Abstract
Objective:
Distress tolerance (DT), the ability to withstand aversive internal states, represents an important risk factor for substance use relapse and a potential treatment target. Neurobiological research in substance using populations suggests that continued substance use could erode DT, whereas abstinence could bolster it. The current study characterized trajectories of behavioral and self-reported indices of DT and examined the prospective effect of substance use on DT trajectories among those seeking treatment for substance use.
Method:
Individuals (N=263, Mage=42.68 (SD=11.8), 70.7% male, 94.7% African American) in residential substance use treatment completed subjective (Distress Tolerance Scale) and behavioral (Mirror Tracing Persistence Task-Computerized Version) DT measures, as well as report of daily substance use (Timeline Follow-Back) over 5 assessment time-points from pre-treatment to 12-months post-treatment. Latent curve modeling estimated DT trajectories and their associations with substance use behavior, including abstinence duration (days until first use) and substance use frequency (percentage of substance use days between assessments).
Results:
Self-reported and behavioral DT indicators both exhibited positive, nonlinear change over time (standardized slope parameter estimates: βDTS=0.61, p<.01; βMTPT-C=0.34, p<.01). Abstinence duration was associated with greater improvement in behavioral (β=.20, p=.03) DT specifically. Frequency of use was statistically significantly associated with attenuated behavioral DT at 6-month (β=−.12, p=.03) and 12-month follow-ups (β=−.08, p=.045).
Conclusions:
Distress tolerance appears to improve appreciably post-treatment, and return to substance use may shape the degree of this improvement. Collectively, these findings support the conceptualization of DT as a malleable treatment target and emphasize the benefit of abstinence on improvement in DT.
Keywords: distress tolerance, substance use, treatment, abstinence
Substance use disorder (SUD) affects approximately 21.5 million people, or 8.1% of the U.S. population (Substance Abuse and Mental Health Services Administration, 2014). Among those who receive treatment for SUD, approximately half relapse to use within one year of discharge from treatment (McLellan et al., 2000; National Institute on Drug Abuse, 2012), highlighting the need for further investigation into the nature and course of risk factors for post treatment relapse.
According to the negative reinforcement model of addiction, individuals learn to use substances as a pre-potent response in order to gain relief from negative affect (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004; Koob & Le Moal, 1997). It follows that the ability to tolerate negative affect in service of a larger goal (i.e. abstinence) will be associated with a lower risk for substance use following treatment. Indeed, distress tolerance (DT), or the actual or perceived ability to persist in goal-directed activity while withstanding physical or psychological discomfort (McHugh et al., 2011), is regarded as a proxy for negative reinforcement behavior, and has consistently been associated with indices of substance use. Lower DT as measured with a behavioral task, namely persistence in a goal directed task while experiencing affective distress, is significantly associated with increased rates of post treatment substance use, treatment dropout, and early relapse (Brandon et al., 2003; Brown, Lejuez, Kahler, & Strong, 2002; Cameron, Reed, & Ninnemann, 2013; Daughters et al., 2005a; Daughters et al., 2005b; Strong et al., 2012). Lower perceived DT, assessed via self-report, has been related to higher rates cannabis use following a quit attempt (Hasan, Babson, Banducci, & Bonn-Miller, 2015), and reports of greater substance use problems (Ali et al., 2013; Burjarski et al., 2012; Howell et al., 2010; Zvolensky et al., 2009).
Taken together, DT represents an important risk factor for relapse to substance use. Accordingly, as substance use treatment development efforts have targeted the mechanisms known to contribute to poor treatment response, novel DT-specific interventions (Bornovalova et al., 2012), and existing treatments with DT-specific components (Dimeff & Linehan, 2008), have been incorporated into substance use treatment with promising results. However, an unanswered question is the degree to which distress tolerance may change over time after treatment entry, in the absence of a DT targeted intervention.
Indeed, neurobiological and cognitive evidence support the notion that abstinence from substance use, and alternatively continued substance use, has significant impact on multiple cognitive and biobehavioral processes as well as neurobiological structure and function, such as executive function (see Snyder, Miyake, & Hankin, 2015 for review), processing of affective stimuli (Schmidt et al., 2014) and emotion regulation (Berking et al., 2011; Dingle, da Costa Neves, Alhadad, & Hides, 2017). While these deficits are exacerbated by substance use (Schulte et al., 2014; Verdejo-García & Pérez-García, 2007; Vonmoos et al., 2014), partial to full recovery is evident among treatment-seeking individuals (Lookatch et al., 2017; Schrimsher & Parker, 2008) and begin to occur with as little as 2–3 weeks of abstinence from substance use (Garavan, Brennan, Hester, & Whelan, 2013; Littlefield et al., 2015; Schulte et al., 2014). Though the way in which cognitive and neural recovery occurs is more complex than mere reversal of damage incurred from continued use (Connolly et al., 2013), neurobiological changes continue to occur, albeit nonlinearly (Durazzo et al., 2015; Zou et al 2018), with prolonged abstinence (Seo & Sinha, 2015). Theoretical conceptualizations posit that successful distress tolerance involves both executive control and the inhibition of emotion-driven responses in order to successfully tolerate negative affective states in favor of a larger goal, such as abstinence. Individuals with low DT who used substances evidence reduced activation in, and functional connectivity between, neural regions involved in inhibitory control, working memory, emotion processing, and motor planning and execution (Daughters et al., 2016), supporting the notion that the neurological impact of substance use contributes to distress tolerance.
The current study had two main objectives. First, we sought to characterize the longitudinal trajectory of DT among substance use treatment-seeking individuals assessed at five time points over a one-year period. The goal here was to fill a gap in the literature regarding the malleability of DT over time for those who use substances and are treatment seeking. Second, given evidence for the recovery of neurobiological and cognitive processes contributing to DT with abstinence from substance use, we tested the impact of both abstinence and substance use frequency on the DT trajectory. We hypothesized that DT would improve following treatment entry, and that such improvements would be associated with longer abstinence duration and decreased frequency of substance use over time.
Methods
Participants
The study sample consisted of 263 patients enrolled in residential substance use treatment in a large urban area. Of these, 70.7% (n = 186) were male, 94.7% were African American (n = 249), 3% Caucasian (n = 8), 1.9% Native American/American Indian (n = 5) and 0.4% Asian (n = 1). Additionally, 192 (73%) individuals had at least a high school education or GED, and 213 (81.0%) were unemployed. The mean age of the sample was 42.68 years (SD = 11.76). Current DSM-IV substance dependence diagnoses included cocaine (n = 86; 32.0%) alcohol (n = 81; 30.8%), hallucinogen (n = 37, 14.1%), opioid (n = 31; 11.8%), marijuana (n = 28; 10.7%), and sedative (n = 2; 0.8%), with 25.1% (n = 66) meeting dependence criteria for more than one substance.
Procedure
Data for this study were part of a larger project assessing the effectiveness of a behavioral treatment for substance use as compared to a contact time matched control condition (Daughters et al., 2017). Patients at a residential treatment facility were approached by research staff and assessed for study eligibility within one week of treatment entry. Study exclusion criteria were: 1) <5th grade English reading level; 2) current psychotic symptoms; and 3) initiation of psychotropic medication within the past three months. Eligible and interested participants provided informed consent and were subsequently randomized to treatment condition (i.e., behavioral activation versus supportive counseling). Participants received 5 to 8 sessions of treatment. Those randomized to the behavioral activation treatment were taught to generate, schedule, and engage in values-congruent, substance-free activities in the attempt to increase positive reinforcement while those in the supportive counseling condition engaged in patient generated discussion of topics related to substance use and recovery while therapists provided unconditional support, reflective listening, and managed group dynamics. Neither treatment was designed to target distress tolerance. Detailed study recruitment, flow, screening, and randomization procedures are published elsewhere in addition to more detailed information regarding treatment conditions (Daughters et al., 2017).
