Abstract
Background. Research has found a strong link between ageism, in the form of negative stereotypes, prejudice, and discrimination toward older people, and risks to their physical and mental health. Little is known, however, about the effectiveness of strategies to reduce ageism.
Objectives. To assess the relative effects of 3 intervention types designed to reduce ageism among youths and adults—education, intergenerational contact, and combined education and intergenerational contact—by conducting a systematic review and meta-analysis.
Search Methods. We searched PubMed, PsycINFO, AgeLine, EBSCO, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Global Index Medicus, Database of Abstracts of Reviews of Effects (DARE), Epistemonikos, Cochrane Database of Systematic Reviews, Campbell Collaboration, PROSPERO, GreyLit, and OpenGrey. We identified additional records by hand-searching reference lists of relevant review articles as well as records included in the meta-analysis. Two independent reviewers completed the search and screening process.
Selection Criteria. Eligible studies were those that (1) evaluated an intervention designed to reduce ageism, (2) examined at least 1 ageism outcome in relation to older adults, (3) used a design with a comparison group (randomized or nonrandomized), and (4) were published after 1970, when the ageism concept was developed.
Data Collection and Analysis. Two independent reviewers extracted study-level data from records using a common data collection spreadsheet. They also assessed study quality by using the Cochrane Risk of Bias Tool, and used the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) tool to assess quality of outcome evidence. Primary outcomes were attitudes toward older people and accuracy of knowledge about aging and older people. Secondary outcomes included comfort with older adults, anxiety about one’s own aging, and interest in working in the field of geriatrics or gerontology. We carried out meta-analyses with statistical mixed models.
Main Results. We identified 63 eligible studies (1976–2018) with a total sample of 6124 participants. Ageism interventions demonstrated a strongly significant effect on attitudes (differences of standardized mean differences [dD] = 0.33; P < .001), knowledge (dD = 0.42; P < .001), and comfort (dD = 0.50; P < .001), but no significant effect on anxiety (dD = 0.13; P = .33) or working with older adults (dD = −0.09; P = .40). Combined interventions with education and intergenerational contact showed the largest effects on attitudes. We found stronger effects for females and for adolescent and young adult groups.
Authors’ Conclusions. Interventions are associated with substantial reduction in ageism and should be part of an international strategy to improve perceptions of older people and the aging process. Additional research using more rigorous designs to examine the effects of interventions is strongly recommended.
Public Health Implications. Ageism has well-established negative effects on the physical and mental health of older people. Findings suggest that relatively low-cost, feasible strategies involving education and intergenerational contact can serve as the basis of effective interventions to reduce ageism.
PLAIN-LANGUAGE SUMMARY
Ageism is the stereotyping, prejudice, and discrimination against people on the basis of their age. Research has shown that ageism directed toward older adults has a negative impact on their health, well-being, and quality of health care received. The scope of ageism is expected to expand in the context of a growing aging population around the world. Despite the scope and health-related consequences of ageism against older adults, the relative effectiveness of common intervention strategies designed to reduce ageism has not been established. We sought to conduct a systematic review and meta-analysis examining the relative effectiveness of ageism interventions characterized by education, intergenerational contact, or both. Our findings showed that interventions significantly reduced ageism outcomes related to attitudes, knowledge, and comfort toward older adults. Interventions that combined elements of both education and intergenerational contact had the largest effect on people’s attitudes toward older adults. Furthermore, interventions had a stronger effect on females as well as adolescent and young adult age groups. This study suggests that relatively low-cost, feasible interventions should be adopted as a part of an international strategy to reduce ageism. Further investigation using rigorous intervention study designs is strongly recommended for future research.
Ageism, defined as stereotyping, prejudice, or discrimination toward people on the basis of age, is a mounting international concern with important health implications.1 A substantial and growing body of research shows that ageism toward older adults is highly prevalent across countries,2 and the scope of this problem is expected to grow with global population aging. Furthermore, compelling findings have emerged demonstrating that negative attitudes toward aging pose a significant risk to health and well-being in the later years.3,4 Adoption of widespread negative attitudes toward aging contributes to mortality risk, poor functional health, and slower recovery from illness.5 Holding negative perceptions of aging also predicts poor mental health.6–8
Not only do pervasive ageist attitudes and stereotypes contribute to negative health outcomes, but ageism among health care professionals can also result in discriminatory practices that place older people at risk. Studies have found widespread negative attitudes toward older people and old age among physicians, medical students, and nurses.9 Such ageist attitudes can lead to practical consequences for older patients, as assumptions regarding functional and cognitive decline lead to more limited provision of medical information, withholding certain treatment options, and exclusion from clinical trials.10–13 Ageist attitudes have also been found among mental health practitioners and trainees (such as assuming that symptoms such as depression are normal among the aged), which in turn may restrict access to treatments.14 Thus, age stereotyping and prejudice among health providers can affect the quality and quantity of care older people receive and in turn lead to negative health outcomes.15
Ageism also promotes other forms of discrimination including the social exclusion of older persons from meaningful roles and relationships.16 The experience of social exclusion related to unfavorable stereotypes has been identified as a chronic stressor for older people that can compromise health.17 Age-related prejudices lead to discrimination and institutional norms based on stereotypes that limit the participation of older adults.18 At an institutional level, ageist attitudes also inhibit the development of health policies that would benefit older individuals.19–21
Given the extent of ageist attitudes and stereotypes and the negative consequences of ageism for health and quality of care, developing effective interventions to reduce ageism is a priority. Support for this view is provided by growing evidence that reducing ageism can promote positive health behaviors among older people.22 Thus, developing interventions to combat ageism is increasingly viewed as a critical component of healthy aging.23 Interventions include educating professionals and the general public, fostering contact between older individuals and young people (e.g., school-aged children, university students), and experimental attempts to change attitudes.
Despite this promise, the effectiveness of interventions to reduce or prevent ageist stereotypes, prejudice, or discrimination has not been established.24 To date, no systematic review and meta-analysis has been conducted, to our knowledge, that addresses the effectiveness of interventions across age groups to reduce ageism toward older adults. Although the extensive literature on ageism and health outcomes sheds light on the scope and impact of the problem, there is no clear guidance about how to reduce negative views of older adults through targeted interventions.
