Abstract
Background
The soil-dwelling bacillus Burkholderia pseudomallei is the etiological-agent of the neglected and life-threatening emerging infection melioidosis. The distribution of B. pseudomallei in West Africa is unknown. In the present study we aimed to determine whether B. pseudomallei and B. thailandensis are present in the environment of central Sierra Leone.
Methodology/Principal findings
In June-July 2017, we conducted an environmental surveillance study–designed in accordance with existing consensus guidelines—in central Sierra Leone. A total of 1,000 soil samples (100 per site) were collected and cultured. B. pseudomallei was not identified in the soil, but we identified seven novel B. thailandensis sequence types with multi-locus sequence typing (MLST) and 16S rRNA gene sequence analyses.
Conclusions/Significance
The presence of B. pseudomallei was not demonstrated, however, multiple novel B. thailandensis sequence types were identified. More environmental and sequencing studies are needed to further understand the genetic diversity, evolution and virulence of these emerging organisms.
Author summary
The environmental bacterium Burkholderia pseudomallei is the cause of melioidosis, an often-fatal but neglected infection prevalent across tropical areas. B. thailandensis is a member of the B. pseudomallei complex, rarely causes disease in humans and is considered a-virulent. Modelling studies have estimated a high prevalence of B. pseudomallei in western Africa. In this study, we performed an environmental surveillance study in the West African country of Sierra Leone. Remarkably, we could not demonstrate the presence of B. pseudomallei in the soil of Sierra Leone. However, by both culture and sequencing methods, we identified multiple B. thailandensis strains and novel genotypes. Patients with debilitating B. thailandensis infection have been occasionally reported in among others Southeast Asia and the US. Environmental and sequencing studies on both B. pseudomallei and B. thailandensis are essential to further understand the genetic diversity and evolution of these neglected but emerging organisms.
Introduction
The Gram-negative environmental bacterium Burkholderia pseudomallei is the etiological agent of melioidosis, an emerging but neglected infectious disease. Disease presentations vary from abscess formation to fulminant sepsis [1]. Melioidosis has a mortality up to 50% in low resource settings and is predominantly found in Southeast-Asia and northern Australia [1]. Infection with B. pseudomallei primarily occurs in people who are in regular contact with soil and water [1,2]. B. thailandensis is a member of the B. pseudomallei complex, is considered a-virulent [3,4] and rarely causes disease in humans [5–10]. Knowledge about the global distribution of B. pseudomallei and B. thailandensis, however, is limited.
Patients from sub-Saharan Africa reported with melioidosis are few and isolated (e.g. the The Gambia, Burkina Faso, Nigeria and Gabon), which most probably is the result of under-recognition and under-reporting. These cases may represent the ‘Tip of the Iceberg’ [1,11]. From the West African country of Sierra Leone, only one case of melioidosis has been reported [12]. Modelling studies, however, estimate that in Sierra Leone annually hundreds of patients suffer from melioidosis, of which the vast majority will die [13]. The tropical climate, heavy rains and abundant rice farming in central Sierra Leone all contribute to the high pre-odds likely-hood for the presence of B. pseudomallei and B. thailandensis in its soils [13]. In the present study we aim to determine whether B. pseudomallei and B. thailandensis are present in the soil of central Sierra Leone.
