Abstract
Introduction
Timely antenatal care (ANC) and postnatal care (PNC) attendance decrease maternal and child mortality by improving maternal and child health (MCH) outcomes. Mobile health or mHealth has been identified as an effective way of improving the uptake of MCH services. The MomConnect programme is an mHealth initiative launched by the National Department of Health of South Africa in August 2014 to support MCH. Although widely used, there is a limited understanding of how, why, for whom and under which health system conditions, the implementation of MomConnect improves the health-seeking behaviour of pregnant women and mothers of infants in ANC and PNC facilities. This paper describes the protocol for a realist evaluation of the MomConnect programme, to provide a theory-based understanding of how, why and under what healthcare conditions the MomConnect programme works or not.
Method and analysis
We will use the realist evaluation approach through its research cycle conducted in three phases. In phase I, a multimethod elicitation study design will be used, including a document review, key informant interviews and a scoping review to formulate an initial programme theory of the MomConnect intervention. Content and thematic analytic approaches will be used to analyse the data that will be fitted into a realist framework to formulate the initial programme theory. In phase II, a multi-case study design will be applied using a multimethod approach in two South African provinces. In each case, a theory-testing approach underpinned by the hypothetico-deduction analytic model will be used to test the initial programme theory. Surveys, interviews and focus group discussions will be conducted with various programme actors and analysed using appropriate methods. Phase III will entail refining the tested/modified programme theory through cross-case analysis.
Expected outcomes
An improved understanding of how and why the MomConnect intervention improves the health-seeking behaviour of pregnant women and mothers of infants, and the health system conditions that influence its implementation.
Ethics and dissemination
Ethics approval was granted by the Stellenbosch University Ethics Committee (S18/09/189). The protocol has been designed and the study will be conducted in line with the principles of the Declaration of Helsinki (1964).
Keywords: quality In healthcare, primary care, public health
Strengths and limitations of this study.
The study provides a blueprint on how, why and for whom the MomConnect programme works (or not) within the South African context.
The proposed study will use a multi-case study design applying a mixed-methods approach, which allows for valid theories to be elicited, tested and refined.
Although cross-case analysis and abstraction allows for theory refining, the cross-case analysis of four or more cases can be very challenging.
The identification of what constitute a mechanism and context in some cases can be confusing.
Introduction
In recent decades, there has been greater use of antenatal (ANC) and postnatal care (PNC) services in South Africa, with higher rates of delivery assisted by professional healthcare providers (HCPs).1 ANC facilitates timely follow-up of pregnant women, to prevent complications such as premature delivery and pre-eclampsia, as well as predict the type of delivery, thereby reducing pregnancy-related morbidity and mortality.2–4 Early PNC is important for the well-being of both mothers and newborns, since it allows clinicians to screen for psychological and physical changes in the first days following birth.4 Despite increasing utilisation in the country as a whole, access to early ANC and PNC services remains limited in certain provinces.1
In South Africa, the maternal mortality ratio declined from 2014 to 2017,5 with an institutional maternal mortality rate of 134/100 000 live births reported in 2016. The case fatality rate for excessive bleeding associated with caesarean delivery dropped from 33.1 (2011–2013) to 31 (2014–2016) deaths per 100 000 caesarean deliveries.5 In total, almost all (98%) of these cases occurred at tertiary hospitals in the public sector, where the majority of caesarean deliveries were performed, and attributable to referral from district hospitals after caesarean delivery with unresolved bleeding.5 Complications of hypertension in pregnancy and obstetric haemorrhaging are hence still major causes of maternal mortality, which can be prevented through early uptake of ANC and PNC services.5
In order to achieve the health outcomes enshrined under the sustainable development goals, which include addressing the challenges faced by maternal and child health (MCH) service delivery,4 6 7 South Africa developed a strategic plan to reduce maternal and child mortality by improving the uptake of ANC and PNC services. The plan included integrating mobile health technology (mHealth) into the healthcare system as a strategy to overcome barriers to universal health coverage.7 The MomConnect programme is an example of the application of this mHealth technology. The present paper presents a protocol for evaluating the MomConnect programme in depth.
Background
mHealth is an element of electronic health used for the provision of healthcare services using information and communication technology.8 mHealth places specific focus on the use of mobile phone technology based on text messages, regarded as a quick and cost-effective form of communication.9 Since mobile phone broadband coverage reaches an estimated 69% of the global population, the growing accessibility of mobile phones has supported the use of mHealth in public health.10 Even people living in rural areas in low and middle-income countries (LMICs) have access to smart phones with internet connectivity11 12 and about 8 out of every 10 people living in LMICs own a mobile phone.13 In 2017, South Africa reached a mobile-cellular subscription rate of 162%.14
There is interest in the use of mHealth in MCH, since health facilities in LMICs are sometimes difficult to access due to long distances. The use of mHealth in LMICs may support MCH12 by promoting healthier lifestyle habits, enhancing medication adherence and enforcing regular attendance of follow-up visits, thereby helping to prevent perinatal complications.15–17 In addition, the use of mHealth facilities improves the communication between healthcare service providers and users,18 and promote the uptake of MCH services. Furthermore, a study by Feroz et al 17 confirmed the relevance of mHealth initiatives in MCH as a tool for promoting health education and behavioural change, in turn leading to improved uptake of MCH services.17 For example, the ‘Text4 Baby’ intervention in the USA and Russia examined preparedness among new mothers towards improved MCH.19 Mothers who received the Text4 Baby messages were three times more likely to feel ready and prepared to be a mother compared with the control group.
