Abstract
Atopic dermatitis (AD) is a chronic and inflammatory skin disease with intense pruritus and xerosis. AD pathogenesis is multifactorial, involving genetic, environmental, and immunological factors, including the participation of Staphylococcus aureus. This bacterium colonizes up to 30–100% of AD skin and its virulence factors are responsible for its pathogenicity and antimicrobial survival. This is a concise review of S. aureus superantigen-activated signaling pathways, highlighting their involvement in AD pathogenesis, with an emphasis on skin barrier disruption, innate and adaptive immunity dysfunction, and microbiome alterations. A better understanding of the combined mechanisms of AD pathogenesis may enhance the development of future targeted therapies for this complex disease.
Keywords: Staphylococcus aureus, enterotoxins, atopic dermatitis, innate immunity, adaptive immunity, microbiome
Introduction
Atopic dermatitis (AD) is a prevalent, chronic, inflammatory, and immune-mediated skin disease [1]. Complex interactions among susceptibility genes encoding skin barrier molecules [2], inflammatory response elements, environmental factors, and infectious agents (especially Staphylococcus aureus and herpes virus) that lead to dysbiosis of the microbial community resident in AD skin [3,4], together with the altered immunologic status of the host, are crucial elements in the pathophysiology of AD [5,6]. Bacterial infection is a powerful trigger for AD flares and has become a matter of concern due to the widespread occurrence of antibiotic-resistant strains (methicillin-resistant S. aureus; MRSA) [7,8].
S. aureus is a Gram-positive bacterium present in 20–30% of healthy subjects. Rates of S. aureus carriage in AD skin reach 30–100% [9,10]. S. aureus produces many virulence factors which determine its pathogenicity and antimicrobial survival, including secreted toxins, enzymes, and cell-surface-associated antigens [11]. Together, these factors allow this bacterium to elude the host’s natural defenses.
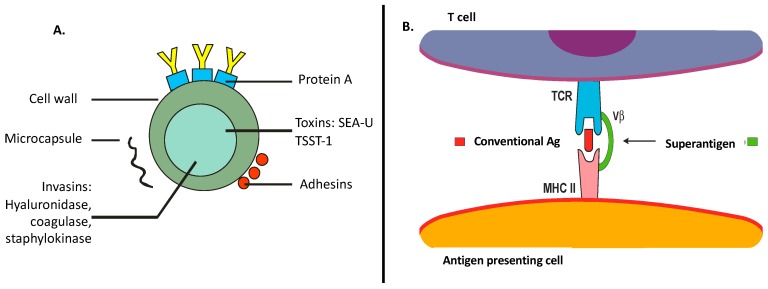
Single-lipid membranes, surrounded by a peptidoglycan and lipoteichoic acid layer anchored by diacylglycerol, are the components of S. aureus’ cell wall [11]. Of note, S. aureus products include a myriad of components that play specific roles in the inflammatory/immune response, as follows: (a) Superantigens (e.g., staphylococcal enterotoxins (SE)A–U and toxic shock syndrome toxin (TSST)-1)—proteins with high mitogenic properties, leading to T- and B-cell expansions causing clonal deletion and massive cytokine production. (b) Cytotoxins (e.g., α-toxin and leukocidins)—trigger cytokine production, hemolysis, and leukocyte cell death within targeting specific cell surface receptors. (c) Enzymes (e.g., β-toxin)—trigger cytotoxicity resulting in cell death, inflammation, and tissue barrier disruptions. (d) Adhesins—cell wall receptors for epidermal and dermal laminin and fibronectin. (e) Other enzymes (e.g., proteases and/or nucleases)—mediate host protein degradations that can also act on self-proteins to degrade biofilms for bacterial dissemination. Altogether, these toxins and enzymes provide critical nutrients that are essential for bacterial growth and survival, targeting different aspects of the host’s immune response and therefore contributing to S. aureus virulence (Figure 1A) [9,11,12].
Figure 1.
(A) Staphylococcus aureus main compounds that contribute to enhanced bacterial virulence factor. SE—staphylococcal enterotoxins; TSST-1—toxic shock syndrome toxin-1. (B) S. aureus as a superantigen: direct binding to the major histocompatibility complex (MHC) class II molecule, with specificity for the T-cell receptor (TCR)-Vβ chain.
S. aureus may act as a conventional antigen or as a superantigen to activate T cells. Unlike conventional antigens, superantigens do not need to be processed and can bind directly to the surface of the major histocompatibility complex (MHC) class II molecule with T-cell receptor (TCR) Vβ-chain specificity, generating a polyclonal T-cell stimulation (Figure 1B) [9,13,14]. Our group previously studied the effects of distinct antigens and mitogens (tetanic toxoid, Candida albicans, SEA, and phytohemagglutinin) in the proliferative response of peripheral blood mononuclear cells (PBMCs) from adults with AD and identified a decreased PBMC proliferation response to these stimuli, suggesting a compromised immune profile due to staphylococcal chronic skin colonization [13]. In this review, we focus on the role/mechanisms of S. aureus in the pathogenesis of AD.
1. Role of S. Aureus Toxins in the Disruption of the Skin Barrier and Innate Immunity
The skin is the first barrier to pathogens and, as a frontline defender, shows a remarkable immune function due to the presence of a diverse set of cells such as keratinocytes, dendritic cell (DCs), mast cells (MCs), and lymphocytes [15]. S. aureus has higher adhesion to corneocytes from AD patients than to those in non-AD individuals. This enhanced binding is mediated by the interaction between bacterial adhesins, such as protein A, and host surface receptors [16]. Moreover, staphylococcal toxins do have immune stimulatory abilities, and there is higher production of such toxins in strains isolated from AD individuals [17].
Most of the innate immune response relies on the identification of nonself molecules by pattern recognition receptors (PRRs). Toll-like receptors (TLRs) are one of the most critical classes of PRRs, particularly bacterial motifs. As membrane-associated receptors, they are expressed at the cell surface where they can survey the extracellular environment for pathogen clues, but are also found in endosomes, thus tracking intracellular stimuli [18]. TLR2 has been identified as a key receptor for S. aureus recognition due to its ability to identify lipoproteins, which are abundantly expressed in the cell wall of Gram-positive bacteria [18]. Interestingly, keratinocytes from AD patients show a reduced response to TLR2 agonists, with lower production of IL-6, IL-8, CCL20, and matrix metalloproteinase-9 (MMP-9) [19]. Although the mechanisms involved in this diminished response are still unknown, TLR2 expression in these cells are equivalent in both AD and healthy subjects. The dysfunction in TLR response in AD patients can be associated with deficiencies in the signaling components. Some studies point out that alterations in the myeloid differentiation protein (MyD88) pathway is needed for the development of SEB-induced AD-like phenotype [20,21].
In parallel with TLRs, another remarkable class of PRRs is the nucleotide-binding oligomerization domain (NOD)-like receptor (NLR) family. NLRs mainly work by forming multicomponent platforms known as inflammasomes, which drive the activation of protease caspase-1; S. aureus components activate the NLRP3 inflammasome [22]. In AD, S. aureus α-hemolysin is capable of activating this complex in keratinocytes, and inflammasome activation is greatly compromised due to the reduced expression of its components, driven by the action of T helper (Th)2 cytokines [23]. Nonetheless, keratinocytes may circumvent this limitation by producing IL-1β and IL-18 in an inflammasome-independent fashion in response to other S. aureus toxins, such as phenol-soluble modulins (PSM), which directly cause cell lysis and cytokine extravasation [24].