As part of a larger initiative coordinated by the World Health Organization (WHO) to understand and address the issue of ageism, we conducted a systematic review and meta-analysis of relevant experimental and quasi-experimental intervention studies to examine the relative effectiveness of major types of ageism interventions. On the basis of previous research,25 we categorized interventions into 3 types: educational interventions that provide instruction of some kind designed to reduce ageism, intergenerational contact interventions that feature an opportunity for contact between younger people and older people, and combined interventions that pair the 2 approaches.
METHODS
We conducted a systematic review and meta-analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.26 Eligible studies met the following inclusion criteria: (1) evaluated an intervention designed to reduce ageism, (2) examined at least 1 ageism outcome in relation to older adults, (3) used a design with a comparison group (randomized or nonrandomized), and (4) was published after 1970, when the ageism concept was developed.27
Literature Search Strategy and Selection Criteria
We searched the following electronic databases (academic, gray literature) up until December 2017 by using translations of a comprehensive “ageism” search strategy developed in consultation with information specialists: PubMed, PsycINFO, AgeLine, EBSCO, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Global Index Medicus, Database of Abstracts of Reviews of Effects (DARE), Epistemonikos, Cochrane Database of Systematic Reviews, Campbell Collaboration, PROSPERO, GreyLit, and OpenGrey. The search strategy combined key terms related to “ageism,” “age discrimination,” “age prejudice,” “age stereotype,” or “social exclusion” with terms related to “elder” or “older adults” (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). We identified additional records by hand-searching reference lists of relevant review articles25,28 and the reference lists of the studies included in this meta-analysis. Following an initial phase of removing duplicates and completely irrelevant records, 2 independent reviewers (among C. S., M. W., and C. B.) screened records for potentially eligible titles and abstracts and subsequently reviewed full texts to determine inclusion in the meta-analysis. Disagreements were resolved with a third reviewer (D. B. or K. P.) via consensus. We used Covidence systematic review management software (Veritas Health Innovation Ltd, Melbourne, Australia) to facilitate the screening process. We assessed study eligibility against a systematic review and meta-analysis protocol registered with PROSPERO (ID: CRD42018088349).
Data Analysis
Extraction.
Two reviewers (among C. S., M. W., and R. C.) independently extracted the following study-level data from records by using a common data collection spreadsheet, which was pilot-tested with an initial sample (n = 10) of records: publication year, country, intervention type and duration, research design, participant inclusion and exclusion criteria, sample size, and participant characteristics (e.g., age, gender, race/ethnicity, educational group). For each ageism outcome measure, we extracted mean and SD data for treatment and control groups. If SDs were not provided in the article or available after contacting authors (n = 15), we derived them by using other information provided in the article (i.e., means, Ns, t or F statistics). In some cases, it was necessary to assume equal SDs for control and intervention groups or for baseline and follow-up in the derivation.
Many studies had only 1 follow-up assessment point (n = 51), and the remaining studies (n = 12) varied greatly in the timing of subsequent follow-up assessments (ranging from several weeks to 5 years). For this reason, we used the first follow-up assessment (range = 1–104 weeks; mean = 15 weeks) for all studies in the analysis. We compared data collection sheets from independent reviewers on all data elements, and we resolved discrepancies through consensus.
Studies with multiple intervention arms.
Several studies contained multiple intervention arms. We selected or combined intervention groups to create a single intervention group for each study. All cases of combined arms involved, for example, identical outcomes and protocols (timing of intervention and follow-up) and comparable goals, not requiring modeling of dependence between arms. We selected the original researchers’ “combined” intervention arm when more than 1 of the 3 intervention types were represented in a study. This selection rule aligned with the theoretical expectation that a combined intervention strategy would be more impactful than an approach involving only 1 mode of intervention.
Outcomes.
We organized the ageism measures used across studies (Table A, available as a supplement to the online version of this article at http://www.ajph.org) into 5 outcome categories through research team consensus that reflect common categories of ageism found in the literature25 and represent both self-directed and other-directed dimensions of the construct.29 The meta-analysis examined 2 primary outcomes: attitudes toward aging, including aging stereotypes, perceptions, and prejudice toward older people, and knowledge on aging, including information and misconceptions on the aging process. We examined 3 additional secondary outcomes: comfort and types of behavioral interactions with older adults, anxiety about one’s own aging process, and interest in working in the field of geriatrics or gerontology. If a study reported more than 1 measure for a given outcome category, we selected the measure most commonly used within the pool of included studies. We determined this by selecting the measure that was used most commonly across the studies that considered the outcome in question.
Risk of bias and quality of evidence assessments.
Two reviewers (among C. S., M. W., and R. C.) independently appraised the risk of bias for individual intervention studies by using the Cochrane Risk of Bias Tool, which assesses studies as low or high risk for the following forms of bias: selection, performance, detection, attrition, reporting, and other.30 We resolved discrepancies between reviewers in assessing risk of bias through consensus within the study team. We used the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) tool to assess the quality of the body of evidence across studies for each ageism outcome.31
Methods of analysis.
We carried out meta-analyses by using statistical mixed models. The dependent variables were the standardized mean differences (SMDs) over time (baseline to postintervention) for control and for intervention (outcome mean differences divided by the SD of the difference).
The primary model included treatment (control vs intervention), time of assessment (a repeated measure: baseline vs first follow up upon treatment completion) as fixed classification factors, the interaction between these factors, and studies as levels of a random classification factor. We specified an unstructured error. Random effects help to model heterogeneity among studies. We examined the effect of the intervention on study outcomes by the treatment multiplied by time interaction in this model. Results are reported in terms of differences of SMDs, denoted dD, because of the numerous measurement instruments and scale ranges used by the studies for each outcome.
We examined additional independent variables, including type of intervention (intergenerational contact–only, educational-only, combined intergenerational contact and education), educational age group (preschool or primary-school students, high-school students, university students), year of publication, country of study, randomized controlled trial versus quasi-randomized, mean age of study participants, participant percentage female, participant percentage White, and participant percentage African American. We added each of these variables to the primary model (as a fixed classification factor for categorical variables and as a covariate for quantitative variables; separate models for each variable) as well as its interaction with treatment and time. To examine whether, for example, specific study-level methodological characteristics moderated treatment effects—whether effects were stronger for or limited to certain levels of these characteristics—the focus was on the interaction with treatment, including examination of homogeneity of regressions for the covariates.32 These examinations of moderator variables were limited to the primary outcomes, attitudes, and knowledge because of the limited number of studies assessing the secondary outcomes. We examined a measure of intervention dosage—number of weeks—in a separate model in which we regressed outcomes on these variables for the intervention group only.
