Abstract
Objectives:
We evaluate the extent to which subjective and objective measures of economic distress account for differences in substance abuse between the mid-1990s and early-2010s.
Methods:
We use cross-sectional survey data for national samples of Americans aged 25–74 in 1995–96 (n=3034) and 2011–14 (n=2598) from the Midlife Development in the US study. Using a logit model, we regress dichotomous indicators of drug and alcohol abuse on economic distress.
Results:
After adjusting for sociodemographic characteristics, the odds of drug abuse in the early-2010s among older individuals (aged 50+) were 2.9 times (95% CI 1.9–4.2) those of the mid-1990s, but there was no significant period difference in drug abuse among younger individuals. Measures of model performance demonstrate that subjective measures of economic distress are better predictors of drug abuse than objective measures. The subjective measures also account for a larger share (26%) of the increase in drug abuse at ages 50 and older than the objective measures (6%). We cannot draw clear conclusions with respect to alcohol abuse because results are sensitive to specification.
Conclusions:
The rise in drug abuse among midlife Americans may relate to perceived economic distress that is not captured by standard economic measures.
Keywords: Drug abuse, alcohol abuse, economic distress
INTRODUCTION
Expectation of life in the U.S. rose nearly every year between 1943 and 2014,1 but between 2014 and 2017 the country experienced the longest sustained decline since 1915–18.2–5 Much of the decline has been attributed to the drug epidemic.5–8 Increased availability of opioids resulting from changes in marketing, prescribing, and insurance coverage of prescription opioids, which led to wider black market dissemination of heroin, fentanyl, and other opioids almost certainly contributed to growing drug abuse.9–12 Indeed, drug-related mortality has increased dramatically in the U.S.: the age-adjusted rate in 2017 (21.7 per 100,000) was 3.6 times that in 1999 (6.1 per 100,000).13
But the US mortality crisis may extend beyond the drug epidemic. Some researchers have noted that alcohol-related mortality and suicides also increased since the late 1990s.14,15 Recognition of these shared trends inspired the term “deaths of despair”16–18 to refer to the cluster of suicides, alcohol-, and drug-related mortality. Other evidence suggests that midlife Americans in particular are afflicted with rising mortality across a variety of causes. Among those aged 25–64, mortality rates increased between 1999 and 2016 not only for external causes, but also digestive diseases, endocrine/nutritional/metabolic disorders, and diseases of the nervous system.19
These disturbing trends have led scholars to speculate that the US mortality crisis stems from a deeper malaise: a rising tide of despair,20–22 particularly among less-educated, middle-aged Americans.14,15 Case and Deaton14 hypothesized that changes in labor market opportunities have triggered growing distress. Job prospects for less-educated Americans have steadily deteriorated since the early 1970s.14,15,22 Socioeconomically disadvantaged Americans have also borne the brunt of mortality crisis.23–27 Expectation of life at age 25 among non-Hispanic white women with less than 12 years of education declined by 3.1 years between 1990 and 2010, whereas their counterparts with 16 or more years of education gained 3.7 years; corresponding figures for non-Hispanic white men were −0.6 and +5.2 years, respectively; among non-Hispanic blacks, life expectancy improved at all education levels, but those with more education enjoyed bigger gains.23 Among women in the bottom 5% of the income distribution, life expectancy at age 40 increased by only 0.04 years between 2001 and 2014, while those in the top 5% gained 2.9 years; corresponding figures for men were 0.3 and 2.3, respectively.27 The despair hypothesis proposes that social disparities in longevity widened because less-educated individuals have been more vulnerable to the consequences of globalization for the labor market.14,22
A recent study demonstrated widening social disparities in perceived economic distress since the mid-1990s: financial strain and employment uncertainty increased more for those with low socioeconomic status than for more advantaged Americans.28 These trends are consistent with the despair hypothesis. The results also suggest that disparities in subjective economic distress widened even more than expected based on changes in objective measures of economic and employment circumstances.28 The authors suggest that efforts to understand widening socioeconomic disparities in health and survival should look beyond standard economic indicators and consider subjective measures that take into account individual differences in perceptions.
Here, we examine the link between economic distress—measured subjectively as well as objectively—and substance abuse. We begin by comparing reported drug and alcohol abuse in 1995–96 and 2011–14 using repeated cross-sectional surveys targeting a national sample of Americans aged 25–74. Given the increase in deaths of despair, we anticipate that:
H1: Prevalence of drug and alcohol abuse will be higher in the early 2010s than the mid-1990s.
Next, we investigate whether subjective measures of economic distress are more strongly associated with drug and alcohol abuse than objective measures of financial and employment conditions. Most prior studies linking economic distress with substance abuse have focused on objective measures, particularly unemployment. Although previous research has focused more on alcohol than drugs, many studies suggest that unemployment is associated with increased substance use or abuse.29,30 Much of the literature assumes that stress is a key mechanism through which adverse economic events cause increased substance use.29,31 Thus, we would expect the impact of economic factors to depend on perception. We found only a few studies that considered subjective measures of economic distress, all of which examined alcohol, but not drug abuse as an outcome.32–34 Kalousova and Burgard34 found perceived decline in economic resources was associated with incidence of alcohol abuse, although unemployment and measured decline in economic resources were not significant. Other studies also found financial strain associated with alcohol abuse,32 at least in some subgroups.33 We hypothesize that:
H2: Subjective measures of economic distress will be more strongly associated with drug and alcohol abuse than objective measures.
