Abstract
Bacteria from the species Trueperella pyogenes are a part of the biota of skin and mucous membranes of the upper respiratory, gastrointestinal, or urogenital tracts of animals, but also, opportunistic pathogens. T. pyogenes causes a variety of purulent infections, such as metritis, mastitis, pneumonia, and abscesses, which, in livestock breeding, generate significant economic losses. Although this species has been known for a long time, many questions concerning the mechanisms of infection pathogenesis, as well as reservoirs and routes of transmission of bacteria, remain poorly understood. Pyolysin is a major known virulence factor of T. pyogenes that belongs to the family of cholesterol-dependent cytolysins. Its cytolytic activity is associated with transmembrane pore formation. Other putative virulence factors, including neuraminidases, extracellular matrix-binding proteins, fimbriae, and biofilm formation ability, contribute to the adhesion and colonization of the host tissues. However, data about the pathogen–host interactions that may be involved in the development of T. pyogenes infection are still limited. The aim of this review is to present the current knowledge about the pathogenic potential and virulence of T. pyogenes.
Keywords: Trueperella pyogenes, virulence, pyolysin, infection, pathogenicity, immune response, Actinomycetales
1. Introduction
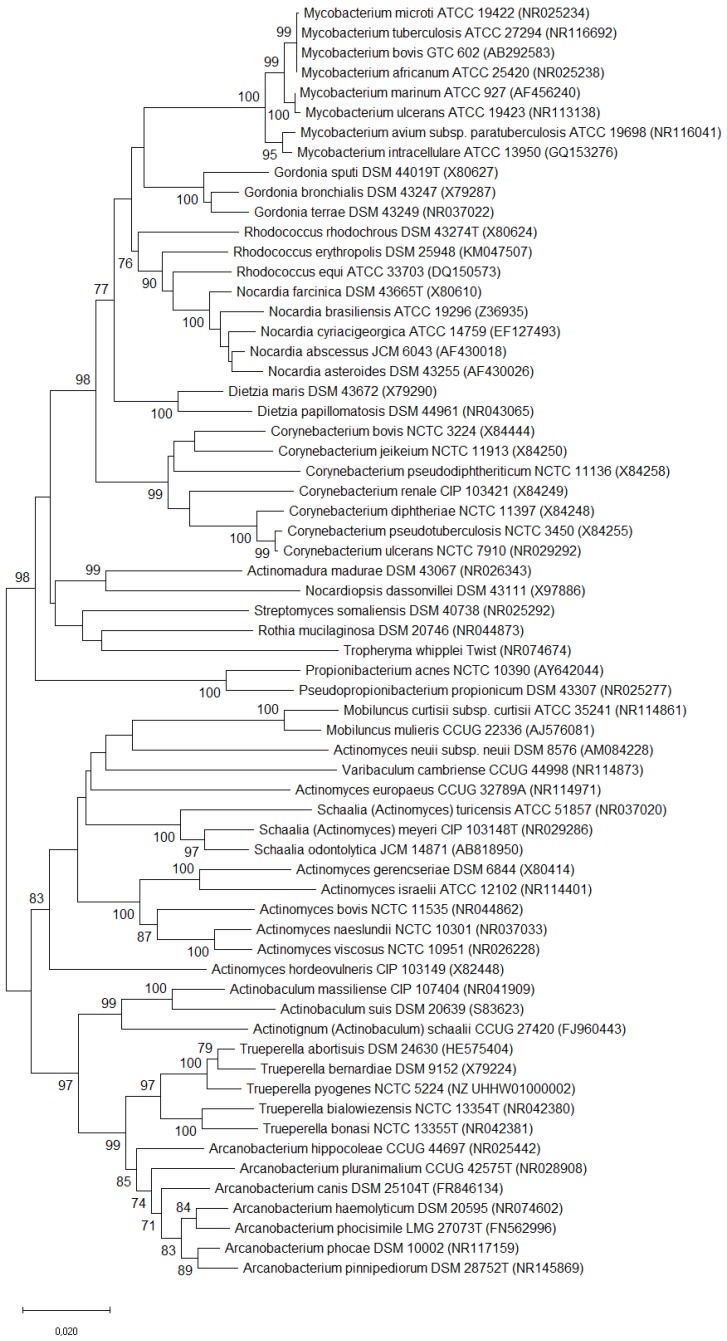
The species Trueperella pyogenes [1], previously classified as Arcanobacterium pyogenes [2], Actinomyces pyogenes [3,4], and formerly as Corynebacterium pyogenes [5], belongs to the family Actinomycetaceae, in the order Actinomycetales of the class Actinobacteria, the so-called actinomycetes [6]. A dendrogram representing the phylogenetic relationship between this bacterium and some other pathogenic Actinomycetales is shown in Figure 1. T. pyogenes is a Gram-positive, pleomorphic, non-spore-forming, non-motile, non-capsulated, facultatively anaerobic rod, which is characterized by a fermentative metabolism and strong proteolytic activity [4]. Its growth requirements are not excessive, but media enriched with blood or serum need to be used for the culture. The preliminary recognition of T. pyogenes isolates is based on the cell morphology; the features of colonies, which are surrounded by a zone of beta-haemolysis on blood agar; and a negative catalase assay. Then, the biochemical properties can be tested for species determination [7]. Sometimes, additional bacteriological methods other than the conventional ones are necessary for the differentiation and appropriate identification of isolates. New techniques, such as loop-mediated isothermal amplification (LAMP) assay, matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry, Fourier transform infrared (FT-IR) spectroscopy, or 16S rRNA gene sequencing may be useful for the diagnostics of T. pyogenes infections [8,9,10,11,12,13]. Those methods enable the recognition of the closely related taxa of the order Actinomycetales, and sometimes the reclassification of some of them [14].
Figure 1.
Neighbor-joining [15,16] phylogenetic tree based on 16S rRNA gene sequences (a total of 1422 positions in the final dataset) of Trueperella pyogenes, other Trueperella species, and related taxa. Only bootstrap values of 70%, based on 1000 replicates, are shown next to the branches [17]. The scale bar represents the number of substitutions per site. The analysis involved 64 nucleotide sequences derived from the GenBank® database, and the evolutionary relationships were calculated in MEGA X [18].
T. pyogenes is considered to be a part of the biota of skin and mucous membranes of the upper respiratory and urogenital tracts of animals [19,20,21]. Moreover, this bacterium was also isolated from the wall of bovine rumen and swine stomachs, as a gastrointestinal microbiota [22,23], and from the udders of clinically healthy cows [24]. However, T. pyogenes is also an important opportunistic pathogen. This species, like other well-known actinomycetes, such as Corynebacterium pseudotuberculosis or Rhodococcus equi, is an etiological agent of common suppurative infections in animals. In the case of C. pseudotuberculosis, the highest susceptibility to the infection is observed in small ruminants, and abscesses are located mainly in the lymph nodes [25,26]. R. equi is a cause of pyogenic infections, mostly in horses, and lesions are found mainly in the respiratory tract [27,28]. Whereas T. pyogenes is pathogenic for a variety of animal species, and purulent or necrotic lesions may occur in different host tissues. Interestingly, there were no relationships found between the virulence gene profiles of T. pyogenes strains and their origin, a type of infection and a host [13,21,29,30,31]. However, Ashrafi Tamai et al. [32] reported a significant association between the virulence genotypes and clonal types of T. pyogenes isolates, and the severity of the clinical symptoms in postpartum cows with metritis.
Although T. pyogenes is a bacterium that has been known of for a long time, many questions concerning the mechanisms of infection pathogenesis, as well as its reservoirs and routes of transmission, still remain poorly understood. The aim of this review is to present the current knowledge about the pathogenicity and virulence potential of this opportunistic animal pathogen.
2. Pathogenicity
T. pyogenes infections occur in both domestic and wild animals worldwide, but are rare in humans. The prevalence of T. pyogenes isolation may differ, depending on a host species and a geographic region. The majority of published data concerns T. pyogenes infections in food animals and comes from Europe [21,33,34,35,36,37,38], China [39,40,41,42,43], Japan [44,45], Brazil [30,46], and the United States [47,48,49,50]. In livestock, the diseases caused by T. pyogenes generate significant economic losses, mainly in cattle and swine breeding, causing a reduction of meat and milk yield, as well as decreased reproductive efficiency and sometimes the necessity to cull diseased animals. The clinical course of these suppurative infections may be severe, with different mortality rates, which increase in the case of misdiagnosis or inappropriate treatment. Beta-lactams, tetracyclines, and macrolides are the antibiotics most often used to treat T. pyogenes infections. A question of the therapy efficacy is especially important, as the antimicrobial resistance in T. pyogenes becomes an emerging problem because of the common use of these drugs in agriculture [29,32,34,39,40,42,44,47,49,51,52].
Generally, the infections caused by T. pyogenes have an opportunistic nature, in which adverse environmental and host-related factors play a relevant role in the disease establishment [45,50,53,54]. Nevertheless, the risk factors of the infection development are sometimes difficult to estimate. Curiously, there are no obvious differences observed between the virulence genotypes of commensal and clinical T. pyogenes isolates, although, in some investigations, a gene encoding one of the virulence determinants, fimbria A, was found more frequently in the isolates obtained from infected cows than from healthy ones [49,55]. However, the in vitro study of Ibrahim et al. [56] showed significant differences in the expression level of eight known virulence genes in T. pyogenes isolated from the uterus of a cow with clinical endometritis, and the isolate from the uterus of a healthy cow. This indicates the importance of the regulatory mechanisms of the virulence gene expression in the infection development, which can be also demonstrated in an example of the pyolysin gene expression [57]. In other study, a relationship between the clonal types of isolates and their origin, from a diseased or healthy host, was noted [21]. All of these findings suggest that other unknown bacterial factors may also contribute to the establishment and development of the T. pyogenes infection.
T. pyogenes may cause infection as a primary etiological agent, but more frequently, this species is involved in polymicrobial diseases, such as mastitis [45], uterine infections [55], interdigital phlegmon [58], or liver abscesses [59]. This bacterium may be recovered from a mix infection of various bacterial species, but especially frequently with Gram-negative anaerobes, such as Fusobacterium necrophorum, Bacteroides spp., or Peptoniphilus (formerly Peptostreptococcus) indolicus. In these cases, purulent and necrotic lesions are usually observed, leading to systemic signs and resulting in animal death. A particularly strong synergistic interaction occurs between T. pyogenes and F. necrophorum [60]. It consists in the stimulation of F. necrophorum growth by a diffusible and heat-labile product of T. pyogenes, which probably decreases the oxygen pressure and the oxidation-reduction potential in a site of infection, generating conditions advantageous for this anaerobe [61]. On the other hand, a leukotoxin produced by F. necrophorum protects T. pyogenes against phagocytosis, because of its ability to lysis leukocytes or to induce their apoptosis, depending on its concentration [59]. Moreover, lactic acid, which is a metabolic product of T. pyogenes, can be used by F. necrophorum as an energy substrate. Other bacteria, especially Escherichia coli, are also often associated with T. pyogenes co-infections, mostly postpartum uterine infections [55,62,63]. However, the synergistic effect between both of these bacteria is not evident. The findings of Zhao et al. [64] indicated that N-acyl homoserine lactones from E. coli and Pseudomonas aeruginosa, which act as the quorum-sensing (QS) signal molecules, can inhibit the growth and virulence of T. pyogenes in vitro. The recent in vivo study of Huang et al. [65], conducted in a mouse model, confirmed these observations.
2.1. T. pyogenes Infections in Animals
In livestock, T. pyogenes infections occur mainly in cattle, swine, sheep, and goats, rarely in horses or birds, and are often associated with heavy economic losses.
In cattle, T. pyogenes mainly causes infections of the reproductive tract and the mammary gland, as well as pneumonia and liver abscessation. The most prevalent diseases in dairy cows related with this bacterium are metritis and endometritis, which may develop in a clinical form in about 23–52% of animals after parturition [29,32,38,39,66]. T. pyogenes together with many other bacteria comprises a vaginal biota of healthy cows [67], and may also colonize and persist in the uterus of dairy cows with normal puerperium [21,38]. However, as an opportunistic pathogen, this bacterium can invade the distant parts of the reproductive tract, especially after parturition, when the protective epithelium of the endometrium is disrupted, and it can also increase the influx of inflammatory cells in these tissues [50,68]. The presence of T. pyogenes in the endometrium is correlated with the damage of the tissue because of the cytolytic activity of the pyolysin against the endometrial stromal cells, which are particularly sensitive to this cholesterol-dependent toxin [68,69]. The ability of T. pyogenes to produce inflammatory lesions in the endometrium was confirmed by the findings of Lima et al. [70]. They noted that after the intrauterine infusion of T. pyogenes suspension containing 109 colony-forming units/mL, moderate to severe endometrial inflammation developed in the studied cows, and additionally, premature luteolysis was observed in some animals. The uterine inflammation, usually later postpartum, associated with T. pyogenes, has a form of subclinical or clinical endometritis, and may reduce the reproductive performance and milk yield [63,71,72]. Bonnett et al. [73] noted that cows with T. pyogenes infection took significantly longer to conceive. Moreover, the study of Boer et al. [63] demonstrated that T. pyogenes isolation at day 21 postpartum was associated with the subsequent diagnosis of purulent vaginal discharge, and this observation was confirmed by Sheldon et al. [74]. T. pyogenes can also have a lethal impact on the oviductal epithelial cells, as it was demonstrated by Mesgaran et al. [75] in the in vitro study. In general, in the cows infected by T. pyogenes, an increased prevalence of clinical endometritis is observed [50]. Frequently, uterine disorders are from co-infections with T. pyogenes and other bacteria, such as E. coli, Streptococcus spp., Staphylococcus spp., Fusobacterium spp., Prevotella spp., and Clostridium spp. [39,55,62,71,76,77,78]. Such polymicrobial uterine infections, especially those with anaerobes, result in an increased purulent secretion and higher severity of lesions [76,79]. The problems regarding parturition, the subsequent negative energy balance, or hyperketonemia are considered to be important risk factors for these diseases [63,80].
Another important and common T. pyogenes infection in cattle is mastitis, which may affect lactating and dry cows, as well as heifers [30,37,43,45,46,81,82,83,84]. T. pyogenes is well known as one of the crucial agents of polymicrobial infection, called summer mastitis, which occurs mainly in pastured cows during the summer, and is associated with pathogen transmission by an insect, Hydrotaea irritans [85,86]. However, Madsen et al. [87] demonstrated no differences in the rates of T. pyogenes isolation from the mastitis cases in stabled and pastured cattle. Similarly, Ribeiro et al. [46] and Ishiyama et al. [45] did not observe a seasonality of the T. pyogenes mastitis occurrence during their long-term survey of the disease. Moreover, it was reported that T. pyogenes alone can cause clinical mastitis called pyogenes mastitis, even with a high severity of symptoms [45,85]. The mammary gland inflammation caused by this bacterium is characterized by severe pyogenic lesions in the mammary tissue, and malodorous and purulent milk, especially in case of co-infection with anaerobes, decreasing the milk yield and the low recovery rate [45]. The anaerobes most often involved in mastitis together with T. pyogenes are P. indolicus, F. necrophorum, and Prevotella melaninogenica (formerly Bacteroides melaninogenicus). All of these bacteria can colonize the mucous membranes and skin of clinically healthy cattle, but P. indolicus and T. pyogenes were the most frequently isolated from a teat skin [88]. Regardless of the many investigations on T. pyogenes mastitis, little is still known about the factors involved in the establishment and persistence of that infection.
T. pyogenes also contributes to many other disorders in cattle, among them, liver abscesses and interdigital phlegmon have a more significant economic impact. Those infections are mixed with anaerobes, mainly F. necrophorum, characterized by the synergistic interaction of both of the bacteria mentioned previously [59]. Liver abscesses related to T. pyogenes infection occur mostly in feedlot cattle, with a varying frequency from 2% to 80% [59,89,90,91]. The infection is associated with T. pyogenes presence in the rumen wall, in which the primary lesions can form and then bacteria can penetrate by a hepatic portal venous system to a liver, where abscesses form as secondary infection foci [60]. In the case of abscesses rupturing, systemic signs can develop, resulting in animal death. The development of liver abscesses is probably associated with ruminal acute or subacute acidosis, which can induce primary damage in the protective surface of the rumen wall.
Bovine interdigital phlegmon incidence in dairy cows is usually 2–5% per lactation, but some cases of outbreaks were also reported [35,58,92,93]. The role of T. pyogenes in the pathogenesis of this polymicrobial disease is not well defined. Kontturi et al. [58] reported that this bacterium is rather a secondary pathogen associated with the healing stage of the infection, while Bay et al. [94] did not detect T. pyogenes at all in the interdigital phlegmon investigation using 16S rRNA gene sequencing.
Moreover, T. pyogenes may cause a variety of other purulent infections in cattle such as pneumonia, encephalitis, pyelonephritis and kidney abscesses, lymphadenitis, endocarditis, and abscesses of various localization [30,31,36,44,46,95,96]. This pathogen was also isolated from cases of septicaemia and abortion [36,44,46,97].
In swine, T. pyogenes is a common agent of pneumonia, pleuritis, endocarditis, osteoarthritis, polyarthritis, mastitis, reproductive tract infections, and septicaemia [13,29,35,44,98,99,100,101,102]. Abscesses—superficial, muscular, or located in different organs—occur frequently, and may lead to the development of systemic purulent infection and inflammation of lungs, liver, kidneys, muscles, bones, joints, or other tissues [13,46,103]. In many cases, these are infection mixed with different microorganisms, as is observed in T. pyogenes infections in cattle. Diseases of swine associated with T. pyogenes are an emerging clinical, epidemiological, and economic problem, because they usually result in the necessity for the elimination of infected animals from a herd, and the discard of carcasses with suppurative lesions at slaughterhouses [103]. It has been reported that a number of factors can predispose to the development of these disorders, among other viral infections, that cause immunosuppression, for example with porcine reproductive and respiratory syndrome virus (PRRSV) [104].
In small ruminants, T. pyogenes is mostly a cause of abscesses formation in different tissues and localized in various parts of the body, including bone marrow and foot (footrot) abscesses [29,31,105,106,107,108,109,110]. Those lesions differ from that observed in the case of caseous lymphadenitis caused by C. pseudotuberculosis [111]. Moreover, T. pyogenes can be associated with purulent, mainly polymicrobial disorders in sheep and goats, such as pneumonia, lymphadenitis, arthritis, osteomyelitis, reproductive tract infections, mastitis, and septicaemia [30,35,36,46,112,113,114].
In other domestic animals, infections related to T. pyogenes are rare. It may be connected with the fact that this bacterium does not belong to their normal biota. Therefore, there are only a few data on the occurrence of T. pyogenes infections in companion animals. The first reported cases referred to otitis externa in a cat and cystitis in a dog [115], lung abscess in a dog [116], and feline pyothorax [117]. Moreover, T. pyogenes was isolated from cases of wound infection, abscesses, vaginitis, pneumonia, and encephalitis in dogs [30,35,36,46]. Recently, an interesting case of T. pyogenes and Brucella abortus co-infection in a cat and a dog was described by Wareth et al. [118]. Both animals lived on a dairy cattle farm, where cases of abortion and mastitis in cows were noted. The bacteria were isolated in a mixed culture from the uterine discharge of a bitch after abortion and a cat with pyometra.