Study assessments occurred at pretreatment (T1), discharge from treatment (T2), 3-months post-treatment (T3), 6-months post-treatment (T4), and 12-months post-treatment (T5). Standard tracking procedures were utilized to obtain all post-treatment assessments (e.g., participants provided detailed contact information at each assessment and received reminder calls from research personnel prior to appointments). All assessments consisted of interview, self-report, and computerized behavioral tasks. Upon completion of each assessment, participants were debriefed and compensated for study participation. All study-related procedures were approved by the Institutional Review Board.
Recruitment flow and retention rates for study assessments are presented in Supplementary Figure 1. Overall retention rates ranged from 82% to 95% [T2 = 95% (n = 251), T3 = 82% (n = 215), T4 = 83% (n = 218), T5 = 84% (n = 221)], with rates of obtained data for distress tolerance variables ranging from 73–99% (see Figure S1). The higher rate of missing data for the MTPC reflects logistical difficulties administering a computerized task outside of the treatment environment. Additionally, rates of obtained data regarding substance use variables are as follows: abstinence duration (90%; n = 237), and substance use frequency [percent days used; T1–2 = 255 (97%), T2–3 = 243 (92%), T3–4 = 231 (88%), T4–5 = 224 (85%)].
Measures
Substance Use Diagnoses.
Past year substance dependence was assessed using the alcohol and substance use modules of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; First, Spitzer, Gibbon & Williams, 1994). This assessment was administered in a structured interview format by trained research staff. Diagnoses were used in the current study to characterize the sample and provide descriptive information concerning the range of substance use problems.
Secondary Covariates.
Several covariates that were not central to our research question were assessed in the present study. These include variables that are reported to be associated with single-time point estimates of DT including anxiety and depressive symptoms (Ali, Seitz-Brown & Daughters, 2015; Gorka, Ali & Daughters, 2012; Keough, Riccardi, Timpano, Mitchell & Schmidt, 2010), age (Gorka, Ali & Daughters, 2012) and gender (Ali, Seitz-Brown & Daughters, 2015). We additionally tested variables that may be related to the interpretation of our secondary research aim of testing the effect of substance use on the DT trajectory, including frequency of substance use in the year prior to study entry, and treatment condition1. Participant age and gender were obtained by research personnel during screening procedures. Participants additionally completed the Beck Anxiety Inventory (BAI; Beck et al., 1988) and the Beck Depression Inventory (BDI; Beck, Steer, & Brown, 1996) at pre-treatment. These 21-item measures were used to evaluate current anxiety and depressive symptoms respectively. Finally, participants rated past year frequency of use across 11 drug classes on a Likert scale ranging from 0 (i.e., Never) to 4 (i.e., 4 or more times per week).
Distress Tolerance.
Behavioral DT was assessed using the Computerized Mirror Tracing Persistence Task (MTPT-C; Strong et al., 2003), which has been widely used to measure distress tolerance among substance using populations (e.g., Bornovaolva et al., 2012; Daughters et al., 2005, Daughters et al., 2008). During this task, participants are instructed to trace a red dot along the outline of a star shape using a computer mouse that is programmed to move the dot in the opposite direction. To increase distress, aversive auditory feedback (i.e., buzzer sound) is presented during errors (i.e., moving the mouse outside of the star boundary, moving mouse too slowly), and the participant must start from the beginning. The task includes four levels of increasing difficulty, which is titrated based on participant skill level. Difficulty on the final phase of the task is programmed to exceed participant skill level and thus buffer against potential practice effects. On this final phase, participants are given the option to end the task at any time by pressing a key on the computer keyboard. At the same time, participants are reminded that their performance on this final phase dictates the magnitude of the “bonus” payment they receive for study participation. All participants work independently on the task until voluntary task termination during the final phase or until the task self-terminates at the maximum 7-minute time limit. Behavioral DT was calculated as the latency (in minutes) to task termination on the final phase of the task.
Monetary compensation was provided at each assessment time point based on a randomized payment schedule determined at study entry, yet participants were told that payment was based on global performance on a group of computerized tasks as part of a larger study battery. These instructions were purposely ambiguous in order to prevent participants from drawing the false conclusion that payment was dependent on latency to task termination. Participants were debriefed on study deception following the final study assessment. Test-retest reliability in the current study was good (ICC = .83, 95% CI = .77-.87).
Perceived DT was assessed using the Distress Tolerance Scale (DTS; Simons & Gaher, 2005), a 15-item self-report measure assessing beliefs about feelings of distress. Individuals rated their degree of agreement with a series of statements using a 1–5 Likert scale with 1 indicating strong agreement and 5 indicating strong disagreement with each statement. The DTS consists of items assessing the perceived ability to tolerate distress (e.g., “Feeling distress or upset is unbearable to me”), appraisal of distress (e.g., “My feelings of distress or being upset are not acceptable”), how much attention is absorbed by the distress (e.g., “My feelings of distress are so intense that they completely take over”), and effort expended to alleviate distress (e.g., “I’ll do anything to avoid feeling distressed or upset”). Items were averaged to yield a DTS mean score. The DTS demonstrated good internal consistency in the current study (α > .88 across all assessment time points), which is in line with previous studies (e.g., Hasan et al, 2015; Vujanovic et al., 2017). In addition, this measure demonstrated good test-retest reliability in the current study (ICC = .78, 95% CI = .72-.82).
Substance Use.
The Timeline Follow-Back (TLFB; Sobell, Maisto, Sobell, & Cooper, 1979) is an interviewer-administered measure assessing substance use in a calendar format. An interviewer guides participants through their recollection of day-by-day substance use in reverse order, beginning with the current assessment date and working backwards until the time of last assessment. This measure demonstrates high test-retest reliability, convergent and discriminant validity, and agreement with collateral reports of substance use and urinalyses (Sobell et al., 1996). Data acquired from the TLFB were used in the current study to determine (1) abstinence duration, defined as the number of weeks from pre-treatment assessment until first substance use and (2) frequency of substance use, defined as the percentage of days on which a patient used substances during intervals between assessments. Regarding abstinence duration, participants who were lost due to attrition prior to first documented use (n = 26) were coded as missing for this variable. For individuals who remained abstinent throughout the study period, abstinence duration was coded as the time elapsed between pre-treatment (T1) and 12-month post-treatment (T5) assessments.
Statistical Analysis
Latent curve modeling (LCM) was used to test the primary aim, namely the latent trajectory of both perceived and behavioral DT. LCM is a useful analytic tool for determining growth trajectories using large data sets with partially missing data that provides higher levels of statistical power than are available with traditional longitudinal analytic methods (e.g., repeated measures analysis of variance; Curran, Obeidat, & Losardo, 2010). This is due to the utilization of maximum likelihood estimation which accounts for missing data by utilizing available data to generate maximum likelihood estimates and weighing individuals with a greater number of repeated observations more heavily than those who have fewer observations. This approach is considered equally as favorable, if not more so, than other missing-data techniques within structural equation modeling (e.g., multiple imputation; see Allison, 2003 for review). In addition, LCM can accommodate unequal spacing between time points and allow for the inclusion of both time-invariant and time-varying predictors of latent trajectories (Bollen & Curran, 2006). The LCM framework typically includes intercept and slope factors (collectively called growth factors), whose means define the estimated average trajectory of a sample outcome. Variability in these growth factors can also be examined to understand individual differences in the shape of change over time.
The analysis proceeded in several stages. First, we performed preliminary analyses to characterize the sample, identify violations of normality, assess missingness, and visualize patterns of change in the data. Additionally, because the DTS is a multi-item measure consisting of multiple subscales, longitudinal measurement invariance was evaluated for this measure to verify that subscales of the DTS represent the same latent constructs across all time points (Horn & McArdle, 1992). However, it was not necessary to evaluate measurement invariance for behavioral DT, as the measure used was persistence time, a “one-item” behavioral variable. See supplemental materials for results of this analysis.
