Abstract
There is considerable global variability in clinical practice regarding the prescription of airway clearance techniques (ACTs) for patients with acute exacerbations of chronic obstructive pulmonary disease (AECOPD). Little is known about the physical therapy practice, and no international guidelines are available. The aim of this survey was to identify current physical therapy practice regarding ACT prescription for patients with AECOPD in Sweden. A cross-sectional, descriptive study was conducted via a Web-based questionnaire, sent to all (n = 70) hospitals that offer physical therapy service for patients with AECOPD in Sweden. Responses were received from 117 physical therapists (76%) across all sites. ACTs were prescribed for more than half of all patients with an AECOPD by 75% of physical therapists. The most frequently used ACTs were positive expiratory pressure (PEP) devices (90%), directed huffing (88%) and cough (71%). Most physical therapists (89%) perceived sputum clearance to be an important aspect of the overall management of patients with AECOPD. The main factors influencing choice of ACT were the ‘degree of dyspnoea or work of breathing’ and ‘access to resources/equipment’. Physical therapists prescribe predominantly PEP-based ACTs for patients with AECOPD in Sweden. Several factors come into consideration that influences the choice of treatment technique.
Keywords: Airway clearance techniques, acute exacerbation, chronic obstructive pulmonary disease, healthcare surveys, mucociliary clearance, physical therapy modalities
Introduction
Chronic obstructive pulmonary disease (COPD) is a disease characterized by symptoms of breathlessness, chronic cough and sputum production.1 Chronic respiratory disease is the third leading cause of global death in the world and imposes a significant morbidity disease burden.2 Acute exacerbations of COPD (AECOPD) are common, clinically important events known to negatively affect lung function, physical capacity, quality of life and mortality.1,3 Increased sputum production is a common feature of AECOPDs that frequently warrant initiation of early therapy to reduce its impact upon clinical outcomes.4,5 Prescription of mucolytic and/or mucoactive agents may target reductions in sputum viscosity and/or rheology, while non-pharmacological therapies such as airway clearance techniques (ACTs) utilize externally applied forces and manipulation of lung volumes, pulmonary pressures and gas flow to shear sputum along the inner surface of the airway lumen towards the mouth6 where it can be cleared.
Specific recommendations in international guidelines regarding ACTs for patients with AECOPD are not common.3 This is likely due to the limited evidence of clinical benefit that has been previously reported.7 Many different types of ACTs exist such as breathing exercises, positioning and use of adjunct devices such as positive expiratory pressure (PEP) therapy or mechanical chest wall oscillation.8 Choice of technique is most commonly determined by respiratory physical therapists in close consideration of patients’ individual needs. The lack of standardized recommendations in this field has certainly contributed to the well-documented variability of treatment regimens within and between countries.9–11 Differences in awareness of the evidence regarding ACTs for patients with AECOPD exist in clinical practice, and rates of ACT prescription by physical therapists have been related to factors such as years of clinical experience.11
The influences underpinning practice variability are not always overt.12,13 For example, previous studies report the most commonly prescribed ACTs by physical therapists from United Kingdom (UK), Canada and Australia, where healthcare systems are similar, were the active cycle of breathing technique (ACBT)9, postural drainage, percussion and vibration10 and physical exercise11, respectively. It is difficult to determine how reflective these findings are of current clinical practice as the studies were conducted more than a decade ago, rendering it possible for practice to have changed since then. Identifying nuances related to local practice clearly warrants examination specific to that local context. Physical therapists in Sweden are integral members of the healthcare team responsible for the management of patients with AECOPD, and airway clearance therapy has formed a large part of physical therapists’ role. The extent to which physical therapy practice in Sweden may differ from other regions of the world has not yet been examined. Such data would be useful to clarify existing motives for the choice of treatment and to identify trends that may warrant future attention to improve healthcare for this important patient group.
This study aimed to determine current physical therapy practice and clinician perspectives regarding ACT prescription for patients with AECOPD in Sweden.
