Abstract
Background
Cardiac rehabilitation (CR) reduces mortality and improves quality of life. Unfortunately, participation in CR remains low and studies have examined the use of home-based tele-monitoring to improve participation in CR. These studies generally utilized single- or three-lead electrocardiogram (ECG) channels with limited sensitivity to detect ischaemic changes. In this report, we describe detection of unexpected, significant left main coronary disease in a patient participating in a home CR programme using a unique 12-lead ECG monitoring system.
Case summary
A 68-year-old man was referred for CR after acute coronary syndrome and stent implantation to the obtuse marginal. Three months following this intervention, he began complaining of chest pain. Repeat coronary angiogram showed a borderline lesion in the left main not felt to be clinically significant. The patient performed CR and was monitored with the Master Caution® System, a digital platform including a garment with 10 textile electrodes (Master Caution garment) configuring a device which enables 12 lead ECG. While being monitored, the ECG technician detected 1–2 mm ST-depression in leads 1, L V2–V5. The patient was asymptomatic at the time the ST-depressions were noted. Repeat angiography revealed a significant increase in the severity of the left main lesion and the patient was referred for bypass surgery.
Discussion
This life-threatening diagnosis could easily have been missed using conventional ECG monitoring and our case demonstrates the potential clinical utility of tele-monitoring with a 12-lead digital home ECG monitoring device.
Keywords: Home cardiac tele-rehabilitation, Electrocardiogram, Ischaemia, Case report
Learning points
In this report, we describe detection of unexpected, significant left main coronary disease.
It was detected during tele-monitored cardiac rehabilitation using the Master Caution Device (MCD) 12-lead electrocardiogram (ECG) device.
This life-threatening diagnosis could easily have been missed using conventional ECG monitoring.
Our case demonstrates the potential clinical utility of 12-lead digital home ECG monitoring using the MCD device.
Introduction
Exercise-based cardiac rehabilitation (CR) has been shown to reduce mortality and improve quality of life following acute coronary syndromes.1 Unfortunately, participation in CR remains low, partially because of practical barriers such as the need to perform CR in the hospital setting.2 Several studies have examined the use of home-based tele-monitoring to improve the results of CR.3 These studies have generally utilized single- or three-lead electrocardiogram (ECG) channels which have limited sensitivity to detect ischaemic changes. In this report, we describe detection of unexpected significant left main coronary disease in a patient participating in home CR using a unique 12-lead ECG monitoring system.
The patient was enrolled in a clinical trial examining the use of a home-based digital monitored CR compared with a standard CR programme in patients with ischaemic heart disease. The participants in the home CR arm are encouraged to perform monitored exercise at home, tailored to the patient’s individual capacity. Our programme includes the use of a commercially available, wearable tracking technology (FitBit charge 2®), along with a proprietary Master Caution garment (MCG, HealthWatch) both of which can connect users’ data to our online network (control centre).
The Master Caution® System is a digital platform that includes a garment with 10 textile electrodes (MCG) attached to the patient’s chest and positioned similarly to stress test electrodes and a Master Caution Device (MCD), approved by FDA, CE, and AMAR (Israeli Ministry of Health’s medical device regulation unit). The MCD is a personal, hand-held battery powered ECG device which is connected to the MCG configuring a 12-lead ECG device. The system enables 12 leads ECG, heart rate detection, skin temperature, respiratory, and body posture, allowing monitoring of ECG and vital signs, and is compatible with the gold standard ECG.