Methods
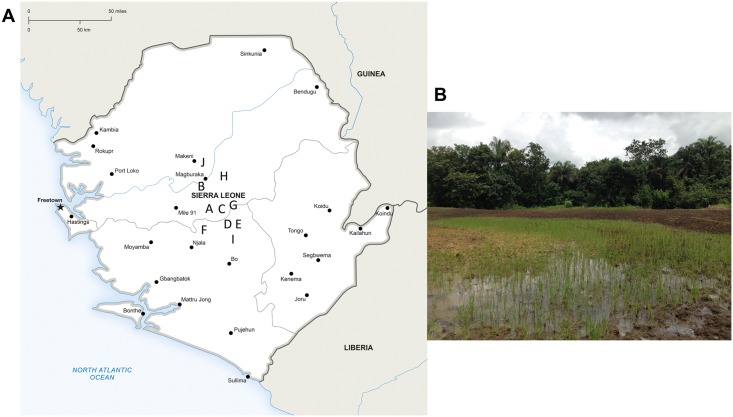
During the rainy season (June-July 2017), an environmental surveillance study–designed in accordance with existing consensus guidelines [14]—was conducted in Tonkolili and Bombali districts, central Sierra Leone (Fig 1A and 1B). Ten different sites were selected based on local maps and consultations with inhabitants on factors known to be associated with B. pseudomallei and B. thailandensis presence (e.g., wet soil such as rice paddies or land use such as goat and cattle farming) [13,14]. Oral informed permission was obtained from landowners and written informed permission from the paramount chief of Yele, Sierra Leone, prior to soil sampling. We used a fixed-interval sampling grid of five meters between soil samples. Thirty grams of soil from a depth of 65 cm [15] was taken for each sample, stored from direct sunlight and kept at room temperature until further processing (for details on geographical features and distribution see Table 1). Culture of suspected Burkholderia isolates from soil samples was done as described previously [14,16]. First, 10 grams of each soil sample was diluted in 10 mL of threonine-basal solution containing colistin at 50 mg/L (TBSS-C50 broth) and crystal violet. This mixture was vortexed and subsequently incubated at 40 °C for 48 hours. Ten μL of the upper layer of enrichment medium was subcultured onto an Ashdown-agar plate and checked for suspected Burkholderia colonies every 24 hours for a period of 7 days. Initial identification of suspected Burkholderia growth was done by colony morphology, positive oxidase test result, antimicrobial drug susceptibility pattern (susceptible to amoxicillin-clavulanic and resistant to gentamicin and colistin) and latex-agglutination tests [14,16] (see S1 Fig for a schematic overview of the culture methodology). All experiments were conducted in a biosafety level 3 laboratory.
Fig 1. Location of soil sampling sites in Sierra Leone and phylogenetic tree of isolated B. thailandensis isolates.
(A) Sierra Leone, showing the location of 10 soil sampling sites to test for the presence of B. pseudomallei, June-July 2017. (B) Rice farm Sierra Leone, site E. Image adapted from onestopmap.com.
Table 1. Geographical features and distribution of Burkholderia strains at ten sampling sites in the Tonkolili and Bombali District, central Sierra Leone (2017).
| Site | Nearest village; location site* | Land use | Soil description | Sample holes positive for Burkholderia thailandensis |
|---|---|---|---|---|
| A | Rochain; lat. N 0.8°24’49.83, long. W 11°51’17.82 |
Rice paddy, next to stream | Clay | 22 |
| B | Matamp; lat. N 0.8°32’9.658, long. W 11°56’30.63 |
Rice paddy, wet | Clay, mud | 3 |
| C | Yele; lat. N 0.8°24’46.17, long. W 11°50’38.28 |
Groundnut farm, goats, next to hospital | Clay | 0 |
| D | Mabara; lat. N 0.8°25’54.51, long. W 11°52’50.15 |
Wet grassland | Clay, mud, brown orange, black, grey | 0 |
| E | Makonkorie; lat. N 0.8°33’13.99, long. W 11°48’54.27 | Rice paddy | Clay, mud | 0 |
| F | Mayessie Junction; lat. N 0.8°26’52.63, long. W 11°57’05.31 | Rice paddy | Clay, mud | 0 |
| G | Patifu Mayawa; lat. N 0.8°26’23.00, long. W 11°49’32.38 | Swamp, goats | Sandy, mud | 0 |
| H | Matotoka; lat N 0.8°39’20.14, long. W 11°51’23.56 |
Rice paddy, after harvest groundnut and potato farm | Clay, red soil | 0 |
| I | Ferry; lat. N 0.8°24’58.66, long. W 11°69’57.46 |
Rice paddy, wet | Sandy soil | 0 |
| J | Matene (near Makeni); lat. N 0.8°47’46.56, long. W 12°01’31.74 | Rice paddy, dry | Dry, sandy, yellow, light brown | 0 |
*lat. = latitude; long. = longitude.
All isolates were identified as B. thailandensis by MLST as well as 16S sequence analyses (see S1 Table). B. pseudomallei was not found. Four B. thailandensis isolates corresponded to the earlier described sequencing type 73 (ST73) [17], but the remaining 28 isolates were of seven novel sequence types (ST1677 through ST1683). ST1677 and ST1680 are single locus variants of ST73, while ST1678, ST1679, ST1681 and ST1682 are double locus variants of ST73 and ST1683 differed at three loci from ST73 (see appendix).
