Abstract
Context:
The objective of this systematic review was to update a prior review and summarize the evidence (newly identified and cumulative) on the impact of contraceptive counseling provided in clinical settings.
Evidence acquisition:
Multiple databases, including PubMed, were searched during 2016–2017 for articles published from March 1, 2011, to November 30, 2016.
Evidence synthesis:
The search strategy identified 24,953 articles; ten studies met inclusion criteria. Two of three new studies that examined contraceptive counseling interventions (i.e., enhanced models to standard of care) among adolescents and young adults found a statistically significant positive impact on at least one outcome of interest. Five of seven new studies that examined contraceptive counseling, in general, or specific counseling interventions or aspects of counseling (e.g., personalization) among adults or mixed populations (adults and adolescents) found a statistically significant positive impact on at least one outcome of interest. In combination with the initial review, six of nine studies among adolescents and young adults and 16 of 23 studies among adults or mixed populations found a statistically significant positive impact of counseling on at least one outcome of interest.
Conclusions:
Overall, evidence supports the utility of contraceptive counseling, in general, and specific interventions or aspects of counseling. Promising components of contraceptive counseling were identified. The following would strengthen the evidence base: improved documentation of counseling content and processes, increased attention to the relationships between client experiences and behavioral outcomes, and examining the comparative effectiveness of different counseling approaches to identify those that are most effective.
Theme information:
This article is part of a theme issue entitled Updating the Systematic Reviews Used to Develop the U.S. Recommendations for Providing Quality Family Planning Services, which is sponsored by the Office of Population Affairs, U.S. Department of Health and Human Services.
CONTEXT
Approximately 45% of U.S. pregnancies each year are unintended, with higher rates among women aged less than 25 years, some racial or ethnic minority groups, and those with lower incomes.1 Unintended pregnancy is preventable with correct and continued contraceptive use. Contraceptive counseling by trained healthcare professionals may help women, men, and couples achieve their reproductive goals by supporting them to choose a method concordant with their goals and preferences, and use their chosen method correctly.
During 2010–2011, the Centers for Disease Control and Prevention and the Office of Population Affairs conducted a series of systematic reviews, including one summarizing the evidence on the impact of contraceptive counseling provided in clinical settings on reproductive health outcomes.2 That review assessed evidence published from January 1, 1985, to February 28, 2011, and identified promising components of counseling (e.g., developing rapport, personalizing discussions to meet clients’ individual needs, and addressing psychosocial determinants of contraceptive use behaviors). Along with expert feedback and findings from two other complementary systematic reviews on the impact of education and reminder systems in family planning programs,3,4 the information was used to develop national recommendations for providing quality family planning services.5 As part of a process to keep the recommendations updated and revised as needed, the intent was to update the systematic reviews (and consider new review topics) every 3–4 years.6
The objective of this systematic review is to update the prior review and summarize the evidence on the impact of contraceptive counseling provided in clinical settings. The newly identified evidence from the updated search and the cumulative evidence from the initial and updated searches are summarized.
EVIDENCE ACQUISITION
This systematic review is reported according to the PRISMA checklist.7 The methods for conducting this updated systematic review were similar to the approach used in the prior reviews and have been described elsewhere.8 Briefly, as part of a series of systematic reviews on the impact of contraceptive counseling and education in clinical settings, six key questions (KQs) were developed (Appendix Table 1, available online). An analytic framework (Appendix Figure 1, available online) was then applied to show the relationships between the population of interest (women of reproductive age receiving Services in a clinical setting); the intervention of interest (contraceptive counseling); and the outcomes of interest Outcomes of interest relevant to KQs 1–3 included client experiences (e.g., satisfaction with the clinic visit, the provider, or counseling received); short-term outcomes (e.g., increased knowledge); medium-term outcomes (e.g., increased contraceptive use); and long-term outcomes (e.g., decreased unintended pregnancy). KQs 4–5 examined barriers and facilitators for clinics in adopting and implementing contraceptive counseling in the family planning setting and unintended negative consequences. This review describes the evidence for KQs 1–5; the evidence for KQ6 is described elsewhere.9
Search strategies were developed that included the identification of key terms (Appendix Table 2, available online), which were used to search multiple databases, including PubMed, to identify potential articles published from March 1, 2011, to November 30, 2016.
Selection of Studies
Retrieval and inclusion criteria were developed a priori. Eligible studies met the following criteria: conducted in the U.S., Canada, Australia, New Zealand, or European countries categorized as “very high” on the Human Development Index10; published in English from March 1, 2011, to November 30, 2016; described a study that addresses at least one KQ; and were full-length articles (abstracts and letters to the editor were excluded). RCTs, nonrandomized trials, cohort, and case-control studies were included. Articles also must have evaluated counseling in a clinic-based setting. Contraceptive counseling was defined as an interactive process between provider and client intended to help the client achieve a reproductive health goal related to pregnancy prevention. Studies that examined the presence or absence of contraceptive counseling in general, as well as studies that examined specific counseling interventions (i.e., enhanced models to standard of care) or approaches (e.g., personalization) were included. Studies that focused solely on prevention of HIV or sexually transmitted infections without a family planning component, or only included males, were not considered.
Some inclusion criteria were specific to KQs. KQs 1–3 sought to examine the relationships between contraceptive counseling and improved long-, medium-, and short-term outcomes and client experiences; thus, included studies had to have a comparison group. Among included studies, those that also examined barriers and facilitators or unintended negative consequences met the inclusion criteria for KQ 4 or 5. Articles that described a multi-component program (e.g., counseling in addition to a non-counseling component) had to report the impact of the counseling component independent of the non-counseling component.
Data Abstraction, Assessment of Study Quality, and Synthesis of Data
Detailed information (including study design, setting, population, intervention, outcomes, and results) was abstracted by a team of four abstractors and reviewed by two authors for relevance to contraceptive counseling; differences were reconciled by consensus. The quality of each piece of evidence was assessed using the grading system developed by the U.S. Preventive Services Task Force, and risk of bias was rated as low, moderate, or high.11 Several study factors were considered when assessing quality, including design, recruitment procedures, outcome measurement, adjustment for potential confounders, attrition, and length of follow-up. Findings are reported separately for studies conducted among adolescents and young adults (aged ≤ 24 years [adolescents were defined as those aged ≤ 21 years; young adults were defined as those aged 22–24 years]) and those conducted among adults or mixed populations (adults and adolescents). This is because adolescents and young adults are a special population of interest with potential unique needs. Findings are also stratified by outcome type (long-, medium-, and short-term outcomes and client experiences); as such, studies that examined multiple outcomes may be discussed more than once. Summary measures of association were not computed across studies because of the diversity of the interventions, study designs, populations, and outcomes.
