Abstract
A systematic method was used to review the existing epidemiologic literature and determine the state of the scientific evidence for potential adverse health outcomes in populations living near oil and natural gas (ONG) operations in the United States. The review utilized adapted systematic review frameworks from the medical and environmental health fields, such as Grading of Recommendations, Assessment, Development and Evaluations (GRADE), the Navigation Guide, and guidance from the National Toxicology Program’s Office of Health Assessment and Translation (OHAT). The review included 20 epidemiologic studies, with 32 different health outcomes. Studies of populations living near ONG operations provide limited evidence (modest scientific findings that support the outcome, but with significant limitations) of harmful health effects including asthma exacerbations and various self-reported symptoms. Study quality has improved over time and the highest rated studies within this assessment have primarily focused on birth outcomes. Additional high-quality studies are needed to confirm or dispute these correlations.
Keywords: oil and natural gas, hydraulic fracturing, fracking, unconventional oil and gas, environmental health, epidemiology, systematic literature review
1. Introduction
The United States has significantly increased its capacity for oil and natural gas (ONG) development through the technological advancements of directional drilling and hydraulic fracturing, with natural gas production reaching a high in 2017 and 2018 [1]. In 2016, more than two-thirds of the 977,000 producing ONG wells in the U.S. used these technologies to access energy reserves in shale and tight oil sands [2]. In places like the Colorado Front Range and Dallas-Fort Worth, Texas, ONG operations are occurring directly alongside population growth. It is estimated that 17.6 million people in the U.S. live within 1 mile of an active ONG well [3].
There currently exists limited research and conflicting scientific information on the health risks for those living next to these operations. The industry surrounding ONG expanded faster than evidence-based epidemiologic research could respond [4,5]. Early community health assessments and surveys of health symptoms in people living near ONG operations raised concerns about the potential chemical hazards, including exposures to air and water pollution [6,7,8]. Additional studies pointed to non-chemical stressors, including psychosocial stress, from living near ONG operations [9,10,11]. These early hypothesis-generating studies gave way to a growing body of observational epidemiologic literature that has quantified associations between residential proximity to ONG operations and the potential for certain adverse human health effects. Several review articles published within the last five years summarize this literature [5,12,13,14].
Our study is the first of its kind to systematically review the entirety of existing epidemiologic literature on the associations between living near ONG development and the potential for harmful health effects. We weigh the level of evidence for each health outcome and aim to present a clear assessment of the methodological rigor, study strengths, and weaknesses, to identify approaches to future research. The scholarship published to date varies in the types of ONG operations studied, the populations of interest (e.g., based on their geography, time period, or demographic characteristics), the health outcomes measured, and the quality of the methods used. While Saunders and colleagues do raise important methodological concerns about many of the articles they review [14], no existing review addresses study quality in a systematic way. In research on the health effects of potential environmental contaminants, where randomized controlled trials are neither ethical nor appropriate, study quality, or certainty in the study aligning with its stated objectives, is integral to interpreting scientific results and extrapolating them for regulatory and other science-based decisions.
The need for public health scientists to systematically evaluate the body of a literature base for an important issue, with limited resources, is necessary to assist in science-based regulatory decision making. Often, these issues are not entirely characterized and may include multiple chemical stressors (which are typically unknown) and variable health outcomes. The current established systematic review frameworks focus on an in-depth evaluation of the toxicological and epidemiological literature for a specific chemical and/or health outcome, however, this approach is unable to be applied directly to the epidemiological literature surrounding ONG development. Therefore, we have adapted these approaches to better answer this environmental health question.
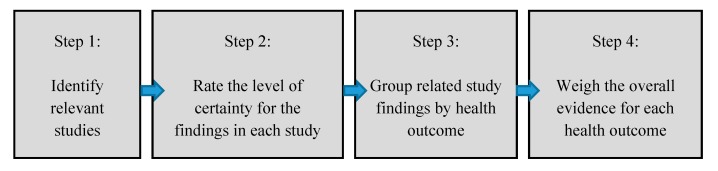
The steps used to conduct the review were adapted from various established systematic review frameworks for the medical and public health fields, including as Grading of Recommendations, Assessment, Development and Evaluations (GRADE) [15] and Meta-analyses Of Observational Studies in Epidemiology (MOOSE for observational studies) [16], and emerging methods in environmental health as outlined by the Navigation Guide [17], and Office of Health Assessment and Translation (OHAT) [18] guidance (Figure 1). Each study was evaluated using 14 study evaluation questions to assess the level of certainty in, or scientific plausibility of, the study findings. The overall weight of evidence was determined for each health outcome separately. This review is not intended to replicate any previous frameworks nor is it to be the single word on study quality in this area of research. Our aim is to be objective and transparent, in a way that can be understood by community members, government and non-government public health and environmental officials and policymakers.
Figure 1.
Steps in the current systematic review of epidemiologic literature.
2. Materials and Methods
2.1. Scope of Analysis
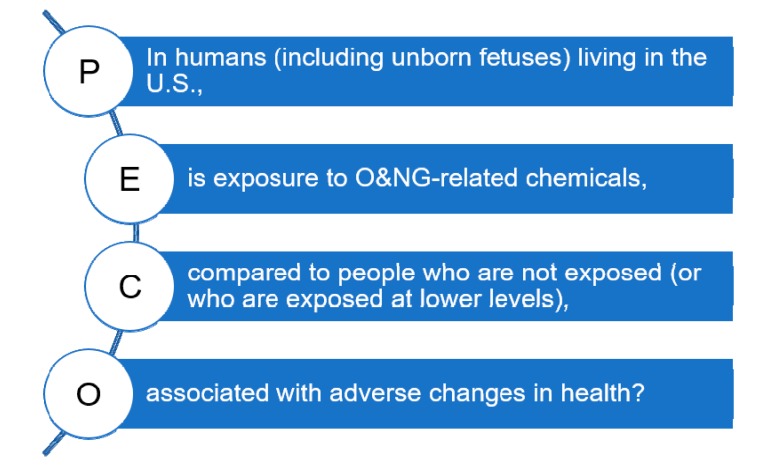
The scope of this literature review is defined by a PECO (populations, exposures, comparators, and outcomes) question [19]: “In humans (including unborn fetuses) living in the U.S., is exposure to chemicals emitted from ONG operations, compared to people who are not exposed (or who are exposed at lower levels), associated with adverse changes in health?” (Figure 2). Unborn fetuses were included as a population of interest to account for the possibility of ONG activities affecting fetal development within the mother’s womb. The term “oil and natural gas operations” (or development) was defined to include all upstream processes involved in the extraction of ONG resources using any combination of vertical drilling, directional/horizontal drilling, and hydraulic fracturing to access energy reserves from conventional and unconventional geologic formations. This review does not include studies evaluating mid- and downstream processes. Since October 2011, the majority of new ONG wells in the U.S. overall have been hydraulically fractured horizontal wells, typically referred to as unconventional wells [2]. Study authors will often use a variety of these terms, and the distinction between conventional and unconventional wells—in source rock, depth, or drilling technique—is muddled in practice [20]. We sought to look across a range of comparators since exposures to ONG-associated chemicals occur along a continuum and it may not always be clear what the pathway of exposure is, how far that pathway reaches, or whether multiple exposure pathways produce synergistic effects on health [5,19]. We then considered whether any and all adverse changes in health occur with these exposures. While it is plausible that ONG may impact health through indirect pathways such as income (e.g., from monetary gains from leasing land or mineral rights), or investment in community infrastructure such as healthcare services [10,21,22], indirect effects were not included in this paper.
Figure 2.
Populations, exposures, comparators, and outcomes (PECO) statement.
