Abstract
Measurements of tibial plateau subchondral bone and articular cartilage slope have been associated with the risk of suffering anterior cruciate ligament (ACL) injury. Such single-plane measures of the tibial plateau may not sufficiently characterize its complex, three-dimensional geometry and how it relates to knee injury. Further, the tibial spines have not been studied in association with the risk of suffering a non-contact ACL injury. We questioned whether the geometries of the tibial spines are associated with non-contact ACL injury risk, and if this relationship is different for males and females. Bilateral MRI scans were acquired on 88 ACL- injured subjects and 88 control subjects matched for sex, age and sports team. Medial and lateral tibial spine geometries were characterized with measurements of length, width, height, volume and anteroposterior location. Analyses of females revealed no associations between tibial spine geometry and risk of ACL injury. Analyses of males revealed that an increased medial tibial spine volume was associated with a decreased risk of ACL injury (OR = 0.667 per 100 mm3 increase). Smaller medial spines could provide less resistance to internal rotation and medial translation of the tibia relative to the femur, subsequently increasing ACL strains and risk of ACL injury.
Keywords: ACL injury, risk factors, tibial plateau geometry, tibial anatomy
Anterior cruciate ligament (ACL) injuries are common, with as many as 175,000 surgical reconstructions reported in 1 year in the United States.1 Many of these injuries occur among young, active individuals, and a large proportion involve non-contact injury mechanisms.2,3 Surgical reconstruction is a successful treatment option to restore function. However, ACL-injury often leads to post-traumatic osteoarthritis (PTOA) in a large proportion of subjects, regardless of whether or not their ACL was reconstructed.4 Both intrinsic and extrinsic factors have been investigated in association with the risk of sustaining a non-contact ACL injury.5 Among intrinsic factors, anatomic knee morphology has received growing interest in the literature. Risk of sustaining an ACL-injury is influenced by many anatomical factors, and the combination of factors that are most predictive of risk may be different between males and females.5
Recent work has focused on the sagittal plane orientation, or slope, of the medial and lateral tibial plateaus, and how they are related to the risk of suffering an ACL injury. Studies have revealed that the medial and lateral compartment subchondral bone6,7 and the lateral compartment articular cartilage surface8 slopes are both associated with the risk of suffering an ACL injury, primarily in females.8–11 Increased posterior-directed tibial plateau slope is associated with an increase in anterior translation of the tibia relative to the femur12 and an increase in ACL strain values.13,14
Proposed mechanisms for ACL-injury have included anterior tibial translation as well as tibial rotation and valgus collapse of the knee.15 Single plane measurements of tibial plateau slope do not provide a comprehensive characterization of the complex, threedimensional, tibial plateau geometry.16 Tibial plateau slope has been shown to be associated with the magnitude of translation between the tibia and fe- mur.12 However, other aspects of tibial plateau geometry may contribute to the amount of tibial rotation about its long axis. Increased rotation of the tibia relative to the femur has been associated with an increased risk of non-contact ACL injury.15 In humans, the proximal tibia exhibits an intercondylar eminence consisting of separate medial and lateral tibial spines connected by a bony ridge. Tibial eminence morphology that consists of distinct medial and lateral spines has been posed to have significant functional and phylogenetic implications in primates,17 which may be transferable to functional knee biomechanics in humans (Supplemantal Text). Each spine experiences contact stress during tibiofemoral articulation18,19 and their size as well as location may influence their level of restraint to the tibiofemoral displacements associated with ACL injury mechanisms. To date, no study has investigated the association between tibial spine geometry and the risk of suffering a non-contact ACL injury.
Our objective was to investigate the association between tibial spine geometry and risk of suffering a non-contact ACL injury. Our hypothesis was that tibial spine geometry would be associated with the risk of suffering a non-contact ACL injury and that this relationship would be different between males and females.
