Abstract
Objective:
There has been substantial research and public interest in mindfulness interventions, biological pathways, and health over the past two decades. This article reviews recent developments in understanding relationships between mindfulness interventions and physical health.
Methods:
A selective review was conducted with the goal of synthesizing conceptual and empirical relationships between mindfulness interventions and physical health outcomes.
Results:
Initial randomized controlled trials (RCTs) in this area suggest that mindfulness interventions can improve pain management outcomes among chronic pain populations, and there is preliminary evidence for mindfulness interventions improving specific stress-related disease outcomes in some patient populations (i.e., clinical colds, psoriasis, IBS, PTSD, diabetes, HIV). We offer a stress buffering framework for the observed beneficial effects of mindfulness interventions and summarize supporting biobehavioral and neuroimaging studies that provide plausible mechanistic pathways linking mindfulness interventions with positive physical health outcomes.
Conclusion:
We conclude with new opportunities for research and clinical implementations to consider in the next two decades.
Keywords: mindfulness, meditation, randomized controlled trial, mechanisms, health
INTRODUCTION
The American Psychosomatic Society and this journal have long supported the development and testing of mindfulness interventions for improving physical health, publishing some of the initial high impact theoretical reviews (1) and empirical studies (2–4). Since this early work, there has been dramatic growth in this area with more high quality randomized controlled trials (RCTs) exploring whether mindfulness interventions can positively influence biopsychosocial and disease pathogenic processes (5,6). While much of the RCT work has focused on how mindfulness interventions can improve mental health outcomes (e.g., by lowering risk for depression relapse in high risk individuals (7)), there are also promising RCTs suggesting that mindfulness interventions can improve physical health. This review considers the progress our field has made in studying mindfulness interventions and physical health over the last two decades. We first introduce mindfulness interventions, then consider outcomes, followed by a description of mechanistic pathways (biological, behavioral, psychological), and conclude with a consideration of open questions and opportunities for the field to address in the coming decades.
Mindfulness Interventions: What are they?
The principle aim of mindfulness-based interventions is to foster greater mindfulness, defined as a process of openly attending, with awareness, to one’s present moment experiences (5,8,9). This definition of mindfulness, like many others in the literature (8,10,11), describes mindful awareness as a process of using one’s attention to monitor one’s moment-to-moment experience through an open lens of equanimity and acceptance (5,12). Mindfulness interventions in the scientific literature appear in many forms, ranging from 3-month residential mindfulness meditation retreats to brief single-session guided mindfulness exercises (5). The 8-week Mindfulness-Based Stress Reduction (MBSR) program is the most popular mindfulness intervention used in the scientific literature, and consists of eight 2.5 hour classes, a day-long retreat, and daily audio-guided home practice (13). The MBSR program, and many of its variants (e.g., Mindfulness-Based Cognitive Therapy (MBCT), Mindfulness-Based Relapse Prevention (MBRP)), focus on helping individuals learn how to mindfully attend to body sensations and emotional reactions through the use of guided exercises (e.g., body scan, gentle stretching, seated meditation) and class discussion. While MBSR dominates the evidence-based scientific landscape of mindfulness interventions, other forms of mindfulness interventions have been empirically tested and show promise for improving health-related biomarkers—including residential mindfulness meditation retreats (14,15), smartphone-delivered mindfulness programs (16), and brief 3–4 day audio-guided mindfulness training in the laboratory (17).
Despite this surge in mindfulness-based RCTs, most have utilized wait-list or treatment as usual (TAU) comparison groups. In recent years, though, there has been greater adoption of active treatment comparison programs. These active comparator programs aim to control for non-mindfulness specific factors such as group and instructor support, positive treatment expectancies, daily home practice, and stress management psychoeducation (5). While wait-list and TAU studies provide an important initial evaluation of whether mindfulness interventions impact health (cf. 18), active treatment comparators allow for inferences about mindfulness-specific effects on health. This review aims to highlight some of the new active treatment controlled mindfulness intervention trials where available.
Mindfulness Interventions and Physical Health: Outcomes
Initial RCTs have demonstrated the potential for mindfulness interventions to improve a range of stress-related disease-specific outcomes (see Table 1). Here we provide some selective highlights of these studies (see also relevant reviews 5,19,20). First, several recent large RCTs show that mindfulness interventions improve pain management outcomes. For example, 8-week mindfulness interventions have been shown to significantly reduce functional disability and improve pain management in chronic low back pain patients (21–23), chronic pain patients misusing opioids (22), rheumatoid arthritis patients (24), and fibromyalgia patients (25) (cf. 26). Two interesting patterns are worth noting in this area. First, there is some initial indication that mindfulness interventions are superior to health education and social support programs for treating chronic pain (22–24), but the evidence is mixed regarding whether mindfulness interventions confer any relative pain treatment advantage over high quality cognitive-behavioral therapy (CBT) programs (21,24). Second, the durability of treatment effects at follow-up is unclear. Some RCTs suggest that decreased perceptions of pain (e.g., intensity, severity) can be sustained at follow-ups ranging from three months to one year (21–23), although there is not strong evidence that functional pain improvements can also be sustained (21,23).
Table 1.
