Abstract
Vaccines are considered one of the greatest advances in modern medicine. The global burden of numerous infectious diseases has been significantly reduced, and in some cases, effectively eradicated through the deployment of specific vaccines. However, efforts to develop effective new vaccines against infectious pathogens such as influenza, Human immunodeficiency virus (HIV), dengue virus (DENV), chikungunya virus (CHIKV), Ebola virus, and Zika virus (ZIKV) have proven challenging. Zika virus is a mosquito-vectored flavivirus responsible for periodic outbreaks of disease in Africa, Southeast Asia, and the Pacific Islands dating back over 50 years. Over this period, ZIKV infections were subclinical in most infected individuals and resulted in mild cases of fever, arthralgia, and rash in others. Concerns about ZIKV changed over the past two years, however, as outbreaks in Brazil, Central American countries, and Caribbean islands revealed novel aspects of infection including vertical and sexual transmission modes. Cases have been reported showing dramatic neurological pathologies including microcephaly and other neurodevelopmental problems in babies born to ZIKV infected mothers, as well as an increased risk of Guillain-Barre syndrome in adults. These findings prompted the World Health Organization to declare ZIKV a public health emergency in 2016, which resulted in expanded efforts to develop ZIKV vaccines and immunotherapeutics. Several ZIKV vaccine candidates that are immunogenic and effective at blocking ZIKV infection in animal models have since been developed, with some of these now being evaluated in the clinic. Additional therapeutics under investigation include anti-ZIKV monoclonal antibodies (mAbs) that have been shown to neutralize infection in vitro as well as protect against morbidity in mouse models of ZIKV infection. In this review, we summarize the current understanding of ZIKV biology and describe our efforts to rapidly develop a vaccine against ZIKV.
Keywords: Flaviviruses, ZIKV vaccine, Animal models, Immunopathology, DNA vaccines, Immunity
1. Introduction
For nearly 70 years after its discovery in 1947, Zika virus (ZIKV) was largely ignored by the world's scientific and medical communities as it was believed to cause only mild, self-limited symptoms in a minority of infected individuals [1], [2]. This indifference turned to grave concern in 2016 after a ZIKV outbreak in Brazil revealed insidious new signs and symptoms of infection as well as new modes of transmission of the virus, specifically transmission through sexual contact [1], [3], [4]. Among these previously unappreciated symptoms was the appearance of severe microcephaly and/or other congenital defects in babies born to ZIKV-infected pregnant women, particularly women infected early in their pregnancy [4], [5]. The appearance of these new sequelae combined with ZIKV's rapid global spread prompted the World Health Organization (WHO) to declare ZIKV infection a public health emergency early in 2016 unleashing a concerted effort by scientists and health professionals to understand the pathogenesis, spread, and treatment options for this emerging infectious agent. While the WHO lifted its Zika declaration by the end of 2016, the scientific research it stimulated has led both to a deeper understanding of ZIKV pathogenesis and to the development of vaccine candidates to combat ZIKV infection and disease.
Zika virus is a member of the Flavivirus genus of the Flaviviridae family, a group of positive-sense, single-stranded RNA viruses. Among this genus are several clinically important viruses including yellow fever virus (YFV), Japanese encephalitis virus (JEV), tick-borne encephalitis virus (TBEV), West Nile virus (WNV) and four subtypes of Dengue virus (DENV1-4). Most if not all flaviviruses are transmitted to vertebrates by insect vectors and thus are also classified as arthropod-borne viruses (arboviruses). Genetically, ZIKV shares ∼70% nucleotide identity with Spondweni virus and ∼50–60% nucleotide identity with JEV, WNV, and all four DENV serotypes [6]. Immunologically, there is cross-reactivity between responses observed to several of these viruses which played a role in early studies to characterize this family of infections [7]. Importantly, efficacious vaccines have been previously developed against YFV and JEV suggesting that flaviviruses are vaccine tractable, but efforts to develop vaccines against other flaviviruses have encountered unique setbacks. These include the difficulty to induce broad neutralizing antibodies against the varied Hepatitis C virus and more recent observations that a live attenuated yellow fever recombinant tetravalent DENVs 1–4 vaccine is associated with more severe infection in specific seronegative individuals and some groups of children following vaccination [8].
In this review, we discuss our efforts to develop a synthetic DNA-based vaccine to respond to the outbreak of ZIKV disease that began in 2016 in Brazil. At the start of our efforts, there were few laboratory experimental systems, reagents, and animal models that could be employed for ZIKV vaccine development. Furthermore, there was a paucity of studies on the biology and immunology of ZIKV to provide guidance on how to effectively combat its spread, but evaluations of vaccines developed against the related YFV and DENV strongly suggested that antibodies against the envelope (E) antigen of ZIKV, by analogy, might be an important immune correlate of protection for a ZIKV vaccine. Despite these obstacles, our group accepted the challenge of developing an effective ZIKV vaccine, and were able to develop a candidate and advance it into Phase I clinical trial seven months after the WHO declaration in 2016.
2. Zika virus history
Historical records and phylogenetic analyses of ZIKV indicate that the virus originated in or near Uganda and from there spread globally eastward from Africa through the tropics [9]. Zika virus was first isolated from a sentinel monkey that developed fever during a study of arboviruses being conducted in the Zika forest of Uganda in 1947. Human serologic evidence of ZIKV-infection was not reported until 1952 in East Africa [10]. MacNamara reported in 1954 on three persons with a febrile illness occurring during an outbreak of yellow fever in Nigeria who manifested Zika virus seroconversion [11]. However, first documented isolation of ZIKV in a human was as part of a challenge study in a human researcher who manifested a mild viral infection characterized by headache, malaise, and total body rash [12]. The first report of ZIKV outside Africa occurred in 1966 in Malaysia, and over the next few decades, cases of ZIKV infection were reported throughout Southeast Asia. Outside of Africa or Asia, the first reported outbreak of ZIKV infection occurred in 2007 on Yap Island in the Western Pacific. Over the next few years, the eastward progression continued with outbreaks of ZIKV infection reported on multiple islands throughout the Pacific Ocean [1]. One of the largest of these outbreaks occurred in French Polynesia in 2013–14 with over 30,000 reported cases. It was during this outbreak that the first evidence of neurologic symptoms following ZIKV infection were noted as there was a dramatic uptick in Guillain-Barré Syndrome cases on the islands after the outbreak started compared to previous years [13]. Analyses suggest that there were multiple introductions of ZIKV into the Western hemisphere beginning in late 2013 or early 2014, with the epicenter of the infestation being Northeast Brazil [14], [15], [16]. By the end of 2016, autochthonous ZIKV transmission was reported in most tropical countries in the Western hemisphere and in the Caribbean as well as in the far southern regions of the continental United States [17].
Zika virus circulates in both an enzootic sylvatic cycle as well as in an urban cycle with mosquito species of the Aedes genus serving as the primary vector for both [11]. Many arboreal Aedes species including Aedes africanus carry ZIKV and thus are likely the major mediators of sylvatic transmission while the urban transmission is primarily mediated by Aedes aegypti mosquitos, although Aedes albopictus, Aedes hensilli and other urban mosquitos may also play a role. In addition to infection acquired during a blood meal from an infected host animal, ZIKV is passed vertically in mosquitos via transovarial transmission [18]. Viral genomes and serum antibodies targeting ZIKV are found in multiple nonhuman primate (NHP) species making them a likely reservoir, but sero-surveys and limited genetic testing indicate that diverse organisms including bats, sheep, goats, cattle, water buffalos, and birds may also be susceptible to infection [12], [19]. Modeling studies show the potential for NHPs to serve as ZIKV reservoirs [20], [21].