In this type of meta-analysis, it is clear that an assumption of studies as fixed (a single true effect size for all studies) is inappropriate. True effect sizes will vary by studies owing not just to sampling error but also to differences in sample composition (e.g., age, ethnicity, education), methods of assessment and study protocol, variable definitions, overall study quality, and numerous other factors. We used mixed models in which we assumed studies to be random (sampled from a population of studies). We assumed effect sizes to differ by studies.
We examined the question of publication bias by constructing funnel plots with sample size plotted against SMD.33
RESULTS
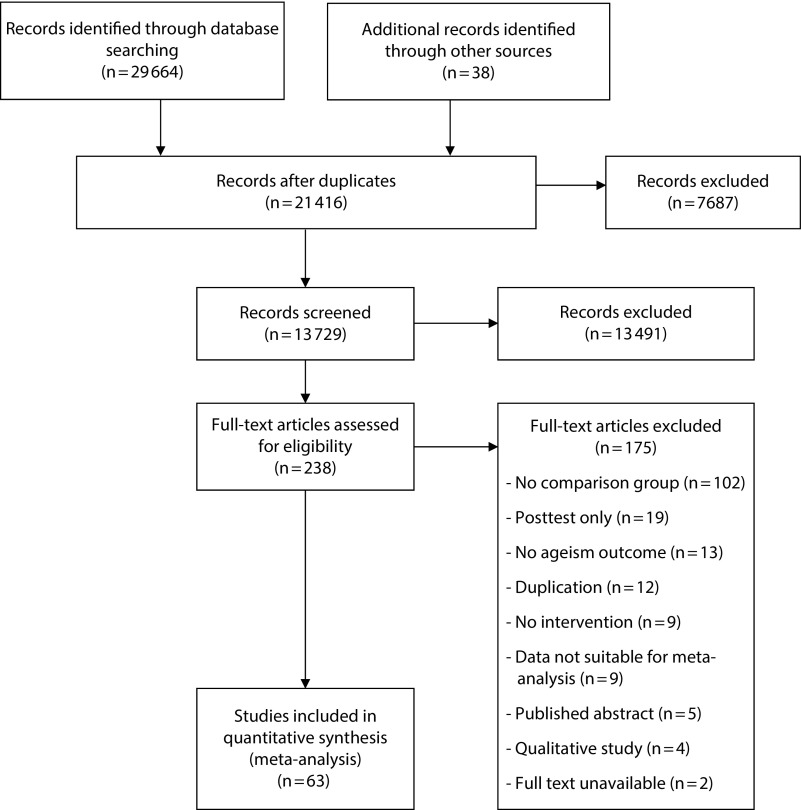
The database and hand searches identified 29 702 total articles, and we identified 238 records for full-text review following removal of duplicates and irrelevant records. We excluded 174 full-text records for several reasons, such as studies lacking a comparison group, pre–post assessment, ageism outcome, and usable data for the purpose of meta-analysis. Exclusions resulted in 6334–96 studies eligible for meta-analysis with a total sample of 6124 participants (Figure 1). Included studies were published between 1976 and 2018. Interventions comprised intergenerational contact–only (33.3%), education-only (36.5%), and combined intergenerational contact and education (30.2%) programs with mean duration of 12.6 weeks (SD = 16.6). Studies included both experimental (8.0%) and quasi-experimental (92.0%) designs. Participants were mostly female (67.2%) and White (66.7%) with mean age 22.4 years (SD = 9.0) across preschool and primary-school (20.7%), high-school (15.9%), undergraduate (20.6%), and graduate or professional (36.5%) educational age groups. The most common ageism outcome category was attitudes toward aging (n = 53) followed by knowledge about aging (n = 19), comfort with older adults (n = 9), interest in working with older adults (n = 6), and anxiety about own aging (n = 5; see Table A for study characteristics).
FIGURE 1—
PRISMA Flow Diagram for Systematic Review of Interventions to Reduce Ageism
Note. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
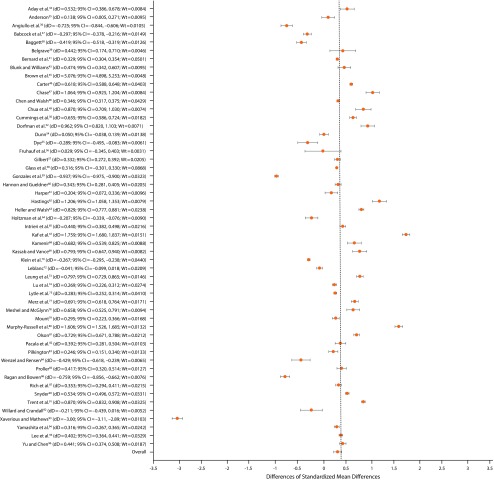
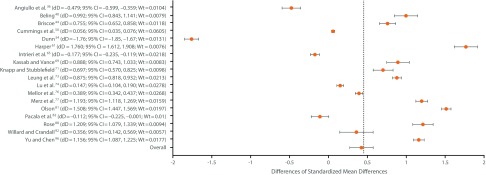
Meta-analyses of the overall effect of ageism interventions for all outcomes are shown in Table 1 and for primary outcomes in Figures 2 and 3. Ageism interventions demonstrated a strongly significant effect on attitudes (dD = 0.33; P < .001), knowledge (dD = 0.42; P < .001), and comfort (dD = 0.50; P < .001), but no significant effect on anxiety (dD = 0.13; P = .33) or working with older adults (dD = −0.09; P = 0.40).
