Abstract
Objectives. To examine associations of county-level demographic, socioeconomic, and labor market characteristics on overall drug mortality rates and specific classes of opioid mortality.
Methods. We used National Vital Statistics System mortality data (2002–2004 and 2014–2016) and county-level US Census data. We examined associations between several census variables and drug deaths for 2014 to 2016. We then identified specific classes of counties characterized by different levels and rates of growth in mortality from specific opioid types between 2002 to 2004 and 2014 to 2016. We ran multivariate and multivariable regression models to predict probabilities of membership in each “opioid mortality class” on the basis of county-level census measures.
Results. Drug mortality rates overall are higher in counties characterized by more economic disadvantage, more blue-collar and service employment, and higher opioid-prescribing rates. High rates of prescription opioid overdoses and overdoses involving both prescription and synthetic opioids cluster in more economically disadvantaged counties with larger concentrations of service industry workers. High heroin and “syndemic” opioid mortality counties (high rates across all major opioid types) are more urban, have larger concentrations of professional workers, and are less economically disadvantaged. Syndemic opioid counties also have greater concentrations of blue-collar workers.
Conclusions. Census data are essential tools for understanding the importance of place-level characteristics on opioid mortality.
Public Health Implications. National opioid policy strategies cannot be assumed universally applicable. In addition to national policies to combat the opioid and larger drug crises, emphasis should be on developing locally and regionally tailored interventions, with attention to place-based structural economic and social characteristics.
Fatal drug overdose rates increased 250% in the United States from 6.1 deaths per 100 000 population in 1999 to 21.7 in 2017.1 Opioids have been the primary contributor to this increase, accounting for more than 47 600 deaths in 2017 alone.1 There is widespread geographic variation in fatal opioid overdose rates, with the highest rates concentrated in Appalachia, New England, Florida, eastern Oklahoma, and the desert Southwest.2–5 In state-level analyses, prescription opioids, heroin, and fentanyl have been found to be differentially implicated in overdoses across different parts of the United States. For example, synthetic opioid deaths are strongly concentrated throughout the East,6 whereas heroin overdoses are high in the Industrial Midwest and New Mexico.7
Our analysis of county-level variation in opioid mortality is grounded in literature emphasizing the importance of ecological factors on population health and reflects and embraces counties as important population health units of analysis.8 Counties are small enough to reflect local economic and social conditions but large enough to be meaningful for policy.9 County governments provide political and economic structure, which ultimately affects health and well-being. Moreover, the county is where most social and health services are delivered and where states administer funding for most social programs.9 Counties are also largely responsible for bearing the costs of the drug crisis in the form of criminal justice, social services, and emergency service provider expenditures.
Census data can be an essential tool for understanding county-level variation in drug mortality rates and in driving policy responses to the crisis. Multiple previous studies have used census data to understand the roles of demographic, socioeconomic, and labor market conditions on county-level variation in life expectancy,8 all-cause mortality,10–13 premature mortality,14,15 and cause-specific mortality from cardiovascular diseases,16 cancers,16 chronic obstructive pulmonary disease,16 diabetes,17 and unintentional injury.18 Using county-level census data, Monnat2 found that drug mortality rates varied across different types of labor markets and were higher in counties characterized by greater economic disadvantage. However, Monnat pooled 10 years of mortality data and did not examine how county characteristics were differentially associated with different classes of opioid mortality. Because previous research has primarily used an omnibus measure of drug mortality deaths, there is limited information about the ecological correlates of mortality linked to different types of opioids.
We extended previous research on geographic differences in opioid mortality by (1) describing the county-level demographic, economic, and labor market characteristics that are associated with overall drug mortality rates in 2014 to 2016 and (2) analyzing how these characteristics vary across “opioid mortality classes”—classes of counties characterized by differential levels and rates of growth in mortality from specific types of opioids. Our analyses were grounded in research showing the importance of various drug supply19 and structural demand factors in driving the opioid overdose crisis, including population aging, economic distress, and employment restructuring.4,20 In this structural approach to explaining the opioid crisis, we focused especially on economic dislocation and place-level distress among the working class.21
METHODS
Mortality data came from the restricted-use death certificate files from the National Vital Statistics System, 2002 to 2004 and 2014 to 2016. These data identify causes of death and county of residence from all death certificates filed in the United States. We categorized drug deaths on the basis of International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (Geneva, Switzerland: World Health Organization; 2011 [ICD-10]) codes, as any death that included an underlying cause of accidental poisoning, intentional poisoning, poisoning of undetermined intent by exposure to drugs, assault by drugs, drug-induced diseases, finding of drugs in the blood, and mental or behavioral disorders attributable to drugs. See Appendix A (available as a supplement to the online version of this article at http://www.ajph.org) for ICD-10 codes. We identified opioid deaths as those with an underlying cause reflecting drug poisoning along with any multiple cause of death opioid-specific code (T40.0–T40.4, T40.6) or any mental and behavioral disorder attributable to opioids (F11.0–F11.9).