Randomized controlled trials examining the effect of mindfulness interventions on health outcomes
| Reference | Population | Mindfulness Intervention | Comparison Group(s) | Outcome | Follow-up Time Point |
Direction of Findings |
|---|---|---|---|---|---|---|
| Cherkin et al (2016) | Adults with chronic low back pain | 8-week MBSR | UC | Pain | 6-mo | ↓ |
| 12-mo | ↓ | |||||
| Functional Disability | 6-mo | ↓ | ||||
| 12-mo | ↓ | |||||
| CBT | Pain | 6-mo | no differences | |||
| 12-mo | no differences | |||||
| Functional Disability | 6-mo | no differences | ||||
| 12-mo | no differences | |||||
| Morone et al (2016) | Older adults with chronic low back pain | 8-week MBSR | HEP | Pain | Immediate | ↓ |
| 6-mo | ↓ | |||||
| Functional Disability | Immediate | ↓ | ||||
| 6-mo | no differences | |||||
| Garland et al (2014) | Chronic pain patients addicted to opioids | 8-week MORE | Social Support | Pain | Immediate | ↓ |
| 3-mo | ↓ | |||||
| Desire for opioids | Immediate | ↓ | ||||
| 3-mo | no differences | |||||
| Davis et al (2015) | RA patients | 8-week Mindful Awareness & Acceptance | CBT-P | Daily pain | Immediate | ↓ |
| Arthritis Education | Daily pain | Immediate | ↓ | |||
| Van Gordon et al (2017) | Fibromyalgia patients | 8-week Meditation Awareness Training | CBT for Groups | Pain | Immediate | ↓ |
| 6-mo | ↓ | |||||
| FMS | Immediate | ↓ | ||||
| 6-mo | ↓ | |||||
| Schmidt et al (2011) | Female fibromyalgia patients | 8-week MBSR | Active Control | FMS | Immediate | no change |
| Wait-List | FMS | Immediate | no change | |||
| Barrett et al (2012) | Healthy community adults | 8-week MBSR | Exercise Program | ARI (incidence, duration, severity) | ↓ | |
| No Treatment Control | ARI (incidence, duration, severity) | ↓ | ||||
| Kabat-Zinn et al (1998) | Psoriasis patients | Ultraviolet light therapy + audio MBSR | Ultraviolet light therapy only | Psoriasis lesions | Immediate | ↓ |
| Garland et al (2012) | IBS female patients | 8-week MBSR | Support Group | IBS symptom severity | Immediate | ↓ |
| Pain catastrophizing | Immediate | ↓ | ||||
| Zernicke et al (2013) | IBS patients | 8-week MBSR | UC | IBS symptom severity | Immediate | ↓ |
| 6-mo | no differences | |||||
| Quality of Life | Immediate | no differences | ||||
| 6-mo | no differences | |||||
| Shomaker et al (2017) | Adolescent girls at risk for type 2 diabetes | 6-week Mindfulness training | CBT | Insulin resistance | Immediate | ↑ |
| 6-mo | ↑ | |||||
| Fasting insulin | Immediate | ↑ | ||||
| 6-mo | ↑ | |||||
| Creswell et al (2009) | HIV patients | 8-week MBSR | 1-day Seminar | CD4+ | Immediate | ↑ |
| Gonzalez-Garcia et al (2013) | HIV patients | 8-week MBCT | UC | CD4+ | Immediate | no differences |
| 3-mo | ↑ | |||||
| Seyed et al (2012) | HIV patients | 8-week MBSR | Education & Support Group | CD4+ | Immediate | ↑ |
| 3-mo | ↑ | |||||
| 6-mo | ↑ | |||||
| 9-mo | ↑ | |||||
| 12-mo | no differences | |||||
| Creswell et al (2016) | Unemployed community adults | 3-day MBSR retreat | 3-day Relaxation retreat | IL-6 | 4-mo | ↓ |
| Creswell et al (2012) | Lonely older adults | 8-week MBSR | Wait-List | CRP | Immediate | no differences |
| IL-6 | Immediate | ↓(marginal) | ||||
| Jedel et al (2014) | Ulcerative colitis patients | 8-week MBSR | Education | CRP | 12-mo | ↓(among flared) |
| IL-6 | 12-mo | no differences | ||||
| Malarkey et al (2015) | Adults at-risk for cardiovascular disease | 6-week MBSR | Lifestyle Education | CRP | Immediate | ↓(marginal) |
| 6-mo | no differences | |||||
| IL-6 | Immediate | no differences | ||||
| 6-mo | no differences | |||||
| Fogarty et al (2015) | RA patients | 8-week MBSR | Wait-List | CRP | Immediate | no differences |
| Bower et al (2015) | Young breast cancer survivors | 6-week MAPS | Wait-List | CRP | Immediate | no change |
| IL-6 | Immediate | ↓(among high compliance subgroup) |
The table is organized so that trials examining similar or related health outcomes are clustered together. The Reference column provides information about the authors; the Population column indicates whether data was obtained from healthy or specific clinical samples; the Mindfulness Intervention column refers to the length and type of mindfulness intervention used; the Comparison Group(s) column refers to the type of control group; the Outcome column indicates the primary outcome of interest for this review; the Follow-up Time Point column provides information about the presence of follow-up measures and how long after the interventions these measures were obtained; and the Direction of Findings column indicates whether there was an increase, decrease, or no change in health-related outcomes in the mindfulness group relative to the control group. Abbreviations. ARI: Acute Respiratory Infection; CBT: Cognitive Behavioral Therapy; CBT-P: Cognitive Behavioral Therapy for Pain; CD4+: CD4+ T-lymphocyte cell count; CRP: C-Reactive Protein; FMS: Fibromyalgia Symptoms; HEP: Health Enhancement Program; IBS: Irritable Bowel Syndrome; IL-6: Interleukin-6; MAPS: Mindful Awareness Practices; MBCT: Mindfulness-Based Cognitive Therapy; MBSR: Mindfulness Based Stress Reduction; MORE: Mindfulness-Oriented Recovery Enhancement; RA: Rheumatoid Arthritis; UC: Usual Care.
Second, several RCTs suggest that mindfulness interventions may impact clinically-relevant stress-related physical health outcomes. There is some initial indication that mindfulness interventions can accelerate treatment-related skin clearing in psoriasis patients (4) and reduce post-traumatic stress disorder (PTSD) symptomatology among veterans (27). Similarly, an active treatment RCT showed decreased susceptibility to (and duration of) colds in a mindfulness group. However this mindfulness intervention did not significantly decrease the number of overall health care visits or cold-related missed work days (28). A wait-list control RCT showed decreases in irritable bowel syndrome (IBS) symptomatology immediately after a mindfulness intervention and at a 6-month follow-up (29,30). Similarly, Garland and colleagues found decreases in IBS symptomatology after a mindfulness intervention compared to a social support active control group (29). A recent active treatment RCT showed decreases in insulin resistance and fasting glucose among individuals at-risk for type 2 diabetes. However, authors reported that class attendance was significantly higher in the mindfulness intervention than in the control group (31). While, these disease-specific findings are promising, only a handful of RCTs have examined clinically relevant outcomes in a rigorous way—an opportunity for future research.
Some studies also suggest that mindfulness interventions can buffer declines in CD4+ T lymphocyte counts among HIV-infected adults (31–33) – a gold-standard clinical measure of HIV-pathogenesis (34). One critical consideration we have raised is that stress buffering mechanisms may drive mindfulness intervention effects (35), as stress is known to trigger the onset or exacerbation of disease pathogenic processes in clinical colds, IBS, diabetes, and HIV progression. While we discuss these stress buffering mechanisms later in this review, the example of HIV-progression is prudent here in that mindfulness interventions appear to be more likely to impact CD4+ T lymphocytes among higher stress samples (31–33), compared to lower stress HIV-positive samples (36).