The PECO question informed our exclusion criteria and studies were excluded if one or more of the following five criteria were met: (1) exposure to ONG chemicals was not directly measured in, or estimated for, study subjects (i.e., excluded studies focused on indirect health effects including community stressors such as degradation of rural life, sexually transmitted infections from newly arrived young male workers, and traffic accidents from increased heavy truck traffic); (2) the study failed to quantify associations between exposures and a specific health outcome (i.e., excluded studies did not measure odds ratios, relative risk, etc.); (3) the study did not include original data or observations (e.g., review articles, commentaries); (4) the study did not define ONG operations to include any or all processes associated with the upstream development and production of ONG, including but not limited to horizontal drilling and hydraulic fracturing; or (5) the study did not take place in the U.S.
2.2. Data Search
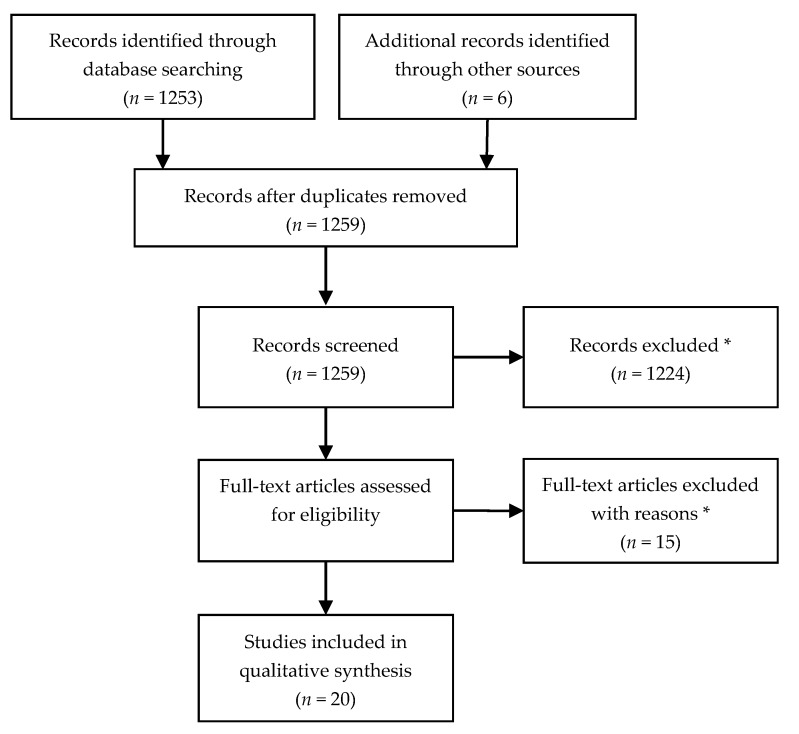
PubMed was the primary research database used to obtain articles. We identified relevant records using the following PubMed search terms: ((“Oil and Gas Industry”[Mesh] OR “Natural Gas”[Mesh]) AND (epidemiolog* or symptom*)) OR ((oil OR natural gas) AND (epidemiolog* OR health OR symptom*) AND (unconventional OR drilling OR shale OR coal OR production OR development) NOT (“Occupational Health”[Mesh] OR “Animal Experimentation”[Mesh]) AND (“2013/01/01”[PDAT]: “2018/10/01”[PDAT])) AND Humans[Mesh]. We verified that no relevant study was published before 2013, and any studies published after our search date of October 1, 2018 were not included in the assessment. In total, 1253 articles were returned by the search and all were screened for eligibility (Figure 3). Review articles, risk assessments, and included studies were also screened for references and identified six additional studies. The majority of articles (98%) did not meet our study inclusion criteria because they were related to the fields of environmental engineering, geology, hydrology or biomedical topics such as plant-based oil extracts/lipids. We kept the search terms broad in an effort to capture the wide variety of terminology that has been used within the interdisciplinary ONG health effects field.
Figure 3.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for study inclusion. * Exclusion criteria is detailed within the methods.
2.3. Level of Certainty Rating and Level of Evidence Conclusions for Individual Studies
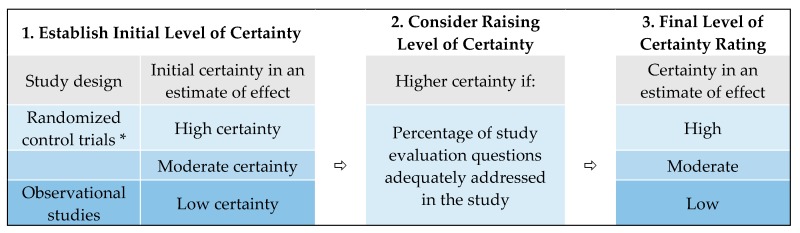
A modified systematic review framework was used to rate the level of certainty (or the certainty in an estimate of effect) for each health outcome (Figure 4). We developed our framework based on established methods of systematic reviews for the medical, public health and environmental health fields. These frameworks incorporate, either explicitly or implicitly, most of Bradford Hill’s criteria for causation such as studies with specificity and biological plausibility and that were temporal and consistent [23]. We consulted these classic criteria to develop a meaningful scope of review (as reflected in the PECO question) and determine criteria for study certainty and weight of evidence [24].
Figure 4.
The approach used for developing level of certainty ratings for each study outcome. * No randomized control trials were identified in this review.
We rated study findings as having low, moderate, or high certainty that the estimated effect was close to that of the true effect. The findings of observational epidemiologic studies were initially ranked as low certainty and were upgraded according to fourteen (14) study evaluation questions that assessed various domains (Table 1). These criteria were based on established frameworks which specify the domains, questions, or study limitations used to evaluate individual studies for use in a systematic review [17,18,25,26,27]. We categorized the study evaluation questions into five groups: population and sample, exposure, health outcomes, confounders, and reporting. Two or more authors reviewed each study evaluation question with a yes-or-no response for each study (Supplementary Tables S1–S20). Conflicting responses were resolved through discussion and additional review of the study. Studies with greater than 50% “yes” answers (i.e., 8 “yes” answers out of 14) were considered for potential upgrade of their findings to moderate certainty; studies with greater than 75% “yes” answers (i.e., 11 “yes” answers out of 14) were considered for potential upgrade to high certainty [28]. All findings of each study were ascribed the same level of certainty after evaluations were complete.
Table 1.
Key study evaluation questions to determine the level of certainty ratings for health outcomes.
| Study Evaluation Questions |
|---|
| Population and Sample |
| 1. Does the control group match the exposed group? |
| 2. Is the sample generalizable to the population of interest? |
| 3. Did the study a priori quantify sample and power? |
| 4. Were missing data addressed and tested? |
| Exposure |
| 5. Was exposure directly measured and quantified? |
| 6. Was the exposure or proxy/surrogate of exposure measured from a point location? |
| 7. Does the proxy/surrogate adequately estimate exposure? |
| 8. Was there a temporal relationship between exposure and outcome? |
| Health Outcomes |
| 9. Was the health outcome determined by a medical provider? |
| 10. Was a dose-response relationship seen in any outcome? |
| Confounders |
| 11. Did the study design or analysis account for important confounding and modifying variables? |
| 12. Did the study design or analysis adjust or control for other environmental exposures that were anticipated to bias results? |
| 13. Were sensitivity analyses attempted for population, outcome, or exposure? |
| Reporting |
| 14. Did the study conclusions match the results? |
| Final level of certainty rating: Low/Moderate/High |
We derived weight-of-evidence conclusions using standards outlined in GRADE [29], the Cochrane Handbook [30], and developed by the Institute of Medicine [31]. For each health outcome, relevant findings from individual studies were grouped and evaluated to derive one of the following weight-of-evidence levels: substantial, moderate, limited, mixed, failing to show an association, or insufficient (Table 2).
Table 2.
