Supplemental Digital Content is available in the text.
Abstract
Background:
Daily rounds in many pediatric intensive care units (PICUs) vary in quality, duration, and participation. We hypothesized that implementing structured interdisciplinary bedside rounds (SIBR®) would improve our rounding process.
Methods:
This was a quality improvement initiative in a 25-bed multidisciplinary PICU in a tertiary children’s hospital. Baseline data included rounding duration; participation of nurses, respiratory care practitioners (RCP), parents; and physician order read-back practices. Interventions were implementing pre-rounding huddles, changing the start of the rounding week, and instituting a SIBR model. All staff, consecutive patients and parents participated over 18 months. We used Mann-Whitney, z-test, and t-tests for statistical analysis with a significance level of 0.05. We tracked data with a statistical process control chart.
Results:
Rounds participation increased for nurses (88% to 100%), RCPs (13% to 61%), and families (24% to 49%) (all p <0.001). Physician order read-back increased (41% to 79%) (p<0.001). The median length of stay (LOS) decreased from 2.1 to 1.9 days (p=0.004) with no changes in mortality or readmissions. The proportion of top responses from family surveys increased from 0.69 to 0.76 (p<0.001). PICU rounding duration (minutes/patient) decreased from 17.1 to 11.3. Most resident physicians felt SIBR positively impacted their education (70%), was more effective than rounds without structure (97%), and that family presence positively impacted learning (70%).
Conclusions:
Implementing a SIBR process in our PICU resulted in greater family and staff satisfaction, improved workflow and decreased rounding time by 34% without compromising education. LOS decreased significantly with no increases in mortality or readmissions.
INTRODUCTION
Structured Interdisciplinary Bedside Round ing (SIBR, Emory University, Atlanta, Georgia), first described in 2014 by Dr. Jason Stein at Emory University,1 offers a framework to streamline care for busy inpatient units. During SIBR, key care team players gather around the patient and family, encouraging them to join in the creation of a treatment plan. This rounding structure promotes transparency, improves communication, and levels the playing field for all participants to ask questions and voice concerns in real time. SIBR builds on the earlier idea of Family-Centered Rounds2 (FCRs) by improving efficiency, decreasing physician practice variation, providing a platform for high-value care initiatives, and conducting outcomes research.
Traditional rounds in a fast-paced intensive care unit (ICU) environment are subject to lapses in communication, causing significant potential for errors, delays in care, and great frustration for patients and staff. Studies have shown that communication failures are associated with medical errors and adverse events.3 Without direct contribution by the patient, caregiver, or the bedside nurse, physicians risk missing critical information that may not have been captured in medical records or during prerounding. Even when conducted at the bedside, traditional teaching rounds leave little room for patient or family participation.
Numerous benefits of FCR have been described since the concept was introduced in 2007.2,4,5 By 2010, >44% of pediatric hospitals reported conducting FCR,6 defined as a planned, purposeful discussion, requiring the permission of patients and families and the cooperation of physicians, nurses, and ancillary staff. The American Academy of Pediatrics, the Institute of Medicine, and the Accreditation Council for Graduate Medical Education have endorsed the FCR concept as the preferred rounding model.7,8 In addition to achieving the ultimate goals of improving patient outcomes and overall quality of care,5 FCR fosters communication, enhances the educational experience for medical trainees, and positively impacts family and staff satisfaction.4,9–11
This study sought to evaluate whether the implementation of SIBR as a part of a quality improvement (QI) initiative would enhance the daily rounding process in a busy pediatric ICU (PICU). The primary aim of this study was to improve rounding efficiency by ≥5 minutes per patient within 6 months of the initiative (October 2014) through the implementation of SIBR. Secondary aims included increased interdisciplinary participation and improvement in family satisfaction.
METHODS
This study was a QI initiative implemented in a 25-bed PICU at a tertiary care University Children’s Hospital and level 1 trauma center. Twelve attending physicians and 6 fellows participated in the study. All patients and their parents hospitalized in our PICU during the 18-month study period (February 2014 to August 2015) participated in the interventions. We formed a core PICU QI team, composed of a clinical nurse specialist, nurse educator, lead respiratory care practitioner (RCP), lead nurse, nurse manager, QI department staff, and PICU physicians. Using QI methodology, we identified several leverage points and planned corresponding interventions. The institutional review board reviewed and approved this study.