EVIDENCE SYNTHESIS
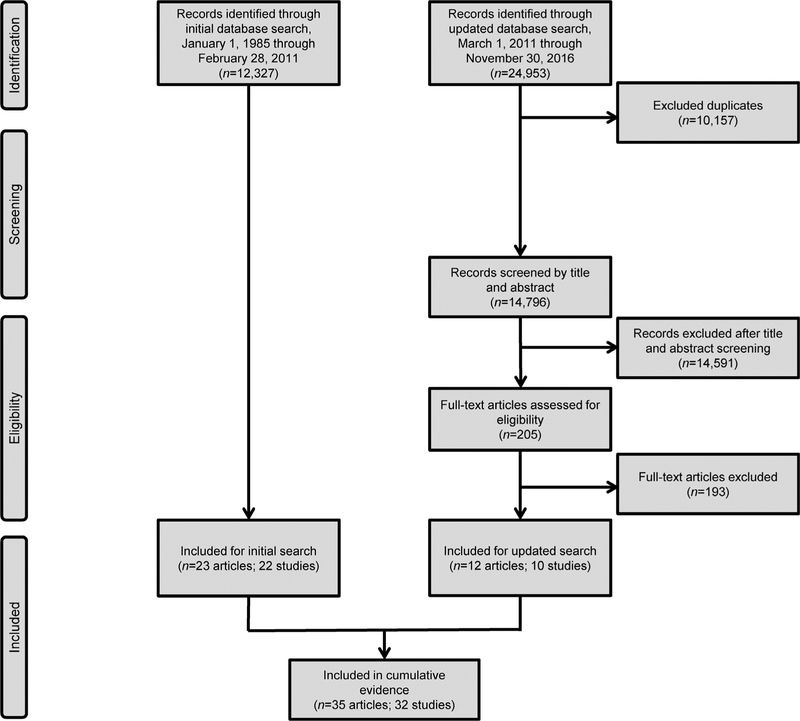
The updated search strategy identified 24,953 articles (Figure 1). After removal of duplicates (n=10,157) and applying the retrieval criteria, 205 full-text articles were reviewed. Of these, ten studies (from 12 articles) met the inclusion criteria.12–23 Findings from two articles among adolescents are considered a single piece of evidence,17,18 as are two articles from one study among adults and adolescents15,19; only the most recent of these will be cited moving forward. Of the ten newly identified studies included in this review, three examined the impact of contraceptive counseling among adolescents and young adults,12,18,20 and seven examined the impact among adults or mixed populations.13–16,21–23 Although most new studies were conducted among the general population of women seeking contraceptive Services, one was conducted among a sample of women post-abortion22 and two were conducted among postpartum women.14,23
Figure 1.
Flow chart of study selection.
In combination with the initial review, the cumulative body of evidence includes 32 studies that examined the impact of contraceptive counseling—nine among adolescents and young adults and 23 among adults or mixed populations. Only newly identified studies from the updated search are summarized in detail in the text, although the cumulative evidence from both the initial and updated searches is summarized in Table 1. For the evidence on adolescents and young adults, Table 2 tallies the significance of findings for behavioral outcomes and client experiences and Appendix Table 3 (available online) describes details of each study. For the evidence on adults or mixed populations, Table 3 tallies the significance of findings for behavioral outcomes and client experiences and Appendix Table 4 (available online) describes details of each study.
Table 1.
Cumulative Evidence on Impact of Contraceptive Counseling in Clinical Settings
| Outcome | Evidence | |
|---|---|---|
| Adolescents and young adults (n = 9) | ||
| Long-term outcomes | Of four studies that examined long-term outcomes,12,24–26 one found a statistically significant positive impact of a counseling intervention on decreasing teen pregnancy.24 | |
| Medium-term outcomes | ||
| Increased contraceptive use | Of six studies that examined contraceptive use (one from the updated search12 and five from the initial review24–28), four found a statistically significant positive impact of counseling interventions.12,24,26,27 | |
| Increased use of more effective contraception | The updated search identified no new evidence on the impact of contraceptive counseling on use of more effective contraception; thus based on two studies that examined this outcome from the initial review,24,28 one found a statistically significant positive impact of a counseling intervention.24 | |
| Increased correct use contraception | Of four studies that examined correct use of contraception (two from the updated search12,20 and two from the initial review25,29), two found a statistically significant positive impact of counseling interventions–one on OC adherence29 and one on consistent condom use.20 | |
| Increased continuation of contraception | Of two studies that examined continuation of contraceptive use (one from the updated search12 and one from the initial review26), one found a statistically significant positive impact of a counseling intervention on continuation at 6 and 12 months.26 | |
| Increased dual-method contraceptive use | The initial review found no evidence on the impact of contraceptive counseling on dual-method contraceptive use. The one newly identified study that examined this outcome found no statistically significant positive impact of an intervention on dual-method use at 3, 6, or 12 months.12 | |
| Increased repeat or follow-up service use | Of three studies that examined repeat or follow-up service use (one from the updated search18 and two from the initial review24,25), one found a statistically significant positive impact of counseling on patients returning for annual exams.24 | |
| Short-term outcomes | The updated search identified no new evidence on the impact of contraceptive counseling on short-term outcomes. One26 of two studies26,29 that examined short-term outcomes in the initial review found a statistically significant positive impact of a counseling intervention on increased knowledge and greater ease coping with contraceptive related problems. | |
| Client experiences | The updated search identified no new evidence on the impact of contraceptive counseling on client experiences. Neither of two studies that examined client satisfaction in the initial review found a statistically significant impact of counseling interventions.25,26 | |
| Barriers/facilitators and unintended negative consequences | No studies from the initial review or the updated search identified barriers or facilitators. The updated search found no new evidence on unintended negative consequences associated with contraceptive counseling in family planning settings. In the initial review, two pre-post studies examined this outcome—one found that providing contraceptive counseling did not promote sexual debut among non-sexually active adolescents,27 whereas the other found lower odds of condom use among females, thought to occur because of an increase in females’ use of more effective contraceptive methods.24 | |
| Adults or mixed populations (n = 23) | ||
| Long-term outcomes | Of six studies that examined long-term outcomes (all from the initial review),30–35 one found no differences between the intervention group and a standard of care control group in unintended pregnancy rates at 6 or 12 months, but did find reduced likelihood of unintended pregnancy at 6 months among previously pregnant intervention participants compared with previously pregnant control participants.32 However, these differences dissipated by 12 months. | |
| Medium-term outcomes | ||