METHODS
Our institutional review board approved this study and subjects provided written consent prior to participation. MRI data in this study were previously collected as part of a larger longitudinal cohort study with a nested, matched case- control design.20 The larger study investigated a wide range of risk factors for non-contact ACL injury with the goal of developing a comprehensive multivariate risk model. Information including: sports studied, recruitment protocol, definition of non-contact ACL injury, entry criteria, time interval between injury and MRI acquisition, and characteristics of the subjects that participated in the MRI portion of the study have been previously described.9 Injuries to local athletes involved in organized sports at the high school and collegiate levels were monitored prospectively over a 4-year time period. Only non-contact ACL injuries, which were defined as injuries occurring without direct contact to the knee, were included in the study. Subjects included 88 first-time, grade- III ACL-injured subjects (61 female, 27 male) and 88 uninjured-controls matched by age, sex, and participation on the same sports team. MRI data were acquired using a Phillips Achivia 3.0T MRI System (Phillips Medical Systems, Best, The Netherlands) with subjects positioned supine, and their knee placed in extension inside an 8-channnel SENSE knee coil. Sagittal-plane Tl-weighted Fast-Field Echo (FFE) scans were acquired with a slice thickness of 1.2 mm and an in-plane resolution of 0.3 mm by 0.3 mm. For ACL-injured subjects, MRIs were obtained after injury but prior to surgery.
DICOM MRI images were viewed using OsiriX Software (Pixmeo, Geneva, Switzerland, version 5.5.1) and segmented using a Cintiq 21UX digitizing tablet (Wacom Technology Corporation, Vancouver, WA). Methods used to segment those data have been described previously.9 Digitized data were transformed to a standardized coordinate system that was fixed in the proximal tibia and interpolated to yield para-sagittal slices orthogonal to the coordinate system.9
In each sagittal slice, the superior-most anterior and posterior prominences of the subchondral bone profile were identified and used to characterize the circumferential rim of the medial and lateral tibial plateaus. A least-squared plane was fit to the circumferential rim points in each compartment. Data superior to the plane, bound by the circumferential rim and the most superior point of the compartment, were defined as the tibial spine (Fig. 1). As previously described,21 compartment minimums were defined as the point of maximum depth of concavity, at the sagittal slice corresponding to the most distal aspects of the medial and lateral femoral condyles (Fig. 1).
Figure 1.
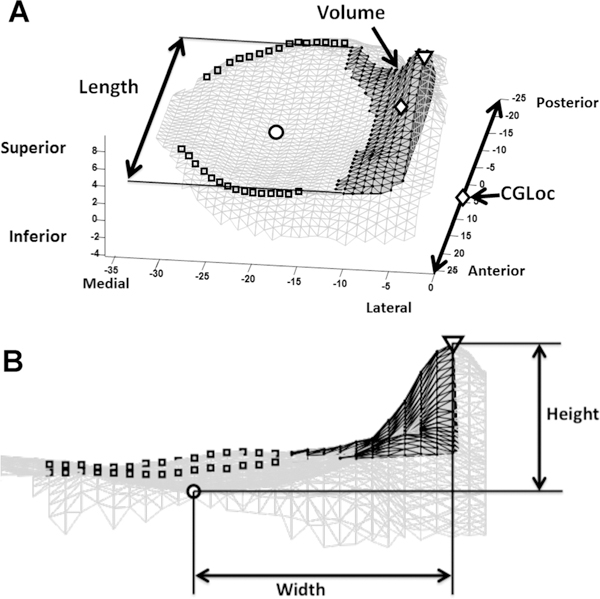
Tibial spine measurements of the medial compartment. Segmented data of medial compartment shown as a gray mesh. Anterior and posterior prominences (squares) of each para-sagittal slice determined to make up the circumferential rim. (A) Tibial spine volume (black mesh with dark gray surface) is defined by the data located between the circumferential rim (squares) and the peak of the tibial spine (triangle) and superior to the plane fit to the circumferential rim. Spine volume center of gravity (diamond) was calculated and its anteroposterior dimension was found. The length of the spine was defined as the difference between the maximum and minimum anteroposterior dimension of tibial spine. (B) Width of spine calculated as the difference between the mediolateral dimension of the peak of the spine (triangle) and the compartment minimum (circle). Height of spine calculated as the difference between the superiorinferior dimension of the spine peak (triangle) and compartment minimum (circle).