TABLE 1—
Mixed Model Meta-Analyses of Ageism Interventions for Primary and Secondary Outcomes: Worldwide, 1976–2018
| No. of Participants |
||||
| Ageism Outcome | No. of Studies | Control Group | Intervention Group | Effect Size, dD (95% CI) |
| Attitudes toward aging | 53 | 2404 | 2783 | 0.33 (0.25, 0.42) |
| Knowledge on aging | 19 | 818 | 756 | 0.42 (0.27, 0.57) |
| Comfort with older adults | 9 | 286 | 348 | 0.50 (0.27, 0.57) |
| Anxiety about own aging | 5 | 217 | 267 | 0.13 (−0.13, 0.38) |
| Working with older adults | 6 | 388 | 375 | −0·09 (−0.30, 0.12) |
Note. CI = confidence interval; dD = differences of standardized mean differences.
FIGURE 2—
Examination of Overall Effect of Ageism Interventions on Primary Attitudes Outcome: Baseline to Posttreatment
Note. CI = confidence interval; dD = differences of standardized mean differences; wt = weight. In 2b, the 4 rightmost columns show, in order, dD for each study (which is dD), the lower confidence limit, the upper confidence limit, and the weight given to each study in the pooled analysis.
FIGURE 3—
Examination of Overall Effect of Ageism Interventions on Primary Knowledge Outcome: Baseline to Posttreatment
Note. CI = confidence interval; dD = differences of standardized mean differences; wt = weight. The 4 rightmost columns show, in order, dD for each study (which is dD), the lower confidence limit, the upper confidence limit, and the weight given to each study in the pooled analysis.
In the moderator analysis (Table B, available as a supplement to the online version of this article at http://www.ajph.org), each intervention type showed a strong effect on primary outcomes of attitudes (intergenerational-only: dD = 0.18; P = .026; education-only: dD = .34; P < .001; combined: dD = 0.43; P < .001) and knowledge (intergenerational-only: dD = 0.53; P = .005; education-only: dD = 0.41; P < .001; combined: dD = 0.36; P < .08). The combined and intergenerational contact–only intervention types demonstrated the strongest effects on the attitudes and knowledge outcomes, respectively. Gender was a significant moderating factor for attitudes (dD = 0.01; P = .009) and knowledge (dD = 0.01; P < .001), with interventions having a greater positive effect on females.
Ageism interventions had significant effects on both primary outcomes among high-school (attitudes: dD = 0.36; P < .001; knowledge: dD = 0.50; P < .027) and university-level (attitudes: dD = 0.39; P < .001; knowledge: dD = 0.42; P < .001) educational age groups. The relation between intervention dosage (number of weeks) and the attitudes outcome was positive but not significant (P = .09); intervention dosage was not related to knowledge (P = .69). There was no significant difference between ageism intervention studies using randomized controlled trials versus non–randomized controlled trial designs on the attitudes outcome. There were too few randomized controlled trials with data on the knowledge outcome to examine this effect. There was also no significant difference on primary outcomes between intervention studies from the United States versus non-US countries.
In general, studies included in this meta-analysis were found to be at high risk of bias according to the Cochrane Risk of Bias Tool (Table C and Figure B, available as supplements to the online version of this article at http://www.ajph.org). The majority of studies used a quasi-experimental design and, therefore, demonstrated shortcomings related to randomization, allocation concealment, and blinding of participants, personnel, and outcome assessors. Using the GRADE tool, we rated the quality of evidence supporting each outcome as low–moderate, largely downgraded because of the limitations in study design (Table D, available as a supplement to the online version of this article at http://www.ajph.org).
Although we would use a mixed model in the analysis regardless of the I2, the I2 values were 78.09 for attitudes and 81.11 for knowledge. The funnel plots for attitudes, knowledge, comfort, and anxiety outcomes showed no clustering of studies in the lower-right portion of the funnel that would indicate lack of publication of smaller or nonsignificant studies; the work outcome showed some evidence of bias (Figures C and D, available as supplements to the online version of this article at http://www.ajph.org).
DISCUSSION
Ageism, in the forms of stereotyping, prejudice, and discrimination toward people on the basis of age, has well-established negative effects on the physical and mental health of older people. However, global health strategies have not considered ageism as a modifiable risk factor. This situation is changing as the WHO has identified reducing ageism as a key target for improving human health.23 Although numerous interventions have addressed ageism, the overall effectiveness of such programs is unknown.24 To fill this knowledge gap, we completed the first meta-analysis, to our knowledge, of interventions designed to reduce ageism toward older people.
Our study provides a comprehensive systematic review and meta-analysis of available experimental and quasi-experimental ageism trials. In this meta-analysis, interventions significantly reduced levels of self-reported ageism among treatment participants versus controls. The size of these proportional reductions was broadly consistent across 3 intervention types, indicating that education, intergenerational contact, and combined programs provide broadly generalizable benefits. The data also suggest that interventions to reduce ageism are particularly effective among females and among adolescent and younger adult educational groups.
This study has several limitations. Given the nature of the available evidence, we were unable to rely primarily on randomized controlled studies. In the meta-analysis, 5 of the studies were randomized controlled trials and 58 employed quasi-experimental designs. Our approach was consistent with a general consensus in the field that inclusion of quasi-experimental studies is justified when more rigorous trials are lacking. As has been recommended,97 we excluded the weakest designs (including observational studies and single-group before-and-after studies) and only included studies that employed an analysis of a treatment and a comparison group with pre and post assessments on each group. The inclusion of non–randomized controlled trials that used comparison group designs is justified because it allows us to address outcomes from pragmatic implementations of ageism interventions that have not been sufficiently studied in randomized controlled trials.98 Our analysis comparing studies using randomized controlled trial versus non–randomized controlled trial designs found no significant differences on the primary outcome (attitudes) with enough studies to conduct such an analysis. However, findings reported in this article should be interpreted with caution because of the methodological limitations of the studies included. This observation points to the need for future studies to employ randomized controlled designs.