Infections related to T. pyogenes were noted sporadically in horses, and included single cases of metritis, orchitis, mastitis, septicaemia, umbilical infection in foals, abscesses, and wound infection [30,36,46,119].
Furthermore, two cases of suppurative disorders in rabbits caused by T. pyogenes were published. In the first case, this bacterium was isolated from lung lesions, and in the second one, from necrotic foci in liver, spleen, lung, and brain [36,120].
The incidence of T. pyogenes infections in birds seems to be very low. Some cases of clinical lameness and osteomyelitis in turkeys were reported [121,122]. A unique case of liver abscesses in pigeons was described by Priya et al. [123].
In wildlife, T. pyogenes may be associated with many types of purulent disorders occurring in free-living and captive animals. T. pyogenes infections were reported the most frequently in ruminants and other herbivores, in which the bacteria were also found as a resident microbiota of the skin and mucous membranes of respiratory and urogenital tracts [20,54,124].
In the United States and Canada, T. pyogenes is an emerging pathogen of captive or free-ranging white-tailed deer (Odocoileus virginianus), which cause intracranial abscessation—suppurative meningoencephalitis disease complex (the intracranial abscess disease) that occurs with a variable frequency, depending on animal populations [54,124,125,126,127]. T. pyogenes may be also involved in pneumonia and necrobacillosis occurring in this animal species [128,129].
Furthermore, T. pyogenes was also isolated as an etiological agent of chronic purulent infections, including keratoconjunctivitis, brain and foot abscesses, in other cervids, such as Key deer (Odocoileus virginianus clavium) [130], fallow deer (Dama dama) [53], roebuck (Capreolus capreolus) [131], red deer (Cervus elaphus) [132], and mule deer (Odocoileus hemionus) [133]. T. pyogenes is a prevalent cause of variably located abscesses in forest musk deer (Moschus berezovskii), noted mainly in farm animals [40,134].
In European bison (Bison bonasus), T. pyogenes is associated with abscesses of the liver, spleen, lungs, lymph nodes, skin, and especially with urogenital tract infections [135]. In female bison, abscesses of various localizations were observed. In male bison, T. pyogenes is considered to be one of the etiological agents of a chronic necrotizing and ulcerative inflammation of the prepuce and penis (balanoposthitis) [135].
Additionally, T. pyogenes infections were reported in antelopes [29,136,137], an okapi (Okapia Johnstoni) [138], bison (Bison bison) [139], Bighorn sheep (Ovis canadensis) [140], a chamois (Rupicapra pyrenaica) [112], camels [141,142,143,144], an elk [36], and reindeer [145,146]. Moreover, some other sporadic cases of infectious diseases associated with T. pyogenes were described in Grey Slender lorises (Loris lydekkerianus nordicus) [147,148], macaws, and elephants [48], as well as in reptiles, a bearded dragon, and a gecko [149].
2.2. T. pyogenes Infections in Humans
Infections caused by T. pyogenes in humans are sporadic, mostly occur in immunosuppressed patients, and are connected with occupational exposure, especially relating to contact with farm animals and their environment [150]. Published data concerning T. pyogenes infections in humans are limited, and include, among others, reports on endocarditis [151,152,153,154,155], endemic leg ulcers [156,157], pneumonia [158], arthritis [159,160], sepsis [161], and various purulent lesions and abscesses [162]. As T. pyogenes was never demonstrated as a commensal microbiota of humans, those infections should be considered as zoonotic diseases [48]. Although, a probability of animal-to-human transmission of this pathogen has not been well estimated and confirmed.
3. Reservoir, Transmission, and Routes of Infection
Most actinomycetes are widespread in the natural environment, being found in various ecological niches as saprophytes, but they may also constitute a commensal biota of humans and animals, and some of them can be opportunistic pathogens [163,164]. Curiously, there is no published characterization of environmental T. pyogenes isolates, for example from soil, which might be considered non-pathogenic, as it is known, for instance, in case of environmental strains of R. equi, a typical soil opportunistic pathogen [165]. Although there are no data on T. pyogenes ability to replicate in soil or water, certainly, it can persist for some period in such environmental conditions. For example, C. pseudotuberculosis, the related actinomycete, can survive for several weeks in the environment [166]. Considering the nutritional requirements of T. pyogenes, it should be assumed that the bacterium can replicate only in the environment rich in peptides, fermentable carbohydrates, inositol, and hemin, and at the temperature range of 20 to 40 °C [4]. Therefore, it seems that a main reservoir and source of this bacterium are animals of various species.
Little is known about the dissemination of T. pyogenes infections, and about the transmission of the pathogen. It is suggested that the majority of infections have an endogenous character, as the bacteria are a common component of the skin and mucous membrane biota [48]. However, the possibility of exogenous infections should also be considered, because bacteria may be transmitted, for instance, by contaminated husbandry utensils and equipment, or directly from animal to animal [30,46]. The natural environment contaminated by T. pyogenes is suggested to be an important source of the bacteria, especially in the case of mammary or foot disorders in domestic and wild animals [46,53,109]. In addition, climate conditions, such as a high humidity and mild temperature, are factors favouring the infection occurrence [53]. In the case of summer mastitis, T. pyogenes, exceptionally, may be transmitted between animals by biting flies [86]. However, a possibility of tissue penetration by these bacteria through a micro-trauma caused by ectoparasites, such as ticks, should be also considered. The preliminary results of the study on ticks collected from the skin of European bison indicated a potential contribution of those arthropods to T. pyogenes transmission [167].
The observations from different studies indicate a potential threat of T. pyogenes transmission from wild to domestic animals, or the other way around [53,135]. It is very possible, regarding the frequent co-occurrence of wildlife species and livestock animals on the same agricultural areas, such as pastures and meadows, which can serve as a reservoir for this pathogen.
The data on the genetic relationship of T. pyogenes isolates occurring in a particular host population, and on the dissemination of strains amongst animals and the environment are lacking. The results of a few epidemiological studies on bovine and swine isolates are available [10,13,21,32,148]. In some of them, an association between the clonal types and the development of clinical infection by a strain was shown [21,32,148], while in other investigations, such a correlation was not found [10,13]. A variety of molecular methods, characterized by various discriminatory powers, were used for T. pyogenes differentiation, which enabled the phylogenetic analysis of strains to be performed, for example the 16S rRNA gene sequencing [135,149], single enzyme amplified fragments length polymorphism (SE-AFLP) [13], BOX-PCR [21,32], the superoxide dismutase A gene (sodA) sequencing [36], random amplification polymorphic DNA (RAPD-PCR), and multilocus sequence analysis (MLSA) [148]. The usefulness of some of them was proved by Nagib et al. [148] during the study on T. pyogenes isolates from lorises, which showed a close relationship, indicating their clonal origin. Unfortunately, the gold standard method used for genomic fingerprinting, pulse field gel electrophoresis (PFGE), was never reported as a technique applied for T. pyogenes phylogenetic investigation.
The routes of T. pyogenes infections are frequently difficult to establish. The T. pyogenes infections develop mainly as a consequence of the mechanical injuries of skin and mucous membranes [48]. Wounds and abrasions of skin are common routes of infection, for example, udder injuries in the case of T. pyogenes mastitis, or hoof injuries in the case of interdigital phlegmon. In the case of mucous membranes damage, such as in metritis, the bacteria can invade deeper tissues after endometrial epithelium, disruption during parturition. Another described route of infection is associated with improperly performed surgical procedures, such as castration or intramuscular injection [103]. Bacteria can also invade tissues through micro-injuries of the skin caused by some arthropoda, like flies or ticks, as it has been mentioned above. In deer, behaviour may influence the pathogen transmission and susceptibility to cranial/intracranial abscess infection, which occur more frequently in adult males [125,127]. Interestingly, Belser et al. [54] noted a higher prevalence of T. pyogenes along the forehead of the males of white-tailed deer than the females, when the rate of the pathogen carriage on the nasopharyngeal mucosa was the same for both sexes. Therefore, it is suggested that the disease development may be a result of cuts or abrasions arising from antler rubbing on trees or from sparring between males.
4. Pathogenesis of T. pyogenes Infection
The pathogenesis of microbial infection is determined by a variety of bacterial and host-related factors. In the case of T. pyogenes, the pathogenicity is attributed to the determinants, which induce the formation of abscesses, empyemas, and pyogranulomatous lesions. However, pathogen–host interactions in T. pyogenes infection are still poorly understood. Some known and putative bacterial factors contribute to the development of T. pyogenes infection, but their role in the infection pathogenesis remains insufficiently explained. Moreover, many researchers highlighted a high phenotypic and genotypic diversity among the studied T. pyogenes isolates of various origins, also taking into consideration virulence genotypes [13,21,29,30,31]. This finding indicates the genetic heterogeneity in the studied T. pyogenes populations. On the other hand, Cohen et al. [124] detected significantly more virulence genes in T. pyogenes isolates from populations of white-tailed deer males, in which a high incidence of the intracranial abscess disease was observed, compared with those detected in the isolates from apparently healthy animals in populations in which the disease was not noted. This finding suggests that the essential differences in the pathogenic potential may exist among T. pyogenes strains, depending on their origin.
4.1. T. pyogenes Virulence
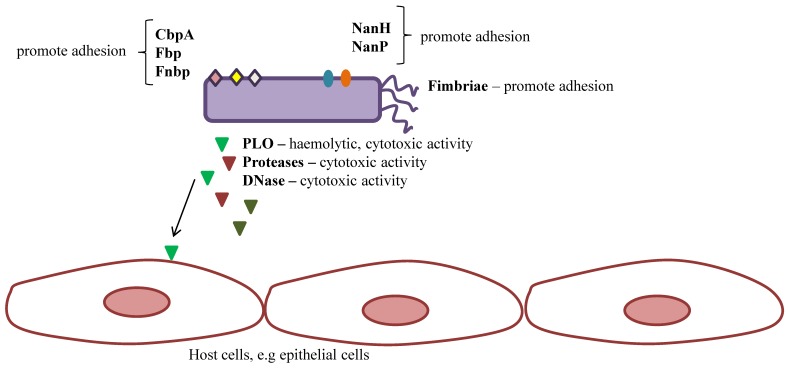
Only few virulence factors in T. pyogenes are recognized to date (Figure 2). They include pyolysin (PLO), the only known toxin of this bacterium; some adhesive factors, such as fimbriae neuraminidases and extracellular matrix-binding proteins; different exoenzymes, such as serine proteases with gelatinase and caseinase activity, or DNAses; as well as the ability to invade host cells and to create biofilm formation [48]. The significance of some of them in the pathogenicity is not clear enough. In general, profiles of genes encoding particular virulence determinants are not correlated with a type of infection and host species. However, a few cases of association between the presence of some determinants and a type of infection were reported [49,55].
Figure 2.
Schematic diagram of known virulence factors of T. pyogenes. Abbreviations: CpbA—collagen-binding protein; Fbp—fibrinogen-binding protein; Fnbp—fibronectin-binding protein; NanH—neuraminidase H; NanP—neuraminidase P; PLO—pyolysin.
4.1.1. Pyolysin
PLO is considered to be both a major virulence factor of T. pyogenes and a host-protective antigen [168,169,170], and, until now, the gene (plo) encoding this protein was detected in all wild-type T. pyogenes strains. This is an exotoxin belonging to the cholesterol-dependent (also called cholesterol-binding) cytolysins (CDCs), which are a family of 51- to 60-kDa single-chain proteins produced by many species of Gram-positive bacteria, for example Streptococcus pneumoniae (pneumolysin), Streptococcus suis (suilysin), Streptococcus pyogenes (streptolysin O), Paenibacillus alvei (alveolysin), Clostridium perfringens (perfringolysin O), or Listeria monocytogenes (listeriolysin O). [171,172]. PLO is the most divergent protein of this group, presenting only 38% to 45 % identity and 58% to 64% similarity to other toxins from the CDC family, when the conserved core of the CDCs (corresponding to amino acid fragment 38–500 of perfringolysin O) is taken into consideration during the analysis [172]. The highest identity of PLO is shown to suilysin, novyilysin, botulinolysin B, and tetanolysin O, which range from 45% to 44% [172]. This protein was purified and characterized for the first time by Ding and Lämmler in 1996 [173], however, its toxic and haemolytic activities were previously reported by Lovell [174]. As a member of the CDC family, PLO displays a cytotoxic effect on a variety of host cells, for example, erythrocytes, polymorphonuclear neutrophils (PMNs), macrophages, epithelial cells, fibroblasts, and endometrial stromal cells. [68,168,171,172]. The cytolytic activity of PLO is associated with its ability to bind to the plasma membrane and to form transmembrane pores, which is a common feature of CDCs [168,172]. The in vitro study showed that PLO is able to cause the lysis of human, sheep, horse, rabbit, and guinea pig erythrocytes [4]. Specific antibodies against PLO completely neutralize its haemolytic activity, suggesting that PLO is the sole haemolysin produced by T. pyogenes [168].
The significance of PLO as a primary virulence factor of T. pyogenes was confirmed in many in vitro and in vivo experiments, with use of PLO-deficient mutants or recombinant proteins [168,175,176]. PLO has a lethal effect on mice and rabbits, and a dermonecrotic effect on guinea pigs after intravenous and intraperitoneal injection [168,174,177,178,179]. Jost et al. [168] observed a loss of haemolytic activity in the PLO-1 mutant strain as a result of the insertional inactivation of the plo gene, as well as its 1.8-log10 reduction in virulence for mice in comparison to the wild-type strain. They also, for the first time, documented the importance of PLO for the in vivo survival of bacteria, studying the effect of the co-challenge of a wild-type strain, and a mutant strain with the inactivated plo gene in a mouse model. Similarly, Zhao et al. [179] demonstrated that the T. pyogenes strain with an in vitro higher expression of the plo gene was more virulent for mice in the in vivo study than the strain with a lower plo expression, designated as avirulent.
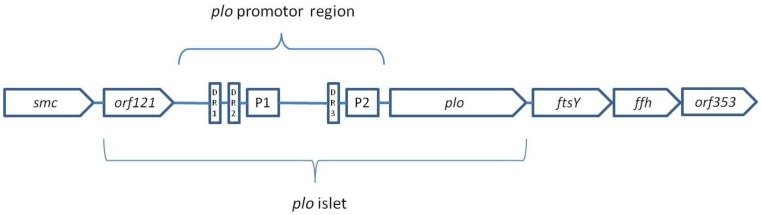
Billington et al. [180] cloned and sequenced the plo gene encoding PLO, which was located in an open reading frame (ORF) of 1605 bp in the T. pyogenes chromosom. The plo gene sequence was also described by Ikegami et al. [181], for which the deduced pyolysin sequence showed a 99.4% similarity and a 97.6% identity to the PLO sequence previously reported by Billington et al. [180]. A consensus ribosome binding site, two promoter sequences (similar to the E. coli σ70 promoter), and three direct repeats (DR1 to D3 with sequence ATTTTTG(C)TGG) were found upstream of the plo gene, and a transcriptional terminator region was found downstream of this gene [180]. Moreover, Rudnick et al. [170] found that the plo gene, along with the mentioned sequences and ORF (orf121), encoded a 13.4 kDa protein of an unknown function, form a genomic islet of 2.7 kb, characterized by a reduced content of G+C (50.2%). This islet, flanked by two housekeeping genes, smc and ftsY (62.5% G+C), is located in the T. pyogenes chromosome (Figure 3) [170]. Interestingly, the codon usage of plo and orf121 differ from that of the genes flanking the islet. The genes smc and ftsY are common in many other bacteria, mainly Gram-positive, and are essential for T. pyogenes viability [170]. Downstream of the ftsY gene are the ffh gene, and then the ORF, orf353. The ftsY and ffh genes encode the FtsY and Ffh proteins, respectively, which have a high similarity to the signal recognition particles from the other bacterial species [170]. The ftsY, ffh, and orf353 genes in T. pyogenes are located in close proximity, and form an operon-like arrangement that is unusual in most other bacteria. It seems that, as in other species, these genes are needed for bacterial growth.
Figure 3.
Schematic presentation of the T. pyogenes chromosomal region containing the plo gene and the surrounding genes. P1 and P2 indicate the positions of two promoters; DR 1–3 indicate the positions of three direct repeats. The scale is not designated.
The differences between the islet and the flanking genes suggest a possibility of horizontal transfer of the plo gene, though any integrase or transposon sequences were not found in this chromosomal region. Taking into consideration the fact that the plo gene is present in all wild-type T. pyogenes strains, including commensal isolates, it seems probable that plo was inserted into the intergenic region between smc and ftsY by homologous recombination; it has to be retained, as both of these genes are obligatorily required for bacterial growth. In addition, it was confirmed by Rudnick et al. [170] that the plo islet is a conserved region of the T. pyogenes chromosome found in all of the studied isolates of various origins.
T. pyogenes is an opportunistic pathogen that, being a part of the host microbiota, has no damaging effect on its organism. Therefore, it is suggested that the regulation of the PLO expression may be critical for the establishment of the status of this bacterium as a pathogen or a commensal. Rudnick et al. [170] reported that the plo gene expression is not regulated in vitro by orf121 located upstream of this gene. In their subsequent investigation, two promoters, P1 and P2, located in the plo islet, were identified as the regulatory sequences controlling the transcription of plo [57]. It was observed that the in vitro haemolytic activity of T. pyogenes was in growth phase depending on a peak in the early stationary phase [57,173]. It indicated that plo is up-regulated during that phase, and indeed a significant increase in the plo specific mRNA was noted. Thus, the suggestion that the PLO expression is controlled at the transcriptional level was confirmed [57]. It was also shown that the P2 promoter is predominant and highly active during the stationary phase of the in vitro growth of bacteria, while the P1 activity is weak. Besides the P1 and P2 promoters, direct repeats (DRs) located in the plo promoter region may be involved in the regulation of the plo gene transcription. The study of Rudnick et al. [57] showed that DRs, especially DR3, may function as binding sites for a soluble T. pyogenes factor being a transcriptional regulator. However, regarding AT-rich sequences of DRs, which can easily bend, it was supposed that DRs may also act as activators of transcription, by promoting RNA polymerase binding to the promoter.
The predicted, on the basis of the plo gene sequence, length of the PLO molecule is 534 amino acids (aa), and then, this protein should have a molecular mass of 57.9 kDa [180]. A signal peptidase cleavage site was found between 27 and 28 aa, indicating that the mature PLO molecule has a weight of 55.1 kDa. According to the Funk et al. [182] study, PLO is an oxygen-stable protein, heat-labile (destroyed at 56 and 100 °C), destroyed by pH 3 and 11, and id sensitive to treatment of protease, trypsin, and amylase.