Multi-locus sequence typing (MLST) and 16S rRNA gene sequence analyses were used to determine the species of the isolated Burkholderia isolates using the MiSeq platform (Illumina, San Diego, CA, USA) as described previously [16]. Assembly of the reads was performed with help of SPAdes 3.9. MLST data analysis was performed based on partial sequences of seven housekeeping genes (see appendix). Allele numbers and sequence types deduced from MLST allelic profiles were assigned using the BIGSdb B. pseudomallei database (https://pubmlst.org/bpseudomallei/). Cluster analysis was subsequently performed in the MEGA 6.06 using the UPGMA algorithm and the Jukes-Cantor model. Bootstrap test was performed for 500 repetitions.
Ethics statement
Oral informed permission was obtained from landowners and written informed permission from the paramount chief of Yele, Sierra Leone, prior to soil sampling.
Results/Discussion
A total of 1,000 samples (100 per site) were collected at ten sampling sites in the Tonkolili and Bombali District, central Sierra Leone (see Table 1). Initial identification methods [14,16], led to the isolation of 32 Burkholderia strains from 25 soil samples. Four Burkholderia strains showed a negative latex-agglutination test; the rest showed (possible) positive latex-agglutination test results.
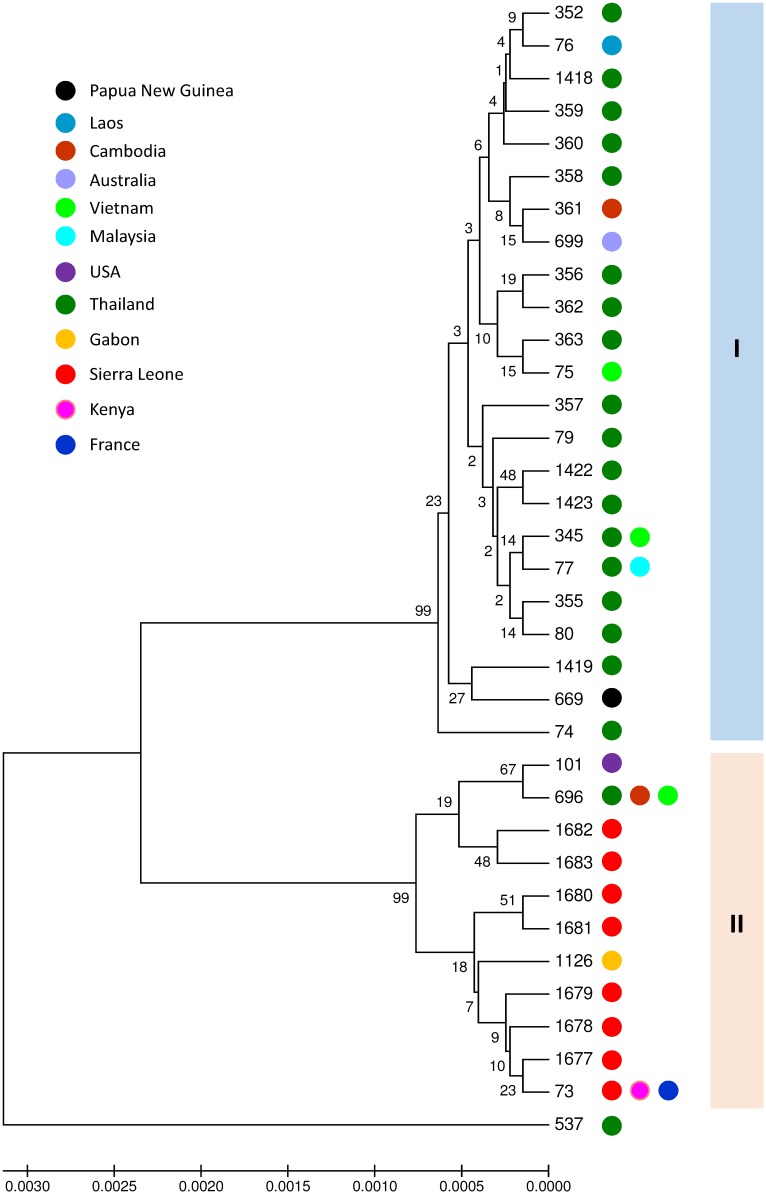
Two main clusters are presented in a phylogenetic tree based on the concatenated sequences of the seven household genes of all B. thailandensis STs available in the PubMLST database (Fig 2). Cluster I contains exclusively isolates from Asia and Oceania, while cluster II comprises isolates from all isolates from Sierra Leone and the one from Gabon (ST1126). One isolate with ST537 was an outlier. Interestingly, ST1126, ST696 and ST101 were identified to express a B. pseudomallei-like capsular polysaccharide (BTCV) [18] possibly explaining why many of the isolated B. thailandensis showed cross-reactivity with the B. pseudomallei latex-agglutination test. MLST data and microarray based comparative genomic hybridization revealed earlier that there is a separate subgroup of B. thailandensis isolates (ST696, ST101 and ST73) containing BTCV strains, which are genetically different from the other B. thailandensis isolates [17].