| Increased contraceptive use | Of nine studies that examined contraceptive use (two from the updated search14,23 and seven from the initial review34,36–41), five found a statistically significant positive impact of counseling14,23,36,39,40 (including three that examined counseling, in general, compared with no counseling14,23,39 and two that examined a specific counseling intervention or aspect).36,40 | |
| Increased use of more effective contraception | Of 13 studies that examined use of more effective contraception (five from the updated search13,15,16,22,23 and eight from the initial review30,34,35,37,41–44), eight found a statistically significant positive impact of counseling13,15,22,23,30,34,35,43 (including one that examined counseling, in general, compared with no counseling23 and seven that examined a specific counseling intervention or aspect).13,15,22,30,34,35,43 | |
| Increased correct use contraception | The updated search found no new evidence on the impact of contraceptive counseling on correct use of contraception. Based on three studies that examined this outcome from the initial review,32,33,38 one found a statistically significant positive impact of a counseling intervention on correct use of OC.32 | |
| Increased continuation of contraceptive use | Of five studies that examined continuation of contraceptive use (two from the updated search15,21 and three from the initial review31,34,42), one found a statistically significant positive impact of a specific aspect of counseling.15 | |
| Increased dual-method contraceptive use | The updated search identified no new evidence on the impact of contraceptive counseling on dual-method contraceptive use. The one study from the initial review that examined this outcome among females seeking services at a STI clinic found a statistically significant positive impact of a counseling intervention on dual-method contraceptive use at 4 and 8 months, however differences dissipated by 12 months.35 | |
| Increased repeat or follow-up service use | The updated search identified no new evidence on the impact of contraceptive counseling on use of repeat or follow-up services. Neither of two studies that examined this outcome in the initial review found a statistically significant impact of counseling interventions.32,35 | |
| Short-term outcomes | The updated search identified no new evidence on the impact of contraceptive counseling on short-term outcomes. Based on four studies that examined these outcomes in the initial review,31,40,43,45 all found a statistically significant positive impact on at least one short-term outcome (i.e., knowledge, positive attitudes toward contraception, intentions to use contraception in the next year). This included one study that examined counseling, in general,45 and three studies that examined a specific counseling intervention or aspect compared with standard of care counseling or absence of the counseling aspect.31,40,43 | |
| Client experiences | Of three studies that examined client experiences (one from the updated search22 and two from the initial review40,44), all found a statistically significant positive impact of counseling on client satisfaction (including one that examined counseling, in general, compared with no counseling44 and two that examined a specific counseling intervention or aspect).22,40 | |
| Barriers/facilitators and unintended negative consequences | One study (from the updated search) reported information on barriers or facilitators.22 The authors commented on the intervention’s resource-intensive training and suggested that training that is more efficient may be important for high-volume clinics with high staff turnover and many different staff members performing counseling. No studies from the initial review or the updated search identified unintended negative consequences associated with contraceptive counseling in family planning settings. | |
OC, oral contraception; STI, sexually transmitted infection.
Table 2.
Summary of Impact of Contraceptive Counseling in Clinical Settings for Adolescents and Young Adults
| Outcomes | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medium-term | Short-term | |||||||||||
| Reference | Quality | Long-term: Decreased pregnancy rate | Increased contraceptive use | Increased use of more effective contraception | Increased correct use of contraception | Increased continuation of contraceptive use | Increased dual-method contraceptive use | Increased repeat or follow-up service use | Increased knowledge | Enhanced other psychosocial determinants | Client experiences: Increased quality and satisfaction with services | Total outcomes with positive impact for studya |
| Berger (1987)27 |
Level II–3; high risk for bias | NA | ↑ | NA | NA | NA | NA | NA | NA | NA | NA | 1/1 |
| Winter (1991)26 |
Level II-1; high risk for bias | ↔ | ↑ | NA | NA | ↑ | NA | NA | ↑ | ↑ | ↔ | 4/6 |
| Hanna (1993)29 |
Level I; moderate risk for bias | NA | NA | NA | ↑ | NA | NA | NA | NA | ↔ | NA | 1/2 |
| Cowley (2002)28 |
Level II–3; high risk for bias | NA | b | b | NA | NA | NA | NA | NA | NA | NA | 0/0 |
| Brindis (2005)24 |
Level II–3; high risk for bias | ↑ | ↑ | ↑ | NA | NA | NA | ↑ | NA | NA | NA | 4/4 |
| Kirby (2010)25 |
Level I; moderate risk for bias | ↔ | ↔ | NA | ↔ | NA | NA | ↔ | NA | NA | ↔ | 0/5 |
| Martin (2011)c,17,18 |
Level II–3; high risk for bias | NA | NA | NA | NA | NA | NA | b | NA | NA | NA | 0/0 |
| Berenson (2012)c,12 |
Level I; high risk for bias | ↔ | ↔ | NA | ↑/↔ | ↔ | ↔ | NA | NA | NA | NA | 1/5 |
| Redding (2015)c,20 |
Level I; moderate risk for bias | NA | NA | NA | ↑/↔ | NA | NA | NA | NA | NA | NA | 1/1 |
| Total studies with positive impacta | 1/4 | 3/6 | 1/2 | 3/4 | 1/2 | 0/1 | 1/3 | 1/1 | 1/2 | 0/2 | ||
Note: ↑statistically significant positive impact; ↓statistically significant negative impact;↔no evidence of a statistically significant impact. All studies examined a specific counseling intervention.
Statistically significant.
No statistical testing conducted.
Newly identified evidencesince2015review. NA, not assessed.
Table 3.
