Abstract
Hyperkalemia is frequently complicated in patients with advanced chronic kidney disease (CKD) because kidney is the major route of potassium excretion. Urinary potassium excretion is reduced according to the decline in glomerular filtration rate, and the risk of hyperkalemia is increased in patients with high potassium intake, advanced age, diabetes mellitus, congestive heart failure, and medications such as renin-angiotensin-aldosterone system(RAAS) blockades. On the other hand, the benefits of RAAS blockades and a high-potassium diet should be considered in CKD patients. To overcome these contradictory treatment strategies, potassium binders have emerged as new options to enhance fecal potassium excretion. In different regions of the world, four types of potassium binders are preferentially used. Whereas sodium polystyrene sulfonate (SPS) exchanges sodium for potassium, calcium polystyrene sulfonate (CPS) has the advantage of avoiding hypervolemia because it exchanges calcium for potassium. SPS was first introduced in the 1950s and used for a long time in western countries, and CPS is currently prescribed in Asia including South Korea. In contrast with the paucity of clinical studies using SPS or CPS, the recent randomized, controlled trials reported that two newer potassium binders, patiromer and sodium zirconium cyclosilicate (ZS-9), effectively and safely reduce serum potassium levels in CKD patients taking RAAS blockades. Our experiences showed that the long-term administration of a small dose of CPS was also effective and safe in treatment of chronic hyperkalemia. Further comparative trials among patiromer, ZS-9, and CPS are required to provide guides to cost-effective management of hyperkalemia in CKD patients.
Keywords: Calcium polystyrene sulfonate, Patiromer, Potassium, Sodium polystyrene sulfonate, Sodium zirconium cyclosilicate
The risk of hyperkalemia in chronic kidney disease
Potassium homeostasis is maintained by internal and external balance. Most of the body potassium is intracellularly located, and the internal balance is affected by transcellular shift of potassium. The external balance is the net result of potassium intake and excretion, and urine and stool are the main routes of potassium excretion1). The kidney is normally the major determinant of external potassium balance, but contribution of colonic potassium secretion to the total potassium excretion would increase as urinary potassium is reduced in chronic kidney disease (CKD).
As CKD advances from stage 1 to 5, urinary potassium excretion is declined2). In response to oral potassium load, the increase in urinary potassium excretion is blunted in CKD patients compared with normal subjects3). However, the basal and stimulated fractional excretion of potassium is enhanced in CKD patients because of magnification phenomenon4).
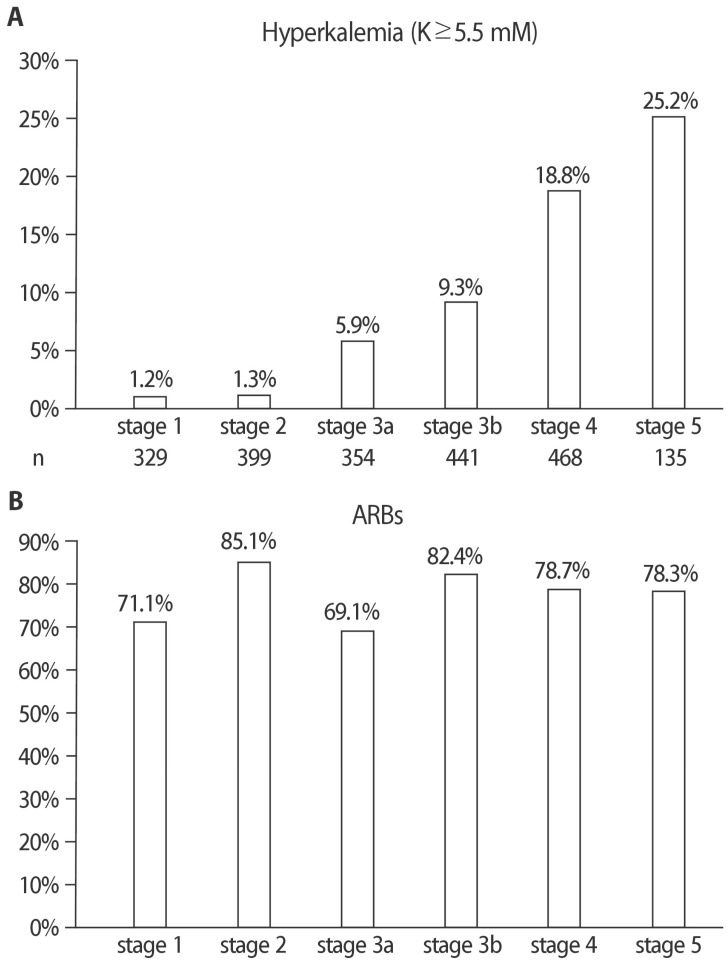