Fig 2. Phylogenetic tree of all B. thailandensis isolates.
Phylogenetic tree of all B. thailandensis isolates with a unique sequence type recorded in the B. pseudomallei MLST website (https://pubmlst.org/bpseudomallei/). Phylogenetic tree is constructed based on the concatenated sequences of the seven household genes used for MLST using the UPGMA algorithm with the Jukes-Cantor model.
In this study, two clearly separated B. thailandensis clusters (I and II) were observed. Various studies have reported human infections by B. thailandensis belonging to both cluster I (ST77, ST80 and ST345) and cluster II (ST73 and ST101) (https://pubmlst.org/bpseudomallei/) [5–10]. It has been postulated that B. thailandensis isolates within cluster II are more virulent than those in cluster I [17], but evidence has not been reported [6,17]. Clinical characteristics are indistinguishable from B. pseudomallei infection and include soft tissue infection, abscess formation, pneumonia and sepsis [5–10]. The most recently described B. thailandensis case occurred in a 29-year old diabetic woman with an infected wound and swelling of her forearm after a car incident in Arkansas, US [6].
Our study has several limitations, including the lack of standard blood culture services for febrile patients across Sierra Leone. This limits targeted soil sampling studies centred around an index case. In addition, we cannot dismiss the possibility of sampling-error, although consensus guidelines were followed [14]. More knowledge about the exact composition of soils in which B. pseudomallei and B. thailandensis reside could help to determine which sites to study in future environmental surveillance studies. Furthermore, bacteria could have been present in a viable, but not cultivable state. It remains difficult to differentiate B. thailandensis and other members of the B. pseudomallei complex from B. pseudomallei by methods commonly available in clinical labs, even in developed countries, which may result in diagnostic confusion. Therefore, improving the detection and differentiation of members of the B. pseudomallei complex to improve patient care and appropriate public health responses is desired. Taken together, B. pseudomallei was not cultured from the soil of central Sierra Leone, but B. thailandensis with novel genotypes were found. B. thailandensis infection in humans have been sporadically reported in the literature in both the US and Asia [5–10]. B. thailandensis in general is considered a-virulent. As a result, clinical disease attributed to B. thailandensis is important. This also holds true for to the melioidosis research community, because no strict biocontainment conditions for B. thailandensis are required. The true clinical relevance of this soil-dwelling bacillus, however, remains to be elucidated. We encourage further environmental and sequencing studies on both B. pseudomallei and B. thailandensis to further understand the genetic diversity, virulence and evolution of these emerging organisms.
Supporting information
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We would like to thank the paramount chief of Yele, Bai Sunthuba Osara III, the soil sampling team Alie Osman Sesay, Moses Bangura, Foday Bangura and Anne Lia Cremers in Sierra Leone, in addition to Harjeet S. Virk, Rosan van der Lee, and Angelique Bijl for help in the laboratory. This publication made use of the Burkholderia pseudomallei MLST website (https://pubmlst.org/bpseudomallei/) cited at the University of Oxford (Jolley & Maiden 2010, BMC Bioinformatics, 11:595).