The apparent increase in virulence and transmissibility of ZIKV during the 2016 Western Hemisphere outbreak suggested to some that it had acquired mutations, but several analyses of diverse global ZIKV isolates found a high degree of similarity between contemporary and early strains of ZIKV. Sequence analyses of ZIKVs show that they segregate into two lineages, African and Asian, that are roughly 89% identical at the genetic level [22]. Despite this divergence, ZIKV circulates as a single serotype [23], [24]. The ZIKV strains responsible for the Brazil and Western hemisphere outbreak from 2014 to 2016 are part of the Asian lineage [14], [17], [22]. Ongoing investigations of sequences of contemporary ZIKVs for their contribution(s) to ZIKV virulence and transmissibility. One study noted that the ∼10 amino acids (aa) bordering a glycosylation site at Asn 154 in ZIKV envelope proteins are not present in other flaviviruses and differ between ZIKV strains suggesting that this region may play a role in virus transmission and/or virulence [25]. Liu et al. identified a spontaneous alanine-to-valine amino acid substitution in the NS1 protein of contemporary ZIKV strains that increases its infectivity of A. aegypti mosquitoes [26]. An analogous change in the genetic sequence of the alphavirus chikungunya in 2013 aided its ability to infect A. albopictus mosquitos which contributed to outbreaks of disease in Indian Ocean nations [27]. Yuan and colleagues identified a serine to asparagine mutation (S139N) that appeared in ZIKV strains around 2013 prior to the outbreak in French Polynesia [28]. This mutation has been stably maintained in ZIKVs isolated after 2013, and in vitro experiments suggest that its presence causes increased ZIKV infection of both human and mouse neural progenitor cells (NPCs) as well as microcephaly and fetal demise in mouse models.
3. Zika virus biology
A typical Zika virion is roughly spherical in shape and consists of a capsid (C) protein-encapsulated genome surrounded by a phospholipid bilayer embedded with envelope (E) and membrane (M) proteins. The ZIKV genome is an ∼11 kb positive-sense, single-stranded RNA that encodes three structural proteins (C, premembrane/membrane (prM), and E) and seven non-structural (NS) proteins (NS1, NS2a, NS2b, NS3, NS4a, NS4b, and NS5). Virions assemble on and bud into the endoplasmic reticulum (ER) using poorly defined processes that produce ∼60 nm diameter non-infectious immature particles containing roughly 60 trimers of prM-E heterodimers. Immature particles have a “spiky” appearance in cryo-electron microscopy (cryo-EM) images due to E proteins adopting a “bent” conformation in which the fusion peptide is exposed but shielded by a full-length prM protein to prevent premature fusion between viral and cellular membranes. As immature particles transit through the secretory pathway, resident furin proteases in the trans Golgi network cleave prM proteins leaving M proteins embedded in the bilayer and ∼90aa soluble “pre” peptides that remain with virions and disassociate after virion release. The function of M proteins on mature virions is unknown. After prM cleavage, ∼90 opposing head-to-tail E protein dimers flatten along the surface into a herringbone-like pattern resulting in ∼50 nm diameter mature, infectious particles. The external portion of each E protein contains three distinct domains (DI, DII, and DIII) and is linked to viral membranes via a helical stem region that is connected to two transmembrane domains (Fig. 1 ) [29].
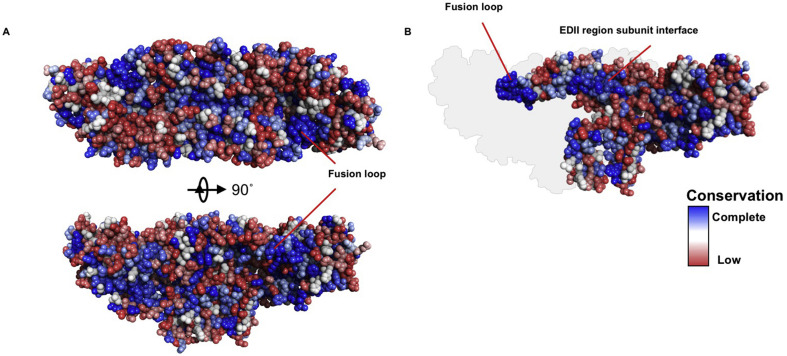
Fig. 1.
Conservation of ZIKV E glycoprotein sequence mapped to representative flavivirus E glycoprotein sequences. (A) A comparative model of ZIKV E glycoprotein and associated prM peptide was generated with Discovery Studio 4.5 (BIOVIA, San Diego, CA, USA). A- CLUSTAL W alignment of representative ZIKV, DENV1, DENV2, DENV3, DENV4, YFV, WNV, JEV, and TBEV E glycoprotein sequences was performed and the relative conservation of residues was mapped to the model. Blue indicates complete conservation among the sequences, shading to white and to red for the least conservation. The ZIKV E glycoprotein dimer is displayed in two orientations. Membrane orientation is behind the protein in the upper panel and below the protein in the lower panel. Conservation is evident in the fusion loop region. (B) ZIKV model as in lower panel of A with one subunit removed to display the interface between the molecules. The deleted subunit is indicated in silhouette. Conservation of the fusion loop and in the subunit interface of the EDII region.
Zika virions enter cells via endocytosis after which the low pH environment of early to late endosomes triggers conformational changes in E proteins. These conformational changes expose the fusion peptide which then mediates merging of the virus and cell membranes. Specific cellular proteins involved in ZIKV/flavivirus entry remain poorly defined, but a variety of non-specific proteins including C-type lectins (specifically DC-SIGN and DC-SIGNR) as well as phosphatidylserine receptors of the TIM (T cell/transmembrane, immunoglobulin, and mucin) or TAM (TYRO3, AXL, and MER) protein families may play a role(s) in virus attachment and/or entry [30]. Studies indicate that AXL binds ZIKV more efficiently than it does other flaviviruses, and it may be central to ZIKV entry into fetal endothelial cells as well as neurons and other cells [31], [32], [33]. However, experiments in mice indicate that AXL is not required for infection suggesting a role for other molecules in viral entry [30], [33], [34].
Inefficiencies in flavivirus assembly and maturation can lead to the release of a mixture of immature virions, mature viruses, and partially mature virions from cells. Wholly immature particles are non-infectious but could be relevant immunologically in eliciting antibody responses to E protein epitopes that are hidden or partially exposed on mature virions. Partially mature viruses are likely infectious and thus contribute along with mature viruses to pathogenesis. In addition to full virions, subviral particles (SVPs) that contain prM and E proteins without capsid or viral genomes are also produced as byproducts of flavivirus assembly. The SVPs are non-infectious, but immunogenic, as transit through the secretory system causes the E proteins on SVPs to adopt similar conformations and packaging as seen on full virions. Cellular expression of just the flavivirus prM and E proteins drives SVP formation and we and others exploited this concept in the development and testing of novel Zika immunogens [35].
4. Zika virus disease
Despite the recent observation of new, severe signs of ZIKV infection, in some populations the majority of people infected will likely experience only subclinical or mild symptoms. ZIKV clinical disease typically presents with symptoms that appear between 6 and 11 days post-infection and generally include rash, mild fever, arthralgia, and conjunctivitis. Virus can be isolated from patients' blood for approximately seven days after clinical presentation and from urine for up to 28 days. Viral RNA can be detected in semen for up to six months following infection. Most symptoms of ZIKV infection resolve by two weeks post infection. Antibodies to ZIKV appear an average of nine days post-infection and are believed to provide long-term, perhaps lifelong protection against future infection [4], [5], [36].
Guillain-Barre syndrome (GBS) is an illness characterized by the progressive loss of motor functions that may result in require the need for mechanical respiratory support. GBS was first appreciated as a complication of ZIKV infection during the 2012 outbreak in French Polynesia and a retrospective analysis of this outbreak found the attack rate of GBS development to be 0.24 cases per 100,000 ZIKV infections [13]. In contrast to Campylobacter jejuni associated GBS, for which anti-ganglioside antibodies are universally detected, detection of such auto-antibodies were only found in approximately 30% of ZIKV-infected individuals suggesting potential alternative etiologies [13]. Although there have been no reports of ZIKV detection in nerve tissues from GBS patients, studies show ZIKV can readily infect neuronal progenitor and stem cells mediated through the NS4A and NS4B proteins and has been detected in neurons and glial cells from the brains of fetuses of mothers infected during pregnancy [37], [38].