Next, perceived and behavioral DT estimates collected at five assessment time points occurring from pre-treatment (T1) to 12-months post-treatment (T5) were entered into separate latent growth models. To determine the functional form of change in DT, a series of nested LCMs were fit to the data for both perceived and behavioral DT. First, we tested an intercept-only model that implied no change in DT in the sample over the study timeframe. Second, a linear slope factor was added to the model to allow for linear change in the outcome over the follow-up period. Factor loadings for this model were set to 0, 1, 4, 7, and 13 to reflect accurate temporal spacing (in months) between assessments. This linear slope model was compared to the intercept-only model using a likelihood ratio test (i.e., chi-square difference), and the slope factor was retained if significant improvement was observed in model fit. Finally, a freed loading slope factor was tested, which allows for non-linear growth in the outcome across study waves (Bollen & Curran, 2006). Specifically, the loadings of the observed indicators on this slope factor are fixed to 0 and 1 for the first and last waves (i.e., T1 and T5 respectively), and freely estimated for all other measurement occasions (i.e., T2, T3, and T4). The freed loading model provides a flexible way to test for non-linear growth while conserving parsimony by estimating fewer factors than more traditional non-linear models (e.g., quadratic latent curve models; Bollen & Curran, 2006). As above, the freed loading slope factor was retained if results of a chi-square difference test indicated that including such a factor significantly improved model fit when compared to the linear slope model.
Once the functional form of change was ascertained for perceived and behavioral DT, a final model was tested constraining time-specific residual variances of the DT indicators to equality over time in an effort to maximize model parsimony. If this restricted model did not result in significant decrement in model fit, it was retained and interpreted as the final model of DT change. However, if equality constraints resulted in significantly poorer fit, residual variance terms were freely estimated at all measurement time points. All models were compared with respect to chi-square goodness of fit, the comparative fit index (CFI; Bentler, 1990), the Tucker-Lewis Index (TLI; Tucker & Lewis, 1973), the root-mean square error of approximation (RMSEA; Browne & Cudeck, 1993), and standardized root-mean-square residual (SRMR; Bentler, 1995). Acceptable fit was determined based on recommended guidelines (Hu & Bentler, 1999). After determining final unconditional latent growth models for both behavioral and perceived DT, secondary covariates were tested for their influence on the latent trajectory of perceived and behavioral DT using a series of conditional latent growth models. All covariates were tested systematically for their association with DT latent factors and were retained in the conditional model of DT if they were significantly related to either DT intercept or slope factors.
Finally, we examined the effect of substance use on both the behavioral and perceived DT trajectories using two separate conditional LCMs that included secondary covariates significantly related to DT latent growth factors. The first conditional model assessed the association between DT growth factors and abstinence duration, which served as a time-invariant covariate in the analysis. This allowed us to test whether DT improvement would be greater for individuals who stayed abstinent for a longer period of time. A second model was used to investigate the impact of a time-varying covariate, frequency of use between each assessment time point, on time-specific fluctuations in DT. Utilizing this variable not only allowed us to quantify amount of substance use but also optimized statistical power when compared to binary measurement approaches of use historically used in treatment outcome research (Fitzmaurice, Lipsitz, & Weiss, 2017). Specifically, we regressed the observed DT variables at each post-treatment wave (i.e., T2-T5) on a wave-specific covariate that represented frequency of use within the interval since the last assessment (i.e., the percentage of days on which substance use occurred during the intervals between T1–2, T2–3, T3–4, and T4–5). Thus, for instance, the observed DT indicator at 3-months post-treatment (T3) was regressed on a covariate reflecting the frequency of substance use for the period between residential discharge (i.e., T2) and 3-months post-treatment (T3). All paths for the effect of the time-varying covariate on DT at contiguous assessment waves were allowed to correlate over time, to account for the continuity in substance use across assessment waves.
Results
Preliminary Analyses
Descriptive statistics of all relevant study variables, including secondary covariates, substance use variables, and DT repeated measures are reported in Supplementary Table 1 (S1). Bivariate correlations between repeated measures of behavioral and perceived DT and substance use variables are presented in Supplementary Table 2 (S2). Self-reported DT at contiguous assessment waves was moderately correlated (median r = .41), with a similar stability estimate for behavioral DT (median r = .46). Contemporaneous associations between behavioral and self-reported DT were generally weak (median r = .10). Correlations between abstinence duration (a time-invariant covariate) and both perceived and behavioral DT were generally weak (median r = .09) as were associations between time-point-specific estimates of frequency of use and behavioral and perceived DT (median r = .06).
Inspection of descriptive statistics and normality plots revealed negative skew for behavioral, but not perceived, DT indicating that a high percentage of participants persisted without quitting on the final phase of the MTPT-C at each time point (T1 = 33.1%, T2 = 42.2%, T3 = 30.4%, T4 = 39.5%, T5 = 37.3%). The Kolmogorov-Smirnov (KS) test of normality was used to investigate distributions of all repeated measures of MTPT-C. Results of this test indicate significant deviation from normality at each time point (KST1 = .19, KST2 = .30, KST3 = .25, KST4 = .31, KST5 = .31). Thus, a robust maximum likelihood estimator was used to estimate the change trajectory of behavioral DT to account for non-normality observed in the data (Muthén & Muthén, 2010).
Unconditional Models of Perceived and Behavioral DT
Model comparison.
Concerning perceived DT, an intercept-only model was first tested and showed poor fit to the data, χ2(13) = 45.53, p < .001; CFI = .89; TLI = .92; RMSEA = .10; SRMR = .14. Next, a linear growth model was tested and demonstrated significantly improved, Δχ2(3) = 18.41, p < .001, but not optimal fit, χ2(10) = 27.12, p = .003; CFI = .94; TLI = .94; RMSEA = .08; SRMR = .10. To test for a non-linear growth trajectory, a freed loading latent growth model was fit to the data, and it demonstrated significant improvement over the linear growth model, Δχ2(3) = 9.65, p = .02, and good model fit overall, χ2(7) = 17.47, p = .01; CFI = .97; TLI = .95; RMSEA = .08; SRMR = .09. Finally, we tested a freed factor loading model with equality constraints imposed on time specific residuals, but this model produced a significant decrement in fit, Δχ2(4) = 9.72, p = .045. Thus, we retained the freed loading model with freely estimated residual variances as the final perceived DT model.
The same sequence of model comparisons was conducted for behavioral DT using a robust maximum likelihood estimator to account for non-normality in the data. The intercept-only model showed poor fit to the data χ2(13) = 68.53, p < .001; CFI = .77; TLI = .82; RMSEA = .13; SRMR = .12. The linear growth model demonstrated significantly improved (Satorra-Bentler Scaled Δχ2(3) = 35.61, p < .001), but not optimal fit to the data, χ2(10) = 32.99, p < .001; CFI = .90; TLI = .90; RMSEA = .09; SRMR = .07. Thus, the freed loading model was tested and led to a significant improvement on the linear LCM, Satorra-Bentler Scaled Δχ2(3) = 17.28, p < .001, and good fit to the data overall, χ2(7) = 15.37, p = .03; CFI = .97; TLI = .95; RMSEA = .07; SRMR = .05. Constraining the observed indicator residual variances to equality significantly degraded model fit, Satorra-Bentler Scaled Δχ2(4) = 13.25, p = .01, so this restriction was rejected, and the freed loading model with freely estimated residuals was retained as the final behavioral DT model.
Parameter estimates.
Unstandardized factor loadings and parameter estimates from the final unconditional freed loading model of both perceived and behavioral DT are presented in Table 1. Factor loadings for the first (T1) and last (T5) assessment waves were set to 0 and 1, respectively, such that the growth factor slope mean reflected the total DT change over the 12-month study period. The freely estimated unstandardized loadings of the intervening waves (T2–4) can be interpreted as the proportion of change occurring between the time point of interest (e.g., T3) and the first time point (i.e., T1) relative to total change occurring between first and last time points (McArdle, 1988). As shown, more than half of the improvement in both perceived and behavioral DT occurred between pre-treatment (T1) and residential discharge (T2) assessments (51% and 55%, respectively). These coefficients suggest that there was significant positive change in perceived and behavioral DT during the time period when participants were enrolled in residential treatment.
Table 1.