Measurements of tibial spine size and location were made for both medial and lateral spines. A triangular mesh surface was constructed using data points defined as the tibial spine. Each triangle was projected in the direction normal to the plane of the circumferential rim to form a prism. Volumes of each prism were summated in each compartment to determine the overall medial and lateral tibial spine volumes (MedVol and LatVol). The centroid was calculated for each volume. The anteroposterior dimension of each centroid was taken to yield the medial and lateral spine center of gravity location (MedCGLoc and LatCGLoc) (Fig. 1).
Measurements of anteroposterior directed length were made between the most anterior and posterior points of the medial and lateral spines (MedLength and LatLength). The vertical height of each spine was determined as the distance from the compartment minimum to the peak of the spine (MedHeight and LatHeight). Lastly, the mediolateral width from the compartment minimum to the peak of the spine was calculated (MedWidth and LatWidth) (Fig. 1).
Measurements of proximal tibia size were taken from the tibial coordinate system8 including the anterior-posterior length, the medial-lateral width and the cross-sectional area of the proximal tibia. These were considered as covariates to adjust for the size of an individual’s proximal tibia.
Statistical Analysis
The reliability of tibial spine measurements was investigated using variance component analysis on a random subset of 26 different subjects’ knees. These analyses estimated the variability between subjects, between examiners, and within examiners. Variance estimates were then used to compute Intraclass Correlation Coefficients (ICCs) for both inter and intra-observer reliability.
ACL injury has been shown to be associated with changes to the tibial plateau subchondral bone.9 Paired t-tests were used to compare tibial spine geometries between the injured and contralateral uninjured knees of ACL-injured subjects and no significant differences were found in the medial and lateral tibial spine measurements (Supplemental Table S1). The same analysis was conducted on control subjects, with the injured and uninjured sides defined to correspond to those of their matched ACL-injured subjects, and again revealed side-to-side symmetry (Supplemental Table S1). Comparable findings were produced when analyzing male and female subjects separately (Supplemental Tables S2 and S3). Though no significant differences were found between the injured and uninjured knees of ACL injured subjects, the uninjured knees were used to assess associations between tibial spine geometry and the risk of ACL- injury. This was done to avoid any potential bias due to changes caused by the injury.
Univariate conditional logistic regression was used to test the associations between tibial spine geometry and location with the risk of suffering an ACL injury. Multivariate conditional logistic regression was then used to determine if measures of tibial spine geometry were independently associated with the risk of suffering a non-contact ACL injury. Separate analyses were completed for males and females, and then repeated using males and females as a combined group. Additionally, analyses were repeated adjusting for both body weight and the size of the proximal tibia as covariates.
RESULTS
Reliability analyses indicated that most measures of tibial spine geometry had good reproducibility with intra-observer ICCs ranging from 0.684 to 0.960 (Table 1). Inter-observer ICCs were slightly lower, but all measurements presented in this study were made by the same investigator. The intra- and inter-observer ICCs for the medial spine volume were 0.860 and 0.858, respectively. Summary statistics for medial and lateral spine measurements of the uninjured knees of ACL-injured subjects and corresponding knees of controls are presented for females, males, and males and females combined (Table 2). While the mean medial spine volume for female cases was 10.2 mm3 greater than controls, the mean medial spine volume for male cases was 121.3 mm3 smaller than controls.
Table 1.
Intra- and Inter-Examiner Interclass Correlation Coefficients (ICCs) for Outcomes Made on a Random Subset of 26 Knees, by Two Examiners at Two Time-Points Each
| Variable | Intra-examiner ICC | Inter-examiner ICC |
|---|---|---|
| MedVol | 0.860 | 0.858 |
| MedHeight | 0.857 | 0.829 |
| MedWidth | 0.782 | 0.709 |
| MedLength | 0.716 | 0.600 |
| MedCGLoc | 0.951 | 0.872 |
| LatVol | 0.684 | 0.684 |
| LatHeight | 0.960 | 0.947 |
| LatWidth | 0.872 | 0.814 |
| LatLenght | 0.792 | 0.782 |
| LatCGLoc | 0.949 | 0.876 |
Table 2.