The initial interventions were a prerounding huddle (June 2014) and a change in the start of the attending service week (July 2014). Prerounding huddles provided an opportunity for the PICU team (lead nurse, lead RCP, attending physician, and fellow) to discuss the overall plan for the day. We reviewed patient acuity, barriers to transfer, potential procedures, admits/transfers, and the rounding plan. Altering the start of the attending week from Monday to Saturday allowed staggering of attending and fellow patient coverage to allow for enhanced transition and continuity of care.
The main intervention was the introduction of the SIBR model (October 2014), adapted to our specific workflow with permission from Dr. Stein. Several months into our QI process, we identified the SIBR model as one that would fit our rounding needs. Hospital administration funded consultation and training by Dr. Stein’s nonprofit team of educators. There were no financial incentives in working with their team. This framework was applied to create a rounding structure that matched the unique demands of the unit (Fig. 1). We developed bedside tools and educational materials for the staff with assistance from Dr. Stein’s team. After implementation, rapid Plan-Do-Study-Act cycles fine-tuned the process. We continued the SIBR model as standard rounding procedure on the unit beyond the study period, including all of 2015.
Fig. 1.
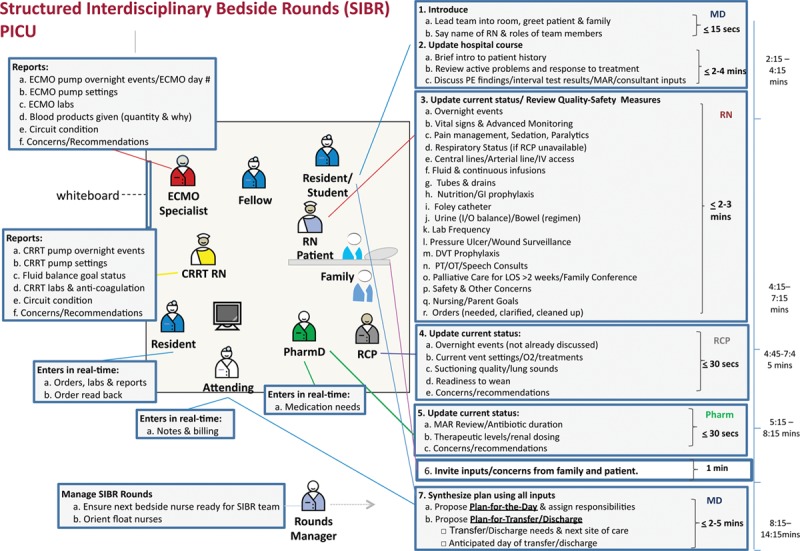
Diagram of SIBR in the PICU. Adapted with permission from Dr. Stein and Centripital. ECMO, extra corporeal membrane oxygenation; CRRT, continuous renal replacement therapy; RN, registered nurse; MD, medical doctor; PE, physical exam; MAR, medication administration record; GI, gastrointestinal; I/O, intake/output; DVT, deep vein thrombosis; PT, physical therapy; OT, occupational therapy; Pharm/Pharm D, pharmacist.
Evaluation Plan and Measurements
Independent observers of daily rounds (PICU fellows, nurses, and medical students) who were not assigned to work in the PICU that day performed data collection. The following data were collected pre- and postintervention: duration of rounds (total time and time per patient), presence and participation of team members in rounds, family experience survey, and percent of physician order read-back. We collected these data from February 2014 to April 2015. Rounding times were determined by dividing the total rounding time by patients rounded on. Rounding data were compiled with weekly or biweekly summaries based on personnel availability. Physician order read-back consisted of resident physicians reading aloud the list of pended electronic orders to ensure that the intended orders were correctly entered before final authentication. Length of stay (LOS), readmission rates, and mortality data were retrieved from Virtual Pediatric Systems (VPS; VPS LLC, Los Angeles, CA), which is a disease registry and collaborative for pediatric critical care. The SIBR model was made standard for the unit, including for all of 2015. Because of this, we compared VPS data from 2013 (baseline) and 2014 (9 months pre-SIBR) to 2015.