Materials and methods
Design, setting and participants
This was a cross-sectional investigation of all currently practicing, registered physical therapists across the 70 hospitals in Sweden responsible for the management of patients with AECOPD. Ethics approval was granted from the regional ethical board, Uppsala, Sweden (Dnr 2014/299), and the study was conducted from September 2014 to February 2015. A senior cardiorespiratory physical therapist at each hospital was first contacted to develop an email database of all physical therapists working with patients with AECOPD at their hospital. This ensured that the study could target knowledge and opinion at the individual level rather than site-specific consensus of practice. This was accompanied by an explanatory statement indicating the purpose of the research project, operational definitions of key concepts, instructions on the target audience for the electronic questionnaire, web portal (webropol) credentials and contact information of the project managers. Formal consent was assumed via completion of surveys. Participants were invited to complete the online questionnaire within 1 month, after which a first reminder email was sent 3 weeks later and a second after 6 weeks. One final contact attempt via telephone or email was made 2 months later to maximize response rates. Each survey was assigned a unique code to allow for de-identified analysis. Surveys were only excluded from analysis where respondents indicated they did not manage patients with an AECOPD.
Survey instrument
The survey was based upon a previously used questionnaire regarding ACT practices among Australian physiotherapists.11 This instrument underwent formal Swedish translation by a professional service (www.Proper-English) and was adapted to include additional questions pertinent to Swedish practice. The survey focused on ACTs used to treat patients with AECOPD and identify factors underpinning their utilization, including therapists’ knowledge of the literature. For the purpose of this investigation, ACTs were defined as any physical therapy technique used with the primary intent of clearing sputum from the airways, and an AECOPD was defined as an admission to hospital for the management of problems relating to an acute exacerbation of previously diagnosed COPD, but excluded those requiring non-invasive ventilation or intubation. The final questionnaire comprised questions covering themes related to the frequency of ACT prescription, perception of ACT effectiveness and importance, perception of the indications and aims of prescribing ACTs, factors influencing choice of ACTs and knowledge of the ACT literature (Online Appendix 1). Most questions utilized close-ended, 5-point Likert-type scales (e.g. ‘very often/always’, ‘often’, ‘sometimes’, ‘rarely’, and ‘very rarely/never’) or multiple-choice responses; however, open-ended questions were also included to allow for a more in-depth description of some aspects of clinical care. The survey took approximately 10–15 minutes to complete.
Methods of data analysis
Responses were summarized via descriptive statistics (frequencies and percentages) for categorical (nominal or Likert-type scales) data. Likert-type scales were analysed as ordinal data and pooled into fewer categories (dichotomized) where appropriate. Relationships between different variables were analysed via χ 2 test. Data were analysed using SPSS version 22.0 (SPSS Inc., Chicago, Illinois, USA). Probability values less than 0.05 were considered statistically significant.
Results
Surveys were distributed to 169 physical therapists, of which 16 reported they did not work with AECOPD patients. Responses were received from 117 of the remaining 153 physical therapists across all 70 hospitals (response rate 76%). Participant characteristics were evenly distributed according to metrics related to clinical experience (Table 1).
Table 1.
Study participant characteristics (n = 117).
| Gender (male/female), n | 17/100 |
|---|---|
| Age (years), mean ± SD | 42 ± 12 |
| Highest education level, basic (2.5–3 years), n (%) | 106 (91) |
| Highest education level, master’s degree/specialist, n (%) | 9 (7) |
| Highest education level, PhD, n (%) | 2 (2) |
| Cardiorespiratory experience (<5 years/>5 years), n (%) | 48 (41)/69 (59) |
| Completed specific cardiopulmonary courses, n (%) | 65 (56) |
PhD: Doctor of Philosophy.
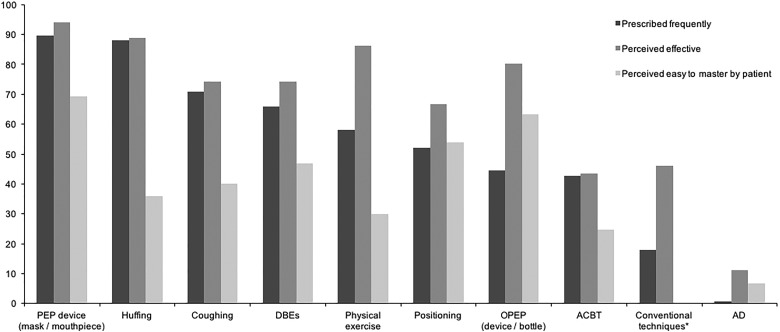
ACT prescription
ACTs were prescribed for more than 60% of all patients with an AECOPD by 75% (n = 88) of physical therapists. Treatment time was typically short, with 95% (n = 111) of physical therapists attributing between 5 minutes and 20 minutes per therapy session. The most frequently prescribed ACTs by physical therapists (combined ‘very often/always’ and ‘often’) were mask/mouthpiece PEP devices (90%; n = 105), directed huffing (88%; n = 103), directed coughing (71%; n = 83) and deep breathing exercises (66%; n = 77). The ACTs least frequently prescribed included manual vibration (7%; n = 8), sustained maximal inspiration (3%; n = 3), gravity-assisted drainage (2%; n = 2), percussion (2%; n = 2) and autogenic drainage (1%; n = 1). A summary of findings related to the incidence of ACT use, perceived effectiveness and ease of mastery is presented in Figure 1. No significant differences in the frequency of ACT prescription (combined ‘very often/always’ or ‘often’ vs. ‘very sometimes’, ‘rarely’ or ‘very rarely/never’) were apparent between respondents with ≤5 years or >5 years cardiorespiratory experience (p > 0.05 for all ACTs).