International attention was focused on ZIKV in 2015 when rates of microcephaly reported in Brazil represented an eight to 10-fold increase in this condition over prior years [39]. Investigation quickly centered on ZIKV based on reports regarding mothers experiencing symptoms of ZIKV infection during their pregnancy and was bolstered by the recovery of ZIKA, RNA from amniotic fluid and/or tissues of fetuses or babies diagnosed with microcephaly [5]. Subsequent investigation in mice and NHP models confirmed that ZIKV is a teratogen that can severely impact fetal development [40], [41], [42], [43]. Further surveillance revealed that ZIKV infection can also lead to retinal and ophthalmologic abnormalities, hearing loss, arthrogryposis, and cerebral and ocular calcifications [44], [45], [46]. Overall, the risk of microcephaly for babies born to mothers infected with ZIKV during pregnancy has ranged from 6%, in a study as part of a US registry of women infected in ZIKV endemic regions and returning to the US regardless of maternal symptomatology, to 46%, in a study of Brazilian women who presented with symptomatic ZIKV infection [4], [38]. In both studies rates of microcephaly and other birth defects were highest when infection occurred early in pregnancy.
Studies in mice highlight a potential for ZIKV to cause male infertility when infection occurs among young animals. Immune-suppressed mice infected at either seven or 10–11 weeks of age demonstrate damage to the seminiferous tubules, testicular atrophy, oligospermia, and reduced rates of fertility [47], [48], [49]. To date there has been no documented effect of ZIKV infection on male fertility in humans, but multiple studies have reported evidence of ZIKV in human seminal fluid and/or infection of a sexual partner after return from a Zika-endemic region [50], [51], [52], [53], [54] including one case of male to male transmission [55]. Prolonged detection of ZIKV RNA in semen for at least 8 weeks was noted in three studies [3], [50], [53], and one these also reported recovery of infectious virus from semen at eight weeks post-infection [3]. These results support the need for further evaluation and surveillance for ZIKA effects on fertility.
5. Zika virus immunology
As seen with other flaviviruses, ZIKV infection induces a polyclonal antibody response and protection from infection and disease correlates most closely with this. Passive transfer of both neutralizing as well as non neutralizing antibodies can protect against challenge in small animal models. Structural similarity between flaviviruses leads to a high degree of cross-reactivity between anti-flavivirus antibody responses, but only a limited amount of cross-neutralization has been observed. While antibodies targeting E, prM, and NS1 are all detected after ZIKV infection, only antibodies targeting E exhibit significant neutralizing activity [56]. Antibodies to NS1 are largely ZIKV specific unless the infection is secondary to infection by another flavivirus in which case cross-reactivity is seen [56]. However, an anti-ZIKV NS1 mAb has been isolated and shown to be effective as a diagnostic tool for ZIKV infection [57]. By far the most potent inducer of protective antibodies is the E protein, with responses mapped to linear epitopes in all three E protein domains as well as to quaternary epitopes formed by the mature structure [58]. Domain III-targeting antibodies typically possess high flavivirus type-specific binding and neutralization activity, although some cross react and neutralize closely related flaviviruses [56]. By contrast, antibodies specific to epitopes in E domains I and II are broadly cross-reactive between flaviviruses, but poorly neutralizing likely due to their relative inaccessibility on mature virions (Fig. 1). There has been only limited study of antibodies to these regions transferring protection in model systems. Antibodies targeting the fusion loop epitope (FLE) and two quaternary epitopes present in the dimeric E protein structure (termed envelope dimer epitopes (EDE) 1 and 2) are highly cross-reactive between DENV and ZIKV, but only the latter possess significant neutralization activity. While not reported, ZIKV infection likely induces antibody responses to the prM protein, and based on studies on anti-prM antibodies induced by DENV, these are likely cross-reactive with other flaviviruses [58].
The sequence and structural similarity between flavivirus E proteins leads to a high degree of cross-reactivity between flavivirus antibody responses and has prompted investigations into how prior flavivirus exposure influences the development of anti-ZIKV responses [56], [59]. The effect(s) of prior DENV exposure on the neutralization capacity of anti-ZIKV antibodies in humans is still unclear [59], [60]. An investigation of late (>6 months post infection) convalescent sera from patients infected with DENVs found that ZIKV cross-reactive antibodies were not durable, and that prior DENV exposure did not affect development of antibody responses to ZIKV infection [61]. One concern for flavivirus cross-reactive antibodies is whether they may enhance infection as observed clinically with DENVs. This phenomenon, termed antibody-dependent enhancement (ADE) of infection, is hypothesized to occur when antibody responses to the primary infecting strain fail to neutralize infection by a second strain, but through binding them, mark these viruses for opsonization by Fc-γ receptor-expressing cells which subsequently get infected. It is important to note that no such ADE activity has been observed with ZIKV in the field to date. In mouse certain highly engineered mouse models the ability to drive ADE or protection and will required more investigation. Studies examining mAbs or early convalescent sera from DENV or WNV infected patients which cross-reacts with ZIKV, found that some of these can neutralize ZIKV infection in vitro and are protective in a ZIKV-challenge mice model [58], [62]. However, other studies have found that some similar or identical non-neutralizing antibodies as well as low levels of neutralizing antibodies mediate ZIKV ADE in vitro. Importantly, at least two studies in rhesus macaques found that prior DENV infection had no effect on anti-ZIKV immunity and did not enhance ZIKV disease [36], [63], [64]. Most importantly, study of acute ZIKV infection in humans previously infected with DENV found no clinical evidence of ADE, but further study is warranted [65]. Further study is clearly warranted however to date there has been no clinical report of ADE for Zika or for Dengue.
Zika virus infections likely induce specific and cross-reactive cellular responses, but how these responses contribute to protection against infection or aid recovery is unclear. Most of the work on cellular responses to ZIKV has relied on mouse models of infection so the applicability of the findings to humans is not yet clear. Infection of wild type, immunocompetent C57/B6 mice induced Th1 polarization of CD4+ T cells and an activated effector phenotype in CD8+ T cells with many CD8+ T cells responding to an epitope in the E protein [66]. Shresta et al. found that mice lacking CD8+ T cells had higher mortality following ZIKV infection and that CD8+ T cells from ZIKV-infected mice recognized epitopes in prM, E, and NS5 [67]. This group also used human leukocyte antigen (HLA) transgenic mice to identify 25 HLA-B*0702 and 1 HLA-A*0101 restricted epitopes that may be relevant to human cellular responses to ZIKV [68]. Cellular responses to at least five of the HLA-B*0702-restricted epitopes were found to offer protection against DENV infection. Grifoni et al. found that DENV-specific T cell responses induced by natural infection or vaccination could also recognize ZIKV-derived peptides and this contributed to a more rapid and robust anti-ZIKV cellular response in DENV-experienced individuals after ZIKV infection [69]. Memory T cells from ZIKV-infected patients that targeted NS1 or E proteins were found to be poorly cross-reactive in donors pre-exposed to DENV [56].
The innate immune system also affects ZIKV infection. Type III interferon (IFN) was shown to act in an autocrine and paracrine manner to protect trophoblast and non-trophoblast cells from ZIKV infection, and it may also help protect full-term placentas from ZIKV infection [70]. Zika virus infection of skin cells or human embryonic stem cell-derived cerebral organoids was found to upregulate Toll-like-Receptor 3 (TLR3), and TLR3 inhibition in these could reduce ZIKV-induced phenotypic changes [71], [72].
6. Flavivirus vaccines
The fact that vaccines have been developed and are in clinical use for other flaviviruses including YFV, JEV, and DENV provides optimism that a vaccine that can protect against ZIKV infection is possible. The YFV vaccine is a live-attenuated vaccine that was developed by several hundred passages of the Asibi YFV strain in mouse embryo tissue cultures and chicken embryo tissue cultures with and then also without nerve tissue [73]. The resultant attenuated strain, 17D has been used in humans since 1937 and has over a 90% success rate. Four types of inactivated and live-attenuated JEV vaccines have been developed and used globally, but only an inactivated Vero cell culture-derived JEV is licensed for use in the United States [74]. These vaccines have served as paradigms for development of ZIKV vaccines.