In contrast to the majority of CDCs, the PLO activity is insensitive to thiols or other reducing agents, in other words, PLO does not require thiol activation [180]. This difference is associated with the divergence within the amino acid sequence of undecapeptide (491–501 aa) of PLO. The undecapeptide is a highly conserved region of each CDC, located near the C terminus of the protein. In some CDCs, including PLO, amino acid substitutions occur in this region [180,183]. In case of PLO undecapeptide (EATGLAWDPWW), a unique cysteine residue (C491), responsible for the thiol-activated nature of CDCs, is replaced with an alanine (A492). This substitution has no essential effect on the haemolytic activity of PLO, but is related to the oxygen stability of this cytotoxin [184]. Moreover, other changes in the PLO undecapeptide were noted, such as the insertion of a proline residue (P499) and the deletion of an arginine residue at the end of the CDCs undecapeptide. It seems that these changes have important effects on the conformation and charge of the undecapeptide [180]. The proline insertion has the greatest effect on the PLO activity, as the deletion of this amino acid resulted in a lack of haemolytic activity [183]. The same effect on the PLO haemolytic activity was observed in the case of the removal or substitution of any of the three tryptophan residues [183]. Therefore, as it was previously demonstrated by Billington et al. [180], the amino acid sequence of the PLO undecapeptide is required for full cytolytic activity.
The cytolytic activity of PLO, like other CDCs, is suppressed by free cholesterol in a concentration of 1µg/mL [180]. However, the presence of cholesterol in the target plasma membrane is absolutely necessary for pore formation by CDCs. The role of the undecapeptide in the initial plasma membrane binding seems to be crucial, in particular, the first tryptophan residue (W497) is important. Although, Billington et al. [183] suggested that other fragments of PLO might also participate in recognition and binding to the host cell membranes.
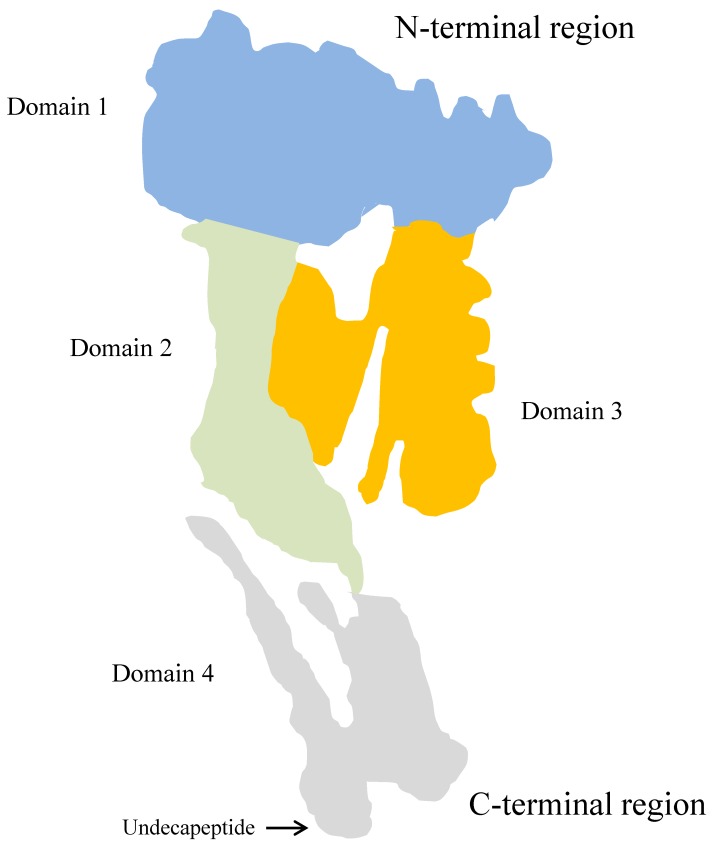
The known secondary and tertiary structures of some CDCs shows a significant similarity [172]. A crystal structure of the PLO molecule presumably is homologous to the structure of other CDCs. The tertiary structure model of PLO, based on the perfringolysin O (PFO)—PLO sequence alignment—was proposed by Pokrajec et al. [185]. The monomeric PLO molecule is rich in β-sheet elements and consists of four domains (D1 to D4), of which D2 and D3 are packed against each other, while D1 is located at the N-terminal and D4 at the C-terminal end of the molecule (Figure 4).
Figure 4.
Simplified model of the pyolysin molecule, based on the perfringolysin O-structure.
Domain 1 contains a-helix and β-sheet elements. The precise role of D1 in the pore-forming process remains undefined. Zhang et al. [186], studying an effect of the replacement of aspartic acid (D238) in this domain with arginine, showed an important role of D1 in maintaining the pore-forming activity of PLO. The investigation of Imaizumi et al. [177] indicated that domain 1, especially the region of 55–74 amino acids, is required for the haemolytic activity of PLO. Yan et al. [187] also confirmed the importance of this region of domain 1, as they demonstrated that the substitution of each amino acid from 58 to 62 in the PLO molecule, particularly isoleucine 61, resulted in the complete loss of its haemolytic activity. Moreover, six B-cell linear epitopes in D1 were identified by Yang et al. [188].
Domain 2 of the molecule forms a long, curved single layer of anti-parallel β-sheet, while the structure of domain 3 is more complex and consists of five strands of anti-parallel β-sheet surrounded by helical layers and short α-helices at either side of the central β-sheet. Domains 2 and 3 are involved in the monomer oligomerization and insertion into the plasma membrane. The separation of D2 and D3, as well as the structural collapse of D2, are required during these processes [189]. The conversion of the D3 short α-helices to two transmembrane β-hairpines starts the molecule insertion into the bilayer, and is a crucial step of the transmembrane β-barrel formation [172].
Domain 4 of the PLO molecule is the only contiguous domain characterized by a β-sandwich structure, connected by a single peptide with the rest of the protein. As it has been mentioned above, the conserved undecapeptide sequence, rich in tryptophan residues, is located at the tip of this domain. This part of the PLO is responsible for host plasma membrane recognition and cholesterol binding [185,190]. However, Pokrajac et al. [185] also demonstrated the ability of D4 to self-oligomerization, but not pore formation. Their findings indicate a greater functional role of this PLO domain in cytolysin activity, compared with the previously described CDCs.
The molecular mechanism of pore-forming by PLO and other CDCs seems to be very similar, and is best described for PFO [172,185]. PLO molecules are secreted to the extracellular environment, probably via the general secretion system, as in the most CDCs [172]. In a form of water-soluble monomers, they bind to the cholesterol-containing areas in the plasma membrane of the eukaryotic host cells [183]. Binding to cholesterol by the PLO domain 4 initiates the oligomerization of the monomers and the formation of incomplete arc-shaped structures, called th pre-pore. Subsequently, the PLO oligomers are inserted into the bilayer by the transmembrane β-hairpins of domain 3, which leads to the formation of a large transmembrane β-barrel pore, which is <50 nm in diameter and protrudes <7 nm above the plasma membrane surface [191]. As a consequence, this process leads to th eleakage of ions and other cytoplasmatic molecules, and finally to the lysis of the host cell.
It seems that a predominant assignment of the cytolytic activity of PLO is to enable access to free iron and other growth factors essential for the bacterial replication contained in the host cells. Furthermore, the ability to lysis phagocytes protects the bacteria against the host immune response. On the other hand, at lower concentrations, PLO can modulate the host immune response.
Despite a wide knowledge about the molecular structure and function of PLO, the precise role of this toxin in the pathogenesis of particular T. pyogenes infections, characterized by different course and clinical manifestations, remains unclear.
4.1.2. Fimbriae
The occurrence of fimbriae in Gram-positive bacteria is a rarity. T. pyogenes is just one of the exceptions [48]. T. pyogenes fimbriae have a filamentous structure, at 200–700 nm in length and 2.5–4.5 nm in width, and probably occur in a limited number on bacterial cells (less than 10 per cell) [48,192]. In T. pyogenes, five fimbriae were described, FimA, FimB, FimC, FimE, and FimG [48,192]. The presence of other fimbrial subunits can be deduced on the base of the T. pyogenes genome sequences, for example FimJ [192,193]. FimA, 45.7 kDa protein, contains a signal peptide, an E box sequence, and is encoded by the fimA gene [48]. FimB, 90.5 kDa protein, has a similar structure, but additionally contains a cell wall-sorting domain and a fibronectin-binding domain, and is encoded by the fimB gene [48]. Both genes, fimA and fimB, are located in a fimbrial gene operon, together with the srtA gene encoding a putative sortase. The other fimbriae, FimC, FimE, and FimG, are encoded by the genes fimC, fimE, and fimG, respectively.
The expression of the fimbriae in vitro is poor; therefore, it is difficult to characterize their properties, thus only their genes or mRNAs are better known. Liu et al. [192] investigated the in vitro expression of FimA, FimC, and FimE. However, even though different culture conditions were used, only the FimE expression could be detected. Zhao et al. [179] studied the expression of the virulence factors of T. pyogenes, including FimA and FimC, in vitro and in vivo on a mouse model. Their results showed that in in vivo conditions, the fimA gene was earlier expressed than fimC, which suggests that FimA is a dominating fimbria in T. pyogenes. This is in accordance with the findings of many studies on fimbrial genes distribution that demonstrated a high prevalence of fimA among various isolates, whereas the genes of other fimbriae were detected with different frequencies [13,21,29,30,31].
A role of fimbriae in the T. pyogenes infection is associated with the bacterial adherence to host cells, but the precise mechanisms of this interaction are not well understood. Taking into consideration that T. pyogenes can be a commensal as well as a pathogen, it seems that fimbriae are equally important for bacteria in both of these forms. Likewise, in the case of infections caused by many other bacteria, T. pyogenes fimbriae are required for cell adhesion and the colonization of host tissues [49,55]. Liu et al. [192], based on their study results, speculated that the poor expression of FimA can limit the formation of other fimbriae, and that the up-regulation of this fimbria production may be associated with T. pyogenes pathogenicity.
4.1.3. Extracellular Matrix-Binding Proteins
T. pyogenes also expresses other proteins, which determine the adhesive properties, and which are associated with the cell wall of the bacteria. These proteins probably also promote adhesion and enhance colonisation through the ability to bind extracellular matrix (ECM) compounds [48]. In the case of Gram-positive bacteria, these proteins belong to the microbial surface components recognizing the adhesive matrix molecules (MSCRAMM) family [194]. Firstly, T. pyogenes shows a fibrinogen-binding activity, however, it was inhibited by proteases [195]. In addition, the 20 kDa fibronectin-binding protein associated with the T. pyogenes cell wall was also detected, but not well characterized [48].
Collagen-binding protein A (CbpA) represents the MSCRAMM family, and is one of the better known extracellular matrix-binding proteins produced by T. pyogenes [48,194,196]. This 121.9 kDa surface protein is encoded by the chromosomal cbpA gene, and displays a 50.4% similarity to Cna, the collagen adhesin of Staphylococcus aureus. CbpA binds almost all types of collagen, but not other ECM. However, Pietrocola et al. [194] reported that CbpA can bind fibronectin, but in a distinct subsite than that recognized by collagen. This protein is involved in the adherence of bacteria to epithelial and fibroblast cell lines [196]. It may be supposed that the T. pyogenes strain, which produces CbpA, has higher potential to colonize collagen-rich tissues. Although, the cbpA gene was found in many isolates of various origins, with different frequencies [13,21,29,30,31].
4.1.4. Neuraminidases
Neuraminidases (sialidases) are one of the most important enzymes of the sialic acid catabolism. Neuraminidases cleave the terminal sialic acid residues from complex glycoproteins, glycolipids, and carbohydrates from the host cell receptors. Neuraminidases are produced by many species of Gram-negative and Gram-positive bacteria or viruses [197]. Bacterial neuraminidases are the main factors for promoting adhesion by exposing the cryptic host cell receptors. In addition, neuraminidases can promote tissue colonisation by reducing mucus viscosity. These compounds also weaken the host’s immune response by exposing IgA particles, making them more susceptible to bacterial proteases [48,197,198,199]. Bacterial neuraminidases are secreted as extracellular enzymes or are anchored to the cell wall. While in Gram-negative bacteria, neuraminidases are usually secreted, neuraminidases of the Gram-positive bacteria are commonly in a cell-associated form [200,201,202,203,204].
The first note about the 50 kDa extracellular neuraminidase of T. pyogenes was reported by Schaufuss and Lämmler [205]. Afterwards, two neuraminidases expressed by T. pyogenes were better characterized [206,207]. Neuraminidase H (NanH) and neuraminidase P (NanP) are 107 kDa and 186,8 kDa proteins, respectively. These neuraminidases are attached to the T. pyogenes cell wall, which results from the presence of specific anchoring motifs in their molecules (LPxTG—for NanH; LAWTG—for NanP). NanH and NanP proteins contain the conserved catalytic RIP/RLP motif (Arg-Ile/Leu-Pro) and five copies of the Asp box motif (Ser-X-Asp-X-Gly-X-Thr-Trp), commonly occurring in the bacterial neuraminidases [206,207]. NanH is the most similar to the neuraminidase from Actinomyces viscosus (61.8% similarity and 31.2% identity) [206]. NanP shows a similarity to the neuraminidase from Micromonospora viridifaciens (61.6% similarity and 45.3% identity) [207]. However, some similarity between NanH and NanP (53.8% similarity and 38.8% identity) was also demonstrated [48].
T. pyogenes strains can produce neuraminidases H and P, encoded by the nanH and nanP genes, respectively [206,207]. The occurrence of these genes is characteristic of the majority of T. pyogenes isolates from cattle [21,29,30,31,36,206,207,208] and swine [29,30,36]. However, the nanH and nanP genes were found at high rates in the bovine isolates studied by Zastempowska and Lassa [37]. The genes encoding neuraminidases are detected with various frequencies in the T. pyogenes isolates from small ruminants, such as goats and sheep [29,30,31,36], and in the forest musk deer isolates [134], while the presence of these genes among the isolates from European bison is much less common [29,135]. In several studies, the nanP gene was detected more frequently than the nanH gene in the tested isolates [30,135,208]. However, Rogovskyy et al. [31] reported that most of T. pyogenes isolates from small ruminants carried mainly the nanH gene.
T. pyogenes neuraminidases play an important role in adhesion to the host cells, as it was shown in the study with epithelial cells [207]. Moreover, T. pyogenes neuraminidases are probably necessary for the colonization of host tissues during the early phase of infection, but they are not essential during further stages of a disease development [48]. The different prevalence of the genes encoding neuraminidases in the T. pyogenes isolates from various origins, suggests that other adhesion factors may be also produced by this species.
4.1.5. Biofilm
The ability to perform biofilm formation is a well-known feature of microorganisms, which promotes their resistance to many disadvantageous factors, for instance antimicrobials, as well as increases the adherence properties and enables better protection against the immune response of the host [48]. T. pyogenes, as with many other bacteria that are resident on the mucous membranes of a host, is able to perform biofilm formation. Biofilm production was noted in a majority of the studied T. pyogenes isolates from different animal species and various types of infections [43,134]. Biofilm formation by T. pyogenes is controlled by a two-component regulatory system PloS/PloR, where PloR up-regulates the expression of biofilm [64,179,209]. In the case of polymicrobial infection, a biofilm formation by T. pyogenes may be inhibited by the QS molecules produced by other bacteria, for example E. coli [64,210]. As in some cases biofilm production may promote the infection development, it seems important to find a therapeutical option for reducing this bacterial property. Da Silva Duarte et al. [211] evaluated the use of the E. coli phage UFV13 for the disruption of the T. pyogenes biofilm, and they obtained a significant decrease of biofilm formation caused by this phage. This finding indicates a necessity of further studies on this issue.
4.1.6. Regulation of Virulence Factor Expression
Jost and Billington [48] suggested the existence of a two-component system comprising a sensor histidine kinase (HK) and response regulator (RR) proteins in T. pyogenes. These signalling systems are common among bacteria, and they enable the detection of an environmental or cellular signal that leads to an appropriate cellular response [212,213]. Zhao et al. [64] determined a LuxR-type two-component regulatory system in T. pyogenes, named PloS/PloR, using a comparative transcriptome analysis between two T. pyogenes isolates from musk deer with different haemolytic activities. The results of the transcriptome analysis showed the presence of ten typical DNA-binding response regulators (RRs) in the T. pyogenes genome. However, a protein crystal structure analysis revealed that only one among the identified DNA-binding RRs had a structure similar to that described previously by Jost and Billington [48]. This RR, called PloR, had a CheY-type receiver domain and a C-terminal LuxR-type HTH DNA-binding domain, while a cognate sensor HK was named PloS. Zhao et al. [64] demonstrated that the expression level of the ploR gene is correlated with the expression level of the plo gene, indicating PloR as an activator of plo, which up-regulates PLO production. On the other hand, it was observed that PloR can down-regulate the expression of T. pyogenes proteases [48]. In addition, it seems that PloR is able to up-regulate the biofilm formation and probably the expression of the fimbriae in T. pyogenes.
The function of the two-component system in T. pyogenes was also investigated in vitro using the N-acyl homoserine lactones of P. aeruginosa and E. coli as QS signal molecules, which can bind to the upstream sensor HK, PloS, and via the PloS/PloR system, may regulate the virulence of bacteria by the inhibition of their growth and biofilm production [64]. Huang et al. [65], studying an effect of N-acyl homoserine lactones on the T. pyogenes virulence in a mouse model, confirmed that those QS molecules inhibited the expression of plo, ploR, and ploS, and increased the survival rate of mice. In conclusion, the function of the two-component system PloS/PloR and the QS system seems to have the essential significance for the modulation of the T. pyogenes virulence.
4.2. Induction of Host Defense Mechanisms by T. pyogenes
The pathogenicity of T. pyogenes is assigned mainly to PLO, a cholesterol-dependent cytolysin, which promotes cell lysis and is responsible for altering the host cytokine profile. This toxin also exerts cytolytic, dermonecrotic, and lethal effects on numerous types of cells, including immunocompetent and non-immune cells [176,186]. It is responsible for the complement cascade induction; modulation of the host cytokine profile; inhibition of respiratory burst; and bactericidal activities in neutrophils, monocytes, and macrophages. These features lead to the modulation of the immune response and to evasion from a host’s immune mechanisms. Because of the presence of neuraminidases NanH and NanP, T. pyogenes is able to adhere to the alimentary and respiratory epithelial mucosa, increasing the mucus viscosity that facilitates bacterial colonization and diminishes the host immune response, including damage to a first line of defence—destruction of IgA by bacterial proteases. Those serine proteases, as it was mentioned above, are involved in the invasion and destruction of tissues [48,196].
For many years, the assessment of PLO involvement in the development of the disease was conducted using in vitro (established cell lines or primary cell cultures) and in vivo (mouse and large animal) models [48,68,69,75,168,186].