The prevalence of hyperkalemia increases as the CKD advances from stage 1 to 5. Figure 1 shows data from the KoreaN cohort Study for Outcomes in patients With Chronic Kidney Disease (KNOW-CKD). When the CKD reaches stages 4 to 5, about one-fifths of the Korean patients appear to have hyperkalemia >5.5mmol/L. Because of the proven renoprotective efficacy, renin-angiotensin-aldosterone system(RAAS) blockades are frequently used in proteinuric patients. Notably, most of the Korean CKD patients are prescribed RAAS blockades including conver ting enzyme inhibitors, angiotensin II receptor blockers, and spironolactone. The resultant inhibition of angiotensin II or aldosterone would impair potassium secretion from the cortical collecting duct and enhance the risk of hyperkalemia in CKD patients5). The associated risk of hyperkalemia with using RAAS blockades can be inferred from the major randomized, controlled clinical trials evaluating the effect of RAAS blockade on renal outcomes. The risk of hyperkalemia seems to increase by at least 2 to 3 times in proteinuric CKD patients taking RAAS blockers6). Hyperkalemia is independently associated with significantly higher all-cause and cardiovascular mortality, and with higher risk of end-stage renal disease7).
Fig. 1. Prevalence of hyperkalemia and use of angiotensin II receptor blockades (ARBs) in Korean patients with chronic kidney disease (CKD). (A) Percentages of patients with hyperkalemia (>5.5 mmol/L) from CKD stage 1 through 5. (B) Percentages of patients taking ARBs from CKD stage 1 through 5. Data were produced from the KNOW-CKD cohort and offered by Drs. Eunjeong Kang and Kook-Hwan Oh.
Recently, the benefits of a highpotassium diet were reported from CKD patients. In particular, a vegetarian diet and its components may slow renal progression and prevent cardiovascular complications8). Thus, we need to control potassium load while maintaining the benefit of high potassium intake. Offering vegetables and fruits may counteract the hyperkalemia-associated adverse effects because of relieving metabolic acidosis as well as constipation. The associated intake of low salt and low protein would be good to kidney health.
Interventions to treat chronic hyperkalemia in CKD
Hyperkalemia can be grouped into acute and chronic. Acute hyperkalemia is caused by abnormal net release of potassium from cells, often due to trauma, metabolic acidosis, and hemolysis, requiring immediate attention, i.e., cardiac monitoring and acute medical interventions such as dialysis. On the other hand, chronic hyperkalemia is caused by impairment of potassium excretory process and/or increased potassium load, requiring ongoing management to correct the underlying disturbances in potassium balance, i.e., nonpharmacological and pharmacological interventions9).
First, nonpharmacological interventions should be applied to CKD patients at risk of hyperkalemia10). It is important to assess estimated glomerular filtration rate (eGFR) to define overall risk of hyperkalemia because the risk of hyperkalemia increases as eGFR declines. Medications that can impair renal potassium excretion need to be investigated in patients with hyperkalemia. Not only RAAS blockers but also nonsteroidal anti-inflammatory drugs, nonselective beta-blockers, calcineurin inhibitors, and heparin can induce hyperkalemia, and they may be discontinued if serum potassium rises to >5.5mmol/L. When RAAS blockers are used, they should be started from low doses and closely monitored. To reduce potassium in diet, cooking procedures (e.g., soaking or boiling) should be modified in order to remove potassium, and hidden sources of potassium(e.g. food additives and low-sodium salt substitutes) should be avoided11).