Figure 1.
Frequency of prescription, perceived effectiveness and perceived ease to master airway clearance techniques by physical therapists in Sweden. Data represent percentages (%) of overall respondents. Conventional techniques comprise postural drainage, percussions and vibrations. ACBT: active cycle of breathing technique; AD: autogenic drainage; DBEs: deep breathing exercises; PEP: positive expiratory pressure.
Perceptions of ACTs
Most physical therapists (89%; n = 104) considered ACTs to be a ‘very important’ or ‘fairly important’ aspect of the overall management (not just physiotherapeutic) of patients with AECOPD. Those who held stronger beliefs regarding the importance of ACTs (combined ‘very’ and ‘fairly important’) prescribed ACTs for a greater proportion of their patients (>60% of patients; p < 0.001). Physical therapists perceived the most effective (‘very effective’ or ‘effective’) ACTs for clearing sputum were mask/mouthpiece PEP devices (94%), directed huffing (89%) and physical exercise (86%). Those perceived to be the easiest for patients to master (combined ‘very easy’ and ‘easy’) were mask/mouthpiece PEP devices (69%), bubble/bottle PEP (62%) and positioning (54%). Directed coughing and physical exercise (for airway clearance) were perceived as being the most difficult techniques to master.
Clinical reasoning
The most frequently considered indicator for ACTs was ‘difficulty managing secretions (e.g. ineffective cough, audible gurgling and crackles on auscultation due to secretions)’ (96%; n = 112). The ‘presence of secretions (whether expectorating or not)’ and ‘recent changes in sputum characteristics (e.g. volume, colour and consistency)’ were also commonly cited (68%; n = 80 for each). The most commonly reported aims of prescribing ACTs were ‘to clear sputum’ (86%; n = 100) and ‘to prevent the development of pulmonary complications (e.g. pneumonia)’ (80%; n = 93). Additionally reported aims included ‘to enhance recovery from AECOPD’ (69%; n = 81), ‘to improve oxygen saturation’ (68%; n = 80) and ‘to increase ventilation’ (68%; n = 79). The least commonly reported aims for prescribing ACTs were ‘to reduce mortality (15%; n = 18) and ‘to reduce the need for antibiotics’ (12%; n = 14). The most common factors influencing physical therapists’ choice of ACT included the ‘degree of [patient] dyspnoea or work of breathing’ (60%; n = 70), ‘access to resources/equipment’ (54%; n = 63) and ‘one that is likely to be easiest to master’ (53%; n = 62). The majority of physical therapists advised patients with AECOPD that ACT cessation should occur ‘never – they should perform daily airway clearance irrespective of clinical status’ (57%; n = 67) or ‘when there was no evidence of sputum (e.g. dry cough)’ (38%; n = 44).
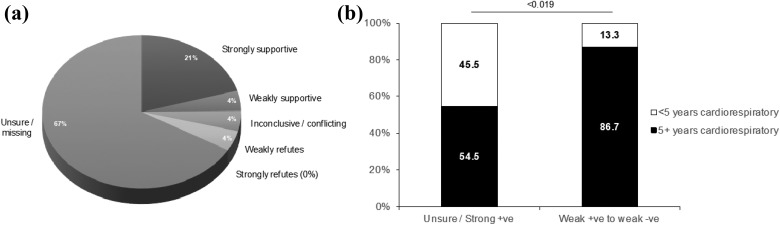
Knowledge of the ACT literature
The majority (66%; n = 75) of physical therapists felt ‘unsure what the current evidence is for ACTs during AECOPD’. Some (21%; n = 24) felt there was ‘strong evidence to support the usefulness of ACTs during AECOPD’ (Figure 2(a)). These two response items were pooled as they appeared reflective of knowledge that was not informed by the leading evidence summary at the time of conducting the survey7 (‘unsure/strong’ group; n = 99) and were compared to the remaining pooled items (‘weak/unsupportive’; n = 15). Despite a numerical imbalance between groups, a significantly greater proportion of respondents with more (>5 years) cardiorespiratory experience recorded ‘weak/unsupportive’ compared to those who recorded ‘unsure/strong’ responses (p = 0.019; Figure 2(b)).