Our review also uncovered 2 important gaps in the ageism intervention literature. First, the majority of ageism intervention studies were from the United States, which may contribute to location bias; future research is necessary in other contexts throughout the world to understand whether the effect of certain interventions varies across different cultures and age-related social norms. Second, studies that examined the effect of ageism interventions among older adults themselves were lacking. Such research is critical given evidence of internalized ageism among older adults and their implicit preferences for younger adults.7
The most important implication of this meta-analysis, however, is the encouraging potential for interventions to reduce ageist stereotyping and prejudice. Furthermore, most of the interventions included in this review were small-scale, low-cost programs. Positive effects were found in intervention over comparison groups in most studies, and negative effects of interventions were rare. Interventions that included both educational and intergenerational contact components demonstrated particularly strong effects, especially for combating negative attitudes toward aging, suggesting that such combined programs should be a high priority for rigorous testing and dissemination. Furthermore, given that ageism constitutes a global crisis, interventions must be developed that are adapted for different national and cultural contexts. Our findings suggest that intervention research will lead to substantial progress in combating ageism and, in turn, improving the health and well-being of older people.
ACKNOWLEDGMENTS
This study was funded by the Bronfenbrenner Center for Translational Research at Cornell University and the Social Sciences and Humanities Research Council of Canada (435-2017-0578). K. P. acknowledges support from a Roybal Center Grant from the National Institute on Aging (P30AG022845).
We thank Vânia de la Fuente-Núñez and Alana Officer for overall guidance and coordination, and for developing the search strategy together with Kavita Kothari and Tomas Allen. We thank Gražina Rapolienė, Sarmite Mikulioniene, Justyna Stypinska, Joana Mendonça, and João Mariano for their assistance in the removal of completely irrelevant records. We also thank Cary Reid for assistance in manuscript review and feedback.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not needed because human participants were not involved.
Footnotes
See also Nelson, p. 1066.
REFERENCES
- 1.Officer A, Schneiders ML, Wu D, Nash P, Thiyagarajan JA, Beard JR. Valuing older people: time for a global campaign to combat ageism. Bull World Health Organ. 2016;94(10):710–710A. doi: 10.2471/BLT.16.184960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.North MS, Fiske ST. Modern attitudes toward older adults in the aging world: a cross-cultural meta-analysis. Psychol Bull. 2015;141(5):993–1021. doi: 10.1037/a0039469. [DOI] [PubMed] [Google Scholar]
- 3.Lamont RA, Swift HJ, Abrams D. A review and meta-analysis of age-based stereotype threat: negative stereotypes, not facts, do the damage. Psychol Aging. 2015;30(1):180–193. doi: 10.1037/a0038586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wurm S, Diehl M, Kornadt AE, Westerhof GJ, Wahl HW. How do views on aging affect health outcomes in adulthood and late life? Explanations for an established connection. Dev Rev. 2017;46:27–43. doi: 10.1016/j.dr.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meisner BA. A meta-analysis of positive and negative age stereotype priming effects on behavior among older adults. J Gerontol B Psychol Sci Soc Sci. 2012;67(1):13–17. doi: 10.1093/geronb/gbr062. [DOI] [PubMed] [Google Scholar]
- 6.Bryant C, Bei B, Gilson K, Komiti A, Jackson H, Judd F. The relationship between attitudes to aging and physical and mental health in older adults. Int Psychogeriatr. 2012;24(10):1674–1683. doi: 10.1017/S1041610212000774. [DOI] [PubMed] [Google Scholar]
- 7.Levy BR, Slade MD, Kunkel SR, Kasl SV. Longevity increased by positive self-perceptions of aging. J Pers Soc Psychol. 2002;83(2):261–270. doi: 10.1037//0022-3514.83.2.261. [DOI] [PubMed] [Google Scholar]
- 8.Wurm S, Benyamini Y. Optimism buffers the detrimental effect of negative self-perceptions of ageing on physical and mental health. Psychol Health. 2014;29(7):832–848. doi: 10.1080/08870446.2014.891737. [DOI] [PubMed] [Google Scholar]
- 9.Chrisler JC, Barney A, Palatino B. Ageism can be hazardous to women’s health: ageism, sexism, and stereotypes of older women in the healthcare system. J Soc Issues. 2016;72(1):86–104. [Google Scholar]
- 10.Briggs R, Robinson S, O’Neill D. Ageism and clinical research. Ir Med J. 2012;105(9):311–312. [PubMed] [Google Scholar]
- 11.Buttigieg SC, Ilinca S, de Sao Jose JM, Larsson AT. Researching ageism in health-care and long term care. In: Ayalon L, Tesch-Römer C, editors. Contemporary Perspectives on Ageism. Vol 19. Cham, Switzerland: Springer; 2018. pp. 493–515. [Google Scholar]
- 12.Higashi RT, Tillack AA, Steinman M, Harper M, Johnston CB. Elder care as “frustrating” and “boring”: understanding the persistence of negative attitudes toward older patients among physicians-in-training. J Aging Stud. 2012;26(4):476–483. doi: 10.1016/j.jaging.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 13.Herrera AP, Snipes SA, King DW, Torres-Vigil I, Goldberg DS, Weinberg AD. Disparate inclusion of older adults in clinical trials: priorities and opportunities for policy and practice change. Am J Public Health. 2010;100(suppl 1):S105–S112. doi: 10.2105/AJPH.2009.162982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bodner E, Palgi Y, Wyman MF. Ageism in mental health assessment and treatment of older adults. In: Ayalon L, Tesch-Römer C, editors. Contemporary Perspectives on Ageism. Vol 19. Cham, Switzerland: Springer; 2018. pp. 241–262. [Google Scholar]
- 15.Wyman MF, Shiovitz-Ezra S, Bengel J. Ageism in the health care system: providers, patients, and systems. In: Ayalon L, Tesch-Römer C, editors. Contemporary Perspectives on Ageism. Vol 19. Cham, Switzerland: Springer; 2018. pp. 193–212. [Google Scholar]
- 16.Wethington E, Pillemer K, Principi A. Research in social gerontology: social exclusion of aging adults. In: Riva P, Eck J, editors. Social Exclusion. Cham, Switzerland: Springer; 2016. pp. 177–195. [Google Scholar]
- 17.Allen JO. Ageism as a risk factor for chronic disease. Gerontologist. 2016;56(4):610–614. doi: 10.1093/geront/gnu158. [DOI] [PubMed] [Google Scholar]
- 18.Voss P, Bodner E, Rothermund K. Ageism: the relationship between age stereotypes and age discrimination. In: Ayalon L, Tesch-Römer C, editors. Contemporary Perspectives on Ageism. Vol 19. Cham, Switzerland: Springer; 2018. pp. 11–31. [Google Scholar]
- 19.Chávez EM, Calvo JM, Jones JA. Dental homes for older Americans: the Santa Fe group call for removal of the dental exclusion in Medicare. Am J Public Health. 2017;107(suppl 1):S41–S43. doi: 10.2105/AJPH.2017.303864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lloyd-Sherlock PG, Ebrahim S, McKee M, Prince MJ. Institutional ageism in global health policy. BMJ. 2016;354:i4514. doi: 10.1136/bmj.i4514. [DOI] [PubMed] [Google Scholar]
- 21.Northridge ME, Estrada I, Schrimshaw EW, Greenblatt AP, Metcalf SS, Kunzel C. Racial/ethnic minority older adults’ perspectives on proposed Medicaid reforms’ effects on dental care access. Am J Public Health. 2017;107(suppl 1):S65–S70. doi: 10.2105/AJPH.2016.303640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wolff JK, Warner LM, Ziegelmann JP, Wurm S. What do targeting positive views on ageing add to a physical activity intervention in older adults? Results from a randomised controlled trial. Psychol Health. 2014;29(8):915–932. doi: 10.1080/08870446.2014.896464. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization. World report on ageing and health. September 30, 2015. Available at: http://www.who.int/ageing/events/world-report-2015-launch/en. Accessed October 22, 2018.