Family Experience Survey
We developed an 11-item survey for patients and families (see Supplemental Digital Content 1, Appendix 1, http://links.lww.com/PQ9/A90) based on the pediatric Family Satisfaction in the ICU 24 survey.12 The pediatric Family Satisfaction in the ICU 24 survey has been validated as a psychometrically sound measure of parent satisfaction with their child’s care in the PICU. The survey emphasized assessing communication and perceived involvement in their child’s care. Parents were approached by the bedside nurse to fill out the survey on the day of PICU discharge. Surveys were available in English or Spanish. Parents were asked to place the completed survey in a designated location in the PICU. Responses were kept anonymous.
Resident Physician Education Survey
Second- and third-year resident physicians in pediatrics and emergency medicine rotating in the unit were asked to take an 11-question survey about the impact of SIBR on their educational experience (see Supplemental Digital Content 2, Appendix 2, http://links.lww.com/PQ9/A91). For analysis, we combined all positive responses (very positive + positive), similarly with negative responses and agree/disagree responses.
Statistical Analysis
A control chart was used to show the progression of rounding duration from baseline to postinterventions. We used paired t tests (LOS), 2-sample t tests (family satisfaction survey), and analysis of variance (rounding duration) for statistical analysis with a significance level of 0.05 (Minitab Version 17.3.1, State College, PA, USA). We used Mann-Whitney U test, t test, and chi-square test to evaluate quality measures from the VPS database also with a significance level of 0.05 (R version 3.4.1).
RESULTS
Rounding Efficiency and Quality Metrics
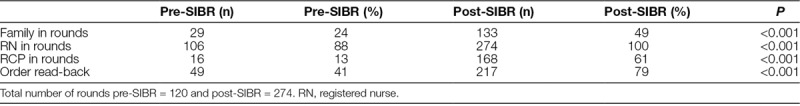
There was a decrease in mean rounding duration (minutes/patient) from a baseline of 17.1 + 2.6 to 12.9 + 4.1 (initial interventions) to 11.3 + 1.9 (post-SIBR implementation). Statistical analysis determined that there were significant differences between baseline rounding duration and the post-SIBR rounding duration after all interventions were implemented (P < 0.001). There was a significant difference between baseline and initial interventions. There was no difference between initial interventions and SIBR implementation. A control chart demonstrated a centerline shift only after the initial interventions occurred and not specifically after SIBR was implemented (Fig. 2). However, special cause variation due to process degradation was detected in September 2014. This degradation resolved after implementation of SIBR. PICU LOS for all patients in the study period decreased significantly. However, there were no significant changes in mortality or unscheduled PICU readmissions within 24 hours (Table 1). Physician order read-back increased from 41% to 79% (P < 0.001) (Table 2).
Fig. 2.
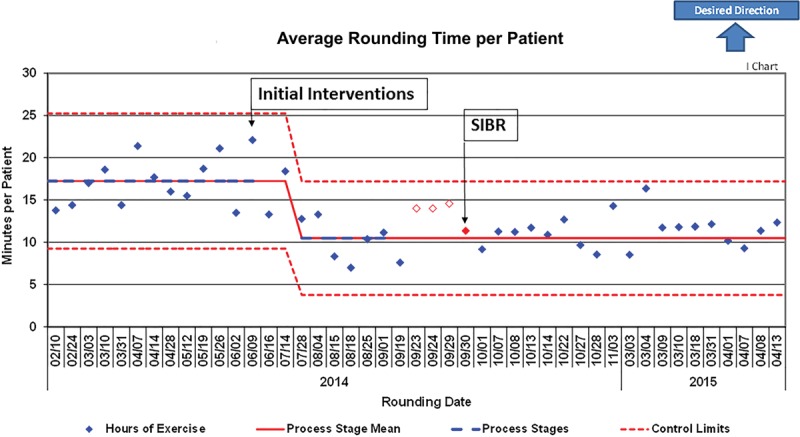
Control chart of average rounding time per patient from baseline to post-SIBR implementation. Red diamonds are points associated with special cause variation.