Figure 2.
Perceptions of the literature regarding airway clearance techniques for patients with acute exacerbations of COPD. (a) Raw categorical responses and (b) dichotomized responses analysed according to <5 years/>5 years of cardiorespiratory experience; χ 2-test. COPD: chronic obstructive pulmonary disease.
Discussion
This is the first study to describe current practice and clinician perspectives and reasoning strategies for the physical therapy management of patients with AECOPD with respect to ACTs in Sweden. Most physical therapists perceived ACTs to be important aspects to patients’ overall management, with three ACTs used more frequently than others: face/mouthpiece PEP devices, directed huffing or coughing and deep breathing exercises. ACTs were most commonly reported as being prescribed for the purpose of clearing sputum and to enhance recovery from the AECOPD. Choice of ACT was most frequently determined by the degree of patients’ dyspnoea or work of breathing and therapists’ access to resources/equipment. Our cross-sectional design and high response rate affirm that the findings are an accurate representation of physical therapy practice in Sweden, thereby enabling comparisons to be made with practice from other countries.9–11
Several findings from this study appear consistent with physical therapy practice across different regions of the world. For example, the infrequent use of ‘conventional’ (manual) ACTs (18%) is comparable to previous reports from the UK (8–26%)9, Australia (45%)11 and New Zealand (5–28%).14 Swedish physical therapists appear to employ ACTs for similar clinical indications and for similar aims underpinned by similar factors to earlier reports such as the availability of resources.15 A comprehensive care programme for patients discharged from hospital after an episode of AECOPD has been shown to reduce hospital readmissions and hospital length of stay16 as well as self-management interventions.17 Increased understanding of the physiological basis for ACTs will enable physical therapists to decide which technique best aligns the patient.18 These homogeneous aspects of clinical practice internationally may be speculated as being reflective of common principles that are innately embedded within the education and physical therapy training across the world. Concerted efforts have been made in recent times to enhance the consistency of respiratory physical therapy practice across Europe, such as the HERMES programme by the European Respiratory Society Physical therapy group.19 The study also showed an association between stronger beliefs of ACT importance and a higher rate of ACT prescription. This was observed in the prior Australian study11 which highlights the impact of clinician’s beliefs and/or personal perceptions upon patient care.
It is clearly important for physical therapists to maintain high awareness of the scientific literature to ensure patient care is not compromised. It was therefore concerning to observe 75 respondents in our study report unclear interpretations of the literature regarding ACTs for patients with AECOPD. It was not possible to determine whether this observation explained any aspects about clinical practice. It was, however, interesting to note that clinicians with greater years of cardiorespiratory experience had more accurate knowledge of the evidence in this field than those with less experience. While this relationship is not confirmatory, it could highlight a possible avenue for future educational strategies.
The present study generated some novel findings. Use of ACBT (43%) was notably lower than in the UK (88%),9 Australia (79%)11 and New Zealand (86%),14 while non-oscillatory PEP devices were utilized very frequently (90%), more than oscillatory PEP devices (44%). The reasons for this are not clear. PEP therapy originated in Scandinavia and has been an anecdotal mainstay of physical therapy practice for many years. The PEP equipment may be funded and provided by the healthcare system. Several mechanisms have been proposed to explain how PEP therapy may facilitate airway clearance in patients with COPD. These include splinting airways open that may be prone to dynamic compression during forced expiratory manoeuvres8,20 and reducing gas trapping and thereby improving ventilation. These are all very well suited to the pathophysiological dysfunction that occurs in the lungs of people with COPD, however confirmatory evidence of these mechanisms occurring in this patient group has been somewhat elusive.21,22 A previous systematic review of PEP therapy for patients with COPD showed inconsistent findings across a limited number of small studies and highlighted a need for further research to determine any likely clinical benefits.23 A more recent Cochrane review reported a statistically significant pooled benefit for ACTs (compared to usual care) in reducing the need for or duration of assisted ventilation during AECOPD, with larger effects suggested for PEP-based versus non-PEP-based techniques.7 A subsequent large randomized controlled trial of PEP therapy for patients with AECOPD, however, failed to show any appreciable benefit on a range of clinically important outcomes.24
Other interesting observations in this study related to the discrepancy between perceived effectiveness and rate of prescription for certain ACTs. Differences were apparent between the rates of prescription of PEP devices versus bottle PEP, yet both were perceived to be highly effective and easy to master. Physical exercise was not prescribed very frequently for the purpose of airway clearance, in contrast with the findings of the previous Australian survey.11 Swedish physical therapists felt, however, that it was one of the most effective ACTs. This discrepancy may be driven by clinicians’ perception that it is challenging for patients to master (Figure 1). As evidence of the effects of physical exercise on airway clearance outcomes is scarce, this may represent an emerging area of clinical interest to explore in future studies.