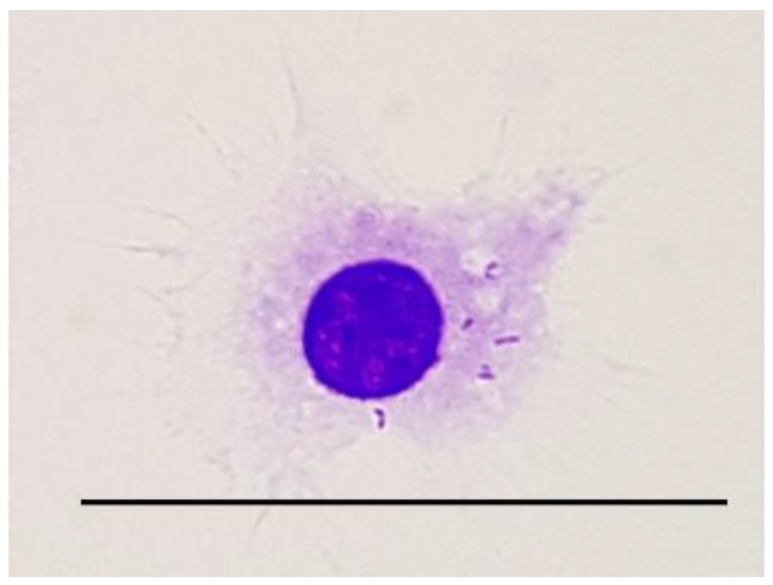
One of the first antibacterial mechanisms of immune response is inflammation, resulting in the recruitment of neutrophils, monocytes, and macrophages to a site of infection. The involvement of those cell populations leads to the phagocytosis and killing of bacteria, clearance of infection, and stimulation of adaptive immune response. Still, T. pyogenes interactions with host phagocytic cells strongly influence the outcome of the disease. Using macrophage established cell line J774A.1, it was clearly shown that this pathogen was easily phagocytosed, and could survive within macrophages up to 72 h, with the survival rate diminishing over time. Probably, this is caused by the presence of antibiotics in a medium used for culturing infected macrophages. Once bacteria exit the infected cell, they are killed by the antibiotic present in the medium. Similar results were obtained when the macrophage cell line RAW264.7 was infected with either T. pyogenes ATCC 19411 strain or T. pyogenes European bison isolate. In this study, phagosome formation, intracellular bacteria survival, and changes in the mitochondrial network and distribution were established at 2, 6, and 24 h post infection (pi) [214]. The formation of phagosomes was noticed as early as 2 h pi, and they were still present within the cells up to 24 h pi, with bacteria either within the phagosome or in the cytoplasm of the infected cells, and the recovery of viable bacteria was possible up to 24 h pi (Figure 5). However, the mitochondrial network morphology and distribution was not visibly altered in the RAW264.7 cells infected with either the ATCC 19411 strain or European bison isolate of T. pyogenes when compared with the uninfected control cells. Further investigations are required in order to elucidate the mechanism of T. pyogenes pathogenesis. Nonetheless, these data are in agreement with the observations done on bovine polymorphonuclear neutrophils (PMNs) infected with T. pyogenes, in which increased phagocytosis was noticed. As this pathogen can survive within phagocytic cells, increased phagocytosis is strongly connected with bacterial dissemination throughout the host [195]. Studies done in a mouse model clearly showed that PLO is responsible for peritonitis [168].
Figure 5.
The macrophage of the RAW264.7 cell line infection with T. pyogenes. Staining using the Giemsa–MayGrünwald method; scale bar = 20 µm (photo courtesy of Anna Hupało-Sikorska, BSc).
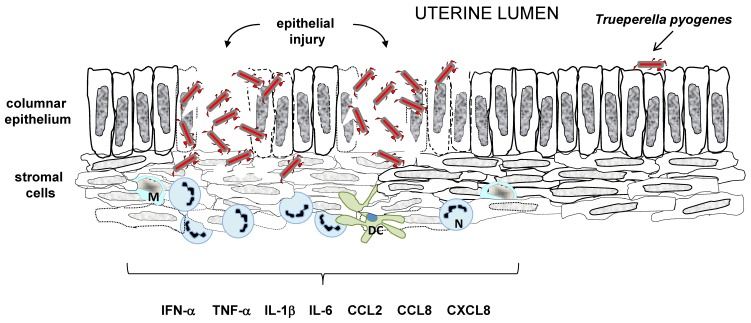
One of the common, most recognized infections in dairy and beef cattle are uterine infections caused by T. pyogenes. They result from the recruitment of neutrophils, from monocytes, and from the induction of a proinflammatory response, accompanied with formation of mucopurulent discharges within the infected uterus. This was confirmed on a large animal model. The uterine endometrium of healthy cows was scratched with a cytobrush (damage to the epithelial layer), and subsequently, an intrauterine administration of 5 × 108 cfu of T. pyogenes was performed. Mucopurulent uterine discharge was evident in the challenged animals, and was associated with the isolation of this pathogen [68].
However, the ability of cows to defend against T. pyogenes infection depends on the interaction between the invading pathogen and the host’s innate immunity. An application of bovine endometrial cell culture in an in vitro model elucidated the PLO involvement in tissue damage and the development of the endometrium pathology of the postpartum period. Recombinant PLO (rPLO) and bacteria-free filtrates (BFF) of T. pyogenes had a similar haemolytic activity on the target cells. Still, the stromal cells and epithelial cells expressed a different level of susceptibility concerning treatment with those factors. The endometrial stromal cells were markedly more sensitive than the epithelial cells. This haemolytic effect was abrogated when the endometrial cells were treated with BFF derived from T. pyogenes with a deleted plo gene (T. pyogenesΔplo), and when anti-PLO antibodies were applied. The difference in susceptibility or resistance to PLO between the stromal and epithelial cells can be explained by a lower level of cholesterol expression in the epithelial cells. It has biological implications to PLO-mediated uterine tissue damage. The columnar epithelium of the endometrium establishes a first line of defence by forming a physical barrier between the uterine lumen and the underlying stroma. As it expresses less sensitivity to PLO, it protects the tissue from colonization by T. pyogenes. Once this barrier is disrupted, the bacteria can colonize the endometrium, and the development of the disease is induced. However, PLO did not induce inflammation, as the treatment of bovine endometrial culture cells with rPLO did not result in increased levels of IL-1β, IL-6, or CXCL8 in the culture supernatant. Nevertheless, during clinical infection, T. pyogenes often causes tissue damage in association with other species of bacteria, expressing together with T. pyogenes pathogens, the associated molecular patterns (PAMPs) and damage associated molecular patterns (DAMPs) responsible for the induction of inflammatory response.
The described sensitivity of stromal cells to PLO-mediated cytolysis is one of the explanations for how T. pyogenes acts as an opportunistic pathogen, responsible for endometrial damage once the protective epithelium is lost after parturition [68].
It has to be remembered that the development of a disease depends on the ability of an infectious agent to adhere, to colonize a host’s target tissue, and develop mechanism(s) that are responsible for avoiding a host’s defence and the involvement of its innate immunity. In the case of T. pyogenes, bovine uterine infections also interplay, as follows: the host–virulent strain of T. pyogenes or host–opportunistic strain of T. pyogenes, should be considered. The model presented by Ibrahim et al. [56] considers all of these factors. They focused on in vitro investigating the interactions between a bovine endometrial epithelial cell culture with either the T. pyogenes strain isolated from the uterus of a postpartum cow developing clinical endometritis, or T. pyogenes collected from the uterus of a healthy cow. The assessment of the presence of strain-specific factors participating in the development of the bovine clinical endometritis was also performed. The outcome of the analysis on a genetic level revealed that both strains presented genes encoding virulence factors; however, there were differences between the expression levels of plo, cbpA, nanH, nanP, fimA, fimC, fimE, and fimG genes, favouring the virulent strain. The proteins encoded by those genes participate in adhesion to the host cells [48,207], so a virulent strain had a higher ability to attach to the epithelium, because of the elevated level of the cell-wall associated molecules. Both strains expressed a cytolytic effect on cultured cells, which means both strains secreted PLO, a major virulence factor. However, this effect was abrogated when the bovine endometrial epithelial cells were treated with heat inactivated bacteria or bacteria-free filtrates. These findings are in line with the results obtained by Amos et al. [68], showing that BFF and rPLO were not responsible for the stimulation of a proinflammatory response in endometrial cells.
To mimic the interplay between the host target tissue and T. pyogenes in the chronic proinflammatory environment, endometrial endothelial cells treated with bacteria were co-cultured in the presence/absence of peripheral blood mononuclear cells (PBMCs). The presence of PBMCs did not influence the viability of the endometrial epithelial cells more than 16 h, upon the treatment with live bacteria, irrespective of a strain. However, the early detection (4 h) of genes encoding proinflammatory mediators (PTGS2, CXCL3, IL6, and CXCL8) was noticed in the endometrial endothelial cells treated with a virulent strain of T. pyogenes, in the presence of PBMCs. This in vitro interaction suggests that the leukocytes found within the endometrium may be responsible for sensitizing the epithelial cells to the initial bacterial infection through the enhancement of uterine innate immunity induction (Figure 6). These data suggest that the development of endometritis in dairy cows after parturition may be caused by a specific characteristic of certain strains of T. pyogenes. Moreover, the presence of immune cells can be the reason for the amplification of the proinflammatory response in the endometrial epithelial tissue towards T. pyogenes pathogenic strains.
Figure 6.
Schematic presentation of the pathogenesis of uterine infection with T. pyogenes. Recruitment of monocytes (M), neutrophils (N), dendritic cells (DC), and other proinflammatory cells—secretion of proinflammatory mediators.
The research of Zhang et al. [186] indicated that the inflammation-inducing effect of PLO depends on its cytolytic activity, but not on PAMPs activity. These findings are in contrast to the results of Amos et al. [68] and Ibrahim et al. [56].
Studies done on bovine oviductal epithelial cells (BOECs), in an in vitro model, suggested a specific mechanism employed by T. pyogenes to avoid an immune response. In the course of T. pyogenes infection, there was no induction of any clear proinflammatory response in the BOECs at either the transcriptional or protein level. The BOECs co-cultured with T. pyogenes remained viable during the first 24 h of incubation when treated with MOI 0.01. However, a higher MOI caused the death of those cells within 24 h of co-culturing. What is interesting, is that the BOECs co-cultured with T. pyogenes expressed a similar level of IL1A, IL1B, and TNFA mRNA as the control cells did. Similar results were obtained when the level of mRNA concerning CXCL8, CXCL1/2, and PTGS2 was assessed. Although, at the same time, the BOECs co-cultured with Bacillus pumilus responded to stimulation, with an increased level of cytokines and chemokines mRNA. It seems that the lack of responsiveness in the BOECs induced by T. pyogenes is one of the escape routes from immune surveillance developed by this pathogen, as the expression of the genes encoding the proinflammatory mediators was similar to the control levels [75].
5. T. pyogenes Genome
The first complete sequence of the T. pyogenes genome was described in 2014 by Machado and Bicalho [215]. However, to date, 19 genome assemblies of this species are available in the GenBank nucleotide database (NCBI). Complete genome sequences were reported for 10 strains, isolated as follows: four from swine, three from cattle, one from goat, one from forest musk deer, and one from water buffalo. Additionally, the vast majority of the sequenced genome of T. pyogenes were derived from strains, which were isolated from animals in China. Other available genome assemblies are scaffolds (n = 3) and contigs (n = 6). The main features of complete T. pyogenes genomes are summarized in Table 1.
Table 1.
General features of the complete T. pyogenes genomes available in the GenBank nucleotide database (NCBI).
| Strain Designation | Strain Origin | Size (Mb) | GC% | Number of | GenBank Accession nr | |||
|---|---|---|---|---|---|---|---|---|
| Genes | CDS | RNA | Pseudogenes | |||||
| TP4 | swine | 2.43 | 59.4 | 2202 | 2102 | 59 | 41 | CP033905.1 |
| TP3 | swine | 2.38 | 59.4 | 2156 | 2058 | 58 | 40 | CP033904.1 |
| TP2 | cattle | 2.25 | 59.7 | 2023 | 1938 | 58 | 27 | CP033903.1 |
| TP1 | cattle | 2.33 | 59.8 | 2125 | 1993 | 58 | 74 | CP033902.1 |
| TP-2849 | swine | 2.38 | 59.4 | 2158 | 2063 | 58 | 37 | CP029004.1 |
| TP4479 | swine | 2.38 | 59.4 | 2153 | 2058 | 58 | 37 | CP029001.1 |
| Arash114 | water buffalo | 2.34 | 59.5 | 2145 | 2054 | 56 | 35 | CP028833.1 |
| 2012CQ-ZSH | goat | 2.30 | 59.7 | 2050 | 1806 | 53 | 191 | CP012649.1 |
| TP8 | forest musk deer | 2.27 | 59.6 | 2091 | 2001 | 50 | 40 | CP007003.1 |
| TP6375 | cattle | 2.34 | 59.5 | 2082 | 1984 | 53 | 45 | CP007519.1 |
The T. pyogenes genome was found to consist of a single circular chromosome comprising from 2.25 to 2.43 mega base pairs, depending on the strain. This species is characterized by high G+C% content. Moreover, the differences in the rate of G+C between the T. pyogenes strains are not significant (59.4–59.8%). tRNA is the most abundant RNA type in these bacteria. The share of rRNA in the whole nucleic acid content ranges from three to nine. In addition, there are also several non-coding RNAs (one or three, depending on the strain). The T. pyogenes genomes are indicated by the relatively high numbers of pseudogenes (from 27 to 191).
The T. pyogenes genome encodes many genes, for which the functions were assigned by the homologies to known proteins. Apart from the virulence-associated genes, the genome of this species can contain several antibiotic resistance genes. Furthermore, the luxS gene regulating the formation of biofilms was also found in the genome sequence [209]. In addition, the presence of a member of the T4virus (vB_EcoM-UFV13) indicates the efficiency in controlling the biofilm formation by T. pyogenes [216]. Moreover, the T. pyogenes genome contains four housekeeping genes (metG, tuf, gyrA, and fusA). The tuf and fusA genes encode the translation elongation factors Tu and G, respectively. Two other genes confer the DNA gyrase subunit A (gyrA) and methionine—tRNA ligase (metG). These genes were successfully used in the multilocus sequence analysis (MLSA) of this species [148]. The genetic analysis showed that T. pyogenes had a more complex system of amino acid and lipid metabolism, and more genes involved in the pathogenicity than are found in Arcanobacterium hemolyticum. These differences may affect the ability to cause infections in different host types by T. pyogenes isolates. Moreover, all of the groups of the family Actinomycetaceae have phosphotransferase systems that are probably essential for the colonization of a wide range of hosts and for the initiation of abscess formation. Some genes were lost or acquired as a result of lateral evolution, which helps in the adaptation of bacteria to a new environment [6]. The T. pyogenes species was reclassified based on 16S rRNA gene sequences, the menaquinone structure, and the phospholipid composition from the genus Arcanobacterium to the genus Trueperella, together with four other species, such as Trueperella abortisuis, Trueperella bernardiae, Trueperella bonsai, and Trueperella bialowiezense. Furthermore, 16S rRNA gene sequence similarities between strains from the genus Trueperella ranged from 95.3% to 98.6% [1]. There was also a draft genome sequence of one human T. bernardiae isolate deposited in the NCBI [217].
The genomes of T. pyogenes also include plasmids. Until now, two plasmids have been described for this species [178,218]. First, a native pAP1 (U83788) is a circular plasmid of 2439 bp, containing three open reading frames (ORFs). Plasmid pAP1 encodes the rep gene, which is required for the initiation of replication. Two other genes, orf112 and orf129, encode the hypothetical proteins of an unknown function. However, pAP1 does not include any antibiotic resistance genes [218]. The other, pAP2 (AY255627), is a circular plasmid of 9304 bp, and it contains seven ORFs. In pAP2, repA is probably required for the replication of this plasmid. Moreover, there are other genes, namely: tetR(33), which encodes the repressor protein and gcrY, and orf95 with unknown functions. In addition, pAP2 is characterized by the presence of two genes encoding antibiotic resistance determinants—erm(X) and tetA(33). In T. pyogenes, erm(X) determines the resistance to macrolide antibiotics, while tetA(33) is associated with low-level tetracycline resistance [178]. Furthermore, plasmid pAP2 contains the insertion sequence IS6100, which is found either in Gram-positive or in Gram-negative bacteria [219].
The knowledge of the complete genome sequence may allow for the identification of new genes that may contribute to the pathogenicity and antibiotic resistance of T. pyogenes. In addition, genome sequencing can help to understand the basics of the metabolism and evolution of the bacterial species.
6. Immunoprotection and Perspectives
The antimicrobial treatment of T. pyogenes infections is often ineffective, because of the increasing resistance of bacteria or the limited distribution of drugs to the site of infection, for example, to abscesses. Hence, vaccination should be considered as a primary method of T. pyogenes infection prevention. It seems that some of the virulence factors of T. pyogenes could be promising candidates for vaccine antigens.
Most studies concerning the stimulation of protective immunity against T. pyogenes infection were done on a mouse model, and only a few were done using a ruminant or swine model. The first trials to protect ruminants against infection with T. pyogenes were focused on animal treatment with whole cells of T. pyogenes or a culture supernatant, and were mostly unsuccessful; however, some therapeutic effects on mastitis development were observed [48,220,221]. In swine, the vaccination of pregnant sows with an autovaccine was an attempt to control the losses of newborn animals. Studies done by Kostro et al. [222] revealed that the administration of T. pyogenes cells treated with a phenol solution to pregnant sows, six and three weeks before anticipated delivery, significantly increased the number of CD4+ T cells, CD8+ T cells, and CD25+ T cells, as well as enhanced the levels of IFN-γ, TNF-α, and IL-10 in a colostrum and milk [222]. The recent trials were concentrated on the protection of heifers against post partum uterine diseases. Pregnant heifers were vaccinated using different routes of immunization (subcutaneously and intravaginally), and different compositions of the vaccine, as follows: (i) inactivated bacterial whole cells (E. coli, T. pyogenes, and F. necrophorum) together with recombinant proteins, FimH, PLO, and leukotoxin (LKT)); (ii) recombinant proteins FimH, PLO, and LKT only; (iii) inactivated bacterial whole cells (E. coli, T. pyogenes, and F. necrophorum) only [223]. The obtained results demonstrated that subcutaneous vaccination significantly decreased the incidents of puerperal metritis, but intravaginal vaccination failed in preventing the disease.
Mice used for the assessment of protective immunity induction against infection with T. pyogenes provide a reliable model that can serve for further comprehensive studies on other animal species. The administration of formalin-inactivated recombinant PLO (rPLO) induced the protection of mice against intraperitoneal challenge with 108 of T. pyogenes cells, and PLO-specific antibodies were detected in the sera of the immunized mice [168,180].
The current trend in vaccine design is concentrated on the development of such a product that will induce immunity against multiple pathogens. Using a mouse model, Zhang et al. [224] and Hu et al. [176] induced specific immunity that protected animals against challenge with T. pyogenes and C. perfringens. However, their approach to solve the problem concerning the stimulation of protective immunity was quite different. Hu and colleagues [176] designed a chimeric protein called rPC-PD4, which was composed of C. perfringens truncated regions of C-domain of phospholipase C (rPLC), and D4 domain of T. pyogenes PLO (rPLO), and was encoded by chimeric genes incorporated into a plasmid vector. The production of specific antibodies, and the presence and level of proinflammatory cytokines (TNF-α, IL-1β), chemokines (CXCL8), and IL-10 in sera of immunized mice were assessed; however, only partial immunity was observed after challenge with T. pyogenes or C. perfringens. Zhang’s group [224] concentrated not only on PLC and PLO as major immunogens, but also on the involvement of formaldehyde inactivated cultures of T. pyogenes and C. perfringens as vaccine antigens, combined with aluminium hydroxide gel. The outcome of their proposal is promising, as the survival rate of immunized mice after challenge with T. pyogenes and C. perfringens was 80% and 100%, respectively. These studies [176,224] present a very interesting approach for the development of a new, safe vaccine against polymicrobial infections.