We calculated separate rates for heroin, prescription opioids, synthetic opioids, and multiple cause (those that included 2 or more opioids). Because opioid deaths are known to be underreported on death certificates, with substantial geographic variation in underreporting,7 we calculated a fifth measure for all drug overdoses minus those that involved an opioid. To smooth potentially large fluctuations from small changes in deaths in small population counties, we pooled deaths across 3-year periods.22 Consistent with Centers for Disease Control and Prevention (CDC) methods, we then calculated age-adjusted rates with the direct method using the 2000 US standard population.
County-level demographic, socioeconomic, and labor market measures came from the 2008 to 2012 American Community Survey (ACS) and 2000 US Census. All census variables in the analysis are listed in Table 1. Using 2000 and 2008 to 2012 measures reduces risk of reverse causality bias and allows a lagged relationship between county-level conditions and mortality.
TABLE 1—
Descriptive Information and Coefficients From Minimally Adjusted Negative Binomial Regressions of County-Level Drug Deaths (2014–2016) on County Census Characteristics (2008–2012): United States
| Mean (SD) | IDR (95% CI) | |
| Population characteristics | ||
| Non-Hispanic White, % | 78.58 (19.52) | 1.11 (1.07, 1.16) |
| Non-Hispanic Black, % | 8.85 (14.48) | 0.85 (0.82, 0.88) |
| Hispanic, % | 8.35 (13.36) | 0.97 (0.93, 1.00) |
| Aged ≥ 65 y, % | 16.11 (4.21) | 1.05 (1.01, 1.09) |
| Veterans, % | 10.99 (2.76) | 1.03 (0.99, 1.06) |
| Moved into county in last 5 y, %a | 32.42 (14.20) | 0.92 (0.89, 0.94) |
| Population densitya | 3.78 (1.69) | 1.14 (1.10, 1.18) |
| Nonmetropolitan, 2013b | 62.90 | 1.01 (0.94, 1.07) |
| Socioeconomic characteristics | ||
| Not working (unemployed or not in labor force), %b | 56.36 (6.24) | 1.20 (1.15, 1.24) |
| No 4-y college degree, % | 80.64 (8.63) | 1.16 (1.13, 1.20) |
| Ratio of federal to county median household income, % | 124.14 (31.41) | 1.11 (1.07, 1.14) |
| Poverty, % | 16.33 (6.39) | 1.13 (1.09, 1.17) |
| Public assistance receipt, % | 0.97 (0.64) | 1.19 (1.15, 1.23) |
| Thiel’s L (inequality at bottom of income distribution) | 0.32 (0.06) | 1.02 (0.99, 1.106) |
| Gini coefficient of income inequality | 0.43 (0.03) | 1.04 (1.01, 1.08) |
| Separated or divorced, % | 13.35 (2.70) | 1.22 (1.18, 1.26) |
| Single-parent families, % | 31.5 (9.17) | 1.15 (1.11, 1.19) |
| Vacant housing units, % | 17.58 (10.31) | 1.07 (1.03, 1.11) |
| Renter-occupied housing units, % | 22.57 (7.35) | 1.00 (0.96, 1.03) |
| Occupational composition | ||
| Administrative and clerical, % | 13.02 (2.10) | 1.02 (0.99, 1.05) |
| Executive and managerial, % | 10.02 (3.37) | 0.94 (0.91, 0.97) |
| Farming, fishing, forestry, %a | 4.84 (5.85) | 0.85 (0.81, 0.88) |
| Personal services, % | 15.21 (3.32) | 1.09 (1.06, 1.13) |
| Production, extraction, construction, % | 19.17 (5.28) | 1.02 (0.99, 1.06) |
| Professional and technical, % | 20.55 (4.07) | 0.99 (0.96, 1.02) |
| Retail sales, % | 9.58 (2.29) | 1.00 (0.97, 1.04) |
| Transportation and material moving, % | 7.61 (2.45) | 1.02 (0.99, 1.05) |
| Industry composition | ||
| Agriculture, fishing, forestry, % a | 5.31 (6.41) | 0.84 (0.81, 0.88) |
| Business and professional, % | 6.48 (3.13) | 0.95 (0.92, 0.99) |
| Construction, % | 7.51 (2.42) | 0.99 (0.96, 1.02) |
| Communication, information, utilities, % a | 2.75 (1.28) | 1.00 (0.96, 1.03) |
| Finance, insurance, real estate, % | 4.72 (1.96) | 0.95 (0.92, 0.98) |
| Education, % | 9.43 (3.29) | 0.99 (0.96, 1.02) |
| Health, % | 13.46 (3.32) | 1.09 (1.06, 1.13) |
| Retail, personal services, food, accommodations, % | 24.04 (4.64) | 1.05 (1.02, 1.09) |
| Mining, % | 1.65 (3.70) | 1.09 (1.05, 1.13) |
| Manufacturing, % | 12.24 (6.93) | 0.94 (0.91, 0.97) |
| Public administration, % | 5.73 (3.22) | 1.06 (1.03, 1.09) |
| Transportation, % | 4.20 (1.71) | 1.00 (0.97, 1.03) |
| Wholesale trade, % | 2.48 (1.19) | 0.96 (0.93, 0.99) |
| Opioid prescribingb | ||
| Retail opioid prescribing per 100 population, 2006–2008 | 82.51 (40.88) | 1.19 (1.16, 1.23) |
| Retail opioid prescribing per 100 population, 2009–2011 | 89.45 (44.31) | 1.20 (1.17, 1.23) |
| Retail opioid prescribing per 100 population, 2012–2014 | 89.33 (42.78) | 1.22 (1.19, 1.26) |
| Retail opioid prescribing per 100 population, 2015–2016 | 75.84 (40.69) | 1.23 (1.20, 1.27) |