There has been significant recent interest in evaluating whether mindfulness interventions can reduce markers of systemic low-grade inflammation (e.g., C-Reactive Protein (CRP) or Interleukin-6 (IL-6)). However, the current RCT evidence is mixed. While some RCTs suggest that mindfulness interventions may reduce IL-6 (14) or CRP (37–39) among older adults and high stress adults, other studies have failed to show any reduction (IL-6:(37,39,40); CRP: (41). Furthermore, while Jedel et al. (2014) reported that a mindfulness intervention reduced CRP, they questioned its clinical significance given that this reduction in CRP did not lower the incidence of ulcerative colitis flare-ups. We offer two provisional conclusions in this area. First, there is not compelling evidence to-date that mindfulness interventions reliably lower markers of systemic inflammation. Second, it may be that mindfulness interventions reduce inflammation, but only among participant groups who have significantly elevated inflammatory biology (e.g., older adults, individuals with inflammatory diseases, or among individuals with high levels of psychological stress and/or obesity). For example, one methodologically strong trial showed that mindfulness training buffered stress-induced inflammatory responses in the skin (42).
In summary, there is initial RCT evidence suggesting that mindfulness interventions can affect physical health. The strongest evidence is in chronic pain conditions, with some promising initial effects also observed for stress-related disease specific conditions (e.g., psoriasis, IBS, diabetes, PTSD, HIV). What are needed are more mechanistic RCTs focused on which components of mindfulness interventions are most effective, and what plausible biobehavioral processes are engaged that impact health and disease over time. Below we describe some promising biological, behavioral, and psychological mechanisms from recent mindfulness training RCTs.
Mindfulness Interventions and Physical Health: Mechanisms
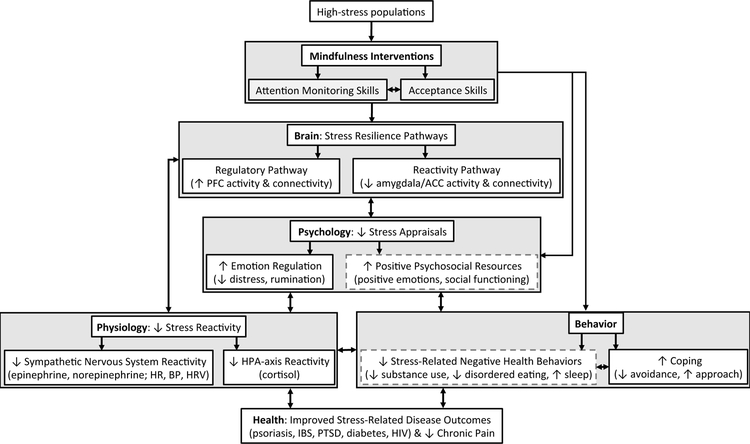
We have developed a mechanistic stress buffering framework positing that mindfulness interventions train central stress resilience pathways in the brain, which in turn mitigate the cumulative wear-and-tear that stress (and stress-related health behaviors) can play in exacerbating or accelerating disease pathogenesis across a broad spectrum of stress-related diseases (35,43,44). A conceptual outline of this framework is shown in Figure 1. One advantage of this framework is that it describes the conditions under which mindfulness interventions are most likely to improve physical health, specifically (1) among high stress patient populations, and (2) when measuring stress-sensitive health and disease outcomes. Indeed, the extant mindfulness intervention RCT outcomes described above are consistent with this framework, as stress is known to trigger the onset or exacerbation of symptoms in chronic pain, psoriasis, IBS, PTSD, and diabetes (45). More recently, we have developed theory and research on the psychological mechanisms for mindfulness intervention effects, positing that the instruction of acceptance and equanimity skills in mindfulness interventions are critical for fostering stress resilience and health benefits (16,46). While we have previously described these theoretical perspectives (5,35,46), here we provide some updates and links to biobehavioral processes relevant to biobehavioral medicine researchers.
Figure 1.
Plausible pathways linking mindfulness interventions with physical health. Mindfulness interventions, which train skills in monitoring present-moment experience with an orientation of acceptance, are proposed to impact physical health primarily among high-stress populations. Stress-buffering pathways in the brain, peripheral physiology, and subjective experience are posited to increase coping resources, which buffer recurrent, exaggerated, or dysregulated biological stress responses and negative health behaviors. Specifically, mindfulness interventions increase activity and connectivity in regulatory prefrontal cortex brain regions (the top-down regulatory pathway) and decrease reactivity and connectivity in regions that gate the body’s fight-or-flight stress response (the bottom-up reactivity pathway). These neural changes alter stress appraisals, decrease physiological stress reactivity in the sympathetic nervous system and hypothalamic-pituitary-adrenal (HPA) axis, and impact coping and health behaviors. Together, changes in neural and physiological stress responding, stress appraisals, coping, and health behaviors may be important mechanisms for improvements in stress-related disease outcomes observed following mindfulness interventions. Pathways outlined in dotted gray lines represent theorized mechanisms for future research.
Mindfulness Intervention Mechanisms: Biological Pathways
Research from our laboratory suggests that mindfulness interventions train two stress resilience pathways in the brain: (1) increasing activity and functional connectivity in stress regulatory regions of the prefrontal cortex (the regulatory pathway), and (2) decreasing activity and functional connectivity in regions gating the brain’s stress alarm system (the reactivity pathway) (35). Regarding the regulatory pathway, we and others have shown that mindfulness interventions increase the coupling of the resting brain (the so-called default mode network) with regulatory regions of the prefrontal cortex in the executive control network (14,47,48), while also increasing connectivity strength among regions within the executive control network (49). As one example, we randomly assigned a sample of stressed unemployed adults to either a 3-day intensive residential mindfulness training retreat or a well-matched relaxation training retreat, and found increased coupling of the resting brain (i.e., the posterior cingulate cortex in the default mode network) with bilateral dorsolateral prefrontal cortex in the mindfulness group, a coupling effect we did not observe in the relaxation training group (14). A pilot mindfulness training study with veterans found the same brain coupling effect after 16 weeks of mindfulness training (48). Notably, both studies observed that this increased coupling of regulatory regions in the prefrontal cortex (dorsolateral prefrontal cortex) was associated with improvements in markers of health—such as intervention-driven reductions in IL-6 in stressed community adults (14) and post-traumatic stress disorder (PTSD) symptomatology among veterans (48).
The mindfulness stress buffering framework also posits that mindfulness interventions turn down the activity and functional connectivity of regions gating the brain’s fight-or-flight response under stress (the reactivity pathway). The central nucleus of the amygdala has long been considered an important node for gating the central stress response (50,51), and recent studies suggest that mindful awareness and mindfulness interventions are associated with modulations in amygdala structure and function (52–55). For example, we have recently shown that mindfulness training decreases stress-related resting state functional connectivity of the amygdala with subgenual anterior cingulate cortex (53), a pathway that may be important in coordinating the brain’s central fight-or-flight stress response (51).