Weight-of-evidence determinations.
| Evidence Level | Definition |
|---|---|
| Substantial | Strong scientific findings that support an association between oil and gas exposure and the outcome, with no credible opposing scientific evidence. |
| Moderate | Strong scientific findings that support an association between oil and gas exposure and the outcome, but these findings have some limitations. |
| Limited | Modest scientific findings that support an association between oil and gas exposure and the outcome, but these findings have significant limitations. |
| Mixed | Both supporting and opposing scientific findings for an association between oil and gas exposure and the outcome, with neither direction dominating. |
| Failing to show an association | Body of research failing to show an association—indicates that the topic has been researched without evidence of an association; is further classified as a limited, moderate or substantial body of research failing to show an association. |
| Insufficient | The outcome has not been sufficiently studied. |
3. Results
Twenty (20) studies met our criteria of a human health epidemiologic study evaluating the potential health effects associated with living near ONG operations in the United States (Table 3, Supplementary Table S21). Weight-of-evidence conclusions were developed for a total of 32 different health effects, and ranged from insufficient evidence to limited evidence (Table 4).
Table 3.
Summary details of epidemiologic studies included in this systematic review.
| First Author | Year | Title | Publication | State | Study Type | Health Finding Category | Positive Associations | Null Associations | Level of Certainty |
|---|---|---|---|---|---|---|---|---|---|
| Busby [34] | 2017 | There’s a World Going on Underground—Infant Mortality and Fracking in Pennsylvania | Journal of Environmental Protection | Pennsylvania | Ecological | Birth outcomes | Early infant mortality | NA | Low (3) |
| Casey [35] | 2016 | Unconventional Natural Gas Development and Birth Outcomes in Pennsylvania, USA | Epidemiology | Pennsylvania | Retrospective cohort | Birth outcomes | Preterm birth and high-risk pregnancy a | Apgar score, small for gestational age, term birth weight | Moderate (9) |
| Casey [60] | 2018 | Associations of Unconventional Natural Gas Development with Depression Symptoms and Disordered Sleep in Pennsylvania | Scientific Reports | Pennsylvania | Case-control and cross-sectional | Self-reported symptoms and diagnoses | Depression symptoms (self-reported) | Disordered sleep (diagnoses) | Low (6) |
| Currie [36] | 2017 | Hydraulic Fracturing and Infant Health: New Evidence from Pennsylvania | Science Advances | Pennsylvania | Retrospective cohort | Birth outcomes | Low birth weight, decreased birth weight, decreased score on infant health index | NA | Low (5) |
| Elliott [52] | 2018 | A Community-based Evaluation of Proximity to Unconventional Oil and Gas Wells, Drinking Water Contaminants, and Health Symptoms in Ohio | Cross-sectional | Ohio | Cross-sectional | Self-reported symptoms | General symptoms (stress, fatigue, muscle or joint pain, any other self-reported health symptoms) | Respiratory, neurological b, dermal, gastrointestinal symptoms (self-reported) | Low (6) |
| Finkel [46] | 2016 | Shale Gas Development and Cancer Incidence in Southwest Pennsylvania | Public Health | Pennsylvania | Ecological | Cancer | Urinary bladder cancer | Thyroid cancer, leukemia | Low (2) |
| Fryzek [47] | 2013 | Childhood Cancer Incidence in Pennsylvania Counties in Relation to Living in Counties with Hydraulic Fracturing Sites | Journal of Environmental Medicine | Pennsylvania | Ecological | Cancer (child) | Central nervous system tumors | All childhood cancer incidence and leukemia | Low (2) |
| Hill [37] | 2018 | Unconventional Natural Gas Development and Infant Health: Evidence from Pennsylvania | Journal of Health Economics | Pennsylvania | Retrospective cohort | Birth outcomes | Low birth weight, decreased term birth weight, premature birth small for gestational age, Apgar score less than 8 | Gestation periods | Moderate (9) |
| Jemielita [53] | 2015 | Unconventional Gas and Oil Drilling is Associated with Increased Hospital Utilization Rates | PLOS ONE | Pennsylvania | Ecological | Hospitalizations | Cardiology and neurology hospitalizations | Hospitalizations for various medical categories, including pulmonary hospitalizations | Low (7) |
| Ma [33] | 2016 | Time Series Evaluation of Birth Defects in Areas with and without Unconventional Natural Gas Development | Journal of Epidemiology and Public Health Reviews | Pennsylvania | Interrupted time series | Birth defects | NA | Birth defects prevalence | Low (5) |
| McKenzie [32] | 2014 | Birth Outcomes and Maternal Residential Proximity to Natural Gas Development in Rural Colorado | Environmental Health Perspectives | Colorado | Retrospective cohort | Birth outcomes and birth defects | Congenital heart defects and neural tube defects | Oral clefts, preterm birth +, term low birth weight +, decreased term birth weight + | Low (6) |
| McKenzie [48] | 2017 | Childhood Hematologic Cancer and Residential Proximity to Oil and Gas Development | PLOS ONE | Colorado | Case-control | Cancer (child) | Childhood acute lymphocytic leukemia | Childhood non-Hodgkin’s lymphoma | Low (8) |
| Peng [54] | 2018 | The Health Implications of Unconventional Natural Gas Development in Pennsylvania | Health Economics | Pennsylvania | Ecological | Hospitalizations | Pneumonia hospitalizations | Hospitalizations for acute myocardial infarction, chronic obstructive pulmonary disease (COPD), asthma, upper respiratory infections | Low (6) |
| Rabinowitz [55] | 2015 | Proximity to Natural Gas Wells and Reported Health Status: Results of a Household Survey in Washington County, Pennsylvania | Environmental Health Perspectives | Pennsylvania | Cross-sectional | Self-reported symptoms | Dermal and upper respiratory symptoms (self-reported) | Lower respiratory, cardiovascular, gastrointestinal, neurological symptoms (self-reported) | Low (7) |
| Rasmussen [56] | 2016 | Association Between Unconventional Natural Gas Development in the Marcellus Shale and Asthma Exacerbations | JAMA Intern Med. | Pennsylvania | Nested case-control | Respiratory diagnoses | Asthma exacerbations | NA | Moderate (8) |
| Stacy [38] | 2015 | Perinatal Outcomes and Unconventional Natural Gas Operations in Southwest Pennsylvania | PLOS ONE | Pennsylvania | Retrospective cohort | Birth outcomes | Decreased birth weight and small for gestational age | Premature birth+ | Moderate (8) |
| Steinzor [61] | 2013 | Investigating Links Between Shale Gas Development and Health Impacts Through a Community Survey Project in Pennsylvania | New Solutions | Pennsylvania | Cross-sectional | Self-reported symptoms | Throat irritation, sinus problems, nasal irritation, eye burning, persistent cough, frequent nose bleeds, loss of sense of smell, severe headaches, skin rashes, swollen painful joints symptoms (self-reported) | Joint pain, sleep disturbances, shortness of breath, forgetfulness, sleep disorders, feeling weak and tired, increased fatigue, lumbar pain, muscle aches or pain, diarrhea symptoms (self-reported) | Low (3) |
| Tustin [57] | 2016 | Associations between Unconventional Natural Gas Development and Nasal and Sinus, Migraine Headache, and Fatigue Symptoms in Pennsylvania | Environmental Health Perspectives | Pennsylvania | Cross-sectional | Self-reported symptoms | Chronic rhinosinusitis (CRS), migraine headache, and fatigue symptoms in combination (self-reported): CRS and fatigue, migraine headache and fatigue, and all three symptoms together | NA | Low (5) |
| Whitworth [39] | 2017 | Maternal Residential Proximity to Unconventional Gas Development and Perinatal Outcomes among a Diverse Urban Population in Texas | PLOS ONE | Texas | Retrospective cohort | Birth outcomes | Preterm birth and fetal death | Small for gestational age and term birth weight | Low (7) |
| Whitworth [40] | 2018 | Drilling and Production Activity Related to Unconventional Gas Development and Severity of Preterm Birth | Environmental Health Perspectives | Texas | Nested case-control | Birth outcomes | Preterm birth | NA | Low (9) |
NA = Not applicable (no result). + Denotes evidence of a significant negative relationship (i.e., with increasing exposure, poor health outcomes improved). a High risk pregnancy was an a priori conclusion and is not a direct effect and therefore was not included in a weight of evidence determination. b Elliot et al. defined the neurologic category to include symptoms of frequent headaches or migraines, dizziness or balance problems, feeling down, difficulties with concentration or memory, difficulty sleeping or insomnia, feeling anxious or nervous, and seizures. Some of these symptoms are traditionally categorized as psychological.