Summary Statistics for Medial and Lateral Tibial Spine Measurements With Males and Females Considered as Separate Groups and as a Combined Group
| Female subjects |
Male subjects |
Males and females combined |
||||
|---|---|---|---|---|---|---|
| Case |
Control |
Case |
Control |
Case |
Control |
|
| Variable | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) |
| MedVOL (mm3) | 275.9 (112.3) | 265.7 (111.6) | 340.8 (173.6) | 462.1 (202.1) | 295.8 (136.4) | 325.9 (170.6) |
| MedHeight (mm) | 9.8 (1.1) | 9.6 (1.2) | 10.7 (1.3) | 11.4 (1.3) | 10.1 (1.2) | 10.2 (1.5) |
| MedWidth (mm) | 17.1 (1.6) | 16.9 (1.8) | 19.3 (1.9) | 19.7 (1.8) | 17.8 (2.0) | 17.8 (2.2) |
| MedLength (mm) | 32.9 (5.4) | 32.9 (5.7) | 37.0 (4.4) | 38.4 (6.2) | 34.1 (5.5) | 34.6 (6.4) |
| MedCGLoc (mm) | 0.8 (2.0) | 1.3 (2.3) | 1.7 (1.8) | 2.2 (2.2) | 1.1 (2.0) | 1.6 (2.3) |
| LatVOL (mm3) | 528.8 (177.0) | 519.5 (151.5) | 719.0 (251.8) | 704.1 (262.7) | 587.1 (219.8) | 576.1 (209.2) |
| LatHeight (mm) | 7.6 (1.2) | 7.7 (1.2) | 8.1 (1.3) | 8.8 (1.6) | 7.8 (1.3) | 8.0 (1.4) |
| LatWidth (mm) | 16.2 (2.0) | 16.0 (2.0) | 18.8 (2.1) | 19.1 (2.3) | 17.0 (2.3) | 17.0 (2.5) |
| LatLength (mm) | 27.1 (5.5) | 26.8 (4.9) | 29.4 (5.1) | 30.6 (6.3) | 27.8 (5.5) | 27.9 (5.6) |
| LatCGLoc (mm) | −5.9 (1.6) | −5.5 (1.6) | −5.4 (1.9) | −6.0 (1.1) | −5.7 (1.7) | −5.6 (1.5) |
Included are the mean and standard deviation (SD) for each variable using the uninjured leg of ACL injury subjects and corresponding leg of control subjects.
Univariate analysis of females and the combined male and female group revealed no significant associations between tibial spine geometry and risk of ACL injury (Table 3). In contrast, analysis of the males as a separate group demonstrated that the medial spine volume (MedVol) had an inverse association with risk of ACL injury (OR = 0.67 for 100 mm3 unit increase or inversely OR = 1.50 for 100 mm3 decrease in medial spine volume, p = 0.04) (Table 3). Comparable results were found when the analysis included adjustment for body weight and the size of the proximal tibia.
Table 3.
Univariate Associations Between Tibial Spine Measurements and Risk of Suffering an ACL Injury
| Female subjects |
Male subjects |
Males and females combined |
||||
|---|---|---|---|---|---|---|
| Variable (unit change) | Odds ratio (95% CI) |
p-Value | Odds ratio (95% CI) |
p-Value | Odds ratio (95% CI) |
p-Value |
| MedVOL (100 mm3) | 1.09 (0.79–1.51) | 0.61 | 0.67 (0.45–0.98) | 0.04 | 0.86 (0.69–1.07) | 0.16 |
| MedHeight (1 mm) | 1.17 (0.83–1.66) | 0.38 | 0.63 (0.38–1.06) | 0.08 | 0.94 (0.72–1.22) | 0.64 |
| MedWidth (1mm) | 1.14 (0.87–1.48) | 0.35 | 0.9 (0.69–1.18) | 0.46 | 1.01 (0.84–1.22) | 0.89 |
| MedLength (1 mm) | 1.0 (0.94–1.06) | 0.96 | 0.96 (0.87–1.05) | 0.38 | 0.99 (0.94–1.04) | 0.60 |
| MedCGLoc (1 mm) | 0.89 (0.75–1.06) | 0.20 | 0.9 (0.68–1.18) | 0.43 | 0.89 (0.77–1.03) | 0.13 |
| LatVOL (100 mm3) | 1.04 (0.83–1.29) | 0.75 | 1.02 (0.83–1.27) | 0.83 | 1.03 (0.88–1.2) | 0.71 |
| LatHeight (1 mm) | 0.94 (0.69–1.27) | 0.67 | 0.73 (0.48–1.11) | 0.14 | 0.85 (0.67–1.08) | 0.18 |
| LatWidth (1 mm) | 1.06 (0.87–1.28) | 0.59 | 0.91 (0.67–1.23) | 0.54 | 1.01 (0.86–1.19) | 0.90 |
| LatLength (1 mm) | 1.01 (0.94–1.09) | 0.74 | 0.94 (0.82–1.07) | 0.33 | 0.99 (0.93–1.06) | 0.80 |
| LatCGLoc (1 mm) | 0.87 (0.69–1.09) | 0.23 | 1.32 (0.87–2.0) | 0.19 | 0.97 (0.8–1.17) | 0.72 |
Odds ratio and 95% confidence interval (CI) obtained from conditional logistic regression using the uninjured leg of ACL injured subjects and corresponding leg of control. Females and males analyzed as both separate and combined groups (Note MedVol and LatVol odds ratios correspond to the effect of a 100 mm3 increase and the odds ratios for the other variables correspond to a 1mm change).