Summary of Impact of Contraceptive Counseling in Clinical Settings for Adults and Mixed Populations
| Outcomes | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medium-term | Short-term | ||||||||||||
| Reference | Quality | Counseling | Long-term: Decreased Increased pregnancy contraceptive rate use | Increased use of more effective contraception | Increased correct use of contraception | Increased continuation of contraceptive use | Increased dual-method contraceptive use | Increased repeat or follow-up service use | Increased knowledge | Enhanced psychosocial determinants | Client experiences: Increased quality and satisfaction with service | Total outcomes with positive impact for studya | |
| Custo (1987)30 |
Level I; moderate risk for bias | Specific intervention | ↔ | NA | ↑ | NA | NA | NA | NA | NA | NA | NA | 1/2 |
| Namerow (1989)32 |
Level II-1; high risk for bias | Specific intervention | ↔ | NA | NA | ↑ | NA | NA | ↔ | NA | NA | NA | 1/3 |
| Todres (1990)45 |
Level II-3; high risk for bias | General counseling | NA | NA | NA | NA | NA | NA | NA | ↑ | NA | NA | 1/1 |
| Weisman (2002)40 |
Level II-2; high risk for bias | Specific aspect | NA | ↑ | NA | NA | NA | NA | NA | NA | ↑/↔ | ↑ | 3/3 |
| Boise (2003)38 |
Level II-3; high risk for bias | Specific intervention | NA | b | NA | b | NA | NA | NA | NA | NA | NA | 0/0 |
| Shlay (2003)35 |
Level I; moderate risk for bias | Specific intervention | ↔ | NA | ↑/↔ | NA | NA | ↑/↔ | ↔ | NA | NA | NA | 2/4 |
| Bender (2004)37 |
Level I; moderate risk for bias | Specific intervention | NA | ↔ | ↔ | NA | NA | NA | NA | NA | NA | NA | 0/2 |
| Gilliam (2004)31 |
Level I; moderate risk for bias | Specific intervention | ↔ | NA | NA | NA | ↔ | NA | NA | ↑ | NA | NA | 1/3 |
| Yassin (2005)41 |
Level II-2; high risk for bias | Specific intervention | NA | B | b | NA | NA | NA | NA | NA | NA | NA | 0/0 |
| Proctor (2006)44 |
Level II-2; high risk for bias | General counseling | NA | NA | ↔ | NA | NA | NA | NA | NA | NA | ↑ | 1/2 |
| Schunmann (2006)34 |
Level II-1; moderate risk for bias | Specific intervention | ↔ | ↔ | ↑ | NA | ↔ | NA | NA | NA | NA | NA | 1/4 |
| Nobili (2007)43 |
Level I; moderate risk for bias | Specific intervention | NA | NA | ↑ | NA | NA | NA | NA | ↑ | ↑ | NA | 3/3 |
| Petersen (2007)33 Petersen (2007)46 |
Level I; moderate risk for bias | Specific intervention | ↔ | NA | NA | ↔ | NA | NA | NA | NA | NA | NA | 0/2 |
| Adams-Skinner (2009)36 |
Level II-2; high risk for bias | Specific intervention | NA | ↑/↔ | NA | NA | NA | NA | NA | NA | NA | NA | 1/1 |
| Langston (2010)42 |
Level I; moderate risk for bias | Specific intervention | NA | NA | ↔ | NA | ↔ | NA | NA | NA | NA | NA | 0/2 |
| Lee (2011)39 |
Level II–2; high risk for bias | General counseling | NA | ↑ | NA | NA | NA | NA | NA | NA | NA | NA | 1/1 |
| Rubenstein (2011)c,21 |
Level II–2; high risk for bias | Specific aspect | NA | NA | NA | NA | ↔ | NA | NA | NA | NA | NA | 0/1 |
| Madden (2013)c,16 |
Level II–2; moderate risk for bias | Specific intervention | NA | NA | ↔ | NA | NA | NA | NA | NA | NA | NA | 0/1 |
| Bommaraju (2015)c,13 |
Level II–2; high risk for bias | Specific intervention | NA | NA | ↑/↔ | NA | NA | NA | NA | NA | NA | NA | 1/1 |
| Cha (2015)c,14 |
Level II–2; high risk for bias | General counseling | NA | ↑ | NA | NA | NA | NA | NA | NA | NA | NA | 1/1 |
| Zapata (2015)c,23 |
Level II–2; high risk for bias | General counseling | NA | ↑ | ↑ | NA | NA | NA | NA | NA | NA | NA | 2/2 |
| Dehlendorf (2016)c,15 Minnis (2014)c,19 |
Level II–2; moderate risk for bias | Specific aspect | NA | NA | ↑/↔ | NA | ↑/↔ | NA | NA | NA | NA | NA | 2/2 |
| Whitaker (2016)c,22 |
Level I; moderate risk for bias | Specific intervention | NA | NA | ↑/↔ | NA | NA | NA | NA | NA | NA | ↑ | 2/2 |
| Total studies with positive impacta | 0/6 | 5/9 | 8/13 | 1/3 | 1/5 | 1/1 | 0/2 | 3/3 | 2/2 | 3/3 | |||
Note: ↑statistically significant positive impact; ↓statistically significant negative impact;↔no evidence of a statistically significant impact.
Statistically significant.
No statistical testing conducted.
Newly identified evidence since 2015 review.
NA, not assessed; NR, not reported.
Adolescents and Young Adults
Three newly identified studies examined the impact of contraceptive counseling among adolescents and young adults,12,18,20 each examining a specific intervention compared with standard counseling. Two studies were RCTs, one rated as having high risk for bias12 and the other rated as having moderate risk for bias20; and one was a pre—post study with a historical comparison group rated as having high risk for bias.18 One study examined a long-term outcome12 and all three studies examined at least one medium-term outcome.12,18,20 None of the studies examined short-term outcomes, client experiences, barriers or facilitators for clinics, or unintended negative consequences. Sample sizes in the three studies ranged from 8718 to 1,155,12 and all participants were aged 14–24 years and recruited from health clinics. A different model or approach to contraceptive counseling was used in each of the three studies.
Long-term outcomes.
One new study examined the impact of contraceptive counseling on reducing pregnancy rates over 12 months and did not find a statistically significant impact.12 In this RCT by Berenson et al.12 evaluating a counseling intervention to improve contraceptive adherence, 1,155 low-income adolescents and young adults aged 16–24 years requesting oral contraception (OC) were recruited from five publicly funded reproductive health clinics. Participants were randomized to receive either (1) face-to-face behavioral counseling that utilized techniques based on the health belief model (n=383); (2) this same counseling followed by monthly phone calls for 6 months from a counselor (n=384); or (3) standard care counseling (n=388). Pregnancy rates did not differ between study groups over 12 months of follow-up.
Medium-term outcomes.
All three newly identified studies examined at least one medium-term outcome,12,18,20 with two finding at least one significantly positive effect.12,20 The RCT by Berenson et al.,12 described above, found that condom use at last sexual intercourse did not differ by study group at 3, 6, or 12 months. However, after adjustment, women who received counseling plus monthly phone calls for 6 months were more likely to report condom use at last sexual intercourse than those who received standard counseling (OR=1.32, 95% CI=1.03, 1.70). The study also examined but did not find a statistically significant impact of the counseling interventions on OC adherence, OC continuation, or dual-method contraceptive use (OC plus a condom) at 3, 6, or 12 months.12
The second new study examined the impact of contraceptive counseling on consistent condom use.20 In this RCT, 828 adolescents aged 14–17 years were recruited from five urban Title X—funded family planning clinics. Adolescents were randomized to receive either a trans-theoretical model—tailored counseling intervention designed to increase condom use (n =424) or standard counseling (n=404). Consistent condom use (defined as using condoms during every sex occasion in the past month or past 3 months if no sex in the past month) was significantly higher among adolescents in the intervention versus control group at 6 months (61% vs 46%, respectively) and 12 months (51% vs 39%, respectively) but not 18 months (p-values not reported).