When these measures are not successful, pharmacologic treatments are necessary. First, alkali agents such as sodium bicarbonate are useful to reduce hypokalemia if they are indicated for correction of metabolic acidosis in CKD patients. Another option is diuretics to induce kaliuresis. If the advanced CKD patients are edematous, loop diuretics are indicated to restore their volume status. However, caution needs to be paid to the risk of prerenal azotemia precipitated by overuse of diuretics. Fludrocortisone acetate may be prescribed to excrete urinary potassium in patients with aldosterone deficiency. However, larger doses (up to 0.4–1.0mg/day) are needed to effectively lower potassium level, and sodium retention, edema, and hypertension may be complicated12).
Before initiating dialytic therapy to treat hyperkalemia in CKD, cation exchange resins can be used to enhance fecal potassium excretion. They are nowadays called potassium binders and emerging as new options to treat chronic hyperkalemia.
Potassium binders to treat chronic hyperkalemia in CKD
1. Sodium polystyrene sulfonate
Sodium polystyrene sulfonate (SPS) is a cation exchange resin, which exchanges sodium for calcium, ammonium, and magnesium in addition to potassium. Thus, it is not very selective for serum potassium lowering and may lead to hypocalcemia and hypomagnesemia. Kayexalate was the commercial name given to the powdered form of SPS, first introduced in the 1950s13).
The main action site of SPS is “distal colon”, where the potassium concentration is high because of colonic secretion. Because the apical BK channel (KCa1.1) is the major secretory K+ channel in the distal colon, SPS needs to be delivered to the rectum, either by retention enema or by oral administration with cathartics. Cation exchange resins seem to act on crypt enterocytes in the distal colon, which have the secretory pathway of potassium from basolateral NKCC1 cotransporter (and Na-K-ATPase) to apical BK channel14). Notably, SPS is ineffective in binding potassium when it stays in the stomach because its sulfonate groups are occupied by hydrogen ions at an acid pH13).
Previously, the efficacy and safety of SPS were concerned. A single dose (30 g) SPS therapy was ineffective in lowering serum potassium concentration in patients with end-stage renal failure15). Gastrointestinal adverse events associated with SPS use were substantial according a systematic review16). In particular, colonic necrosis was serious because of mortality. However, recent randomized clinical trials showed that SPS was effective in treating mild hyperkalemia in CKD patients17,18). The evidence base for SPS is more limited than Patiromer and ZS-9 because clinical trials were performed on small numbers of patients over short periods. However, use of SPS may continue due to clinical familiarity and lower cost18).
Recently, Abuelo pointed out fallacies in treatment of hyperkalemia19). Among these, the efficacy and safety of SPS were the issues; “1) SPS is of uncertain efficacy, and if effective, it is only after a delay of several hours, making its usefulness questionable for severe hyperkalemia. 2) Intestinal necrosis, usually of the colon, is an infrequent, but often fatal complication of sodium polystyrene sulfonate.” According to him, the truths are the followings; 1) Recent clinical studies and case series of SPS use confirmed its effectiveness in almost 800 patients; single 60- to 80-g doses were followed by average falls in serum potassium of 0.9 to 1.7mmol/L. Regarding onset of action, a significant fall of 0.6 mmol/L was noted in potassium concentrations measured from 0 to 4 hours after SPS administration. 2) It is not clear if SPS causes intestinal necrosis; instead, it may just be a marker for risk factors for intestinal necrosis, such as chronic and end stage renal disease. Even if SPS with or without sorbitol can rarely produce intestinal necrosis, it is so uncommon (much <1%).”
2. Calcium polystyrene sulfonate
Calcium polystyrene sulfonate (CPS) is a cation exchange resin, which exchanges calcium for potassium. Compared with SPS, CPS may have a higher potassium-selectivity at cation exchange20). Although CPS has been widely used for patients with advanced CKD in many countries including South Korea, few studies were reported on its efficacy and adverse effects.
We retrospectively analyzed our data of using CPS to treat mild hyperkalemia in outpatient CKD patients21). Eight hundred eighty-four patients were initially screened, but 247 patients were finally analyzed because those with prior CPS use, administration for less than a week, admission history, dialysis therapy, and kidney transplantation were excluded. We evaluated only the periods with a fixed dosage.