If mindfulness interventions can foster stress resilience pathways in the brain, they would also be expected to modulate peripheral sympathetic nervous system and hypothalamic-pituitary-adrenal (HPA) responses to exogenous stressors (35). Indeed, some initial work suggests that mindfulness interventions can buffer sympathetic nervous system and HPA-axis responses to acute stress (16,56), although not all RCT studies show sympathetic nervous system and HPA-axis stress buffering effects (42,57). There are still major questions in this area, such as how mindfulness interventions impact coping responses under stress (e.g., using approach or avoidance behaviors;;58), and whether mindfulness intervention driven stress and coping responses play an important mechanistic role in explaining stress-related physical health outcomes in patient populations.
Mindfulness Intervention Mechanisms: Health Behavior Pathways
Mindfulness interventions are posited to affect not only stress-related biological pathways, but also stress-related health behaviors (35). While it is well known that stress is associated with negative health behaviors such as greater tobacco use, increased difficulty with smoking cessation, increased likelihood of smoking relapse (59,60), poorer diet and eating behaviors (60,61), and impaired sleep quality (62), less is known about how mindfulness-based interventions can impact these behaviors. Some of the strongest evidence from RCTs in this area suggests that mindfulness interventions can reduce substance-use behaviors in at-risk populations, such as cigarette use among heavy smokers (63), drug relapse and alcohol consumption among substance-abusing individuals (64), and opioid misuse among adults suffering from chronic pain (22). One recent meta-analytic review found that mindfulness-based treatments reduced substance misuse, substance craving, substance-related stress, and frequency of post-treatment relapse relative to both TAU and active comparator interventions such as CBT or relapse prevention treatment (65). Surprisingly, few rigorous RCTs have evaluated whether mindfulness interventions impact diet, sleep, physical exercise, or other salutary health behaviors. Some initial RCTs suggest that mindfulness interventions can affect eating behaviors, such as reducing binge eating (66) and sweet consumption (67,68). While initial RCTs indicate that mindfulness interventions can improve measures of self-reported sleep (69,70), they have not been shown to be superior to CBT (70), and little research has used objective sleep measures (e.g., actigraphy or polysomnography) (cf. 71). In summary, more high-quality RCTs are needed to study the effects of mindfulness interventions on health behaviors, in particular studies that relate changes in health behaviors to alterations in health and disease outcomes.
Mindfulness Intervention Mechanisms: Psychological Pathways
There has been much interest in the psychological mechanisms and pathways linking mindfulness interventions with health, and prominent models have posited that psychological processes such as emotion regulation, self-awareness, attentional control, self-reported mindfulness skills, and decentering may be important mechanisms (72–76). We have taken a different approach, which is consistent with definitions and theory on mindfulness (5,8), by focusing on the psychological skills taught in mindfulness interventions. Specifically, we have developed Monitor and Acceptance Theory (MAT), which posits that learning how to (1) use one’s attention to monitor present moment experiences while (2) adopting an orientation of acceptance toward these experiences may be critical psychological mechanisms for mindfulness intervention effects (46). Indeed, there is initial evidence that self-reported increases in these two basic mindfulness skills (attention monitoring and acceptance) are related to improvements in mental health outcomes following mindfulness interventions (77,78). MAT posits that learning acceptance skills is critical for regulating emotion and developing the capacity to be less reactive to stressful experiences, and that removing acceptance skills training from mindfulness interventions will attenuate or eliminate their stress buffering health benefits.
We recently tested this MAT prediction in two mindfulness intervention RCTs. Participants were randomly assigned to (1) mindfulness training that included the standard attention monitoring and acceptance skills training (Monitor + Accept), (2) mindfulness training that included attention monitoring skills training only (Monitor Only), or (3) control. In both studies, we observed stress buffering benefits in the Monitor + Accept group compared to the other groups. Specifically, an 8-week Monitor + Accept mindfulness intervention group showed significantly greater stress buffering effects on daily life stress perceptions at post-treatment, compared to a well-matched 8-week Monitor Only mindfulness intervention group and an assessment only control group (Chin et al., under review). We further controlled for nonspecific treatment effects (e.g., social contact, instructor effects) in a 2-week smartphone-based intervention study, showing that Monitor + Accept mindfulness training was significantly more effective in buffering cortisol and blood pressure reactivity responses to a laboratory stress challenge, compared to both a Monitor Only mindfulness training group and a structurally-matched placebo control training group (16) (cf. 79). Together, these findings provide promising evidence that acceptance skills training may be a necessary component for driving stress buffering effects in mindfulness interventions, although it is still unknown whether these stress buffering effects translate into improved stress-related health and disease outcomes over time.
Discussion
Since the early reviews and empirical work published in this journal twenty years ago (e.g., 1–4), mindfulness intervention research has come a long way. Some of the strongest physical health RCT evidence to-date suggests that mindfulness interventions can improve pain symptom management among chronic pain populations, and they may improve some stress-related health and disease outcomes in at-risk populations (e.g., psoriasis, clinical colds, IBS, PTSD, diabetes, HIV). While there have been some initial efforts at conceptualizing and empirically testing how mindfulness interventions impact other stress-related diseases that are highly prevalent and drive a significant burden of health care costs (76,e.g., cardiovascular disease, cancer 80), more high-quality RCT research is needed evaluating their efficacy and public health impacts. We are also beginning to identify promising neural, physiological, behavioral, and psychological mechanisms linking mindfulness interventions with physical health. Our stress buffering framework, and initial supporting studies, suggest that mindfulness interventions foster two stress resilience pathways in the brain (the regulatory and reactivity pathways), and can potentially foster regulation of HPA and SAM-axis stress reactivity in ways that may help explain how mindfulness interventions impact stress-related health and disease outcomes over time (35). Furthermore, our more recent work has focused on the psychological mechanisms for stress buffering effects, showing that acceptance skills training may be a critical component driving stress resilience effects in mindfulness interventions (16). This mechanistic work suggests new ways to approach the next generation of RCTs, indicating that mindfulness intervention effects on physical health may be best observed by measuring stress-sensitive health outcomes among high stress populations.
While the first wave of physical health focused RCT studies is promising, our understanding of mindfulness interventions and physical health still lags behind the larger RCT literature linking mindfulness interventions with mental health outcomes (5) and there are still many unanswered questions. Here we enumerate some leading questions in this area, with the hope that they stimulate new research:
Do mindfulness interventions have any relative treatment advantages on physical health compared to other high quality behavioral stress management interventions? While there is consistent evidence that mindfulness interventions improve health relative to wait-list, treatment as usual, and some health education programs, the conditions under which mindfulness interventions provide relative treatment advantages compared to other behavioral treatment programs, such as CBT (e.g., 21), are currently unclear1. In this review we have aimed to highlight some of the higher quality active treatment controlled RCTs of mindfulness interventions, but they are still few in number. These trials are important in helping us evaluate whether there are mindfulness-specific effects above and beyond factors such as group support, relaxation, daily home practice, and placebo expectancies (cf. 82). We suspect that mindfulness interventions can be efficacious under some circumstances, and our recent work (and others, 83) has focused on the most stringent treatment controlled approach to date—namely pitting two different forms of mindfulness intervention against each other in a dismantling study approach (16).