Table 4.
Summary of the overall weight-of-evidence determinations for each health outcome.
| Health Outcome Categories | Total Number of Studies | Health Outcomes | Reference | Number of Studies Per Certainty Rating | Weight of Evidence | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Positive Association | Null Association | |||||||||
| High | Moderate | Low | Low | Moderate | High | |||||
| Birth defects | 2 | Congenital heart defects | McKenzie [32] | 1 | Insufficient | |||||
| Oral clefts | McKenzie [32] | 1 | Insufficient | |||||||
| Neural tube defects | McKenzie [32] | 1 | Insufficient | |||||||
| Birth defects prevalence | Ma [33] | 1 | Insufficient | |||||||
| Birth outcomes | 8 | Decreased term birth weight or low birth weight | Casey [35]; Currie [36]; Hill [37]; McKenzie [32]; Stacy [38]; Whitworth [39] | 2 | 1 | 2 | 1 | Mixed | ||
| Early infant mortality | Busby [34] | 1 | Insufficient | |||||||
| Fetal death | Whitworth [39] | 1 | Insufficient | |||||||
| Gestation period | Hill [37] | 1 | Insufficient | |||||||
| Low infant health index | Currie [36] | 1 | Insufficient | |||||||
| Low APGAR score a | Casey [35]; Hill [37] | 1 | 1 | Mixed | ||||||
| Preterm/premature birth | Casey [35]; Hill [37]; McKenzie [32]; Stacy [38]; Whitworth [39,40] | 1 | 3 | 1 | 1 | Mixed | ||||
| Small for gestational age | Casey [35]; Hill [37]; Stacy [38]; Whitworth [39] | 2 | 1 | 1 | Mixed | |||||
| Cancer | 3 | Cancer incidence (childhood) | Fryzek [47] | 1 | Insufficient | |||||
| Leukemia (childhood non-specific and acute lymphocytic leukemia) | Fryzek [47]; McKenzie [48] | 1 | 1 | Mixed | ||||||
| Non-Hodgkin’s lymphoma (childhood) | McKenzie [48] | 1 | Insufficient | |||||||
| CNS tumorsb(child) | Fryzek [47] | 1 | Insufficient | |||||||
| Urinary bladder | Finkel [46] | 1 | Insufficient | |||||||
| Thyroid | Finkel [46] | 1 | Insufficient | |||||||
| Leukemia | Finkel [46] | 1 | Insufficient | |||||||
| Cardiovascular | 3 | Hospitalizations | Jemielita [53]; Peng [54] | 1 | 1 | Mixed | ||||
| Self-reported symptoms | Rabinowitz [55] | 1 | Insufficient | |||||||
| Dermal | 2 | Self-reported symptoms | Elliott [52]; Rabinowitz [55] | 1 | 1 | Mixed | ||||
| Gastrointestinal | 2 | Self-reported symptoms | Elliott [52]; Rabinowitz [55] | 2 | Limited- failing to show an association | |||||
| Neurological | 4 | Hospitalizations | Jemielita [53] | 1 | Insufficient | |||||
| Self-reported symptoms | Elliott [52]; Rabinowitz [55]; Tustin [57] | 3 | Limited- failing to show an association | |||||||
| Psychological | 2 | Self-reported symptoms | Casey [36]; Tustin [57] | 1 | 1 | Mixed | ||||
| Diagnosed sleep disturbances | Casey [36] | 1 | Insufficient | |||||||
| Respiratory | 6 | Self-reported symptoms | Elliott [52]; Rabinowitz [55]; Tustin [57] | 1 | 2 | Mixed | ||||
| Hospitalizations | Jemielita [53]; Peng [54] | 1 | 1 | Mixed | ||||||
| Asthma exacerbation | Rasmussen [56] | 1 | Limited | |||||||
| Other | 2 | Self-reported symptoms (multiple) | Elliott [52]; Tustin [57] | 2 | Limited | |||||
| Hospitalizations (all) | Jemielita [53] | 1 | Insufficient | |||||||
a APGAR score: Appearance, Pulse, Grimace, Activity and Respiration score. b CNS: Central Nervous System.
Across all health outcomes, four of the 20 studies received a moderate level of certainty rating. All others received a rating of low certainty. The majority of the studies were retrospective cohort (six studies) or ecological (six studies) study designs. There were five cross sectional studies, two nested case controls, and two case-controls. The average score across all studies was 6, with a score range from 2 to 9 (Supplementary Table S22).
3.1. Birth Defects and Birth Outcomes
This review identified nine studies comprising 12 low to moderate certainty findings that identified the relationship between women who lived near ONG operations and the likelihood that their child was born with birth defects or other types of adverse health outcomes at birth.
Two studies evaluated birth defects (congenital heart defects, oral clefts, and neural tube defects) in infants of mothers who lived at varying proximities to ONG development during pregnancy [32,33]. These low-certainty studies resulted in insufficient evidence to determine if living near ONG operations during pregnancy is associated with birth defects since there was only one study per outcome.
Eight studies evaluated adverse birth outcomes [32,34,35,36,37,38,39,40]. These studies examined commonly used indicators of infant health status such as preterm birth, gestational age, Apgar score, birth weight, infant mortality, and fetal death. Overall, there are conflicting findings across studies resulting in either mixed or insufficient evidence of adverse birth outcomes associated with living near ONG operations during pregnancy (Table 4). Three of the eight studies and their findings were upgraded to a moderate level of certainty rating due to strength in their study designs that reduced risk-of-bias [35,37,38]. These studies demonstrated both positive and null associations for multiple health outcomes. All three were retrospective cohort studies that demonstrated evidence of a dose-response relationship and included a valid exposure surrogate as taken from a point location. All other studies were ranked as low certainty because of limitations within the study design or missing key elements. For example, most studies failed to adequately quantify exposure either directly, or through a proxy/surrogate estimate. In many cases, this measure of exposure was limited to either presence or absence of wells in a county or was solely proximity-based. Although some studies calculated inverse distance-weighted well counts, they failed to quantify other metrics such as well development phase or total natural gas volume [39].
Birth outcomes have received the most scholarly attention for this topic, due to the relatively easy access to birth certificate or birth health records data, and the ability to pinpoint exposures to ONG operations during the 40-week gestation period [36]. While the overall evidence is rated as mixed or insufficient for various outcomes, the most recently published studies on ONG and birth outcomes have used innovative methodologies that improve or alleviate some of the weaker assumptions in early work. For example, Hill in 2018 took advantage of the little assumed difference between pregnant women living near permitted but not yet drilled wells and those living near active wells to define a better comparison or control group [37]. Additionally, three of the four moderate certainty studies evaluated birth outcomes and have identified positive associations between living near ONG operations and these adverse health outcomes.
ONG operations can emit volatile organic compounds (VOCs) into the air and contribute to increased particulate matter 10 micrometers or less in diameter (≤PM10) during upstream development activities. Some of these VOCs have the potential to cause developmental effects in test animals following high levels of exposure—generally at much higher levels than what has been observed for individual VOCs at ONG operations [41]. Systematic reviews of a broad set of data have identified positive associations between maternal exposures to fine particulate matter in ambient outdoor air pollution in urban areas and adverse birth outcomes. Other studies have documented adverse developmental and reproductive health outcomes in animals exposed to ONG-related chemicals used as fracturing fluids in the hydraulic fracturing process [42,43,44,45]. Although these substances may be released from operations, the exposure concentrations and complete routes of exposure have not been well characterized.