Experiences from the licensed DENV vaccine does, however, provide a cautionary lesson for the development of a ZIKV vaccine. Dengvaxia is a live-attenuated vaccine consisting of four chimeric YFV 17D vaccines each containing a substitution of their prM and E genes with those from one of the four DENV strains [75]. Analysis of data from Phase III studies of Dengvaxia noted an increase in incidence of severe DENV infections among young children that resulted in the vaccine being licensed for use only in individuals greater than age 9 years [67]. A more recent analysis by the company found that regardless of age, vaccination of sero-naïve individuals was associated with significant risk for severe DENV infection. While the increase in severe DENV infections has been attributed by some to ADE, prospective studies from a large Thai cohort did not find any correlation between in vitro ADE and clinical severity of secondary cases of DENV [76]. Moreover, a recent study found no evidence of severe Zika virus infections occurring during pregnancy in relation to DENV sero status [77]. As of this writing, 4 different nucleic acid vaccines (3 DNA plasmid, 1 mRNA), 2 inactivated virus vaccines, and a measles vectored vaccine all targeting Zika virus have advanced into clinical trials (Table 1 ).
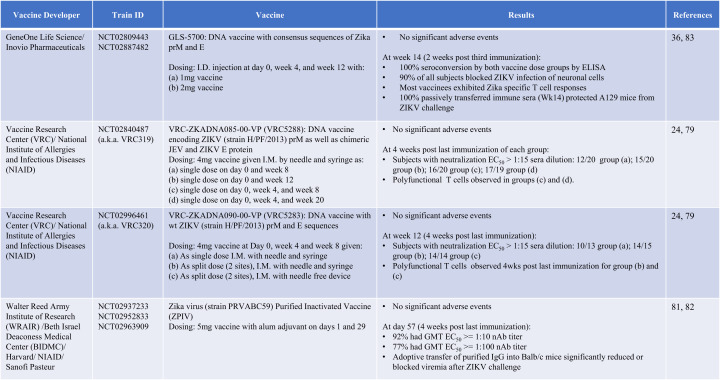
Table 1.
Summary of Zika vaccine development advanced into clinical trials.
7. Development of a ZIKV vaccine using synthetic DNA technology
The DNA vaccine platform has been used for over twenty-five years to create candidate vaccines against numerous pathogens. DNA vaccines are created by cloning an antigen(s) from a pathogen into a DNA plasmid. The vaccines are administered into either the muscle or skin where resident cells take up the vaccine, produce the encoded antigen, and present it to the immune system. The DNA vaccine platform reliably induces both cellular and humoral immunity and carries virtually no risk of causing disease since they deliver only a small portion of the full pathogen genome. Additionally, DNA vaccines can be designed, manufactured, and distributed faster and cheaper than virus- or protein-based vaccines.
Our group has extensive experience in designing improved vaccine cassettes for synthetic DNA vaccines against pathogens, and know-how in rapidly moving vaccine candidates into the clinic [78], [79], [80], [81], [82], [83]. In the past five years, we have developed synthetic DNA vaccine candidates targeting Ebola virus and Middle East respiratory syndrome coronavirus (MERS-CoV) in response to outbreaks of each virus [78], [83]. Each vaccine encodes a synthetic consensus viral surface protein antigen, either the Ebola virus glycoprotein (GP) [83] or the spike protein of MERS-CoV, that can induce immunity to diverse strains of each virus. Both vaccines are administered using electroporation (EP) enhanced intramuscular (i.m.) delivery using CELLECTRA® EP. The Ebola virus vaccine has also been administered with a novel EP-enhanced intradermal (i.d) delivery platform that is simpler and more tolerable than i.m. delivery [83]. The Ebola virus vaccine was advanced through animal studies and into the clinic in less than 18 months (NCT02464670). The MERS-CoV reached the clinic in 11 months (NCT02670187), after preclinical studies showed the vaccine protected NHPs from infection and disease and was immunogenic in a number of species including camels.
With this background, we thought that a rapid approach to development and deployment of a ZIKV vaccine was reasonable when the WHO declared it a public health emergency. At the start of our efforts, there was extensive research on the pathogenesis and immunogenicity of related flaviviruses such as dengue and West Nile virus, but little-published literature on ZIKV. Additionally, there were few available reagents and established assays to investigate ZIKV. While the lack of resources provided unique developmental challenges, we were able to leverage our experiences in creating synthetic DNA vaccine for other pathogens to produce a ZIKV vaccine and get it into the clinic within seven months (Fig. 2 ).
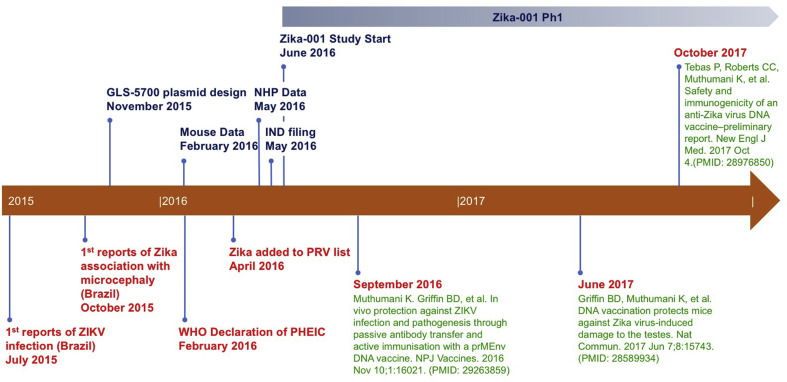
Fig. 2.
Timeline of Zika DNA vaccine development. July of 2015 marked the first reports of Zika infection in Brazil with the first association of Zika with microcephaly reported in October of 2015. Following that report, we started plasmid design and in vitro testing. In February of 2016, about the same time that the WHO declared that Zika was a “Public Health Emergency of International Concern”, we completed the first mouse studies and had begun NHP immunogenicity studies. In May, 2017, the first NHP study was completed and the IND has filed shortly after. The GLS-5700 phase 1 clinical trial started in June 2017, a short 7 months after the initial vaccine design was started (NCT02809443). All the preclinical work has since been published in September of 2016 and June of 2017, and the preliminary report of the clinical trial data was published in October 2017.
We designed and synthesized multiple ZIKV DNA vaccines and evaluated each in mice for their ability to induce ZIKV-specific immune responses. The vaccines were all administered by EP-enhanced i.m. injection using CELLECTRA® EP. Among the candidates tested were vaccines encoding consensus sequences of ZIKV structural genes as well as vaccines encoding structural gene sequences from Brazilian ZIKV strains and the MR766 ZIKV strain that originated in Africa. While all of the vaccine candidate tested were immunogenic, the final vaccine that was down-selected was GLS-5700 due to its consistent ability to induce strong, ZIKV-specific humoral and cellular immunity in multiple haplotype mouse immunogenicity studies. The GLS-5700 vaccine contains a synthetic ZIKV prM-E consensus sequence antigen created by aligning the prM and E sequences of multiple ZIKV isolates collected between 1952 and 2015 and determining the consensus nucleotide at each position. Consensus antigens account for genetic changes that appear over time in a pathogen potentially making them more adept at inducing cross-reactive immune responses against multiple diverse strains of a pathogen.
When evaluated in immunocompetent mice, GLS-5700 induced full seroconversion after two immunizations, but a third dose of the vaccine generated the highest antibody levels that were maintained at least one month following the final immunization. In addition to binding to a recombinant ZIKV prME antigen in ELISAs, antibodies induced by GLS-5700 could also bind to ZIKV prME produced in infected cells by Western blot and indirect immunofluorescence analyses. Importantly, the GLS-5700-induced antibody response could neutralize ZIKV infection in vitro with a high titer. Mice receiving three doses of the vaccine also generated a modest cellular response to ZIKV which included polyfunctional T cells [84].