Finally, we evaluate the extent to which economic distress accounts for the period trend in reported drug and alcohol abuse. A prior study found that increases in the unemployment rate were associated with higher prevalence of substance use disorders involving analgesics, especially among working-age white men with low educational attainment.35 Other aggregate-level studies have examined the associations between changing economic conditions and opioid prescription rates36–38 or drug mortality.10,37,39,40 None of these studies included subjective measures of economic distress. If growing substance abuse is being driven by despair, then we expect that:
H3: Compared with objective measures, subjective measures of economic distress will account for a larger share of the trends in substance abuse.
METHODS
Data
We use data from the two cross-sectional waves of the Midlife Development in the US study (MIDUS). In 1995–96 (Wave M1), MIDUS targeted a national sample of non-institutionalized, English-speaking adults aged 25–74 in the coterminous United States, selected by random digit dialing with oversampling of older people and men.41 Among those who completed the phone interview (N=3,487, 70% response rate), 3,034 (87%) also completed mail-in self-administered questionnaires (SAQ). In 2011–14 (Wave R1), a new refresher cohort with the same age range was sampled from the national population.42 Among those who completed the phone interview (N=3,577, 59% response rate), 2,598 (73%) also completed the SAQ. We restrict our analyses to those who completed the SAQ, yielding a pooled analysis sample of 5,632 respondents. Using the two cross-sectional waves from MIDUS allows us to identify period effects by comparing Americans of the same age range separated by nearly two decades.
Measures
Drug and Alcohol Abuse
With respect to drug abuse, the respondent is first asked whether s/he uses any of a long list of drugs (i.e., sedatives, tranquilizers, amphetamines, prescription painkillers, inhalants, marijuana/hashish, cocaine/crack/free base, hallucinogens, heroin, prescription anti-depressants) “on your own”—that is, “without a doctor’s prescription, in larger amounts that prescribed, or for a long period than prescribed.” The question refers to “analgesics or other prescription painkillers”, but notes, “This does not include normal use of aspirin, Tylenol without codeine, etc., but does include use of Tylenol with codeine and other prescribed painkillers like Demerol, Darvon, and Percodan.” Those who report any non-medical drug use are then asked about seven problems related to that use during the past 12 months: 1) role interference as a result of use; 2) use in hazardous situations; 3) emotional or psychological problems as a result of use; 4) strong desire or urge to use; 5) a great deal of time using/recovering; 6) using more or for longer than intended; and 7) using more to get the same effect. These are the same seven symptoms included in the Drug Dependence scale of the Composite International Diagnostic Interview Short Form (CIDI-SF).43 Although the MIDUS screener question asks about the same types of drugs as the CIDI-SF, it refers only to non-medical use whereas the CIDI-SF screener includes any use of the listed drugs. More than 90% of the sample report no drug-related problems and less than 5% acknowledge more than one problem. Because of the skewed distribution and the lack of variation beyond a simple dichotomy, we code the respondent as exhibiting drug abuse if s/he reports any of these seven behaviors.
Our measure of alcohol abuse is similar in construction. The seven symptoms included in the Alcohol Dependence scale of the CIDI-SF parallel the Drug Dependence scale,43 but one symptom (i.e., use in hazardous situations) was not asked in later waves of MIDUS; thus, our measure is based on six alcohol-related problems. Unlike the CIDI-SF scale for Alcohol Dependence, which counts these symptoms only if the respondent reports having at least four drinks in a single day within the past 12 months, our measure does not condition based on alcohol consumption because that screener question is not asked in MIDUS. More than 70% of the sample report no alcohol-related problem, while less than 5% admit more than one such problem. Given the skewed distribution, we code the respondent as exhibiting alcohol abuse if s/he reports any of those six problems in the past 12 months. As a sensitivity test, we rerun the analyses using an alternative measure of alcohol abuse based on the four indicators that are also included in the Michigan Alcohol Screening Test (MAST).44
Relative Socioeconomic Status (SES)
Our preliminary examination of the bivariate relationship between socioeconomic status (SES) and substance abuse uses a composite measure of relative SES, which is constructed from six components: respondent’s (and spouse’s) education, respondent’s (and spouse’s) occupation, annual household income, and current net assets of the respondent and spouse. Education of the respondent and his/her spouse/partner (if applicable) are measured in terms of degree completion, with 12 categories ranging from less than 8th grade (=1) to completion of a professional degree (e.g., PhD, MD, JD, etc.) (=12). We categorize the current or most recent occupation of the respondent and his/her spouse/partner (if applicable) into four categories: Farming/Construction/Maintenance/Production/Transportation/Military (=1); Service/Sales/Admin/Office (=2); Management/Business/Financial (=3); Professional (=4). Annual household income is calculated for the respondent, spouse/partner (if applicable), and all other family members living in the household; and total net assets are calculated for the respondent and spouse/partner combined (see Supplementary Material for more details).
Within each cross-sectional survey wave, we standardize the six items and then compute the SES index as the average across relevant items (e.g., six items if married/partnered and both respondent and spouse/partner have ever been employed; three items if not married/partnered and respondent has never been employed; Cronbach’s α=0.75). Because income and assets are strongly and positively skewed, we apply a square root transformation to those items before computing the index. We then convert the score to a percentile rank denoting the respondent’s position within the distribution at a given survey wave, scaled to range from 0 (1st percentile) to 1 (99th percentile). Thus, a one-unit change represents the difference between a person in the bottom versus the top percentile of the SES continuum.