In South Africa, there has been specific interest in the Cell-Life Mobile Alliance for Maternal Action (MAMA) SMS application as a tool for improving MCH outcomes. This service targets pregnant women and mothers with babies up to 3 months old and focuses on HIV prevention particularly mother-to-child transmission of HIV. The use of the MAMA application improved health-seeking behaviour in the target population, and increased the rates of exclusive breast feeding, delivery in health facilities, use of skilled birth attendants for delivery and adherence to recommended ANC and PNC visits.20 21
The MomConnect intervention
The MomConnect intervention is a prototype for mHealth in South Africa.22 MomConnect is a flagship programme of the South African National Department of Health launched in August 2014. The programme uses mobile phone technology to provide pregnant and postpartum women with twice-weekly health information text messages, and access to a helpdesk for patient queries and feedback.23 24 The ultimate goal of the MomConnect programme is to register all pregnant women on a national database and provide users with important information on health promotion via a platform for feedback, free of charge.25
By dialling *120*550#, on a mobile phone, users subscribe to the MomConnect service and receive messages which encourage them to register at the nearest clinic offering ANC services. Once registered at a clinic, the user gains access to a two-way interactive system through unstructured supplementary service data-based surveys and help desk assistance.23 26 The help desk service is mostly used to obtain information on maternal health rather than discussing the services received at a clinic.26 Engelhard et al 27 demonstrated the feasibility and efficacy of the helpdesk in improving quality of care, but also emphasised the need to benchmark its performance and explore opportunities for improvement elsewhere.27
By August 2017, the MomConnect programme had registered over 1.7 million pregnant women at over 95% of public health facilities, representing 63% of all women attending their first ANC appointment and suggesting that the programme is meeting its target of identifying and responding to users’ needs.28 An evaluation of the MomConnect programme in 2016 showed that participants reported that the intervention empowered them to better manage their health during pregnancy and that of their babies, and that mothers developed a particular connection with, and trusted the source of the messages.29
The MomConnect programme has seen a rapid scaling-up through strong government support and partnerships between key stakeholders. Because of its expanding coverage, MomConnect represents a powerful platform for real-time data collection and linkage to additional services to improve patient care.23 The MomConnect initiative has contributed to the integration of information systems to support MCH clinical services,30 and represents an important starting point to link other health services and databases.31 The challenges experienced during the use of the MomConnect intervention in most clinics was related to poor network coverage.29 The need for improvement in areas such as registration and language has also been highlighted.29
Studies to date have largely focused on the effectiveness of mHealth programmes such as the use of SMS services to remind patients of the timely use of ANC and PNC services and its resultant effect on health-seeking behaviour.17 29 32 33 These studies did not provide consistent results on how the use of mobile phones influences the uptake of ANC and PNC services. For instance, LeFevre et al 34 showed the importance of the MomConnect programme in MCH, but other elements such as why some women used the services more than others were not explored. In addition, the mechanisms through which the use of mobile phones influences health-seeking behaviour have not been clearly explained. Towards this end, a realist evaluation is proposed to understand how, why, for whom and under what health systems conditions the MomConnect programme improves the health-seeking behaviour of pregnant women and mothers of infants in the uptake of MCH services.
Study setting
The study will be conducted in the Gauteng (GT) and Free State (FS) provinces of South Africa (figure 1). These provinces were selected based on the highest (GT) and lowest (FS) rates of MomConnect registration from September 2014 to June 2017. GT accounted for 299 417 (22.2%) and FS for 64 416 (4.8%) of the total number of national registrations of 1 337 889 for this period.34 The district health barometer (DHB) 2016/2017 reported 71.2% of PNC visits within 6 days in GT which is lower than the national average of 75% and also lower than that of FS (85.9%), which is higher than the national average. ANC first visit before 20 weeks was 58.4% in GT far less than the national average in the same period (1). However, our selection of the study participating provinces is based on the highest and lowest rates of MomConnect registration and not on ANC/PNC attendance rates.
Figure 1.
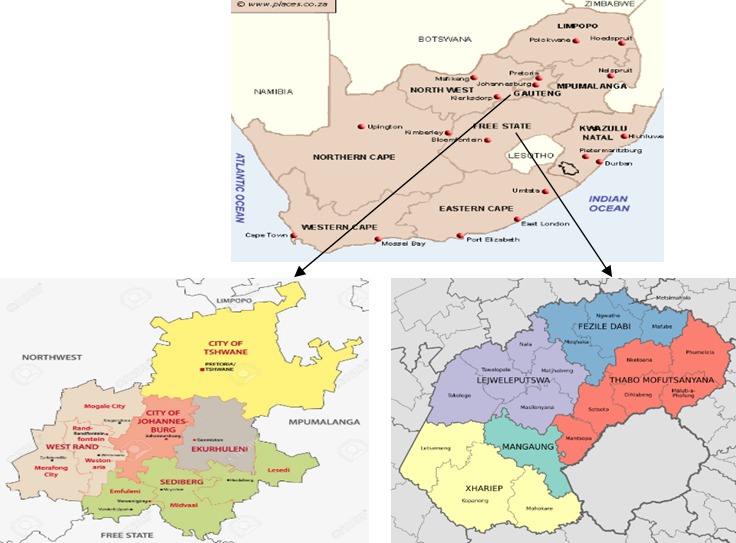
Map of South Africa and study settings (Setting 1: Gauteng and Setting 2: Free State).