The next step of pre-clinical development for GLS-5700 required a model system to evaluate whether the immune responses generated in mice are able to protect animals from ZIKV infection and/or disease. Previous research on dengue and West Nile viruses indicated that immunocompetent mice did not develop disease following infection, but mice lacking a functioning innate immune system could support flavivirus replication and suffer disease [85]. Based on these results, we set out with collaborators to develop a ZIKV challenge model in mice lacking the interferon α/β receptor (IFNAR−/- or A129) as their inability to respond to type I interferon allows for robust viral replication. We found that infecting these mice with ZIKV by different routes, including intravenous, subcutaneous, intraperitoneal, or intracranial injection, resulted in in vivo viral replication that caused mice to develop disease that could lead to death when high viral challenge doses were used. Signs of disease in ZIKV infected mice include weight loss, decreased mobility, and/or temporary paralysis [48], [85]. Post-mortem examination of infected mice revealed ZIKV-induced neurologic effects that were detectable by histology. Subsequent characterization of this model by our collaborators led to one of the first reports of ZIKV-induced damage to the reproductive system and fertility of male mice [49]. The clearly observable effects of ZIKV infection in the A129 mice made this the ideal model to evaluate the protective efficacy of GLS-5700. Cohorts of A129 mice that received three immunizations and cohorts receiving just a single immunization of GLS-5700 were fully protected from morbidity and mortality following ZIKV-challenge compared to sham-vaccinated cohorts which proved to be a critical milestone in development. Vaccination also lowered viral loads in blood, semen, and other tissues and protected male mice from ZIKV-induced testicular damage. Combined with data from immune competent mice, testing in the A129 model established that GLS-5700-induced immunity could protect against ZIKV-mediated disease, and also suggested that it may also prevent transmission of the virus through lowering viral loads.
Further preclinical testing of GLS-5700 was conducted in a newly developed ZIKV-challenge model in rhesus macaques. While these animals do not develop clinical disease following ZIKV challenge, they support viral replication which can be monitored by performing RT-PCR on blood and other tissues. Immunization of rhesus monkeys with GLS-5700 by CELLECTRA® EP-enhanced i.d. injection induced modest cellular responses after two doses, but robust antibody responses. All monkeys receiving GLS-5700 fully seroconverted after the second immunization and this antibody response was able to neutralize ZIKV-infection in an in vitro assay with a high titer. Passive transfer of immunized monkey sera into A129 mice prior to ZIKV challenge protected them from morbidity and mortality suggesting that the antibody response induced by GLS-5700 was the main driver of protection. Importantly, monkeys vaccinated with GLS-5700 had no, or significantly reduced, viral loads in blood following ZIKV challenge compared to sham-vaccinated animals.
Based on the encouraging preclinical data in animal models, the FDA approved GLS-5700 for clinical testing on June 20, 2016 (NCT02809443), which was nearly seven months after our initial vaccine design/synthesis and the WHO's worldwide warning about ZIKV. Interim results (through Week 14) of the phase I clinical trial of GLS-5700 have been reported [84]. Flavivirus antibody-naïve volunteers in this trial received three doses of either 1 mg or 2 mg of GLS-5700 by intradermal injection followed by CELLECTRA®EP. GLS-5700 was well tolerated without any reported serious adverse events (SAEs). The majority of subjects in each dose group had binding antibody titers to ZIKV-prME after two immunizations, and 100% of subjects had a response after three immunizations. The majority of subjects in each group had significant in vitro neutralizing antibody titers against ZIKV after the third injection. The antibody responses of a majority of patients in each group blocked ZIKV infection of a glioblastoma cell line. The protective capacity of these GLS-5700-induced human immune responses was investigated by passive transfer of serum from immunized subjects into A129 mice prior to a lethal ZIKV challenge. The results of these studies showed that sera collected after the third immunization protected mice from morbidity and mortality following ZIKV challenge. The protective efficacy of the serum transfer had no correlation with its measured in vitro neutralization titer suggesting that the antibodies may engage alternative effector mechanisms to block disease. This data is consistent with reports of vaccines to other flaviviruses and suggests reevaluation of the protective criteria for flavivirus vaccines is important. A follow-on study for GLS-5700 is currently being assessed as part of a double-blind, placebo-controlled study in Puerto Rico, a ZIKV endemic region (NCT02887482). The rapid development timeline of GLS-5700 further highlights the potential of the DNA vaccine platform for meeting the challenge of developing therapies to treat and/or stop the spread of emerging infectious diseases.
8. Future directions
In the past two years, more has been learned about the pathogenesis of ZIKV than in the previous 68 years since its discovery. Once believed to cause only mild, self-limited illness, ZIKV is now known to be a teratogen and a significant risk factor for the development of Guillain-Barre’ syndrome. Important ongoing research is trying to elucidate the etiology and extent of ZIKV-mediated birth defects and the risk factors that lead to them. Although there is no evidence of ZIKV infection affecting sperm development and fertility in human males, the dramatic effects of ZIKV on the genitalia of male mice along with the fact that ZIKV RNA can be detected in sperm for months after infection suggest that further study and evaluation of this phenomenon is warranted. It is also necessary to further understand sexual transmission of ZIKV and how it contributes to ZIKV-mediated congenital abnormalities.
Along with the rapid acquisition of knowledge into the biology of ZIKV infection, there has been a rapid and concerted efforts to develop immunotherapies such as vaccines and mAb therapeutics to prevent and/or treat ZIKV infection. Within seven months of initial vaccine design/synthesis and four months after the WHO declared ZIKV a world health emergency, a collaborative group led by Gene One Life Science and Inovio Pharmaceuticals had a vaccine candidate approved for clinical testing, and initial results suggest that this candidate is safe and immunogenic [84]. Additional candidates using different vaccine platforms have also been developed with some of these now being evaluated clinically. ZIKV-targeting mAbs may be another important weapon for combating infection and disease especially in people who are not good candidates for vaccination, such as pregnant women. Although some mAbs have shown protective efficacy in animal models, much work remains to be done to advance these therapeutics into the clinic such as evaluating the protective dose(s) and assuring that they cannot mediate ADE of ZIKV, DENV, or other flaviviruses. While much work remains, the rapid efforts by scientists and world health agencies to understand ZIKV-infection and develop treatment options against it provide a blueprint for responding to other emerging infectious disease threats.
Conflict of interest
JJK, MJ and JNM are employees of GeneOne Life Science Inc. CCR, SW and JJK are employees of Inovio Pharmaceuticals and as such receive salary and benefits, including ownership of stock and stock options. KM discloses grant funding, industry collaborations, speaking honoraria, and fees for consulting. He has received consulting fees from Inovio Pharmaceuticals related to DNA vaccine development. He has a patent application for DNA vaccine development and delivery of DNA encoded monoclonal antibodies pending to Inovio Pharmaceuticals. Remuneration includes direct payments.
DBW discloses grant funding, SAB and Board service, industry collaborations, speaking honoraria, and fees for consulting. His service includes serving on scientific review committees and advisory boards. Remuneration includes direct payments and/or stock or stock options. He notes potential conflicts associated with this work with Pfizer, Bristol Myers Squibb, Inovio Pharmaceuticals, Merck, VGXI, Geneos, Astrazeneca and potentially others. Licensing of technology from this laboratory has created over 150 jobs in the biotech/pharma industry. The other authors declare no competing financial interests.
Acknowledgements
The authors would like to acknowledge other members of the Weiner laboratory for significant contributions and/or critical reading and editing of the review. K.M. received support from the Wistar Science Discovery Award. KM and DBW also note funding by Inovio Pharmaceuticals Inc. PA, USA and Gene One Life Science Inc. Seoul, Korea, through scientific research agreements with the Wistar Institute.