Objective Measures of Economic Distress
Because we want to compare different dimensions of economic distress, our regression models test individual measures of economic distress—some of which are underlying components of the composite score. As conceptualized by Voydanoff,45 economic distress includes both objective and subjective dimensions. We operationalize objective economic distress with three measures of economic deprivation (i.e., income, assets, and health insurance coverage) and two measures of employment instability (i.e., current work status, maximum unemployment spell).
Two measures of economic deprivation are also underlying components of relative SES: annual household income and total net assets (see above). Our third measure of economic deprivation is a dichotomous variable indicating whether the respondent was covered by health insurance at the time of the survey.
The first measure of employment instability is current work status, categorized as: employed; retired; unemployed or temporarily laid off; homemaker or never employed; and all else, which includes students, those who volunteered that they are on maternity/sick leave or permanently disabled, and other responses. Our second measure is the lifetime maximum period of unemployment (when not a student), categorized as: never (including those never employed); less than six months; six months to less than two years; and two or more years.
Subjective Measures of Economic Distress
Our subjective measures of economic distress include the same measures of financial strain (current financial strain, intergenerational disadvantage) and employment uncertainty (current and future) used by Glei et al.28 Current financial strain is represented by an index based on five questions from the SAQ:
“Using a scale from 0 to 10 where 0 means ‘the worst possible financial situation’ and 10 means `the best possible financial situation,’ how would you rate your financial situation these days?”
“Looking ahead ten years into the future, what do you expect your financial situation will be like at that time?” [using the same 0–10 scale]
“Using a 0 to 10 scale where 0 means ǹo control at all’ and 10 means `very much control,’ how would you rate the amount of control you have over your financial situation these days?”
“In general, would you say you (and your family living with you) have more money than you need, just enough for your needs, or not enough to meet your needs?”
“How difficult is it for you (and your family) to pay your monthly bills?” [response categories: very difficult, somewhat difficult, not very difficult, not at all difficult]
Each item is standardized based on the distribution of the pooled sample and coded so that higher values indicate more financial strain. Then, we compute the mean across the five items (Cronbach’s α=0.84).
Intergenerational financial disadvantage is based on the following question: “When your parents were the age you are now, were they better off or worse off financially than you are now?” Responses were coded on a seven-point scale from “a lot better off” to “a lot worse off”; higher values indicate that the respondent perceived him/herself as worse off than his/her parents.
We measure employment uncertainty using the respondent’s ratings of his/her current work situation (“Please think of the work situation you are in now, whether part-time or full-time, paid or unpaid, at home or at a job. Using a scale from 0 to 10 where 0 means `the worst possible work situation’ and 10 means `the best possible work situation,’ how would you rate your work situation these days?”) and his/her expected work situation 10 years in the future (“Looking ahead ten years into the future, what do you expect your work situation will be like at that time?”, using the same scale). We reverse-code these measures so that higher values indicate worse evaluations (i.e., more uncertainty).
Control Variables
The control variables include age, sex, period (R1 vs. M1 wave), race/ethnicity, whether the respondent is married or partnered, and educational attainment.
Analytical strategy
We used the ice command in Stata 14.246 to implement multiple imputation for missing data.47,48 Among the pooled analysis sample (N=5,632), the variables with the highest percentages of missing data were household income (18%), assets (13%), maximum unemployment spell (7%), rating of future work situation (6%), and rating of current work situation (5%). We used multiple imputation to impute missing data on at least one analysis variable for 36% of the pooled sample. All analysis variables and several auxiliary variables (e.g., measures of physical and mental health, smoking status) were included as predictors for multiple imputation. All analyses were weighted using post-stratification weights. We used the lpolyci command in Stata 14.246 to perform local mean smoothing—also known as the Nadaraya-Watson estimator49,50, plotting each outcome variable by age and by SES percentile for the two survey waves.
Next, we fitted a series of logistic regression models for each outcome. The baseline model controlled for sex, age, period, race/ethnicity, marital status, and educational attainment. Based on the age patterns revealed by bivariate analysis, we also included an interaction between period and a dichotomous variable indicating that the respondent was aged 50 or older. We tested several alternative specifications for that interaction: 1) 10-year age groups; 2) age groups <30, 30–49, 50–69, and 70+; 3) cubic specification for age; and 4) dummy for ages 50+. The model that that interacted period with a simple dummy for ages 50+ yielded the best fit (lowest BIC). In Model 2a, we added objective measures of economic distress. Model 2b substituted subjective measures of economic distress. The final model (Model 3) included both objective and subjective measures of economic distress.
RESULTS
Table 1 presents descriptive statistics for all analysis variables by survey wave. As expected, the prevalence of drug abuse was higher in the early-2010s (9.4%) than in the mid-1990s (8.2%), as was the percentage reporting alcohol abuse (28.3% vs. 26.6%, respectively, as measured by the CIDI-SF scale). Compared with 1995–96, average household income (adjusted for inflation) was lower in 2011–14. The mean level of assets (in real dollars) was higher in the later period, but the average is deceptive because the distribution is extremely skewed. A higher percentage of respondents reported no net assets or a deficit in 2011–14 (45%) than in 1995–96 (36%). The percentage currently employed was lower and the unemployed fraction higher in 2011–14 than in 1995–96. Mean levels of subjective economic distress were similar in the two time periods, but as shown in earlier work,28 the averages hide socioeconomic differences in the trend: economic distress was much higher in 2011–14 (compared with 1995–96) among those with low socioeconomic status, whereas levels of economic distress were similar (or even lower in the later period) among the most socioeconomically advantaged.