Table 1.
Lengths of Stay, Mortality Ratios, and Unscheduled PICU Readmissions for 2013–2014 and 2015
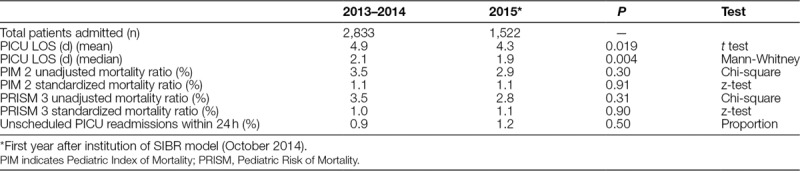
Table 2.
Percent of Involvement and Order Read-Back During Rounds (Pre- and Post-SIBR Implementation)
Interdisciplinary and Family Participation in Rounds
Among the 475 patient encounters, there was a significant increase in family participation (24%–49%), nurse participation (88%–100%), and RCP participation (13%–61%) in daily bedside rounds (Table 2).
Family Experience
There were 172 responses to the family survey preintervention and 254 postintervention with a significant increase in the proportion of top responses postintervention from 0.69 to 0.76 (P < 0.001 for 1,848 preintervention and 2,752 postintervention total question responses) (Fig. 3).
Fig. 3.
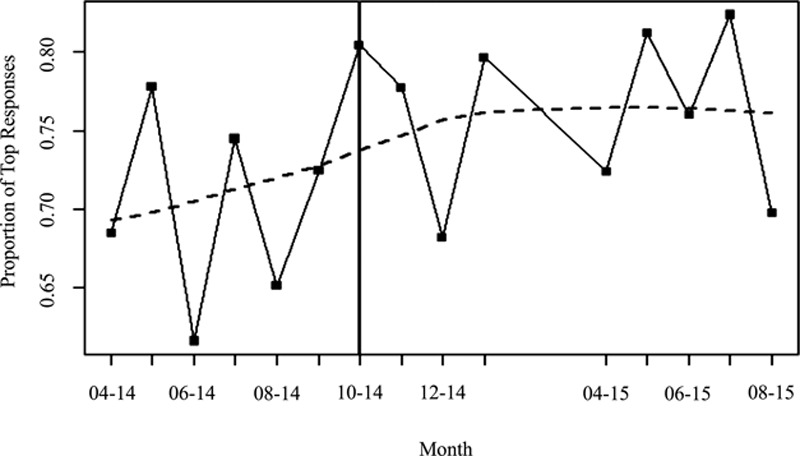
Family experience survey. Proportion of top responses in family survey increased from 0.69 to 0.76 (P < 0.001). Vertical line on 10–14 indicates implementation of SIBR.
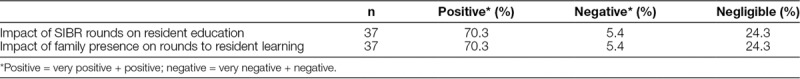
Resident Physician Education
A total of 37 resident physicians completed the 11-question survey on the impact of SIBR on their education. The response rate was 60% for the study period with a total of 62 residents rotating through the PICU during that time. Most resident physicians who responded felt that SIBR positively impacted their education, family presence positively impacted learning (Table 3), and SIBR was more effective than rounds without structure (see Supplemental Digital Content 3, Table 1, http://links.lww.com/PQ9/A92).
Table 3.