Unstandardized factor loadings and parameter estimates from unconditional latent curve models of perceived and behavioral DT.
| Parameter | Perceived DT (DTS) | Behavioral DT (MTPT-C) |
|---|---|---|
| Factor Loadings: Slope | ||
| T1 | 0 (0) | 0 (0) |
| T2 | 0.51 (0.16)** | 0.55 (0.13)*** |
| T3 | 0.65 (0.17)*** | 0.78 (0.12)*** |
| T4 | 0.64 (0.20)** | 0.97 (0.09)*** |
| T5 | 1 (0) | 1 (0) |
| Mean | ||
| Intercept | 2.91 (0.06)*** | 3.79 (0.19)*** |
| Slope | 0.31 (0.07)*** | 0.81 (0.22)*** |
| Variance | ||
| Intercept | 0.48 (0.09)*** | 4.93 (1.09)*** |
| Slope | 0.25 (0.16) | 5.80 (1.65)*** |
| Intercept-Slope r | −0.52 (0.14)*** | −0.49 (0.13)*** |
Note: Standard errors are displayed in parentheses; DT = Distress Tolerance; DTS = Distress Tolerance Scale; MTPT-C = Mirror Tracing Persistence Task- Computerized Version; T1 = pre-treatment assessment; T2 = residential discharge assessment; T3 = 3-month follow-up assessment; T4 = 6-month follow-up assessment; T5 = 12-month follow-up assessment;
= p < .05,
= p < .01,
= p < .001
Regarding additional parameter estimates, slope factor means reflecting the expected change in DT from the first to final assessment waves (T1 to T5) indicate that both perceived and behavioral DT exhibit a significant propensity to increase nonlinearly over time. Cohen’s d effect sizes to gauge the degree of DT change were computed by estimating the difference in mean perceived and behavioral DT scores between the first and last time points and dividing this difference by the standard deviation of scores at the first time point. Similar improvements were observed for perceived (d = 0.36) and behavioral (d = 0.33) DT. Furthermore, significant variance in perceived and behavioral DT intercept factors indicate significant individual differences in DT at pre-treatment (T1). Significant variance in the behavioral, but not perceived, DT slope factor indicates significant inter-individual variability in behavioral DT change over follow up. Finally, significant negative correlations between both perceived and behavioral DT intercept and slope factors indicate greater DT improvement over time among individuals with low pre-treatment DT. Overall, these models explain 39–59% and 46–70% of the variance in time-specific measurements of perceived and behavioral DT, respectively.
Conditional Models of Perceived and Behavioral DT
Secondary Covariates.
Associations between secondary covariates and both perceived and behavioral DT latent factors can be found in Supplementary Table 3 (S3). As shown, gender, anxiety, and depressive symptoms were associated with perceived DT intercept, while gender and past year frequency of use were associated with the perceived DT slope factor. Treatment condition was not associated with either intercept or slope factor for perceived DT. Thus, gender, anxiety and depressive symptoms, and past year frequency of use were retained in the conditional model of perceived DT. Regarding behavioral DT, gender was the only variable associated with behavioral DT intercept. There were no significant associations between any covariate and behavioral DT slope factor. Thus, gender was the only variable retained in the conditional behavioral DT latent growth model2.
Abstinence duration.
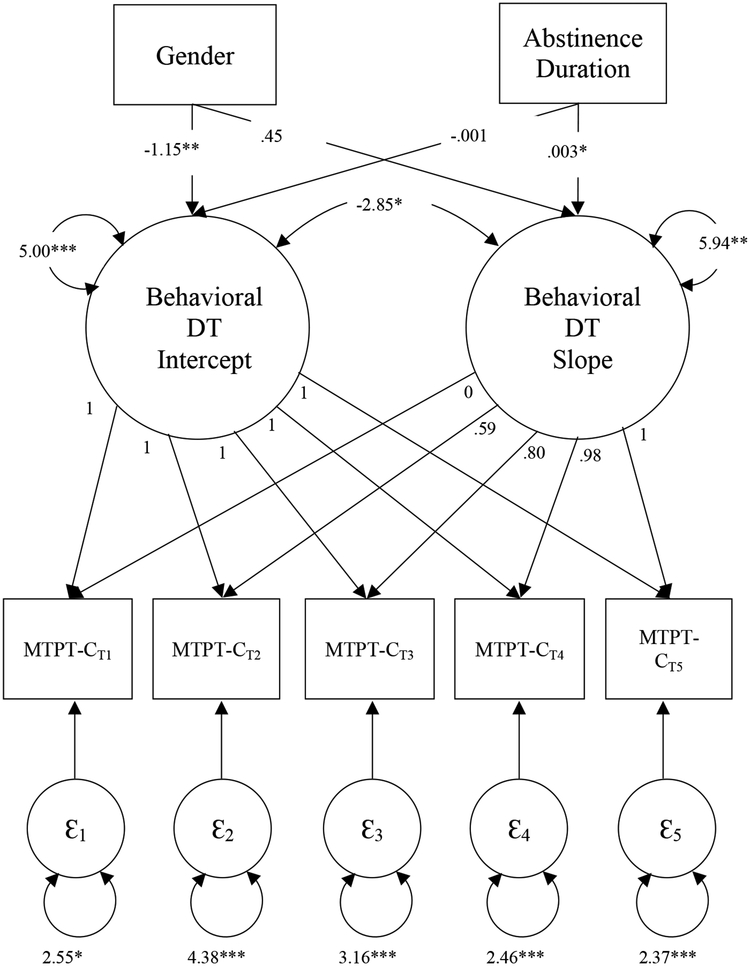
The conditional model estimating the association between abstinence duration and perceived DT trajectory with covariates of gender, depressive and anxiety symptoms, and past-year frequency of use included in the model demonstrated good fit to the data, χ2(22) = 36.54 p = .03; CFI = .96; TLI = .94; RMSEA = .05; SRMR = .06. Abstinence duration was not associated with the perceived DT intercept (b = 0.0001, SE = 0.001, p = .66 β = .04) or slope factor (b = 0.001, SE = 0.001, p = .10, β = .34). This model along with path estimates is displayed in Supplementary Figure 2. Regarding behavioral DT, the conditional model estimating the association between abstinence duration and the trajectory of behavioral DT when including gender as a covariate adequately fit the data, χ2(13) = 32.44, p = .002; CFI = .94; TLI = .90; RMSEA = .08; SRMR = .05. Results are displayed in Figure 1. As shown, abstinence duration was significantly and positively associated with the behavioral DT slope factor (b = .003, SE = .001, p = .03, β = .20) but not the intercept factor (b = −.002, SE = .001, p = .11, β = −.12) such that a longer duration of abstinence prior to first use was associated with greater increases in behavioral DT over time.
Figure 1.
Path diagram depicting the conditional latent growth model testing the association of abstinence duration and behavioral DT latent factors while including gender as an added covariates.
Note: MTPT-C = Mirror Tracing Persistence Task – Computerized Version; T1 = pre-treatment assessment; T2 = residential discharge assessment; T3 = 3-month follow-up assessment; T4 = 6-month follow-up assessment; T5 = 12-month follow-up assessment; p < .05 = *, p < .01 = **, p < .001 = ***
Time-varying covariate: Frequency of use.
Finally, we tested a LCM with frequency of use serving as a time-varying covariate in the perceived DT model while including gender, depressive and anxiety symptoms, and past year frequency of use in the model. However, due to a negative residual variance estimate in the latent slope factor (b = −0.01, SE = .08, p = .90, β = −3.15), this model was not interpreted and was re-run while constraining the variance of the slope factor to be 0. This model adequately fit the data, χ2(37) = 59.47, p = .01; CFI = .94; TLI = .92; RMSEA = .05; SRMR = .05, and revealed that time-specific DTS scores (i.e., perceived DT) were not related to frequency of use reported since previous assessment (bs = −.40–1.00, SEs = .18-.96, ps = .20-.70; see Supplementary Figure 3 for full results).