Nonetheless, the latest trials to stimulate immunoprotection against T. pyogens infection are the most promising so far. The studies of Huang’s group [225,226] done on a mouse model, concentrated on genetic immunization. Two pathways to stimulate protective immunity against T. pyogenes infection were used. The first one applied the modification of the cytokine environment of immunized animals together with delivering the gene encoding PLO [225], the second one focused on immunization with a DNA vaccine containing genes encoding four different virulence factors of T. pyogenes, and simultaneous vaccine protection against destruction by the host environment [226].
In the first study, concurrent immunization with two plasmids carrying the plo gene and the IL1β gene, respectively, resulted in the protection of mice from intraperitoneal challenge, with 3.7 × 108 cfu of T. pyogenes [225]. PLO-specific antibodies were detected in the sera of immunized mice with a higher titer of the IgG2a subtype than the IgG1 subtype. The T-cell profile analysis indicated an increased level of CD8+ T-cells and CD4+ T-cells. These results correlated with the detection and assessment of the cytokine levels evaluated in the supernatant collected from the spleen lymphocytes culture (increased levels of IFN-γ, and IL-2, and slightly diminished IL-4). In this model, IL-1β enhanced the immunogenicity of the vaccine by influencing the activity of the macrophages, the major population of the phagocytic cell, as well as antigen presenting cells (APCs), and also the B-cells, which act as APCs during early phases of immune response development, later transforming into plasma cells secreting antigen-specific antibodies, hence humoral immunity.
In the second research of Huang’s group [226], the plo, cbpA, fimA, and nanH genes were paralleled as a single chimeric gene with an attached CpG ODN 1826 motif, so as to overcome low immunogenicity and susceptibility to host endonucleases. Finally, the chimeric gene was incorporated into the expression plasmid vector, and then this construct was encapsulated in chitosan nanoparticles to protect the DNA. The chimeric gene DNA vaccine introduced intramuscularly initiated production of antibodies specific for the target epitopes of PLO, CbpA, NanH, and FimA in mice. Moreover, the level of IgG2a was higher than the IgG1 in the sera of immunized mice, suggesting that immunization with this vaccine mainly primed the Th1 profile.
Compared with the subunit and conventional vaccines, DNA vaccines express some advantages as future stimulants of immunity. They are easy to manufacture, stable, and confer potential safety. Moreover, many genes encoding specific antigen proteins can be inserted in a carrier genome, and once introduced to the host, stimulate protective immunity against a variety of infections. In this context, the studies done by Huang et al. [225,226] are very important, not only in the induction of effective protection against T. pyogenes infection. They also proved that the formulated chitosan-CpG ODN nanoparticles are stable in eukaryotic cells, are able to protect the chimeric gene in the encapsulated plasmid from degradation, promote its expression, and also participate in the induction and enhancement of the immune response, so they could serve as a safe and efficient drug release carrier system.
7. Conclusions
T. pyogenes has significant importance as an opportunistic animal pathogen causing a variety of purulent infections. These infections pose a huge economic problem in livestock breeding. Therefore, it is crucial to understand the mechanisms of pathogenicity of this bacterium and the routes of its transmission for the development of an effective prevention strategy.
Although some of virulence determinants in T. pyogenes are well recognized, little is known about the dissemination of infections. It is interesting, there is still limited data about the pathogen–host interactions that may be involved in the development of T. pyogenes infection. Especially, the determination of factors that have a key role in transformation from a commensal to a pathogenic bacterium is needed. Although it seems that animals are the main reservoir of this bacterium, the epidemiological relationships between the particular isolates remain unclear.
Acknowledgments
The authors thank Dorota Rzewuska for the technical support during editing the manuscript.
Author Contributions
Conceptualization, M.R.; writing (original draft preparation), M.R., E.K., D.C.-C., M.K.-Ś., I.S., and M.G.; writing (review), M.R., E.K., and M.G.
Funding
This work was supported by KNOW (the Leading National Research Centre) Scientific Consortium “Healthy Animal–Safe Food”, decision of Polish Ministry of Science and Higher Education, no. 05-1/KNOW2/2015.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Yassin A.F., Hupfer H., Siering C., Schumann P. Comparative chemotaxonomic and phylogenetic studies on the genus Arcanobacterium Collins et al. 1982 emend. Lehnen et al. 2006: Proposal for Trueperella gen. nov. and emended description of the genus Arcanobacterium. Int. J. Syst. Evol. Microbiol. 2011;61:1265–1274. doi: 10.1099/ijs.0.020032-0. [DOI] [PubMed] [Google Scholar]
- 2.Ramos C.P., Foster G., Collins M.D. Phylogenetic analysis of the genus Actinomyces based on 16S rRNA gene sequences: Description of Arcanobacterium phocae sp. nov., Arcanobacterium bernardiae comb. nov., and Arcanobacterium pyogenes comb. nov. Int. J. Syst. Bacteriol. 1997;47:46–53. doi: 10.1099/00207713-47-1-46. [DOI] [PubMed] [Google Scholar]
- 3.Collins M.D., Jones D., Kroppenstedt R.M., Schleifer K.H. Chemical studies as a guide to the classification of Corynebacterium pyogenes and Corynebacterium haemolyticum. J. Gen. Microbiol. 1982;128:335–341. doi: 10.1099/00221287-128-2-335. [DOI] [PubMed] [Google Scholar]
- 4.Reddy C.A., Cornell C.P., Fraga A.M. Transfer of Corynebacterium pyogenes (Glage) Eberson to the genus Actinomyces as Actinomyces pyogenes (Glage) comb. nov. Int. J. Syst. Bacteriol. 1982;32:419–429. doi: 10.1099/00207713-32-4-419. [DOI] [Google Scholar]
- 5.Rogosa M., Cummins C.S., Lelliott R.A., Keddie R.M. Coryneform group of bacteria. In: Buchanan R.E., Gibbons N.E., editors. Bergey’s Manual of Determinative Bacteriology. 8th ed. The Williams and Wilkins Company; Baltimore, MD, USA: 1974. pp. 599–632. [Google Scholar]
- 6.Zhao K., Li W., Kang C., Du L., Huang T., Zhang X., Wu M., Yue B. Phylogenomics and Evolutionary Dynamics of the Family Actinomycetaceae. Genome Biol. Evol. 2014;6:2625–2633. doi: 10.1093/gbe/evu211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ding H., Lämmler C. Evaluation of the API Coryne test system for identification of Actinomyces pyogenes. Zentralbl. Veterinarmed. B. 1992;39:273–276. doi: 10.1111/j.1439-0450.1992.tb01168.x. [DOI] [PubMed] [Google Scholar]
- 8.Hijazin M., Hassan A.A., Alber J., Lämmler C., Timke M., Kostrzewa M., Prenger-Bernighoff E., Zschöck M. Evaluation of Matrix-Assisted Laser Desorption Ionization-Time of Flight Mass Spectrometry (MALDI-TOF MS) for species identification of bacteria of genera Arcanobacterium and Trueperella. Vet. Microbiol. 2012;157:243–245. doi: 10.1016/j.vetmic.2011.12.022. [DOI] [PubMed] [Google Scholar]
- 9.Zhang W., Meng X., Wang J. Sensitive and rapid detection of Trueperella pyogenes using loop-mediated isothermal amplification method. J. Microbiol. Methods. 2013;93:124–126. doi: 10.1016/j.mimet.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Nagib S., Rau J., Sammra O., Lämmler C., Schlez K., Zschöck M., Prenger-Berninghoff E., Klein G., Abdulmawjood A. Identification of Trueperella pyogenes isolated from bovine mastitis by Fourier transform infrared spectroscopy. PLoS ONE. 2014;9:e10465. doi: 10.1371/journal.pone.0104654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Randall L.P., Lemma F., Koylass M., Rogers J., Ayling R.D., Worth D., Klita M., Steventon A., Line K., Wragg P., et al. Evaluation of MALDI-ToF as a method for the identification of bacteria in the veterinary diagnostic laboratory. Res. Vet. Sci. 2015;101:42–49. doi: 10.1016/j.rvsc.2015.05.018. [DOI] [PubMed] [Google Scholar]
- 12.Abdulmawjood A., Wickhorst J., Hashim O., Sammra O., Hassan A.A., Alssahen M., Lämmler C., Prenger-Berninghoff E., Klein G. Application of a loop-mediated isothermal amplification (LAMP) assay for molecular identification of Trueperella pyogenes isolated from various origins. Mol. Cell Probes. 2016;30:205–210. doi: 10.1016/j.mcp.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Moreno L.Z., Matajira C.E.C., da Costa B.L.P., Ferreira T.S.P., Silva G.F.R., Dutra M.C., Gomes V.T.M., Silva A.P.S., Christ A.P.G., Sato M.I.Z., et al. Characterization of porcine Trueperella pyogenes by matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS), molecular typing and antimicrobial susceptibility profiling in Sao Paulo State. Comp. Immunol. Microbiol. Infect. Dis. 2017;51:49–53. doi: 10.1016/j.cimid.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 14.Rowlinson M.C., Bruckner D.A., Hinnebusch C., Nielsen K., Deville J.G. Clearance of Cellulosimicrobium cellulans Bacteriemia in a Child without Central Venous Catheter Removal. J. Clin. Microbiol. 2006;44:2650–2654. doi: 10.1128/JCM.02485-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saitou N., Nei M. The neighbor-joiningmethod: A newmethod for reconstructingphylogenetictrees. Mol. Biol. Evol. 1987;4:406–425. doi: 10.1093/oxfordjournals.molbev.a040454. [DOI] [PubMed] [Google Scholar]
- 16.Tamura K., Nei M., Kumar S. Prospects for inferringverylargephylogenies by using the neighbor-joiningmethod. Proc. Natl. Acad. Sci. USA. 2004;101:11030–11035. doi: 10.1073/pnas.0404206101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Felsenstein J. Confidencelimits on phylogenies: Anapproachusing the bootstrap. Evolution. 1985;39:783–791. doi: 10.1111/j.1558-5646.1985.tb00420.x. [DOI] [PubMed] [Google Scholar]
- 18.Kumar S., Stecher G., Li M., Knyaz C., Tamura K. MEGA X: MolecularEvolutionary Genetics Analysis acrosscomputingplatforms. Mol. Biol. Evol. 2018;35:1547–1549. doi: 10.1093/molbev/msy096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Queen C., Ward A.C., Hunter D.L. Bacteria isolated from nasal and tonsillar samples of clinically healthy Rocky Mountain bighorn and domestic sheep. J. Wildl. Dis. 1994;30:1–7. doi: 10.7589/0090-3558-30.1.1. [DOI] [PubMed] [Google Scholar]
- 20.Rzewuska M., Osińska B., Bielecki W., Skrzypczak M., Stefańska I., Binek M. Microflora of urogenital tract in European bison (Bison bonasus) In: Kita J., Anusz K., editors. Health Threats for the Eurpean Bison Particularly in Free-Roaming Populations in Poland. Warsaw University of Life Sciences; Warsaw, Poland: 2006. pp. 27–28. [Google Scholar]
- 21.Silva E., Gaivão M., Leitão S., Jost B.H., Carneiro C., Vilela C.L., Lopes da Costa L., Mateus L. Genomic characterization of Arcanobacterium pyogenes isolates recovered from the uterus of dairy cows with normal puerperium or clinical metritis. Vet. Microbiol. 2008;132:111–118. doi: 10.1016/j.vetmic.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 22.Narayanan S., Nagaraja T.G., Wallace N., Staats J., Chengappa M.M., Oberst R.D. Biochemical and ribotypic comparison of Actinomyces pyogenes and A. pyogenes-like organisms from liver abscesses, ruminal wall, and ruminal contents of cattle. Am. J. Vet. Res. 1998;59:271–276. [PubMed] [Google Scholar]
- 23.Jost B.H., Post K.W., Songer J.G., Billington S.J. Isolation of Arcanobacterium pyogenes from the porcine gastric mucosa. Vet. Res. Commun. 2002;26:419–425. doi: 10.1023/A:1020572223059. [DOI] [PubMed] [Google Scholar]
- 24.Spittel S., Hoedemaker M. Mastitis diagnosis in dairy cows using PathoProof real-time polymerase chain reaction assay in comparison with conventional bacterial culture in a Northern German field study. Berl. Munchener Tierarztliche Wochenschr. 2012;125:494–502. [PubMed] [Google Scholar]
- 25.Williamson L.H. Caseous lymphadenitis in small ruminants. Vet. Clin. N. Am. Food Anim. Pract. 2001;17:359–371. doi: 10.1016/S0749-0720(15)30033-5. [DOI] [PubMed] [Google Scholar]
- 26.Stefańska I., Gieryńska M., Rzewuska M., Binek M. Survival of Corynebacterium pseudotuberculosis within macrophages and induction of phagocytes death. Pol. J. Vet. Sci. 2010;13:143–149. [PubMed] [Google Scholar]
- 27.Muscatello G. Rhodococcus equi pneumonia in the foal—Part 1: Pathogenesis and epidemiology. Vet. J. 2012;192:20–26. doi: 10.1016/j.tvjl.2011.08.014. [DOI] [PubMed] [Google Scholar]
- 28.Witkowski L., Rzewuska M., Takai S., Chrobak-Chmiel D., Kizerwetter-Świda M., Feret M., Gawryś M., Witkowski M., Kita J. Molecular characterization of Rhodococcus equi isolates from horses in Poland: pVapA characteristics and plasmid new variant, 85-kb type V. BMC Vet. Res. 2017;13:35. doi: 10.1186/s12917-017-0954-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rzewuska M., Czopowicz M., Gawryś M., Markowska-Daniel I., Bielecki W. Relationships between antimicrobial resistance, distribution of virulence factor genes and the origin of Trueperella pyogenes isolated from domestic animals and European bison (Bison bonasus) Microb. Pathog. 2016;96:35–41. doi: 10.1016/j.micpath.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 30.Risseti R.M., Zastempowska E., Twarużek M., Lassa H., Pantoja J.C.F., de Vargas A.P.C., Guerra S.T., Bolanõs C.A.D., de Paula C.L., Alves A.C., et al. Virulence markers associated with Trueperella pyogenes infections in livestock and companion animals. Lett. Appl. Microbiol. 2017;65:125–132. doi: 10.1111/lam.12757. [DOI] [PubMed] [Google Scholar]
- 31.Rogovskyy A.S., Lawhon S., Kuczmanski K., Gillis D.C., Wu J., Hurley H., Rogovska Y.V., Konganti K., Yang C.Y., Duncan K. Phenotypic and genotypic characteristics of Trueperella pyogenes isolated from ruminants. J. Vet. Diagn. Investig. 2018;30:348–353. doi: 10.1177/1040638718762479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ashrafi Tamai I., Mohammadzadeh A., Zahraei Salehi T., Mahmoodi P. Genomic characterisation, detection of genes encoding virulence factors and evaluation of antibiotic resistance of Trueperella pyogenes isolated from cattle with clinical metritis. Antonie Van Leeuwenhoek. 2018;111:2441–2453. doi: 10.1007/s10482-018-1133-6. [DOI] [PubMed] [Google Scholar]
- 33.Guérin-Faublée V., Flandrois J.P., Broye E., Tupin F., Richard Y. Actinomyces pyogenes: Susceptibility of 103 clinical animal isolates to 22 antimicrobial agents. Vet. Res. 1993;24:251–259. [PubMed] [Google Scholar]
- 34.Werckenthin C., Alesík E., Grobbel M., Lübke-Becker A., Schwarz S., Wieler L.H., Wallmann J. Antimicrobial susceptibility of Pseudomonas aeruginosa from dogs and cats as well as Arcanobacterium pyogenes from cattle and swine as determined in the BfT-GermVet monitoring program 2004–2006. Berl. Munchener Tierarztliche Wochenschr. 2007;120:412–422. [PubMed] [Google Scholar]
- 35.Urumova V., Lyutzkanov M., Tsachev I., Marutsov P., Zhelev G. Investigations on the involvement of Arcanobacterium pyogenes in various infections in productive and companion animals and sensitivity of isolates to antibacterials. Revue Méd. Vét. 2009;160:582–585. [Google Scholar]
- 36.Hijazin M., Ülbegi-Mohyla H., Alber J., Lämmler C., Hassan A.A., Abdulmawjood A., Prenger-Berninghoff E., Weiss R., Zschöck M. Molecular identification and further characterization of Arcanobacterium pyogenes isolated from bovine mastitis and from various other origins. J. Dairy Sci. 2011;94:1813–1819. doi: 10.3168/jds.2010-3678. [DOI] [PubMed] [Google Scholar]
- 37.Zastempowska E., Lassa H. Genotypic characterization and evaluation of an antibiotic resistance of Trueperella pyogenes (Arcanobacterium pyogenes) isolated from milk of dairy cows with clinical mastitis. Vet. Microbiol. 2012;161:153–158. doi: 10.1016/j.vetmic.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 38.Pohl A., Lübke-Becker A., Heuwieser W. Minimum inhibitory concentrations of frequently used antibiotics against Escherichia coli and Trueperella pyogenes isolated from uteri of postpartum dairy cows. J. Dairy Sci. 2018;101:1355–1364. doi: 10.3168/jds.2017-12694. [DOI] [PubMed] [Google Scholar]
- 39.Liu M., Wu C., Liu Y., Zhao J., Yang Y., Shen J. Identification, susceptibility, and detection of integron-gene cassettes of Arcanobacterium pyogenes in bovine endometritis. J. Dairy Sci. 2009;92:3659–3666. doi: 10.3168/jds.2008-1756. [DOI] [PubMed] [Google Scholar]
- 40.Zhao K.L., Liu Y., Zhang X.Y., Palahati P., Wang H.N., Yue B.S. Detection and characterization of antibiotic resistance genes in Arcanobacterium pyogenes strains from abscesses of forest musk deer. J. Med. Microbiol. 2011;60:1820–1826. doi: 10.1099/jmm.0.033332-0. [DOI] [PubMed] [Google Scholar]