Table 1.
Descriptive statistics for analysis variables, weighted
| Wave
M1 1995–96 (N=3034) |
Wave
R1 2011–14 (N=2598) |
Pooled M1 & R1 (N=5632) |
|
|---|---|---|---|
| Outcomes | |||
| Any drug abuse, % | 8.2 | 9.4 | 8.7 |
| Any alcohol abuse (based on CIDI-SF scale), % | 26.6 | 28.3 | 27.4 |
| Any alcohol abuse (based on MAST items), % | 7.5 | 7.0 | 7.2 |
| Demographic characteristics | |||
| Male, % | 47.7 | 48.0 | 47.8 |
| Age (20–76), mean (SD) | 45.5 (13.5) | 49.0 (13.6) | 47.1 (13.6) |
| Non-Latino white, % | 81.7 | 80.7 | 81.2 |
| Non-Latino black, % | 8.1 | 7.8 | 8.0 |
| Non-Latino other race, % | 3.8 | 4.2 | 4.0 |
| Latino, % | 6.3 | 7.2 | 6.8 |
| Married or living with a partner, % | 72.2 | 69.1 | 70.8 |
| Education | |||
| H.S. graduate or less | 49.6 | 39.1 | 44.8 |
| Some college | 25.8 | 27.6 | 26.6 |
| B.A./B.S. or higher | 24.6 | 33.3 | 28.6 |
| Objective economic/employment measures | |||
| Household income (0–833),a mean (SD) | 69.3 (73.8) | 53.4 (53.4) | 62.0 (65.7) |
| No assets or a deficit, % | 36.1 | 45.3 | 40.3 |
| Net assets (0–1820),a mean (SD) | 106.2 (275.9) | 139.3 (287.7) | 121.5 (281.9) |
| Covered by health insurance, % | 87.4 | 86.0 | 86.8 |
| Current employment status | |||
| Working, % | 71.4 | 62.3 | 67.2 |
| Unemployed, % | 4.3 | 12.3 | 8.0 |
| Homemaker/never employed, % | 8.5 | 5.9 | 7.3 |
| Retired, % | 12.8 | 14.9 | 13.7 |
| Other, % | 3.1 | 4.7 | 3.8 |
| Maximum unemployment spell | |||
| Never unemployed,b % | 39.0 | 50.6 | 44.4 |
| <6 months, % | 22.9 | 10.0 | 16.9 |
| 6 months to <2 years, % | 16.6 | 16.1 | 16.4 |
| 2+ years, % | 21.5 | 23.3 | 22.3 |
| Subjective economic distress | |||
| Index of current financial strain (−1.96 to 2.9), mean (SD) | −0.1 (0.9) | 0.1 (1.1) | 0.0 (1.0) |
| Current financial situation (0–10=worst), mean (SD) | 4.1 (2.2) | 4.3 (2.5) | 4.2 (2.4) |
| Future financial situation (0–10=worst), mean (SD) | 2.6 (2.1) | 3.2 (2.4) | 2.9 (2.2) |
| Control over financial situation (0–10=no control), mean (SD) | 3.4 (2.5) | 4.0 (2.7) | 3.7 (2.6) |
| Money to meet needs (0–2=not enough), mean (SD) | 1.2 (0.6) | 1.2 (0.7) | 1.2 (0.7) |
| Difficulty paying monthly bills (0–3=very difficult), mean (SD) | 1.3 (0.9) | 1.3 (1.0) | 1.3 (0.9) |
| Intergenerational financial disadvantage (0–6=a lot worse off), mean (SD) | 2.6 (1.8) | 3.0 (1.9) |
2.7 (1.9) |
| Current work uncertainty (0–10=worst), mean (SD) | 2.8 (2.4) | 3.3 (2.8) | 3.0 (2.6) |
| Future work uncertainty (0–10=worst), mean (SD) | 2.4 (2.5) | 2.9 (2.7) | 2.6 (2.6) |
Expressed in thousands of 1995 dollars.
Includes those never employed for six or more months (N=137 at M1, N=54 at R1).
Figure 1 shows the bivariate association between substance use and age at the two waves. In 1995–96, prevalence of drug abuse declined with age, leveling out above age 60 at a very low level. In contrast, the age pattern appears very different by 2011–14: the percentage reporting drug abuse is as high, if not higher, at ages 50–70 than at ages 35–49. We find a similar pattern alcohol abuse: linear decline in alcohol abuse with age in the mid-1990s has been replaced with a more bi-model distribution across age by the early 2010s. Comparing the prevalence of substance abuse between the two periods, the biggest differences are among youngest respondents and those in midlife (50–69).
Figure 1. Smoothed bivariate plots of drug abuse and alcohol abuse by age at MIDUS waves M1 and R1.
Note: These graphs have been restricted to the targeted age range (25–74) because we have only a few respondents aged 20–24 (n=10 at M1, n=5 at R1) and a small number aged 75–76 at R1 (n=0 at M1, n=58 at R1). Thus, our estimates outside the targeted age range are very unstable.