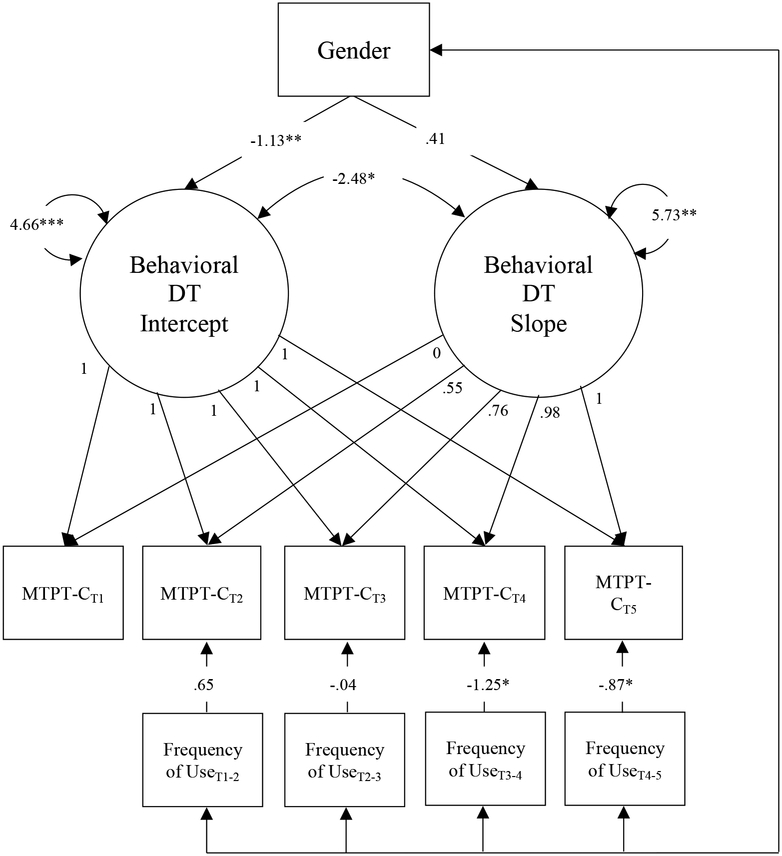
Analysis steps were next replicated using the behavioral DT model. The conditional LCM with frequency of use as a time-varying covariate and gender as a time-invariant covariate adequately fit the data χ2(26) = 62.57, p < .001; CFI = .90; TLI = .87; RMSEA = .07; SRMR = .05. Results revealed that higher frequency of use from the immediately prior assessment to the current assessment significantly predicted lower MTPT-C scores (i.e. lower behavioral DT) in the later phases of follow-up (T4: b = −1.25, SE = .57, p = .03, β = −.12; T5: b = −.87, SE = .43, p = .045, β = −.08), but not earlier phases (ps = .52 and .96 for T2 and T3; see Figure 2).
Figure 2.
Path diagram depicting the conditional latent growth model testing the influence of time-specific frequency of use on the behavioral DT trajectory including gender as a covariate.
Note: MTPT-C = Mirror Tracing Persistence Task – Computerized Version; T1 = pre-treatment assessment; T2 = residential discharge assessment; T3 = 3-month follow-up assessment; T4 = 6-month follow-up assessment; T5 = 12-month follow-up assessment; p < .05 = *, p < .01 = **, p < .001 = ***
Discussion
The current study tested the trajectory of distress tolerance among individuals seeking treatment for substance use over a series of five assessment waves from residential treatment entry to 12-months post-treatment. We additionally tested the relationship between DT change over time and two indicators of substance use: abstinence duration and frequency of substance use over follow-up. Previous findings suggest that DT represents a malleable treatment target, supported by the efficacy of novel DT-targeted treatment approaches in improving DT among diverse substance using populations (e.g., Bornovalova et al., 2012; Brown et al., 2014). The current study provides an important contribution to the current literature by providing evidence that individuals who use substances show improvement in both behavioral and perceived DT over a one-year period even in the absence of DT targeted-treatment. This finding not only provides missing information regarding the malleability of DT, but provides the foundational knowledge upon which to base future hypotheses concerning factors that may influence change in DT over time.
Relatedly, this study additionally identified two potential factors influencing the DT trajectory post-treatment: abstinence duration and frequency of use. As predicted, longer duration of abstinence prior to first use was associated with improvements in behavioral DT, a finding consistent with previous literature highlighting the importance of sustained abstinence for the recovery of cognitive and affective processes related to DT and related neurobiological structure and function (Fox et al., 2007; Garavan, Brennan, Hester, & Whelan, 2013; Schmidt, Pennington, Cardoos, Durazzo, & Meyerhoff, 2017; Wang et al., 2012). In addition, we found that greater post-treatment frequency of use was associated with poorer behavioral DT at the subsequent assessment, but only in the advanced phases of follow-up. That is, participants who used more frequently after 3 months exhibited unfavorable deflections in DT trajectory at 6 months, and an analogous pattern was evident for the span between 6- and 12-month follow-up waves. However, there was no evidence to suggest that regularity of use immediately post-treatment was related to behavioral DT performance at the 3-month follow-up. One potential explanation for this pattern of findings could be limited variance in substance use in the early phases of the study. Specifically, the number of individuals using substances increased substantially over the course of the study (e.g., 2.28% of participants used between pre-treatment and residential discharge as compared to 49.81% between 6- and 12-month follow-up).
Although the strength of association varied across follow-up from small to moderate, the general finding is that substance use frequency may negatively impact future behavioral DT. This can be viewed in the context of a cycle of use described by the negative reinforcement theory, wherein substance use occurring in response to negative affect in turn increases subsequent levels of negative affect (Baker et al., 2004). The current findings add to this by suggesting that substance use may additionally reduce an individual’s ability to tolerate future distress. This finding is consistent with research showing that prior heavy use predicts future avoidance behavior and decreased problem solving (Weiss, Bold, Sullivan, Armeli, & Tennen, 2017), and can guide efforts to manage post-treatment relapse. For example, when individuals experience a lapse, it may be important to bolster their distress tolerance, so that the cycle of use is interrupted. Indeed, intervening after the first instance of a lapse could limit how frequently the substance is used, thus lowering the extent to which DT is compromised. Additionally, current findings provide preliminary evidence to support the strategy of “delaying” use when an urge arises, in order to increase abstinence duration and thus allow time for DT to be restored.
Contrary to hypotheses, we did not find a relationship between either abstinence duration or frequency of substance use on perceived DT change over time. Theoretical perspectives posit that those who use substances not only evidence impairments in cognitive and behavioral functioning, but additionally lack insight and self-awareness as a by-product of substance use (Goldstein et al., 2009). Thus, it may be that individuals who used substances were not accurate reporters of current symptoms, particularly when providing self-directed evaluations of DT. Another possibility may be existing method variance when testing the relationship between DT and various outcomes. Previous work has demonstrated that self-report measures of DT are often related to one another as are behavioral measures, yet self-report and behavioral indices are typically weakly associated with one another (McHugh et al., 2011; Glassman et al., 2016). In addition, perceived DT has more often been associated with self-reported substance use problems and symptom measures (Ali et al., 2013; Burjarski et al., 2012; Howell et al., 2010; Zvolensky et al., 2009) whereas behavioral DT has been consistently related to reports of substance use behavior (Brandon et al., 2003; Brown, Lejuez, Kahler, & Strong, 2002; Cameron, Reed, & Ninnemann, 2013; Daughters et al., 2005a; Daughters et al., 2005b; Strong et al., 2012). Another possibility is that differing operationalizations of DT capture separable aspects of the DT construct that are in turn differentially related to substance use-related phenomena (Zvolensky et al., 2010; Glassman et al., 2016). Taken together, it will be important for future studies to disentangle these possibilities in order to identify factors that impact perceived DT change over time and the way in which this change relates to clinical outcomes.
Though findings from this study are both novel and important, methodological limitations should be considered. One such limitation is the interpretation of the relationship between abstinence duration and DT change. Traditional LCM approaches define time-invariant covariates as factors which remain stable over time (e.g., gender; Bollen & Curran, 2006). In the present study, abstinence duration was a variable that evolved over the course of the study and was not measurable at the initial assessment wave. As such, the temporal precedence of this variable could not be established, and thus our interpretation of the predictive or causal relationship between abstinence duration and DT change is limited.