Resident SIBR Survey on Perceived Impact of Rounds and Family Presence
DISCUSSION
Daily rounds in our PICU lacked a set format and varied in quality, duration, and participation. Implementation of a structured, interdisciplinary rounding process improved many facets of our PICU performance, including unit workflow, family and staff satisfaction without having a negative impact on perceived resident education. We saw that our LOS decrease significantly without an increase in mortality or unscheduled readmissions. We hypothesize that these positive changes were associated with enriched communication as seen in previous studies.3,13
A key benefit of SIBR is fostering effective, accurate, and timely communication by bringing together team members with the patient and family at the same time and place. It promotes shared situational awareness and is essential to delivering high-quality care. Improved team communication and staff satisfaction have been documented as benefits of FCR and other explicitly structured rounds.14,15
A growing body of evidence shows that active participation by nurses, RCPs, and pharmacists on rounds leads to increased understanding of patient care goals and plans, requiring fewer clarifications and reducing the potential for error.16–18 In addition to improved care coordination, this interdisciplinary approach upgrades team dynamics, leading to greater staff satisfaction.19 Moreover, positive effects of multidisciplinary rounds can translate into reduced mortality in adult medical ICUs, as demonstrated in a study of 112 hospitals (107,324 patients)20 and a survival benefit in surgical ICU patients (60,330 patients).21 Previously reported barriers to nursing participation on rounds included uncertainty about how much physicians value nurse opinions and not knowing a specific time when rounds would be conducted for their patient.22 Making an explicit rounding plan during the morning huddle enabled our nurses to incorporate rounds into their workflow. Centering patient presentations around the nurses’ report of subjective and objective data empowered nurses to share insights and help guide treatment plans.
The results demonstrate better interdisciplinary involvement on all levels, but the most dramatic change involved RCPs (from 13% to 63%). In our PICU, RCPs have greater patient ratios than nursing, making it more challenging to participate in rounds for their patients. Their input is invaluable for patients with complex ventilator or nebulization needs. Although nursing participation was already high (88%–100%), most importantly, the perception of the quality of nursing contribution improved because they were given a defined role.
Promoting closed-loop communication was one way in which engaging team members from different disciplines improved rounding efficiency. We achieved this result by incorporating read-back of all physician orders into the rounding structure. This change increased order read-back practice from 41% to 79%. A consistent order read-back process can be a useful error prevention tool with complex patients and computerized physician order entry.
Introducing explicit structures to our process decreased rounding time by 34% without compromising the quality of patient care or teaching. Although the standardized rounding structure was our main intervention, it is apparent that the whole process contributed to the change. The interventions in the preplanning stage (prerounding huddle and changing the start of the rounding week) significantly impacted rounding efficiency. These were important parts of the process that sequentially laid the foundation for SIBR to be effective and may have contributed more to the overall decrease in rounding duration because of improved team situational awareness and continuity of care. Figure 2 demonstrates a centerline shift after the initial interventions, but not specifically post-SIBR. However, introduction of SIBR appeared to resolve the special cause degradation noted during September 2014. Similar to previous reports, we accomplished these results by standardizing each team members’ role and order of discussion.23 With the implementation of structured FCR and cutting down on nonessential activities during rounds, Vats et al24 demonstrated a reduction in overall rounding time. This finding translated to a reduction in attending physician working hours from 7.55 to 4.03. In our unit, reduced rounding time improved efficiency by reducing variability in attending physician rounding styles and allowed for better planning of patient care activities and didactics.
We achieved shorter rounds even as family participation increased. Apprehensions about time management were common among our staff and have been reported in the literature as one of the barriers to FCR.25 Modest increases in rounding times have been reported to be associated with increased family participation.26,27 However, a 2010 survey of 265 US and Canadian hospitals by the Pediatric Research in Inpatient Settings network disputed the concern that FCR requires more time by showing that higher daily census and academic environment, not FCR, were significantly associated with longer rounding duration.15 One PICU study concluded that the benefits of FCR outweighed the slightly longer times.27 Shorter rounds significantly improved the overall workflow in our unit, allowing more time for new admissions, procedures, family conferences, and teaching. We found that our overall PICU LOS decreased significantly without increasing mortality or readmission rates.
