Abstract
Background
Optical coherence tomography (OCT)-derived fractional flow reserve (FFR)—which may be calculated using fluid dynamics—demonstrated an excellent correlation with the wire-based FFR. However, the applicability of the OCT-derived FFR in the assessment of tandem lesions is currently unclear.
Case summary
We present two cases of tandem lesions in the mid segment of the left anterior descending (LAD) artery which could have assessed accurately by OCT-derived FFR. The first patient underwent wire-based FFR at the far distal site of LAD, showed a value of 0.66. The OCT-derived FFR was calculated, yielding a value of 0.64. In the absence of stenosis at the proximal lesion, the OCT-derived FFR was calculated as 0.79, which was as same as the wire-based FFR obtained after stenting to the proximal lesion. Thus, additional stenting was performed at the distal lesion. The second patient underwent wire-based FFR at the far distal site of LAD, showed a value of 0.76 which was as same vale as OCT-derived FFR. Considering the absence of stenosis in the proximal lesion, the OCT-derived FFR was estimated as 0.88. After coronary stenting in the proximal lesion, the wire-based FFR yielded a value of 0.90. Therefore, additional intervention to the distal lesion was deferred.
Discussion
The described reports are the first two cases which performed physiological assessment using OCT in tandem lesions. The OCT-derived FFR might be able to estimate the wire-based FFR and the severity of each individual lesion in patients with tandem lesions.
Keywords: Case series, Optical coherence tomography, Fractional flow reserve, Percutaneous coronary intervention, Coronary artery disease
Learning points
Although physiological and anatomical assessments are important for coronary revascularization, the use of both modalities simultaneously in daily clinical practice is challenging.
Optical coherence tomography (OCT)-derived fractional flow reserve (FFR), which is calculated using fluid dynamics, was reported to be able to estimate wire-based FFR in the non-tandem coronary lesions.
The present cases indicated that the OCT-derived FFR can estimate the wire-based FFR and the severity of each individual lesion in patients with tandem lesions.
Introduction
Percutaneous coronary intervention (PCI) has become the predominant procedure for coronary revascularization among patients with coronary artery disease. Functional assessment of coronary stenosis by fractional flow reserve (FFR) improves clinical outcomes and reduces unnecessary revascularizations.1,2 On the other hand, although anatomical assessment is also important for PCI procedures, economic issues and lack of appropriate facilities occasionally do not allow the use of both modalities. Optical coherence tomography (OCT) provides high-resolution images of coronary structures with excellent reproducibility.3,4 Recently, the OCT-derived FFR—which is calculated using fluid dynamics—demonstrated a significant correlation with the wire-based FFR.5 The OCT-derived FFR can be calculated within 3–5 min after completion of OCT in the catheter laboratory. However, the applicability of the OCT-derived FFR in the assessment of tandem lesions is currently unclear. Herein, we present two cases with tandem lesions assessed by the OCT-derived FFR, showing excellent correlation with the wire-based FFR.