Moreover, α-hemolysin contributes to disruption of the skin barrier by interacting with lipid sphingomyelin, generating pores in the cell membrane that culminate in keratinocyte lysis. AD patients show a higher susceptibility to α-hemolysin action once Th2 cytokines promote the downregulation of acid sphingomyelinase, which increases the availability of α-hemolysin targets [25]. In addition, AD patients show defective filaggrin expression, contributing to disease severity. Filaggrin is highly expressed in differentiated keratinocytes and promotes the secretion of acid sphingomyelinase and resistance to α-hemolysin activity [26,27].
The α-toxin can also compromise the keratinocyte layer by altering E-cadherin integrity. Curiously, this effect can be blocked by pharmacological activation of the G-protein-coupled estrogen receptor (GPER), which ultimately promotes repression of the host protein ADAM10, a receptor for α-hemolysin responsible for cleaving E-cadherin [28]. Moreover, S. aureus could compromise the keratinocyte biology at the transcriptional level. Brauweiler et al. (2017) showed that S. aureus lipoteichoic acid (LTA) profoundly affects the keratinocyte genetic program, repressing genes associated with cell differentiation by interfering with the protein p63, which is a master transcription regulator in skin [29].
Using a murine model of S. aureus epicutaneous exposure to induce an AD-like disease, Liu et al. (2017) uncovered the role of PSMα in promoting IL-36 secretion by keratinocytes, which directly activates T cells to produce IL-17 and drives skin inflammation [30]. Interestingly, Baldry et al. (2018), using the same approach, suggested that another PSM, such as δ-toxin, would be more relevant to induce inflammation once the use of a mutant strain for δ-toxin or the pharmacological inhibition of its production with solonamide could efficiently block AD development [31]. In support of the latter findings, Matsuo et al. (2018) showed that δ-toxin, when combined with ovalbumin, could promote an AD-like phenotype without any other bacterial component, inducing production of the Th2-recruiting chemokines CCL17 and CCL22 in keratinocytes [32].
In sharp contrast to the epicutaneous model, previous systems such as tape stripping, in combination with chemically induced AD-like lesions, did not indicate a remarkable contribution of S. aureus toxins in AD pathogenesis. It is possible that the effects of toxins such as SEA were mostly coadjuvant, with mild contributions to the cytokine pool and disease phenotype due to the harsh stress caused by this method [33]. However, evidence from human skin biopsies did show a high expression of SEA in AD tissues, which suggests an indisputable contribution of these toxins to immune activation [34].
In addition to keratinocytes, S. aureus toxins also interfere in the activity of immune cells, particularly those which reside in or are recruited to the skin. Saloga et al. (1996) investigated the immune response kinetics after a single intracutaneous dose of SEB and showed the activation of resident Langerhans cells, degranulation of MCs, and recruitment of eosinophils followed by the influx of mononuclear cells (monocytes/macrophages and lymphocytes) [35]. Thus, staphylococcal toxins alone may exert multiple actions on skin immunity.
A milestone work from Nakamura et al. (2013) demonstrated that the δ-toxin is one of the main activators of MCs, triggering their degranulation and reinforcing the causal link between S. aureus colonization and AD development [31]. δ-Toxin promotes MC degranulation by activating the receptor Mas-related G-protein-coupled receptor member X2 (MRGPRX2), promoting Ca2+ influx and release of granule content. As MRGPRX2 is also expressed in keratinocytes, this suggests that the contribution of δ-toxin to AD pathogenesis can be extended to other cell types [36]. Interestingly, SEB was initially proposed to inhibit IL-4 production in the MC line HMC-1 [37], but whether this effect applies to primary MCs is still unknown.
Other granulocytes can also infiltrate AD lesions. Basophils can release histamine in response to a diverse set of S. aureus toxins in an IgE-dependent manner [38,39], while eosinophils respond to SEB, protein A, and peptidoglycan through the receptor CD48 with secretion of the enzyme eosinophil peroxidase and the neutrophil chemoattractant IL-8 [40]. Staphylococcal toxins inhibit eosinophil apoptosis, therefore not only triggering but also perpetuating the allergic response by postponing cell death [41].
DCs belongs to a key immune population in the initiation and polarization of T-cell responses due to their ability to present antigens and to secrete polarizing factors according to different stimuli [42,43]. Concerning their role in AD pathogenesis, SEB-stimulated DCs develop a Th2-polarizing phenotype, which supports the atopic profile in these patients [44]. In turn, Th2 products may affect the innate response as described by Kasraie et al. (2016), who showed that IL-31, a T-cell cytokine involved in pruritus, activates monocytes and macrophages, enhancing the inflammatory response [45].
Curiously, the altered DC phenotype in AD patients is not limited to resident skin populations. Kapitány et al. (2017) observed that CD1c+ blood pre-DCs, precursors of dermal DCs from AD patients, have an altered response (either constitutively or after SEB stimulation), with heightened production of Th2-associated chemokines [46]. These authors also noticed that these cells are more premature, which could be the result of the particular serum cytokine signature in those patients or due to an altered hemopoiesis with early release of immature cells. These results reinforce the notion that AD is far beyond a restricted dermatological disease but rather a condition of systemic immune dysfunction. Indeed, some works showed that epicutaneous SEB sensitization can enhance Th17-driven lung inflammation by inducing the production of the IL-17 polarizing cytokine IL-6 [47] and that α-toxin can help infection by viruses, such as herpes simplex virus 1, by facilitating viral entry into the host cell [48].
Intriguingly, while SEB induced apoptosis of the human monocytic cell line THP-1 [49], similar to what was described for T cells [50], TSST-1 showed the opposite effect, protecting primary monocytes from death [51]. The proposed mechanism of action for SEB-induced death relies on induction of TNF-α, which activates the extrinsic apoptotic pathway [49], while TSST-1 promotes GM-CSF (Granulocyte Macrophage Colony-Stimulating Factor) secretion, promoting cell survival [51]. The scenario that prevails in the host may depend on multiple factors, such as the host immune response or differences in the toxin profile secreted among different S. aureus strains.
SEB efficiently activates monocytes, inducing production of TNF-α in a TLR2- and TLR4-dependent way, in nonatopic individuals compared to AD patients, corroborating the anergic/exhausted profile described in AD [52]. Similarly, α-toxin was a strong inducer of CXCL10 in macrophages from healthy individuals but not in AD counterparts [53], which could contribute to a dampened Th1 response in atopic subjects. A possible explanation could rely on the reduced expression of immune receptors such as the lower expression of TLR2 in AD macrophages [54], which can compromise the triggering of an effective immune response, allowing bacterial overgrowth. Although α-toxin was shown to promote TLR2 expression in monocytes from non-AD subjects, thus enhancing their cytokine response [55], the effects on AD cells can have a divergent outcome, supporting the atopic response.
The host genetic background must be considered for a full appreciation of the immune mechanisms triggered by staphylococcal toxins. Krogman et al. (2017), using transgenic mice expressing different alleles of HLA-DR (Human Leukocyte Antigen – DR isotype) molecules, showed how the immune response changes in response to TSST-1, with some alleles favoring an increased inflammatory response and tissue damage [56]. Nieburh et al. (2008) identified a single-nucleotide polymorphism in the TLR2 gene from AD patients that increases the production of IL-6 and IL-12p70 by monocytes [57], potentially aggravating their inflammatory reaction. Those genetic differences may help to explain why AD patients show very intense S. aureus proliferation and respond with deleterious inflammation, even though the bacterium is a component of skin microbiota. Another variable that should be considered is the age of the host, since atopic children may exhibit different response kinetics to bacterial antigens than adults [52].