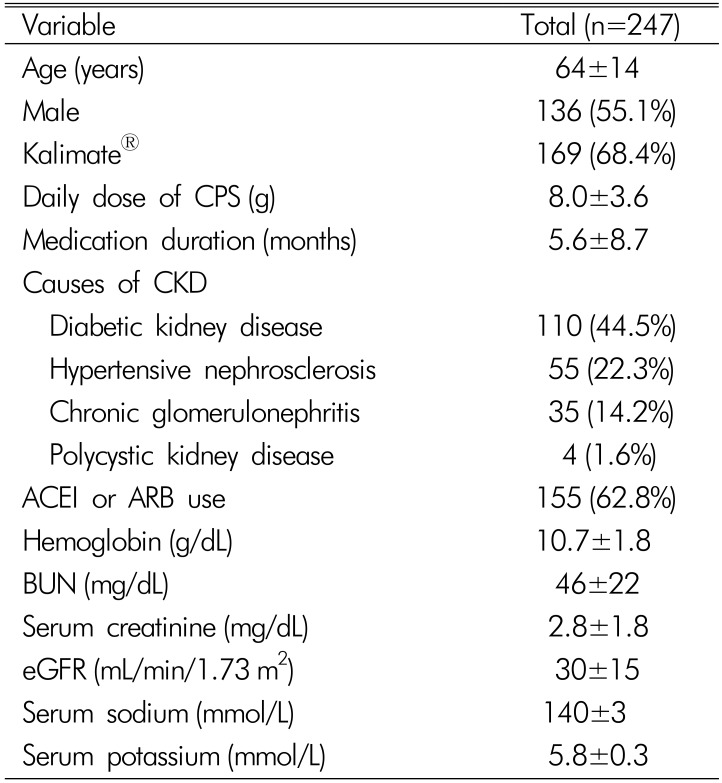
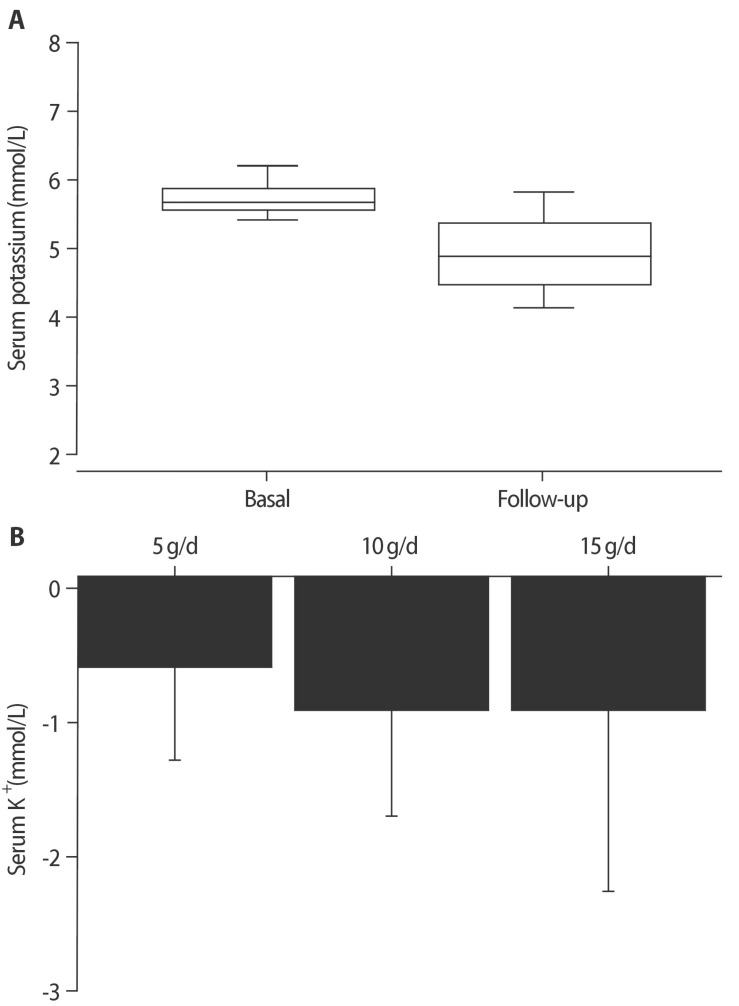
Table 1 shows baseline characteristics of the patients enrolled in this study21). All patients used small doses of CPS, ranging 2.5 to 15 grams per day. The mean duration of medication was 5.6 months, and ACE inhibitors or ARBs were commonly used. When all patients were taken together, the serum potassium level was significantly decreased by CPS treatment (Fig. 2). Hyperkalemia was corrected (<5.0mmol/L) in 57.5% of our patients, and the serum potassium lowering effect of CPS was dose-dependent. Notably, the response (serum potassium lowering ≥0.3mmol/L) was >70% irrespective of using and discontinuing ACE inhibitors and ARBs. Many patients complained of unpleasant taste with CPS, and constipation was noted in 8% from our medical records. However, no serious adverse events including colonic necrosis were reported. Although the incidence may be negligible, colonic mucosal necrosis has been reported in a Korean uremic patient following administration of CPS22).