Subsequent multivariate analyses included two models focusing on the medial tibial spine geometry. First, the MedLength, MedWidth, and MedHeight were combined in a model. No significant associations with risk were identified when females, males, or males and females combined were analyzed (Table 4). The second multivariate model investigated the combination of the MedVol and MedCGLoc (Table 4). No significant associations were identified when this model was applied to males and females combined or to females as a group. When males were analyzed as a group, MedCGLoc was not significantly related to risk. However, there was a significant inverse relationship between MedVol and the risk of suffering an ACL injury (OR = 0.66 for 100 mm3 increase or inversely OR = 1.52 for 100 mm3 decrease, p = 0.046), similar to the result of the univariate analysis.
Table 4.
Multivariate Associations Between Tibial Spine Measurements and Risk of Suffering an ACL Injury
| Female subjects |
Male subjects |
Males and females combined |
||||
|---|---|---|---|---|---|---|
| Variable (unit change) | Odds ratio (95% CI) |
p-Value | Odds ratio (95% CI) |
p-Value | Odds ratio (95% CI) |
p-Value |
| Model 1 | ||||||
| MedHeight (1 mm) | 1.15 (0.81–1.63) | 0.434 | 0.66 (0.37–1.16) | 0.148 | 0.94 (0.72–1.24) | 0.670 |
| MedWidth (1 mm) | 1.12 (0.86–1.47) | 0.41 | 0.97 (0.71–1.31) | 0.84 | 1.03 (0.85–1.24) | 0.80 |
| MedLength (1 mm) | 0.99 (0.94–1.06) | 0.87 | 0.99 (0.89–1.1) | 0.84 | 0.99 (0.94–1.04) | 0.65 |
| Model 2 | ||||||
| MedVOL (100 mm3) | 1.2 (0.84–1.72) | 0.31 | 0.66 (0.44–0.99) | 0.046 | 0.89 (0.71–1.13) | 0.34 |
| MedCGLoc (1 mm) | 0.86 (0.72–1.04) | 0.13 | 1.03 (0.75–1.41) | 0.86 | 0.92 (0.79–1.07) | 0.27 |
Odds ratio and 95% confidence interval (CI) obtained from conditional logistic regression using the uninjured leg of ACL injured subjects and corresponding leg of control subjects. Females and males analyzed as both separate and combined groups. Model 1 investigated the combined effects of the three dimensions of the size of the medial spine (MedHeight, MedWidth, and MedLength, respectively). Model 2 investigated the combined affects of the overall size and anteroposterior location of the medial spine (MedVol and MedCGLoc, respectively) (Note MedVol odds ratio corresponds to the effect of a 100 mm3 increase).