GT and FS provinces differ from each other in terms of socioeconomic and demographic characteristics of their inhabitants.1 The use of mobile phones in GT and FS in 2016 was 98.2% and 94.9%, respectively.35 Table 1 presents information on the socioeconomic and demographic characteristics of the populations living in GT and FS. Western Rand and Johannesburg city districts were identified as study settings located in the best resourced province (GT), while in FS (less resourced province) two districts, Xhariep and Fezile Dabi, were selected. Xhariep is the largest district in FS and is among the best resourced’ districts in the province. The selected sub-districts in which the study facilities will be chosen included Randfontein and Johannesburg Sub-district A in GT and FS Naledi and Moqhaka (see table 1). The district health information system (DHIS) data of 2016 were used to select the district and sub-districts included in the study. The detail on how districts and sub-districts were selected is provided in the Sampling and data collection section.
Table 1.
Socioeconomic and demographic factors
| Gauteng | Free state | |
| 1.Western Rand district | 1. Xhariep district | |
| Population | 884 031 | 135 036 |
| Sub-districts | Sub-districts: 4
|
Sub-districts: 4
|
| Houses headed by female | 31.75% | 37.6% |
| Formal dwelling | 76.3% | 89.1% |
| Unemployment rate | 26.3% | 26.8% |
| 2. Johannesburg city district | 2. Fezile Dabi district | |
| Population | 5 006 517 | 507 525 |
| Sub-districts | Sub-districts:7
|
Sub-districts: 4
|
| Houses headed by female | 37.7% | 37.5% |
| Formal dwelling | 81.3% | 85.6% |
| Unemployment rate | 61.5% | 33.9% |
DHB 1016/1017 and DHIS data 2016.
DHB, district health barometer; DHIS, district health information system.
ANC first visits before 20 weeks was 58.4% less than the national target of 62.1 in GT while FS had 65.8% of ANC first visits in the same period.1 However, our selection of provinces is based on highest and lowest rate of the MomConnect registration as mentioned above in this section and not on ANC/PNC.
Methods
The study will be guided by the realist evaluation approach, which was introduced through the seminal work of Pawson and Tilley36 to address the question: ‘What works, for whom, why, in what situation, and how?’ with regards to intervention, programmes and policies. The philosophical ontology of realist evaluation is realism, and its epistemological foundation lies in scientific realism.36 Realist evaluation belongs to the family of theory-driven approaches of evaluation. In this light, the approach aims to develop and refine hypotheses of generative causality explicating why and how intervention inputs bring about changes in key outcomes.37 The proposed study will be developed following three different phases, as described in figure 2, and reported following the guidelines for reporting realist evaluation studies.37
Figure 2.
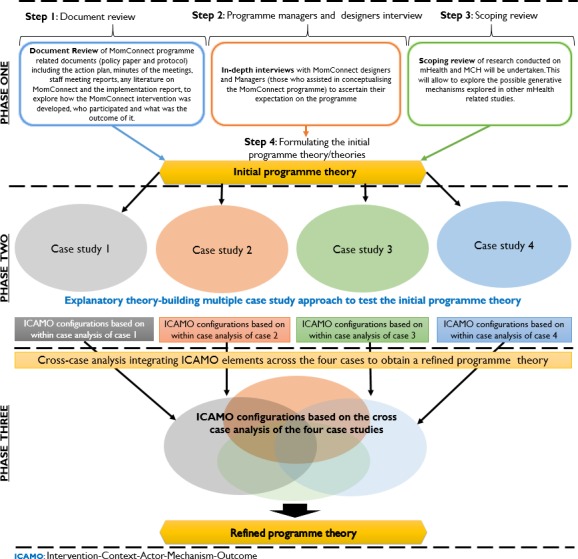
Study design showing phases I to III. Adapted from Mukumbang et al and Van Belle et al 43 50 (Source: study author). ICAMO, Intervention-Context-Actor-Mechanism-Outcome.
Phase I: Gleaning the initial programme theory (12–18 months)
Phase I will address the first objective of the study re-formulating the initial programme theory (IPT) of how the MomConnect programme was expected to work for different actors (designers, health workers and MCH clients). A multimethod elicitation study will be conducted using data collected from the following sources: document review, exploratory study with key informant interviews and a scoping review.38 Since phase I of the study requires many substudies, it is estimated to take between 12 and 18 months depending on funding availability.
Document review
The document review will explore documents such as the action plans, staff meeting reports and other minutes; any literature on MomConnect and the national monitoring and evaluation report. Permission will be requested from the MomConnect monitoring and evaluation team to access these documents and explore how MomConnect was developed, who participated and with what intended objectives.
Document analysis,39 as a methodological process for review and evaluation, will be used to examine and interpret MomConnect documents, including capturing the meaning, gaining understanding and developing empirical knowledge on how the intervention was developed and implemented.39 The Intervention-Context-Actors-Mechanism-Outcomes (ICAMO) heuristic tool40 will be used to guide a content analysis approach.