- 41.Zhang D.X., Tian K., Han L.M., Wang Q.X., Liu Y.C., Tian C.L., Liu M.C. Resistance to β-lactam antibiotic may influence nanH gene expression in Trueperella pyogenes isolated from bovine endometritis. Microb. Pathog. 2014;71–72:20–24. doi: 10.1016/j.micpath.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 42.Zhang D., Zhao J., Wang Q., Liu Y., Tian C., Zhao Y., Yu L., Liu M. Trueperella pyogenes isolated from dairy cows with endometritis in Inner Mongolia, China: Tetracycline susceptibility and tetracycline-resistance gene distribution. Microb. Pathog. 2017;105:51–56. doi: 10.1016/j.micpath.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 43.Alkasir R., Wang J., Gao J., Ali T., Zhang L., Szenci O., Bajcsy Á.C., Han B. Properties and antimicrobial susceptibility of Trueperella pyogenes isolated from bovine mastitis in China. Acta Vet. Hung. 2016;64:1–12. doi: 10.1556/004.2016.001. [DOI] [PubMed] [Google Scholar]
- 44.Yoshimura H., Kojima A., Ishimaru M. Antimicrobial susceptibility of Arcanobacterium pyogenes isolated from cattle and pigs. J. Vet. Med. B Infect. Dis. Vet. Public Health. 2000;47:139–143. doi: 10.1046/j.1439-0450.2000.00315.x. [DOI] [PubMed] [Google Scholar]
- 45.Ishiyama D., Mizomoto T., Ueda C., Takagi N., Shimizu N., Matsuura Y., Makuuchi Y., Watanabe A., Shinozuka Y., Kawai K. Factors affecting the incidence and outcome of Trueperella pyogenes mastitis in cows. J. Vet. Med. Sci. 2017;79:626–631. doi: 10.1292/jvms.16-0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ribeiro M.G., Risseti R.M., Bolanõs C.A.D., Caffaro K.A., de Morais A.C.B., Lara G.H.B., Zamprogna T.O., Paes A.C., Listoni F.J.P., Franco M.M.J. Trueperella pyogenes multispecies infections in domestic animals: A retrospective study of 144 cases (2002 to 2012) Vet. Q. 2015;35:82–87. doi: 10.1080/01652176.2015.1022667. [DOI] [PubMed] [Google Scholar]
- 47.Trinh H.T., Billington S.J., Field A.C., Songer J.G., Jost B.H. Susceptibility of Arcanobacterium pyogenes from different sources to tetracycline, macrolide and lincosamide antimicrobial agents. Vet. Microbiol. 2002;85:353–359. doi: 10.1016/S0378-1135(01)00524-7. [DOI] [PubMed] [Google Scholar]
- 48.Jost B.H., Billington S.J. Arcanobacterium pyogenes: Molecular pathogenesis of an animal opportunist. Antonie Van Leeuwenhoek. 2005;88:87–102. doi: 10.1007/s10482-005-2316-5. [DOI] [PubMed] [Google Scholar]
- 49.Santos T.M., Caixeta L.S., Machado V.S., Rauf A.K., Gilbert R.O., Bicalho R.C. Antimicrobial resistance and presence of virulence factor genes in Arcanobacterium pyogenes isolated from the uterus of postpartum dairy cows. Vet. Microbiol. 2010;145:84–89. doi: 10.1016/j.vetmic.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 50.Bicalho M.L., Lima F.S., Machado V.S., Meira E.B., Ganda E.K., Foditsch C., Bicalho R.C., Gilbert R.O. Associations among Trueperella pyogenes, endometritis diagnosis, and pregnancy outcomes in dairy cows. Theriogenology. 2016;85:267–274. doi: 10.1016/j.theriogenology.2015.09.043. [DOI] [PubMed] [Google Scholar]
- 51.Markowska-Daniel I., Urbaniak K., Stępniewska K., Pejsak Z. Antibiotic susceptibility of bacteria isolated from respiratory tract of pigs in Poland between 2004 and 2008. Pol. J. Vet. Sci. 2010;13:29–36. [PubMed] [Google Scholar]
- 52.Feßler A.T., Schwarz S. Antimicrobial Resistance in Corynebacterium spp., Arcanobacterium spp., and Trueperella pyogenes. Microbiol. Spectr. 2017;5 doi: 10.1128/microbiolspec.ARBA-0021-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lavín S., Ruiz-Bascarán M., Marco I., Abarca M.L., Crespo M.J., Franch J. Foot infections associated with Arcanobacterium pyogenes in free-living fallow deer (Dama dama) J. Wildl. Dis. 2004;40:607–611. doi: 10.7589/0090-3558-40.3.607. [DOI] [PubMed] [Google Scholar]
- 54.Belser E.H., Cohen B.S., Keeler S.P., Killmaster C.H., Bowers J.W., Miller K.V. Epethelial presence of Trueperella pyogenes predicts site-level presence of cranial abscess disease in white-tailed deer (Odocoileus virginianus) PLoS ONE. 2015;10:e0120028. doi: 10.1371/journal.pone.0120028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bicalho M.L., Machado V.S., Oikonomou G., Gilbert R.O., Bicalho R.C. Association between virulence factors of Escherichia coli, Fusobacterium necrophorum, and Arcanobacterium pyogenes and uterine diseases of dairy cows. Vet. Microbiol. 2012;157:125–131. doi: 10.1016/j.vetmic.2011.11.034. [DOI] [PubMed] [Google Scholar]
- 56.Ibrahim M., Peter S., Wagener K., Drillich M., Ehling-Schulz M., Einspanier R., Gabler C. Bovine Endometrial Epithelial Cells Scale Their Pro-inflammatory Response In vitro to Pathogenic Trueperella pyogenes Isolated from the Bovine Uterus in a Strain-Specific Manner. Front. Cell. Infect. Microbiol. 2017;7:264. doi: 10.3389/fcimb.2017.00264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rudnick S.T., Jost B.H., Billington S.J. Transcriptional regulation of pyolysin production in the animal pathogen, Arcanobacterium pyogenes. Vet. Microbiol. 2008;132:96–104. doi: 10.1016/j.vetmic.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 58.Kontturi M., Junni R., Simojoki H., Malinen E., Seuna E., Klitgaard K., Kujala-Wirth M., Soveri T., Pelkonen S. Bacterial species associated with interdigital phlegmon outbreaks in Finnish dairy herds. BMC Vet. Res. 2019;29:44. doi: 10.1186/s12917-019-1788-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tadepalli S., Narayanan S.K., Stewart G.C., Chengappa M.M., Nagaraja T.G. Fusobacterium necrophorum: A ruminal bacterium that invades liver to cause abscesses in cattle. Anaerobe. 2009;15:36–43. doi: 10.1016/j.anaerobe.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 60.Scanlan C.M., Hathcock T.L. Bovine rumenitis-liver abscess complex: A bacteriological review. Cornell Vet. 1983;73:288–297. [PubMed] [Google Scholar]
- 61.Roberts D.S. The pathogenic synergy of Fusiformis necrophorus and Corynebacterium pyogenes. II. The response of F. necrophorus to a filterable product of C. pyogenes. Br. J. Exp. Pathol. 1967;48:674–679. [PMC free article] [PubMed] [Google Scholar]
- 62.Azawi O.I., Al-Abidy H.F., Ali A.J. Pathological and bacteriological studies of hydrosalpinx in buffaloes. Reprod. Domest. Anim. 2010;45:416–420. doi: 10.1111/j.1439-0531.2008.01207.x. [DOI] [PubMed] [Google Scholar]
- 63.de Boer M., Heuer C., Hussein H., McDougall S. Minimum inhibitory concentrations of selected antimicrobials against Escherichia coli and Trueperella pyogenes of bovine uterine origin. J. Dairy Sci. 2015;98:4427–4438. doi: 10.3168/jds.2014-8890. [DOI] [PubMed] [Google Scholar]
- 64.Zhao K., Li W., Huang T., Song X., Zhang X., Yue B. Comparative transcriptome analysis of Trueperella pyogenes reveals a novel antimicrobial strategy. Arch. Microbiol. 2017;199:649–655. doi: 10.1007/s00203-017-1338-5. [DOI] [PubMed] [Google Scholar]
- 65.Huang T., Song X., Zhao K., Jing J., Shen Y., Zhang X., Yue B. Quorum-sensing molecules N-acyl homoserine lactones inhibit Trueperella pyogenes infection in mouse model. Vet. Microbiol. 2018;213:89–94. doi: 10.1016/j.vetmic.2017.11.029. [DOI] [PubMed] [Google Scholar]
- 66.Malinowski E., Lassa H., Markiewicz H., Kaptur M., Nadolny M., Niewitecki W., Ziętara J. Sensitivity to antibiotics of Arcanobacterium pyogenes and Escherichia coli from the uteri of cows with metritis/endometritis. Vet. J. 2011;187:234–238. doi: 10.1016/j.tvjl.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 67.Zambrano-Nava S., Boscán-Ocando J., Nava J. Normal bacterial flora from vaginas of Criollo Limonero cows. Trop. Anim. Health Prod. 2011;43:291–294. doi: 10.1007/s11250-010-9701-4. [DOI] [PubMed] [Google Scholar]
- 68.Amos M.R., Healey G.D., Goldstone R.J., Mahan S.M., Düvel A., Schuberth H.J., Sandra O., Zieger P., Dieuzy-Labaye I., Smith D.G., et al. Differential endometrial cell sensitivity to a cholesterol-dependent cytolysin links Trueperella pyogenes to uterine disease in cattle. Biol. Reprod. 2014;90:54. doi: 10.1095/biolreprod.113.115972. [DOI] [PubMed] [Google Scholar]
- 69.Griffin S., Healey G.D., Sheldon I.M. Isoprenoids increase bovine endometrial stromal cell tolerance to the cholesterol-dependent cytolysin from Trueperella pyogenes. Biol. Reprod. 2018;99:749–760. doi: 10.1093/biolre/ioy099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lima F.S., Greco L.F., Bisinotto R.S., Ribeiro E.S., Martinez N.M., Thatcher W.W., Santos J.E., Reinhard M.K., Galvão K.N. Effects of intrauterine infusion of Trueperella pyogenes on endometrial mRNA expression of proinflammatory cytokines and luteolytic cascade genes and their association with luteal life span in dairy cows. Theriogenology. 2015;84:1263–1272. doi: 10.1016/j.theriogenology.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 71.Wagener K., Grunert T., Prunner I., Ehling-Schulz M., Drillich M. Dynamics of uterine infections with Escherichia coli, Streptococcus uberis and Trueperella pyogenes in post-partum dairy cows and their association with clinical endometritis. Vet. J. 2014;202:527–532. doi: 10.1016/j.tvjl.2014.08.023. [DOI] [PubMed] [Google Scholar]
- 72.Carneiro L.C., Cronin J.G., Sheldon I.M. Mechanisms linking bacterial infections of the bovine endometrium to disease and infertility. Reprod. Biol. 2016;16:1–7. doi: 10.1016/j.repbio.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 73.Bonnett B.N., Martin S.W., Meek A.H. Associations of clinical findings, bacteriological and histological results of endometrial biopsy with reproductive performance of postpartum dairy cows. Prev. Vet. Med. 1993;15:205–220. doi: 10.1016/0167-5877(93)90114-9. [DOI] [Google Scholar]
- 74.Sheldon I.M., Lewis G.S., LeBlanc S., Gilbert R.O. Defining postpartum uterine disease in cattle. Theriogenology. 2006;65:1516–1530. doi: 10.1016/j.theriogenology.2005.08.021. [DOI] [PubMed] [Google Scholar]
- 75.Danesh Mesgaran S., Gärtner M.A., Wagener K., Drillich M., Ehling-Schulz M., Einspanier R., Gabler C. Different inflammatory responses of bovine oviductal epithelial cells in vitro to bacterial species with distinct pathogenicity characteristics and passage number. Theriogenology. 2018;106:237–246. doi: 10.1016/j.theriogenology.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 76.Bonnett B.N., Martin S.W., Gannon V.P., Miller R.B., Etherington W.G. Endometrial biopsy in Holstein-Friesian dairy cows. III. Bacteriological analysis and correlations with histological findings. Can. J. Vet. Res. 1991;55:168–173. [PMC free article] [PubMed] [Google Scholar]
- 77.Sheldon I.M., Cronin J., Goetze L., Donofrio G., Schuberth H.J. Defining postpartum uterine disease and the mechanisms of infection and immunity in the female reproductive tract in cattle. Biol. Reprod. 2009;81:1025–1032. doi: 10.1095/biolreprod.109.077370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jaureguiberry M., Madoz L.V., Giuliodori M.J., Wagener K., Prunner I., Grunert T., Ehling-Schulz M., Drillich M., de la Sota R.L. Identification of Escherichia coli and Trueperella pyogenes isolated from the uterus of dairy cows using routine bacteriological testing and Fourier transform infrared spectroscopy. Acta Vet. Scand. 2016;58:81. doi: 10.1186/s13028-016-0262-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sheldon I.M., Williams E.J., Miller A.N., Nash D.M., Herath S. Uterine diseases in cattle after parturition. Vet. J. 2008;176:115–121. doi: 10.1016/j.tvjl.2007.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Prunner I., Wagener K., Pothmann H., Ehling-Schulz M., Drillich M. Risk factors for uterine diseases on small- and medium-sized dairy farms determined by clinical, bacteriological, and cytological examinations. Theriogenology. 2014;82:857–865. doi: 10.1016/j.theriogenology.2014.06.015. [DOI] [PubMed] [Google Scholar]
- 81.Seno N., Azuma R. A study on heifer mastitis in Japan and its causative microorganisms. Natl. Inst. Anim. Health Q. (Tokyo) 1983;23:82–91. [PubMed] [Google Scholar]
- 82.Quinn A.K., Vermunt J.J., Twiss D.P. Arcanobacterium pyogenes mastitis in a 18-month-old heifer. N. Z. Vet. J. 2002;50:167–168. doi: 10.1080/00480169.2002.36305. [DOI] [PubMed] [Google Scholar]
- 83.Ericsson Unnerstad H., Lindberg A., Persson Waller K., Ekman T., Artursson K., Nilsson-Ost M., Bengtsson B. Microbial aetiology of acute clinical mastitis and agent-specific risk factors. Vet. Microbiol. 2009;137:90–97. doi: 10.1016/j.vetmic.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 84.Hertl J.A., Schukken Y.H., Welcome F.L., Tauer L.W., Gröhn Y.T. Effects of pathogen-specific clinical mastitis on probability of conception in Holstein dairy cows. J. Dairy Sci. 2014;97:6942–6954. doi: 10.3168/jds.2014-8203. [DOI] [PubMed] [Google Scholar]
- 85.Hillerton J.E., Bramley A.J., Watson C.A. The epidemiology of summer mastitis: A survey of clinical cases. Br. Vet. J. 1987;143:520–530. doi: 10.1016/0007-1935(87)90041-8. [DOI] [PubMed] [Google Scholar]
- 86.Chirico J., Jonsson P., Kjellberg S., Thomas G. Summer mastitis experimentally induced by Hydrotaea irritans exposed to bacteria. Med. Vet. Entomol. 1997;11:187–192. doi: 10.1111/j.1365-2915.1997.tb00312.x. [DOI] [PubMed] [Google Scholar]
- 87.Madsen M., Aalbaek B., Hansen J.W. Comparative bacteriological studies on summer mastitis in grazing cattle and pyogenes mastitis in stabled cattle in Denmark. Vet. Microbiol. 1992;32:81–88. doi: 10.1016/0378-1135(92)90009-I. [DOI] [PubMed] [Google Scholar]
- 88.Madsen M., Høi Sørensen G., Aalbaek B., Hansen J.W., Bjørn H. Summer mastitis in heifers: Studies on the seasonal occurrence of Actinomyces pyogenes, Peptostreptococcus indolicus and Bacteroidaceae in clinically healthy cattle in Denmark. Vet. Microbiol. 1992;30:243–255. doi: 10.1016/0378-1135(92)90118-D. [DOI] [PubMed] [Google Scholar]
- 89.Nagaraja T.G., Chengappa M.M. Liver abscesses in feedlot cattle: A review. J. Anim. Sci. 1998;76:287–298. doi: 10.2527/1998.761287x. [DOI] [PubMed] [Google Scholar]
- 90.Nagaraja T.G., Lechtenberg K.F. Liver abscesses in feedlot cattle. Vet. Clin. N. Am. Food Anim. Pract. 2007;23:351–369. doi: 10.1016/j.cvfa.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 91.Amachawadi R.G., Nagaraja T.G. Liver abscesses in cattle: A review of incidence in Holsteins and of bacteriology and vaccine approaches to control in feedlot cattle. J. Anim. Sci. 2016;94:1620–1632. doi: 10.2527/jas.2015-0261. [DOI] [PubMed] [Google Scholar]
- 92.Oberbauer A.M., Berry S.L., Belanger J.M., McGoldrick R.M., Pinos-Rodriquez J.M., Famula T.R. Determining the heritable component of dairy cattle foot lesions. J. Dairy Sci. 2013;96:605–613. doi: 10.3168/jds.2012-5485. [DOI] [PubMed] [Google Scholar]
- 93.Kontturi M., Kujala M., Junni R., Malinen E., Seuna E., Pelkonen S., Soveri T., Simojoki H. Survey of interdigital phlegmon outbreaks and their risk factors in free stall dairy herds in Finland. Acta Vet. Scand. 2017;59:46. doi: 10.1186/s13028-017-0313-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bay V., Griffiths B., Carter S., Evans N.J., Lenzi L., Bicalho R.C., Oikonomou G. 16S rRNA amplicon sequencing reveals a polymicrobial nature of complicated claw horn disruption lesions and interdigital phlegmon in dairy cattle. Sci. Rep. 2018;8:15529. doi: 10.1038/s41598-018-33993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Power H.T., Rebhun W.C. Bacterial endocarditis in adult dairy cattle. J. Am. Vet. Med. Assoc. 1983;182:806–808. [PubMed] [Google Scholar]
- 96.Ertas H.B., Kilic A., Özbey G., Muz A. Isolation of Arcanobacterium (Actinomyces) pyogenes from abscessed cattle kidney and identification by PCR, Turk. J. Vet. Anim. Sci. 2005;29:455–459. [Google Scholar]
- 97.Hinton M. Corynebacterium pyogenes and bovine abortion. J. Hyg. Camb. 1974;72:365–368. doi: 10.1017/S0022172400023597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Turner G.V. A microbiological study of polyarthritis in slaughter pigs. J. S. Afr. Vet. Assoc. 1982;53:99–101. [PubMed] [Google Scholar]
- 99.Høie S., Falk K., Lium B.M. An abattoir survey of pneumonia and pleuritis in slaughter weight swine from 9 selected herds. IV. Bacteriological findings in chronic pneumonic lesions. Acta Vet. Scand. 1991;32:395–402. doi: 10.1186/BF03546970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hariharan H., MacDonald J., Carnat B., Bryenton J., Heaney S. An investigation of bacterial causes of arthritis in slaughter hogs. J. Vet. Diagn. Investig. 1992;4:28–30. doi: 10.1177/104063879200400107. [DOI] [PubMed] [Google Scholar]