DISCUSSION
A smaller medial tibial spine volume was associated with an increased risk of suffering a non-contact ACL injury among males, but not females. For every 100 mm3 decrease in medial tibial spine volume, there was an associated 50% increase in risk of suffering an ACL injury. For perspective, this represents a change in volume of less than one standard deviation. The actual mean difference between male cases and controls in this study was 121.3 mm3. This suggests that small decreases in medial tibial spine volume could have a substantial impact on a male’s risk of suffering a non-contact ACL injury. No measures of tibial spine geometry were associated with the risk of suffering an ACL injury in females, or when a combined group of males and females were analyzed. Multivariate analysis focusing on medial spine geometry revealed the same inverse association between medial tibial spine volume and the risk of suffering an ACL injury in males. Meaning that this relationship was independent of subject’s body weight, proximal tibia size and anteroposterior location of tibial spine’s center of gravity.
The relationship between the volume of the medial spine and risk of suffering a non-contact ACL injury in males may be based on how the volume is distributed. Distribution of spine volume as it relates to the size of the inclined surface, or wedge shape, could influence the magnitude of rotation and translation between the tibia and femur. The primary biomechanical function of the ACL is to resist anterior directed shear forces applied to the tibia, relative to the femur. Additionally, by virtue of its posterior-anterior and lateral-medial orientation, it also provides restraint to internal rotation and medial displacement of the tibia relative to the femur. Each of these displacements, either considered in isolation or in combination, have been proposed as mechanisms involved in ACL strain and injury.15 Both in vivo and in vitro studies have demonstrated that the application of an internal tibial torque increases ACL strain values, while external torque produces a decrease in ACL strain values.22,23 Thus, it is reasonable that the size of the medial tibial spine, and not the lateral spine, is associated with risk of suffering an ACL injury. Internal torque applied to the tibia causes the medial femoral condyle to contact and translate up the medial tibial spine, increasing ACL strain values. Decreased medial tibial spine volume may be correlated with a decreased wedge shape, and a subsequent decreased restraint to translation of the tibia relative to the femur. This would require the ACL to provide larger contributions to the restraint of tibial displacement, increasing the loads placed on the ACL and resulting in an increased risk of injury. Further research should confirm this relationship.
Meta-analyses have established the relationship between posterior directed tibial plateau slope and the risk of suffering an ACL injury.6,7 In contrast, the geometry of the tibial spine has not been investigated in association with the risk of suffering a non-contact ACL injury. In addition, there is very little known about the role of tibial spines in controlling knee biomechanics. The slope in each compartment is often defined using the sagittal profile obtained from the mid-compartment. Li et al.18 described the center point of joint contact on the tibial plateau as being located on the spine (in contrast to a mid-compartment or peripheral location) of the medial compartment during flexion, and on the lateral compartment spine at each flexion angle measured except for 30°. Additionally, previous work has shown that in a load- bearing knee, the highest compressive contact pressures are located on the cartilage of the medial tibial spines.19 Measurements made at one mid-compartment para-sagittal slice, where the articular contact is not focused, might not fully characterize the geometry of the tibial plateau or its biomechanical function. Consequently, three-dimensional characterization of the geometry of the tibial spines may better describe the biomechanical function of the knee as it relates to increased ACL strains and risk of ACL injury.
Strengths of the current study result from its rigorous study design. Detailed information on subject injury history was collected to ensure that no confounding factors from previous injury or joint disease had the potential to alter tibial spine geometry. The approach used to match the ACL injured subjects with their uninjured-controls removed any bias due to differences in sex or age of the subjects. Furthermore, recruiting matched uninjured-controls from the same sports team served to control for the type, and amount of exposure to ACL injury risk. Consequently, calculated odds ratios using conditional logistic regression were comparable to the estimates of relative risk associated with tibial spine geometry that would be derived from a fully prospective study.24 Subjects were not matched on height or weight so that these variables could be investigated as risk factors in the overall study. Instead, body weight was included in the analyses as a covariate and was used as an alternative method of standardizing for the size of subjects. Additionally, measurements of proximal tibia size were included as covariates to standardize for the overall size of the tibial plateau. Adjustments for body weight and proximal tibia size had little influence on the results indicating that the association between medial spine volume and risk of ACL injury in males is independent of the subject’s weight, and size of their tibial plateau.
New measurements of tibial spine size and location were created in the development of this study. Compartment specific, three-dimensional characterization of tibial spine geometry through methods that were standardized and reproducible were the goals of this study. Analyses of reliability revealed good intra-observer ICCs for all measures aside from the LatVol. supporting the use of our methods protocol. Geometries of the medial and lateral tibial compartments were different. Lateral compartment geometry was less concave than the medial compartment; making consistently identifying the circumferential rim more difficult.