3.2. Cancer
We identified seven low certainty study outcomes from three studies that assessed the relationship between living near ONG operations and the likelihood of developing cancer [46,47,48]. The studies examined various types of both adult-onset and childhood cancers. Specifically, they looked at the incidence of cancers of the urinary bladder and thyroid, leukemia, all childhood cancers, childhood leukemia (and specifically acute lymphocytic leukemia), childhood non-Hodgkin’s lymphoma, and childhood central nervous system tumors. Overall, the weight of evidence is insufficient for all but one of the cancer outcomes since there is only one study for each. There is mixed evidence for childhood leukemia owing to conflicting study findings.
None of the three cancer studies and their findings were upgraded to a moderate level of certainty rating. Two of the studies were ecological, conducted at the county level in Pennsylvania, and did not control for potential confounding variables [46,47]. For example, it is probable that there are social characteristics of county populations (e.g., race or ethnicity, occupation, smoking status, etc.), differing access to medical care and screening, and other environmental exposures (e.g., major roadways, particularly in a place like Allegheny County where Pittsburgh is located) that would explain some of the study findings. Fryzek et al. also incorrectly interpreted their standardized incidence ratio results, as has been noted by Saunders et al. [14]. McKenzie et al. used a case-control design to study childhood cancers in rural Colorado [48]. However, their data source was exclusively the state’s cancer registry and therefore there was no comparison group made up of children without cancer. Additional research on this topic might consider incorporating a more appropriate comparison group from household surveys [49]. For studies of cancer, it is crucial for researchers to consider what would be an appropriate time frame from exposure to ONG operations to the potential development of cancer. ONG operations began in earnest in the late 2000s in Pennsylvania, but Fryzek et al. used data only through 2009; this truncated period between community exposure and cancer endpoint is a major limitation [47]. As noted elsewhere [50], the study period was not matched to the theoretical lag period or latency period for adult carcinogenesis.
ONG operations may release chemicals into the air and water, such as benzene, polycyclic aromatic hydrocarbons, and diesel exhaust [51]. Although long-term exposure to these substances, such as benzene, may increase the risk of developing certain types of cancer, the development of cancer is complex because many other non-environmental influences, such as genetics and lifestyle behaviors, also contribute to cancer risk.
3.3. Respiratory Health Outcomes
There were three low to moderate rated health outcomes from six studies evaluating the associations between living near ONG and respiratory health effects [52,53,54,55,56,57]. A single moderate certainty study with one study outcome indicated a limited weight of evidence for an association with asthma exacerbations [56]. The current literature provides a link between regulated air pollutants (ozone and particulate matter) and lung, heart disease and other respiratory health effects [58]. The influence, specifically, of ONG contributing to respiratory health outcomes is not fully understood, particularly within the context of other behavioral/lifestyle influences (e.g., smoking) exacerbating the deleterious effects of air pollutants. Additionally, there may be many other environmental sources of emissions for air pollutants including vehicles and wildfires.
Five other low-rated studies evaluated the occurrence of respiratory effects (various self-reported symptoms and hospitalizations) and found conflicting evidence for both categories. The two hospitalization studies used ecological study design, which is limited since the estimation of exposure is based on an average in the population. The three other studies documented self-reported symptoms. Health outcomes were not determined by a medical provider.
3.4. Neurological Health Outcomes
We identified four studies that assessed the relationship between living near ONG development and the likelihood of neurological health effects [52,53,55,57]. Three studies identified self-reported neurological symptoms (Elliott et al. [52]: severe headaches, dizziness; Rabinowitz et al. [55]: neurologic problems, severe headache/migraine, dizziness/balance problems, depression, difficulty concentrating/remembering, difficulty sleeping/insomnia, anxiety/nervousness, seizures; Tustin et al. [57]: migraine headache, fatigue) and yielded a limited weight of evidence for a null association with neurological health effects. The other outcome, neurological hospitalizations, had insufficient evidence, with only one positive study published [53]. VOCs are known to produce neurological effects, such as central nervous system damage, headaches, dizziness, visual disorders, loss of coordination, and memory impairment in test animals and humans [59].
3.5. Other Health Outcomes
We found limited evidence of a positive association between general multiple self-reported symptoms and living near ONG development, with two studies assessing this relationship [52,57]. The two studies however characterized symptoms differently: Elliott and her colleagues combined feeling stress, fatigue, muscle or joint pain, or any other health symptom into a “general health symptom” grouping [52]; while Tustin and his co-authors found significant effects only when at least two of the three symptoms they considered—chronic rhinosinusitis, migraine, and fatigue—were experienced jointly [57].
Two epidemiologic studies evaluated a variety of indicators of psychological well-being, including depression, anxiety and sleep disturbances [60,61]. Measures of mental health are not necessarily a result of direct exposure to substances emitted from oil and gas operations but could be indirectly associated with non-chemical environmental stressors such as noise, light, odors, or social stress of living near a hotly debated, politicized, and potentially risky industry. For example, studies have shown associations between living in areas with increased noise and traffic, such as by airports, with increased psychological symptoms [62,63,64,65].
There was mixed evidence for self-reported dermal symptoms, self-reported psychological symptoms, and cardiovascular hospitalizations. Other health effects, including neurological and all hospitalizations, diagnosed sleep disturbances, and self-reported cardiovascular symptoms, had insufficient evidence due to a single low-rated study per outcome. There was a demonstrated lack of evidence (no association) for gastrointestinal self-reported symptoms. Three studies evaluated self-reported dermal symptoms, such as rash, irritation, burning, itching, and hair loss, in relation to ONG in Pennsylvania, resulting in mixed evidence [52,55,61]. Skin-related health effects may be possible due to direct exposure to soil or water. However, the routes of exposure to ONG-related chemicals were not well characterized in these studies and encounters with other skin irritants were not documented, making it difficult to interpret these conclusions.
4. Discussion
In this paper, we summarized the observational epidemiologic literature on the health effects of populations living near ONG operations and assessed the methodological rigor of the studies published to date. Specifically, we used a modified systematic review framework, adapted from GRADE, the Navigation Guide, and guidance from OHAT, to determine the level of certainty that the study findings represent the true effect of exposures to ONG-related substances, and to make overarching weight-of-evidence determinations for a variety of health outcomes.
The strength of our review lies in its transparency and objectivity. We adapted previous systematic review guidelines to make the criteria for evaluating studies as clear as possible. We considered a wide variety of study evaluation questions to represent those domains. Our review framework can also be applied to other research questions in environmental health. For researchers, policymakers, and public health practitioners, this type of review can swiftly help elucidate key findings and gaps in the knowledge base that need to be addressed.
We found 20 published epidemiologic studies that evaluate potential associations between ONG operations and health outcomes. These studies assessed 32 different health outcomes ranging from self-reported symptoms to confirmed disease diagnoses. Since only a few outcomes were covered by multiple studies, there was insufficient weight of evidence for most health outcomes. We found studies of populations living near ONG operations provide limited evidence (modest scientific findings that support the outcome, but with significant limitations) of harmful health effects including asthma exacerbations and various self-reported symptoms. For all other health outcomes, we found conflicting evidence (mixed), insufficient evidence, or in some cases, a lack of evidence of the possibility for harmful health effects.
There are important limitations to our approach. First, it is not a meta-analysis as the current line of inquiry, including different exposure measures (and surrogates), health outcomes, and geographic/geologic locations, is not suited to conducting a meta-analysis. Second, although we clearly stated our criteria for upgrading a study to a moderate or high level of certainty ranking, the number of study evaluation questions and the ranking cutoffs may still be viewed as arbitrary since Rooney et al. (2016) compares these systematic review methods and notes that the scoring of studies may be influenced by the number of elements and may not account for the differences in relative importance across the risk of bias domains [66]. Study certainty is difficult to quantify, but we used a quantifiable framework and did not allow factors such as media coverage or other publicity (positive or negative) to color our ranking system.