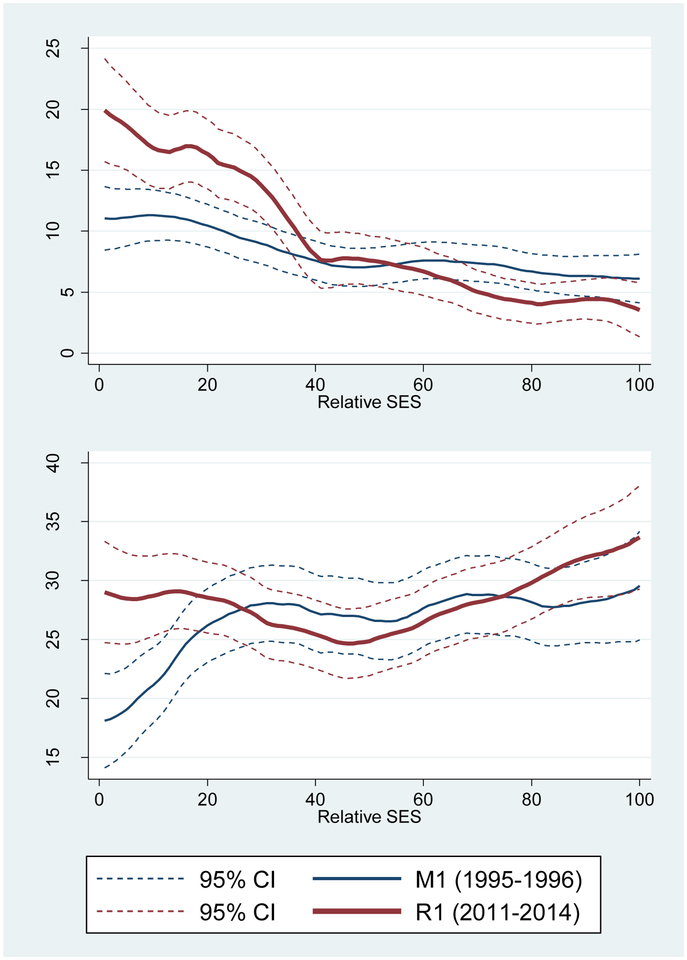
Figure 2 presents a similar plot by relative SES. Reported drug abuse was higher in 2011–14 than in 1995–96 among the bottom third of the socioeconomic spectrum, whereas there was little difference (perhaps even lower abuse) among the most socioeconomically advantaged. The pattern is less clear for alcohol abuse: prevalence of abuse appears higher in the later period among the bottom quintile of SES (largely because prevalence was particularly low at M1 among this group), but also appears higher among the top quintile of SES. Unlike drug abuse, which appears to be inversely associated with SES, the relationship between SES and alcohol is generally positive at both survey waves.
Figure 2. Smoothed bivariate plots of drug abuse and alcohol abuse by relative SES at MIDUS waves M1 and R1.
Rising substance abuse may be associated with higher economic distress, particularly at the bottom of the SES spectrum. The composite measure of SES incorporates multiple dimensions of disadvantage, but does not allow us to determine whether some aspects matter more than others. Thus, in our regression models, we test individual measures in place of the composite measure. For example, educational attainment is included among the sociodemographic control variables. Income and assets are included as objective measures of economic deprivation.
In Model 1, shown in Tables 2 (drug abuse) and 3 (alcohol abuse), we present results from logistic regression models that control for multiple sociodemographic factors simultaneously. The odds of drug abuse was higher in 2011–14 (relative to 1995–96) for those aged 50 and older (OR=2.87, CI=1.94–4.25), but not significant for younger individuals (Table 2). There is a similar pattern for alcohol abuse (ages 50+: OR=1.63, CI=1.30–2.03; ages <50: OR=1.03, CI=0.85–1.24; Table 3). Thus, we find only partial support for our first hypothesis: drug and alcohol abuse is higher in the more recent period, but only for the older age group. Consistent with the bivariate results for the composite measure of relative SES (Figure 2), education is associated with lower odds of drug abuse, but higher odds of alcohol abuse.
Table 2.
Odds ratios and 95% Confidence Intervals (CI) from logit models predicting any drug abuse, pooled data from MIDUS Waves M1 (1995–96) and R1 (2011–14), N=5632
| (1) | (2a) | (2b) | (3) | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Male | 1.73 | 1.35–2.21 | 1.99 | 1.51–2.63 | 1.78 | 1.39–2.29 | 1.93 | 1.47–2.54 |
| Age - 40 | 0.94 | 0.93–0.95 | 0.95 | 0.93–0.96 | 0.94 | 0.93–0.96 | 0.94 | 0.92–0.96 |
| Period 2011–14 × Age <50 | 1.00 | 0.71–1.39 | 0.95 | 0.67–1.34 | 0.84 | 0.61–1.16 | 0.88 | 0.63–1.24 |
| Period 2011–14 × Age 50+ | 2.87 | 1.94–4.25 | 2.69 | 1.78–4.07 | 2.19 | 1.45–3.30 | 2.42 | 1.58–3.72 |
| (Non-Latino white) | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Latino black | 1.01 | 0.61–1.68 | 0.95 | 0.57–1.58 | 0.91 | 0.56–1.49 | 0.95 | 0.58–1.57 |
| Non-Latino other race | 1.07 | 0.59–1.93 | 1.05 | 0.57–1.94 | 1.19 | 0.66–2.14 | 1.20 | 0.64–2.22 |
| Latino | 1.44 | 0.96–2.17 | 1.31 | 0.85–2.03 | 1.49 | 0.99–2.23 | 1.48 | 0.97–2.27 |
| Married or living with a partner | 0.54 | 0.42–0.70 | 0.64 | 0.49–0.85 | 0.65 | 0.50–0.85 | 0.66 | 0.50–0.87 |
| (H.S. graduate or less) | -- | -- | -- | -- | -- | -- | -- | -- |
| Some college | 0.97 | 0.73–1.29 | 1.02 | 0.76–1.37 | 1.09 | 0.81–1.45 | 1.06 | 0.79–1.42 |
| B.A./B.S. or higher | 0.54 | 0.40–0.72 | 0.66 | 0.48–0.90 | 0.76 | 0.56–1.03 | 0.74 | 0.54–1.02 |
| Household incomea | -- | -- | 1.08 | 0.93–1.25 | -- | -- | 1.16 | 1.01–1.33 |
| No assets or a deficit | -- | -- | 1.40 | 1.05–1.87 | -- | -- | 1.14 | 0.85–1.54 |
| Net assetsa | -- | -- | 0.91 | 0.75–1.10 | -- | -- | 1.02 | 0.86–1.22 |
| Covered by health insurance | -- | -- | 0.52 | 0.38–0.73 | -- | -- | 0.62 | 0.45–0.85 |
| Current employment status | ||||||||
| (Working) | -- | -- | -- | -- | -- | -- | -- | -- |