Newer evidence suggests that in addition to their inflammation-promoting roles, staphylococcal toxins may also counterbalance the host regulatory mechanisms. Though glucocorticoids (GC) are a common therapeutic strategy in AD management, utilizing the glucocorticoid receptor (GR) to dampen the inflammatory reaction, some patients become unresponsive to treatment. Huang et al. (2018) showed that SEB can block GC action by impeding the nuclear translocation of GR in keratinocytes, favoring the persistence of inflammation [58]. Also, staphylococcal enterotoxins can modulate the induction of myeloid-derived suppressor cells (MDSCs). While lower doses of toxins favor MDSC generation, higher doses (the likely scenario in AD patients who show S. aureus overgrowth) modulate MDSC response, thus circumventing inflammation control [59].
2. S. Aureus: Straight Relationship with Adaptive Immunity in AD
Decreased skin microbiota diversity associated with high susceptibility to S. aureus colonization [10,60,61] is described in the skin of AD patients. S. aureus is able to secrete more than 20 different toxins that play an important role in AD adaptive immune response. Around 60% of isolated S. aureus strains are capable of secreting exotoxins [62], acting on distinct T- and B-cell pathways. As superantigens, they can stimulate cytokine secretion and T-cell proliferation; as conventional allergens, they can induce production of staphylococcal-specific IgE exotoxin [63].
Classically, AD immune pathogenesis is described as a dysfunction of the Th1/Th2 balance [64]. Acute flares of AD are characterized by Th2 and Th22 cell infiltrates, whereas Th1 cells are detected in chronic lesions [65]. However, there are reports of novel subsets of human Th cells, such as Th17 and Th22 cells [66], that are present in the inflammatory response of AD [5,27,64,67]. AD has several immune subtype profiles, all having a common Th2/Th22 polarization, but also displays differential immune skewing, such as increased Th17 that has been identified in the skin of intrinsic, Asian, and early pediatric AD patients [68]. Th17-derived IL-17 is able to coordinate local tissue inflammation through upregulation of proinflammatory cytokines and chemokines, including IL-6, TNF-α, IL-1β, CXCL1, CCL2, CXCL2, CCL7, and CCL20 [67]. In cooperation with IL-17, IL-22 triggers antimicrobial peptide production and initiates an acute phase response [69,70]. In recent publications, there was expression of Th22 cells and IL-22-producing CD8+ T cells present in acute and chronic AD skin lesions [65,71].
The major Th2 cytokine involved in AD acute flares is IL-4, which mediates enhanced expression of fibronectin and fibrinogen, working as adhesion molecules for S. aureus and therefore contributing to AD skin bacterial chronic colonization. AD patients with colonized skin by S. aureus have increased disease severity, elevated eosinophil blood counts, total IgE serum levels, CCL17 and periostin (Th2 biomarkers) plasma levels, and suppressed activity of Treg cells [72] when compared with those without S. aureus colonization [73], corroborating the chronic immune activation described in AD.
Th2 cells can also incite B cells, which leads to IgE and IL-5 production, stimulating maturation and survival of eosinophils in some types of AD [65]. Furthermore, purified eosinophils from AD patients stimulated with TLR2/6 agonist and SEB showed decreased levels of TIMP-1, TIMP-2, and CCL5, revealing a potential breakdown in the remodeling process mediated by eosinophils [74].
B-cell activation can also be modulated by S. aureus exotoxins (working as allergens) and stimulating exotoxin-specific IgE antibody production. SEA- or SEB-specific IgE levels are significantly elevated in the plasma of children with AD and correlate with disease severity when compared with non-AD children [75]. Enhanced production of IgE antibodies against S. aureus antigens is also described in adults with AD and is associated with asthma severity [76]. B cells are also a relevant source of cytokine secretion by a T-cell-independent pathway. Parcina et al. (2013) demonstrated that protein A, an important virulence factor of S. aureus, induced increased B-cell proliferation and regulatory B cells (Breg) secreting IL-10 via the plasmacytoid dendritic cells (pDC) pathway [77], suggesting a tolerogenic immune profile in AD.
Pruritus is one of the major symptoms in AD patients and it is associated with impaired quality of life, as demonstrated in studies evaluating the patients’ perspectives of the disease using PO-SCORAD [78,79]. IL-31 is a Th2 cytokine associated with AD severity and pruritus [80,81]. Staphylococcal toxins, such as α-toxin and SEB, are capable of inducing a potent secretion of IL-31 by CD4+ T cells in AD patients [45,82].
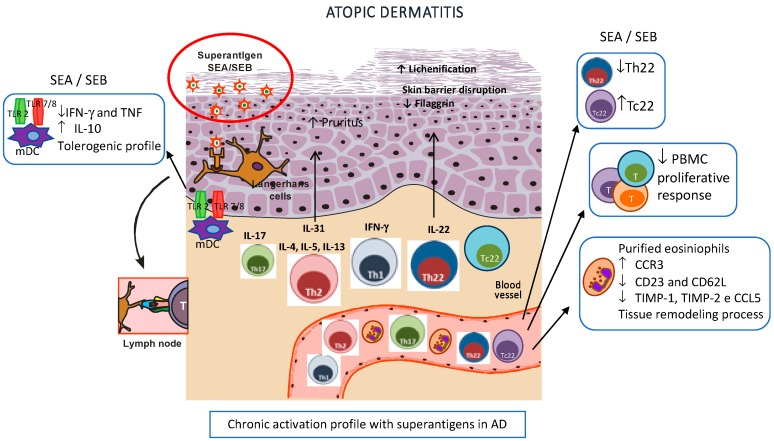
In Figure 2, we have summarized the noteworthy findings in AD pathogenesis related to chronic staphylococcal enterotoxin activation described in previous studies by our group.
Figure 2.
Superantigen-activated dendritic cells stimulate T helper (Th)2 cells to produce IL-4, IL-5, IL-13, and IL-31, leading to skin barrier disruption, decreased antimicrobial peptide production, impaired keratinocyte differentiation, and pruritus. In chronic atopic dermatitis (AD), there is an enrollment of Th1, Th22, and Th17 subsets that leads to epidermal thickening and abnormal keratinocyte proliferation (lichenification). Effects of staphylococcal enterotoxins in AD: 1. Dysfunctional CD4+ IL-22-secreting T cells and upregulated Tc22 cells. 2. Reduced peripheral blood mononuclear cell (PBMC) proliferative response corroborating an exhausted immune profile. 3. Increased frequency of CCR3+ and decreased expression of CD23 and CD62L receptors, and TIMP-1, TIMP-2, and CCL5 in purified eosinophils of AD patients even in a nonstimulated condition, indicating a potential breakdown in the tissue remodeling process in AD mediated by eosinophils. 4. Enhanced frequency of IL-10 under TLR4 and decreased frequency of IFN-γ and TNF under TLR2 and 7/8 stimulation in classic mDC (myeloid dendritic cells), indicating a tolerogenic profile in AD. All these findings together corroborate the chronic activated profile related to superantigens in AD pathogenesis.
3. Microbiome and AD
An assembly of microbiota resides our human skin and cohabits in an established balance [10]. The molecular approach to the human microbiome reveals high diversity of skin microbiota within and between distinct topographical regions [10,61,83,84].