Timeline
| Time | Events | |
|---|---|---|
| Case 1 | Five years prior to admission | Medical history of dyslipidaemia and hypertension and diabetes mellitus. |
| Eight months prior to admission | Patient was suffering from chest pain during exercise. | |
| Two months prior to admission | Exercise-electrocardiography test demonstrated ischaemic ST-segment depression in leads V3–V6. | |
| One month prior to admission | Coronary angiography was performed. Tandem lesion in the mid segment of the left anterior descending (LAD) was found. | |
| One day after admission | Optical coherence tomography (OCT)-guided percutaneous coronary intervention (PCI) was performed. | |
| Case 2 | Eight years prior to admission | Medical history of hypertension. |
| Five months prior to admission | Patient was suffering from chest pain during exercise. | |
| One months prior to admission | Exercise-electrocardiography test demonstrated ischaemic ST-segment depression in leads V4–V6. | |
| Two weeks prior to admission | Coronary angiography was performed. Tandem lesion in the mid segment of the LAD was found. | |
| One day after admission | OCT-guided PCI was performed. |
Case presentation
Case 1
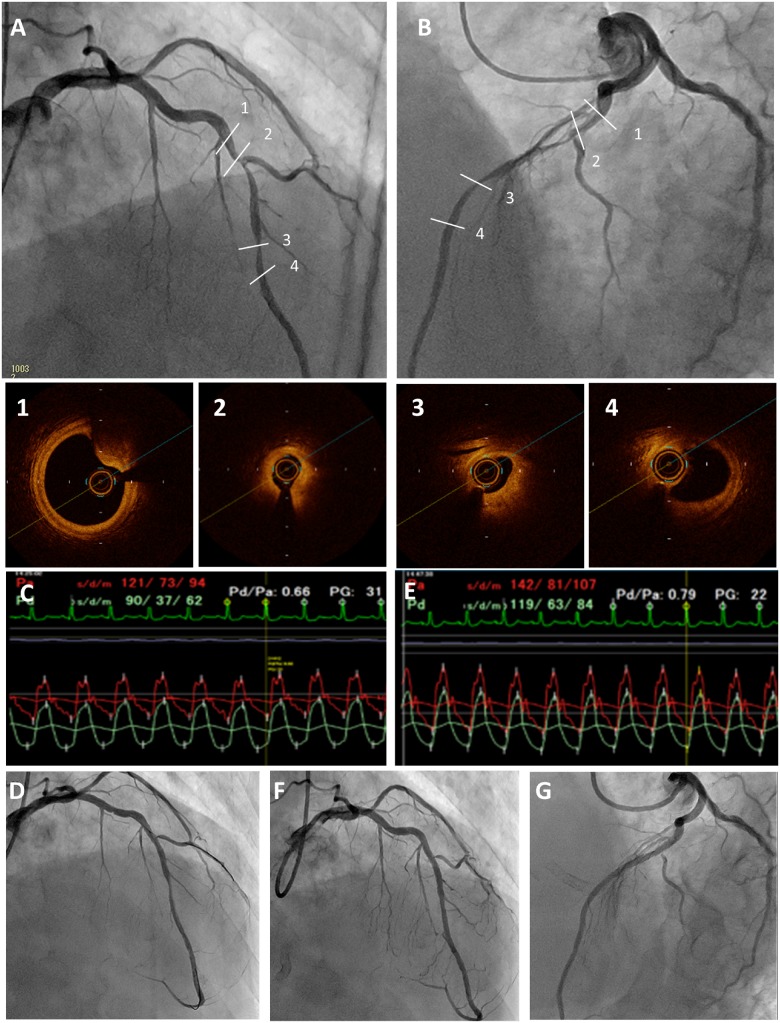
A 63-year-old male patient with a history of hypertension, dyslipidaemia, and diabetes mellitus was admitted to the hospital due to angina with Canadian Cardiovascular Society (CCS) Class III symptoms, despite treatment with maximal doses of a beta-blocker and nitrates. He had blood pressure of 110/64 mmHg, heart rate of 64 b.p.m., and oxygen saturation of 98% on room air. On physical examination, he had regular cardiac rhythm with normal S1 and S2, with no murmurs appreciated and clear lungs. Exercise electrocardiography demonstrated ischaemic ST-segment depression. Coronary angiography showed the presence of a tandem lesion in the mid segment of the left anterior descending (LAD) artery (Figure 1A). The proximal stenosis was severe, whereas the distal stenosis was intermediate. The wire-based FFR was performed with an intracoronary injection of 2 mg nicorandil, yielding a value of 0.66 (Figure 1B). Optical coherence tomography was performed (Figures 1A-1-4) and showed a minimal lumen area (MLA) of 0.83 mm2 at the proximal lesion and 1.02 mm2 at the distal lesion in the mid LAD artery (Figure 1A-2 and A-3). Subsequently, the OCT-derived FFR was calculated as previously reported,5 yielding a value of 0.64. In the absence of stenosis at the proximal lesion in the mid LAD artery (i.e. successful stenting at the proximal tandem lesion) (Figure 1A-2), the OCT-derived FFR yielded a value of 0.79, indicating that additional intervention at the distal lesion may be required. A 3.0 × 18 mm drug-eluting stent was implanted in the proximal lesion, followed by post-dilation. The wire-based FFR was repeated after stenting at the proximal lesion, yielding a value of 0.79, which was the same to that obtained from the OCT-derived FFR (Figure 1C and D). Thus, additional stenting was performed at the distal lesion (Figure 1E). The patient was discharged the following day without any complications or exertional chest pain. He is asymptomatic at 7-month follow-up.
Figure 1.