Note. CI = confidence interval; IDR = incidence density ratio. n = 3079. All variables come from the 2008–2012 American Community Survey (ACS) 5-y estimates unless otherwise indicated. All variables are standardized at a mean of 0 and SD of 1, except nonmetropolitan, which is a binary variable. The regressions model death counts (offset by the log of the county population size) using multilevel (random intercept) negative binomial models (counties nested in states). All models are adjusted for county percentage aged ≥ 65 years, percentage non-Hispanic White, and population density. Models for percentage non-Hispanic Black and percentage Hispanic control only for percentage aged ≥ 65 y and population density. Sensitivity models using variables from the 2000 Census and 2012–2016 ACS are presented in Appendix E. Results were relatively unaffected by using data from these alternative years.
Because of nonnormality, this variable was logged for regression analysis.
Metro status, labor force participation rate, and opioid prescribing are not from the ACS.
Metropolitan status came from the US Department of Agriculture Economic Research Service’s Rural-Urban Continuum Codes, 2013. We collapsed the codes to create a binary indicator in which categories 1 to 3 indicated a metropolitan county and 4 to 9 indicated a nonmetropolitan county.
To account for opioid supply, we included county-level retail opioid prescribing from the CDC.23 These data report retail opioid prescriptions dispensed per 100 persons. A limitation is that they excluded prescriptions from high-volume prescribing pain clinics (i.e., “pill mills”). Prescribing information was missing for between 6% and 13% of counties, depending on year. We imputed average missing prescribing values using a Markov chain Monte Carlo model with 500 imputations.24 We used the average prescribing rate for 2009 to 2011 to capture years of peak prescribing, but we tested alternate models with prescribing rates for 2006 to 2008 and 2012 to 2014. Findings were relatively unaffected by these substitutions (Appendix G, available as a supplement to the online version of this article at http://www.ajph.org). County-level prescribing data before 2006 are not available.
Our analyses included 3079 US counties. We restricted analyses to the 48 conterminous states and Washington, DC. We merged Broomfield County, Colorado, (created in 2003) and 29 independent cities in Virginia with populations of less than 65 000 people into their respective counties. This reduced the potential for ACS measurement error.
We used multilevel negative binomial regression (random intercepts to account for nesting of counties in states) to model overall drug mortality counts for 2014 to 2016, offset by the log of the county population, as a function of county-level census characteristics. We standardized all variables before including them in regression models, enabling comparison of the relative strength of associations across different factors. We adjusted each model for county racial and age composition and population density. We did not attempt to determine the mechanisms through which these factors are associated with drug mortality. We simply aimed to show the relative importance of several census variables for understanding county-level differences in drug mortality.
Then, we identified opioid-specific mortality classes using latent profile analysis (LPA). LPA is appropriate for this study for several reasons.25 First, we wanted counties to be represented in higher dimensional space (e.g., classes), and multidimensional scaling is usually limited to 2 dimensions or 2 classes. Second, we did not know the number of clusters a priori. LPA permitted us to identify the correct number of clusters on the basis of statistical tests instead of subjective criteria, as with hierarchical cluster analysis. Third, LPA permits posterior estimates of the probability of correct classification, allowing us to drop poorly fitted cases from classes.
We used LPA to create county classifications on the basis of age-adjusted opioid mortality rates for 2014 to 2016 and the change in rates between 2002 to 2004 and 2014 to 2016 using the opioid-specific mortality rates described (e.g., prescription opioids, heroin, synthetic, multiple), including rates for drug overdose deaths that did not specify an opioid on the death certificate.
We chose 2002 to 2004 as the base period because it captures the first wave of the opioid overdose crisis.20 Moreover, using 2002 to 2004 instead of 1999 to 2001 (the first years for which data are available with ICD-10 codes) reduces endogeneity with our 2000 Census covariates. We chose 2014 to 2016 as the ending point, as this was the most current restricted mortality data available from the CDC at the time of analysis.