Table 1. Patient characteristics at baseline: A retrospective analysis of using calcium polystyrene sulfonate21).
Values are expressed as mean±standard deviation for continuous variables and number (%) for categorical variables. CPS, calcium polystyrene sulfonate; CKD, chronic kidney disease; ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin II receptor blockade; BUN, blood urea nitrogen; eGFR, estimated glomerular filtration rate.
Fig. 2. Effects of calcium polystyrene sulfonate on serum potassium. (A) Serum potassium concentrations were compared before and after administration of calcium polystyrene sulfonate (*, p<0.001 by paired t-test). (B) Serum potassium concentrations were lowered by calcium polystyrene sulfonate in a dose-dependent fashion (p<0.001 by oneway ANOVA test). https://doi.org/10.1371/journal.pone.0173542.g003.
Recently, a comparative study between CPS and SPS was reported from Japanese pre-dialysis patients with hyperkalemia20). After 4-week treatments, serum potassium lowering was similar (CPS, 0.60 to 1.90mmol/L; SPS, 1.08 to 1.88 mmol/L, p=0.51). Whereas CPS had a tendency to serum sodium lowering, SPS significantly increased serum sodium concentration. CPS had no significant effects on serum calcium and magnesium, but SPS significantly decreased serum calcium and magnesium concentration. Thus, CPS may be superior to SPS in terms of side effects.
3. Patiromer
Patiromer is a non-absorbable polymer consisting of smooth spherical beads approximately 100 µm in diameter. The active moiety of the polymer is composed of alpha-fluorocarboxylic acid that contains a calcium ion which dissociates in favor of a potassium ion to promote fecal potassium excretion in the distal colon13). Oral administration of patiromer can increase fecal potassium in a dose-related fashion, and doses of 15 to 30 g/day increased daily fecal potassium by approximately 15 to 20 mmol23).
Randomized, controlled trials have evaluated the efficacy and safety of patiromer in hyperkalemic CKD patients already treated with RAAS blockers. Serum potassium lowering was demonstrated by daily doses between 8.4 to 30 g up to 52 weeks. Major adverse events were constipation and hypomagnesemia6). Based on these results, patiromer was approved by the Food and Drug Administration in 2015.
4. Sodium zirconium cyclosilicate
Sodium zirconium cyclosilicate (ZS-9) is a crystal that is highly selective for potassium ion trapping24). Thus, it may act throughout the gastrointestinal tract and explain the rapid onset of action. ZS-9 was also tested for treating hyperkalemia in CKD, heart failure or diabetic outpatients. Daily doses between 1.25 to 15 g up to four weeks were used in randomized, controlled trials and showed effective serum potassium lowering. Major adverse events were edema and diarrhea6). Based on these results, ZS-9 was approved by the Food and Drug Administration in 2018. Very recently, a long-term experience of using ZS-9 over 12 months was reported25).