In addition, it is important to note the variable spacing between assessment time points which ranged from one month between treatment entry and discharge to 6 months between the 6- and 12-month follow-up assessments. Though this spacing is common among substance use treatment efficacy studies (e.g., Bowen et al., 2014), it is possible that we were unable to capture subtler, nuanced fluctuations in DT over the course of the study. Additionally, it may be that substance use has a more immediate effect on DT than could be determined due to large time intervals between assessments. This may be particularly important when considering the relationship between substance use frequency and DT, as we did not find evidence for a relationship between behavioral DT and substance use early in the follow-up period or at all for perceived DT in the current study. Thus, future studies assessing DT and substance use at more frequent intervals post-treatment may be needed to disentangle temporal relationships between substance use and DT change.
Despite these limitations, this study extends previous research that mainly focuses on DT as a protective factor against subsequent use, by modeling the improvement in DT post-treatment, and by suggesting that behavioral DT may in turn be influenced by substance use. The study is strengthened by the use of data spanning one year that can demonstrate change in DT over time, and capture the effect of substance use on this trajectory. By identifying the latent trajectory of DT within a treatment-seeking population, this study not only provides evidence for the malleability of both perceived and behavioral DT but additionally offers the foundational work upon which future hypotheses can be tested regarding individual differences in DT change and the importance of this change in predicting future behavior. What is more, by testing the effects of substance use on the DT trajectory, we have provided clinically relevant information regarding when in the course of treatment maximal DT change can be expected and where in this time course substance use has the greatest influence on this change. Additionally, the use of latent growth modeling is a sophisticated technique that computes growth parameters while flexibly handling missing DT data using maximum likelihood estimation. Finally, the study focuses on a predominantly African American, residential treatment-seeking, low income sample, who represent an understudied population.
Future Directions
Findings from the current study set the stage for future investigations of DT change among individuals who use substances. First, it remains unknown the extent to which DT improvements may be evident among more racially diverse populations and in other SUD treatment settings (e.g., outpatient care). Relatedly, the rate of DT change was best characterized as non-linear, with more than half of the total increase in both perceived and behavioral DT occurring while participants were in the restricted environment of residential treatment (i.e., between treatment entry and residential treatment discharge). We then observed fluctuations in the rate of DT improvement among individuals in residential treatment after treatment discharge, when environmental factors between participants were no longer held constant. Though we examined two factors that influenced this change, namely abstinence duration and frequency of use, future studies may wish to directly examine other factors that might affect DT change. This is important given that the effect size of substance use variables on behavioral DT slope were small to moderate, suggesting that there are likely other factors at play that influence the DT trajectory during this time. Those that will be important to consider may be environmental factors known to influence the course of recovery post-treatment including housing and financial stability, employment, and social networks (Davies, Elison, Ward, & Laudet, 2015; Sinha, 2007; Walton, Blow, Bingham, & Chermack, 2003; Worley, Witkiewitz, Brown, Kivlahan, & Longabaugh, 2015). Such factors represent chronic stressors which are known to induce functional and architectural changes in neural regions associated with cognition and emotion regulation (Arnsten, 2015). As these biologically-based processes are necessary for successful DT, it is likely important to account for additional influences on these processes, such as environmental factors when evaluating distress tolerance improvement. Additionally, drug classes vary in the patterns of neurobiological recovery during prolonged abstinence following treatment. For example, there is more consistent evidence of cognitive recovery when abstaining from alcohol use, compared to cannabis use (Schulte et al., 2014). Therefore, it is important to examine whether the type of drug used influences the effect of substance use on DT trajectory.
Further, we demonstrated that DT has a significant propensity to change over time, the majority of which occurred while participants were in residential treatment. Though this effect was small to moderate in magnitude, change was observed in both behavioral and perceived DT without targeted intervention. Thus, in order to synthesize findings from DT-targeted treatment studies and current findings, it will be important to directly compare DT improvement longitudinally as a function of DT-specific intervention with improvements observed as a function of standard care, as demonstrated in the current study. This line of inquiry would provide information as to whether DT-targeted intervention accelerates DT improvement above and beyond what is seen with non-targeted treatment, and whether such improvements are sustained post-intervention.
Having uncovered evidence for the effect of substance use on subsequent DT, an important next step is to examine the bi-directional effects between substance use and DT within the same model to test existing theories of DT and substance use. Such bidirectional effects would support the role of DT in promoting a cycle of use (i.e., a spiraling distress and addiction cycle; Koob & LeMoal, 1997), which is characteristic of substance use disorders. Future research may then identify the mechanisms by which substance use reduces behavioral DT. Indeed, as previously reviewed, DT may be linked to processes such as inhibitory control and emotional regulation (Daughters et al., 2016). Such processes in turn are found to deteriorate following substance use (Grant & Chamberlain, 2014; Vonmoos et al., 2014), and may therefore lead to lower DT. Clarifying such mechanisms could in turn help develop targeted treatments aimed at bolstering DT to limit relapse.
Conclusion
In sum, the current study provides evidence for improvement in both perceived and behavioral distress tolerance among individuals in residential substance use treatment, and identifies two factors - abstinence duration and substance use frequency - which may attenuate this improvement for behavioral DT specifically. Such findings suggest the importance of relapse prevention and early intervention on post-treatment substance use as important steps that may aid in the improvement of DT over time and thus lead to substance use recovery. As such, this study provides a nuanced view of the relationship between DT and substance use, while emphasizing the need for further investigation concerning the longitudinal course of DT in this population. It will be important for such studies to rigorously evaluate not only pre-treatment DT, but DT improvement, as a key factor contributing to substance use treatment success.
Supplementary Material
Public Health Significance Statement:
The current study identifies distress tolerance as an important treatment target that shows improvement over time among individuals who use alcohol and illicit substances, particularly with prolonged abstinence. This result underlines the importance of attending to distress tolerance over the course of substance use treatment.
Appendix A
Table A1.
Description of previously published studies from the current data
| This manuscript includes analyses of data collected as part of a larger Randomized Clinical Trial. The results of this parent RCT (Manuscript 1: Daughters et al., 2017) compared depressive symptoms, substance use consequences, and abstinence over a one-year follow-up period among individuals who use substances randomized to two treatment conditions: behavioral activation treatment for substance use and supportive counseling. A second manuscript (Manuscript 2: Anand, Chen, Lindquist, & Daughters, 2017) examining the relationship between affect intensity and emotion differentiation in predicting relapse risk within the year following substance use treatment has also been published using this data. The current manuscript (Manuscript 3) sought to characterize the longitudinal trajectory of both perceived and behavioral distress tolerance among residential-treatment seeking individuals by examining repeated task-based and self-report measures of distress tolerance administered from pre-treatment to 1-year post-treatment. In addition, we examined the relationship between this longitudinal trajectory and substance use, including both frequency of post-treatment use and abstinence duration following inpatient treatment. Distress tolerance is not examined in either previous work (Manuscript 1 or 2). Frequency of use is used as a secondary outcome variable in Manuscript 1 and abstinence duration is examined as a primary outcome variable in Manuscript 2. |
Footnotes
This research was supported by R01 DA026424. Trial Registration at Clinicaltrials.gov Identifier: NCT01189552 and National Science Foundation Graduate Research Fellowship DGE-1650116
Effects of treatment condition were additionally tested in substance use variables including abstinence duration and time point specific estimates of frequency of use. Treatment condition was not related to abstinence duration, t (235) = .87, p = .39, or frequency of use at any time point. T1–2: χ2(5) = 4.60, p = .47; T2–3: χ2(115) = 113.91, p = .51; T3–4: χ2(108) = 112.77, p = .36; T4–5: χ2(119) = 118.56, p = .49.
We additionally tested the behavioral DT conditional models including the same secondary covariates (i.e., gender, anxiety and depressives symptoms, and past year frequency of use) used in the perceived DT model. When including these covariates, the significant association between abstinence duration behavioral DT slope factor remained (b = .003, SE = .001, p = .03, β = .20). In addition, frequency of use from T3–4 remained significantly predictive of behavioral DT at T4 (b = -1.20, SE = .56, p = .03) while the effect of frequency of use from T4–5 on DT at T5 became slightly weaker (b = -.80, SE = .43, p = .06).