We normalized mortality rates using z-scores to remove scale differences and allow comparisons across classes. To minimize extreme scores that can result in classes with few cases, we Winsorized scores at the 0.5 and 99.5 percentiles, roughly corresponding to ±2.6 SD. We found evidence for 6 classes on the basis of fit indices and examination of latent class means (Appendix B, available as a supplement to the online version of this article at http://www.ajph.org).26,27
We compared the means of county-level census measures across the different opioid classes. We then modeled the probability of membership in each of the opioid classes as a function of the county-level covariates using multinomial logistic regression. Because there are strong correlations between several census variables, they are ideal for generating indices that capture latent constructs. We used exploratory factor analysis to identify which of the 34 census variables grouped together. Eigenvalues indicated that the first 4 factors, representing 27 of the census variables, collectively explained 70% of the variance. We created 4 factor-weighted indices that combined the variables loading highly (≥ 0.40) onto their respective factors. We standardized all factors (mean = 0; SD = 1). The variables included in each factor are presented in Appendix D (available as a supplement to the online version of this article at http://www.ajph.org). The first index, urban professional (α = 0.86), reflects high-growth urban counties with a large white-collar presence. The second index measures economic disadvantage (α = 0.90). The third index, blue-collar presence (α = 0.84), reflects a large presence of working-class and manual laborers. Service economy (α = 0.65) represents the final index. Maps showing the geographic distribution of these indices are presented in Appendix D.
Multinomial logistic regression models simultaneously included our 4 indices and controlled for racial/ethnic and age composition, opioid prescribing, and metropolitan status. Models adjusted SEs for the clustering of counties in states and were weighted by the probability of LPA class membership.
We used SAS version 9.4 (SAS Institute, Cary, NC) for descriptive statistics, Mplus version 7 (Muthen & Muthen, Los Angeles, CA) and SAS version 9.4 for latent class analysis, and StataMP version 15 (StataCorp LP, College Station, TX) for regression analysis.
RESULTS
A map of county-level drug mortality rates for 2014 to 2016 is shown in Appendix C (available as a supplement to the online version of this article at http://www.ajph.org). High rates are concentrated throughout New England, Central Appalachia, parts of the Industrial Midwest, eastern Oklahoma, and the desert Southwest. Low rates are observed throughout the Southern Black Belt, Texas, and the Northern Great Plains.
Regression models revealed that several demographic, socioeconomic, and labor market characteristics are associated with drug mortality rates (Table 1). Each of the economic disadvantage indicators and percentages of workers in various service occupations and industries are associated with significantly higher drug mortality rates. Higher shares of new residents; workers employed in executive or managerial and farming, fishing, or forestry occupations; and workers employed in agriculture, fishing, forestry, business or professional, finance, insurance, and real estate, manufacturing, and wholesale trade industries are associated with significantly lower drug mortality rates. Counties with higher opioid-prescribing rates have significantly higher drug mortality rates. Sensitivity models showing regression results using the 2000 Census and 2012 to 2016 ACS are presented in Appendix E (available as a supplement to the online version of this article at http://www.ajph.org).
Turning to the LPA results (Appendix B), most counties (1701; 55%) are in the low opioid overdose class. These counties have comparatively low mortality rates and change between 2002 to 2004 and 2014 to 2016 from each of the specific opioid types. The LPA classified 270 counties (8.8%) into the high prescription opioid class, characterized by above average rates of prescription opioid mortality in 2014 to 2016 and rates of growth since 2002 to 2004. The high heroin class (n = 165; 5.4%) is characterized by sharply rising heroin mortality rates between 2002 to 2004 and 2014 to 2016, with rates in 2014 to 2016 the highest in the nation. The emerging heroin class (n = 447; 14.5%) incorporates counties with slightly lower and slower-growing heroin mortality rates than the high heroin class, but the average heroin mortality rate in the emerging class still outpaced most other classes.
There were 2 classes that involved high rates of fatal overdose from multiple opioid drugs. First, counties in the synthetic+ class (n = 211; 6.9%) have above average and fast-growing mortality rates from synthetic opioids alone or in combination with prescription opioids and, to a lesser extent, heroin. Counties in the final class (n = 129; 4.2%) are in the depths of the opioid crisis, having very high and rapidly growing mortality rates from all types of opioids: heroin, prescription, synthetic, and combinations. We termed this class the syndemic opioid class because it reflects an aggregation of multiple concurrent or sequential epidemics, wherein the combination of high death rates from multiple opioids greatly exacerbates the crisis.28 The remaining 156 counties (5.1%) were unclassified.