Do stress buffering pathways explain how mindfulness interventions impact physical health outcomes? While we have outlined some promising RCT evidence for a stress buffering mechanistic framework, which explains the biological embedding of mindfulness interventions, it is certainly possible that other pathways may provide a better evidence-based framework of mindfulness intervention physical health effects. For example, mindfulness interventions also boost positive emotions (e.g., (84,85) and social connections (37,86,87) that may ultimately improve physical health outcomes. Indeed, positive affectivity and positive social relationship processes are known to independently promote physical health outcomes (88,89). The effects of mindfulness on positive emotions and social relationships may be directly associated with health, or may still operate through stress buffering pathways (i.e., mindfulness improves positive affect and social functioning, which lowers stress, and ultimately improves health outcomes).
What is the necessary mindfulness intervention dose for physical health benefits? As described in this review, the current evidence base indicates that 8-week mindfulness interventions can impact physical health outcomes—but do smaller intervention doses have benefits? Although brief mindfulness interventions and inductions lasting two weeks or less show small overall effects in reducing negative affect and distress (e.g., 90) and in buffering stimulated pain responses (17), at least two weeks of daily mindfulness training may be needed to see biological stress buffering effects (16). Furthermore, intervention dosing likely depends on participant factors, quality of mindfulness practice, and specific outcomes measured.
How long do mindfulness intervention effects last following intervention? There are currently few high quality RCTs that include follow-up assessments, and these studies provide mixed evidence. Some studies show maintenance of post-treatment effects (e.g., 27), some studies show no relative treatment advantage of mindfulness interventions at post-treatment but show advantages at longer-term follow-up assessments (e.g., 64), and yet other studies show immediate post-treatment benefits that degrade at follow-up assessments (e.g., 23). One explanation for these divergent effects is that some participants complete daily home practice and incorporate mindfulness skills into their daily lives during and after the intervention in ways that might propagate intervention effects over time. It will be important for future RCTs to find effective ways of measuring continued mindfulness practices (formal and informal) both during mindfulness interventions and in subsequent follow-up periods to test whether these practice variables explain health effects over time.
Do smartphone and online mindfulness interventions improve physical health? There is tremendous public interest in smartphone and online mindfulness interventions (e.g., Headspace, Brightmind, Calm), although almost no published studies have evaluated how these programs affect health. These programs do have certain advantages relative to 8-week group-based mindfulness programs—they are widely available, they can be delivered remotely to hard-to-reach individuals who own smartphones, and they are relatively inexpensive. To our knowledge, our recent 14-day smartphone study is the first to link a remote mindfulness intervention with biomarkers of health (i.e., cortisol and blood pressure reactivity) (16). Given their popularity, more research is needed to test the efficacy of these mindfulness interventions for health outcomes, patients’ motivation for engaging in these programs, as well as the safety of these stress management interventions with minimal instructor support.
Conclusions
An early review in this journal began with the title, “What do we really know about mindfulness-based stress reduction?” (1). We certainly know a great deal more now about the effects of MBSR and other mindfulness interventions on physical health, but many questions remain. There is a significant need for high quality RCTs in this area, as many clinicians are now using mindfulness-based therapeutic approaches, and large numbers of individuals are seeking out mindfulness programs online or in their communities. We believe that Psychosomatic Medicine is well poised to advance these research efforts in the coming decades.
Acknowledgments
Portions of this manuscript were presented at the 2017 American Psychosomatic Society annual conference in Seville, Spain as part of David Creswell’s APS Herbert Weiner Early Career Award address. The writing of this manuscript was supported in part by grants from the National Center for Complementary & Integrative Health (NCCIH) of the National Institutes of Health (R21AT008493, R01AT008685, F32AT009508). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank the members of the Health and Human Performance Laboratory at Carnegie Mellon University for all their help and support in conducting this work on mindfulness interventions.
Abbreviations:
- RCT
randomized controlled trial
- MBSR
Mindfulness-Based Stress Reduction
- MBCT
Mindfulness-Based Cognitive Therapy
- MBRP
Mindfulness-Based Relapse Prevention
- TAU
Treatment-As-Usual
- IBS
Irritable bowel syndrome
- PTSD
Post-Traumatic Stress Disorder
- CRP
C Reactive Protein
- IL-6
Interleukin-6
- HPA
Hypothalamic pituitary adrenal
- MAT
Monitor and Acceptance Theory
- SAM
Sympathetic adrenal medullary
- CBT
Cognitive Behavioral Therapy
Footnotes
Conflict of Interest Disclosure: The authors declare no financial conflicts of interest but disclose that David Creswell’s lab received research funding from the mindfulness company Headspace for conducting a mindfulness training study in 2018.
There are multiple ways to operationalize relative treatment advantages, and while our discussion has focused on the overall magnitude of health improvements, it is important to note that this can also be measured via cost-effectiveness. Group-based MBSR may be more cost effective compared to individually-focused treatments (81).
This article is based on the Herbert E. Weiner Early Career Award Lecture presented by award recipient J. David Creswell on March 18, 2017, at the 75th Annual Scientific Meeting of the American Psychosomatic Society in Sevilla, Spain.