References
- Ali B, Ryan JS, Beck KH, & Daughters SB (2013). Trait aggression and problematic alcohol use among college students: the moderating effect of distress tolerance. Alcoholism: clinical and experimental research, 37(12), 2138–2144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali B, Seitz-Brown CJ, & Daughters SB (2015). The interacting effect of depressive symptoms, gender, and distress tolerance on substance use problems among residential treatment-seeking substance users. Drug and alcohol dependence, 148, 21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison PD (2003). Missing data techniques for structural equation modeling. Journal of abnormal psychology, 112(4), 545. [DOI] [PubMed] [Google Scholar]
- Arnsten AF (2015). Stress weakens prefrontal networks: molecular insults to higher cognition. Nature Neuroscience, 18(10), 1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction Motivation Reformulated: An affective processing model of negative reinforcement. Psychological Review, 111(1), 33–51. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, & Steer RA (1988). An inventory for measuring clinical anxiety: psychometric properties. Journal of consulting and clinical psychology, 56(6), 893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological bulletin, 107(2), 238. [DOI] [PubMed] [Google Scholar]
- Bentler PM, & Hu LT (1995). Evaluating model fit. Structural equation modeling: Concepts, Issues, and Applications, 76–99. [Google Scholar]
- Berking M, Margraf M, Ebert D, Wupperman P, Hofmann SG, & Junghanns K (2011). Deficits in emotion-regulation skills predict alcohol use during and after cognitive–behavioral therapy for alcohol dependence. Journal of Consulting and Clinical Psychology, 79(3), 307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA, & Curran PJ (2006). Latent curve models: A structural equation perspective (Vol. 467). John Wiley & Sons. [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Hunt ED, & Lejuez CW (2012). Initial RCT of a distress tolerance treatment for individuals with substance use disorders. Drug and Alcohol Dependence, 122(1–2), 70–76. doi: 10.1016/j.drugalcdep.2011.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, … & Larimer ME (2014). Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial. JAMA Psychiatry, 71(5), 547–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon TH, Herzog TA, Juliano LM, Irvin JE, Lazev AB, & Simmons VN (2003). Pretreatment task persistence predicts smoking cessation outcome. Journal of Abnormal Psychology, 112(3), 448–456. [DOI] [PubMed] [Google Scholar]
- Brown RA, Bloom EL, Hecht J, Moitra E, Herman DS, & Stein MD (2014). A pilot study of a distress tolerance treatment for opiate-dependent patients initiating buprenorphine: rationale, methodology, and outcomes. Behavior Modification, 38(5), 730–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, & Strong DR (2002). Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology, 111(1), 180–185. [PubMed] [Google Scholar]
- Browne MW, & Cudeck R (1993). Alternative ways of assessing model fit In Bollen KA & Long JS (Eds.), Testing Structural Equation Models, (pp. 126–162). Beverly Hills, CA: Sage. [Google Scholar]
- Bujarski SJ, Norberg MM, & Copeland J (2012). The association between distress tolerance and cannabis use-related problems: the mediating and moderating roles of coping motives and gender. Addictive Behaviors, 37(10), 1181–1184. [DOI] [PubMed] [Google Scholar]
- Cameron A, Reed KP, & Ninnemann A (2013). Reactivity to negative affect in smokers: The role of implicit associations and distress tolerance in smoking cessation. Addictive Behaviors, 38(12), 2905–2912. [DOI] [PubMed] [Google Scholar]
- Connolly CG, Bell RP, Foxe JJ, & Garavan H (2013). Dissociated grey matter changes with prolonged addiction and extended abstinence in cocaine users. PloS one, 8(3), e59645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ, Obeidat K, & Losardo D (2010). Twelve frequently asked questions about growth curve modeling. Journal of Cognition and Development, 11(2), 121–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Lejuez C, Kahler CW, Strong DR, & Brown RA (2005). Psychological distress tolerance and duration of most recent abstinence attempt among residential treatment-seeking substance abusers. Psychology of Addictive Behaviors, 19(2), 208. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Lejuez CW, Bornovalova MA, Kahler CW, Strong DR, & Brown RA (2005). Distress tolerance as a predictor of early treatment dropout in a residential substance abuse treatment facility. Journal of Abnormal Psychology, 114(4), 729–734. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Ross TJ, Bell RP, Yi JY, Ryan J, & Stein EA (2016). Distress tolerance among substance users is associated with functional connectivity between prefrontal regions during a distress tolerance task. Addiction Biology, 22(5), 1378–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Magidson JF, Anand D, Seitz‐Brown CJ, Chen Y, & Baker S (2017). The effect of a behavioral activation treatment for substance use on post-treatment abstinence: A Randomized Controlled Trial. Addiction, 113(3), 535–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Sargeant MN, Bornovalova MA, Gratz KL, & Lejuez CW (2008). The relationship between distress tolerance and antisocial personality disorder among male inner-city treatment seeking substance users. Journal of Personality Disorders, 22(5), 509–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies G, Elison S, Ward J, & Laudet A (2015). The role of lifestyle in perpetuating substance use disorder: the Lifestyle Balance Model. Substance Abuse Treatment, Prevention, and Policy, 10(1), 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimeff LA, & Linehan MM (2008). Dialectical behavior therapy for substance abusers. Addiction Science & Clinical Practice, 4(2), 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingle GA, Neves DDC, Alhadad SS, & Hides L (2017). Individual and interpersonal emotion regulation among adults with substance use disorders and matched controls. British Journal of Clinical Psychology, 57(2), 186–202. [DOI] [PubMed] [Google Scholar]
- Durazzo TC, Mon A, Gazdzinski S, Yeh PH, & Meyerhoff DJ (2015). Serial longitudinal magnetic resonance imaging data indicate non‐linear regional gray matter volume recovery in abstinent alcohol‐dependent individuals. Addiction biology, 20(5), 956–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW (1994). Structured clinical interview for DSM-IV patient edition (SCID-NP, Version 2.0) New York, NY: Biometrics Research Department. [Google Scholar]
- Fitzmaurice GM, Lipsitz SR, & Weiss RD (2017). Statistical considerations in the choice of endpoint for drug use disorder trials. Drug & Alcohol Dependence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox H, Axelrod S, Paliwal P, Sleeper J, & Sinha R (2007). Difficulties in emotion regulation and impulse control during cocaine abstinence. Drug and Alcohol Dependence, 89(2), 298–301. [DOI] [PubMed] [Google Scholar]
- Garavan H, Brennan K, Hester R, & Whelan R (2013). The neurobiology of successful abstinence. Current Opinion in Neurobiology, 23(4), 668–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RZ, Bechara A, Garavan H, Childress AR, Paulus MP, & Volkow ND (2009). The neurocircuitry of impaired insight in drug addiction. Trends in Cognitive Sciences, 13(9), 372–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorka SM, Ali B, & Daughters SB (2012). The role of distress tolerance in the relationship between depressive symptoms and problematic alcohol use. Psychology of Addictive Behaviors, 26(3), 621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graaf RD, Bijl RV, Smit F, Ravelli A, & Vollebergh WA (2000). Psychiatric and sociodemographic predictors of attrition in a longitudinal study The Netherlands Mental Health Survey and Incidence Study (NEMESIS). American Journal of Epidemiology, 152(11), 1039–1047. [DOI] [PubMed] [Google Scholar]
- Grant JE, & Chamberlain SR (2014). Impulsive action and impulsive choice across substance and behavioral addictions: cause or consequence? Addictive behaviors, 39(11), 1632–1639. [DOI] [PubMed] [Google Scholar]