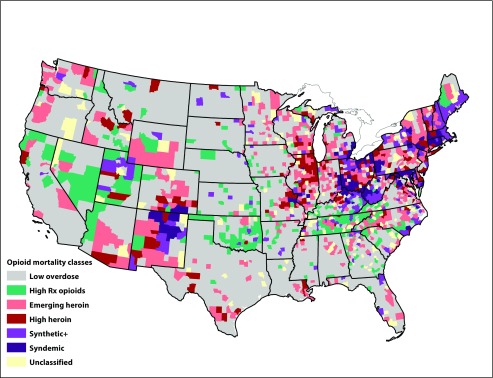
The geographic distribution of opioid classes is shown in Figure 1, with maps showing levels of mortality and rates of growth for specific opioids in Appendix B. The overlap between these maps gives us confidence that our LPA accurately classified counties. The patterns are also consistent with those in a recent study of state-level growth and levels of mortality from specific opioids6 and with the map of overall drug mortality rates shown in Appendix C. High prescription opioid counties are concentrated in southern Appalachia, eastern Oklahoma, parts of the desert Southwest and Mountain West, and sprinkled throughout the Great Plains. High and emerging heroin counties are concentrated throughout parts of New York, the Industrial Midwest, central North Carolina, and the Southwest and Northwest. The synthetic+ and syndemic classes are concentrated throughout New England, central Appalachia, and central New Mexico.
FIGURE 1—
The Geographic Distribution of Opioid Mortality Classes by County: United States
Note. Classes are derived from absolute mortality rates in 2014–2016 and the change in rates between 2002–2004 and 2014–2016. Counties in the synthetic+ class have above average and fast-growing mortality rates from synthetic opioids alone or in combination with prescription opioids and, to a lesser extent, heroin.
Mean overall drug and opioid-specific mortality rates and means of all county characteristics by opioid class are shown in Appendix F. Overall drug mortality and opioid-specific mortality rates in 2014 to 2016 were highest in the syndemic class (41.3 overall drug and 31.7 opioid deaths per 100 000 population), followed by synthetic+ (30.3, 20.9), high prescription opioid (27.3, 16.9), high heroin (25.1, 16.7), emerging heroin (19.3, 10.8), and low overdose (11.0, 3.5). On average, the low overdose class is less White and more rural than are the high opioid classes. However, nonmetropolitan counties are most heavily represented in the prescription opioid class; 73% of counties in the high prescription opioid class are nonmetropolitan compared with 35% in the syndemic class. The prescription opioid class counties are also the most economically disadvantaged, have the highest blue-collar and service economy index scores, and have the lowest urban professional index score. These counties also have the highest average prescribing rates. The emerging heroin and syndemic class counties have the highest urban professional scores. The 2 heroin classes have the lowest average opioid-prescribing rates.
Relative risk ratios of opioid mortality class membership (compared with the low overdose class) are presented in Table 2. Economic disadvantage is associated with significantly greater odds of being in the synthetic+ class and significantly lower odds of being in the high heroin class versus the low overdose class. The blue-collar index and service economy index are associated with significantly greater odds of being in any of the 5 opioid classes versus the low overdose class. The urban professional index is associated with significantly greater odds of being in the heroin, synthetic+, or syndemic classes versus the low overdose class. High opioid prescribing significantly increases odds of membership in the prescription opioid and syndemic classes. Results were relatively unaffected by substituting opioid prescribing for 2006 to 2008 and 2012 to 2014 (see Appendix G, available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 2—
Relative Risk Ratios of Opioid Class Membership: United States
| High Rx Opioid (n = 270), RRR (95% CI) | Emerging Heroin (n = 447), RRR (95% CI) | High Heroin (n = 165), RRR (95% CI) | Synthetic+ (n = 211), RRR (95% CI) | Syndemic (n = 129), RRR (95% CI) | |
| Economic disadvantage index | 1.18 (0.90, 1.56) | 0.74 (0.54, 1.01) | 0.63 (0.42, 0.92) | 1.56 (1.12, 2.19) | 1.18 (0.60, 2.16) |
| Blue-collar index | 1.67 (1.22, 2.28) | 2.75 (1.98, 3.81) | 2.21 (1.28, 3.82) | 1.86 (1.33, 2.59) | 4.15 (1.67, 10.31) |
| Urban professional index | 0.86 (0.61, 1.22) | 3.67 (2.73, 4.94) | 2.07 (1.09, 3.96) | 2.67 (1.65, 4.32) | 6.45 (2.31, 18.06) |
| Service economy index | 1.61 (1.30, 1.99) | 1.57 (1.30, 1.89) | 1.48 (1.07, 2.05) | 1.53 (1.17, 2.00) | 1.72 (1.15, 2.57) |
| Opioid prescribing, 2009–2011 | 1.55 (1.24, 1.94) | 0.93 (0.74, 1.17) | 1.05 (0.81, 1.35) | 1.15 (0.94, 1.42) | 1.34 (1.04, 1.72) |
| Non-Hispanic White, % | 1.62 (1.13, 2.33) | 1.19 (0.83, 1.70) | 1.03 (0.66, 1.62) | 2.65 (1.44, 4.90) | 2.23 (0.77, 6.48) |
| Aged ≥ 65 y, % | 1.07 (0.83, 1.38) | 1.00 (0.80, 1.25) | 0.96 (0.71, 1.30) | 0.91 (0.69, 1.21) | 1.00 (0.69, 1.44) |
| Nonmetropolitan county | 0.66 (0.41, 1.07) | 1.09 (0.77, 1.55) | 1.00 (0.63, 1.59) | 0.88 (0.60, 1.31) | 0.56 (0.27, 1.15) |
Note. CI = 95% confidence interval; RRR = relative risk ratio. The reference category was low overdose (n = 1701). The table excludes 156 counties that did not load highly onto any class. RRRs are on the basis of multinomial logistic regression model with clustered SEs. The probability of latent profile analysis class membership was used as a model weight. Index variables, percentage non-Hispanic White, and percentage aged ≥ 65 y are from the 2000 US Census. All variables are z-score standardized except nonmetropolitan county, which is a binary variable. Sensitivity models weighting by the log of the county population and substituting opioid-prescribing rates from 2006 to 2008 and 2012 to 2014 are presented in Appendix G (available as a supplement to the online version of this article at http://www.ajph.org).