In the past decade, many studies confirmed that engaging parents in decision-making activities, such as daily rounds, universally enhances patient and family experience.4,28 We observed that as family participation increased, family satisfaction improved as well. We received a significantly higher number of top responses on the family survey in addition to several comments on how important and educational it was for them to be included in rounds. Many families wish to participate in hospital rounds,4,29 and studies demonstrate the benefits of the shared decision-making model. Parents value an opportunity to contribute information and concerns as staff formulate treatment plans.2,4,28 Participating in the discussion and witnessing the decision-making process instills confidence and fosters a more trusting relationship with the medical team. Not surprisingly, several studies, including the only randomized trial of family-centered versus “conference room” rounds performed in Canada,30 supported our findings by showing that effective communication between patients and providers strongly correlates with overall quality-of-care ratings and family satisfaction.28,31
We are just beginning to explore factors that maximize family participation. For example, a study in a tertiary care PICU revealed that demographics such as race, educational level, ages of children or family members, and if the family member was a medical professional had no association with whether a family chose to attend rounds.32 Another study suggested that special consideration should be given on the first day of admission, as parents seemed to be more likely to have privacy concerns during FCR and were less likely to ask questions and understand the plan of care.4 All these factors point to the importance of situational awareness during FCR, paying close attention to the cognitive abilities of the patient and family, their emotional states, immediate physical environments, and timing of any given rounding encounter.33
The bedside is an ideal setting for trainees to refine their patient examination and interaction skills under direct observation with the opportunity for immediate feedback.34 In turn, attending physicians and experienced nurses can model compassion, professionalism, and demonstrate effective patient and team communication. Thus, SIBR is an indispensable teaching instrument. Most of the surveyed residents (70%) perceived that SIBR had a positive impact on their education and 97% considered it more effective than rounds without a structure.
In their comments, the residents recognized several benefits of SIBR including less time spent for order clarification after rounds due to read-backs, streamlined workflow, and more emphasis on synthesizing data, rather than reporting which is now done mostly by nurses. Some echoed concerns from other studies that if residents are unsure about the diagnosis or treatment plans, families may lose confidence in the resident and team. However, families stated in surveys that they appreciated being included in the interdisciplinary rounds and even found them educational.
Despite recognizing the need for more shared decision-making and the benefits of family presence on rounds, some studies report that resident physicians feel that parental presence leads to less teaching4 and may limit discussion during rounds which could adversely affect patient care.28 In contrast, most of the residents who responded (70%) felt that family presence positively affected their education. Only 5% felt negative effects, and 24% stated that there were negligible effects. This finding is consistent with other studies where residents find valuable nondidactic learning by seeing how attending physicians interact with other team members and families.25
Study Limitations
The results are limited to a single center and are not adjusted for illness severity, which may correlate with duration and style of rounds. The presence of independent observers on rounds may have potentially affected rounding behavior. Other objective patient outcome measures such as a central line or urinary catheter infection rates were not specifically studied as the baseline levels were low. The PICU pharmacists have been an integral part of the rounding team even before SIBR interventions. They had been present in rounds as part of their weekday workflow, but we did not measure their participation rate in rounds before or after any interventions. Language barriers led to the biggest limitation in evaluating family presence during rounds. Approximately one-third of the patients in Loma Linda’s PICU are primarily non-English speaking and have limited ability to participate in SIBR. Family language preference was not specified when collecting data, and we were unable to determine to what extent language barriers deterred family involvement in rounds. Although residents felt that SIBR rounds contributed in a positive way toward their education, this was not measured with any objective testing. The resident survey was not validated—which could potentially yield inaccurate results.
Future Directions
The benefits of family-centered care are undeniable. As hospitals adopt the shared decision-making mindset, the question is no longer whether to conduct FCR, but how to do it efficiently. The goals may include developing FCR “best practices” for individual programs, identifying barriers for nursing or family participation, partnering with language services, and creating models for faculty development programs. Research is necessary to develop valid tools that assess family-centered and interdisciplinary care. Finally, studies could look at how the SIBR framework affects medical outcomes, safety, resource utilization, and costs.
CONCLUDING SUMMARY
Implementation of a SIBR process improves the quality of rounds in a PICU as evidenced by expanded interdisciplinary participation, more consistent read-back of physician orders, and improved family satisfaction. As a result of all interventions, efficiency increased with shorter rounding times per patient and significantly decreased lengths of PICU stay. Consistent rounding structure and family participation during PICU rounds positively impact resident perception of their education.
ACKNOWLEDGMENTS
The authors are grateful to our medical students, residents, fellows, attendings, and pediatric intensive care unit staff (nurses, respiratory care practitioners, and pharmacists) for assistance with the study.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online May 16, 2019.