Many aspects of clinical reasoning governing the physical therapy management of patients with AECOPD are largely unguided by international COPD management recommendations. This has no doubt driven much of the variability within and between different regions of the world. An example of this in our study was the lack of consensus regarding when ACTs should be ceased. The largest response category was actually that patients should not cease performing ACTs at all after AECOPD. That is, a perception that ACTs are part of a lifelong maintenance strategy, irrespective of a patient’s clinical status.
The survey instrument used for this study does not possess known psychometric properties, however it has been used in a previous Australian study with identical research aims specific to that country. Details regarding its evidence-based development and design, plus testing for face validity have been previously described.11 No sample size calculation was made for this study due of the cross-sectional nature of survey distribution for this study (i.e. all hospitals in Sweden treating patients with AECOPD). We did observe an overt gender imbalance within our respondent sample (female, n = 100; male, n = 17). The significance of this is not clear, however we feel it is likely representative of the physical therapy profession in Sweden. A limitation of the study is that the survey questions related to specific ACTs applied in isolation and those applied in combination with each other or adjuncts such as aerosol therapy. Additionally, our study did not capture data regarding the size, bed capacity or mean duration of hospital stay for patients with AECOPD at the participating hospitals in this study. This may have provided interesting insight into the possible relationship between ACT practice and factors related to workforce training, clinical settings or access to local resources. Finally, we cannot currently say that one ACT is better than another for the average patient with AECOPD. Several factors will always come into consideration that influence clinicians’ choice of technique, frequency of prescription and timing regarding ACT cessation. In the absence of definitive evidence to guide clinicians regarding ACT prescription, it seems sensible that therapists approach this aspect of respiratory medicine within a personalized airway clearance management framework.18
Conclusions
This cross-sectional national survey provides some of the first robust evidence detailing physical therapy practice regarding ACTs for patients with AECOPD in Sweden. Physical therapists were shown to prescribe ACTs very frequently, especially those based upon PEP, and most physical therapists perceived ACTs to be an important aspect of patients’ overall management.
Supplemental Material
Supplemental Material, Appendix_1_Part_A_Chronic_Respiratory_Disease for Airway clearance techniques for patients with acute exacerbations of chronic obstructive pulmonary disease: Physical therapy practice in Sweden by Elisabeth Westerdahl, Christian Osadnik and Margareta Emtner in Chronic Respiratory Disease
Acknowledgement
This work was supported by a scholarship from Uppsala University, Uppsala, Sweden.