The third new study examined the impact of contraceptive counseling using if—then plans to overcome barriers to contraceptive use on repeat visits for emergency contraception or pregnancy testing.18 In this pre—post study from the United Kingdom with a historical comparison group, 87 adolescents aged 14–19 years using user-dependent contraceptive methods (injections, pills, condoms) were recruited from a family planning clinic. The number of consultations for emergency contraception and pregnancy testing were compared from baseline (9 months before the intervention) to follow-up (9 months after the intervention); intervention participants were also compared with 131 teen girls recruited 1-year prior who received standard counseling. Consultations for emergency contraception or pregnancy testing decreased from baseline (49%) to follow-up (34%) among the intervention group (statistical testing not reported), compared with a nonsignificant reduction from 57% to 53% among the historical control group.
Adults or Mixed Populations (Adults and Adolescents)
Seven newly identified studies examined the impact of contraceptive counseling among adults or mixed populations13–16,21–23: Two examined the impact of counseling, in general, compared with no counseling,14,23 and five examined a specific counseling intervention or aspect of counseling compared with standard of care counseling.13,15,16,21,22 One study was an RCT rated as having moderate risk for bias22; two were prospective cohort studies, both rated as having moderate risk for bias15,16; one was a retrospective cohort study rated as having high risk for bias21; and three were cohort analyses of program or cross-sectional survey data, all rated as having high risk for bias.13,14,23 All seven studies examined at least one medium-term outcome,13–16,21–23 one examined client experiences,22 and one study examined barriers or facilitators for clinics in adopting and implementing contraceptive counseling interventions.22 None of the studies reported on long-term outcomes, short-term outcomes, or unintended negative consequences. Sample sizes in the seven studies ranged from 5021 to 193,310,14 and the age of participants ranged from 14 to 53 years. Participants were recruited from health clinics in four studies,13,15,21,22 through self-referral in one,16 and from birth certificates in two studies.14,23
Medium-term outcomes.
All seven newly identified studies examined at least one medium-term outcome,13–16,21–23 with five finding a significantly positive effect on at least one outcome.13–15,22,23
Two new studies examined contraceptive use, both of which found a statistically significant impact of receiving counseling compared with not receiving counseling.14,20 The first study by Cha and colleagues14 was a cohort analysis of cross-sectional survey data from 193,310 postpartum women with a recent live birth, comparing women who reported receiving and not receiving prenatal contraceptive counseling. Those who received prenatal contraceptive counseling versus those who did not had higher odds of postpartum contraceptive use (any method; 82% vs 72%, OR=1.72, 95% CI=1.64, 1.80). The second study by Zapata et al.23 was another cohort analysis of cross-sectional survey data from postpartum women with a recent live birth reporting on receipt of contraceptive counseling (n = 9,536); women who received counseling both prenatally and postpartum and those who received counseling during only one period were compared with those who did not receive counseling during either period. Compared with postpartum women receiving no counseling, those counseled during one time period (OR=2.01, 95% CI=1.55, 2.59) and both time periods (OR=2.74, 95% Cl=2.18, 3.45) had higher odds of postpartum contraceptive use (69% vs 81% and 87%, respectively; trend p-value<0.0001).
Five new studies of specific counseling interventions or aspects of counseling examined use of more effective contraception,13,15,16,22,23 with four finding a statistically significant impact of counseling.13,15,22,23 Whitaker and colleagues22 reported on one RCT conducted with 60 women aged 15–29 years presenting for pregnancy termination at an urban academic clinic; participants either received standard counseling (n=31), or Motivational Interviewing—based counseling to encourage the use of highly effective contraception (n=29). Significantly more women in the intervention group than control group reported using a long-acting reversible contraceptive (LARC) method at 1 (65.5% vs 32.3%, RR=2.03, 95% CI=1.14, 3.61) and 3 months (60.0% vs 30.8%, RR=1.95, 95% 0=1.01, 3.77), although more women who at baseline intended to use a LARC method post-abortion were allocated to the intervention group. Use of any effective method (an intrauterine device or a hormonal method) did not statistically differ between women in the intervention and control groups at 1 or 3 months. In the second study, a prospective cohort study among 348 women aged 16–53 years seen for contraceptive care at six clinics by Dehlendorf et al.,15 patients rated their perception of the interpersonal quality of the counseling session using a scale based on dimensions of patient-centered care. Counseling sessions were also audio recorded, and research staff coded the interpersonal communication behaviors of clinicians using a validated scheme. Patients who reported high interpersonal quality of family planning care versus those who did not were more likely to be using a highly or moderately effective method at 6 months (66.0% vs 55.0%, OR=2.0, 95% 0=1.2, 3.5), although no audio recording—based measures of provider communication behaviors were associated with use of a highly or moderately effective method at 6 months. The third study was a cohort analysis of program data from 771 women (mean age of 28 years) not seeking pregnancy and receiving gynecological services from a system of Title X—funded county primary care health centers. Electronic medical records were used to compare women who did and did not receive (per provider report) reproductive life plan—based counseling delivered by providers trained to have an open dialogue with patients about their future life plans and the impact of pregnancy and parenthood on these plans, and to discuss contraceptive options in order of typical use efficacy.13 Results from multinomial logistic regression suggested that receiving reproductive life plan—based counseling was associated with LARC use versus no method or a non-medical method (natural family planning or barrier method; OR=1.6, 95% 0=1.03, 2.61), but not associated with use of depot medroxyprogesterone acetate, pills, patch or ring versus no method or a non-medical method. However, the authors concluded no association based on results from model comparisons (i.e., examination of the change in—2 log likelihood comparing models with and without the reproductive life plan counseling variable). The fourth study was a cohort analysis of cross-sectional survey data from postpartum women by Zapata and colleagues2,5 described above. In this study, compared with postpartum women who received no counseling, the odds of using a more versus less effective contraceptive method postpartum were higher for women counseled either prenatally or postpartum (OR=2.10, 95% CI=1.65, 2.67) and for women counseled both prenatally and postpartum (OR=2.33, 95% 0=1.87, 2.89, 32% vs 49% and 56%, respectively; trend p-value<0.0001). The fifth remaining study found no statistically significant effect of counseling on LARC uptake after adjustment between women at intervention versus control clinics as part of the Contraceptive CHOICE project, in which intervention clinics used counseling where methods were presented in order of effectiveness, although women in both groups had very high (>70%) LARC uptake.16
Two new studies examined continuation of contraceptive use15,21; one of which found a statistically significant positive impact of a specific aspect of counseling.15 In this prospective cohort study described above by Dehlendorf et al.,15 patients were more likely to maintain contraceptive method use at 6 months if they reported receiving high interpersonal quality of family planning care (45.6% vs 36.1%, 0R=1.8, 95% CI=1.1, 3.0) and if they had been seen by a provider rated as having high scores for “invests in the beginning” (55.7% vs 36.8%, OR=2.3, 95% CI=1.2, 4.3) and “elicits the patient perspective” (48.8% vs 38.1%, 0R=1.8, 95% CI=1.01, 3.2) based on audio-recorded counseling sessions. However, neither “demonstrates empathy” nor “invests in the end” were associated with contraceptive continuation. Among a subanalysis of 67 adolescents aged 16—21 years, patient—provider interactions around both method choice and method use were coded as to whether they were interactive and appropriately targeted. At the 6-month follow-up, use of a hormonal or LARC method among adolescents was more common among those who had received interactive and appropriately targeted counseling (80%) than among those who did not receive this type of counseling (50%; no statistical testing was conducted). The second study was a retrospective analysis of two cohorts, each with 25 women, receiving two different counseling approaches described as “just try it” and “are you really sure.” This study found no significant effect of one counseling approach over another on implant continuation rates at 12 months.21
Client experiences.