In patients with AD, the skin microbiota is altered by endogenous factors, such as skin barrier protein mutations (filaggrin, among others) or exogenous stimuli, such as soaps, topical corticosteroids, and antibiotics, leading to a modified/noneffective response of the host to allergens, pathogens, and tissue damage [85].
The microbiome can exert both beneficial and harmful influences in AD skin once it interacts with the local immune system [86]. S. aureus is directly correlated with increased expression of IL-4, IL-13, IL-22, IL-31, TSLP, and other cytokines and decreased expression of cathelicidin, evidencing the impact of skin dysbiosis on disease exacerbation [87]. An example of a beneficial relationship between bacteria and the skin is that the commensal bacterium Staphylococcus epidermidis modulates TLR3-dependent inflammation by initiating a TLR2-mediated cross-talk mechanism to suppress inflammation, indicating that more microbiome diversity seems to be more beneficial once a diverse ecosystem is more resistant [88], suggesting that the timing of exposure to commensal bacteria may affect the development of tolerance.
When analyzing lesional skin and S. aureus colonization in AD subjects, there is evidence of loss of microbial diversity during acute flares in patients with AD, in contrast with microbiome diversity restoration after successful anti-inflammatory treatment [61]. Kennedy et al. showed relevant findings such as the absence of S. aureus colonization of children prior to AD onset and colonization of antecubital fossa with commensal staphylococci at month two in infants, which is associated with decreased incidence of AD at the age of one year [89].
Furthermore, the characterization of the microbiome in children and adults with AD still requires more studies. Shi et al. [90] recently published data on microbiome studies performed in both pediatric and adult patients with AD. These authors detected significant differences in the microbiome profile of AD individuals, with two defined patterns according to age (young children and adults–teenagers). Microbiome diversity was increased in nonlesional skin of young patients when compared with adults. Staphylococcus was abundant in nonlesional and lesional AD skin in both age groups, suggesting susceptibility to pathogen colonization [90].
Recent studies indicate that certain strains of commensal flora composed of coagulase-negative staphylococci (CoNS) compete with S. aureus on the skin, increasing antimicrobial peptide production [10,91]. Additional studies in AD individuals are needed to confirm whether colonization with commensal bacteria will modulate the uncontrolled immune response with clinical improvement of the cutaneous lesions in AD patients.
4. Perspectives Targeting S. Aureus in AD
Increasing evidence corroborates that S. aureus has a pivotal role in AD pathogenesis, correlating with disease flares and severity. However, many questions remain unresolved, especially regarding the best strategy against S. aureus in AD skin.
Well-established AD treatment options, such as narrowband UVB phototherapy, systemic cyclosporine, topical corticosteroids, and calcineurin inhibitors, indicate that therapeutic success is a reflection of the immunomodulatory mechanism of action suppressing staphylococcal-enterotoxin-activated T cells, improving the skin barrier function, and consequently decreasing S. aureus colonization [92]. Recent assays have evaluated the effect of dupilumab (anti-IL-4Rα) on the host–microbe interface in atopic dermatitis (available online in clinicaltrials.gov, identifier: NCT03389893) [92]. Likewise, other monoclonal antibodies are under investigation, for example, nemolizumab (CIM331), a humanized antibody against the IL-31 receptor [93] (clinicaltrials.gov, identifier: NCT01986933). Furthermore, it is important for future research to address the interactions between the gut and skin microbiomes, including S. aureus species, and therapies targeting the immune system via microbioma modulation
A recent AD clinical trial utilizing topical application of commensal Roseomonas mucosa demonstrated significant decreases in disease severity scores, topical steroid requirements, and S. aureus colonization, with no adverse events or treatment complications [94].
We also have to consider that vaccines against S. aureus represent a possible novel approach to manipulating the AD skin microbiome. Next-generation anti-S. aureus vaccines will require an association between targeting specific effector T-cell subsets combined with inducing specific neutralizing antitoxin antibodies [10,92,95].
One remarkable point for future therapeutic target strategies for AD should address the interaction between host and pathogen, focusing on the pathogenic role of staphylococcal enterotoxins in modulating cytokine release by activated effector T cells and affecting population-level responses to pathogens.
Acknowledgments
We are thankful to the Laboratory of Dermatology and Immunodeficiencies (LIM-56), Department of Dermatology, University of Sao Paulo Medical School.
Author Contributions
Conceptualization, Writing—Review and Editing, Supervision: R.L.O., M.N.S. and V.A.; Writing—Original Draft Preparation: F.S.Y.Y. and J.F.L.; Review of literature: Y.Á.L.R.; All authors contributed to discussing and reviewing the manuscript.
Funding
This research was funded by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), grants number 2016/24161-1 and 2018/23211-0.
Conflicts of Interest
The authors declare no conflict of interests.
Key Contribution
A better understanding of the role/mechanisms of S. aureus in the pathogenesis of AD may contribute to the development of future targeted therapies for this complex disease.
References
- 1.Leung D.Y.M. New insights into atopic dermatitis: Role of skin barrier and immune dysregulation. Allergol. Int. 2013;62:151–161. doi: 10.2332/allergolint.13-RAI-0564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elias P.M., Schmuth M. Abnormal skin barrier in the etiopathogenesis of atopic dermatitis. Curr. Opin. Allergy Clin. Immunol. 2009;9:437–446. doi: 10.1097/ACI.0b013e32832e7d36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salava A., Lauerma A. Role of the skin microbiome in atopic dermatitis. Clin. Trans. Allergy. 2014;4:33. doi: 10.1186/2045-7022-4-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakatsuji T., Chen T.H., Narala S., Chun K.A., Two A.M., Yun T., Shafiq F., Kotol P.F., Bouslimani A., Melnik A.V., et al. Antimicrobials from human skin commensal bacteria protect against staphylococcus aureus and are deficient in atopic dermatitis. Sci. Transl. Med. 2017;9 doi: 10.1126/scitranslmed.aah4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hayashida S., Uchi H., Moroi Y., Furue M. Decrease in circulating th17 cells correlates with increased levels of ccl17, ige and eosinophils in atopic dermatitis. J. Dermatol. Sci. 2011;61:180–186. doi: 10.1016/j.jdermsci.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 6.De Benedetto A., Agnihothri R., McGirt L.Y., Bankova L.G., Beck L.A. Atopic dermatitis: A disease caused by innate immune defects? J. Investig. Dermatol. 2009;129:14–30. doi: 10.1038/jid.2008.259. [DOI] [PubMed] [Google Scholar]