The majority of findings from the studies were ranked as low certainty, primarily due to limitations of the study designs that make it difficult to establish clear links between exposures to substances potentially emitted directly from ONG operations and the health outcomes evaluated. These limitations are inherent to observational epidemiologic studies and include indirect exposure measurements, confounding bias, and subjective methods to determine health outcomes. The field of environmental health incorporates these types of studies along with exposure and risk assessments to inform public health and policies. In addition to these factors, differences in the observational epidemiologic study types (e.g., retrospective cohort, case-control, ecological) make it difficult to compare results across studies with various health outcomes. These epidemiologic studies may also reflect the interactions of non-chemical or chemical stressors that may or may not be related to ONG operations that can contribute to adverse health outcomes in a population. Study quality has improved in recent years with better exposure measures and more thorough methods to account for possible confounders.
Although these observational epidemiologic studies alone are not sufficient to determine causality, they provide helpful information to direct further investigation into the public health implications of ONG activity near residential areas. Taken together, these studies make it clear that the identities and exposure levels of substances people are exposed to when living, working, or going to school near ONG development have not been well characterized. Epidemiologic studies that include more controlled designs with direct measurement of exposure and diagnosed health outcomes are needed to confirm or dispute the associations published in the literature. Incorporating a health impact assessment framework within an epidemiologic study may be useful. One such framework, developed by the Agency for Toxic Substances and Disease Registry (ATSDR) can be used to assess the health impacts of multiple chemicals and stressors [67].
Additionally, we have little empirically driven understanding of the factors (biological, geological, meteorological, and social) that drive ONG-related exposure patterns and vulnerability to such exposures. For example, there may be regional differences across the U.S., with varying technological controls or regulatory environments. Researchers should integrate community members [68,69,70] and concepts of health equity and environmental justice [69] into their research approaches. They should also consider using policy as a starting point rather than the conclusion in order to evaluate policies and ONG industry practices that have been implemented thus far (e.g., setback distances, number of wells drilled per well pad, etc.). Having an understanding and familiarity with the populations at risk for health effects from ONG development across states and regions within states is also important to prioritize evidence-based health-protective policy interventions and to improve public health prevention strategies [52,68,69,70,71].
ONG regulatory policy has not been informed by robust epidemiologic research literature. Now, 15–20 years since the widespread application of hydraulic fracturing and horizontal drilling in states as diverse as Colorado, Pennsylvania, Texas, and Kansas, the epidemiologic literature on the potential health effects of ONG operations is still inadequate to definitively guide policy, as evidenced by the mainly low certainty and conflicting studies reviewed here. Regulators and policymakers, then, should work with public health researchers to pose specific questions that need to be answered, and partner with public health officials to evaluate the public’s concerns. Public health officials should continue to monitor health concerns in areas with substantial ONG operations through centralized data collection and analysis. Multi-state collaborations should be considered to collect consistent data from differing oil and gas basins across the United States with the aim to more comprehensively evaluate the potential for adverse health effects.
Acknowledgments
We thank Katelyn Hall for assistance with criteria question development. This research was supported by general funds from the State of Colorado.
Supplementary Materials
The following materials are available online at https://www.mdpi.com/1660-4601/16/12/2123/s1, Tables S1–S20: Study evaluation individual assessments, Table S21: Full summary details of epidemiologic studies included in systematic review, Table S22: Summary of answers to study evaluation questions.
Author Contributions
A.M.B., T.S.M., M.V.D., and D.I.V. initiated the manuscript and developed the overall strategy. A.B. and S.H. conceptualized the systematic review study evaluation questions and coded the articles for study quality (certainty). A.M.B. and S.H.H. wrote the first draft of the manuscript. A.S.N., S.M.W., M.V.D., K.R., T.S.M., and D.I.V. revised the final manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.U.S. Energy Information Administration U.S. Natural Gas Production Hit A New Record High in 2018. [(accessed on 5 June 2019)]; Available online: https://www.eia.gov/todayinenergy/detail.php?id=38692.
- 2.U.S. Energy Information Administration Hydraulically Fractured Horizontal Wells Account For Most New Oil And Natural Gas Wells. [(accessed on 14 January 2019)]; Available online: https://www.eia.gov/todayinenergy/detail.php?id=37815.
- 3.Czolowski E.D., Santoro R.L., Srebotnjak T., Shonkoff S.B.C. Toward consistent methodology to quantify populations in proximity to oil and gas development: A national spatial analysis and review. Environ. Health Perspect. 2017;125 doi: 10.1289/EHP1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitka M. Rigorous evidence slim for determining health risks from natural gas fracking. J. Am. Med. Assoc. 2012;307:2135–2136. doi: 10.1001/jama.2012.3726. [DOI] [PubMed] [Google Scholar]
- 5.Werner A.K., Vink S., Watt K., Jagals P. Environmental health impacts of unconventional natural gas development: A review of the current strength of evidence. Sci. Total Environ. 2015;505:1127–1141. doi: 10.1016/j.scitotenv.2014.10.084. [DOI] [PubMed] [Google Scholar]
- 6.Health Impact Assessment for Battlement Mesa, Garfield County, Colorado. [(accessed on 9 September 2010)]; Available online: https://www.garfield-county.com/public-health/documents/1%20%20%20Complete%20HIA%20without%20Appendix%20D.pdf.
- 7.Ferrar K.J., Kriesky J., Christen C.L., Marshall L.P., Malone S.L., Sharma R.K., Michanowicz D.R., Goldstein B.D. Assessment and longitudinal analysis of health impacts and stressors perceived to result from unconventional shale gas development in the Marcellus Shale region. Int. J. Occup. Environ. Health. 2013;19:104–112. doi: 10.1179/2049396713Y.0000000024. [DOI] [PubMed] [Google Scholar]
- 8.Weinberger B., Greiner L.H., Walleigh L., Brown D. Health symptoms in residents living near shale gas activity: A retrospective record review from the Environmental Health Project. Prev. Med. Rep. 2017;8:112–115. doi: 10.1016/j.pmedr.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson B.J., Theodori G.L. Local leaders’ perceptions of energy development in the Barnett Shale. South. Rural Sociol. 2009;24:113–129. [Google Scholar]
- 10.Brasier K.J., Filteau M., McLaughlin D.K., Jacquet J., Stedman R.C., Kelsey T.W., Goetz S.J. Residents’ perceptions of community and environmental impacts from development of natural gas in the Marcellus Shale: A comparison of Pennsylvania and New York cases. J. Rural Soc. Sci. 2011;26:32–61. [Google Scholar]
- 11.Powers M., Saberi P., Pepino R., Strupp E., Bugos E., Cannuscio C.C. Popular epidemiology and “fracking”: Citizens’ concerns regarding the economic, environmental, health and social impacts of unconventional natural gas drilling operations. J. Community Health. 2015;40:534–541. doi: 10.1007/s10900-014-9968-x. [DOI] [PubMed] [Google Scholar]
- 12.Hays J., Shonkoff S.B.C. Toward an understanding of the environmental and public health impacts of unconventional natural gas development: A categorical assessment of the peer-reviewed scientific literature, 2009–2015. PLoS ONE. 2016;11 doi: 10.1371/journal.pone.0154164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stacy S.L. A review of the human health impacts of unconventional natural gas development. Curr. Epidemiol. Rep. 2017;4:38–45. doi: 10.1007/s40471-017-0097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saunders P.J., McCoy D., Goldstein R., Saunders A.T., Munroe A. A review of the public health impacts of unconventional natural gas development. Environ. Geochem. Health. 2018;40:1–57. doi: 10.1007/s10653-016-9898-x. [DOI] [PubMed] [Google Scholar]
- 15.Guyatt G.H., Oxman A.D., Vist G.E., Kunz R., Falck-Ytter Y., Alonso-Coello P., Schünemann H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D., Moher D., Becker B.J., Sipe T.A., Thacker S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. J. Am. Med. Assoc. 2003;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 17.Woodruff T.J., Sutton P. The navigation guide systematic review methodology: A rigorous and transparent method for translating environmental health science into better health outcomes. Environ. Health Perspect. 2014;122:1007–1014. doi: 10.1289/ehp.1307175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rooney A.A., Boyles A.L., Wolfe M.S., Bucher J.R., Thayer K.A. Systematic review and evidence integration for literature-based environmental health science assessments. Environ. Health Perspect. 2014;122:711–718. doi: 10.1289/ehp.1307972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson P.I., Sutton P., Atchley D.S., Koustas E., Lam J., Sen S., Robinson K.A., Axelrad D.A., Woodruff T.J. The Navigation Guide—Evidence-based medicine meets environmental health: Systematic review of human evidence for PFOA effects on fetal growth. Environ. Health Perspect. 2014;122:1028–1039. doi: 10.1289/ehp.1307893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.U.S. Energy Information Administration Hydraulically Fractured Wells Provide Two-Thirds of U.S. Natural Gas Production. [(accessed on 13 February 2019)]; Available online: https://www.eia.gov/todayinenergy/detail.php?id=26112.