The RCT by Whitaker and colleagues22 assessed the effect of Motivational Interviewing—based counseling on client experiences. During telephone follow-up with participants at 3 months, significantly more women in the intervention group (92%) compared with those in the control group (65%) reported satisfaction with the counseling they received (p=0.04).
Barriers and facilitators for clinics.
The Whitaker and colleagues22 study provided the first evidence on barriers and facilitators for clinics in adopting and implementing contraceptive counseling interventions. The intervention lasted a median of 24 minutes (range of 14–39 minutes) and the authors reported that no sessions ended early, suggesting that clinic staff tolerated any disruption to clinic flow because of the intervention. However, the authors also reported that clinic staff did not approach 20% of eligible patients because of the unavailability of a trained counselor after one of two trained counselors left the institution. The training was described as resource intensive, which prevented training a replacement. The authors commented that training that is more efficient might be important for high-volume clinics that have high staff turnover and many different staff members performing counseling.
DISCUSSION
The cumulative review included 32 studies published from January 1, 1985, to November 30, 2016, that examined the impact of contraceptive counseling, in general, or specific counseling interventions or aspects of counseling. Of nine studies (three from the updated search12,18,20 and six from the initial review24–29) that examined the impact of counseling interventions among adolescents and young adults, six found a statistically significant positive impact of counseling on at least one outcome of interest.12,20,24,26,27,29 Twenty-three studies (seven from the updated search13–16,21–23 and 16 from the initial review30–45) examined the impact of counseling among adults or mixed populations, including five that examined counseling, in general, compared with no counseling,14,23,39,44,45 and 18 that examined specific counseling interventions or aspects.13,15,16,21,22,30–38,40–43 Of these, 16 found a statistically significant positive impact of counseling on at least one outcome of interest.13–15,22,23,30–32,34–36,39,40,43–45
Overall, findings support the provision of contraceptive counseling, compared with no counseling, on contraceptive use behaviors. With respect to specific components of counseling, because of the diversity of interventions or aspects of counseling examined—some of which incorporated multiple approaches—this review was unable to assess the impact of a single counseling component separate from the others or to compare the relative effectiveness of one approach versus another. Nevertheless, components of counseling approaches that resulted in some statistically significant positive change in outcomes of interest can be considered when developing or updating contraceptive counseling guidelines for family planning clients. Promising components to support method choice from the cumulative body of evidence include an emphasis on the quality of interaction between counselor and client (e.g., developing a rap-port)15,22,24,36,43,44; personalizing discussions to meet clients’ individual needs15,20,22,29,34,35, 40,43; and addressing psychosocial determinants of contraceptive use behaviors (e.g., perceived benefits and barriers, outcome expectations).15,26,29,31,34,43 Other promising components to support contraceptive behaviors once a method is chosen include setting goals; discussing possible difficulties with achieving goals (e.g., side effects, difficulty obtaining the method) and developing action plans to deal with potential difficulties29,31,32,36; and multiple contacts with clients20,24,26,27,35,36 New components that emerged from the updated evidence that resulted in some statistically significant positive effects include an emphasis on shared decision making,15 asking about the patient’s reproductive life plan/pregnancy intentions,13 and discussion of contraceptive methods by level of effectiveness.13,22 Across the cumulative body of evidence, seven of the counseling interventions that had a significant impact on multiple outcomes15,22,24,26,32,35,40 included at least one of these promising components.
Limitations
This body of evidence has several limitations. Of the 32 studies in this review, none were determined to have a low risk for bias, and half were determined to have a high risk for bias.12–14,18,21,23,24,26–28,32,38–41,44,45 Studies were considered to be at risk for bias for reasons including selection bias, recall bias, self-report bias, attrition bias, or short follow-up times for behavioral outcomes. Among the RCTs examined, primary weaknesses included lack of30,33,34,42 or no reporting of12,20,25,29,35,44 blinding; no reporting of allocation procedures, including concealment12,25,29,30,35,37,43; and no concealment of allocation.34 Some studies were conducted among small samples (fewer than 100 individuals)21,22,28,29,31,36,38,43,45 or stated not reaching sample size goals based on power calculations20 and may have been underpowered to detect meaningful differences in outcomes. Other studies did not state clearly how outcomes of interest were measured or they used instruments with questionable validity.213,26,40 Some studies failed to adequately establish comparability between study groups, limiting the ability to definitively attribute outcomes to the counseling intervention.18,21,26,34,37,41,45 in one cohort analysis of cross-sectional survey data, the temporal order between receipt of contraceptive counseling during a recent clinical visit and contraceptive use at last intercourse was uncertain. As previously mentioned, some studies were conducted among subpopulations that may not represent the general population of women seeking family planning Services, but represent groups that may especially benefit from quality family planning services (i.e., postpartum women14,23,31,44 and those receiving post-pregnancy termination care22,34,37,41–43 or services at a sexually transmitted infection clinic).35 Further, limited new evidence was found that examined the impact of contraceptive counseling on client experiences. Given the importance of patient-centered care and the potential negative consequences of perceived pressure to use specific contraceptive methods, understanding client perceptions of patient-centered care and satisfaction are important. Also, studies examining contraceptive counseling often do not consider client factors that might impede contraceptive use behaviors, such as current intimate partner sexual or domestic violence. Last, it is possible that additional articles meeting the inclusion criteria for this systematic review have been published since the updated search of the literature.