| Unemployed | -- | -- | 1.13 | 0.72–1.78 | -- | -- | 0.74 | 0.45–1.21 |
| Homemaker/never employed | -- | -- | 0.92 | 0.52–1.61 | -- | -- | 0.82 | 0.48–1.42 |
| Retired | -- | -- | 1.18 | 0.68–2.06 | -- | -- | 1.22 | 0.69–2.18 |
| Other | -- | -- | 2.08 | 1.23–3.51 | -- | -- | 1.16 | 0.67–2.01 |
| Maximum unemployment spell | ||||||||
| (Never)b | -- | -- | -- | -- | -- | -- | -- | -- |
| <6 months | -- | -- | 1.40 | 0.97–2.02 | -- | -- | 1.38 | 0.95–2.02 |
| 6 months to <2 years | -- | -- | 1.37 | 0.95–1.96 | -- | -- | 1.28 | 0.89–1.86 |
| 2+ years | -- | -- | 1.97 | 1.34–2.90 | -- | -- | 1.91 | 1.31–2.79 |
| Index of current financial strainc | -- | -- | -- | -- | 1.40 | 1.20–1.64 | 1.37 | 1.16–1.62 |
| Intergenerational financial disadvantagec | -- | -- | -- | -- | 1.17 | 1.02–1.34 | 1.16 | 1.01–1.33 |
| Current work uncertaintyc | -- | -- | -- | -- | 1.19 | 1.02–1.38 | 1.18 | 1.00–1.39 |
| Future work uncertaintyc | -- | -- | -- | -- | 1.12 | 0.94–1.32 | 1.13 | 0.95–1.34 |
| log Ld | −1539.6 | −1493.7 | −1473.1 | −1448.8 | ||||
| Pseudo R2 | 0.077 | 0.105 | 0.118 | 0.132 | ||||
| BIC | 3182.8 | 3194.6 | 3084.3 | 3139.5 | ||||
| AUC | 0.706 | 0.732 | 0.742 | 0.751 |
Expressed in thousands of 1995 dollars and standardized based on (weighted) pooled distribution.
Includes those never employed for six or more months.
Standardized based on the (weighted) pooled distribution.
Mean log L across five multiply-imputed datasets.
Table 3.
Odds ratios and 95% Confidence Intervals (CI) from logit models predicting any alcohol abuse (based on the CIDI-SF), pooled data from MIDUS Waves M1 (1995–96) and R1 (2011–14), N=5632
| (1) | (2a) | (2b) | (3) | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Male | 2.11 | 1.83–2.44 | 1.94 | 1.65–2.27 | 2.13 | 1.84–2.46 | 1.93 | 1.65–2.26 |
| Age - 40 | 0.96 | 0.95–0.96 | 0.96 | 0.95–0.96 | 0.96 | 0.95–0.96 | 0.96 | 0.95–0.96 |
| Period 2011–14 × Age <50 | 1.03 | 0.85–1.24 | 1.10 | 0.90–1.33 | 1.02 | 0.84–1.23 | 1.10 | 0.91–1.34 |
| Period 2011–14 × Age 50+ | 1.63 | 1.30–2.03 | 1.70 | 1.35–2.14 | 1.57 | 1.26–1.96 | 1.66 | 1.32–2.09 |
| (Non-Latino white) | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Latino black | 0.68 | 0.49–0.95 | 0.72 | 0.51–1.01 | 0.66 | 0.47–0.92 | 0.71 | 0.50–1.01 |
| Non-Latino other race | 1.15 | 0.82–1.63 | 1.17 | 0.83–1.65 | 1.17 | 0.83–1.65 | 1.22 | 0.86–1.73 |
| Latino | 0.80 | 0.60–1.06 | 0.82 | 0.62–1.09 | 0.79 | 0.59–1.04 | 0.83 | 0.63–1.10 |
| Married or living with a partner | 0.76 | 0.65–0.90 | 0.73 | 0.61–0.87 | 0.79 | 0.67–0.93 | 0.73 | 0.62–0.87 |
| (H.S. graduate or less) | -- | -- | -- | -- | -- | -- | -- | -- |
| Some college | 1.30 | 1.08–1.55 | 1.21 | 1.01–1.46 | 1.29 | 1.07–1.55 | 1.20 | 0.99–1.44 |
| B.A./B.S. or higher | 1.40 | 1.18–1.67 | 1.23 | 1.02–1.47 | 1.45 | 1.21–1.73 | 1.24 | 1.03–1.50 |
| Household incomea | -- | -- | 1.10 | 1.03–1.18 | -- | -- | 1.13 | 1.05–1.22 |
| No assets or a deficit | -- | -- | 0.81 | 0.68–0.97 | -- | -- | 0.74 | 0.62–0.89 |
| Net assetsa | -- | -- | 1.02 | 0.94–1.10 | -- | -- | 1.04 | 0.97–1.13 |
| Covered by health insurance | -- | -- | 0.86 | 0.68–1.09 | -- | -- | 0.93 | 0.73–1.17 |
| Current employment status | ||||||||
| (Working) | -- | -- | -- | -- | -- | -- | -- | -- |
| Unemployed | -- | -- | 0.97 | 0.71–1.33 | -- | -- | 0.85 | 0.61–1.17 |
| Homemaker/never employed | -- | -- | 0.60 | 0.42–0.86 | -- | -- | 0.59 | 0.41–0.85 |
| Retired | -- | -- | 0.84 | 0.64–1.10 | -- | -- | 0.86 | 0.66–1.14 |
| Other | -- | -- | 1.00 | 0.67–1.50 | -- | -- | 0.86 | 0.57–1.29 |
| Maximum unemployment spell | ||||||||
| (Never)b | -- | -- | -- | -- | -- | -- | -- | -- |
| <6 months | -- | -- | 1.00 | 0.82–1.23 | -- | -- | 0.99 | 0.81–1.21 |
| 6 months to <2 years | -- | -- | 1.19 | 0.97–1.46 | -- | -- | 1.15 | 0.93–1.41 |
| 2+ years | -- | -- | 0.96 | 0.77–1.20 | -- | -- | 0.93 | 0.75–1.16 |
| Index of current financial strainc | -- | -- | -- | -- | 1.07 | 0.98–1.17 | 1.17 | 1.06–1.29 |