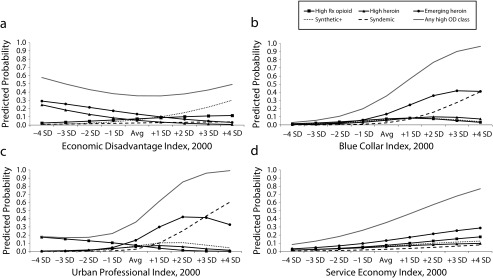
To enable comparisons across all classes, predicted probabilities of opioid class membership across levels of the 4 indices are presented in Figure 2. Probabilities are from fully adjusted models with all covariates held at their means. Higher county economic disadvantage (1) is associated with lower probability of membership in both heroin classes but higher probability of membership in the prescription opioid and synthetic+ classes. Higher blue-collar worker presence (2) is associated with higher probabilities of membership in the emerging heroin and syndemic classes. Higher values on the urban professional index (3) are related to rapidly rising probability of membership in the syndemic class. Finally, higher values on the service economy index (4) are associated with rising probability of membership in each of the 5 high opioid classes. Appendix H (available as a supplement to the online version of this article at http://www.ajph.org) shows that opioid prescribing is associated only with increased probability of membership in the high prescription opioid class and, to a much smaller extent, the syndemic class.
FIGURE 2—
Predicted Probabilities of Opioid Mortality Class Membership by Levels of Census-Variable Derived Indices (a) Economic Disadvantage Index, (b) Blue-Collar Index, (c) Urban Professional Index, and (d) Service Economy Index: United States
Note. Avg = average (mean). Predicted probabilities are calculated from fully adjusted multinomial logistic regression models with all covariates held at means.
DISCUSSION
Counties are important analytical units for understanding how ecological conditions relate to population health. Consistent with recent research on the geography of drug overdose, we found substantial county-level variation in overall drug mortality rates.2–4,29 After controlling for demographic controls, overall drug mortality rates are higher in counties characterized by more economic disadvantage, larger concentrations of blue-collar and service industries and occupations, and higher rates of opioid prescribing.
Our study also shows important geographic variation in mortality from specific types of opioids. Using latent profile analysis methods, we found that counties cluster into 6 distinct “classes” of opioid mortality, characterized by differential mortality rates and changes in rates from different types of opioids. The geographic patterns for these classes closely match those found in recent analyses that examined levels and changes in mortality rates for prescription opioids, heroin, and synthetic opioids across US states, leading us to have strong confidence in our classes.6
We found substantial variation in the importance of different place-level factors for different opioid mortality classes—an empirical observation not considered in previous research on geographic differences in opioid mortality.19,30 For example, we found that high rates of prescription opioid deaths and deaths from combinations of synthetic and prescription opioids (synthetic+ class) cluster in more economically disadvantaged counties, but economic disadvantage is associated with lower odds of membership in the heroin classes. High blue-collar and service worker presence—what we might collectively think of as the “working class”—were associated with increased odds of being in all 5 high opioid mortality classes versus the low mortality class. The nature of blue-collar and service work might increase risk for work-related injury or physical wear and tear, thereby increasing demand for pain treatments in these contexts.31
Moreover, qualitative accounts show that declines in good-paying and secure employment for the working class have manifested in collective psychosocial despair, family and community breakdown, and increased substance misuse.32,33 Graham and Pinto34 show that working-class Whites are less hopeful and optimistic about their futures than are any other group in the United States. Optimism in this group started to decline in the 1970s34 and continued to do so throughout the 1990s and 2010s.35 Interventions aimed at addressing the overdose crisis in these places must consider the likely absence of alternative pain treatment services, underfunded public services resulting from community economic disinvestment, and the need for services that address not just drug addiction but chronic pain and despair.
By contrast, the heroin and syndemic classes (counties with high mortality across all types of opioids) are more urban, have larger shares of professional workers, and are less economically disadvantaged. Interventions in these places should be structured differently on the basis of their relatively advantaged social and economic contexts. However, it is also possible that there are groups of disadvantaged residents in these counties that are driving these higher overdose rates.