Exploratory qualitative study
An exploratory qualitative analysis of programme managers and designers’ assumptions and perspectives will be undertaken simultaneously.41 In-depth interviews (IDIs) with 10–15 key informants, including programme designers (those who assisted in programme conceptualisation) and managers (those who assisted in programme implementation and coordination) will be conducted to explore their expectations on how MomConnect was supposed to work. Key informants will be selected using purposive sampling, and face-to-face interviews will be conducted using an interview guide with each key informant.
The IDIs with key informants will be audiorecorded and transcribed verbatim. Summary sheets and field notes will be written up for each interview at the end of the day. Thematic analysis based on the generic inductive approach41 will be conducted using Atlas.ti software V.8.0.
Scoping review
The scoping review of research conducted on mHealth and MCH will be performed by searching the following databases: Academic research complete, Medline, Pubmed, Scopus, Health System Evidence and Google scholar using medical subject headings (MeSH) terms. The following MeSH terms combinations (Boolean phrases) will be used to search the identified databases: [‘mHealth’ AND ‘maternal health’], [‘mobile phone’ AND ‘maternal health’ AND ‘child health’], [‘mHealth AND ‘maternal health services’], [mHealth PRE/15 maternal] and [mHealth PRE/15 maternal AND child AND health].
A thematic analysis42 will be used to explore the various modalities of mHealth, relevant context conditions, possible generative mechanisms and important outcomes reported in other studies conducted on mHealth interventions and MCH. Using abductive reasoning, we will conduct configurational mapping informed by the ICAMO heuristic tool to formulate tentative models of how and why mHealth programmes work in general.
Formulating the initial programme theory
A configurational mapping approach40 guided by the ICAMO heuristic tool will be used to synthesise the information gleaned from the document review, qualitative exploration study with key informants and scoping review, to formulate the IPT that will be tested in phase II.40 The theory formulated will be informed by various abductive reasoning through deductive, inductive and retroductive reasoning forms of inferences making.
Phase II: Testing the initial programme theory (12 –18 months)
The IPT formulated in phase I will be tested in the selected cases using a multimethod study design. In each case, a theory refining research approach will be used, underpinned by the hypothetico-deduction analytic model informed by data from both quantitative and qualitative methods.43 44 Quantitative assessments will be performed using a cross-sectional design, whereby a survey will be used to explore how socioeconomic characteristics influence the uptake of MCH to determine for whom the intervention works. The cross-sectional study could identify possible demi-regularities and contrastives related to the MCH uptake. The qualitative approaches will help us explore the different mechanisms and various context conditions by which the outcomes are generated.
Sampling and data collection
A representative sampling frame from the DHIS was used to obtain the study sample based on ANC first visits before 20 weeks for June 2016. This period was the latest month in the master frame data of DHIS which could be used to calculate the sample. All the districts in each province were drawn to identify districts with the highest and lowest ANC first visits before 20 weeks. In GT, West Rand and Johannesburg districts have the highest (69.0%) and lowest (57.3%) rates, respectively. The Randfontein sub-district in West Rand District was identified as the best sub-district with the highest rate of ANC first visits before 20 weeks (80.3%), while Johannesburg A was the sub-district with the lowest rate in the Johannesburg district (50.6%). Similarly, in the FS Province the districts with the highest (73.4%) and lowest (69.1%) rates are Xhariep and Fezile Dabi districts, respectively. Naledi Sub-district (Xhariep District) was identified as the sub-district with the highest rate (80.4%) while Moqhaka Sub-district (Fezile Dabi District) was the sub-district with the lowest rate (55.0%).
OpenEpi software and MS Excel were used to randomly select four facilities in each sub-district (see table 2). The sample size in each facility was calculated,45 assuming 50% prevalence of MCH services agreement per facility, a precision (d) of 0.10 and a 95% CI. The monthly estimated number of MCH visits for each facility and the proportion of ANC first visits before 20 weeks were used to calculate the sample size using an online calculator.45 In cases where the ratio of the sample size (n) to the population size (N) is >5%, finite population correction was used.46 The number of users found in all four facilities will be multiplied by a design effect of 1.5 to get the total number of participants (table 2).
Table 2.
Selected sample by districts, sub-districts, facilities and participants
| District |
Gauteng
(District with highest rate) |
Gauteng
(District with lowest rate) |
Free State
(District with highest rate) |
Free Sate
(District with lowest rate) |
| Sub-district | Randfontein sub-district (8 facilities) | Johannesburg A (14 facilities) |
Naledi (4 facilities) |
Moqhaka (4 facilities) |
| Facility | Kocksoord Clinic ANC 1 visit <20 weeks =82.0% |
Mayibuye Clinic ANC 1 visit <20 weeks =49.0% |
Vanstadensrus Clinic ANC 1 visit <20 weeks =75.0% |
Thusanong (Kroon) Clinic ANC 1 visit <20 weeks =69.0% |
| Sample per facility* | Number of participants = 53×1.5=80 |
Number of participants=85×1.5=127 | Number of participants = 66×1.5=99 |
Number of participants = 74×1.5=111 |
*Estimated number of participants (based on proportional sampling).