Despite these limitations, the evidence base for contraceptive counseling also has several strengths. Nearly half of the studies (14 of 32) in this review were RCTs,12,20,22,25,29–31,33,35,37,42,43 and many used random number tables or computer randomization for group allocation,20,25,31,33,34,37,42,44 concealed group allocation20,22,31,33,42,44 and used blinding.22,31,37,43 Several studies followed participants for at least 12 months.12,20,21,25,26,30–35 Other strengths included high participation rates,15,21,29,32,33,41 high completion rates,33,35,41,44 small differences in follow-up rates between study groups,20,30,32–34,37,42,44 and study groups with similar baseline characteristics.12,20,25,29,30,32–36,42,44 Several studies also used instruments with psychometric evidence of validity or reliability to measure constructs of interest,15,26,36 and at least three measured pregnancy by using urine tests versus self-report.24,32Several studies directly acknowledged training study staff,16,18,22,24–29,38,42 and six reported using standardized provider tools to improve intervention implementation.12,15,20,22,28,30
CONCLUSIONS
Overall, evidence supports the utility of contraceptive counseling, in general, and specific interventions or aspects of counseling to impact reproductive health outcomes and client experiences. In combination with the initial review, six of nine studies among adolescents and young adults and 16 of 23 studies among adults or mixed populations found a statistically significant positive impact of counseling on at least one outcome of interest. Despite the diversity of counseling approaches included in this systematic review and the inability to compare the relative effectiveness of one approach versus another, promising counseling components to support both method choice and use emerged (e.g., developing rapport, personalizing discussions, addressing psychosocial determinants, setting goals, developing action plans, and shared decision making). The following would strengthen the evidence base: improved documentation of counseling content and processes, increased attention to the relationships between client experiences and behavioral outcomes, and examining the comparative effectiveness of different counseling approaches to identify those that are most effective.
Supplementary Material
ACKNOWLEDGMENTS
This product was supported, in part, by a contract between the Office of Population Affairs and Atlas Research, Inc (HHSP233201500126I, HHSP233201450040A).
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Office of Population Affairs.
Footnotes
The authors have no financial disclosures or conflicts of interest to disclose.
THEME NOTE
This article is part of a theme issue entitled Updating the Systematic Reviews Used to Develop the U.S. Recommendations for Providing Quality Family Planning Services, which is sponsored by the Office of Population Affairs, U.S. Department of Health and Human Services.
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2018.07.006.
REFERENCES
- 1.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med. 2016;374(9):843–852. 10.1056/NEJMsa1506575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zapata LB, Tregear SJ, Curtis KM, et al. Impact of contraceptive counseling in clinical settings: a systematic review. Am J Prev Med. 2015;49(2):S31–S45. (suppl 1) 10.1016/j.amepre.2015.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pazol K, Zapata LB, Tregear SJ, Mautone-Smith N, Gavin LB. Impact of contraceptive education on contraceptive knowledge and decision making: a systematic review. Am J Prev Med.2015;49(2):S46–S56. (suppl 1). 10.1016/j.amepre.2015.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zapata LB, Tregear SJ, Tiller M, Pazol K, Mautone-Smith N, Gavin LB. Impact of reminder systems in clinical settings to improve family planning outcomes: a systematic review. Am J Prev Med. 2015;49(2):S57–S64. (suppl 1) 10.1016/j.amepre.2015.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gavin L, Moskosky S, Carter M, et al. Providing quality family planning services: recommendations of CDC and the U.S. Office of Population Affairs. MMWR Recomm Rep.2014;63(RR-04):1–54. [PubMed] [Google Scholar]
- 6.Gavin LB, Moskosky SB, Barfield WD. Introduction to the supplement: development of federal recommendations for family planning services. Am J Prev Med. 2015;49(2):S1–S5. (suppl 1) 10.1016/j.amepre.2015.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tregear S, Gavin L, Williams J. Systematic review methodology: providing quality family planning services. Am J Prev Med. 2015;49(2): S23–S30. (suppl 1) 10.1016/j.amepre.2015.03.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fox E, Reyna A, Malcolm NM, et al. Client preferences for contraceptive counseling: a systematic review. Am J Prev Med. 2018;55(5): 691–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.UN Development Programme. Human Development Report 2016: human development for everyone Published http://hdr.undp.org/en/2016-report/ PublishedAccessed January 2018 2016. [Google Scholar]
- 11.Harris RP, Helfand M, Woolf SH, et al. Current methods of the U.S. Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(3):21–35. (suppl) 10.1016/S0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 12.Berenson AB, Rahman M. A randomized controlled study of two educational interventions on adherence with oral contraceptives and condoms. Contraception. 2012;86(6):716–724. 10.1016/j.contraception.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bommaraju A, Malat J, Mooney JL. Reproductive life plan counseling and effective contraceptive use among urban women utilizing Title X services. Womens Health Issues.2015;25(3):209–215. 10.1016/j.whi.2015. [DOI] [PubMed] [Google Scholar]
- 14.Cha S, Chapman DA, Wan W, Burton CW, Masho SW. Intimate partner violence and postpartum contraceptive use: the role of race/ethnicity and prenatal birth control counseling. Contraception. 2015;92 (3):268–275. 10.1016/j.contraception.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 15.Dehlendorf C, Henderson JT, Vittinghoff B, et al. Association of the quality of interpersonal care during family planning counseling with contraceptive use. Am J Obstet Gynecol. 2016;215(1):78.e1–78.e9. 10.1016/j.ajog.2016.01.173. [DOI] [PubMed] [Google Scholar]
- 16.Madden T, Mullersman JL, Omvig KJ, Secura GM, Peipert JF. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception.2013;88(2):243–249. 10.1016/j.contraception.2012.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martin J, Sheeran P, Slade P, Wright A, Dibble T. Implementation intention formation reduces consultations for emergency contraception and pregnancy testing among teenage women. Health Psychol. 2009;28 (6):762–769. 10.1037/a0016200. [DOI] [PubMed] [Google Scholar]
- 18.Martin J, Slade P, Sheeran P, Wright A, Dibble T. “If-then” planning in one-to-one behaviour change counselling is effective in promoting contraceptive adherence in teenagers. J Fam Plann Reprod Health Care. 2011;37(2):85–88. 10.1136/jfprhc.2010.0016. [DOI] [PubMed] [Google Scholar]