Collectively, our findings highlight the importance and value of census data for understanding geographic variation in a timely and important population health crisis. Census data allow a more complete understanding of the ecological correlates of drug mortality, helping to inform the development of place-specific policies to address health crises. Our findings support the contention that population health crises and their causes and consequences follow different trajectories across places. The opioid crisis is not monolithic across the United States. Each class we identified is distinct in its socioeconomic and labor market conditions, suggesting different causes and the need for different policy responses to address the crisis. We call on researchers to explore place-based trajectories and to use historical and forthcoming census and ACS data to better understand heterogeneity in this and other population health crises.
Limitations
Findings should be considered in light of some limitations. First, because this is ecological research, we do not distinguish between place-based and individual effects, and we cannot account for individual decedents’ duration of residence. Second, aggregate measures of county-level conditions mask important in-county differences. Third, death certificates may misclassify cause of death, leading to an undercount of opioid deaths.7 We attempted to minimize this concern by including mortality from deaths where an opioid was not specified on the death certificate. Fourth, relationships between county environments and drug mortality likely play out over an extended period, but we considered only relatively recent county conditions (2000 onward) and did not consider changes in county environments over time. Future research should examine the role of changing labor markets since the 1980s and concomitant socioeconomic changes on drug mortality rates.
Finally, it was beyond the scope of our study to examine variation in mortality rates across demographic subgroups (e.g., gender, race/ethnicity, age). Future research should examine whether relationships between the ecological measures we assessed and opioid mortality rates apply equally to opioid and other drug mortality across these subgroups.
Public Health Implications
National policy strategies to combat the opioid crisis cannot be assumed to be universally applicable. For example, policies targeting the prescription opioid supply are unlikely to be effective in places characterized by high rates of heroin and synthetic opioid overdose. Addressing our opioid overdose crisis requires more than supply side interventions. A multifaceted supply and demand–based response is required.20 In addition to important national policies to combat the opioid and larger drug crisis, emphasis should be placed on developing locally and regionally tailored interventions. Ultimately, interventions are unlikely to be effective if they do not consider the diverse social and economic profiles of places and if they do not address structural upstream contributors to the opioid crisis.
ACKNOWLEDGMENTS
The authors acknowledge funding from the US Department of Agriculture (USDA), the National Institute of Food and Agriculture (grant 2018-68006-27640). S. M. M. also acknowledges funding from the Institute for New Economic Thinking, support from the Population Research Institute at the Pennsylvania State University (which receives core funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development [P2CHD041025]), and support from the USDA Agricultural Experiment Station Multistate Research Project (W4001, Social, Economic and Environmental Causes and Consequences of Demographic Change in Rural America).
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
HUMAN PARTICIPANT PROTECTION
This study was approved by the Iowa State University institutional review board.
Footnotes
REFERENCES
- 1.Hedegaard H, Minino A, Warner M. Drug Overdose Deaths in the United States, 1999–2017. Hyattsville, MD: National Center for Health Statistics; 2018. [Google Scholar]
- 2.Monnat SM. Factors associated with county-level differences in US drug-related mortality rates. Am J Prev Med. 2018;54(5):611–619. doi: 10.1016/j.amepre.2018.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Monnat SM. The contributions of socioeconomic and opioid supply factors to US drug mortality rates: urban-rural and within-rural differences. J Rural Stud. 2019;68:319–335. [Google Scholar]
- 4.Rigg KK, Monnat SM, Chavez MN. Opioid-related mortality in rural America: geographic heterogeneity and intervention strategies. Int J Drug Policy. 2018;57:119–129. doi: 10.1016/j.drugpo.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 5.Rossen LM, Bastian B, Warner M, Khan D. Drug Poisoning Mortality: United States, 1999–2016. Hyattsville, MD: National Center for Health Statistics; 2017. [Google Scholar]
- 6.Kiang MV, Basu S, Chen J, Alexander MJ. Assessment of changes in the geographical distribution of opioid-related mortality across the United States by opioid type, 1999–2016. JAMA Netw Open. 2019;2(2):e190040. doi: 10.1001/jamanetworkopen.2019.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruhm CJ. Geographic variation in opioid and heroin involved drug poisoning mortality rates. Am J Prev Med. 2017;53(6):745–753. doi: 10.1016/j.amepre.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Murray CJ, Kulkarni SC, Michaud C et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med. 2006;3(9):e260. doi: 10.1371/journal.pmed.0030260. [Erratum in PLoS Med. 2006;3(12):e545] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lobao LM, Hooks G, Tickamyer AR, editors. The Sociology of Spatial Inequality. Albany, NY: State University of New York Press; 2007. [Google Scholar]