References
- 1.Bishop SR. What do we really know about mindfulness-based stress reduction? Psychosomatic Medicine. 2002;64:71–83. [DOI] [PubMed] [Google Scholar]
- 2.Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosomatic Medicine. 2003;65:571–81. [DOI] [PubMed] [Google Scholar]
- 3.Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, Urbanowski F, Harrington A, Bonus K, Sheridan JF. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic medicine. 2003;65:564–570. [DOI] [PubMed] [Google Scholar]
- 4.Kabat-Zinn J, Wheeler E, Light T, Skillings A, Scharf MJ, Cropley TG, Hosmer D, Bernhard JD. Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA). Psychosomatic Medicine. 1998;60:625–632. [DOI] [PubMed] [Google Scholar]
- 5.Creswell JD. Mindfulness Interventions. Annual Review of Psychology. 2017;68:491–516. [DOI] [PubMed] [Google Scholar]
- 6.Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. The Journal of the American Medical Association. 2008;300:1350–52. [DOI] [PubMed] [Google Scholar]
- 7.Kuyken W, Warren FC, Taylor RS, Whalley B, Crane C, Bondolfi G, Hayes R, Huijbers M, Ma H, Schweizer S, Segal Z, Speckens A, Teasdale JD, Van Heeringen K, Williams M, Byford S, Byng R, Dalgleish T. Efficacy of Mindfulness-Based Cognitive Therapy in Prevention of Depressive Relapse: An Individual Patient Data Meta-analysis From Randomized Trials. JAMA Psychiatry. 2016;73:565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Segal ZV, Abbey S, Speca M, Velting D, Devins G. Mindfulness: A Proposed Operational Definition. Clinical Psychology: Science and Practice. 2004;11:230–241. [Google Scholar]
- 9.Brown KW, Ryan RM, Creswell JD. Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry. 2007;18:211–237. [Google Scholar]
- 10.Quaglia JT, Brown KW, Lindsay EK, Creswell JD, Goodman RJ. From conceptualization to operationalization of mindfulness In: Handbook of Mindfulness: New York: Guilford Press; 2014. [Google Scholar]
- 11.Kabat-Zinn J Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Delta; 1990. [Google Scholar]
- 12.Lindsay EK, Creswell JD. Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clinical Psychology Review. 2017;51:48–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kabat-Zinn J An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry. 1982;4:33–47. [DOI] [PubMed] [Google Scholar]
- 14.Creswell JD, Taren AA, Lindsay EK, Greco CM, Gianaros PJ, Fairgrieve A, Marsland AL, Brown KW, Way BM, Rosen RK. Alterations in resting-state functional connectivity link mindfulness meditation with reduced interleukin-6: a randomized controlled trial. Biological psychiatry. 2016;80:53–61. [DOI] [PubMed] [Google Scholar]
- 15.Epel ES, Puterman E, Lin J, Blackburn EH, Lum PY, Beckmann ND, Zhu J, Lee E, Gilbert A, Rissman RA, Tanzi RE, Schadt EE. Meditation and vacation effects have an impact on disease-associated molecular phenotypes. Translational Psychiatry. 2016;6:e880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lindsay EK, Young S, Smyth JM, Brown KW, Creswell JD. Acceptance lowers stress reactivity: Dismantling mindfulness training in a randomized controlled trial. Psychoneuroendocrinology. 2018;87:63–73. [DOI] [PubMed] [Google Scholar]
- 17.Zeidan F, Emerson NM, Farris SR, Ray JN, Jung Y, McHaffie JG, Coghill RC. Mindfulness Meditation-Based Pain Relief Employs Different Neural Mechanisms Than Placebo and Sham Mindfulness Meditation-Induced Analgesia. Journal of Neuroscience. 2015;35:15307–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Freedland KE. Demanding Attention: Reconsidering the Role of Attention Control Groups in Behavioral Intervention Research. Psychosomatic Medicine. 2013;75:100–102. [DOI] [PubMed] [Google Scholar]
- 19.Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, Berger Z, Sleicher D, Maron DD, Shihab HM, Ranasinghe PD, Linn S, Saha S, Bass EB, Haythornthwaite JA. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Internal Medicine. 2014;174:357–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Black DS, Slavich GM. Mindfulness meditation and the immune system: a systematic review of randomized controlled trials. Annals of the New York Academy of Sciences. 2016;1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ, Hansen KE, Turner JA. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA. 2016;315:1240–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garland EL, Manusov EG, Froeliger B, Kelly A, Williams JM, Howard MO. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: Results from an early-stage randomized controlled trial. Journal of Consulting and Clinical Psychology. 2014;82:448–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morone NE, Greco CM, Moore CG, Rollman BL, Lane B, Morrow LA, Glynn NW, Weiner DK. A mind-body program for older adults with chronic low back pain: A randomized clinical trial. JAMA Internal Medicine. 2016;176:329–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davis MC, Zautra AJ, Wolf LD, Tennen H, Yeung EW. Mindfulness and cognitive–behavioral interventions for chronic pain: Differential effects on daily pain reactivity and stress reactivity. Journal of Consulting and Clinical Psychology. 2015;83:24–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Gordon W, Shonin E, Dunn TJ, Garcia-Campayo J, Griffiths MD. Meditation awareness training for the treatment of fibromyalgia syndrome: A randomized controlled trial. British Journal of Health Psychology. 2017;22:186–206. [DOI] [PubMed] [Google Scholar]
- 26.Schmidt S, Grossman P, Schwarzer B, Jena S, Naumann J, Walach H. Treating fibromyalgia with mindfulness-based stress reduction: Results from a 3-armed randomized controlled trial. PAIN®. 2011;152:361–69. [DOI] [PubMed] [Google Scholar]
- 27.Polusny MA, Erbes CR, Thuras P, Moran A, Lamberty GJ, Collins RC, Rodman JL, Lim KO. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: A randomized clinical trial. JAMA. 2015;314:456–65. [DOI] [PubMed] [Google Scholar]
- 28.Barrett B, Hayney MS, Muller D, Rakel D, Ward A, Obasi CN, Brown R, Zhang Z, Zgierska A, Gern J, West R, Ewers T, Barlow S, Gassman M, Coe CL. Meditation or Exercise for Preventing Acute Respiratory Infection: A Randomized Controlled Trial. The Annals of Family Medicine. 2012;10:337–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garland EL, Gaylord SA, Palsson O, Faurot K, Douglas Mann J, Whitehead WE. Therapeutic mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity, catastrophizing, and affective processing of pain sensations. Journal of Behavioral Medicine. 2012;35:591–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zernicke KA, Campbell TS, Blustein PK, Fung TS, Johnson JA, Bacon SL, Carlson LE. Mindfulness-Based Stress Reduction for the Treatment of Irritable Bowel Syndrome Symptoms: A Randomized Wait-list Controlled Trial. International Journal of Behavioral Medicine. 2013;20:385–96. [DOI] [PubMed] [Google Scholar]