Conclusion
Chronic hyperkalemia is a major concern in CKD patients, especially taking RAAS blockades for diabetes and/or cardiac disease. Potassium binding agents may be useful to maintain the serum potassium in the normal range without reducing the dose or discontinuing RAAS inhibitors and restricting intake of fruits and vegetables. The old potassium binders, SPS and CPS, have been used for decades over the world. Although their efficacy and safety are still controversial, small doses of CPS should be efficacious and safe to treat mild hyperkalemia. New agents such as patiromer and sodium zirconium cyclosilicate are promising because of the recent clinical studies, and comparative clinical trials between patiromer, sodium zirconium cyclosilicate, and CPS are required to provide guides to cost-effective management of chronic hyperkalemia.
Acknowledgments
The author is deeply thankful for data sharing from Drs. Eunjeong Kang and Kook-Hwan Oh at Seoul National University Hospital.
Footnotes
Conflict of interest: The author declares no relevant financial interests.
References
- 1.Zacchia M, Abategiovanni ML, Stratigis S, Capasso G. Potassium: from physiology to clinical implications. Kidney Dis (Basel) 2016;2:72–79. doi: 10.1159/000446268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ueda Y, Ookawara S, Ito K, Miyazawa H, Kaku Y, Hoshino T, Tabei K, Morishita Y. Changes in urinary potassium excretion in patients with chronic kidney disease. Kidney Res Clin Pract. 2016;35:78–83. doi: 10.1016/j.krcp.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Preston RA, Afshartous D, Garg D, Medrano S, Alonso AB, Rodriguez R. Mechanisms of impaired potassium handling with dual renin-angiotensin-aldosterone blockade in chronic kidney disease. Hypertension. 2009;53:754–760. doi: 10.1161/HYPERTENSIONAHA.108.125252. [DOI] [PubMed] [Google Scholar]
- 4.Bricker NS, Fine LG, Kaplan M, Epstein M, Bourgoignie JJ, Light A. Magnification phenomenon in chronic renal disease. N Engl J Med. 1978;299:1287–1293. doi: 10.1056/NEJM197812072992307. [DOI] [PubMed] [Google Scholar]
- 5.Palmer BF. Managing hyperkalemia caused by inhibitors of the renin-angiotensin-aldosterone system. N Engl J Med. 2004;351:585–592. doi: 10.1056/NEJMra035279. [DOI] [PubMed] [Google Scholar]
- 6.Georgianos PI, Agarwal R. Revisiting RAAS blockade in CKD with newer potassium-binding drugs. Kidney Int. 2018;93:325–334. doi: 10.1016/j.kint.2017.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kovesdy CP, Matsushita K, Sang Y, Brunskill NJ, Carrero JJ, Chodick G, Hasegawa T, Heerspink HL, Hirayama A, Landman GWD, Levin A, Nitsch D, Wheeler DC, Coresh J, Hallan SI, Shalev V, Grams ME CKD Prognosis Consortium. Serum potassium and adverse outcomes across the range of kidney function: a CKD prognosis consortium meta-analysis. Eur Heart J. 2018;39:1535–1542. doi: 10.1093/eurheartj/ehy100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chauveau P, Koppe L, Combe C, Lasseur C, Trolonge S, Aparicio M. Vegetarian diets and chronic kidney disease. Nephrol Dial Transplant. 2019;34:199–207. doi: 10.1093/ndt/gfy164. [DOI] [PubMed] [Google Scholar]
- 9.Alvo M, Warnock DG. Hyperkalemia. West J Med. 1984;141:666–671. [PMC free article] [PubMed] [Google Scholar]
- 10.Palmer BF, Clegg DJ. Diagnosis and treatment of hyperkalemia. Cleve Clin J Med. 2017;84:934–942. doi: 10.3949/ccjm.84a.17056. [DOI] [PubMed] [Google Scholar]
- 11.De Nicola L, Di Lullo L, Paoletti E, Cupisti A, Bianchi S. Chronic hyperkalemia in non-dialysis CKD: controversial issues in nephrology practice. J Nephrol. 2018;31:653–664. doi: 10.1007/s40620-018-0502-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kovesdy CP. Management of hyperkalaemia in chronic kidney disease. Nat Rev Nephrol. 2014;10:653–662. doi: 10.1038/nrneph.2014.168. [DOI] [PubMed] [Google Scholar]