- 7.Saeed K., Marsh P., Ahmad N. Cryptic resistance in staphylococcus aureus: A risk for the treatment of skin infection? Curr. Opin. Infectious Dis. 2014;27:130–136. doi: 10.1097/QCO.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 8.Turner N.A., Sharma-Kuinkel B.K., Maskarinec S.A., Eichenberger E.M., Shah P.P., Carugati M., Holland T.L., Fowler V.G., Jr. Methicillin-resistant staphylococcus aureus: An overview of basic and clinical research. Nat. Rev. Microbiol. 2019;17:203–218. doi: 10.1038/s41579-018-0147-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krakauer T. Update on staphylococcal superantigen-induced signaling pathways and therapeutic interventions. Toxins. 2013;5:1629–1654. doi: 10.3390/toxins5091629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paller A.S., Kong H.H., Seed P., Naik S., Scharschmidt T.C., Gallo R.L., Luger T., Irvine A.D. The microbiome in patients with atopic dermatitis. J. Allergy Clin. Immunol. 2019;143:26–35. doi: 10.1016/j.jaci.2018.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oliveira D., Borges A., Simoes M. Staphylococcus aureus toxins and their molecular activity in infectious diseases. Toxins. 2018;10:252. doi: 10.3390/toxins10060252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tam K., Torres V.J. Staphylococcus aureus secreted toxins and extracellular enzymes. Microbiol. Spectr. 2019;7:2. doi: 10.1128/microbiolspec.GPP3-0039-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orfali R.L., Sato M.N., Takaoka R., Azor M.H., Rivitti E.A., Hanifin J.M., Aoki V. Atopic dermatitis in adults: Evaluation of peripheral blood mononuclear cells proliferation response to staphylococcus aureus enterotoxins a and b and analysis of interleukin-18 secretion. Exp. Dermatology. 2009;18:628–633. doi: 10.1111/j.1600-0625.2009.00842.x. [DOI] [PubMed] [Google Scholar]
- 14.Tuffs S.W., Haeryfar S.M.M., McCormick J.K. Manipulation of innate and adaptive immunity by staphylococcal superantigens. Pathogens. 2018;7:53. doi: 10.3390/pathogens7020053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matejuk A. Skin immunity. Arch. Immunol. Ther. Exp. (Warsz) 2018;66:45–54. doi: 10.1007/s00005-017-0477-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cole G.W., Silverberg N.L. The adherence of staphylococcus aureus to human corneocytes. Arch. Dermatol. 1986;122:166–169. doi: 10.1001/archderm.1986.01660140056017. [DOI] [PubMed] [Google Scholar]
- 17.Ezepchuk Y.V., Leung D.Y., Middleton M.H., Bina P., Reiser R., Norris D.A. Staphylococcal toxins and protein a differentially induce cytotoxicity and release of tumor necrosis factor-alpha from human keratinocytes. J. Investig. Dermatol. 1996;107:603–609. doi: 10.1111/1523-1747.ep12583377. [DOI] [PubMed] [Google Scholar]
- 18.Kumar H., Kawai T., Akira S. Pathogen recognition by the innate immune system. Int. Rev. Immunol. 2011;30:16–34. doi: 10.3109/08830185.2010.529976. [DOI] [PubMed] [Google Scholar]
- 19.Niebuhr M., Heratizadeh A., Wichmann K., Satzger I., Werfel T. Intrinsic alterations of pro-inflammatory mediators in unstimulated and tlr-2 stimulated keratinocytes from atopic dermatitis patients. Exp. Dermatol. 2011;20:468–472. doi: 10.1111/j.1600-0625.2011.01277.x. [DOI] [PubMed] [Google Scholar]
- 20.Kissner T.L., Ruthel G., Cisney E.D., Ulrich R.G., Fernandez S., Saikh K.U. Myd88-dependent pro-inflammatory cytokine response contributes to lethal toxicity of staphylococcal enterotoxin b in mice. Innate Immun. 2011;17:451–462. doi: 10.1177/1753425910374092. [DOI] [PubMed] [Google Scholar]
- 21.Fassbender S., Opitz F.V., Johnen S., Forster I., Weighardt H. Myd88 contributes to staphylococcal enterotoxin b-triggered atopic dermatitis-like skin inflammation in mice. J. Investig. Dermatol. 2017;137:1802–1804. doi: 10.1016/j.jid.2017.04.015. [DOI] [PubMed] [Google Scholar]
- 22.Munoz-Planillo R., Franchi L., Miller L.S., Nunez G. A critical role for hemolysins and bacterial lipoproteins in staphylococcus aureus-induced activation of the nlrp3 inflammasome. J. Immunol. 2009;183:3942–3948. doi: 10.4049/jimmunol.0900729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Niebuhr M., Baumert K., Heratizadeh A., Satzger I., Werfel T. Impaired nlrp3 inflammasome expression and function in atopic dermatitis due to th2 milieu. Allergy. 2014;69:1058–1067. doi: 10.1111/all.12428. [DOI] [PubMed] [Google Scholar]
- 24.Syed A.K., Reed T.J., Clark K.L., Boles B.R., Kahlenberg J.M. Staphlyococcus aureus phenol-soluble modulins stimulate the release of proinflammatory cytokines from keratinocytes and are required for induction of skin inflammation. Infect. Immun. 2015;83:3428–3437. doi: 10.1128/IAI.00401-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brauweiler A.M., Goleva E., Leung D.Y.M. Th2 cytokines increase staphylococcus aureus alpha toxin-induced keratinocyte death through the signal transducer and activator of transcription 6 (stat6) J. Investig. Dermatol. 2014;134:2114–2121. doi: 10.1038/jid.2014.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brauweiler A.M., Bin L., Kim B.E., Oyoshi M.K., Geha R.S., Goleva E., Leung D.Y. Filaggrin-dependent secretion of sphingomyelinase protects against staphylococcal alpha-toxin-induced keratinocyte death. J. Allergy Clin. Immunol. 2013;131:421–427. doi: 10.1016/j.jaci.2012.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Batista D.I.S., Perez L., Orfali R.L., Zaniboni M.C., Samorano L.P., Pereira N.V., Sotto M.N., Ishizaki A.S., Oliveira L.M.S., Sato M.N., et al. Profile of skin barrier proteins (filaggrin, claudins 1 and 4) and th1/th2/th17 cytokines in adults with atopic dermatitis. J. Eur. Acad. Dermatol. Venereol. 2015;29:1091–1095. doi: 10.1111/jdv.12753. [DOI] [PubMed] [Google Scholar]