ANC, antenatal care.
The study participants will include all pregnant women and mothers of infants registered under the MomConnect programme, who are ≥18 years of age, irrespective of parity (including stillbirths/miscarriages) and socioeconomic status. They will be identified through the MomConnect registration registers at facility level. HCPs will include clinical staff in charge of ANC and PNC at facility level and will be selected based on their prior experience with the MomConnect programme.
A structured questionnaire survey tool has been developed (online additional file 1) to collect quantitative data from pregnant women and mothers of infants registered with the MomConnect programme. This tool will assess their understanding of how psychological determinants, sociocultural context and structural context influence their uptake of MCH services. An appointment will be made with each participant, using the contact details captured in the MomConnect database, to invite them to the facility to participate in the study. In addition, the survey instruments will be administered telephonically to those participants who are unable to visit the facility during the study period.
bmjopen-2019-029745supp001.pdf (289.6KB, pdf)
Furthermore, a facility assessment questionnaire (online additional file 2) will be administered to HCPs at facility level to explore the structural and contextual attributes that may influence the uptake of ANC and PNC services.
bmjopen-2019-029745supp002.pdf (199.6KB, pdf)
Qualitative assessments will include IDIs and focus group discussion (FGDs). An estimated 10–20 IDI will be conducted with HCPs at facility level to explore their perceptions on the resources, implementation processes and programme uptake of the MomConnect programme. See online additional files 3, 4, and 5 for interview and FGD guidelines with patients and HCPs. Four FGDs (one per facility) consisting of between 10 and 15 participants will be conducted by the field workers and the principal researcher to explore participants' perceptions regarding the uptake of MCH services and expectations of the MomConnect programme. Daily activities in selected ANC and PNC facilities will be observed as well. IDIs and FGDs will be audiorecorded and transcribed verbatim to be analysed using Atlas.ti 8.0. The interview guide and survey questionnaire are designed in English but will be translated into the local language used in the different study settings (Afrikaans, Setswana, Sesotho, Zulu, Xhosa) and back-translated to English. Data gathered from the above sources will be transcribed, translated and back-translated in preparation for analysis.
In each case, a theory refining research approach underpinned by the hypothetico-deduction analytic model will be used for both quantitative and qualitative studies.43 44 The hypothetico-deduction approach is the most appropriate when testing an existing theory or a theory formulated a priori. This approach allows for various aspects and the entire hypothesis or initial theory to be examined in light of the new evidence that is emerging in the various cases.
Data analysis
Inferential and descriptive analyses of the quantitative data including proportions and frequencies will be performed using Stata V.15. Socioeconomic and demographic data will be used as independent variables while the uptake of MCH will be used as the dependent variable, which will allow us to determine for whom the intervention works. For bivariate analysis, categorical data will be analysed using Χ2 test. Logistic regression models will be constructed to assess the effects of independent variables as predictors of dependent outcomes of interest. The power of each dependent variable will be tested before the variable is included in the model, and variables with positive and negative outcomes will be maintained. A p value <0.05 will be used to indicate statistical significance along with a 95% corresponding CI.
For qualitative data, IDI and FGDs will be analysed separately using a thematic content analysis approach to identify and make explicit the mechanism by which observed outcomes are generated using the ICAMO framework. FGDs and IDI transcripts will be uploaded onto Atlas.ti 8.0 for analysis.
Deductive and inductive thematic analyses will be applied to analyse the data collected through observation, IDIs and FGDs following these seven steps: (1) Familiarising with the data set; (2) development of a coding framework, (3) coding a portion of the dataset for each case study, (4) testing code reliability, (5) identifying initial themes emerging from the data, (6) using the code manual to apply codes to the entire script and (7) connecting codes into themes through abstraction.
Modifying the initial programme theory
In-case analysis36 will be conducted using retroductive reasoning47 to modify the ICAMO elements through configuration mapping based on the data obtained from each case to modify the IPT. In other words, ICAMO configurations will be modified into case-based programme theories (for each of the four facilities). Each case-based modified theory will be tested to check their explanatory power through the process of counterfactual thinking towards a functional theory.48 ICAMO matrices will be used to present data for each higher-level outcome of concern.
Phase III: Refining the modified programme theory (6–12 months)
A cross-case analysis of the four case studies will be conducted using retrodictive reasoning to construct ICAMO matrices (ICAMO configuration obtained from each of the four case studies) to obtain a refined programme theory or model. Retrodiction is used to examine the similarities and differences between the theories or models obtained from the different cases. The retrodictive cross-case analysis will allow us to obtain a more refined programme theory to the IPT and the case-specific theories. A refined theory is a clear or functional explanation theory that can be used to give details of the programme elements and their roles in orchestrating the observed outcomes in certain context conditions for the different actors involved. This refined theory, although obtained through analytic generalisation, remains close enough to the observed data, yet provides explanations that are sufficiently general to explain outcomes across settings and social activities.36
Quality control
The RAMESES II guideline for conducting and reporting realist evaluation37 will be used to ensure quality control in the study.
First, to elicit the IPT, all the above steps will be followed to ensure the trustworthiness of data collected from various sources, thus capturing a wide range of intended and unintended outcomes, context-mechanism interactions and relevant actors.