| Intergenerational financial disadvantagec | -- | -- | -- | -- | 1.03 | 0.94–1.11 | 1.04 | 0.96–1.13 |
| Current work uncertaintyc | -- | -- | -- | -- | 1.09 | 0.98–1.21 | 1.09 | 0.98–1.21 |
| Future work uncertaintyc | -- | -- | -- | -- | 0.91 | 0.82–1.01 | 0.91 | 0.82–1.02 |
| log Ld | −3062.9 | −3040.8 | −3056.4 | −3027.3 | ||||
| Pseudo R2 | 0.074 | 0.081 | 0.076 | 0.085 | ||||
| BIC | 6229.5 | 6288.8 | 6250.9 | 6296.4 | ||||
| AUC | 0.681 | 0.686 | 0.682 | 0.688 |
Expressed in thousands of 1995 dollars and standardized based on (weighted) pooled distribution.
Includes those never employed for six or more months.
Standardized based on the (weighted) pooled distribution.
Mean log L across five multiply-imputed datasets.
We add objective measures of economic distress in Model 2a. Income is not significantly associated with drug abuse, but it is positively associated with alcohol abuse. Lack of assets is associated with higher odds of drug abuse, but lower odds of alcohol abuse; the level of assets (among those with any assets) is not significant for either outcome. Health insurance coverage is associated with lower odds of drug abuse, but not significantly associated with alcohol abuse. There are few significant differences in substance abuse by current employment status, but maximum unemployment spell is associated with drug abuse: compared with those who were never unemployed, those who were unemployed for two or more years are more likely to report drug abuse. Inclusion of the objective economic/employment measures yields only a modest reduction in the period coefficient for drug abuse and actually magnifies the period coefficient for alcohol abuse.
We substitute subjective measures of economic distress for the objective measures in Model 2b. Current financial strain has the strongest association with drug abuse, but perceived intergenerational financial disadvantage and current work uncertainty are also positively associated with drug abuse. The story is very different for alcohol abuse: none of the subjective measures of economic distress is associated with alcohol abuse. Based on variance explained (pseudo R2) and predictive ability (AUC), the subjective measures are more strongly associated with drug abuse than the objective measures, but the converse is true for alcohol abuse. Subjective economic distress also improves model fit (i.e., reduces BIC) for drug abuse while the objective measures do not. None of the measures of economic distress improve model fit for alcohol abuse. Thus, the results are consistent with our second hypothesis for drug abuse, but not alcohol abuse.
Regarding our third hypothesis, we find that inclusion of the subjective measures of economic distress attenuates the period coefficient for drug abuse above age 50 by 26%, but there is little change in the period coefficent for alcohol abuse. Thus, our third hypothesis is only partially supported: perceived economic distress is more strongly linked with the trend in drug abuse than objective economic measures, but the same is not true for alcohol abuse.
Model 3 includes both the objective and subjective measures of economic distress. In the case of alcohol abuse, we find that current financial strain becomes significantly associated with alcohol abuse net of income, assets, and employment history.
To test the sensitivity of the results to the definition of alcohol abuse, we re-estimated the analyses using the MAST items to identify alcohol abuse (Table 4; see Supplementary Material for details). The results differ with respect to the following: the trend in alcohol abuse (i.e., the period coeffient is not significant based on the MAST); whether SES is positively associated with alcohol abuse (i.e., there is no association based on the MAST); and the relationship between perceived economic distress and alcohol abuse (i.e., it is much stronger based on the MAST).
Table 4.