One limitation associated with the study design was that MRI data were not obtained prior to injury. In order to avoid potential bias created by the injury, the uninjured contralateral knee was used. However, measurements of tibial spine geometry made on the injured knees of ACL injured subjects were not statistically different in comparison to their uninjured contralateral knee. Additionally, analyses assessing risk using the injured knee of ACL-injured subjects and corresponding knee of controls produced equivalent results (Supplemental Table S4). Another limitation of the current study was the unequal number of male and female subjects recruited. Although, statistically significant associations were found between medial spine volume and risk of suffering an ACL injury in males, despite a smaller sample size and lower statistical power to detect associations.
Tibial spine geometry has a different association with the risk of sustaining an ACL injury for males in comparison to females. Different associations suggest that the biomechanics of an ACL injury may also differ between the sexes. Measurements of tibial spine volume were larger and more variable in males compared to females. This may help explain why the association between tibial spine geometry and risk of injury was observed only in males. Additionally, injury often occurs when the knee is near extension, where the centers of the tibiofemoral contact regions are thought to be located on the tibial spine in both the medial and lateral compartments.18 Medial compartment spine and knee ligaments are structures responsible for resisting internal tibial rotation and medial tibial translation. Males are thought to suffer ACL injury with their knees in greater extension than females,15 which provides an explanation as to why medial tibial spine volume is associated with the risk in males only. In thirty degrees of knee flexion, the center of the tibiofemoral contact region shifts to the mid-compartment of the lateral plateau, in contrast to the medial plateau where the center of tibiofemoral contact stays on the spine throughout all of knee flexion.18 Females may have a greater tendency to be injured with the knee further in flexion than males,15 which could contribute to previous reports indicating that lateral compartment tibial slope (measured at a mid-compartment location) has a greater association with risk of ACL injury in females.8–11
In the current study, additional analysis revealed that males had a larger medial tibial spine volume than females. This difference remained significant after controlling for body weight. An explanation for the lack of difference seen between female case and control subjects may be that the geometry of the tibial spine is an inherent risk factor among all females. Females exhibited less variability and smaller medial tibial spine volumes across ACL- injured and control subjects when compared to male subjects. ACL strain increases with anterior and medial translation as well as internal rotation of the tibia relative to the femur. Smaller tibial spines seen among all female subjects would provide less restraint to these translations than the tibial spines of their male counterparts. Thus, increasing strain placed on the ACL and increasing the risk of ACL injury. This may explain, at least in part, the 2–8-fold increase in the incidence of ACL injuries in females compared to males.25
Analyses of males revealed that a decreased medial tibial spine volume was associated with an increased risk of an ACL injury. The different risk factors for ACL injury between females and males support the hypothesis that the ACL injury mechanisms are different for females and males. Smaller medial spines could provide less resistance to internal rotation and medial translation of the tibia relative to the femur, subsequently increasing ACL strains and risk of ACL injury.
Supplementary Material
ACKNOWLEDGMENTS
Financial support includes research funding through NIH R01-AR050421 and MRI equipment funding through DOE SC 0001753.
Grant sponsor: NIH; Grant number: R01-AR050421; Grant sponsor: DOE; Grant number: SC 0001753.
Footnotes
Conflicts of interest: None.
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Work performed at the McClure Musculoskeletal Research Center of the University of Vermont, College of Medicine, Department of Orthopaedics and Rehabilitation.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article at the publisher’s web-site.