- 24.Officer A, de la Fuente-Núñez V. A global campaign to combat ageism. Bull World Health Organ. 2018;96(4):295–296. doi: 10.2471/BLT.17.202424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chonody JM. Addressing ageism in students: a systematic review of the pedagogical intervention literature. Educ Gerontol. 2015;41(12):859–887. [Google Scholar]
- 26.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 27.Butler RN. Age-ism: another form of bigotry. Gerontologist. 1969;9(4):243–246. doi: 10.1093/geront/9.4_part_1.243. [DOI] [PubMed] [Google Scholar]
- 28.Eymard AS, Douglas DH. Ageism among health care providers and interventions to improve their attitudes toward older adults: an integrative review. J Gerontol Nurs. 2012;38(5):26–35. doi: 10.3928/00989134-20120307-09. [DOI] [PubMed] [Google Scholar]
- 29.São José JM, Amado CA, Ilinca S, Buttigieg SC, Taghizadeh Larsson A. Ageism in health care: a systematic review of operational definitions and inductive conceptualizations. Gerontologist. 2019;59(1):e98–e108. doi: 10.1093/geront/gnx020. [DOI] [PubMed] [Google Scholar]
- 30.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. Cochrane Collaboration. March 2011. Available at: http://handbook-5-1.cochrane.org. Accessed June 15, 2018. [Google Scholar]
- 31.Guyatt GH, Oxman AD, Vist GE et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Henderson CR., Jr Analysis of covariance in the mixed model: higher-level, nonhomogeneous, and random regressions. Biometrics. 1982;38(3):623–640. [PubMed] [Google Scholar]
- 33.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aday RH, McDuffie W, Sims CR. Impact of an intergenerational program on Black adolescents’ attitudes toward the elderly. Educ Gerontol. 1993;19(7):663–673. [Google Scholar]
- 35.Anderson KR. Ageism: The Effect of the Gerontological Education, Self-Attribution Information and the Intergenerational Contact on Attitudes of Adolescents Toward the Elderly [dissertation] San Diego, CA: California School of Professional Psychology; 1980. [Google Scholar]
- 36.Angiullo L, Whitbourne SK, Powers C. The effects of instruction and experience on college students’ attitudes toward the elderly. Educ Gerontol. 1996;22(5):483–495. [Google Scholar]
- 37.Babcock RL, MaloneBeach EE, Woodworth-Hou B. Intergenerational intervention to mitigate children’s bias against the elderly. J Intergener Relatsh. 2016;14(4):274–287. [Google Scholar]
- 38.Baggett S. Attitudinal consequences of older adult volunteers in the public school setting. Educ Gerontol. 1981;7(1):21–31. [Google Scholar]
- 39.Belgrave M. The effect of a music therapy intergenerational program on children and older adults’ intergenerational interactions, cross-age attitudes, and older adults’ psychosocial well-being. J Music Ther. 2011;48(4):486–508. doi: 10.1093/jmt/48.4.486. [DOI] [PubMed] [Google Scholar]
- 40.Beling J. Effect of service-learning on knowledge about older people and faculty teaching evaluations in a physical therapy class. Gerontol Geriatr Educ. 2003;24(1):31–46. doi: 10.1300/J021v24n01_03. [DOI] [PubMed] [Google Scholar]
- 41.Bernard MA, McAuley WJ, Belzer JA, Neal KS. An evaluation of a low‐intensity intervention to introduce medical students to healthy older people. J Am Geriatr Soc. 2003;51(3):419–423. doi: 10.1046/j.1532-5415.2003.51119.x. [DOI] [PubMed] [Google Scholar]
- 42.Bloom RL. The Effect of Type of Psychosocial Training on Nursing Staff Empathy and Attitudes Towards Geriatric Residents [dissertation] San Diego, CA: California School of Professional Psychology; 1994. [Google Scholar]
- 43.Blunk EM, Williams SW. The effects of curriculum on preschool children’s perceptions of the elderly. Educ Gerontol. 1997;23(3):233–241. [Google Scholar]
- 44.Briscoe VJ. The Effects of Gerontology Nursing Teaching Methods on Nursing Student Knowledge, Attitudes, and Desire to Work With Older Adult Clients [dissertation] Minneapolis, MN: Walden University; 2004. [Google Scholar]
- 45.Brown DS, Gardner DL, Perritt L, Kelly DG. Improvement in attitudes toward the elderly following traditional and geriatric mock clinics for physical therapy students. Phys Ther. 1992;72(4):251–257. doi: 10.1093/ptj/72.4.251. [DOI] [PubMed] [Google Scholar]
- 46.Carter D. An investigation into the efficacy of cross-generational classroom interactions in promoting attitudinal change in children and youth. Educ Psychol. 2001;21(4):431–442. [Google Scholar]
- 47.Chase CA. An intergenerational e-mail pal project on attitudes of college students toward older adults. Educ Gerontol. 2010;37(1):27–37. [Google Scholar]
- 48.Chen S, Walsh SM. Effect of a creative‐bonding intervention on Taiwanese nursing students’ self‐transcendence and attitudes toward elders. Res Nurs Health. 2009;32(2):204–216. doi: 10.1002/nur.20310. [DOI] [PubMed] [Google Scholar]
- 49.Chua PH, Jung Y, Lwin MO, Theng YL. Let’s play together: effects of video-game play on intergenerational perceptions among youth and elderly participants. Comput Human Behav. 2013;29(6):2303–2311. [Google Scholar]