Timeline
| Date | Events |
|---|---|
| 29 August 2017 | Patient hospitalized with chest pain. Underwent percutaneous coronary intervention to obtuse marginal branch with resolution of symptoms. |
| January 2018 | Patient again develops chest pain. Repeat coronary angiogram showed a borderline lesion in the left main not felt to be clinically significant. Additional imaging was not performed. |
| 11 April 2018 | Patient referred to cardiac rehabilitation (CR). |
| 11 April 2018 | Recruitment to the study: patient is randomized to the home CR arm. |
| 16 April 2018 | Patient is fitted for Healthwatch garment, begins exercise training and monitoring. |
| 23 April 2018 | Received the Fitbit charge 2 watch and application as part of home tele-rehabilitation study (for use at home after 6 weeks in facility). |
| While being monitored with the garment transient ST-depressions are noted and patient referred to his treating cardiologist for further evaluation. | |
| 25 April 2018 | The patient complains to our research coordinator about chest pain and is referred to emergency room (ER), but refuses and goes to his cardiologist instead. |
| Afterward the same day | The treating cardiologist sends the patient for stress-echocardiography. |
| 13 May 2018 | Stress-echocardiography demonstrates hypokinesis with exercise of the anterior wall consistent with ischaemia in the left anterior descending artery territory. |
| 30 May 2018 | Patient underwent angiography which revealed a significant worsening of the lesion in the left main coronary artery to a 70–90% stenosis. Patient is referred for coronary artery bypass surgery. |
Case presentation
The patient was recruited and was randomized to the home CR arm. He is a 68-year-old man with past medical history of hyperlipidaemia and hypertension who developed exertional chest pain which continued to worsen. Physical examination was unremarkable. Exercise testing revealed chest pain and ST-depressions and the patient underwent cardiac catheterization with drug-eluting stent implantation to the obtuse marginal. No additional coronary imaging was performed. The patient was discharged on dual anti-platelet therapy with aspirin and clopidogrel as well as rosuvastatin and was referred for CR 1 month following this intervention. Three months following the intervention, he began complaining of chest pain. Repeat coronary angiogram showed a borderline lesion in the left main not felt to be clinically significant and additional imaging was not performed (Figure 1). Of note, the patient was non-compliant with lipid-lowering therapy. While he was exercising, and being monitored via the MCD, the ECG technician monitoring his ECG’s detected 1–2 mm ST-depression in leads 1, L V2–V5 (Figure 2). The patient was asymptomatic at the time the ST-depressions were noted.
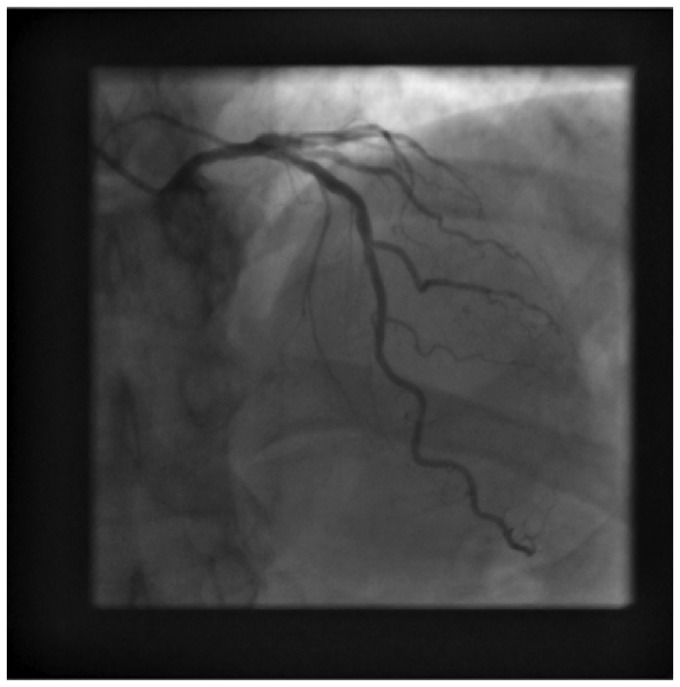
Figure 1.
Initial coronary angiogram showing minimal lesion in the left main.
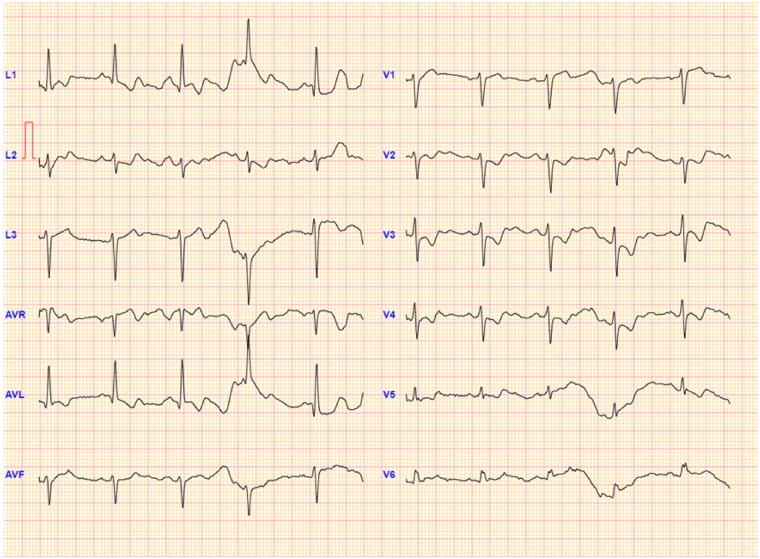
Figure 2.