Preliminary data presented at the American Academy Section on Critical Care, Oral Abstract Session I, Washington, DC, October 26, 2015.
During the quality improvement process, hospital administration funded Structured Interdisciplinary Bedside Rounds training for staff by a nonprofit team of physician and nurse educators at Centripital (Atlanta, GA). For more information, please contact jason.stein@centripital.org.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
To cite: Lopez M, Vaks Y, Wilson M, Mitchell K, Lee C, Ejike J, Oei G, Kaufman D, Hambly J, Tinsley C, Bahk T, Samayoa C, Pappas J, Abd-Allah S. Impacting Satisfaction, Learning, and Efficiency Through Structured Interdisciplinary Rounding in a Pediatric Intensive Care Unit: A Quality Improvement Project. Pediatr Qual Saf 2019;3:e176.
REFERENCES
- 1.Stein J, Payne C, Methvin A, et al. Reorganizing a hospital ward as an accountable care unit. J Hosp Med. 2015;10:36–40. [DOI] [PubMed] [Google Scholar]
- 2.Muething SE, Kotagal UR, Schoettker PJ, et al. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119:829–832. [DOI] [PubMed] [Google Scholar]
- 3.Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79:186–194. [DOI] [PubMed] [Google Scholar]
- 4.Aronson PL, Yau J, Helfaer MA, et al. Impact of family presence during pediatric intensive care unit rounds on the family and medical team. Pediatrics. 2009;124:1119–1125. [DOI] [PubMed] [Google Scholar]
- 5.Mittal V. Family-centered rounds: a decade of growth. Hosp Pediatr. 2014;4:6–8. [DOI] [PubMed] [Google Scholar]
- 6.Sisterhen LL, Blaszak RT, Woods MB, et al. Defining family-centered rounds. Teach Learn Med. 2007;19:319–322. [DOI] [PubMed] [Google Scholar]
- 7.Committee on Hospital Care and Institute For Patient- and Family-Centered Care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129:394–404. [DOI] [PubMed] [Google Scholar]
- 8.Mittal V. Family-centered rounds. Pediatr Clin North Am. 2014;61:663–670. [DOI] [PubMed] [Google Scholar]
- 9.Ingram TC, Kamat P, Coopersmith CM, et al. Intensivist perceptions of family-centered rounds and its impact on physician comfort, staff involvement, teaching, and efficiency. J Crit Care. 2014;29:915–918. [DOI] [PubMed] [Google Scholar]
- 10.Phipps LM, Bartke CN, Spear DA, et al. Assessment of parental presence during bedside pediatric intensive care unit rounds: effect on duration, teaching, and privacy. Pediatr Crit Care Med. 2007;8:220–224. [DOI] [PubMed] [Google Scholar]
- 11.Subramony A, Hametz PA, Balmer D. Family-centered rounds in theory and practice: an ethnographic case study. Acad Pediatr. 2014;14:200–206. [DOI] [PubMed] [Google Scholar]
- 12.Epstein D, Unger JB, Ornelas B, et al. Psychometric evaluation of a modified version of the family satisfaction in the ICU survey in parents/caregivers of critically ill children*. Pediatr Crit Care Med. 2013;14:e350–e356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Joint Commission. Sentinel Event Data - Event Type by Year. Available at: https://www.jointcommission.org/sentinel_event.aspx. Accessed October 18, 2017.