- 28.Triplett K.D., Pokhrel S., Castleman M.J., Daly S.M., Elmore B.O., Joyner J.A., Sharma G., Herbert G., Campen M.J., Hathaway H.J., et al. Gper activation protects against epithelial barrier disruption by staphylococcus aureus alpha-toxin. Sci. Rep. 2019;9:1343. doi: 10.1038/s41598-018-37951-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brauweiler A.M., Hall C.F., Goleva E., Leung D.Y.M. Staphylococcus aureus lipoteichoic acid inhibits keratinocyte differentiation through a p63-mediated pathway. J. Investig. Dermatol. 2017;137:2030–2033. doi: 10.1016/j.jid.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu H., Archer N.K., Dillen C.A., Wang Y., Ashbaugh A.G., Ortines R.V., Kao T., Lee S.K., Cai S.S., Miller R.J., et al. Staphylococcus aureus epicutaneous exposure drives skin inflammation via il-36-mediated t cell responses. Cell Host Microbe. 2017;22:653–666 e655. doi: 10.1016/j.chom.2017.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baldry M., Nakamura Y., Nakagawa S., Frees D., Matsue H., Nunez G., Ingmer H. Application of an agr-specific antivirulence compound as therapy for staphylococcus aureus-induced inflammatory skin disease. J. Infect. Dis. 2018;218:1009–1013. doi: 10.1093/infdis/jiy259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matsuo K., Nagakubo D., Komori Y., Fujisato S., Takeda N., Kitamatsu M., Nishiwaki K., Quan Y.S., Kamiyama F., Oiso N., et al. Ccr4 is critically involved in skin allergic inflammation of balb/c mice. J. Investig. Dermatol. 2018;138:1764–1773. doi: 10.1016/j.jid.2018.02.027. [DOI] [PubMed] [Google Scholar]
- 33.Kim B.S., Choi J.K., Jung H.J., Park K.H., Jang Y.H., Lee W.J., Lee S.J., Kim S.H., Kang H.Y., Kim J.M., et al. Effects of topical application of a recombinant staphylococcal enterotoxin a on dncb and dust mite extract-induced atopic dermatitis-like lesions in a murine model. Eur. J. Dermatol. 2014;24:186–193. doi: 10.1684/ejd.2014.2302. [DOI] [PubMed] [Google Scholar]
- 34.Lee H.W., Kim S.M., Kim J.M., Oh B.M., Kim J.Y., Jung H.J., Lim H.J., Kim B.S., Lee W.J., Lee S.J., et al. Potential immunoinflammatory role of staphylococcal enterotoxin a in atopic dermatitis: Immunohistopathological analysis and in vitro assay. Ann. Dermatol. 2013;25:173–180. doi: 10.5021/ad.2013.25.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saloga J., Leung D.Y., Reardon C., Giorno R.C., Born W., Gelfand E.W. Cutaneous exposure to the superantigen staphylococcal enterotoxin b elicits a t-cell-dependent inflammatory response. J. Investig. Dermatol. 1996;106:982–988. doi: 10.1111/1523-1747.ep12338479. [DOI] [PubMed] [Google Scholar]
- 36.Azimi E., Reddy V.B., Lerner E.A. Brief communication: Mrgprx2, atopic dermatitis and red man syndrome. Itch (Philadelphia, Pa.) 2017;2:e5. doi: 10.1097/itx.0000000000000005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ackermann L., Pelkonen J., Harvima I.T. Staphylococcal enterotoxin b inhibits the production of interleukin-4 in a human mast-cell line hmc-1. Immunology. 1998;94:247–252. doi: 10.1046/j.1365-2567.1998.00508.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jorgensen J., Bach-Mortensen N., Koch C., Fomsgaard A., Baek L., Jarlov J.O., Espersen F., Jensen C.B., Skov P.S., Norn S. Bacteria and endotoxin induce release of basophil histamine in patients with atopic dermatitis. In vitro experiments with s. Aureus, teichoic acid, e. Coli and e. Coli lps. Allergy. 1987;42:395–397. doi: 10.1111/j.1398-9995.1987.tb02227.x. [DOI] [PubMed] [Google Scholar]
- 39.Wehner J., Neuber K. Staphylococcus aureus enterotoxins induce histamine and leukotriene release in patients with atopic eczema. Br. J. Dermatol. 2001;145:302–305. doi: 10.1046/j.1365-2133.2001.04352.x. [DOI] [PubMed] [Google Scholar]
- 40.Minai-Fleminger Y., Gangwar R.S., Migalovich-Sheikhet H., Seaf M., Leibovici V., Hollander N., Feld M., Moses A.E., Homey B., Levi-Schaffer F. The cd48 receptor mediates staphylococcus aureus human and murine eosinophil activation. Clin. Exp. Allergy. 2014;44:1335–1346. doi: 10.1111/cea.12422. [DOI] [PubMed] [Google Scholar]
- 41.Wedi B., Wieczorek D., Stunkel T., Breuer K., Kapp A. Staphylococcal exotoxins exert proinflammatory effects through inhibition of eosinophil apoptosis, increased surface antigen expression (cd11b, cd45, cd54, and cd69), and enhanced cytokine-activated oxidative burst, thereby triggering allergic inflammatory reactions. J. Allergy Clin. Immunol. 2002;109:477–484. doi: 10.1067/mai.2002.121702. [DOI] [PubMed] [Google Scholar]
- 42.Mildner A., Jung S. Development and function of dendritic cell subsets. Immunity. 2014;40:642–656. doi: 10.1016/j.immuni.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 43.dos Santos V.G., Orfali R.L., Titz T.D., Duarte A.J.D., Sato M.N., Aoki V. Evidence of regulatory myeloid dendritic cells and circulating inflammatory epidermal dendritic cells-like modulated by toll-like receptors 2 and 7/8 in adults with atopic dermatitis. Int. J. Dermatol. 2017;56:630–635. doi: 10.1111/ijd.13537. [DOI] [PubMed] [Google Scholar]
- 44.Mandron M., Aries M.F., Brehm R.D., Tranter H.S., Acharya K.R., Charveron M., Davrinche C. Human dendritic cells conditioned with staphylococcus aureus enterotoxin b promote th2 cell polarization. J. Allergy Clin. Immunol. 2006;117:1141–1147. doi: 10.1016/j.jaci.2005.12.1360. [DOI] [PubMed] [Google Scholar]
- 45.Kasraie S., Niebuhr M., Werfel T. Interleukin (il)-31 induces pro-inflammatory cytokines in human monocytes and macrophages following stimulation with staphylococcal exotoxins. Allergy. 2010;65:712–721. doi: 10.1111/j.1398-9995.2009.02255.x. [DOI] [PubMed] [Google Scholar]
- 46.Kapitany A., Beke G., Nagy G., Doan-Xuan Q.M., Bacso Z., Gaspar K., Boros G., Dajnoki Z., Biro T., Rajnavolgyi E., et al. Cd1c+ blood dendritic cells in atopic dermatitis are premature and can produce disease-specific chemokines. Acta Derm. -Venereol. 2017;97:325–331. doi: 10.2340/00015555-2540. [DOI] [PubMed] [Google Scholar]
- 47.Yu J., Oh M.H., Park J.U., Myers A.C., Dong C., Zhu Z., Zheng T. Epicutaneous exposure to staphylococcal superantigen enterotoxin b enhances allergic lung inflammation via an il-17a dependent mechanism. PLoS ONE. 2012;7:e39032. doi: 10.1371/journal.pone.0039032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bin L., Kim B.E., Brauweiler A., Goleva E., Streib J., Ji Y., Schlievert P.M., Leung D.Y. Staphylococcus aureus alpha-toxin modulates skin host response to viral infection. J. Allergy Clin. Immunol. 2012;130:683–691 e682. doi: 10.1016/j.jaci.2012.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang X., Shang W., Yuan J., Hu Z., Peng H., Zhu J., Hu Q., Yang Y., Liu H., Jiang B., et al. Positive feedback cycle of tnfalpha promotes staphylococcal enterotoxin b-induced thp-1 cell apoptosis. Front. Cell. Infection Microbiol. 2016;6:109. doi: 10.3389/fcimb.2016.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kedzierska A., Kaszuba-Zwoinska J., Slodowska-Hajduk Z., Kapinska-Mrowiecka M., Czubak M., Thor P., Wojcik K., Pryjma J. Seb-induced t cell apoptosis in atopic patients--correlation to clinical status and skin colonization by staphylococcus aureus. Arch. Immunol. Ther. Exp. 2005;53:63–70. [PubMed] [Google Scholar]
