease agreement with UPMC Health System.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None
REFERENCES
- 1.Mills KT, Bundy JD, Kelly TN, et al. Global Disparities of Hypertension Prevalence and Control. Circulation. 2016;134(6):441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2016 update. Circulation. 2016;133(4):e38–e360. [DOI] [PubMed] [Google Scholar]
- 3.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017. [Google Scholar]
- 4.Muldoon M, Kronish I, Shimbo D. Of signal and noise: Overcoming challenges in blood pressure measurement to optimize hypertension care. Circulation: Cardiovascular Quality and Outcomes. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135(9):825–834. [DOI] [PubMed] [Google Scholar]
- 6.Huebschmann AG, Mizrahi T, Soenksen A, Beaty BL, Denberg TD. Reducing Clinical Inertia in Hypertension Treatment: a Pragmatic Randomized Controlled Trial. J Clin Hypertens (Greenwich). 2012;14(5):322–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martin LR, Williams SL, Haskard KB, DiMatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1(3):189–199. [PMC free article] [PubMed] [Google Scholar]
- 8.Anthony CA, Polgreen LA, Chounramany J, et al. Outpatient blood pressure monitoring using bi-directional text messaging. J Am Soc Hypertens. 2015;9(5):375–381. [DOI] [PubMed] [Google Scholar]
- 9.Bosworth HB, Powers BJ, Olsen MK, et al. Home blood pressure management and improved blood pressure control: results from a randomized controlled trial. Arch Intern Med. 2011;171(13):1173–1180. [DOI] [PubMed] [Google Scholar]
- 10.Chandak AJ A Self-management of hypertension using technology enabled interventions in primary care settings. Technol Health Care. 2015;23(2):119–128. [DOI] [PubMed] [Google Scholar]
- 11.McLean GB R;Saunderson K;Hanlon P;Murray E;Little P;McManus RJ;Yardley L;Mair FS Digital interventions to promote self-management in adults with hypertension systematic review and meta-analysis. Journal of hypertension. 2016;34(4):600–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suffoletto B, Muldoon M. Not all texts are created equal: Design considerations for text message interventions to improve antihypertensive medication adherence. J Clin Hypertens (Greenwich). 2017;19(12):1285–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Omboni S, Gazzola T, Carabelli G, Parati G. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta-analysis of randomized controlled studies. Journal of hypertension. 2013;31(3):455–467; discussion 467–458. [DOI] [PubMed] [Google Scholar]
- 14.Parati G, Omboni S, Albini F, et al. Home blood pressure telemonitoring improves hypertension control in general practice. The TeleBPCare study. Journal of hypertension. 2009;27(1):198–203. [DOI] [PubMed] [Google Scholar]
- 15.Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. Jama. 2013;310(1):46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Logan AG, McIsaac WJ, Tisler A, et al. Mobile phone-based remote patient monitoring system for management of hypertension in diabetic patients. Am J Hypertens. 2007;20(9):942–948. [DOI] [PubMed] [Google Scholar]
- 17.Walker W, Polk T, Hande A, Bhatia D. Remote blood pressure monitoring using a wireless sensor network. Paper presented at: 6th Annual IEEE Emerging Information Technology Conference 2006. [Google Scholar]
- 18.Powers BJ, Olsen MK, Smith VA, Woolson RF, Bosworth HB, Oddone EZ. Measuring blood pressure for decision making and quality reporting: where and how many measures? Annals of internal medicine. 2011;154(12):781–788. [DOI] [PubMed] [Google Scholar]
- 19.Agresti A An introduction to categorical data analysis. Vol 135: Wiley New York; 1996. [Google Scholar]
- 20.Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-Measured Blood Pressure Monitoring in the Management of Hypertension: A Systematic Review and Meta-analysis. Ann Intern Med. 2013;159(3):185–194. [DOI] [PubMed] [Google Scholar]
- 21.Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ. 2004;329(7458):145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pickering TG, White WB, Giles TD, et al. When and how to use self (home) and ambulatory blood pressure monitoring. J Am Soc Hypertens. 2010;4(2):56–61. [DOI] [PubMed] [Google Scholar]
- 23.Lee CJ, Park S. The Role of Home Blood Pressure Telemonitoring for Blood Pressure Control. Pulse (Basel). 2016;4(2–3):78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tucker KL, Sheppard JP, Stevens R, et al. Self-monitoring of blood pressure in hypertension: A systematic review and individual patient data meta-analysis. PLoS Med. 2017;14(9):e1002389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Magid DJ, Olson KL, Billups SJ, Wagner NM, Lyons EE, Kroner BA. A pharmacist-led, American Heart Association Heart360 Web-enabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes. 2013;6(2):157–163. [DOI] [PubMed] [Google Scholar]
- 26.Ogedegbe G, Tobin JN, Fernandez S, et al. Counseling African Americans to Control Hypertension: cluster-randomized clinical trial main effects. Circulation. 2014;129(20):2044–2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Drolet BC. Text messaging and protected health information: what is permitted? Jama. 2017;317(23):2369–2370. [DOI] [PubMed] [Google Scholar]
- 28.Self-Measured Blood Pressure Monitoring: Action Steps for Clinicians In: Prevention CfDCa, ed. Atlanta GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2014. [Google Scholar]
- 29.Shimbo D, Abdalla M, Falzon L, Townsend RR, Muntner P. Role of Ambulatory and Home Blood Pressure Monitoring in Clinical Practice: A Narrative Review. Ann Intern Med. 2015;163(9):691–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kronish IM, Kent S, Moise N, et al. Barriers to conducting ambulatory and home blood pressure monitoring during hypertension screening in the United States. J Am Soc Hypertens. 2017;11(9):573–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nordmann A, Frach B, Walker T, Martina B, Battegay E. Reliability of patients measuring blood pressure at home: prospective observational study. BMJ. 1999;319(7218):1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Parker RA, Paterson M, Padfield P, et al. Are self-reported telemonitored blood pressure readings affected by end-digit preference: a prospective cohort study in Scotland. BMJ Open. 2018;8(1):e019431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Agarwal R, Bills JE, Hecht TJW, Light RP. Role of Home Blood Pressure Monitoring in Overcoming Therapeutic Inertia and Improving Hypertension Control. Hypertension (Dallas, Tex: 1979). 2011;57(1):29. [DOI] [PubMed] [Google Scholar]
- 34.Stergiou GS, Bliziotis IA. Home blood pressure monitoring in the diagnosis and treatment of hypertension: a systematic review. Am J Hypertens. 2011;24(2):123–134. [DOI] [PubMed] [Google Scholar]
- 35.Marvel FA, Wang J, Martin SS. Digital Health Innovation: A Toolkit to Navigate From Concept to Clinical Testing. JMIR Cardio. 2018;2(1):e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.