References
- 1.Musso D., Nilles E.J., Cao-Lormeau V.M. Rapid spread of emerging Zika virus in the Pacific area. Clin Microbiol Infect. 2014;20:O595–O596. doi: 10.1111/1469-0691.12707. [DOI] [PubMed] [Google Scholar]
- 2.Organization PAH Epidemiological Alert: neurological syndrome, congenital malformations, and Zika virus infection. Implic Public Health Am. 2015:1–11. [Google Scholar]
- 3.Musso D., Roche C., Robin E., Nhan T., Teissier A., Cao-Lormeau V.M. Potential sexual transmission of Zika virus. Emerg Infect Dis. 2015;21:359–361. doi: 10.3201/eid2102.141363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brasil P., Pereira J.P., Moreira M.E., Ribeiro Nogueira R.M., Damasceno L., Wakimoto M. Zika Virus Infection in Pregnant Women in Rio de Janeiro. N Engl J Med. 2016;375:2321–2334. doi: 10.1056/NEJMoa1602412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Calvet G., Aguiar R.S., Melo A.S.O., Sampaio S.A., de Filippis I., Fabri A. Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: a case study. Lancet Infect Dis. 2016;16:653–660. doi: 10.1016/S1473-3099(16)00095-5. [DOI] [PubMed] [Google Scholar]
- 6.Xu X., Vaughan K., Weiskopf D., Grifoni A., Diamond M.S., Sette A. Identifying candidate targets of immune responses in Zika virus based on homology to epitopes in other flavivirus species. PLoS Curr. 2016;8 doi: 10.1371/currents.outbreaks.9aa2e1fb61b0f632f58a098773008c4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dick G.W.A. Zika Virus (I). Isolations and serological specificity. Trans R Soc Trop Med Hyg. 1952;46:509–520. doi: 10.1016/0035-9203(52)90042-4. [DOI] [PubMed] [Google Scholar]
- 8.Normile D. Safety concerns derail dengue vaccination program. Science. 2017;358:1514–1515. doi: 10.1126/science.358.6370.1514. [DOI] [PubMed] [Google Scholar]
- 9.Dick G.W.A. Paper: epidemiological notes on some viruses isolated in Uganda (yellow fever, rift valley fever, Bwamba fever, West Nile, Mengo, Semliki forest, Bunyamwera, Ntaya, Uganda S and Zika viruses) Trans R Soc Trop Med Hyg. 1953;47:13–48. doi: 10.1016/0035-9203(53)90021-2. [DOI] [PubMed] [Google Scholar]
- 10.Smithburn K.C. Studies on certain viruses isolated in the tropics of Africa and South America. Immunological reactions as determined by cross-neutralization tests. J Immunol. 1952 Apr;68(4):441–460. [PubMed] [Google Scholar]
- 11.MacNamara F.N. Zika virus: a report on three cases of human infection during an epidemic of jaundice in Nigeria. Trans R Soc Trop Med Hyg. 1954;48:139–145. doi: 10.1016/0035-9203(54)90006-1. [DOI] [PubMed] [Google Scholar]
- 12.Simpson D.I.H. Zika virus infection in man. Trans R Soc Trop Med Hyg. 1964;58:339–348. [PubMed] [Google Scholar]
- 13.Cao-Lormeau V.-M., Blake A., Mons S., Lastère S., Roche C., Vanhomwegen J. Guillain-Barré Syndrome outbreak associated with Zika virus infection in French Polynesia: a case-control study. Lancet. 2016;387:1531–1539. doi: 10.1016/S0140-6736(16)00562-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Faria N.R., da Silva Azevedo R.S., Kraemer M.U.G., Souza R., Cunha M.S., Hill S.C. Zika virus in the Americas: early epidemiological and genetic findings. Science. 2016;352:345–349. doi: 10.1126/science.aaf5036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Faria N.R., Quick J., Claro I.M., Thézé J., de Jesus J.G., Giovanetti M. Establishment and cryptic transmission of Zika virus in Brazil and the Americas. Nature. 2017;546:406–410. doi: 10.1038/nature22401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grubaugh N.D., Ladner J.T., Kraemer M.U.G., Dudas G., Tan A.L., Gangavarapu K. Genomic epidemiology reveals multiple introductions of Zika virus into the United States. Nature. 2017;546:401–405. doi: 10.1038/nature22400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Metsky H.C., Matranga C.B., Wohl S., Schaffner S.F., Freije C.A., Winnicki S.M. Zika virus evolution and spread in the Americas. Nature. 2017;546:411–415. doi: 10.1038/nature22402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thangamani S., Huang J., Hart C.E., Guzman H., Tesh R.B. Vertical transmission of Zika virus in Aedes aegypti mosquitoes. Am J Trop Med Hyg. 2016;95:1169–1173. doi: 10.4269/ajtmh.16-0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weaver S.C., Costa F., Garcia-Blanco M.A., Ko A.I., Ribeiro G.S., Saade G. Zika virus: history, emergence, biology, and prospects for control. Antivir Res. 2016;130:69–80. doi: 10.1016/j.antiviral.2016.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Favoretto S., Araujo D., Oliveira D., Duarte N., Mesquita F., Zanotto P. First detection of Zika virus in neotropical primates in Brazil: a possible new reservoir. bioRxiv. 2016:049395. [Google Scholar]
- 21.Althouse B.M., Vasilakis N., Sall A.A., Diallo M., Weaver S.C., Hanley K.A. Potential for Zika virus to establish a sylvatic transmission cycle in the Americas. PLoS Negl Trop Dis. 2016 doi: 10.1371/journal.pntd.0005055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haddow A.D., Schuh A.J., Yasuda C.Y., Kasper M.R., Heang V., Huy R. Genetic characterization of zika virus strains: geographic expansion of the asian lineage. PLoS Negl Trop Dis. 2012;6(2):e1477. doi: 10.1371/journal.pntd.0001477. Epub 2012 Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dowd K.A., Ko S.-Y., Morabito K.M., Yang E.S., Pelc R.S., DeMaso C.R. Rapid development of a DNA vaccine for Zika virus. Science. 2016 doi: 10.1126/science.aai9137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aliota M.T., Dudley D.M., Newman C.M., Mohr E.L., Gellerup D.D., Breitbach M.E. Heterologous protection against Asian Zika virus challenge in rhesus macaques. PLoS Negl Trop Dis. 2016;10(12):e0005168. doi: 10.1371/journal.pntd.0005168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sirohi D, Chen Z, Sun L, Klose T, Pierson TC, Rossmann MG, et al. The 3.8 Å resolution cryo-EM structure of Zika virus. [DOI] [PMC free article] [PubMed]
- 26.Liu Y., Liu J., Du S., Shan C., Nie K., Zhang R. Evolutionary enhancement of Zika virus infectivity in Aedes aegypti mosquitoes. Nature. 2017 May 25;545(7655):482–486. doi: 10.1038/nature22365. Epub 2017 May 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weaver S.C., Lecuit M. Chikungunya virus and the global spread of a mosquito-borne disease. N Engl J Med. 2015;372:1231–1239. doi: 10.1056/NEJMra1406035. [DOI] [PubMed] [Google Scholar]
- 28.Yuan L., Huang X.-Y., Liu Z.-Y., Zhang F., Zhu X.-L., Yu J.-Y. A single mutation in the prM protein of Zika virus contributes to fetal microcephaly. Science. 2017;358:933–936. doi: 10.1126/science.aam7120. [DOI] [PubMed] [Google Scholar]
- 29.Swanstrom J.A., Plante J.A., Plante K.S., Young E.F., McGowan E., Gallichotte E.N. Dengue virus envelope dimer epitope monoclonal antibodies isolated from dengue patients are protective against Zika virus. mBio. 2016;7 doi: 10.1128/mBio.01123-16. e01123–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hastings A.K., Yockey L.J., Jagger B.W., Hwang J., Uraki R., Gaitsch H.F. TAM receptors are not required for Zika virus infection in mice. Cell Rep. 2017;19:558–568. doi: 10.1016/j.celrep.2017.03.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Richard A.S., Shim B.-S., Kwon Y.-C., Zhang R., Otsuka Y., Schmitt K. AXL-dependent infection of human fetal endothelial cells distinguishes Zika virus from other pathogenic flaviviruses. Proc Natl Acad Sci. 2017;114:2024–2029. doi: 10.1073/pnas.1620558114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meertens L., Labeau A., Dejarnac O., Cipriani S., Sinigaglia L., Bonnet-Madin L. Axl mediates ZIKA virus entry in human glial cells and Modulates innate immune responses. Cell Rep. 2017;18:324–333. doi: 10.1016/j.celrep.2016.12.045. [DOI] [PubMed] [Google Scholar]