- 51.Bratton D.L., May K.R., Kailey J.M., Doherty D.E., Leung D.Y. Staphylococcal toxic shock syndrome toxin-1 inhibits monocyte apoptosis. J. Allergy Clin. Immunol. 1999;103:895–900. doi: 10.1016/S0091-6749(99)70435-5. [DOI] [PubMed] [Google Scholar]
- 52.Mandron M., Aries M.F., Boralevi F., Martin H., Charveron M., Taieb A., Davrinche C. Age-related differences in sensitivity of peripheral blood monocytes to lipopolysaccharide and staphylococcus aureus toxin b in atopic dermatitis. J. Investig. Dermatol. 2008;128:882–889. doi: 10.1038/sj.jid.5701112. [DOI] [PubMed] [Google Scholar]
- 53.Kasraie S., Niebuhr M., Kopfnagel V., Dittrich-Breiholz O., Kracht M., Werfel T. Macrophages from patients with atopic dermatitis show a reduced cxcl10 expression in response to staphylococcal alpha-toxin. Allergy. 2012;67:41–49. doi: 10.1111/j.1398-9995.2011.02710.x. [DOI] [PubMed] [Google Scholar]
- 54.Niebuhr M., Lutat C., Sigel S., Werfel T. Impaired tlr-2 expression and tlr-2-mediated cytokine secretion in macrophages from patients with atopic dermatitis. Allergy. 2009;64:1580–1587. doi: 10.1111/j.1398-9995.2009.02050.x. [DOI] [PubMed] [Google Scholar]
- 55.Niebuhr M., Schorling K., Heratizadeh A., Werfel T. Staphylococcal alpha-toxin induces a functional upregulation of tlr-2 on human peripheral blood monocytes. Exp. Dermatol. 2015;24:381–383. doi: 10.1111/exd.12674. [DOI] [PubMed] [Google Scholar]
- 56.Krogman A., Tilahun A., David C.S., Chowdhary V.R., Alexander M.P., Rajagopalan G. Hla-dr polymorphisms influence in vivo responses to staphylococcal toxic shock syndrome toxin-1 in a transgenic mouse model. HLA. 2017;89:20–28. doi: 10.1111/tan.12930. [DOI] [PubMed] [Google Scholar]
- 57.Niebuhr M., Langnickel J., Draing C., Renz H., Kapp A., Werfel T. Dysregulation of toll-like receptor-2 (tlr-2)-induced effects in monocytes from patients with atopic dermatitis: Impact of the tlr-2 r753q polymorphism. Allergy. 2008;63:728–734. doi: 10.1111/j.1398-9995.2008.01721.x. [DOI] [PubMed] [Google Scholar]
- 58.Huang K., Ran L., Wang W., Zhou R., Cai X., Li R., Li Y., Zhou C., He W., Wang R. Glucocorticoid insensitivity by staphylococcal enterotoxin b in keratinocytes of allergic dermatitis is associated with impaired nuclear translocation of the glucocorticoid receptor alpha. J. Dermatological Sci. 2018;92:272–280. doi: 10.1016/j.jdermsci.2018.11.010. [DOI] [PubMed] [Google Scholar]
- 59.Stoll H., Ost M., Singh A., Mehling R., Neri D., Schafer I., Velic A., Macek B., Kretschmer D., Weidenmaier C., et al. Staphylococcal enterotoxins dose-dependently modulate the generation of myeloid-derived suppressor cells. Front. Cell. Infection Microbiol. 2018;8:321. doi: 10.3389/fcimb.2018.00321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wichmann K., Uter W., Weiss J., Breuer K., Heratizadeh A., Mai U., Werfel T. Isolation of alpha-toxin-producing staphylococcus aureus from the skin of highly sensitized adult patients with severe atopic dermatitis. Br. J. Dermatol. 2009;161:300–305. doi: 10.1111/j.1365-2133.2009.09229.x. [DOI] [PubMed] [Google Scholar]
- 61.Kong H.H., Oh J., Deming C., Conlan S., Grice E.A., Beatson M.A., Nomicos E., Polley E.C., Komarow H.D., Program N.C.S., et al. Temporal shifts in the skin microbiome associated with disease flares and treatment in children with atopic dermatitis. Genome Res. 2012;22:850–859. doi: 10.1101/gr.131029.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Roesner L.M., Werfel T., Heratizadeh A. The adaptive immune system in atopic dermatitis and implications on therapy. Expert. Rev. Clin. Immunol. 2016;12:787–796. doi: 10.1586/1744666X.2016.1165093. [DOI] [PubMed] [Google Scholar]
- 63.Breuer K., Wittmann M., Kempe K., Kapp A., Mai U., Dittrich-Breiholz O., Kracht M., Mrabet-Dahbi S., Werfel T. Alpha-toxin is produced by skin colonizing staphylococcus aureus and induces a t helper type 1 response in atopic dermatitis. Clin. Exp. Allergy. 2005;35:1088–1095. doi: 10.1111/j.1365-2222.2005.02295.x. [DOI] [PubMed] [Google Scholar]
- 64.Eyerich K., Novak N. Immunology of atopic eczema: Overcoming the th1/th2 paradigm. Allergy. 2013;68:974–982. doi: 10.1111/all.12184. [DOI] [PubMed] [Google Scholar]
- 65.Biedermann T., Skabytska Y., Kaesler S., Volz T. Regulation of t cell immunity in atopic dermatitis by microbes: The yin and yang of cutaneous inflammation. Front. Immunol. 2015;6:353. doi: 10.3389/fimmu.2015.00353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Auriemma M., Vianale G., Amerio P., Reale M. Cytokines and t cells in atopic dermatitis. Eur. Cytokine Netw. 2013;24:37–44. doi: 10.1684/ecn.2013.0333. [DOI] [PubMed] [Google Scholar]
- 67.Koga C., Kabashima K., Shiraishi N., Kobayashi M., Tokura Y. Possible pathogenic role of th17 cells for atopic dermatitis. J. Investig. Dermatol. 2008;128:2625–2630. doi: 10.1038/jid.2008.111. [DOI] [PubMed] [Google Scholar]
- 68.D’Auria E., Banderali G., Barberi S., Gualandri L., Pietra B., Riva E., Cerri A. Atopic dermatitis: Recent insight on pathogenesis and novel therapeutic target. Asian-Pac. J. Allergy Immunol. 2016;34:98–108. doi: 10.12932/AP0732.34.2.2016. [DOI] [PubMed] [Google Scholar]
- 69.Liang S.C., Tan X.Y., Luxenberg D.P., Karim R., Dunussi-Joannopoulos K., Collins M., Fouser L.A. Interleukin (il)-22 and il-17 are coexpressed by th17 cells and cooperatively enhance expression of antimicrobial peptides. J. Exp. Med. 2006;203:2271–2279. doi: 10.1084/jem.20061308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Duhen T., Geiger R., Jarrossay D., Lanzavecchia A., Sallusto F. Production of interleukin 22 but not interleukin 17 by a subset of human skin-homing memory t cells. Nat. Immunol. 2009;10:857–863. doi: 10.1038/ni.1767. [DOI] [PubMed] [Google Scholar]
- 71.Orfali R.L., da Silva Oliveira L.M., de Lima J.F., de Carvalho G.C., Ramos Y.A.L., Pereira N.Z., Pereira N.V., Zaniboni M.C., Sotto M.N., da Silva Duarte A.J., et al. Staphylococcus aureus enterotoxins modulate il-22-secreting cells in adults with atopic dermatitis. Sci. Rep. 2018;8:6665. doi: 10.1038/s41598-018-25125-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Laborel-Preneron E., Bianchi P., Boralevi F., Lehours P., Fraysse F., Morice-Picard F., Sugai M., Sato’o Y., Badiou C., Lina G., et al. Effects of the staphylococcus aureus and staphylococcus epidermidis secretomes isolated from the skin microbiota of atopic children on cd4+ t cell activation. PLoS ONE. 2015;10:e0141067. doi: 10.1371/journal.pone.0141067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Simpson E.L., Villarreal M., Jepson B., Rafaels N., David G., Hanifin J., Taylor P., Boguniewicz M., Yoshida T., De Benedetto A., et al. Patients with atopic dermatitis colonized with staphylococcus aureus have a distinct phenotype and endotype. J. Investig. Dermatol. 2018;138:2224–2233. doi: 10.1016/j.jid.2018.03.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Titz T.D., Orfali R.L., de Lollo C., dos Santos V.G., Duarte A.J.D., Sato M.N., Aoki V. Impaired cd23 and cd62l expression and tissue inhibitors of metalloproteinases secretion by eosinophils in adults with atopic dermatitis. J. Eur. Acad. Dermatol. Venereol. 2016;30:2072–2076. doi: 10.1111/jdv.13825. [DOI] [PubMed] [Google Scholar]