- 10.Yang T-C, Jensen L, Haran M. Social capital and human mortality: explaining the rural paradox with county-level mortality data. Rural Sociol. 2011;76(3):347–374. doi: 10.1111/j.1549-0831.2011.00055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang TC, Jensen L. Exploring the inequality–mortality relationship in the US with Bayesian spatial modeling. Popul Res Policy Rev. 2015;34(3):437–460. doi: 10.1007/s11113-014-9350-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McLaughlin DK, Stokes CS. Income inequality and mortality in US counties: does minority racial concentration matter? Am J Public Health. 2002;92(1):99–104. doi: 10.2105/ajph.92.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cosby AG, McDoom-Echebiri MM, James W, Khandekar H, Brown W, Hanna HL. Growth and persistence of place-based mortality in the United States: the rural mortality penalty. Am J Public Health. 2019;109(1):155–162. doi: 10.2105/AJPH.2018.304787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cullen MR, Cummins C, Fuchs VR. Geographic and racial variation in premature mortality in the US: analyzing the disparities. PLoS One. 2012;7(4):e32930. doi: 10.1371/journal.pone.0032930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mansfield CJ, Wilson JL, Kobrinski EJ, Mitchell J. Premature mortality in the United States: the roles of geographic area, socioeconomic status, household type, and availability of medical care. Am J Public Health. 1999;89(6):893–898. doi: 10.2105/ajph.89.6.893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chan MPL, Weinhold RS, Thomas R, Gohlke JM, Portier CJ. Environmental predictors of US county mortality patterns on a national basis. PLoS One. 2015;10(12):e0137832. doi: 10.1371/journal.pone.0137832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turi KN, Grigsby-Toussaint DS. Spatial spillover and the socio-ecological determinants of diabetes-related mortality across US counties. Applied Geography. 2017;85:62–72. doi: 10.1016/j.apgeog.2017.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karb RA, Subramanian SV, Fleegler EW. County poverty concentration and disparities in unintentional injury deaths: a fourteen-year analysis of 1.6 million U.S. fatalities. PLoS One. 2016;11(5):e0153516. doi: 10.1371/journal.pone.0153516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ruhm CJ. Drivers of the fatal drug epidemic. J Health Econ. 2019;64:25–42. doi: 10.1016/j.jhealeco.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Ciccarone D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy. 2019;pii: S0955-3959(19):30018-0. doi: 10.1016/j.drugpo.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Case A, Deaton A. Morbidity and Mortality in the 21st Century. Washington, DC: Brookings Institution; 2017. [Google Scholar]
- 22.van Belle G, Fisher LD, Heagerty PJ, Lumley T. Biostatistics: A Methodology for the Health Sciences. 2nd ed. New York, NY: Wiley; 2004. [Google Scholar]
- 23.Centers for Disease Control and Prevention. Quintiles Transactional Data Warehouse, 2006–2016; 2018. Available at: https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html. Accessed September 1, 2018.
- 24.Carpenter J, Kenward M. Multiple Imputation and Its Application. New York, NY: Wiley; 2013. [Google Scholar]
- 25.Morgan GB. Mixed mode latent class analysis: an examination of fit index performance for classification. Struct Equ Model. 2015;22(1):76–86. [Google Scholar]
- 26.Collier ZK, Leite WL. A comparison of three-step approaches for auxiliary variables in latent class and latent profile analysis. Struct Equ Model. 2017;24(6):819–830. [Google Scholar]
- 27.Abar B, Loken E. Consequences of fitting nonidentified latent class models. Struct Equ Model. 2012;19(1):1–15. [Google Scholar]
- 28.Singer M, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet. 2017;389(10072):941–950. doi: 10.1016/S0140-6736(17)30003-X. [DOI] [PubMed] [Google Scholar]
- 29.Rossen LM, Khan D, Warner M. Trends and geographic patterns in drug-poisoning death rates in the US, 1999–2009. Am J Prev Med. 2013;45(6):e19–e25. doi: 10.1016/j.amepre.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Currie J, Jin JY, Schenll M. US employment and opioids: is there a connection? Cambridge, MA: National Bureau of Economic Research; 2018. NBER working paper 24440.
- 31.Keyes KM, Cerda M, Brady JE, Havens JR, Galea S. Understanding the rural–urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014;104(2):E52–E59. doi: 10.2105/AJPH.2013.301709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sherman J. Those Who Work, Those Who Don’t: Poverty, Morality, and Family in Rural America. Minneapolis, MN: University of Minnesota Press; 2009. [Google Scholar]
- 33.Quinones S. Dreamland: The True Tale of America’s Opiate Epidemic. New York, NY: Bloomsbury Press; 2015. [Google Scholar]
- 34.Graham C, Pinto S. Unequal hopes and lives in the USA: optimism, race, place, and premature mortality. J Popul Econ. 2019;32(2):665–733. [Google Scholar]
- 35.O’Connor KJ, Graham C. Longer, More Optimistic Lives: Historic Optimism and Life Expectancy in the United States. New York, NY: Brookings Institution; 2018. [Google Scholar]