- 21.Hardy K., Kelsey T.W. Local income related to Marcellus shale activity in Pennsylvania. Community Dev. 2015;46:329–340. doi: 10.1080/15575330.2015.1059351. [DOI] [Google Scholar]
- 22.Tunstall T. Recent economic and community impact of unconventional oil and gas exploration and production on South Texas counties in the Eagle Ford Shale area. J. Reg. Anal. Policy. 2015;45:82–92. [Google Scholar]
- 23.Schünemann H., Hill S., Guyatt G., Akl E.A., Ahmed F. The GRADE approach and Bradford Hill’s criteria for causation. J. Epidemiol. Community Health. 2011;65:392–395. doi: 10.1136/jech.2010.119933. [DOI] [PubMed] [Google Scholar]
- 24.Hill A.B. The environment and disease: Association or causation? Proc. R. Soc. Med. 1965;58:295–300. doi: 10.1177/0141076814562718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guyatt G.H., Oxman A.D., Kunz R., Vist G.E., Falck-Ytter Y., Schünemann H.J. What is “quality of evidence” and why is it important to clinicians? BMJ. 2008;336:995–998. doi: 10.1136/bmj.39490.551019.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wells G., Shea B., O’Connell D., Peterson J., Welch V., Losos M., Tugwell P. Newcastle-Ottawa quality assessment scale: Case control studies. [(accessed on 19 May 2019)]; Available online: http://www.ohri.ca/programs/clinical_epidemiology/nosgen.pdf.
- 27.Higgins J.P., Altman D.G., Sterne J. Assessing Risk of Bias in Included Studies. In: Higgins J.P., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; London, UK: 2011. Chapter 8. [Google Scholar]
- 28.Balise V.D., Meng C.X., Cornelius-Green J.N., Kassotis C.D., Kennedy R., Nagel S.C. Systematic review of the association between oil and natural gas extraction processes and human reproduction. Fertil. Steril. 2016;106:795–819. doi: 10.1016/j.fertnstert.2016.07.1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berkman N.D., Lohr K.N., Ansari M., McDonagh M., Balk E., Whitlock E., Reston J., Bass E., Butler M., Gartlehner G., et al. Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Agency for Healthcare Research and Quality; Rockville, MD, USA: 2008. Grading the Strength of a Body of Evidence When Assessing Health Care Interventions for the Effective Health Care Program of the Agency for Healthcare Research and Quality: An Update. Chapter 15. [PubMed] [Google Scholar]
- 30.Schünemann H.J., Oxman A.D., Vist G.E., Higgins J.P., Deeks J., Glasziou P., Guyatt G.H. Assessing the Quality of a Body of Evidence. In: Higgins J.P., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; London, UK: 2011. Chapter 12.2. [Google Scholar]
- 31.Eden J., Levit L., Berg A., Morton S. Finding What Works in Health Care: Standards for Systematic Reviews. National Academies Press; Washington, DC, USA: 2011. [PubMed] [Google Scholar]
- 32.McKenzie L.M., Guo R., Witter R.Z., Savitz D.A., Newman L.S., Adgate J.L. Birth outcomes and maternal residential proximity to natural gas development in rural Colorado. Environ. Health Perspect. 2014;122:412–417. doi: 10.1289/ehp.1306722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ma Z., Sneeringer K.C., Liu L., Kuller L.H. Time series evaluation of birth defects in areas with and without unconventional natural gas development. J. Epidemiol. Public Heal. Rev. 2016;1 doi: 10.16966/2471-8211.107. [DOI] [Google Scholar]
- 34.Busby C., Mangano J.J. There’s a world going on underground—Infant mortality and fracking in Pennsylvania. J. Environ. Prot. (Irvine, Calif). 2017;08:381–393. doi: 10.4236/jep.2017.84028. [DOI] [Google Scholar]
- 35.Casey J.A., Savitz D.A., Rasmussen S.G., Ogburn E.L., Pollak J., Mercer D.G., Schwartz B.S. Unconventional natural gas development and birth outcomes in Pennsylvania, USA. Epidemiology. 2016;27:163–172. doi: 10.1097/EDE.0000000000000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Currie J., Greenstone M., Meckel K. Hydraulic fracturing and infant health: New evidence from Pennsylvania. Sci. Adv. 2017;3:e1603021. doi: 10.1126/sciadv.1603021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hill E.L. Shale gas development and infant health: Evidence from Pennsylvania. J. Health Econ. 2018;61:134–150. doi: 10.1016/j.jhealeco.2018.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stacy S.L., Brink L.A.L., Larkin J.C., Sadovsky Y., Goldstein B.D., Pitt B.R., Talbott E.O. Perinatal outcomes and unconventional natural gas operations in Southwest Pennsylvania. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0126425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Whitworth K.W., Marshall A.K., Symanski E. Maternal residential proximity to unconventional gas development and perinatal outcomes among a diverse urban population in Texas. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0180966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Whitworth K.W., Marshall A.K., Symanski E. Drilling and production activity related to unconventional gas development and severity of preterm birth. Environ. Health Perspect. 2018;126 doi: 10.1289/EHP2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McMullin T.S., Bamber A.M., Bon D., Vigil D.I., Van Dyke M. Exposures and Health Risks from Volatile Organic Compounds in Communities Located Near Oil and Gas Exploration and Production Activities in Colorado (U.S.A.) Int. J. Environ. Res. Public Health. 2018;15:1500. doi: 10.3390/ijerph15071500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Inayat-Hussain S.H., Fukumura M., Muiz Aziz A., Jin C.M., Jin L.W., Garcia-Milian R., Vasiliou V., Deziel N.C. Prioritization of reproductive toxicants in unconventional oil and gas operations using a multi-country regulatory data-driven hazard assessment. Environ. Int. 2018;117:348–358. doi: 10.1016/j.envint.2018.05.010. [DOI] [PubMed] [Google Scholar]
- 43.Kassotis C.D., Tillitt D.E., Davis J.W., Hormann A.M., Nagel S.C. Estrogen and androgen receptor activities of hydraulic fracturing chemicals and surface and ground water in a drilling-dense region. Endocrinology. 2014;155:897–907. doi: 10.1210/en.2013-1697. [DOI] [PubMed] [Google Scholar]
- 44.Kassotis C.D., Klemp K.C., Vu D.C., Lin C.H., Meng C.X., Besch-Williford C.L., Pinatti L., Zoeller R.T., Drobnis E.Z., Balise V.D., et al. Endocrine-disrupting activity of hydraulic fracturing chemicals and adverse health outcomes after prenatal exposure in male mice. Endocrinology. 2015;156:4458–4473. doi: 10.1210/en.2015-1375. [DOI] [PubMed] [Google Scholar]
- 45.Kassotis C.D., Bromfield J.J., Klemp K.C., Meng C.X., Wolfe A., Zoeller R.T., Balise V.D., Isiguzo C.J., Tillitt D.E., Nagel S.C. Adverse reproductive and developmental health outcomes following prenatal exposure to a hydraulic fracturing chemical mixture in female C57Bl/6 mice. Endocrinology. 2016;157:3469–3481. doi: 10.1210/en.2016-1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Finkel M.L. Shale gas development and cancer incidence in southwest Pennsylvania. Public Health. 2016;141:198–206. doi: 10.1016/j.puhe.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 47.Fryzek J., Pastula S., Jiang X., Garabrant D.H. Childhood cancer incidence in Pennsylvania counties in relation to living in counties with hydraulic fracturing sites. J. Occup. Environ. Med. 2013;55:796–801. doi: 10.1097/JOM.0b013e318289ee02. [DOI] [PubMed] [Google Scholar]