- 75.Lin Y.T., Yang Y.H., Hwang Y.W., Tsai M.J., Tsao P.N., Chiang B.L., Shau W.Y., Wang L.F. Comparison of serum specific ige antibodies to staphylococcal enterotoxins between atopic children with and without atopic dermatitis. Allergy. 2000;55:641–646. doi: 10.1034/j.1398-9995.2000.00523.x. [DOI] [PubMed] [Google Scholar]
- 76.Tanaka A., Suzuki S., Ohta S., Manabe R., Furukawa H., Kuwahara N., Fukuda Y., Kimura T., Jinno M., Hirai K., et al. Association between specific ige to staphylococcus aureus enterotoxins a and b and asthma control. Ann. Allerg Asthma Immunol. 2015;115:191. doi: 10.1016/j.anai.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 77.Parcina M., Miranda-Garcia M.A., Durlanik S., Ziegler S., Over B., Georg P., Foermer S., Ammann S., Hilmi D., Weber K.J., et al. Pathogen-triggered activation of plasmacytoid dendritic cells induces il-10-producing b cells in response to staphylococcus aureus. J. Immunol. 2013;190:1591–1602. doi: 10.4049/jimmunol.1201222. [DOI] [PubMed] [Google Scholar]
- 78.Boccardi D., D’Auria E., Turati F., DI M.V., Sortino S., Riva E., Cerri A. Disease severity and quality of life in children with atopic dermatitis: Po-scorad in clinical practice. Minerva Pediatrica. 2017;69:373–380. doi: 10.23736/S0026-4946.16.04294-8. [DOI] [PubMed] [Google Scholar]
- 79.Coutanceau C., Stalder J.F. Analysis of correlations between patient-oriented scorad (po-scorad) and other assessment scores of atopic dermatitis severity and quality of life. Dermatology. 2014;229:248–255. doi: 10.1159/000365075. [DOI] [PubMed] [Google Scholar]
- 80.Raap U., Wichmann K., Bruder M., Stander S., Wedi B., Kapp A., Werfel T. Correlation of il-31 serum levels with severity of atopic dermatitis. J. Allergy Clin. Immunol. 2008;122:421–423. doi: 10.1016/j.jaci.2008.05.047. [DOI] [PubMed] [Google Scholar]
- 81.Sonkoly E., Muller A., Lauerma A.I., Pivarcsi A., Soto H., Kemeny L., Alenius H., Dieu-Nosjean M.C., Meller S., Rieker J., et al. Il-31: A new link between t cells and pruritus in atopic skin inflammation. J. Allergy Clin. Immunol. 2006;117:411–417. doi: 10.1016/j.jaci.2005.10.033. [DOI] [PubMed] [Google Scholar]
- 82.Niebuhr M., Werfel T. Innate immunity, allergy and atopic dermatitis. Curr. Opin. Allergy Clin. Immunol. 2010;10:463–468. doi: 10.1097/ACI.0b013e32833e3163. [DOI] [PubMed] [Google Scholar]
- 83.Grice E.A., Kong H.H., Conlan S., Deming C.B., Davis J., Young A.C., Program N.C.S., Bouffard G.G., Blakesley R.W., Murray P.R., et al. Topographical and temporal diversity of the human skin microbiome. Science. 2009;324:1190–1192. doi: 10.1126/science.1171700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Huttenhower C., Gevers D., Knight R., Abubucker S., Badger J.H., Chinwalla A.T., Creasy H.H., Earl A.M., FitzGerald M.G., Fulton R.S., et al. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486:207–214. doi: 10.1038/nature11234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kuo I.H., Yoshida T., De Benedetto A., Beck L.A. The cutaneous innate immune response in patients with atopic dermatitis. J. Allergy Clin. Immunol. 2013;131:266–278. doi: 10.1016/j.jaci.2012.12.1563. [DOI] [PubMed] [Google Scholar]
- 86.Werfel T., Allam J.P., Biedermann T., Eyerich K., Gilles S., Guttman-Yassky E., Hoetzenecker W., Knol E., Simon H.U., Wollenberg A., et al. Cellular and molecular immunologic mechanisms in patients with atopic dermatitis. J. Allergy Clin. Immunol. 2016;138:336–349. doi: 10.1016/j.jaci.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 87.Nakatsuji T., Chen T.H., Two A.M., Chun K.A., Narala S., Geha R.S., Hata T.R., Gallo R.L. Staphylococcus aureus exploits epidermal barrier defects in atopic dermatitis to trigger cytokine expression. J. Investig. Dermatol. 2016;136:2192–2200. doi: 10.1016/j.jid.2016.05.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Schommer N.N., Gallo R.L. Structure and function of the human skin microbiome. Trends Microbiol. 2013;21:660–668. doi: 10.1016/j.tim.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kennedy E.A., Connolly J., Hourihane J.O., Fallon P.G., McLean W.H., Murray D., Jo J.H., Segre J.A., Kong H.H., Irvine A.D. Skin microbiome before development of atopic dermatitis: Early colonization with commensal staphylococci at 2 months is associated with a lower risk of atopic dermatitis at 1 year. J. Allergy Clin. Immunol. 2017;139:166–172. doi: 10.1016/j.jaci.2016.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shi B., Bangayan N.J., Curd E., Taylor P.A., Gallo R.L., Leung D.Y.M., Li H. The skin microbiome is different in pediatric versus adult atopic dermatitis. J. Allergy Clin. Immunol. 2016;138:1233–1236. doi: 10.1016/j.jaci.2016.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Parlet C.P., Brown M.M., Horswill A.R. Commensal staphylococci influence staphylococcus aureus skin colonization and disease. Trends Microbiol. 2019 doi: 10.1016/j.tim.2019.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Clowry J., Irvine A.D., McLoughlin R.M. Next-generation anti-staphylococcus aureus vaccines: A potential new therapeutic option for atopic dermatitis? J. Allergy Clin. Immunol. 2019;143:78–81. doi: 10.1016/j.jaci.2018.08.038. [DOI] [PubMed] [Google Scholar]
- 93.Ruzicka T., Hanifin J.M., Furue M., Pulka G., Mlynarczyk I., Wollenberg A., Galus R., Etoh T., Mihara R., Yoshida H., et al. Anti-interleukin-31 receptor a antibody for atopic dermatitis. New Engl. J. Med. 2017;376:826–835. doi: 10.1056/NEJMoa1606490. [DOI] [PubMed] [Google Scholar]
- 94.Myles I.A., Earland N.J., Anderson E.D., Moore I.N., Kieh M.D., Williams K.W., Saleem A., Fontecilla N.M., Welch P.A., Darnell D.A., et al. First-in-human topical microbiome transplantation with roseomonas mucosa for atopic dermatitis. JCI Insight. 2018;3:3. doi: 10.1172/jci.insight.120608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Blicharz L., Rudnicka L., Samochocki Z. Staphylococcus aureus: An underestimated factor in the pathogenesis of atopic dermatitis? Adv. Dermatol. Allergol. 2019;36:11–17. doi: 10.5114/ada.2019.82821. [DOI] [PMC free article] [PubMed] [Google Scholar]