- 33.Nowakowski T.J., Pollen A.A., Di Lullo E., Sandoval-Espinosa C., Bershteyn M., Kriegstein A.R. Expression analysis highlights AXL as a candidate Zika virus entry receptor in neural stem cells. Cell Stem Cell. 2016;18:591–596. doi: 10.1016/j.stem.2016.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li F., Wang P.-R., Qu L.-B., Yi C.-H., Zhang F.-C., Tang X.-P. AXL is not essential for Zika virus infection in the mouse brain. Emerg Microbes Infect. 2017;6:e16. doi: 10.1038/emi.2017.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Muthumani K., Griffin B.D., Agarwal S., Kudchodkar S.B., Reuschel E.L., Choi H. In vivo protection against ZIKV infection and pathogenesis through passive antibody transfer and active immunisation with a prMEnv DNA vaccine. NPJ Vaccines. 2016;1:16021. doi: 10.1038/npjvaccines.2016.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bardina S.V., Bunduc P., Tripathi S., Duehr J., Frere J.J., Brown J.A. Enhancement of Zika virus pathogenesis by preexisting antiflavivirus immunity. Science. 2017;356:175–180. doi: 10.1126/science.aal4365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liang Q., Luo Z., Zeng J., Chen W., Foo S.S., Lee S.A. Zika virus NS4A and NS4B proteins deregulate Akt-mTOR Signaling in human fetal neural stem cells to inhibit Neurogenesis and induce Autophagy. Cell Stem Cell. 2016;19:663–671. doi: 10.1016/j.stem.2016.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Honein M.A., Dawson A.L., Petersen E.E., Jones A.M., Lee E.H., Yazdy M.M. Birth defects among fetuses and infants of US women with evidence of possible Zika virus infection during pregnancy. JAMA. 2017;317:59. doi: 10.1001/jama.2016.19006. [DOI] [PubMed] [Google Scholar]
- 39.Lazear H.M., Diamond M.S. Zika virus: new clinical syndromes and its emergence in the western hemisphere. J Virol. 2016;90:4864–4875. doi: 10.1128/JVI.00252-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Coyne C.B., Lazear H.M. Zika virus - reigniting the TORCH. Nat Rev Microbiol. 2016;14:707–715. doi: 10.1038/nrmicro.2016.125. [DOI] [PubMed] [Google Scholar]
- 41.Miner J.J., Cao B., Govero J., Smith A.M., Fernandez E., Cabrera O.H. Zika virus infection during pregnancy in mice causes placental damage and fetal demise. Cell. 2016;165:1081–1091. doi: 10.1016/j.cell.2016.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cugola F.R., Fernandes I.R., Russo F.B., Freitas B.C., Dias J.L.M., Guimarães K.P. The Brazilian Zika virus strain causes birth defects in experimental models. Nature. 2016;534:267–271. doi: 10.1038/nature18296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Adams Waldorf K.M., Stencel-Baerenwald J.E., Kapur R.P., Studholme C., Boldenow E., Vornhagen J. Fetal brain lesions after subcutaneous inoculation of Zika virus in a pregnant nonhuman primate. Nat Med. 2016;22:1256–1259. doi: 10.1038/nm.4193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ventura C.V., Maia M., Travassos S.B., Martins T.T., Patriota F., Nunes M.E. Risk factors associated with the ophthalmoscopic findings identified in infants with presumed Zika virus congenital infection. JAMA Ophthalmol. 2016;134:912. doi: 10.1001/jamaophthalmol.2016.1784. [DOI] [PubMed] [Google Scholar]
- 45.de Miranda H.A., Costa M.C., Frazão M.A.M., Simão N., Franchischini S., Moshfeghi D.M. Expanded Spectrum of congenital ocular findings in microcephaly with presumed Zika infection. Ophthalmology. 2016;123:1788–1794. doi: 10.1016/j.ophtha.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 46.Leal M.C., Muniz L.F., Ferreira T.S.A., Santos C.M., Almeida L.C., Van Der Linden V. Hearing loss in infants with microcephaly and evidence of congenital Zika virus infection — Brazil, November 2015–May 2016. MMWR Morb Mortal Wkly Rep. 2016;65(34):917–919. doi: 10.15585/mmwr.mm6534e3. PMID: 27585248. [DOI] [PubMed] [Google Scholar]
- 47.Govero J., Esakky P., Scheaffer S.M., Fernandez E., Drury A., Platt D.J. Zika virus infection damages the testes in mice. Nature. 2016;540:438–442. doi: 10.1038/nature20556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ma W., Li S., Ma S., Jia L., Zhang F., Zhang Y. Zika virus causes testis damage and leads to male infertility in mice. Cell. 2016;167:1511–1524. doi: 10.1016/j.cell.2016.11.016. e10. [DOI] [PubMed] [Google Scholar]
- 49.Griffin B.D., Muthumani K., Warner B.M., Majer A., Hagan M., Audet J. DNA vaccination protects mice against Zika virus-induced damage to the testes. Nat Commun. 2017;8:1–8. doi: 10.1038/ncomms15743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Atkinson B., Hearn P., Afrough B., Lumley S., Carter D., Aarons E.J. Detection of zika virus in semen. Emerg Infect Dis. 2016:940. doi: 10.3201/eid2205.160107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brooks J.T., Friedman A., Kachur R.E., LaFlam M., Peters P.J., Jamieson D.J. Update: interim guidance for prevention of sexual transmission of Zika virus - United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:323–325. doi: 10.15585/mmwr.mm6529e2. [DOI] [PubMed] [Google Scholar]
- 52.Musso D., Gubler D.J. Zika virus. Clin Microbiol Rev. 2016;29:487–524. doi: 10.1128/CMR.00072-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Harrower J., Kiedrzynski T., Baker S., Upton A., Rahnama F., Sherwood J. Sexual transmission of Zika virus and persistence in semen, New Zealand, 2016. Emerg Infect Dis. 2016:1855–1857. doi: 10.3201/eid2210.160951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Foy B.D., Kobylinski K.C., Foy J.L.C., Blitvich B.J., da Rosa A.T., Haddow A.D. Probable non-vector-borne transmission of Zika virus, Colorado, USA. Emerg Infect Dis. 2011;17:880–882. doi: 10.3201/eid1705.101939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Deckard D.T., Chung W.M., Brooks J.T., Smith J.C., Woldai S., Hennessey M. Male-to-Male sexual transmission of Zika virus — Texas, January 2016. MMWR Morb Mortal Wkly Rep. 2016;65:372–374. doi: 10.15585/mmwr.mm6514a3. [DOI] [PubMed] [Google Scholar]
- 56.Stettler K., Beltramello M., Espinosa D.A., Graham V., Cassotta A., Bianchi S. Specificity, cross-reactivity, and function of antibodies elicited by Zika virus infection. Science. 2016;353:823–826. doi: 10.1126/science.aaf8505. [DOI] [PubMed] [Google Scholar]