In phase II, to assess the reliability of data collection, a pilot study will be conducted in two healthcare facilities selected for convenience in the sub-district with the highest and lowest rates of ANC first visits before 20 weeks in GT and FS, respectively. The pilot will include HCPs, pregnant women and mothers.
At all levels of the study, quality control and credibility will be assured through data familiarisation by all the investigators and discursive interactions.
Ethics and dissemination
Ethics approval has been granted by the Health Research Ethics Committee of the Stellenbosch University (Ref No: S18/09/189). An approval to conduct the study in the selected facilities is currently being processed by the relevant provincial Department of Health. Consent forms will be used to obtain permission from study participants before data collection. Personal information will be protected by not disclosing names during data analysis or reporting. Different papers will be published from the study, and the results will be presented in academic open day, national and international conferences.
Discussion
Despite the relevance of mHealth in improving MCH being increasingly recognised,49 an empirical investigation to understand how the outcomes are generated is still lacking. This protocol specifies the research plan to investigate how and why the MomConnect programme works or achieves its goal of improving MCH services in South Africa. Study investigators will also seek to understand MomConnect as part of an mHealth programme that uses mobile phones by focusing on how contextual factors affect the use of MCH services.
The proposed study draws on a theory-driven evaluation (TDE) approach, which describes a process under which components are hypothesised to affect outcomes, and considers the specific conditions under which such processes operate.50 TDE is commonly used in the social sciences to investigate how programmes cause intended or observed outcomes,51 as well as address issues around internal and external validities, which is of potential relevance to both researchers and policymakers.50 52 53 The proposed study will use a realist evaluation approach, which is a type of TDE.37 Pawson and Tilley36 developed the realist evaluation to address the question: ‘What works, for whom, why, in what situation and how?’ Realist evaluation is selected to assess in particular how the use of mobile phones influences the uptake of MCH services.
The protocol is an important quality tool as it allows for follow-up by anticipating the challenges and barriers that may occur during the study.54 55 This study protocol also assists in thinking through how to generate the internal consistency and external validity of results and to explain how the intervention works in a given context to produce the observed outcome. The lack of such protocol can lead to some issues, such as lack of explanation of the change at or between individual, institutional or contextual levels because these were not documented from the start.56 Moreover, writing a detailed research protocol is important in helping other researchers to replicate relevant study findings for contribution towards the broader research community. Constructing a comprehensive protocol including clear aims, rationale, analysis plans and expectations lends additional credibility to research across study fields.56
It is expected that this study will improve our understanding of how and why the MomConnect intervention impacts the health-seeking behaviours of pregnant women and mothers of infants. This study is also expected to provide a detailed description of the health system conditions that influence the implementation of the MomConnect programme to improve the uptake of ANC and PNC services. Finally, the study will provide some recommendations to improve the roll-out and implementation of MomConnect elsewhere.
bmjopen-2019-029745supp003.pdf (204.5KB, pdf)
bmjopen-2019-029745supp004.pdf (197.9KB, pdf)
bmjopen-2019-029745supp005.pdf (200.5KB, pdf)
Supplementary Material
Footnotes
Contributors: The study was conceived by EMK and PD. The first manuscript was written by EMK. FCM and EN provided methodological support. FCM, PD and EN provided critical contributions towards developing and refining the manuscript. All authors read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Ethics approval: Stellenbosch University Human Research Ethics Committee (Ref No S18/09/189).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not required.
Map disclaimer: The depiction of boundaries on the map(s) in this article do not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
References
- 1. Massyn N, Padarath A, Peer N, et al. . District Health Barometer. 2017. www.hst.org.za/./District-Health-Barometer-201617.aspx.
- 2. Symon A, Pringle J, Cheyne H, et al. . Midwifery-led antenatal care models: mapping a systematic review to an evidence-based quality framework to identify key components and characteristics of care. BMC Pregnancy Childbirth 2016;16:168 10.1186/s12884-016-0944-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ram F, Singh A. Is antenatal care effective in improving maternal health in rural uttar pradesh? Evidence from a district level household survey. J Biosoc Sci 2006;38:433–48. 10.1017/S0021932005026453 [DOI] [PubMed] [Google Scholar]
- 4. Massyn N, Peer N, Padarath A, et al. . District Health Barometer. 2016. www.hst.org.za/./-District-Health-Barometer-201516.aspx.
- 5. Moodley J, Chb MB, Fawcus S, et al. . Improvements in maternal mortality in South Africa. South African Medical Research 2018;108:4–8. [Google Scholar]
- 6. Sachs JD. From millennium development goals to sustainable development goals. Lancet 2012;379:2206–11. 10.1016/S0140-6736(12)60685-0 [DOI] [PubMed] [Google Scholar]
- 7. Le Blanc D. Towards Integration at Last? The Sustainable Development Goals as a Network of Targets. Sustainable Development 2015;23:176–87. 10.1002/sd.1582 [DOI] [Google Scholar]
- 8. Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health 2014;14:188–203. 10.1186/1471-2458-14-188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? Global Health 2006;2:9 10.1186/1744-8603-2-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sanou B. ICT Facts & Figures. The world in 2015. Itu 150 Años (1865 - 2015). 2015:1–6 http://www.itu.int/en/ITU-D/Statistics/Documents/facts/ICTFactsFigures2015.pdf.