- 31.Creswell JD, Myers HF, Cole SW, Irwin MR. Mindfulness meditation training effects on CD4+ T lymphocytes in HIV-1 infected adults: A small randomized controlled trial. Brain Behavior and Immunity. 2009;23:184–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gonzalez-Garcia M, Ferrer MJ, Borras X, Muñoz-Moreno JA, Miranda C, Puig J, Perez-Alvarez N, Soler J, Feliu-Soler A, Clotet B, Fumaz CR. Effectiveness of Mindfulness-Based Cognitive Therapy on the Quality of Life, Emotional Status, and CD4 Cell Count of Patients Aging with HIV Infection. AIDS and Behavior. 2013;18:676–85. [DOI] [PubMed] [Google Scholar]
- 33.SeyedAlinaghi S, Jam S, Foroughi M, Imani A, Mohraz M, Djavid GE, Black DS. Randomized Controlled Trial of Mindfulness-Based Stress Reduction Delivered to Human Immunodeficiency Virus–Positive Patients in Iran: Effects on CD4+ T Lymphocyte Count and Medical and Psychological Symptoms. Psychosomatic Medicine. 2012;74:620–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McCune JM. The dynamics of CD4+ T-cell depletion in HIV disease. Nature. 2001;410:974–79. [DOI] [PubMed] [Google Scholar]
- 35.Creswell JD, Lindsay EK. How does mindfulness training affect health? A mindfulness stress buffering account. Current Directions in Psychological Science. 2014;23:401–7. [Google Scholar]
- 36.Hecht FM, Moskowitz JT, Moran P, Epel ES, Bacchetti P, Acree M, Kemeny ME, Mendes WB, Duncan LG, Weng H, Levy JA, Deeks SG, Folkman S. A Randomized, Controlled Trial of Mindfulness-Based Stress Reduction in HIV Infection. Brain, Behavior, and Immunity [Internet]. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Creswell JD, Irwin MR, Burklund LJ, Lieberman MD, Arevalo JMG, Ma J, Breen EC, Cole SW. Mindfulness-Based Stress Reduction training reduces loneliness and pro-inflammatory gene expression in older adults: A small randomized controlled trial. Brain, Behavior, and Immunity. 2012;26:1095–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jedel S, Hoffman A, Merriman P, Swanson B, Voigt R, Rajan KB, Shaikh M, Li H, Keshavarzian A. A Randomized Controlled Trial of Mindfulness-Based Stress Reduction to Prevent Flare-Up in Patients with Inactive Ulcerative Colitis. Digestion. 2014;89:142–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Malarkey WB, Jarjoura D, Klatt M. Workplace based mindfulness practice and inflammation: A randomized trial. Brain, Behavior, and Immunity. 2013;27:145–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bower JE, Crosswell AD, Stanton AL, Crespi CM, Winston D, Arevalo J, Ma J, Cole SW, Ganz PA. Mindfulness meditation for younger breast cancer survivors: A randomized controlled trial: Mindfulness for Young Cancer Survivors. Cancer. 2015;121:1231–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fogarty FA, Booth RJ, Gamble GD, Dalbeth N, Consedine NS. The effect of mindfulness-based stress reduction on disease activity in people with rheumatoid arthritis: a randomised controlled trial. Annals of the Rheumatic Diseases. 2015;74:472–74. [DOI] [PubMed] [Google Scholar]
- 42.Rosenkranz MA, Davidson RJ, MacCoon DG, Sheridan JF, Kalin NH, Lutz A. A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation. Brain, Behavior, and Immunity. 2013;27C:174–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Creswell JD. Biological pathways linking mindfulness with health In: Handbook of Mindfulness: Theory, Research, and Practice. New York, NY: Guilford Press; 2014. [Google Scholar]
- 44.Erickson KI, Creswell JD, Verstynen TD, Gianaros PJ. Health Neuroscience: Defining a New Field. Current Directions in Psychological Science. 2014;23:446–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. Journal of the American Medical Association. 2007;298:1685–87. [DOI] [PubMed] [Google Scholar]
- 46.Lindsay EK, Creswell JD. Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clinical Psychology Review. 2017. p. 48–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brewer JA, Worhunsky PD, Gray JR, Tang Y-Y, Weber J, Kober H. Meditation experience is associated with differences in default mode network activity and connectivity. Proceedings of the National Academy of Sciences. 2011;108:20254–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.King AP, Erickson TM, Giardino ND, Favorite T, Rauch SAM, Robinson E, Kulkarni M, Liberzon I. A Pilot Study of Group Mindfulness-Based Cognitive Therapy (mbct) for Combat Veterans with Posttraumatic Stress Disorder (ptsd). Depression and Anxiety. 2013;30:638–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Taren AA, Gianaros PJ, Greco CM, Lindsay EK, Fairgrieve A, Brown KW, Rosen RK, Ferris JL, Julson E, Marsland AL, Creswell JD. Mindfulness meditation training and executive control network resting state functional connectivity: A randomized controlled trial. Psychosomatic Medicine. 2017;79:674–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ulrich-Lai YM, Herman JP. Neural regulation of endocrine and autonomic stress responses. Nature Reviews Neuroscience. 2009;10:397–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Arnsten AFT. Stress signalling pathways that impair prefrontal cortex structure and function. Nature Reviews Neuroscience. 2009;10:410–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hölzel BK, Carmody J, Evans KC, Hoge EA, Dusek JA, Morgan L, Pitman RK, Lazar SW. Stress reduction correlates with structural changes in the amygdala. Social Cognitive and Affective Neuroscience. 2010;5:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taren AA, Gianaros PJ, Greco CM, Lindsay EK, Fairgrieve A, Brown KW, Rosen RK, Ferris JL, Julson E, Marsland AL, Bursley JK, Ramsburg J, Creswell JD. Mindfulness meditation training alters stress-related amygdala resting state functional connectivity: a randomized controlled trial. Social Cognitive and Affective Neuroscience. 2015;10:1758–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Taren AA, Creswell JD, Gianaros PJ. Dispositional Mindfulness Co-Varies with Smaller Amygdala and Caudate Volumes in Community Adults. PLoS ONE. 2013;8:e64574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Way BM, Creswell JD, Eisenberger NI, Lieberman MD. Dispositional mindfulness and depressive symptomatology: Correlations with limbic and self-referential neural activity during rest. Emotion. 2010;10:12–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nyklíček I, Van Beugen S, Van Boxtel GJ. Mindfulness-Based Stress Reduction and Physiological Activity During Acute Stress: A Randomized Controlled Trial. Health Psychology. 2013;32:1110–13. [DOI] [PubMed] [Google Scholar]
- 57.Creswell JD, Pacilio LE, Lindsay EK, Brown KW. Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology. 2014;44:1–12. [DOI] [PubMed] [Google Scholar]
- 58.Weinstein N, Brown KW, Ryan RM. A multi-method examination of the effects of mindfulness on stress attribution, coping, and emotional well-being. Journal of Research in Personality. 2009;43:374–85. [Google Scholar]
- 59.Cohen S, Lichtenstein E. Perceived stress, quitting smoking, and smoking relapse. Health Psychology. 1990;9:466. [DOI] [PubMed] [Google Scholar]
- 60.Ng DM, Jeffery RW. Relationships Between Perceived Stress and Health Behaviors in a Sample of Working Adults. Health Psychology. 2003;22:638–42. [DOI] [PubMed] [Google Scholar]