Coronary angiography of 30 right anterior oblique 30 cranial view (A) and 45 left anterior oblique 20 cranial view (B) showing the presence of a tandem lesion in the mid segment of the left anterior descending artery. Optical coherence tomography images showed the proximal lesion in the left anterior descending artery with mild calcified plaque and a reference lumen area of 5.92 mm2 (1), a minimal lumen area of 0.83 mm2 at the proximal stenosis (2), and a minimal lumen area of 1.02 mm2 at the distal stenosis of the mid left anterior descending artery (3). The distal reference lumen area was 2.81 mm2 (4). Pressure loss (ΔP) was calculated from the following equation: ΔP = FV + SV2. The F and S were calculated from the optical coherence tomography data. F is the coefficient of pressure due to viscous friction (Poiseuille resistance), whereas S is the coefficient of local pressure loss due to abrupt enhancement (flow separation). V represents coronary flow velocity. The F coefficient was calculated as the sum of all optical coherence tomography slices, which were 100 μm in longitudinal length. In this case, the F was calculated as 0.221 mmHg s/cm. The S coefficient was calculated using the proximal reference area and minimum lumen area. In this case, the S was calculated as 0.013 mmHg s2/cm2. The stenotic flow reserve in the diastolic phase was calculated using the following formulas: P = 100 − (FV + SV2), P = 10 + V × (100 − 10)/4.2. The intersection point of both formulas was defined as the SFR in the diastolic phase. The SFR in the systolic phase was calculated using the following formulas: P = 100 − (FV + SV2), P = 10 + V × (100 − 10)/2. The intersection point of both formulas was defined as the SFR in the systolic phase. In this case, the SFR (diastolic/systolic) was calculated as 2.36/1.56. The pressure loss in the lesion was calculated using the following formula: FV + SV2. The pressure loss in the diastolic phase was calculated as follows: 0.224 × (20 × 2.36) + 0.013 × (20 × 2.36)2 = 39.5 mmHg. The pressure loss in the systolic phase was calculated as follows: 0.224 × (10 × 1.56) + 0.013 × (10 × 1.56)2 = 6.66 mmHg. [(60 − 39.5)×2/3 + (120 − 6.66) × 1/3]/80 = 0.64. Therefore, the optical coherence tomography-derived fractional flow reserve yielded a value of 0.64. The wire-based fractional flow reserve was 0.66 (C). In the absence of stenosis at the proximal lesion in the mid left anterior descending artery, the optical coherence tomography-derived fractional flow reserve yielded a value of 0.79. Angiography after stent implantation at the proximal lesion (D). The wire-based fractional flow reserve after stenting at the proximal lesion was 0.79 (E). Angiography of 30 right anterior oblique 30 cranial view (F) and 45 left anterior oblique 20 cranial view (G) after additional stenting at the distal segment.
Case 2
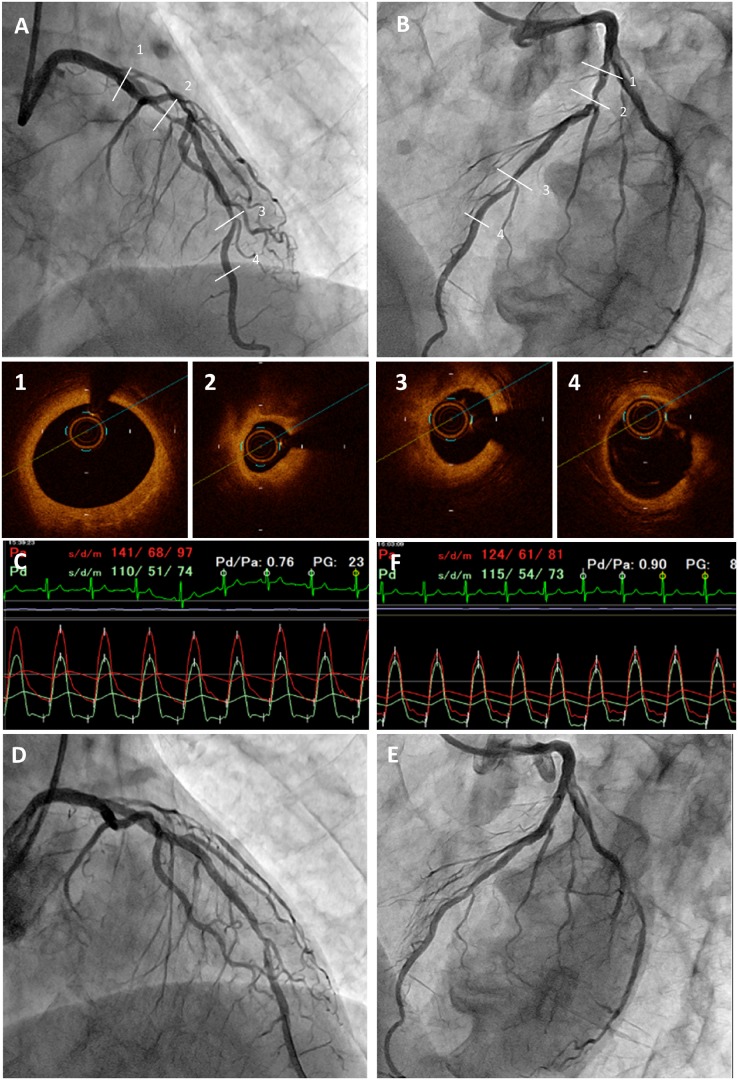
A 71-year-old male patient with CCS Class III angina was admitted to the hospital despite treatment with maximal doses of a beta-blocker and nitrates. He had blood pressure of 100/64 mmHg, heart rate of 72 b.p.m., and oxygen saturation of 98% on room air. On physical examination, he had regular cardiac rhythm with normal S1 and S2, with no murmurs appreciated and clear lungs. Exercise electrocardiography showed ischaemic ST-segment depression and presence of a tandem lesion in the mid segment of the LAD artery (Figure 2A). At the far distal site, the wire-based FFR was 0.76 (Figure 2B). Optical coherence tomography was performed (Figures 2A-1-4) and the OCT-derived FFR yielded a value of 0.76. Considering the absence of stenosis in the proximal lesion (Figure 2A-2), the OCT-derived FFR was estimated as 0.88. After coronary stenting in the proximal lesion, the wire-based FFR yielded a value of 0.90 (Figure 2C and D). Therefore, additional intervention to the distal lesion was deferred. The patient is asymptomatic at 7-month follow-up.