- 11. Premji S. Mobile health in maternal and newborn care: fuzzy logic. Int J Environ Res Public Health 2014;11:6494–503. 10.3390/ijerph110606494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Oyeyemi SO, Wynn R. The use of cell phones and radio communication systems to reduce delays in getting help for pregnant women in low- and middle-income countries: a scoping review. Glob Health Action 2015;8:28887–95. 10.3402/gha.v8.28887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. World Bank. World Development Report 2016: Digital Dividends. 2016. http://www.worldbank.org/en/publication/wdr2016.
- 14. Services P. South Africa Profile (Latest data available: 2017), 2017:1–3. [Google Scholar]
- 15. Watterson JL, Walsh J, Madeka I. Using mHealth to improve usage of antenatal care, postnatal care, and immunization: a systematic review of the literature. Biomed Res Int 2015;2015:1–9. 10.1155/2015/153402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Poorman E, Gazmararian J, Parker RM, et al. . Use of text messaging for maternal and infant health: a systematic review of the literature. Matern Child Health J 2015;19:969–89. 10.1007/s10995-014-1595-8 [DOI] [PubMed] [Google Scholar]
- 17. Feroz A, Perveen S, Aftab W. Role of mHealth applications for improving antenatal and postnatal care in low and middle income countries: a systematic review. BMC Health Serv Res 2017;17:704 10.1186/s12913-017-2664-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wambugu S, Villella C. mHealth for Health Information Systems in Low- and Middle-Income Countries: Challenges and Opportunities in Data Quality, Privacy. and Security. mHealth Information System 2016:1–19. [Google Scholar]
- 19. Parker RM, Dmitrieva E, Frolov S, et al. . Text4baby in the United States and Russia: an opportunity for understanding how mHealth affects maternal and child health. J Health Commun 2012;17 Suppl 1:30–6. 10.1080/10810730.2011.649162 [DOI] [PubMed] [Google Scholar]
- 20. USAIDS. Mobile Alliance for Maternal Action (MAMA). mHealth knowledge. 2015. http://www.mhealthknowledge.org/search/site/MAMA.
- 21. Ausen-anifrani S, Burman MK, Pastick K. SMS Maama. United Nation Found. 2016:1–14 http://www.askmama.co.za/.
- 22. Peter JE, Barron P, Pillay Y. Using mobile technology to improve maternal, child and youth health and treatment of HIV patients. S Afr Med J 2015;106:3 10.7196/SAMJ.2016.v106i1.10209 [DOI] [PubMed] [Google Scholar]
- 23. Barron P, Peter J, LeFevre AE, et al. . Mobile health messaging service and helpdesk for South African mothers (MomConnect): history, successes and challenges. BMJ Glob Health 2018;3:e000559 10.1136/bmjgh-2017-000559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Seebregts C, Dane P, Parsons AN, et al. . Designing for scale: optimising the health information system architecture for mobile maternal health messaging in South Africa (MomConnect). BMJ Glob Health 2018;3:e000563–7. 10.1136/bmjgh-2017-000563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mehl GL, Tamrat T, Bhardwaj S, et al. . Digital health vision: could MomConnect provide a pragmatic starting point for achieving universal health coverage in South Africa and elsewhere? BMJ Glob Health 2018;3:e000626–5. 10.1136/bmjgh-2017-000626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Xiong K, Kamunyori J, Sebidi J. The MomConnect helpdesk: how an interactive mobile messaging programme is used by mothers in South Africa. BMJ Glob Health 2018;3:e000578 10.1136/bmjgh-2017-000578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Engelhard M, Copley C, Watson J, et al. . Optimising mHealth helpdesk responsiveness in South Africa: towards automated message triage. BMJ Glob Health 2018;3:e000567–9. 10.1136/bmjgh-2017-000567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pillay Y, Motsoaledi PA. Digital health in South Africa: innovating to improve health. BMJ Glob Health 2018;3:4–6. 10.1136/bmjgh-2018-000722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Skinner D, Delobelle P, Pappin M, et al. . User assessments and the use of information from MomConnect, a mobile phone text-based information service, by pregnant women and new mothers in South Africa. BMJ Glob Health 2018;3:e000561 10.1136/bmjgh-2017-000561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Heekes A, Tiffin N, Dane P, et al. . Self-enrolment antenatal health promotion data as an adjunct to maternal clinical information systems in the Western Cape Province of South Africa. BMJ Glob Health 2018;3:e000565 10.1136/bmjgh-2017-000565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Peter J, Benjamin P, LeFevre AE, et al. . Taking digital health innovation to scale in South Africa: ten lessons from MomConnect. BMJ Glob Health 2018;3:1–4. 10.1136/bmjgh-2017-000592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Free C, Phillips G, Watson L, et al. . The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Med 2013;10:e1001363 10.1371/journal.pmed.1001363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Agarwal S, Perry HB, Long LA, et al. . Evidence on feasibility and effective use of mHealth strategies by frontline health workers in developing countries: systematic review. Trop Med Int Health 2015;20:1003–14. 10.1111/tmi.12525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. LeFevre AE, Dane P, Copley CJ, et al. . Unpacking the performance of a mobile health information messaging program for mothers (MomConnect) in South Africa: evidence on program reach and messaging exposure . BMJ Glob Health 2018;3:e000583 10.1136/bmjgh-2017-000583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Statistics South Africa c General Household Survey 2016. 2018. http://microdata.worldbank.org/index.php/catalog/2879/.