- 13.Sterns RH, Grieff M, Bernstein PL. Treatment of hyperkalemia: something old, something new. Kidney Int. 2016;89:546–554. doi: 10.1016/j.kint.2015.11.018. [DOI] [PubMed] [Google Scholar]
- 14.Sorensen MV, Matos JE, Praetorius HA, Leipziger J. Colonic potassium handling. Pflugers Arch. 2010;459:645–656. doi: 10.1007/s00424-009-0781-9. [DOI] [PubMed] [Google Scholar]
- 15.Gruy-Kapral C, Emmett M, Santa Ana CA, Porter JL, Fordtran JS, Fine KD. Effect of single dose resin-cathartic therapy on serum potassium concentration in patients with end-stage renal disease. J Am Soc Nephrol. 1998;9:1924–1930. doi: 10.1681/ASN.V9101924. [DOI] [PubMed] [Google Scholar]
- 16.Harel Z, Harel S, Shah PS, Wald R, Perl J, Bell CM. Gastrointestinal adverse events with sodium polystyrene sulfonate (Kayexalate) use: a systematic review. Am J Med. 2013;126:264.e9–264.e24. doi: 10.1016/j.amjmed.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 17.Lepage L, Dufour AC, Doiron J, Handfield K, Desforges K, Bell R, Vallée M, Savoie M, Perreault S, Laurin LP, Pichette V, Lafrance JP. Randomized clinical ttrial of sodium polystyrene sulfonate for the treatment of mild hyperkalemiain CKD. Clin J Am Soc Nephrol. 2015;10:2136–2142. doi: 10.2215/CJN.03640415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beccari MV, Meaney CJ. Clinical utility of patiromer, sodium zirconium cyclosilicate, and sodium polystyrene sulfonate for the treatment of hyperkalemia: an evidence-based review. Core Evid. 2017;12:11–24. doi: 10.2147/CE.S129555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abuelo JG. Treatment of Severe Hyperkalemia: Confronting 4 fallacies. Kidney Int Rep. 2017;3:47–55. doi: 10.1016/j.ekir.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakayama Y, Ueda K, Yamagishi SI, Sugiyama M, Yoshida C, Kurokawa Y, Nakamura N, Moriyama T, Kodama G, Minezaki T, Ito S, Nagata A, Taguchi K, Yano J, Kaida Y, Shibatomi K, Fukami K. Compared effects of calcium and sodium polystyrene sulfonate on mineral and bone metabolism and volume overload in pre-dialysis patients with hyperkalemia. Clin Exp Nephrol. 2018;22:35–44. doi: 10.1007/s10157-017-1412-y. [DOI] [PubMed] [Google Scholar]
- 21.Yu MY, Yeo JH, Park JS, Lee CH, Kim GH. Long-term efficacy of oral calcium polystyrene sulfonate for hyperkalemiain CKD patients. PLoS One. 2017;12(3):e0173542. doi: 10.1371/journal.pone.0173542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joo M, Bae WK, Kim NH, Han SR. Colonic mucosal necrosis following administration of calcium polystryrene sulfonate (Kalimate) in a uremic patient. J Korean Med Sci. 2009;24:1207–1211. doi: 10.3346/jkms.2009.24.6.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang I. RLY5016: A novel, non-absorbed, therapeutic polymer for serum potassium control. J Am Soc Nephrol. 2010;21:482A–483A. [Google Scholar]
- 24.Stavros F, Yang A, Leon A, Nuttall M, Rasmussen HS. Characterization of structure and function of ZS-9, a K+ selective ion trap. PLoS One. 2014;9:e114686. doi: 10.1371/journal.pone.0114686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spinowitz BS, Fishbane S, Pergola PE, Roger SD, Lerma EV, Butler J, von Haehling S, Adler SH, Zhao J, Singh B, Lavin PT, McCullough PA, Kosiborod M, Packham DK ZS-005 Study Investigators. Sodium zirconium cyclosilicateamong individuals with hyperkalemia: A 12-month phase 3 study. Clin J Am Soc Nephrol. 2019 May 20;:pii: CJN.12651018. doi: 10.2215/CJN.12651018. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]