- 50.Cummings SM, Williams MM, Ellis RA. Impact of an intergenerational program on 4th graders’ attitudes toward elders and school behaviors. J Hum Behav Soc Environ. 2002;6(3):91–107. [Google Scholar]
- 51.Cummings SM, Cassie KM, Galambos C, Wilson E. Impact of an infusion model on social work students’ aging knowledge, attitudes, and interests. J Gerontol Soc Work. 2006;47(3-4):173–186. doi: 10.1300/J083v47n03_11. [DOI] [PubMed] [Google Scholar]
- 52.Dorfman LT, Murty S, Ingram JG, Evans RJ. Incorporating intergenerational service-learning into an introductory gerontology course. J Gerontol Soc Work. 2003;39(1-2):219–240. [Google Scholar]
- 53.Downe‐Wamboldt BL, Melanson PM. Attitudes of baccalaureate student nurses toward aging and the aged: results of a longitudinal study. Educ Gerontol. 1990;16(1):49–59. [Google Scholar]
- 54.Dunn S. Effects of a Simulation Game on Trainees’ Knowledge and Attitudes About Age-Related Changes in Learning and Work Behaviors of Older Workers [dissertation] Denton, TX: University of North Texas; 2000. [Google Scholar]
- 55.Dye CA. Attitude change among health professionals: implications for gerontological nursing. J Gerontol Nurs. 1979;5(5):31–35. doi: 10.3928/0098-9134-19790901-10. [DOI] [PubMed] [Google Scholar]
- 56.Fruhauf CA, Jarrott SE, Lambert-Shute JJ. Service-learners at dementia care programs: an intervention for improving contact, comfort, and attitudes. Gerontol Geriatr Educ. 2004;25(1):37–52. doi: 10.1300/J021v25n01_03. [DOI] [PubMed] [Google Scholar]
- 57.Gilbert MA. Effects of Exposure to Well-Elderly on Children’s Negative Stereotypic Attitudes [dissertation] Hempstead, NY: Hofstra University; 1999. [Google Scholar]
- 58.Glass JC, Jr, Trent C. Changing ninth-graders’ attitudes toward older persons: possibility and persistence through education. Res Aging. 1980;2(4):499–512. [Google Scholar]
- 59.Gonzales E, Morrow-Howell N, Gilbert P. Changing medical students’ attitudes toward older adults. Gerontol Geriatr Educ. 2010;31(3):220–234. doi: 10.1080/02701960.2010.503128. [DOI] [PubMed] [Google Scholar]
- 60.Hannon PO, Gueldner SH. The impact of short-term quality intergenerational contact on children’s attitudes toward older adults. J Intergener Relatsh. 2008;5(4):59–76. [Google Scholar]
- 61.Harper SP. Instructional Design for Affective Learning in Online Nursing Education [dissertation] Minneapolis, MN: Capella University; 2007. [Google Scholar]
- 62.Hastings KL. The Effect of Participation in an Intergenerational Program on Preschool Children’s Attitudes Toward the Elderly [dissertation] Denton, TX: Texas Woman’s University; 1992. [Google Scholar]
- 63.Heller BR, Walsh FJ. Changing nursing students’ attitudes toward the aged: an experimental study. J Nurs Educ. 1976;15(1):9–17. [PubMed] [Google Scholar]
- 64.Holtzman JM, Beck JD, Hodgetts PG, Coggan PG, Ryan N. Geriatrics program for medical students and family practice residents. I. Establishing attitudes toward the aged. J Am Geriatr Soc. 1977;25(11):521–524. doi: 10.1111/j.1532-5415.1977.tb00832.x. [DOI] [PubMed] [Google Scholar]
- 65.Intrieri RC, Kelly JA, Brown MM, Castilla C. Improving medical students’ attitudes toward and skills with the elderly. Gerontologist. 1993;33(3):373–378. doi: 10.1093/geront/33.3.373. [DOI] [PubMed] [Google Scholar]
- 66.Jansen DA, Morse WA. Positively influencing student nurse attitudes toward caring for elders. Gerontol Geriatr Educ. 2004;25(2):1–14. doi: 10.1300/J021v25n02_01. [DOI] [PubMed] [Google Scholar]
- 67.Kaf WA, Barboa LS, Fisher BJ, Snavely LA. Effect of interdisciplinary service learning experience for audiology and speech-language pathology students working with adults with dementia. Am J Audiol. 2011;20(2):S241–S249. doi: 10.1044/1059-0889(2011/10-0025). [DOI] [PubMed] [Google Scholar]
- 68.Kamenir CL. A classroom experience to improve young children’s views of the elderly. Gerontol Geriatr Educ. 1983;4(1):97–109. doi: 10.1300/J021v04n01_15. [DOI] [PubMed] [Google Scholar]
- 69.Kassab C, Vance L. An assessment of the effectiveness of an intergenerational program for youth. Psychol Rep. 1999;84(1):198–200. doi: 10.2466/pr0.1999.84.1.198. [DOI] [PubMed] [Google Scholar]
- 70.Klein DA, Council KJ, McGuire SL. Education to promote positive attitudes about aging. Educ Gerontol. 2005;31(8):591–601. [Google Scholar]
- 71.Knapp JL, Stubblefield P. Changing students’ perceptions of aging: The impact of an intergenerational service learning course. Educ Gerontol. 2000;26(7):611–621. [Google Scholar]
- 72.LeBlanc PA. Attitudes of Nursing Students Toward the Elderly as Influenced by Lecture-Discussion With and Without Simulation [dissertation] Hattiesburg, MS: University of Southern Mississippi; 1995. [Google Scholar]
- 73.Leung AY, Chan SS, Kwan CW, Cheung MK, Leung SS, Fong DY. Service learning in medical and nursing training: a randomized controlled trial. Adv Health Sci Educ Theory Pract. 2012;17(4):529–545. doi: 10.1007/s10459-011-9329-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lu WH, Hoffman KG, Hosokawa MC, Gray MP, Zweig SC. First year medical students’ knowledge, attitudes, and interest in geriatric medicine. Educ Gerontol. 2010;36(8):687–701. [Google Scholar]