- 101.Iwamatsu S., Morio A., Watanabe K., Ikeo T., Yamashita T., Yoshino H. Suppurative cerebral lesions caused by infection with Actinomyces pyogenes in breeding swine. J. Jpn. Vet. Med. Assoc. 1986;39:238–242. doi: 10.12935/jvma1951.39.238. [DOI] [Google Scholar]
- 102.Dong W.L., Kong L.C., Wang Y., Gou C.L., Xu B., Ma H.X., Gao Y.H. Aminoglycoside resistance of Trueperella pyogenes isolated from pigs in China. J. Vet. Med. Sci. 2017;79:1836–1839. doi: 10.1292/jvms.16-0597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Jarosz Ł.S., Gradzki Z., Kalinowski M. Trueperella pyogenes infections in swine: Clinical course and pathology. Pol. J. Vet. Sci. 2014;17:395–404. doi: 10.2478/pjvs-2014-0055. [DOI] [PubMed] [Google Scholar]
- 104.Pejsak Z., Markowska-Daniel I., Samorek M., Truszczyński M. Wykrywanie i ocena właściwości krajowych izolatów Arcanobacterium pyogenes wyosobnionych od świń. Med. Weter. 2006;62:781–784. [Google Scholar]
- 105.Tadayon R.A., Cheema A.H., Muhammed S.I. Microorganisms associated with abscesses of sheep and goats in the south of Iran. Am. J. Vet. Res. 1980;41:798–802. [PubMed] [Google Scholar]
- 106.Al Dughaym A.M. Isolation of Serratia, Arcanobacterium and Burkholderia species from visceral and cutaneous abscesses in four emaciated ewes. Vet. Rec. 2004;155:425–426. doi: 10.1136/vr.155.14.425. [DOI] [PubMed] [Google Scholar]
- 107.Lin C.C., Chen T.H., Shyu C.L., Su N.Y., Chan J.P. Disseminated abscessation complicated with bone marrow abscess caused by Arcanobacterium pyogenes in a goat. J. Vet. Med. Sci. 2010;72:1089–1092. doi: 10.1292/jvms.09-0540. [DOI] [PubMed] [Google Scholar]
- 108.Barbour E.K., Itani H.H., Shaib H.A., Saade M.F., Sleiman F.T., Nour A.A., Harakeh S. Koch’s postulate of Arcanobacterium pyogenes and its immunogenicity in local and imported Saanen goats. Vet. Ital. 2010;46:319–327. [PubMed] [Google Scholar]
- 109.Raadsma H.W., Egerton J.R. A review of footrot in sheep: Aetiology, risk factors and control methods. Livest. Sci. 2013;156:106–114. doi: 10.1016/j.livsci.2013.06.009. [DOI] [Google Scholar]
- 110.Wani A.H., Verma S., Sharma M., Wani A. Infectious lameness among migratory sheep and goats in north-west India, with particular focus on anaerobes. Rev. Sci. Tech. 2015;34:855–867. doi: 10.20506/rst.34.3.2401. [DOI] [PubMed] [Google Scholar]
- 111.Stefańska I., Rzewuska M., Binek M. Corynebacterium pseudotuberculosis—Zakażenia u zwierząt. Postęp. Mikrobiol. 2007;46:101–112. [Google Scholar]
- 112.Lavin S., Marco I., Franch J., Abarca L. Report of a case of pyogenic arthritis associated with Actinomyces pyogenes in a chamois (Rupicapra pyrenaica) Zentralbl. Veterinarmed. B. 1998;45:251–253. doi: 10.1111/j.1439-0450.1998.tb00790.x. [DOI] [PubMed] [Google Scholar]
- 113.Seifi H.A., Saifzadeh S., Farshid A.A., Rad M., Farrokhi F. Mandibular pyogranulomatous osteomyelitis in a Sannen goat. J. Vet. Med. A Physiol. Pathol. Clin. Med. 2003;50:219–221. doi: 10.1046/j.1439-0442.2003.00520.x. [DOI] [PubMed] [Google Scholar]
- 114.Kidanemariam A., Gouws J., van Vuuren M., Gummow B. Ulcerative balanitis and vulvitis of Dorper sheep in South Africa: A study on its aetiology and clinical features. J. S. Afr. Vet. Assoc. 2005;76:197–203. doi: 10.4102/jsava.v76i4.426. [DOI] [PubMed] [Google Scholar]
- 115.Billington S.J., Post K.W., Jost B.H. Isolation of Arcanobacterium (Actinomyces) pyogenes from cases of feline otitis externa and canine cystitis. J. Vet. Diagn. Investig. 2002;14:159–162. doi: 10.1177/104063870201400212. [DOI] [PubMed] [Google Scholar]
- 116.Hesselink J.W., van den Tweel J.G. Hypertrophic osteopathy in a dog with a chronic lung abscess. J. Am. Vet. Med. Assoc. 1990;196:760–762. [PubMed] [Google Scholar]
- 117.Dickie C.W. Feline pyothorax caused by a Borrelia-like organism and Corynebacterium pyogenes. J. Am. Vet. Med. Assoc. 1979;174:516–517. [PubMed] [Google Scholar]
- 118.Wareth G., El-Diasty M., Melzer F., Murugaiyan J., Abdulmawjood A., Sprague L.D., Neubauer H. Trueperella pyogenes and Brucella abortus coinfection in a dog and a cat on a dairy farm in Egypt with recurrent cases of mastitis and abortion. Vet. Med. Int. 2018;2018:2056436. doi: 10.1155/2018/2056436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Rampacci E., Passamonti F., Bottinelli M., Stefanetti V., Cercone M., Nannarone S., Gialletti R., Beccati F., Coletti M., Pepe M. Umbilical infections in foals: Microbiological investigation and management. Vet. Rec. 2017;180:543. doi: 10.1136/vr.103999. [DOI] [PubMed] [Google Scholar]
- 120.Shahbazfar A.A., Kolahian S., Ashrafi Helan J., Mohammadpour H. Multi abscessation with multinodular abscesses in a New Zealand white rabbit (Oryctolagus cuniculus) following Arcanobacterium pyogenes infection. Revue Méd. Vét. 2013;164:23–26. [Google Scholar]
- 121.Barbour E.K., Brinton M.K., Caputa A., Johnson J.B., Poss P.E. Characteristics of Actinomyces pyogenes involved in lameness of male turkeys in north-central United States. Avian Dis. 1991;35:192–196. doi: 10.2307/1591313. [DOI] [PubMed] [Google Scholar]
- 122.Brinton M.K., Schellberg L.C., Johnson J.B., Frank R.K., Halvorson D.A., Newman J.A. Description of osteomyelitis lesions associated with Actinomyces pyogenes infection in the proximal tibia of adult male turkeys. Avian Dis. 1993;37:259–262. doi: 10.2307/1591485. [DOI] [PubMed] [Google Scholar]
- 123.Priya P.M., Abhinay G., Ambily R., Siju J. A Unique Case of Trueperella Pyogenes Causing Hepatic Abscesses in Pigeons. Int. J. Vet. Med. Res. Rep. 2013:1–3. doi: 10.5171/2013.486054. [DOI] [Google Scholar]
- 124.Cohen B.S., Belser E.H., Keeler S.P., Yabsley M.J., Miller K.V. A Headache from Our Past? Intracranial Abscess Disease, Virulence Factors of Trueperella Pyogenes, And A Legacy of Translocating White-Tailed Deer (Odocoileus Virginianus) J. Wildl. Dis. 2018;54:671–679. doi: 10.7589/2017-09-216. [DOI] [PubMed] [Google Scholar]
- 125.Karns G.R., Lancia R.A., Deperno C.S., Conner M.C., Stoskopf M.K. Intracranial abscessation as a natural mortality factor for adult male white-tailed deer (Odocoileus virginianus) in Kent County, Maryland, USA. J. Wildl. Dis. 2009;45:196–200. doi: 10.7589/0090-3558-45.1.196. [DOI] [PubMed] [Google Scholar]
- 126.Turner M.M., Deperno C.S., Conner M.C., Eyler T.B., Lancia R.A., Klaver R.W., Stoskopf M.K. Habitat, wildlife, and one health: Arcanobacterium pyogenes in Maryland and Upper Eastern Shore white-tailed deer populations. Infect. Ecol. Epidemiol. 2013;3:19175. doi: 10.3402/iee.v3i0.19175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cohen B.S., Belser E.H., Keeler S.P., Yabsley M.J., Miller K.V. Isolation and genotypic characterization of Trueperella (Arcanobacterium) pyogenes recovered from active cranial abscess infections of male white-tailed deer (Odocoileus virginianus) J. Zoo Wildl. Med. 2015;46:62–67. doi: 10.1638/2014-0124R1.1. [DOI] [PubMed] [Google Scholar]
- 128.Chirino-Trejo M., Woodbury M.R., Huang F. Antibiotic sensitivity and biochemical characterization of Fusobacterium spp. and Arcanobacterium pyogenes isolated from farmed white-tailed deer (Odocoileus virginianus) with necrobacillosis. J. Zoo Wildl. Med. 2003;34:262–268. doi: 10.1638/02-019. [DOI] [PubMed] [Google Scholar]
- 129.Tell L.A., Brooks J.W., Lintner V., Matthews T., Kariyawasam S. Antimicrobial susceptibility of Arcanobacterium pyogenes isolated from the lungs of white-tailed deer (Odocoileus virginianus) with pneumonia. J. Vet. Diagn. Investig. 2011;23:1009–1013. doi: 10.1177/1040638711416618. [DOI] [PubMed] [Google Scholar]
- 130.Nettles V.F., Quist C.F., Lopez R.R., Wilmers T.J., Frank P., Roberts W., Chitwood S., Davidson W.R. Morbidity and mortality factors in key deer (Odocoileus virginianus clavium) J. Wildl. Dis. 2002;38:685–692. doi: 10.7589/0090-3558-38.4.685. [DOI] [PubMed] [Google Scholar]
- 131.Wickhorst J.P., Hassan A.A., Sheet O.H., Eisenberg T., Sammra O., Alssahen M., Lämmler C., Prenger-Berninghoff E., Zschöck M., Timke M., et al. Trueperella pyogenes isolated from a brain abscess of an adult roebuck (Capreolus capreolus) Folia Microbiol. (Praha) 2018;63:17–22. doi: 10.1007/s12223-017-0533-8. [DOI] [PubMed] [Google Scholar]
- 132.Badger S.B. Infectious epiphysitis and valvular endocarditis in a red deer (Cervus elaphus) N. Z. Vet. J. 1982;30:17–18. doi: 10.1080/00480169.1982.34863. [DOI] [PubMed] [Google Scholar]
- 133.Muñoz Gutiérrez J.F., Sondgeroth K.S., Williams E.S., Montgomery D.L., Creekmore T.E., Miller M.M. Infectious keratoconjunctivitis in free-ranging mule deer in Wyoming: A retrospective study and identification of a novel alphaherpesvirus. J. Vet. Diagn. Investig. 2018;30:663–670. doi: 10.1177/1040638718787862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhao K., Tian Y., Yue B., Wang H., Zhang X. Virulence determinants and biofilm production among Trueperella pyogenes recovered from abscesses of captive forest musk deer. Arch. Microbiol. 2013;195:203–209. doi: 10.1007/s00203-013-0869-7. [DOI] [PubMed] [Google Scholar]
- 135.Rzewuska M., Stefańska I., Osińska B., Kizerwetter-Świda M., Chrobak D., Kaba J., Bielecki W. Phenotypic characteristics and virulence genotypes of Trueperella (Arcanobacterium) pyogenes strains isolated from European bison (Bison bonasus) Vet. Microbiol. 2012;160:69–76. doi: 10.1016/j.vetmic.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 136.Portas T.J., Bryant B.R. Morbidity and mortality associated with Arcanobacterium pyogenes in a group of captive blackbuck (Antilope cervicapra) J. Zoo Wildl. Med. 2005;36:286–289. doi: 10.1638/04-058.1. [DOI] [PubMed] [Google Scholar]
- 137.Twomey D.F., Boon J.D., Sayers G., Schock A. Arcanobacterium pyogenes septicemia in a southern pudu (Pudu puda) following uterine prolapse. J. Zoo Wildl. Med. 2010;41:158–160. doi: 10.1638/2009-0008.1. [DOI] [PubMed] [Google Scholar]
- 138.Franzen D., Lamberski N., Zuba J., Richardson G.L., Fischer A.T., Rantanen N.W. Diagnosis and Medical and Surgical Management of Chronic Infectious Fibrinous Pleuritis in an Okapi (Okapia Johnstoni) J. Zoo Wildl. Med. 2015;46:427–430. doi: 10.1638/2014-0232R.1. [DOI] [PubMed] [Google Scholar]
- 139.Zarnke R.L., Schlater L.K. Abscesses in a free-ranging bison in Alaska. J. Wildl. Dis. 1984;20:151–152. doi: 10.7589/0090-3558-20.2.151. [DOI] [PubMed] [Google Scholar]
- 140.Besser T.E., Frances Cassirer E., Highland M.A., Wolff P., Justice-Allen A., Mansfield K., Davis M.A., Foreyt W. Bighorn sheep pneumonia: Sorting out the cause of a polymicrobial disease. Prev. Vet. Med. 2013;108:85–93. doi: 10.1016/j.prevetmed.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 141.Moustafa A.M. First observation of camel (Camelus dromedarius) lymphadenitis in Libya. A case report. Rev. Elev. Med. Vet. Pays. Trop. 1994;47:313–314. [PubMed] [Google Scholar]
- 142.Wareth G., Murugaiyan J., Khater D.F., Moustafa S.A. Subclinical pulmonary pathogenic infection in camels slaughtered in Cairo, Egypt. J. Infect. Dev. Ctries. 2014;8:909–913. doi: 10.3855/jidc.4810. [DOI] [PubMed] [Google Scholar]
- 143.Ali A., Derar R., Al-Sobayil F., Al-Hawas A., Hassanein K. A retrospective study on clinical findings of 7300 cases (2007–2014) of barren female dromedaries. Theriogenology. 2015;84:452–456. doi: 10.1016/j.theriogenology.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 144.Tarazi Y.H., Al-Ani F.K. An outbreak of dermatophilosis and caseous lymphadenitis mixed infection in camels (Camelus dromedaries) in Jordan. J. Infect. Dev. Ctries. 2016;10:506–511. doi: 10.3855/jidc.7023. [DOI] [PubMed] [Google Scholar]
- 145.Aschfalk A., Josefsen T.D., Steingass H., Müller W., Goethe R. Crowding and winter emergency feeding as predisposing factors for kerato-conjunctivitis in semi-domesticated reindeer in Norway. Dtsch. Tierarztl. Wochenschr. 2003;110:295–298. [PubMed] [Google Scholar]
- 146.Tryland M., das Neves C.G., Sunde M., Mørk T. Cervid herpesvirus 2, the primary agent in an outbreak of infectious keratoconjunctivitis in semidomesticated reindeer. J. Clin. Microbiol. 2009;47:3707–3713. doi: 10.1128/JCM.01198-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Eisenberg T., Nagib S., Hijazin M., Alber J., Lämmler C., Hassan A.A., Timke M., Kostrzewa M., Prenger-Berninghoff E., Schauerte N., et al. Trueperella pyogenes as cause of a facial abscess in a grey slender loris (Loris lydekkerianus nordicus)—A case report. Berl. Munchener Tierarztliche Wochenschr. 2012;125:407–410. [PubMed] [Google Scholar]
- 148.Nagib S., Glaeser S.P., Eisenberg T., Sammra O., Lämmler C., Kämpfer P., Schauerte N., Geiger C., Kaim U., Prenger-Berninghoff E., et al. Fatal infection in three Grey Slender Lorises (Loris lydekkerianus nordicus) caused by clonally related Trueperella pyogenes. BMC Vet. Res. 2017;13:273. doi: 10.1186/s12917-017-1171-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ülbegi-Mohyla H., Hijazin M., Alber J., Lämmler C., Hassan A.A., Abdulmawjood A., Prenger-Berninghoff E., Weiss R., Zschöck M. Identification of Arcanobacteriumpyogenes isolated by post mortem examinations of a bearded dragon and a gecko by phenotypic and genotypic properties. J. Vet. Sci. 2010;11:265–267. doi: 10.4142/jvs.2010.11.3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Funke G., von Graevenitz A., Clarridge J.E., Bernard K.A. Clinical microbiology of coryneform bacteria. Clin. Microbiol. Rev. 1997;10:125–159. doi: 10.1128/CMR.10.1.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Jootar P., Gherunpong V., Saitanu K. Corynebacterium pyogenes endocarditis. Report of a case with necropsy and review of the literature. J. Med. Assoc. Thail. 1978;61:596–601. [PubMed] [Google Scholar]
- 152.Kavitha K., Latha R., Udayashankar C., Jayanthi K., Oudeacoumar P. Three cases of Arcanobacterium pyogenes-associated soft tissue infection. J. Med. Microbiol. 2010;59:736–739. doi: 10.1099/jmm.0.016485-0. [DOI] [PubMed] [Google Scholar]
- 153.Plamondon M., Martinez G., Raynal L., Touchette M., Valiquette L. A fatal case of Arcanobacterium pyogenes endocarditis in a man with no identified animal contact: Case report and review of the literature. Eur. J. Clin. Microbiol. Infect. Dis. 2007;26:663–666. doi: 10.1007/s10096-007-0354-9. [DOI] [PubMed] [Google Scholar]
- 154.Chesdachai S., Larbcharoensub N., Chansoon T., Chalermsanyakorn P., Santanirand P., Chotiprasitsakul D., Ratanakorn D., Boonbaichaiyapruck S. Arcanobacterium pyogenes endocarditis: A case report and literature review. Southeast. Asian. J. Trop. Med. Public Health. 2014;45:142–148. [PubMed] [Google Scholar]
- 155.Andy Tang S.O., Leong T.S., Ruixin T., Chua H.H., Chew L.P. Thrombotic thrombocytopenic purpura-like syndrome associated with Arcanobacterium pyogenes endocarditis in a post-transplant patient: A case report. Med. J. Malaysia. 2018;73:344–346. [PubMed] [Google Scholar]
- 156.Kotrajaras R., Tagami H. Corynebacterium pyogenes. Its pathogenic mechanism in epidemic leg ulcers in Thailand. Int. J. Dermatol. 1987;26:45–50. doi: 10.1111/j.1365-4362.1987.tb04575.x. [DOI] [PubMed] [Google Scholar]
- 157.Drancourt M., Oulès O., Bouche V., Peloux Y. Two cases of Actinomyces pyogenes infection in humans. Eur. J. Clin. Microbiol. Infect. Dis. 1993;12:55–57. doi: 10.1007/BF01997060. [DOI] [PubMed] [Google Scholar]
- 158.Hermida Amejeiras A., Romero Jung P., Cabarcos Ortiz De Barrón A., Treviño Castallo M. One case of pneumonia with Arcanobacterium pyogenes. An. Med. Int. 2004;21:334–336. doi: 10.4321/s0212-71992004000700006. [DOI] [PubMed] [Google Scholar]
- 159.Nicholson P., Kiely P., Street J., Mahalingum K. Septic arthritis due to Actinomyces pyogenes. Injury. 1998;29:640–642. doi: 10.1016/S0020-1383(98)00142-9. [DOI] [PubMed] [Google Scholar]
- 160.Lynch M., O’Leary J., Murnaghan D., Cryan B. Actinomyces pyogenes septic arthritis in a diabetic farmer. J. Infect. 1998;37:71–73. doi: 10.1016/S0163-4453(98)90862-3. [DOI] [PubMed] [Google Scholar]
- 161.Levy C.E., Pedro R.J., von Nowakonski A., Holanda L.M., Brocchi M., Ramo M.C. Arcanobacterium pyogenes sepsis in farmer, Brazil. Emerg. Infect. Dis. 2009;15:1131–1132. doi: 10.3201/eid1507.081072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Gahrn-Hansen B., Frederiksen W. Human infections with Actinomyces pyogenes (Corynebacterium pyogenes) Diagn. Microbiol. Infect. Dis. 1992;15:349–354. doi: 10.1016/0732-8893(92)90022-L. [DOI] [PubMed] [Google Scholar]
- 163.Sullivan D.C., Chapman S.W. Bacteria that masquerade as fungi: Actinomycosis/nocardia. Proc. Am. Thorac. Soc. 2010;7:216–221. doi: 10.1513/pats.200907-077AL. [DOI] [PubMed] [Google Scholar]
- 164.Mochon A.B., Sussland D., Saubolle M.A. Aerobic Actinomycetes of Clinical Significance. Microbiol. Spectr. 2016;4 doi: 10.1128/microbiolspec.DMIH2-0021-2015. [DOI] [PubMed] [Google Scholar]