- 36. Pawson R, Tilley N. Realistic evaluation. Sage. 1997. https://journals.sagepub.com/doi/pdf/.
- 37. Wong G, Westhorp G, Manzano A, et al. . RAMESES II reporting standards for realist evaluations. BMC Med 2016;14:96–114. 10.1186/s12916-016-0643-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Downs DS, Hausenblas HA. Elicitation studies and the theory of planned behavior: a systematic review of exercise beliefs. Psychol Sport Exerc 2005;6:1–31. 10.1016/j.psychsport.2003.08.001 [DOI] [Google Scholar]
- 39. Bowen GA. Document analysis as a qualitative research method. Qualitative Research Journal 2009;9:27–40. 10.3316/QRJ0902027 [DOI] [Google Scholar]
- 40. Mukumbang FC, Marchal B, Van Belle S, et al. . A realist approach to eliciting the initial programme theory of the antiretroviral treatment adherence club intervention in the Western Cape Province, South Africa. BMC Med Res Methodol 2018;18:47 10.1186/s12874-018-0503-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Thomas DR. A General Inductive Approach for Analyzing Qualitative Evaluation Data. Am J Eval 2006;27:237–46. 10.1177/1098214005283748 [DOI] [Google Scholar]
- 42. Ritchie J, Spencer L. Qualitative Data Analysis for Applied Policy Reasearch. The qualitative researcher’s companion 2002:305–29. [Google Scholar]
- 43. Mukumbang FC, Marchal B, Van Belle S, et al. . Unearthing how, why, for whom and under what health system conditions the antiretroviral treatment adherence club intervention in South Africa works: A realist theory refining approach. BMC Health Serv Res 2018;18:343 10.1186/s12913-018-3150-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Eastwood JG, Jalaludin BB, Kemp LA. Realist explanatory theory building method for social epidemiology: a protocol for a mixed method multilevel study of neighbourhood context and postnatal depression. Springerplus 2014;3:12 10.1186/2193-1801-3-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Naing L, Winn T, Rusli BN. Practical issues in calculating the sample size for prevalence studies. Arch Orofac Sci 2006;1:9–14. [Google Scholar]
- 46. Burstein H. Finite population correction for binomial confidence limits. J Am Stat Assoc 1975;70:67–9. 10.1080/01621459.1975.10480263 [DOI] [Google Scholar]
- 47. Zoltan D. Plenary Speech Researching complex dynamic systems : ‘Retrodictive qualitative modelling’ in the language classroom. Cambridge University Pree 2011;47:80–91. [Google Scholar]
- 48. Roese NJ. Counterfactual thinking. Psychol Bull 1997;121:133–48. 10.1037/0033-2909.121.1.133 [DOI] [PubMed] [Google Scholar]
- 49. Lee SH, Nurmatov UB, Nwaru BI, et al. . Effectiveness of mHealth interventions for maternal, newborn and child health in low- and middle-income countries: Systematic review and meta-analysis. J Glob Health 2016;6:1–17. 10.7189/jogh.06.010401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Van Belle SB, Marchal B, Dubourg D, et al. . How to develop a theory-driven evaluation design? Lessons learned from an adolescent sexual and reproductive health programme in West Africa. BMC Public Health 2010;10:141–51. 10.1186/1471-2458-10-741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Coryn CLS, Noakes LA, Westine CD, et al. . A systematic review of theory-driven evaluation practice from 1990 to 2009. Am J Eval 2011;32:199–226. 10.1177/1098214010389321 [DOI] [Google Scholar]
- 52. Chen H-T. The conceptual framework of the theory-driven perspective. Eval Program Plann 1989;12:391–6. 10.1016/0149-7189(89)90057-8 [DOI] [Google Scholar]
- 53. Chen H-T, Rossi H. Issues in the Theory-Driven. Evaluation Program Planning 1989;12:299–306. [Google Scholar]
- 54. Chen L, Wang W, Du X, et al. . Effectiveness of a smart phone app on improving immunization of children in rural Sichuan Province, China: study protocol for a paired cluster randomized controlled trial. BMC Public Health 2014;14:262 10.1186/1471-2458-14-262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mukumbang FC, Van Belle S, Marchal B, et al. . Realist evaluation of the antiretroviral treatment adherence club programme in selected primary healthcare facilities in the metropolitan area of Western Cape Province, South Africa: a study protocol. BMJ Open 2016;6:e009977–88. 10.1136/bmjopen-2015-009977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Prashanth NS, Marchal B, Hoeree T, et al. . How does capacity building of health managers work? A realist evaluation study protocol. BMJ Open 2012;2:e000882 10.1136/bmjopen-2012-000882 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-029745supp001.pdf (289.6KB, pdf)
bmjopen-2019-029745supp002.pdf (199.6KB, pdf)
bmjopen-2019-029745supp003.pdf (204.5KB, pdf)
bmjopen-2019-029745supp004.pdf (197.9KB, pdf)
bmjopen-2019-029745supp005.pdf (200.5KB, pdf)