ST-depression in leads 1, L V2–V5. The patient was asymptomatic at the time the ST-depressions were noted. Detected using Master Caution Device monitoring technique.
The patient was referred by his treating physician for stress-echocardiography that demonstrated severe ischaemia in the anterior wall. Repeat angiography revealed a significant worsening of the lesion in the left main coronary artery to a 70–90% stenosis (Figure 3), felt to be mainly due to rapid progression as a result of poor compliance with medical therapy. The lesion was felt to be atheromatous and not due to spasm or dissection based on the angiographic characteristics. The patient was referred for coronary artery bypass surgery due to the ostial nature of the lesion. He refused and percutaneous coronary intervention was successfully performed at another institution with resolution of the complaints of chest pain. Currently, the patient feels well without complaints of chest pains.
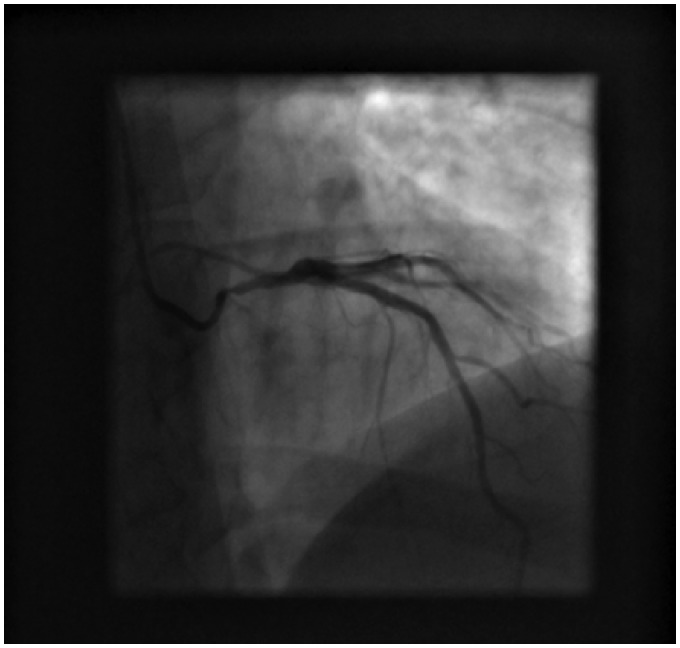
Figure 3.
Repeat angiography after ST-depression noted showing progression of the ostial left main lesion.
Discussion
In conclusion, significant ischaemia due to clinically unexpected, rapidly progressive left main disease was detected during tele-monitored CR using a 12-lead ECG device. This life-threatening diagnosis could easily have been missed using conventional ECG monitoring and our case demonstrates the potential clinical utility of 12-lead digital home ECG monitoring using the MCD device.
Lead author biography

Sara Katzburg is the director of research and development in O2 novelty center and associate researcher at Hadassah Medical School. She received her PhD degree from the Hebrew University Hadassah Medical School. Currently she concentrates on the development of remote advanced digital intervention programs for cardiovascular and metabolic patients. The programs include a mobile remote digital platform, which integrates different biosensors and provides the medical team with behavioral and physiological data.
Funding
HealthWatch LTD provided the Master-Caution device and technical support for the study.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. de Vries H, Kemps HM, van Engen-Verheul MM, Kraaijenhagen RA, Peek N.. Cardiac rehabilitation and survival in a large representative community cohort of Dutch patients. Eur Heart J 2015;36:1–10. [DOI] [PubMed] [Google Scholar]
- 2. De Vos C, Li X, Van Vlaenderen I, Saka O, Dendale P, Eyssen M, Paulus D.. Participating or not in a cardiac rehabilitation programme: factors influencing a patient's decision. Eur J Prev Cardiol 2013;20:341–348. [DOI] [PubMed] [Google Scholar]
- 3. Kraal JJ, Peek N, Van den Akker-Van Marle ME, Kemps HM.. Effects of home-based training with tele-monitoring guidance in low to moderate risk patients entering cardiac rehabilitation: short term results of the FIT@Home study. Eur J Prev Cardiolog 2014;21:26–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.