- Hasan NS, Babson KA, Banducci AN, & Bonn-Miller MO (2015). The prospective effects of perceived and laboratory indices of distress tolerance on cannabis use following a self-guided quit attempt. Psychology of Addictive Behaviors, 29(4), 933. [DOI] [PubMed] [Google Scholar]
- Horn JL, & McArdle JJ (1992). A practical and theoretical guide to measurement invariance in aging research. Experimental Aging Research, 18(3–4), 117–144. [DOI] [PubMed] [Google Scholar]
- Howell AN, Leyro TM, Hogan J, Buckner JD, & Zvolensky MJ (2010). Anxiety sensitivity, distress tolerance, and discomfort intolerance in relation to coping and conformity motives for alcohol use and alcohol use problems among young adult drinkers. Addictive Behaviors, 35(12), 1144–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu SH, Collins SE, & Marlatt GA (2013). Examining psychometric properties of distress tolerance and its moderation of mindfulness-based relapse prevention effects on alcohol and other drug use outcomes. Addictive behaviors, 38(3), 1852–1858. [DOI] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Keough ME, Riccardi CJ, Timpano KR, Mitchell MA, & Schmidt NB (2010). Anxiety symptomatology: The association with distress tolerance and anxiety sensitivity. Behavior Therapy, 41(4), 567–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, & Le Moal M (1997). Drug abuse: hedonic homeostatic dysregulation. Science, 278(5335), 52–58. [DOI] [PubMed] [Google Scholar]
- Littlefield AK, Stevens AK, Cunningham S, Jones RE, King KM, Schumacher JA, & Coffey SF (2015). Stability and change in multi-method measures of impulsivity across residential addictions treatment. Addictive Behaviors, 42, 126–129. [DOI] [PubMed] [Google Scholar]
- Lookatch SJ, Elledge LC, Anderson S, Shorey RC, Stuart GL, & Moore TM (2017). Cognitive and psychological changes during 28-day residential substance use treatment. Addiction Research & Theory, 25(4), 334–341. [Google Scholar]
- McArdle JJ (1988). Dynamic but structural equation modeling of repeated measures data In Handbook of multivariate experimental psychology (pp. 561–614). Springer; US. [Google Scholar]
- McLellan AT, Lewis DC, O’brien CP, & Kleber HD (2000). Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA, 284(13), 1689–1695. [DOI] [PubMed] [Google Scholar]
- Muthen LK, & Muthén BO (2010). Mplus user’s guide, v. 6.1. Los Angeles, CA: Muthen and Muthen, UCLA. [Google Scholar]
- National Institute on Drug Abuse, (2012). Prinicples of drug addition treatment: A Research-based guide (3rd ed.). NIH Publication No. 12–4180. Rockville, MD: National Institute on Drug Abuse. [Google Scholar]
- Perkins KA, Giedgowd GE, Karelitz JL, Conklin CA, & Lerman C (2012). Smoking in response to negative mood in men versus women as a function of distress tolerance. Nicotine & Tobacco Research, 14(12), 1418–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt A, Borgwardt S, Gerber H, Wiesbeck GA, Schmid O, Riecher-Rössler A, … & Walter M (2014). Acute effects of heroin on negative emotional processing: relation of amygdala activity and stress-related responses. Biological Psychiatry, 76(4), 289–296. [DOI] [PubMed] [Google Scholar]
- Schmidt TP, Pennington DL, Cardoos SL, Durazzo TC, & Meyerhoff DJ (2017). Neurocognition and inhibitory control in polysubstance use disorders: Comparison with alcohol use disorders and changes with abstinence. Journal of Clinical and Experimental Neuropsychology, 39(1), 22–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte MH, Cousijn J, den Uyl TE, Goudriaan AE, van den Brink W, Veltman DJ, … & Wiers RW (2014). Recovery of neurocognitive functions following sustained abstinence after substance dependence and implications for treatment. Clinical Psychology Review, 34(7), 531–550. [DOI] [PubMed] [Google Scholar]
- Schrimsher GW, & Parker JD (2008). Changes in cognitive function during substance use disorder treatment. Journal of Psychopathology and Behavioral Assessment, 30(2), 146–153. [Google Scholar]
- Seo D, & Sinha R (2015). Neuroplasticity and predictors of alcohol recovery. Alcohol research: current reviews, 37(1), 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, & Gaher RM (2005). The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion, 29(2), 83–102. [Google Scholar]
- Sinha R (2007). The role of stress in addiction relapse. Current Psychiatry Reports, 9(5), 388–395. [DOI] [PubMed] [Google Scholar]
- Snyder HR, Miyake A, & Hankin BL (2015). Advancing understanding of executive function impairments and psychopathology: bridging the gap between clinical and cognitive approaches. Frontiers in Psychology, 6, 328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, & Cooper AM (1979). Reliability of alcohol abusers’ self reports of drinking behavior. Behaviour Research & Therapy, 17(2), 157–160. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Buchan G, Cleland PA, Fedoroff I, Leo GI (1996). The reliability of the Timeline Followback method applied to drug, cigarette, and cannabis use. Presented at the 30th Annual Meeting of the Association for Advancement of Behavior Therapy New York, NY. [Google Scholar]
- Strong DR, Brown RA, Sims M, Herman DS, Anderson BJ, & Stein MD (2012). Persistence on a Stress-challenge Task Before Initiating Buprenorphine Treatment Was Associated With Successful Transition From Opioid Use to Early Abstinence. Journal of Addiction Medicine, 6(3), 219–225. doi: 10.1097/ADM.0b013e31825d927f [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong DR, Lejuez CW, Daughters S, Marinello M, Kahler CW, & Brown RA (2003). The computerized mirror tracing task, version 1. Unpublished manual.
- Substance Abuse Mental Health Services Administration (2014). Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. NSDUH Series H-48, HHS Publication No.(SMA) 14–4863. Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Tucker LR, & Lewis C (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38(1), 1–10. [Google Scholar]
- Verdejo-García A, & Pérez-García M (2007). Profile of executive deficits in cocaine and heroin polysubstance users: common and differential effects on separate executive components. Psychopharmacology, 190(4), 517–530. [DOI] [PubMed] [Google Scholar]
- Vonmoos M, Hulka LM, Preller KH, Minder F, Baumgartner MR, & Quednow BB (2014). Cognitive impairment in cocaine users is drug-induced but partially reversible: evidence from a longitudinal study. Neuropsychopharmacology, 39(9), 2200–2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujanovic AA, Meyer TD, Heads AM, Stotts AL, Villarreal YR, & Schmitz JM (2017). Cognitive-behavioral therapies for depression and substance use disorders: an overview of traditional, third-wave, and transdiagnostic approaches. The American Journal of Drug and Alcohol Abuse, 43(4), 402–415. [DOI] [PubMed] [Google Scholar]
- Wang X, Li B, Zhou X, Liao Y, Tang J, Liu T, … & Hao, W. (2012). Changes in brain gray matter in abstinent heroin addicts. Drug and Alcohol Dependence, 126(3), 304–308. [DOI] [PubMed] [Google Scholar]
- Walton MA, Blow FC, Bingham CR, & Chermack ST (2003). Individual and social/environmental predictors of alcohol and drug use 2 years following substance abuse treatment. Addictive Behaviors, 28(4), 627–642. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Bold KW, Sullivan TP, Armeli S, & Tennen H (2017). Testing bidirectional associations among emotion regulation strategies and substance use: a daily diary study. Addiction, 112(4), 695–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worley MJ, Witkiewitz K, Brown SA, Kivlahan DR, & Longabaugh R (2015). Social network moderators of naltrexone and behavioral treatment effects on heavy drinking in the COMBINE study. Alcoholism: Clinical and Experimental Research, 39(1), 93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou X, Durazzo TC, & Meyerhoff DJ (2018). Regional Brain Volume Changes in Alcohol‐Dependent Individuals During Short‐Term and Long‐Term Abstinence. Alcoholism: clinical and experimental research, 42(6), 1062–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Marshall EC, Johnson K, Hogan J, Bernstein A, & Bonn-Miller MO (2009). Relations between anxiety sensitivity, distress tolerance, and fear reactivity to bodily sensations to coping and conformity marijuana use motives among young adult marijuana users. Experimental and clinical psychopharmacology, 17(1), 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.