Authors’ note: EW and CO contributed equally to this work.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iD: Elisabeth Westerdahl  https://orcid.org/0000-0002-8363-1662
https://orcid.org/0000-0002-8363-1662
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Eur Respir J 2017; 49(3): 1700214. [DOI] [PubMed] [Google Scholar]
- 2. GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388(10053): 1459–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wedzicha JA, Miravitlles M, Hurst JR, et al. Management of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J 2017; 49(3): 1600791. [DOI] [PubMed] [Google Scholar]
- 4. Langer D, Hendriks E, Burtin C, et al. A clinical practice guideline for physiotherapists treating patients with chronic obstructive pulmonary disease based on a systematic review of available evidence. Clin Rehabil 2009; 23(5): 445–462. [DOI] [PubMed] [Google Scholar]
- 5. Sahin H, Varol Y, Naz I, et al. The effect of pulmonary rehabilitation on COPD exacerbation frequency per year. Clin Respir J 2016; 12(1): 165–174. [DOI] [PubMed] [Google Scholar]
- 6. Osadnik CR, McDonald CF, Holland AE. Advances in airway clearance technologies for chronic obstructive pulmonary disease. Expert Rev Respir Med 2013; 7(6): 673–685. [DOI] [PubMed] [Google Scholar]
- 7. Osadnik CR, McDonald CF Jones AP, et al. Airway clearance techniques for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012. March 14; (3): CD008328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fagevik Olsen M, Lannefors L, Westerdahl E. Positive expiratory pressure – common clinical applications and physiological effects. Respir Med 2015; 109(3): 297–307. [DOI] [PubMed] [Google Scholar]
- 9. Yohannes AM, Connolly MJ. A national survey: percussion, vibration, shaking and active cycle breathing techniques used in patients with acute exacerbations of chronic obstructive pulmonary disease. Physiotherapy 2007; 93(2): 110–113. [Google Scholar]
- 10. Harth L, Stuart J, Montgomery C, et al. Physical therapy practice patterns in acute exacerbations of chronic obstructive pulmonary disease. Can Respir J 2009; 16(3): 86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Osadnik CR, McDonald CF, Holland AE. Airway clearance techniques in acute exacerbations of COPD: a survey of Australian physiotherapy practice. Physiotherapy 2013; 99: 101–106. [DOI] [PubMed] [Google Scholar]
- 12. McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2015. February 23; (2): CD003793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Torres-Sanchez I, Cruz-Ramirez R, Cabrera-Martos I, et al. Results of physiotherapy treatments in exacerbations of chronic obstructive pulmonary disease: a systematic review. Physiother Can 2017; 69(2): 122–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lee A, Button B, Denehy L. Current Australian and New Zealand physiotherapy practice in the management of patients with bronchiectasis and chronic obstructive pulmonary disease. NZJ Physiother 2008; 36(2): 49–58. [Google Scholar]
- 15. Wadell K, Janaudis Ferreira T, Arne M, et al. Hospital-based pulmonary rehabilitation in patients with COPD in Sweden – a national survey. Respir Med 2013; 107(8): 1195–1200. [DOI] [PubMed] [Google Scholar]
- 16. Ko FW, Cheung NK, Rainer TH, et al. Comprehensive care programme for patients with chronic obstructive pulmonary disease: a randomised controlled trial. Thorax 2017; 72(2): 122–128. [DOI] [PubMed] [Google Scholar]
- 17. Lenferink A, Brusse-Keizer M, van der Valk PD, et al. Self-management interventions including action plans for exacerbations versus usual care in patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2017; 8: CD011682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McIlwaine M, Bradley J, Elborn JS, et al. Personalising airway clearance in chronic lung disease. Eur Respir Rev 2017; 26(143): 160086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Troosters T, Pitta F, Oberwaldner B, et al. Development of a syllabus for postgraduate respiratory physiotherapy education: the Respiratory Physiotherapy HERMES project. Eur Respir J 2015; 45(5): 1221–1223. [DOI] [PubMed] [Google Scholar]
- 20. Nield MA, Soo Hoo GW, Roper JM, et al. Efficacy of pursed-lips breathing: a breathing pattern retraining strategy for dyspnea reduction. J Cardiopulm Rehabil Prev 2007; 27(4): 237–244. [DOI] [PubMed] [Google Scholar]
- 21. Osadnik C, Stuart-Andrews C, Ellis S, et al. Positive expiratory pressure via mask does not improve ventilation inhomogeneity more than huffing and coughing in individuals with stable chronic obstructive pulmonary disease and chronic sputum expectoration. Respiration 2014; 87(1): 38–44. [DOI] [PubMed] [Google Scholar]
- 22. Wood J. The use of positive expiratory pressure therapy does not appear to be effective in people hospitalised with an acute exacerbation of chronic obstructive pulmonary disease (AECOPD). J Physiother 2015; 61(1): 43. [DOI] [PubMed] [Google Scholar]
- 23. Fagevik Olsen M, Westerdahl E. Positive expiratory pressure in patients with chronic obstructive pulmonary disease – a systematic review. Respiration 2009; 77(1): 110–118. [DOI] [PubMed] [Google Scholar]
- 24. Osadnik CR, McDonald CF, Miller BR, et al. The effect of positive expiratory pressure (PEP) therapy on symptoms, quality of life and incidence of re-exacerbation in patients with acute exacerbations of chronic obstructive pulmonary disease: a multicentre, randomised controlled trial. Thorax 2014; 69(2): 137–143. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Appendix_1_Part_A_Chronic_Respiratory_Disease for Airway clearance techniques for patients with acute exacerbations of chronic obstructive pulmonary disease: Physical therapy practice in Sweden by Elisabeth Westerdahl, Christian Osadnik and Margareta Emtner in Chronic Respiratory Disease