- 19.Minnis AM, Mavedzenge SN, Luecke B, Dehlendorf C. Provider counseling to young women seeking family planning services. Perspect Sex Reprod Health. 2014;46(4):223–231. 10.1363/46e1414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Redding CA, Prochaska JO, Armstrong K, et al. Randomized trial outcomes of a TTM-tailored condom use and smoking intervention in urban adolescent females. Health Educ Res.2015;30(1):162–178. 10.1093/her/cyu015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rubenstein J, Rubenstein P, Barter J, Pittrof R. Counselling styles and their effect on subdermal contraceptive implant continuation rates. Eur J Contracept Reprod Health Care.2011;16(3):225–228. 10.3109/13625187.2011.561939. [DOI] [PubMed] [Google Scholar]
- 22.Whitaker AK, Quinn MT, Munroe B, Martins SL, Mistretta SQ, Gilliam ML. A motivational interviewing-based counseling intervention to increase postabortion uptake of contraception: a pilot randomized controlled trial. Patient Educ Couns. 2016;99(10):1663–1669. 10.1016/j.pec.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zapata LB, Murtaza S, Whiteman MK, et al. Contraceptive counseling and postpartum contraceptive use. Am J Obstet Gynecol. 2015;212(2): 171.e1–171.e8. 10.1016/j.ajog.2014.07.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brindis CD, Geierstanger SP, Wilcox N, McCarter V, Hubbard A. Evaluation of a peer provider reproductive health service model for adolescents. Perspect Sex Reprod Health.2005;37(2):85–91. 10.1363/3708505. [DOI] [PubMed] [Google Scholar]
- 25.Kirby D, Raine T, Thrush G, Yuen C, Sokoloff A, Potter SC. Impact of an intervention to improve contraceptive use through follow-up phone calls to female adolescent clinic patients. Perspect Sex Reprod Health. 2010;42(4):251–257. 10.1363/4225110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Winter L, Breckenmaker LC. Tailoring family planning services to the special needs of adolescents. Pam Plann Perspect. 1991;23(1):24–30. 10.2307/2135397. [DOI] [PubMed] [Google Scholar]
- 27.Berger DK, Perez G, Kyman W, et al. Influence of family planning counseling in an adolescent clinic on sexual activity and contraceptive use. J Adolesc Health Care.1987;8(5):436–440. 10.1016/0197-0070(87)90233-6. [DOI] [PubMed] [Google Scholar]
- 28.Cowley CB, Farley T, Beamis K Well, maybe I’ll try the pill for just a few months…”: brief motivational and narrative-based interventions to encourage contraceptive use among adolescents at high risk for early childbearing. Pam Syst Health. 2002;20(2):183–204. 10.1037/h0089493. [DOI] [Google Scholar]
- 29.Hanna KM. Effect of nurse-client transaction on female adolescents’ oral contraceptive adherence. Image J Nurs Sch. 1993;25(4):285–290. 10.1111/j.1547-5069.1993.tb00261.x. [DOI] [PubMed] [Google Scholar]
- 30.Custo G, Saitto C, Cerza S, Sertoli G. The Adjusted Contraceptive Score (ACS) improves the overall performance of behavioural and barrier contraceptive methods. Adv Contracept Deliv Syst. 1987;3(4): 367–373. [PubMed] [Google Scholar]
- 31.Gilliam M, Knight S, McCarthy M Jr. Success with oral contraceptives: a pilot study. Contraception. 2004;69(5):413–418. 10.1016/j.contraception.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 32.Namerow PB, Weatherby N, Williams-Kaye J. The effectiveness of contingency-planning counseling. Pam Plann Perspect. 1989; 21 (3): 115–119. 10.2307/2135661. [DOI] [PubMed] [Google Scholar]
- 33.Petersen R, Albright J, Garrett JM, Curtis KM. Pregnancy and STD prevention counseling using an adaptation of motivational interviewing: a randomized controlled trial. Perspect Sex Reprod Health. 2007;39(1):21–28. 10.1363/3902107. [DOI] [PubMed] [Google Scholar]
- 34.Schunmann C, Glasier A. Specialist contraceptive counselling and provision after termination of pregnancy improves uptake of long-acting methods but does not prevent repeat abortion: a randomized trial. Hum Reprod. 2006;21(9):2296–2303 10.1093/humrep/del168. [DOI] [PubMed] [Google Scholar]
- 35.Shlay JC, Mayhugh B, Foster M, Maravi ME, Baron AB, Douglas JM Jr. Initiating contraception in sexually transmitted disease clinic setting: a randomized trial. Am J Obstet Gynecol.2003;189(2):473–481. 10.1067/S0002-9378(03)00493-9. [DOI] [PubMed] [Google Scholar]
- 36.Adams-Skinner J, Exner T, Pili C, Wallace B, Hoffman S, Leu CS. The development and validation of a tool to assess nurse performance in dual protection counseling. Patient Educ Couns. 2009;76(2):265–271. 10.1016/j.pec.2008.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bender SS, Geirsson RT. Effectiveness of preabortion counseling on postabortion contraceptive use. Contraception. 2004;69(6):481–487. 10.1016/j.contraception.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 38.Boise R, Petersen R, Curtis KM, et al. Reproductive health counseling at pregnancy testing: a pilot study. Contraception. 2003;68(5):377–383. 10.1016/j.contraception.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 39.Lee JK, Parisi SM, Schwarz BB. Contraceptive counseling and use among women with poorer health. J Womens Health Issues Care. 2013;2 (1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weisman CS, Maccannon DS, Henderson JT, Shortridge B, Orso CL. Contraceptive counseling in managed care: preventing unintended pregnancy in adults. Womens Health Issues.2002;12(2):79–95. 10.1016/S1049-3867(01)00147-5. [DOI] [PubMed] [Google Scholar]
- 41.Yassin AS, Cordwell D. Does dedicated pre-abortion contraception counselling help to improve post-abortion contraception uptake? J Pam Plann Reprod Health Care. 2005;31 (2):115–116. 10.1783/1471189053629347. [DOI] [PubMed] [Google Scholar]
- 42.Langston AM, Rosario L, Westhoff CL. Structured contraceptive counseling—a randomized controlled trial. Patient Educ Couns. 2010;81 (3):362–367. 10.1016/j.pec.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 43.Nobili MP, Piergrossi S, Brusati V, Moja BA. The effect of patient-cen-tered contraceptive counseling in women who undergo a voluntary termination of pregnancy. Patient Educ Couns. 2007;65(3):361–368. 10.1016/j.pec.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 44.Proctor A, Jenkins TR, Loeb T, Elliot M, Ryan A. Patient satisfaction with 3 methods of postpartum contraceptive counseling: a randomized, prospective trial. J Reprod Med.2006;51(5):377–382. [PubMed] [Google Scholar]
- 45.Todres R Effectiveness of counseling in the transmission of family planning and sexuality knowledge. J Sex Educ Ther. 1990;16(4): 279–285. 10.1080/01614576.1990.11075001. [DOI] [Google Scholar]
- 46.Petersen R, Albright JB, Garrett JM, Curtis KM. Acceptance and use of emergency contraception with standardized counseling intervention: results of a randomized controlled trial. Contraception. 2007;75(2): 119–125. 10.1016/j.contraception.2006.08.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.