- 57.Balmaseda A., Stettler K., Medialdea-Carrera R., Collado D., Jin X., Zambrana J.V. Antibody-based assay discriminates Zika virus infection from other flaviviruses. Proc Natl Acad Sci U S A. 2017;114:8384–8389. doi: 10.1073/pnas.1704984114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dejnirattisai W., Supasa P., Wongwiwat W., Rouvinski A., Barba-Spaeth G., Duangchinda T. Dengue virus sero-cross-reactivity drives antibody-dependent enhancement of infection with zika virus. Nat Immunol. 2016;17:1102–1108. doi: 10.1038/ni.3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rogers T.F., Goodwin E.C., Briney B., Sok D., Beutler N., Strubel A. Zika virus activates de novo and cross-reactive memory B cell responses in dengue-experienced donors. Sci Immunol. 2017;2 doi: 10.1126/sciimmunol.aan6809. eaan6809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Robbiani D.F., Bozzacco L., Keeffe J.R., Khouri R., Olsen P.C., Gazumyan A. Recurrent potent human neutralizing antibodies to Zika virus in Brazil and Mexico. Cell. 2017;169:597–609. doi: 10.1016/j.cell.2017.04.024. e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Collins M.H., McGowan E., Jadi R., Young E., Lopez C.A., Baric R.S. Lack of durable cross-neutralizing antibodies against Zika virus from dengue virus infection. Emerg Infect Dis. 2017;23:773–781. doi: 10.3201/eid2305.161630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Priyamvada L., Quicke K.M., Hudson W.H., Onlamoon N., Sewatanon J., Edupuganti S. Human antibody responses after dengue virus infection are highly cross-reactive to Zika virus. Proc Natl Acad Sci. 2016;113:7852–7857. doi: 10.1073/pnas.1607931113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McCracken M.K., Gromowski G.D., Friberg H.L., Lin X., Abbink P., De La Barrera R. Impact of prior flavivirus immunity on Zika virus infection in rhesus macaques. PLoS Pathog. 2017;13:1–22. doi: 10.1371/journal.ppat.1006487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pantoja P., Pérez-Guzmán E.X., Rodríguez I.V., White L.J., González O., Serrano C. Zika virus pathogenesis in rhesus macaques is unaffected by pre-existing immunity to dengue virus. Nat Commun. 2017;8:15674. doi: 10.1038/ncomms15674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Terzian A.C.B., Schanoski A.S., MTdO Mota, da Silva R.A., Estofolete C.F., Colombo T.E. Viral load and cytokine response profile does not support antibody-dependent enhancement in dengue-primed Zika virus–infected patients. Clin Infect Dis. 2017;65:10–15. doi: 10.1093/cid/cix558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pardy R.D., Rajah M.M., Condotta S.A., Taylor N.G., Sagan S.M., Richer M.J. Analysis of the T Cell response to Zika virus and identification of a novel CD8+ T cell epitope in immunocompetent mice. PLoS Pathog. 2017;13 doi: 10.1371/journal.ppat.1006184. e1006184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Elong Ngono A., Vizcarra E.A., Tang W.W., Sheets N., Joo Y., Kim K. Mapping and role of the CD8+ T cell response during primary Zika virus infection in mice. Cell Host Microbe. 2017;21:35–46. doi: 10.1016/j.chom.2016.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wen J., Tang W.W., Sheets N., Ellison J., Sette A., Kim K. Identification of Zika virus epitopes reveals immunodominant and protective roles for dengue virus cross-reactive CD8+ T cells. Nat Microbiol. 2017;2:17036. doi: 10.1038/nmicrobiol.2017.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grifoni A., Pham J., Sidney J., O'Rourke P.H., Paul S., Peters B. Prior Dengue virus exposure shapes T cell immunity to Zika virus in humans. J Virol. 2017 doi: 10.1128/JVI.01469-17. JVI.01469–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bayer A., Lennemann N.J., Ouyang Y., Bramley J.C., Morosky S., Marques E.T.D.A. Type III interferons produced by human placental trophoblasts confer protection against Zika virus infection. Cell Host Microbe. 2016;19:705–712. doi: 10.1016/j.chom.2016.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hamel R., Dejarnac O., Wichit S., Ekchariyawat P., Neyret A., Luplertlop N. Biology of Zika virus infection in human skin cells. J Virol. 2015;89:8880–8896. doi: 10.1128/JVI.00354-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dang J., Tiwari S.K., Lichinchi G., Qin Y., Patil V.S., Eroshkin A.M. Zika virus depletes neural progenitors in human cerebral organoids through activation of the innate immune receptor TLR3. Cell Stem Cell. 2016;19:258–265. doi: 10.1016/j.stem.2016.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pulendran B. Learning immunology from the yellow fever vaccine: innate immunity to systems vaccinology. Nat Rev Immunol. 2009 doi: 10.1038/nri2629. [DOI] [PubMed] [Google Scholar]
- 74.Yun S.-I., Lee Y.-M. Japanese encephalitis. Hum Vaccines Immunother. 2014;10:263–279. doi: 10.4161/hv.26902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Villar L., Dayan G.H., Arredondo-Garcia J.L., Rivera D.M., Cunha R., Deseda C. Efficacy of a tetravalent dengue vaccine in children in Latin America. N Engl J Med. 2015;372:113–123. doi: 10.1056/NEJMoa1411037. [DOI] [PubMed] [Google Scholar]
- 76.Endy T.P., Nisalak A., Chunsuttitwat S., Vaughn D.W., Green S., Ennis F.A. Relationship of preexisting dengue virus (DV) neutralizing antibody levels to viremia and severity of disease in a prospective cohort study of DV infection in Thailand. J Infect Dis. 2004;189:990–1000. doi: 10.1086/382280. [DOI] [PubMed] [Google Scholar]
- 77.Halai U.A., Nielsen-Saines K., Moreira M.L., de Sequeira P.C., Junior J.P.P., de Araujo Zin A. Maternal Zika virus disease severity, virus load, prior dengue antibodies, and their relationship to birth outcomes. Clin Infect Dis. 2017;65:877–883. doi: 10.1093/cid/cix472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Muthumani K., Falzarano D., Reuschel E.L., Tingey C., Flingai S., Villarreal D.O. A synthetic consensus anti-spike protein DNA vaccine induces protective immunity against Middle East respiratory syndrome coronavirus in nonhuman primates. Sci Transl Med. 2015;7:301ra132. doi: 10.1126/scitranslmed.aac7462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Trimble C.L., Peng S., Kos F., Gravitt P., Viscidi R., Sugar E. A phase I trial of a human papillomavirus DNA vaccine for HPV16+ cervical intraepithelial neoplasia 2/3. Clin Cancer Res. 2009;15:361–367. doi: 10.1158/1078-0432.CCR-08-1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shedlock D.J., Talbott K.T., Cress C., Ferraro B., Tuyishme S., Mallilankaraman K. A highly optimized DNA vaccine confers complete protective immunity against high-dose lethal lymphocytic choriomeningitis virus challenge. Vaccine. 2011;29:6755–6762. doi: 10.1016/j.vaccine.2010.12.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mallilankaraman K., Shedlock D.J., Bao H., Kawalekar O.U., Fagone P., Ramanathan A.A. A DNA vaccine against chikungunya virus is protective in mice and induces neutralizing antibodies in mice and nonhuman primates. PLoS Negl Trop Dis. 2011;5:e928. doi: 10.1371/journal.pntd.0000928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.MacGregor R.R., Boyer J.D., Ugen K.E., Lacy K.E., Gluckman S.J., Bagarazzi M.L. First human trial of a DNA-based vaccine for treatment of human immunodeficiency virus type 1 infection: safety and host response. J Infect Dis. 1998;178:92–100. doi: 10.1086/515613. [DOI] [PubMed] [Google Scholar]
- 83.Shedlock D.J., Aviles J., Talbott K.T., Wong G., Wu S.J., Villarreal D.O. Induction of broad cytotoxic T cells by protective DNA vaccination against Marburg and Ebola. Mol Ther. 2013;21:1432–1444. doi: 10.1038/mt.2013.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tebas P., Roberts C.C., Muthumani K., Reuschel E.L., Kudchodkar S.B., Zaidi F.I. Safety and immunogenicity of an anti–Zika virus DNA vaccine — preliminary report. N Engl J Med. 2017 doi: 10.1056/NEJMoa1708120. NEJMoa1708120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lazear H.M., Govero J., Smith A.M., Platt D.J., Fernandez E., Miner J.J. A mouse model of Zika virus pathogenesis. Cell Host Microbe. 2016;19:720–730. doi: 10.1016/j.chom.2016.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]