- 165.Prescott J.F. Rhodococcus equi: An animal and human pathogen. Clin. Microbiol. Rev. 1991;4:20–34. doi: 10.1128/CMR.4.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Dorella F.A., Pacheco L.G., Oliveira S.C., Miyoshi A., Azevedo V. Corynebacterium pseudotuberculosis: Microbiology, biochemical properties, pathogenesis and molecular studies of virulence. Vet. Res. 2006;37:201–218. doi: 10.1051/vetres:2005056. [DOI] [PubMed] [Google Scholar]
- 167.Rzewuska M., Rodo A., Bielecki W. Dermacentor reticulatus ticks as possible vectors of Trueperella pyogenes infection in European bison (Bison bonasus): Preliminary studies. J. Comp. Pathol. 2016;154:120. doi: 10.1016/j.jcpa.2015.10.164. [DOI] [Google Scholar]
- 168.Jost B.H., Songer J.G., Billington S.J. An Arcanobacterium (Actinomyces) pyogenes mutant deficient in production of the pore-forming cytolysin pyolysin has reduced virulence. Infect. Immun. 1999;67:1723–1728. doi: 10.1128/iai.67.4.1723-1728.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Billington S.J., Songer J.G., Jost B.H. Molecular characterization of the pore-forming toxin, pyolysin, a major virulence determinant of Arcanobacterium pyogenes. Vet. Microbiol. 2001;82:261–274. doi: 10.1016/S0378-1135(01)00373-X. [DOI] [PubMed] [Google Scholar]
- 170.Rudnick S.T., Jost B.H., Songer J.G., Billington S.J. The gene encoding pyolysin, the pore-forming toxin of Arcanobacterium pyogenes, resides within a genomic islet flanked by essential genes. FEMS Microbiol. Lett. 2003;225:241–247. doi: 10.1016/S0378-1097(03)00527-5. [DOI] [PubMed] [Google Scholar]
- 171.Alouf J.E. Cholesterol-binding cytolytic protein toxins. Int. J. Med. Microbiol. 2000;290:351–356. doi: 10.1016/S1438-4221(00)80039-9. [DOI] [PubMed] [Google Scholar]
- 172.Heuck A.P., Moe P.C., Johnson B.B. The cholesterol-dependent cytolysin family of gram-positive bacterial toxins. Subcell. Biochem. 2010;51:551–577. doi: 10.1007/978-90-481-8622-8_20. [DOI] [PubMed] [Google Scholar]
- 173.Ding H., Lämmler C. Purification and further characterization of a haemolysin of Actinomyces pyogenes. Zentralbl. Veterinarmed. B. 1996;43:179–188. doi: 10.1111/j.1439-0450.1996.tb00303.x. [DOI] [PubMed] [Google Scholar]
- 174.Lovell R. Further studies on the toxin of Corynebacterium pyogenes. J. Pathol. Bacteriol. 1944;56:525–529. doi: 10.1002/path.1700560406. [DOI] [Google Scholar]
- 175.Kume T., Tainaka M., Saito H., Hiruma M., Nishio S., Kashiwazaki M., Mitani K., Nakajima Y. Research on experimental Corynebacterium pyogenes infections in pigs. Kitasato Arch. Exp. Med. 1983;56:119–135. [PubMed] [Google Scholar]
- 176.Hu Y., Zhang W., Bao J., Wu Y., Yan M., Xiao Y., Yang L., Zhang Y., Wang J. A chimeric protein composed of the binding domains of Clostridium perfringens phospholipase C and Trueperella pyogenes pyolysin induces partial immunoprotection in a mouse model. Res. Vet. Sci. 2016;107:106–115. doi: 10.1016/j.rvsc.2016.04.011. [DOI] [PubMed] [Google Scholar]
- 177.Imaizumi K., Serizawa A., Hashimoto N., Kaidoh T., Takeuchi S. Analysis of the functional domains of Arcanobacterium pyogenes pyolysin using monoclonal antibodies. Vet. Microbiol. 2001;81:235–242. doi: 10.1016/S0378-1135(01)00342-X. [DOI] [PubMed] [Google Scholar]
- 178.Jost B.H., Field A.C., Trinh H.T., Songer J.G., Billington S.J. Tylosin resistance in Arcanobacterium pyogenes is encoded by an erm X determinant. Antimicrob. Agents Chemother. 2003;47:3519–3524. doi: 10.1128/AAC.47.11.3519-3524.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Zhao K., Liu M., Zhang X., Wang H., Yue B. In vitro and in vivo expression of virulence genes in Trueperella pyogenes based on a mouse model. Vet. Microbiol. 2013;163:344–350. doi: 10.1016/j.vetmic.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 180.Billington S.J., Jost B.H., Cuevas W.A. The Arcanobacterium (Actinomyces) pyogenes hemolysin, pyolysin, is a novel member of the thiol-activated cytolysin family. J. Bacteriol. 1997;179:6100–6106. doi: 10.1128/jb.179.19.6100-6106.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Ikegami M., Hashimoto N., Kaidoh T., Sekizaki T., Takeuchi S. Genetic and biochemical properties of a hemolysin (pyolysin) produced by a swine isolate of Arcanobacterium (Actinomyces) pyogenes. Microbiol. Immunol. 2000;44:1–7. doi: 10.1111/j.1348-0421.2000.tb01239.x. [DOI] [PubMed] [Google Scholar]
- 182.Funk P.G., Staats J.J., Howe M., Nagaraja T.G., Chengappa M.M. Identification and partial characterization of an Actinomyces pyogenes hemolysin. Vet. Microbiol. 1996;50:129–142. doi: 10.1016/0378-1135(96)00008-9. [DOI] [PubMed] [Google Scholar]
- 183.Billington S.J., Esmay P.A., Songer J.G., Jost B.H. Identification and role in virulence of putative iron acquisition genes from Corynebacterium pseudotuberculosis. FEMS Microbiol. Lett. 2002;208:41–45. doi: 10.1111/j.1574-6968.2002.tb11058.x. [DOI] [PubMed] [Google Scholar]
- 184.Imaizumi K., Matsunaga K., Higuchi H., Kaidoh T., Takeuchi S. Effect of amino acid substitutions in the epitope regions of pyolysin from Arcanobacterium pyogenes. Vet. Microbiol. 2003;91:205–213. doi: 10.1016/S0378-1135(02)00299-7. [DOI] [PubMed] [Google Scholar]
- 185.Pokrajac L., Harris J.R., Sarraf N., Palmer M. Oligomerization and hemolytic properties of the C-terminal domain of pyolysin, a cholesterol-dependent cytolysin. Biochem. Cell Biol. 2013;91:59–66. doi: 10.1139/bcb-2012-0065. [DOI] [PubMed] [Google Scholar]
- 186.Zhang W., Wang H., Wang B., Zhang Y., Hu Y., Ma B., Wang J. Replacing the 238th aspartic acid with an arginine impaired the oligomerization activity and inflammation-inducing property of pyolysin. Virulence. 2018;9:1112–1125. doi: 10.1080/21505594.2018.1491256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Yan M., Hu Y., Bao J., Xiao Y., Zhang Y., Yang L., Wang J., Zhang W. Isoleucine 61 is important for the hemolytic activity of pyolysin of Trueperella pyogenes. Vet. Microbiol. 2016;182:196–201. doi: 10.1016/j.vetmic.2015.11.031. [DOI] [PubMed] [Google Scholar]
- 188.Yang L., Zhang Y., Wang H., Ma B., Xu L., Wang J., Zhang W. Identification of B-cell linear epitopes in domains 1-3 of pyolysin of Trueperella pyogenes using polyclonal antibodies. Vet. Microbiol. 2017;210:24–31. doi: 10.1016/j.vetmic.2017.08.018. [DOI] [PubMed] [Google Scholar]
- 189.Pokrajac L., Baik C., Harris J.R., Sarraf N.S., Palmer M. Partial oligomerization of pyolysin induced by a disulfide-tethered mutant. Biochem. Cell Biol. 2012;90:709–717. doi: 10.1139/o2012-029. [DOI] [PubMed] [Google Scholar]
- 190.Harris J.R., Lewis R.J., Baik C., Pokrajac L., Billington S.J., Palmer M. Cholesterol microcrystals and cochleate cylinders: Attachment of pyolysin oligomers and domain 4. J. Struct. Biol. 2011;173:38–45. doi: 10.1016/j.jsb.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 191.Preta G., Jankunec M., Heinrich F., Griffin S., Sheldon I.M., Valincius G. Tethered bilayer membranes as a complementary tool for functional and structural studies: The pyolysin case. Biochim. Biophys. Acta. 2016;1858:2070–2080. doi: 10.1016/j.bbamem.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 192.Liu M., Wang B., Liang H., Ma B., Wang J., Zhang W. Determination of the expression of three fimbrial subunit proteins in cultured Trueperella pyogenes. Acta Vet. Scand. 2018;60:53. doi: 10.1186/s13028-018-0407-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Bisinotto R.S., Filho J.C.O., Narbus C., Machado V.S., Murray E., Bicalho R.C. Identification of fimbrial subunits in the genome of Trueperella pyogenes and association between serum antibodies against fimbrial proteins and uterine conditions in dairy cows. J. Dairy Sci. 2016;99:3765–3776. doi: 10.3168/jds.2015-10401. [DOI] [PubMed] [Google Scholar]
- 194.Pietrocola G., Valtulina V., Rindi S., Jost B.H., Speziale P. Functional and structural properties of CbpA, a collagen-binding protein from Arcanobacterium pyogenes. Microbiology. 2007;153:3380–3389. doi: 10.1099/mic.0.2007/009100-0. [DOI] [PubMed] [Google Scholar]
- 195.Lämmler C., Ding H. Characterization of Fibrinogen-binding Properties of Actinomyces pyogenes. J. Vet. Med. B. 1994;41:588–596. doi: 10.1111/j.1439-0450.1994.tb00268.x. [DOI] [PubMed] [Google Scholar]
- 196.Esmay P.A., Billington S.J., Link M.A., Songer J.G., Jost B.H. The Arcanobacterium pyogenes collagen-binding protein, CbpA, promotes adhesion to host cells. Infect. Immun. 2003;71:4368–4374. doi: 10.1128/IAI.71.8.4368-4374.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Taylor G. Sialidases: Structures, biological significance and therapeutic potential. Curr. Opin. Struct. Biol. 1996;6:830–837. doi: 10.1016/S0959-440X(96)80014-5. [DOI] [PubMed] [Google Scholar]
- 198.Pettigrew M.M., Fennie K.P., York M.P., Daniels J., Ghaffar F. Variation in the Presence of Neuraminidase Genes among Streptococcus pneumoniae Isolates with Identical Sequence Types. Infect. Immun. 2006;74:3360–3365. doi: 10.1128/IAI.01442-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Moriyama T., Barksdale L. Neuraminidase of Corynebacterium diphtheriae. J. Bacteriol. 1967;9:1565–1581. doi: 10.1128/jb.94.5.1565-1581.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Soong G., Muir A., Gomez M.I., Waks J., Reddy B., Planet P., Singh P.K., Kanetko Y., Wolfgang M.C., Hsiao Y.S., et al. Bacterial neuraminidase facilitates mucosal infection by participating in biofilm production. J. Clin. Investig. 2006;116:2297–2305. doi: 10.1172/JCI27920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Moncla B.J., Braham P., Hillier S.L. Sialidase (neuraminidase) activity among gram-negative anaerobic and capnophilic bacteria. J. Clin. Microbiol. 1990;28:422–425. doi: 10.1128/jcm.28.3.422-425.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Crennell S.J., Garman E.F., Philippon C., Vasella A., Laver W.G., Vim E.R., Taylor G.L. The structures ofSalmonella typhimurium LT2 neuraminidase and its complexes with three inhibitors at high resolution. J. Mol. Biol. 1996;259:264–280. doi: 10.1006/jmbi.1996.0318. [DOI] [PubMed] [Google Scholar]
- 203.Ada G.L., French E.L., Lind P.E. Purification and properties of neuraminidase from Vibrio cholera. J. Gen. Microbiol. 1961;24:409–425. doi: 10.1099/00221287-24-3-409. [DOI] [PubMed] [Google Scholar]
- 204.Godoy V.G., Dallas M.M., Russo T.A., Malamy M.H. A role for Bacteroides fragilis neuraminidase in bacterial growth in two model systems. Infect. Immun. 1993;61:4415–4426. doi: 10.1128/iai.61.10.4415-4426.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Schaufuss P., Lämmler C. Characterization of Extracellular Neuraminidase produced by Actinomyces pyogenes. Zentralblatt. Bakteriol. 1989;271:28–35. doi: 10.1016/S0934-8840(89)80050-7. [DOI] [PubMed] [Google Scholar]
- 206.Jost B.H., Songer J.G., Billington S.J. Cloning, expression, and characterization of a neuraminidase gene from Arcanobacterium pyogenes. Infect. Immun. 2001;69:4430–4437. doi: 10.1128/IAI.69.7.4430-4437.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Jost B.H., Songer J.G., Billington S.J. Identification of a second Arcanobacterium pyogenes neuraminidase and involvement of neuraminidase activity in host cell adhesion. Infect. Immun. 2002;70:1106–1112. doi: 10.1128/IAI.70.3.1106-1112.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Ozturk D., Turutoglu H., Pehlivanoglu F., Guler L. Virulence Genes, Biofilm Production and Antibiotic Susceptibility in Trueperella pyogenes isolated from Cattle. Isr. J. Vet. Med. 2016;71:36–42. [Google Scholar]
- 209.Zhang S., Qiu J., Yang R., Shen K., Xu G., Fu L. Complete genome sequence of Trueperella pyogenes, isolated from infected farmland goats. Genome Announc. 2016;4:e01421-16. doi: 10.1128/genomeA.01421-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Kasimanickam V.R., Owen K., Kasimanickam R.K. Detection of genes encoding multidrug resistance and biofilm virulence factor in uterine pathogenic bacteria in postpartum dairy cows. Theriogenology. 2016;85:173–179. doi: 10.1016/j.theriogenology.2015.10.014. [DOI] [PubMed] [Google Scholar]
- 211.da Silva Duarte V., Dias R.S., Kropinski A.M., da Silva Xavier A., Ferro C.G., Vidigal P.M.P., da Silva C.C., de Paula S.O. A T4virus prevents biofilm formation by Trueperella pyogenes. Vet. Microbiol. 2018;218:45–51. doi: 10.1016/j.vetmic.2018.03.025. [DOI] [PubMed] [Google Scholar]
- 212.Zschiedrich C.P., Keidel V., Szurmant H. Molecular Mechanisms of Two-Component Signal Transduction. J. Mol. Biol. 2016;428:3752–3775. doi: 10.1016/j.jmb.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Herrou J., Crosson S., Fiebig A. Structure and function of HWE/HisKA2-family sensor histidine kinases. Curr. Opin. Microbiol. 2017;36:47–54. doi: 10.1016/j.mib.2017.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Hupało-Sikorska A., Gregorczyk K.P., Rzewuska M., Szulc-Dąbrowska L., Struzik J., Gieryńska M. Proceedings of XVIII Conference DIAGMOL 2017—Molecular Biology in Diagnostics of Infectious Diseases and Biotechnology. Warsaw University of Life Sciences; Warsaw, Poland: 2017. Involvement of macrophages during Trueperella pyogenes infection; pp. 45–46. [Google Scholar]
- 215.Machado V.S., Bicalho R.C. Complete genome sequence of Trueperella pyogenes, an important opportunistic pathogen of livestock. Genome Announc. 2014;2:e00400-14. doi: 10.1128/genomeA.00400-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.da Silva Duarte V., Dias R.S., Kropinski A.M., Vidigal P.M.P., Sousa F.O., da Silva Xavier A., da Silva C.C., de Paula S.O. Complete genome sequence of vB_EcoM_UFV13, a new bacteriophage able to disrupt Trueperella pyogenes biofilm. Genome Announc. 2016;4:e01292-16. doi: 10.1128/genomeA.01292-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Bernier A.M., Bernard K. Draft genome sequence of Trueperella bernardiae LCDC 89-0504T, isolated from a human blood culture. Genome Announc. 2016;4:e01634-15. doi: 10.1128/genomeA.01634-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Billington S.J., Jost B.H., Songer J.G. The Arcanobacterium (Actinomyces) pyogenes plasmid pAP1 is a member of the pIJ101/pJV1 family of rolling circle replication plasmids. J. Bacteriol. 1998;180:3233–3236. doi: 10.1128/jb.180.12.3233-3236.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Tauch A., Götker S., Pühler A., Kalinowski J., Thierbach G. The 27.8-kb R-plasmid pTET3 from Corynebacterium glutamicum encodes the aminoglycoside adenyltransferase gene cassette aadA9 and the regulated tetracycline efflux system Tet 33 flanked by active copies of the widespread insertion sequence IS6100. Plasmid. 2002;48:117–129. doi: 10.1016/S0147-619X(02)00120-8. [DOI] [PubMed] [Google Scholar]
- 220.Lovell R., Foggie A., Pearson J.K. Field trials with Corynebacterium pyogenes alum-precipitated toxoid. J. Comp. Pathol. 1950;60:225–229. doi: 10.1016/S0368-1742(50)80021-8. [DOI] [PubMed] [Google Scholar]
- 221.Hunter P., van der Lugt J.J., Gouws J.J., Onderstepoort J. Failure of an Actinomyces pyogenes vaccine to protect sheep against an intravenous challenge. Vet. Res. 1990;57:239–241. [PubMed] [Google Scholar]
- 222.Kostro K., Lisiecka U., Żmuda A., Niemczuk K., Stojecki K., Taszkun I. Selected parameters of immune response in pregnant sows vaccinated against Trueperella pyogenes. Bull. Vet. Inst. Pulawy. 2014;58:17–21. doi: 10.2478/bvip-2014-0003. [DOI] [Google Scholar]
- 223.Machado V.S., Bicalho M.L., Meira Junior E.B., Rossi R., Ribeiro B.L., Lima S., Santos T., Kussler A., Foditsch C., Ganda E.K., et al. Subcutaneous immunization with inactivated bacterial components and purified protein of Escherichia coli, Fusobacterium necrophorum and Trueperella pyogenes prevents puerperal metritis in Holstein dairy cows. PLoS ONE. 2014;9:e91734. doi: 10.1371/journal.pone.0091734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Zhang W., Wang P., Wang B., Ma B., Wang J. A combined Clostridium perfringens/Trueperella pyogenes inactivated vaccine induces complete immunoprotection in a mouse model. Biologicals. 2017;47:1–10. doi: 10.1016/j.biologicals.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 225.Huang T., Zhao K., Zhang Z., Tang C., Zhang X., Yue B. DNA vaccination based on pyolysin co-immunized with IL-1β enhances host antibacterial immunity against Trueperella pyogenes infection. Vaccine. 2016;34:3469–3477. doi: 10.1016/j.vaccine.2016.04.025. [DOI] [PubMed] [Google Scholar]
- 226.Huang T., Song X., Jing J., Zhao K., Shen Y., Zhang X., Yue B. Chitosan-DNA nanoparticles enhanced the immunogenicity of multivalent DNA vaccination on mice against Trueperella pyogenes infection. J. Nanobiotechnol. 2018;16:8. doi: 10.1186/s12951-018-0337-2. [DOI] [PMC free article] [PubMed] [Google Scholar]