- 61.Groesz LM, McCoy S, Carl J, Saslow L, Stewart J, Adler N, Laraia B, Epel E. What is eating you? Stress and the drive to eat. Appetite. 2012;58:717–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Becker NB, De Jesus SN, Marguilho R, Viseu J, Del Rio KA, Buela-Casal G. Sleep quality and stress: A literature review In: Advanced Research in Health, Education and Social Sciences: Towards a better practice. Sibiu, Romania: Editura Universitară; 2015. [Google Scholar]
- 63.Brewer JA, Mallik S, Babuscio TA, Nich C, Johnson HE, Deleone CM, Minnix-Cotton CA, Byrne SA, Kober H, Weinstein AJ, Carroll KM, Rounsaville BJ. Mindfulness training for smoking cessation: Results from a randomized controlled trial. Drug & Alcohol Dependence. 2011;119:72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, Carroll HA, Harrop E, Collins SE, Lustyk K, Larimer ME. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry. 2014;71:547–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li W, Howard MO, Garland EL, McGovern P, Lazar M. Mindfulness treatment for substance misuse: A systematic review and meta-analysis. Journal of Substance Abuse Treatment. 2017;75:62–96. [DOI] [PubMed] [Google Scholar]
- 66.O’Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: a literature review: Mindfulness interventions for eating behaviours. Obesity Reviews. 2014;15:453–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mason AE, Epel ES, Aschbacher K, Lustig RH, Acree M, Kristeller J, Cohn M, Dallman M, Moran PJ, Bacchetti P, Laraia B, Hecht FM, Daubenmier J. Reduced reward-driven eating accounts for the impact of a mindfulness-based diet and exercise intervention on weight loss: Data from the SHINE randomized controlled trial. Appetite. 2016;100:86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mason AE, Epel ES, Kristeller J, Moran PJ, Dallman M, Lustig RH, Acree M, Bacchetti P, Laraia BA, Hecht FM, Daubenmier J. Effects of a mindfulness-based intervention on mindful eating, sweets consumption, and fasting glucose levels in obese adults: data from the SHINE randomized controlled trial. Journal of Behavioral Medicine. 2015;1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Black DS, O’Reilly GA, Olmstead R, Breen EC, Irwin MR. Mindfulness Meditation and Improvement in Sleep Quality and Daytime Impairment Among Older Adults With Sleep Disturbances: A Randomized Clinical Trial. JAMA Internal Medicine. 2015;175:494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Garland SN, Carlson LE, Stephens AJ, Antle MC, Samuels C, Campbell TS. Mindfulness-Based Stress Reduction Compared With Cognitive Behavioral Therapy for the Treatment of Insomnia Comorbid With Cancer: A Randomized, Partially Blinded, Noninferiority Trial. Journal of Clinical Oncology. 2014;32:1–9. [DOI] [PubMed] [Google Scholar]
- 71.Britton WB, Haynes PL, Fridel KW, Bootzin RR. Polysomnographic and Subjective Profiles of Sleep Continuity Before and After Mindfulness-Based Cognitive Therapy in Partially Remitted Depression: Psychosomatic Medicine. 2010;72:539–48. [DOI] [PubMed] [Google Scholar]
- 72.Bernstein A, Hadash Y, Lichtash Y, Tanay G, Shepherd K, Fresco DM. Decentering and Related Constructs A Critical Review and Metacognitive Processes Model. Perspectives on Psychological Science. 2015;10:599–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspectives on Psychological Science. 2011;6:537–59. [DOI] [PubMed] [Google Scholar]
- 74.Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. Journal of Clinical Psychology. 2006;62:373–86. [DOI] [PubMed] [Google Scholar]
- 75.Vago DR, Silbersweig DA. Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Frontiers in Human Neuroscience. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Loucks EB, Schuman-Olivier Z, Britton WB, Fresco DM, Desbordes G, Brewer JA, Fulwiler C. Mindfulness and Cardiovascular Disease Risk: State of the Evidence, Plausible Mechanisms, and Theoretical Framework. Current Cardiology Reports. 2015;17:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review. 2015;37:1–12. [DOI] [PubMed] [Google Scholar]
- 78.Quaglia JT, Braun SE, Freeman SP, McDaniel MA, Brown KW. Meta-analytic evidence for effects of mindfulness training on dimensions of self-reported dispositional mindfulness. Psychological Assessment. 2016;28:803. [DOI] [PubMed] [Google Scholar]
- 79.Engert V, Kok BE, Papassotiriou I, Chrousos GP, Singer T. Specific reduction in cortisol stress reactivity after social but not attention-based mental training. Science Advances. 2017;3:e1700495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Carlson LE, Doll R, Stephen J, Faris P, Tamagawa R, Drysdale E, Speca M. Randomized Controlled Trial of Mindfulness-Based Cancer Recovery Versus Supportive Expressive Group Therapy for Distressed Survivors of Breast Cancer (MINDSET). Journal of Clinical Oncology. 2013;31:3119–26. [DOI] [PubMed] [Google Scholar]
- 81.Cherkin DC, Herman PM. Cognitive and Mind-Body Therapies for Chronic Low Back Pain and Neck Pain: Effectiveness and Value. JAMA Internal Medicine. [DOI] [PubMed] [Google Scholar]
- 82.Sevinc G, Hölzel BK, Hashmi J, Greenberg J, McCallister A, Treadway M, Schneider ML, Dusek JA, Carmody J, Lazar SW. Common and Dissociable Neural Activity After Mindfulness-Based Stress Reduction and Relaxation Response Programs. Psychosomatic Medicine. 2018;80:439–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Britton WB, Davis JH, Loucks EB, Peterson B, Cullen BH, Reuter L, Rando A, Rahrig H, Lipsky J, Lindahl JR. Dismantling Mindfulness-Based Cognitive Therapy: Creation and validation of 8-week focused attention and open monitoring interventions within a 3-armed randomized controlled trial. Behaviour Research and Therapy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Geschwind N, Peeters F, Drukker M, van Os J, Wichers M. Mindfulness training increases momentary positive emotions and reward experience in adults vulnerable to depression: a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2011;79:618. [DOI] [PubMed] [Google Scholar]
- 85.Lindsay EK, Chin B, Greco CM, Young S, Brown KW, Wright AGC, Smyth JS, Burkett D, Creswell JD. How mindfulness training promotes positive emotions: Dismantling monitor and acceptance in two randomized controlled trials. Journal of Personality and Social Psychology. in press; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Carson JW, Carson KM, Gil KM, Baucom DH. Mindfulness-based relationship enhancement. Behavior Therapy. 2004;35:471–494. [Google Scholar]
- 87.Lim D, Condon P, DeSteno D. Mindfulness and Compassion: An Examination of Mechanism and Scalability. PLoS ONE. 2015;10:e0118221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cohen S Social relationships and health. American psychologist. 2004;59:676. [DOI] [PubMed] [Google Scholar]
- 89.Pressman SD, Cohen S. Does positive affect influence health? Psychological bulletin. 2005;131:925. [DOI] [PubMed] [Google Scholar]
- 90.Schumer MC, Lindsay EK, Creswell JD. Brief mindfulness for negative affectivity: a systematic review and meta-analysis. Journal of Consulting and Clinical Psychology. in press; [DOI] [PMC free article] [PubMed] [Google Scholar]