- 75.Lytle A, Levy SR, Meeks S. Reducing ageism: education about aging and extended contact with older adults. Gerontologist. 2019;59(3):580–588. doi: 10.1093/geront/gnx177. [DOI] [PubMed] [Google Scholar]
- 76.Mellor D, McCabe M, Rizzuto L, Gruner A. Respecting our elders: evaluation of an educational program for adolescent students to promote respect toward older adults. Am J Orthopsychiatry. 2015;85(2):181–190. doi: 10.1037/ort0000041. [DOI] [PubMed] [Google Scholar]
- 77.Merz CC, Stark SL, Morrow-Howell NL, Carpenter BD. When I’m 64: effects of an interdisciplinary gerontology course on first-year undergraduates’ perceptions of aging. Gerontol Geriatr Educ. 2018;39(1):35–45. doi: 10.1080/02701960.2016.1144600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Meshel DS, McGlynn RP. Intergenerational contact, attitudes, and stereotypes of adolescents and older people. Educ Gerontol. 2004;30(6):457–479. [Google Scholar]
- 79.Mount J. Effects of a practicum with well elderly on physical therapy students’ attitudes towards older people and their intention to work with the elderly. Gerontol Geriatr Educ. 1993;13(4):13–24. [Google Scholar]
- 80.Murphy‐Russell S, Die AH, Walker JL., Jr Changing attitudes toward the elderly: the impact of three methods of attitude change. Educ Gerontol. 1986;12(3):241–251. [Google Scholar]
- 81.Olson CJ. A curriculum module enhances students’ gerontological practice-related knowledge and attitudes. J Gerontol Soc Work. 2003;38(4):85–102. [Google Scholar]
- 82.Pacala JT, Boult C, Bland C, O’Brien J. Aging game improves medical students’ attitudes toward caring for elders. Gerontol Geriatr Educ. 1995;15(4):45–57. [Google Scholar]
- 83.Pilkington WJ. Effects of a Communication Program on Nursing Home Staff’s Attitudes and Communication Skills and Residents’ Levels of Life Satisfaction [dissertation] New York, NY: St John’s University; 1995. [Google Scholar]
- 84.Wenzel MPS, Rensen SS. Changes in attitudes among children and elderly adults in intergenerational group work. Educ Gerontol. 2000;26(6):523–540. [Google Scholar]
- 85.Proller NL. The effects of an adoptive grandparent program on youth and elderly participants. J Child Contemp Soc. 1989;20(3-4):195–203. [Google Scholar]
- 86.Ragan AM, Bowen AM. Improving attitudes regarding the elderly population: the effects of information and reinforcement for change. Gerontologist. 2001;41(4):511–515. doi: 10.1093/geront/41.4.511. [DOI] [PubMed] [Google Scholar]
- 87.Rich PE, Myrick RD, Campbell C. Changing children’s perceptions of the elderly. Educ Gerontol. 1983;9(5-6):483–491. [Google Scholar]
- 88.Rose MA. The importance of influencing nursing students’ attitudes toward older adults. Public Health Nurs. 1984;1(3):152–157. doi: 10.1111/j.1525-1446.1984.tb00444.x. [DOI] [PubMed] [Google Scholar]
- 89.Slotnick HB, Reichelt CR, Gardner R., Jr Gifted students meet the institutionalized elderly: learning about aging and the aged in a rural nursing home. J Educ Gift. 1985;9(1):45–58. [Google Scholar]
- 90.Snyder JR. The influence of instruction on college students’ attitudes toward older adults. Gerontol Geriatr Educ. 2005;26(2):69–79. doi: 10.1300/j021v26n02_05. [DOI] [PubMed] [Google Scholar]
- 91.Trent C, Glass JC, Crockett J. Changing adolescent 4-H club members’ attitudes toward the aged. Educ Gerontol. 1979;4(1):33–48. [Google Scholar]
- 92.Willard M, Crandall J. Intergenerational service-learning to combat ageism in exercise science students. Kentucky Association of Health, Physical Education, Recreation and Dance. 2016;53(2):55–67. [Google Scholar]
- 93.Xaverius PK, Mathews RM. Evaluating the impact of intergenerational activities on elders’ engagement and expressiveness levels in two settings. J Intergener Relatsh. 2004;1(4):53–69. [Google Scholar]
- 94.Yamashita T, Hahn SJ, Kinney JM, Poon LW. Impact of life stories on college students’ positive and negative attitudes toward older adults. Gerontol Geriatr Educ. 2018;39(3):326–340. doi: 10.1080/02701960.2017.1311884. [DOI] [PubMed] [Google Scholar]
- 95.Lee YS, Shin SH, Greiner PA. Can education change attitudes toward aging? A quasi-experimental design with a comparison group. J Nurs Educ Pract. 2015;5(9):90–99. [Google Scholar]
- 96.Yu CY, Chen KM. Experiencing simulated aging improves knowledge of and attitudes toward aging. J Am Geriatr Soc. 2012;60(5):957–961. doi: 10.1111/j.1532-5415.2012.03950.x. [DOI] [PubMed] [Google Scholar]
- 97.Higgins JP, Ramsay C, Reeves BC et al. Issues relating to study design and risk of bias when including non‐randomized studies in systematic reviews on the effects of interventions. Res Synth Methods. 2013;4(1):12–25. doi: 10.1002/jrsm.1056. [DOI] [PubMed] [Google Scholar]
- 98.Valentine JC, Thompson SG. Issues relating to confounding and meta‐analysis when including non‐randomized studies in systematic reviews on the effects of interventions. Res Synth Methods. 2013;4(1):26–35. doi: 10.1002/jrsm.1064. [DOI] [PubMed] [Google Scholar]