Figure 2.
Coronary angiography of 30 right anterior oblique 30 cranial view (A) and 45 left anterior oblique 20 cranial view (B) showing the presence of a tandem lesion in the mid segment of the left anterior descending artery. Optical coherence tomography images revealed the presence of a proximal lesion in the left anterior descending artery without significant plaque (1), a minimal lumen area of 1.07 mm2 at the proximal stenosis (2), and a minimal lumen area of 1.82 mm2 at the distal stenosis of the mid left anterior descending artery (3). The distal segment had a minimal lumen area of 3.04 mm2 (4). The wire-based fractional flow reserve was 0.76 (C). Angiography of 30 right anterior oblique 30 cranial view (D) and 45 left anterior oblique 20 cranial view (E) after stent implantation in the proximal lesion. The wire-based fractional flow reserve was 0.90 (F).
Discussion
The FFR method is currently the gold standard for the physiological assessment of intermediate coronary lesions, identifying ischaemia-inducible stenosis which requires revascularization.6 Optical coherence tomography, which has a 10-fold higher spatial resolution than intravascular ultrasound, enables the anatomical and morphologic assessments of coronary arteries, providing more accurate lumen measurements with excellent reproducibility.3,4 Nevertheless, the use of both modalities in daily clinical practice is challenging. In addition, simple FFR measurements are unable to predict the actual functional severity of each individual stenosis in tandem lesions due to the mutual flow volume interaction between the stenoses.7 The resting index (i.e. resting distal coronary pressure to aortic pressure and instantaneous wave-free ratio) is useful for the evaluation of tandem lesions,8 although it is also influenced by the severity of each stenosis.9 Therefore, in clinical practice, the functional severity of each lesion may be accurately assessed by the wire-based FFR only after optimal stenting for the most severe of the two lesions.
Several studies have shown a correlation between the MLA detected through intravascular imaging devices and the FFR.10,11 The OCT-derived FFR—considering the MLA, percentage of the area of stenosis, length of the stenosis, and fluid dynamics—has been reported to strongly correlate with the wire-based FFR vs. conventional measurements.5 The results of this novel method can be obtained within a few minutes after completion of OCT. Theoretically, it is possible to calculate the OCT-derived FFR accurately for tandem lesions without mutual flow volume interaction between the stenoses. Moreover, as demonstrated in the present cases, this approach enables us to evaluate the severity of each lesion and pressure loss, unaffected by another stenosis. In daily clinical practice, repeated FFR measurements for tandem lesions are usually time-consuming and costly. The present cases indicated that the OCT-derived FFR is able to estimate the wire-based FFR and the severity of each individual lesion in patients with tandem lesions.
Conclusions
The OCT-derived FFR was very useful in assessing the functional severity of coronary tandem lesions, without being influenced by each stenosis. Thus, the OCT-derived FFR may be useful for the assessment of the functional severity of tandem lesions.
Lead author biography

Yoshiyuki Okuya is a medical doctor at the Department of Cardiology, Tokushima Red Cross Hospital in Japan. He obtained Ph.D from Chiba University in 2018. His main interest is complex PCI.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: F.S. received lecture fees from Abbott Vascular Japan. The other authors have no conflict of interest to declare.