- 48.McKenzie L.M., Allshouse W.B., Byers T.E., Bedrick E.J., Serdar B., Adgate J.L. Childhood hematologic cancer and residential proximity to oil and gas development. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0170423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Short P.F., Vasey J.J., Moran J.R. Long-term effects of cancer survivorship on the employment of older workers. Health Serv. Res. 2008;43:193–210. doi: 10.1111/j.1475-6773.2007.00752.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Goldstein B.D., Malone S. Obfuscation does not provide comfort: Response to the article by Fryzek et al. on hydraulic fracturing and childhood cancer. J. Occup. Environ. Med. 2013;55:1376–1378. doi: 10.1097/JOM.0000000000000014. [DOI] [PubMed] [Google Scholar]
- 51.Adgate J.L., Goldstein B.D., McKenzie L.M. Potential public health hazards, exposures and health effects from unconventional natural gas development. Environ. Sci. Technol. 2014;48:8307–8320. doi: 10.1021/es404621d. [DOI] [PubMed] [Google Scholar]
- 52.Elliott E.G., Ma X., Leaderer B.P., McKay L.A., Pedersen C.J., Wang C., Gerber C.J., Wright T.J., Sumner A.J., Brennan M., et al. A community-based evaluation of proximity to unconventional oil and gas wells, drinking water contaminants, and health symptoms in Ohio. Environ. Res. 2018;167:550–557. doi: 10.1016/j.envres.2018.08.022. [DOI] [PubMed] [Google Scholar]
- 53.Jemielita T., Gerton G.L., Neidell M., Chillrud S., Yan B., Stute M., Howarth M., Saberi P., Fausti N., Penning T.M., et al. Unconventional gas and oil drilling is associated with increased hospital utilization rates. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0131093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Peng L., Meyerhoefer C., Chou S.Y. The health implications of unconventional natural gas development in Pennsylvania. Health Econ. 2018;27:956–983. doi: 10.1002/hec.3649. [DOI] [PubMed] [Google Scholar]
- 55.Rabinowitz P.M., Slizovskiy I.B., Lamers V., Trufan S.J., Holford T.R., Dziura J.D., Peduzzi P.N., Kane M.J., Reif J.S., Weiss T.R., et al. Proximity to natural gas wells and reported health status: Results of a household survey in Washington County, Pennsylvania. Environ. Health Perspect. 2015;123:21–26. doi: 10.1289/ehp.1307732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rasmussen S.G., Ogburn E.L., McCormack M., Casey J.A., Bandeen-Roche K., Mercer D.G., Schwartz B.S. Association between unconventional natural gas development in the Marcellus Shale and asthma exacerbations. JAMA Intern. Med. 2016;176:1334–1343. doi: 10.1001/jamainternmed.2016.2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tustin A.W., Hirsch A.G., Rasmussen S.G., Casey J.A., Bandeen-Roche K., Schwartz B.S. Associations between unconventional natural gas development and nasal and sinus, migraine headache, and fatigue symptoms in Pennsylvania. Environ. Health Perspect. 2017;125:189–197. doi: 10.1289/EHP281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Environmental Protection Agency Research on Health and Environmental Effects of Air Quality. [(accessed on 12 February 2019)]; Available online: https://www.epa.gov/air-research/research-health-and-environmental-effects-air-quality.
- 59.National Library of Medicine Volatile Organic Compounds (VOCs) [(accessed on 2 December 2019)]; Available online: https://toxtown.nlm.nih.gov/chemicals-and-contaminants/volatile-organic-compounds-vocs.
- 60.Casey J.A., Wilcox H.C., Hirsch A.G., Pollak J., Schwartz B.S. Associations of unconventional natural gas development with depression symptoms and disordered sleep in Pennsylvania. Sci. Rep. 2018;8 doi: 10.1038/s41598-018-29747-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Steinzor N., Subra W., Sumi L. Investigating links between shale gas development and health impacts through a community survey project in Pennsylvania. New Solut. 2013;23:55–83. doi: 10.2190/NS.23.1.e. [DOI] [PubMed] [Google Scholar]
- 62.Morrell S., Taylor R., Lyle D. A review of health effects of aircraft noise. Aust. N. Z. J. Public Health. 1997;21:221–236. doi: 10.1111/j.1467-842X.1997.tb01690.x. [DOI] [PubMed] [Google Scholar]
- 63.Stansfeld S., Haines M., Brown B. Noise and health in the urban environment. Rev. Environ. Health. 2000;15:43–82. doi: 10.1515/REVEH.2000.15.1-2.43. [DOI] [PubMed] [Google Scholar]
- 64.Recio A., Linares C., Banegas J.R., Díaz J. Road traffic noise effects on cardiovascular, respiratory, and metabolic health: An integrative model of biological mechanisms. Environ. Res. 2016;146:359–370. doi: 10.1016/j.envres.2015.12.036. [DOI] [PubMed] [Google Scholar]
- 65.Pedersen E. City Dweller Responses to Multiple Stressors Intruding into Their Homes: Noise, Light, Odour, and Vibration. Int. J. Environ. Res. Public Health. 2015;12:3246–3263. doi: 10.3390/ijerph120303246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rooney A.A., Cooper G.S., Jahnke G.D., Lam J., Morgan R.L., Boyles A.L., Ratcliffe J.M., Kraft A.D., Schunemann H.J., Schwingl P., et al. How credible are the study results? Evaluating and applying internal validity tools to literature-based assessments of environmental health hazards. Environ. Int. 2016;92–93:617–629. doi: 10.1016/j.envint.2016.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Framework for Assessing Health Impacts of Multiple Chemicals and Other Stressors (Update) [(accessed on 13 June 2019)]; Available online: https://www.atsdr.cdc.gov/interactionprofiles/ip-ga/ipga.pdf.
- 68.Macey G.P., Breech R., Chernaik M., Cox C., Larson D., Thomas D., Carpenter D.O. Air concentrations of volatile compounds near oil and gas production: A community-based exploratory study. Environ. Heal. 2014;13:82. doi: 10.1186/1476-069X-13-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Penning T.M., Breysse P.N., Gray K., Howarth M., Yan B. Environmental health research recommendations from the Inter-Environmental Health Sciences Core Center Working Group on unconventional natural gas drilling operations. Environ. Health Perspect. 2014;122:1155–1159. doi: 10.1289/ehp.1408207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Korfmacher K.S., Elam S., Gray K.M., Haynes E., Hughes M.H. Unconventional natural gas development and public health: Toward a community-informed research agenda. Rev. Environ. Health. 2014;29:293–306. doi: 10.1515/reveh-2014-0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Clough E., Bell D. Just fracking: A distributive environmental justice analysis of unconventional gas development in Pennsylvania, USA. Environ. Res. Lett. 2016;11 doi: 10.1088/1748-9326/11/2/025001. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.