- 14.Dodek PM, Raboud J. Explicit approach to rounds in an ICU improves communication and satisfaction of providers. Intensive Care Med. 2003;29:1584–1588. [DOI] [PubMed] [Google Scholar]
- 15.Mittal VS, Sigrest T, Ottolini MC, et al. Family-centered rounds on pediatric wards: a PRIS network survey of US and Canadian hospitalists. Pediatrics. 2010;126:37–43. [DOI] [PubMed] [Google Scholar]
- 16.Gausvik C, Lautar A, Miller L, et al. Structured nursing communication on interdisciplinary acute care teams improves perceptions of safety, efficiency, understanding of care plan and teamwork as well as job satisfaction. J Multidiscip Healthc. 2015;8:33–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rehder KJ, Uhl TL, Meliones JN, et al. Targeted interventions improve shared agreement of daily goals in the pediatric intensive care unit. Pediatr Crit Care Med. 2012;13:6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vazirani S, Hays RD, Shapiro MF, et al. Effect of a multidisciplinary intervention on communication and collaboration among physicians and nurses. Am J Crit Care. 2005;14:71–77. [PubMed] [Google Scholar]
- 19.Deitrick LM, Baker K, Paxton H, et al. Hourly rounding: challenges with implementation of an evidence-based process. J Nurs Care Qual. 2012;27:13–19. [DOI] [PubMed] [Google Scholar]
- 20.Kim MM, Barnato AE, Angus DC, et al. The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med. 2010;170:369–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoo EJ, Edwards JD, Dean ML, et al. Multidisciplinary critical care and intensivist staffing: results of a statewide survey and association with mortality. J Intensive Care Med. 2016;31:325–332. [DOI] [PubMed] [Google Scholar]
- 22.Sharma A, Norton L, Gage S, et al. A quality improvement initiative to achieve high nursing presence during patient- and family-centered rounds. Hosp Pediatr. 2014;4:1–5. [DOI] [PubMed] [Google Scholar]
- 23.Tripathi S, Arteaga G, Rohlik G, et al. Implementation of patient-centered bedside rounds in the pediatric intensive care unit. J Nurs Care Qual. 2015;30:160–166. [DOI] [PubMed] [Google Scholar]
- 24.Vats A, Goin KH, Villarreal MC, et al. The impact of a lean rounding process in a pediatric intensive care unit. Crit Care Med. 2012;40:608–617. [DOI] [PubMed] [Google Scholar]
- 25.Rappaport DI, Cellucci MF, Leffler MG. Implementing family-centered rounds: pediatric residents’ perceptions. Clin Pediatr (Phila). 2010;49:228–234. [DOI] [PubMed] [Google Scholar]
- 26.Levin AB, Fisher KR, Cato KD, et al. An evaluation of family-centered rounds in the PICU: room for improvement suggested by families and providers. Pediatr Crit Care Med. 2015;16:801–807. [DOI] [PubMed] [Google Scholar]
- 27.Gupta PR, Perkins RS, Hascall RL, et al. The effect of family presence on rounding duration in the PICU. Hosp Pediatr. 2017;7:103–107. [DOI] [PubMed] [Google Scholar]
- 28.Cameron MA, Schleien CL, Morris MC. Parental presence on pediatric intensive care unit rounds. J Pediatr. 2009;155:522–528. [DOI] [PubMed] [Google Scholar]
- 29.Rotman-Pikielny P, Rabin B, Amoyal S, et al. Participation of family members in ward rounds: attitude of medical staff, patients and relatives. Patient Educ Couns. 2007;65:166–170. [DOI] [PubMed] [Google Scholar]
- 30.Landry MA, Lafrenaye S, Roy MC, Cyr C. A randomized, controlled trial of bedside versus conference-room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120:275–280. [DOI] [PubMed] [Google Scholar]
- 31.Homer CJ, Marino B, Cleary PD, et al. Quality of care at a children’s hospital: the parent’s perspective. Arch Pediatr Adolesc Med. 1999;153:1123–1129. [DOI] [PubMed] [Google Scholar]
- 32.Drago MJ, Aronson PL, Madrigal V, et al. Are family characteristics associated with attendance at family centered rounds in the PICU? Pediatr Crit Care Med. 2013;14:e93–e97. [DOI] [PubMed] [Google Scholar]
- 33.Beck J, Meyer R, Kind T, et al. The importance of situational awareness: a qualitative study of family members’ and nurses’ perspectives on teaching during family-centered rounds. Acad Med. 2015;90:1401–1407. [DOI] [PubMed] [Google Scholar]
- 34.Jouriles NJ, Emerman CL, Cydulka RK. Direct observation for assessing emergency medicine core competencies: interpersonal skills. Acad Emerg Med. 2002;9:1338–1341. [DOI] [PubMed] [Google Scholar]