Supplementary Material
References
- 1. Pijls NHJ, Fearon WF, Tonino PAL, Siebert U, Ikeno F, Bornschein B, van't Veer M, Klauss V, Manoharan G, Engstrøm T, Oldroyd KG, Ver Lee PN, MacCarthy PA, De Bruyne B.. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J Am Coll Cardiol 2010;56:177–184. [DOI] [PubMed] [Google Scholar]
- 2. Fearon WF, Bornschein B, Tonino PAL, Gothe RM, Bruyne BD, Pijls NHJ, Siebert U.. Economic evaluation of fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease. Circulation 2010;122:2545–2550. [DOI] [PubMed] [Google Scholar]
- 3. Wijns W, Shite J, Jones MR, Lee SW-L, Price MJ, Fabbiocchi F, Barbato E, Akasaka T, Bezerra H, Holmes D.. Optical coherence tomography imaging during percutaneous coronary intervention impacts physician decision-making: ILUMIEN I study. Eur Heart J 2015;36:3346–3355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Minami Y, Hou J, Xing L, Jia H, Hu S, Vergallo R, Soeda T, Lee H, Zhang S, Yu B, Jang I-K.. Serial optical coherence tomography and intravascular ultrasound analysis of gender difference in changes of plaque phenotype in response to lipid-lowering therapy. Am J Cardiol 2016;117:1890–1895. [DOI] [PubMed] [Google Scholar]
- 5. Seike F, Uetani T, Nishimura K, Kawakami H, Higashi H, Aono J, Nagai T, Inoue K, Suzuki J, Kawakami H, Okura T, Yasuda K, Higaki J, Ikeda S.. Intracoronary optical coherence tomography-derived virtual fractional flow reserve for the assessment of coronary artery disease. Am J Cardiol 2017;120:1772–1779. [DOI] [PubMed] [Google Scholar]
- 6. Pijls NH, Van Gelder B, Van der Voort P, Peels K, Bracke FA, Bonnier HJ, el Gamal MI.. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation 1995;92:3183–3193. [DOI] [PubMed] [Google Scholar]
- 7. Pijls NH. Fractional flow reserve to guide coronary revascularization. Circ J 2013;77:561–569. [DOI] [PubMed] [Google Scholar]
- 8. Kikuta Y, Cook CM, Sharp ASP, Salinas P, Kawase Y, Shiono Y, Giavarini A, Nakayama M, De Rosa S, Sen S, Nijjer SS, Al-Lamee R, Petraco R, Malik IS, Mikhail GW, Kaprielian RR, Wijntjens GWM, Mori S, Hagikura A, Mates M, Mizuno A, Hellig F, Lee K, Janssens L, Horie K, Mohdnazri S, Herrera R, Krackhardt F, Yamawaki M, Davies J, Takebayashi H, Keeble T, Haruta S, Ribichini F, Indolfi C, Mayet J, Francis DP, Piek JJ, Di Mario C, Escaned J, Matsuo H, Davies JE.. Pre-angioplasty instantaneous wave-free ratio pullback predicts hemodynamic outcome in humans with coronary artery disease: primary results of the international multicenter iFR GRADIENT Registry. JACC Cardiovasc Interv 2018;11:757–767. [DOI] [PubMed] [Google Scholar]
- 9. Nijjer SS, Petraco R, van de Hoef TP, Sen S, van Lavieren MA, Foale RA, Meuwissen M, Broyd C, Echavarria-Pinto M, Al-Lamee R, Foin N, Sethi A, Malik IS, Mikhail GW, Hughes AD, Mayet J, Francis DP, Di Mario C, Escaned J, Piek JJ, Davies JE.. Change in coronary blood flow after percutaneous coronary intervention in relation to baseline lesion physiology: results of the JUSTIFY-PCI study. Circ Cardiovasc Interv 2015;8:e001715.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kang S-J, Ahn J-M, Song H, Kim W-J, Lee J-Y, Park D-W, Yun S-C, Lee S-W, Kim Y-H, Lee CW, Park S-W, Park S-J.. Usefulness of minimal luminal coronary area determined by intravascular ultrasound to predict functional significance in stable and unstable angina pectoris. Am J Cardiol 2012;109:947–953. [DOI] [PubMed] [Google Scholar]
- 11. Gonzalo N, Escaned J, Alfonso F, Nolte C, Rodriguez V, Jimenez-Quevedo P, Bañuelos C, Fernández-Ortiz A, Garcia E, Hernandez-Antolin R, Macaya C.. Morphometric assessment of coronary stenosis relevance with optical coherence tomography: a comparison with fractional flow reserve and intravascular ultrasound. J Am Coll Cardiol 2012;59:1080–1089. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.