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This work was supported by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) research grant 2018 (to EB), the Amsterdam University Fund (to EB) and Foundation de Drie Lichten, The Netherlands (to EB); WJW is financially supported by the Netherlands Organization for Scientific Research [NOW; VIDI grant to WJW, grant number: 91716475]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Wiersinga WJ, Virk HS, Torres AG, Currie BJ, Peacock SJ, Dance DAB, et al. Melioidosis. Nat Rev Dis Primers. 2018;4:17107 10.1038/nrdp.2017.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trinh TT, Hoang TS, Tran DA, Trinh VT, Gohler A, Nguyen TT, et al. A simple laboratory algorithm for diagnosis of melioidosis in resource-constrained areas: a study from north-central Vietnam. Clin Microbiol Infect. 2018;24(1):84.e1–.e4. [DOI] [PubMed] [Google Scholar]
- 3.Tuanyok A, Mayo M, Scholz H, Hall CM, Allender CJ, Kaestli M, et al. Burkholderia humptydooensis sp. nov., a New Species Related to Burkholderia thailandensis and the Fifth Member of the Burkholderia pseudomallei Complex. Appl Environ Microbiol. 2017;83(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brett PJ, DeShazer D, Woods DE. Burkholderia thailandensis sp. nov., a Burkholderia pseudomallei-like species. Int J Syst Bacteriol. 1998;48 Pt 1:317–20. [DOI] [PubMed] [Google Scholar]
- 5.Glass MB, Gee JE, Steigerwalt AG, Cavuoti D, Barton T, Hardy RD, et al. Pneumonia and septicemia caused by Burkholderia thailandensis in the United States. J Clin MIcrobiol. 2006;44(12):4601–4. 10.1128/JCM.01585-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gee JE, Elrod MG, Gulvik CA, Haselow DT, Waters C, Liu L, et al. Burkholderia thailandensis Isolated from Infected Wound, Arkansas, USA. Emerg Infect Dis. 2018;24(11):2091–4. 10.3201/eid2411.180821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dance DAB, Sarovich D, Price EP, Limmathurotsakul D, Currie BJ. Human Infection with Burkholderia thailandensis, China, 2013. Emerg Infect Dis. 2018;24(5):953–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lertpatanasuwan N, Sermsri K, Petkaseam A, Trakulsomboon S, Thamlikitkul V, Suputtamongkol Y. Arabinose-positive Burkholderia pseudomallei infection in humans: case report. Clin Infect Dis. 1999;28(4):927–8. [DOI] [PubMed] [Google Scholar]
- 9.Chang K, Luo J, Xu H, Li M, Zhang F, Li J, et al. Human Infection with Burkholderia thailandensis, China, 2013. Emerg Infect Dis. 2017;23(8):1416–8. 10.3201/eid2308.170048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zueter AM, Abumarzouq M, Yusof MI, Wan Ismail WF, Harun A. Osteoarticular and soft-tissue melioidosis in Malaysia: clinical characteristics and molecular typing of the causative agent. J Infect Dev Ctries. 2017;11(1):28–33. 10.3855/jidc.7612 [DOI] [PubMed] [Google Scholar]
- 11.Birnie E, Wiersinga WJ, Limmathurotsakul D, Grobusch MP. Melioidosis in Africa: should we be looking more closely? Future Microbiol. 2015;10(2):273–81. 10.2217/fmb.14.113 [DOI] [PubMed] [Google Scholar]
- 12.Wall RA, Mabey DC, Corrah PT, Peters L. A case of melioidosis in West Africa. J Infect Dis. 1985;152(2):424–5. [DOI] [PubMed] [Google Scholar]
- 13.Limmathurotsakul D, Golding N, Dance DA, Messina JP, Pigott DM, Moyes CL, et al. Predicted global distribution of Burkholderia pseudomallei and burden of melioidosis. Nature Microbiol. 2016;1(1):15008. [DOI] [PubMed] [Google Scholar]
- 14.Limmathurotsakul D, Dance DA, Wuthiekanun V, Kaestli M, Mayo M, Warner J, et al. Systematic review and consensus guidelines for environmental sampling of Burkholderia pseudomallei. PLoS Negl Trop Dis. 2013;7(3):e2105 10.1371/journal.pntd.0002105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manivanh L, Pierret A, Rattanavong S, Kounnavongsa O, Buisson Y, Elliott I, et al. Burkholderia pseudomallei in a lowland rice paddy: seasonal changes and influence of soil depth and physico-chemical properties. Sci Reports. 2017;7(1):3031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wiersinga WJ, Birnie E, Weehuizen TA, Alabi AS, Huson MA, Huis RA. Clinical, environmental, and serologic surveillance studies of melioidosis in Gabon, 2012–2013. Emerg Infect Dis. 2015;21(1):40 10.3201/eid2101.140762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sim BM, Chantratita N, Ooi WF, Nandi T, Tewhey R, Wuthiekanun V, et al. Genomic acquisition of a capsular polysaccharide virulence cluster by non-pathogenic Burkholderia isolates. Genome Biol. 2010;11(8):R89 10.1186/gb-2010-11-8-r89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hantrakun V, Thaipadungpanit J, Rongkard P, Srilohasin P, Amornchai P, Langla S, et al. Presence of B. thailandensis and B. thailandensis expressing B. pseudomallei-like capsular polysaccharide in Thailand, and their associations with serological response to B. pseudomallei. PLoS Negl Trop Dis. 2018;12(1):e0006193 10.1371/journal.pntd.0006193 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.