REFERENCES
- 1.Spindler KP, Wright RW. 2008. Clinical practice. Anterior cruciate ligament tear. N Engl J Med 359:2135–2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boden BP, Dean GS, Feagin JA Jr, et al. 2000. Mechanisms of anterior cruciate ligament injury. Orthopedics 23:573–578. [DOI] [PubMed] [Google Scholar]
- 3.McNair PJ, Marshall RN, Matheson JA. 1990. Important features associated with acute anterior cruciate ligament injury. N Z Med J 103:537–539. [PubMed] [Google Scholar]
- 4.Lohmander LS, Englund PM, Dahl LL, et al. 2007. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 35:1756–1769. [DOI] [PubMed] [Google Scholar]
- 5.Smith HC, Vacek P, Johnson RJ, et al. 2012. Risk factors for anterior cruciate ligament injury: a review of the literature —part 1: neuromuscular and anatomic risk. Sports Health 4:69–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wordeman SC, Quatman CE, Kaeding CC, et al. 2012. In vivo evidence for tibial plateau slope as a risk factor for anterior cruciate ligament injury: a systematic review and meta-analysis. Am J Sports Med 40:1673–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeng C, Cheng L, Wei J, et al. 2014. The influence of the tibial plateau slopes on injury of the anterior cruciate ligament: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 22:53–65. [DOI] [PubMed] [Google Scholar]
- 8.Beynnon BD, Vacek PM, Sturnick DR, et al. 2014. Geometric profile of the tibial plateau cartilage surface is associated with the risk of non-contact anterior cruciate ligament injury. J Orthop Res 32:61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beynnon BD, Hall JS, Sturnick DR, et al. 2014. Increased slope of the lateral tibial plateau subchondral bone is associated with greater risk of noncontact ACL injury in females but not males. A prospective cohort study with a nested, matched, case-control analysis. Am J Sports Med 42:1039–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hohmann E, Bryant A, Reaburn P, et al. 2011. Is there a correlation between posterior tibial slope and non-contact anterior cruciate ligament injuries? Knee Surg Sports Trau-matol Arthrosc 19:S109–114. [DOI] [PubMed] [Google Scholar]
- 11.Todd MS, Lalliss S, Garcia E, et al. 2010. The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med 38:63–67. [DOI] [PubMed] [Google Scholar]
- 12.Dejour H, Bonnin M. 1994. Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br Vol 76:745–749. [PubMed] [Google Scholar]
- 13.McLean SG, Oh YK, Palmer ML, et al. 2011. The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. J Bone Joint Surg Am Vol 93:1310–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lipps DB, Oh YK, Ashton-Miller JA, et al. 2012. Morphologic characteristics help explain the gender difference in peak anterior cruciate ligament strain during a simulated pivot landing. Am J Sports Med 40:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krosshaug T, Nakamae A, Boden BP, et al. 2007. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med 35:359–367. [DOI] [PubMed] [Google Scholar]
- 16.Feucht MJ, Mauro CS, Brucker PU, et al. 2013. The role of the tibial slope in sustaining and treating anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 21:134–145. [DOI] [PubMed] [Google Scholar]
- 17.White JL, Gebo DL. 2004. Unique proximal tibial morphology in strepsirrhine primates. Am J Primatol 64:293–308. [DOI] [PubMed] [Google Scholar]
- 18.Li G, DeFrate LE, Park SE, et al. 2005. In vivo articular cartilage contact kinematics of the knee: an investigation using dual-orthogonal fluoroscopy and magnetic resonance image-based computer models. Am J Sports Med 33:102–107. [DOI] [PubMed] [Google Scholar]
- 19.Walker PS, Erkman MJ. 1975. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res 109:184–192. [DOI] [PubMed] [Google Scholar]
- 20.Smith HC, Johnson RJ, Shultz SJ, et al. 2012. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Med 40:521–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hashemi J, Chandrashekar N, Mansouri H, et al. 2010. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med 38:54–62. [DOI] [PubMed] [Google Scholar]
- 22.Beynnon BD, Johnson RJ, Fleming BC, et al. 1997. The effect of functional knee bracing on the anterior cruciate ligament in the weightbearing and nonweightbearing knee. Am J Sports Med 25:353–359. [DOI] [PubMed] [Google Scholar]
- 23.Fleming BC, Renstrom PA, Beynnon BD, et al. 2001. The effect of weightbearing and external loading on anterior cruciate ligament strain. J Biomech 34:163–170. [DOI] [PubMed] [Google Scholar]
- 24.Breslow NE, Lubin JH, Marek P, et al. 1983. Multiplicative models and cohort analysis. J Am Stat Assoc 78:1–12. [Google Scholar]
- 25.Prodromos CC, Han Y, Rogowski J, et al. 2007. A metaanalysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy 23:1320–1325, e1326. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