Odds ratios and 95% Confidence Intervals (CI) from logit models predicting any alcohol abuse (based on the MAST), pooled data from MIDUS Waves M1 (1995–96) and R1 (2011–14), N=5632
| (1) | (2a) | (2b) | (3) | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Male | 1.70 | 1.32–2.19 | 1.60 | 1.22–2.10 | 1.73 | 1.33–2.24 | 1.56 | 1.18–2.04 |
| Age - 40 | 0.95 | 0.94–0.96 | 0.95 | 0.94–0.97 | 0.95 | 0.94–0.97 | 0.95 | 0.93–0.97 |
| Period 2011–14 × Age <50 | 0.89 | 0.64–1.24 | 0.86 | 0.62–1.20 | 0.82 | 0.59–1.13 | 0.84 | 0.61–1.16 |
| Period 2011–14 × Age 50+ | 1.51 | 0.98–2.32 | 1.38 | 0.88–2.16 | 1.29 | 0.84–1.99 | 1.31 | 0.84–2.04 |
| (Non-Latino white) | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Latino black | 0.70 | 0.39–1.26 | 0.67 | 0.37–1.22 | 0.64 | 0.35–1.19 | 0.67 | 0.36–1.24 |
| Non-Latino other race | 1.50 | 0.88–2.55 | 1.44 | 0.83–2.49 | 1.59 | 0.93–2.71 | 1.59 | 0.93–2.73 |
| Latino | 1.04 | 0.67–1.62 | 0.97 | 0.61–1.53 | 1.03 | 0.66–1.61 | 1.03 | 0.65–1.62 |
| Married or living with a partner | 0.55 | 0.43–0.72 | 0.61 | 0.46–0.81 | 0.62 | 0.48–0.80 | 0.62 | 0.46–0.82 |
| (H.S. graduate or less) | -- | -- | -- | -- | -- | -- | -- | -- |
| Some college | 1.09 | 0.80–1.48 | 1.13 | 0.82–1.55 | 1.17 | 0.85–1.59 | 1.14 | 0.83–1.58 |
| B.A./B.S. or higher | 0.94 | 0.69–1.27 | 1.04 | 0.74–1.45 | 1.17 | 0.86–1.59 | 1.13 | 0.81–1.58 |
| Household incomea | -- | -- | 1.00 | 0.85–1.18 | -- | -- | 1.05 | 0.91–1.22 |
| No assets or a deficit | -- | -- | 1.05 | 0.78–1.42 | -- | -- | 0.88 | 0.64–1.20 |
| Net assetsa | -- | -- | 1.00 | 0.85–1.17 | -- | -- | 1.07 | 0.92–1.25 |
| Covered by health insurance | -- | -- | 0.69 | 0.48–0.98 | -- | -- | 0.78 | 0.55–1.12 |
| Current employment status | ||||||||
| (Working) | -- | -- | -- | -- | -- | -- | -- | -- |
| Unemployed | -- | -- | 1.39 | 0.87–2.22 | -- | -- | 0.99 | 0.61–1.61 |
| Homemaker/never employed | -- | -- | 0.71 | 0.38–1.30 | -- | -- | 0.65 | 0.35–1.21 |
| Retired | -- | -- | 1.33 | 0.76–2.35 | -- | -- | 1.39 | 0.80–2.43 |
| Other | -- | -- | 1.72 | 1.02–2.92 | -- | -- | 1.13 | 0.65–1.97 |
| Maximum unemployment spell | ||||||||
| (Never)b | -- | -- | -- | -- | -- | -- | -- | -- |
| <6 months | -- | -- | 1.05 | 0.76–1.44 | -- | -- | 1.03 | 0.75–1.40 |
| 6 months to <2 years | -- | -- | 0.91 | 0.61–1.34 | -- | -- | 0.85 | 0.57–1.27 |
| 2+ years | -- | -- | 0.86 | 0.59–1.25 | -- | -- | 0.82 | 0.56–1.20 |
| Index of current financial strainc | -- | -- | -- | -- | 1.31 | 1.11–1.53 | 1.35 | 1.14–1.60 |
| Intergenerational financial disadvantagec | -- | -- | -- | -- | 1.02 | 0.87–1.18 | 1.03 | 0.88–1.20 |
| Current work uncertaintyc | -- | -- | -- | -- | 1.18 | 1.01–1.37 | 1.17 | 1.01–1.37 |
| Future work uncertaintyc | -- | -- | -- | -- | 1.01 | 0.85–1.21 | 1.01 | 0.85–1.20 |
| log Ld | −1372.4 | −1361.4 | −1346.6 | −1339.6 | ||||
| Pseudo R2 | 0.062 | 0.069 | 0.079 | 0.084 | ||||
| BIC | 2848.5 | 2930.1 | 2831.4 | 2921.0 | ||||
| AUC | 0.688 | 0.700 | 0.715 | 0.719 |
Expressed in thousands of 1995 dollars and standardized based on (weighted) pooled distribution.
Includes those never employed for six or more months.
Standardized based on the (weighted) pooled distribution.
Mean log L across five multiply-imputed datasets.
CONCLUSIONS/DISCUSSION
We find that differences in the prevalence of drug abuse between the mid-1990s and early-2010s vary by age and by SES. We are not aware of any prior comparisons of trends in drug abuse by age or SES, but Jalal et al.51 observed a bi-modal distribution in unintentional drug overdose trends, with bigger rises in mortality at young ages (25–40) and in later life (50–60). Our results for drug abuse show a similar pattern at older ages, but little period difference at younger ages, except perhaps below age 30. This difference in the trend for drug abuse versus drug mortality among young people may relate to the type of drugs involved. Jalal et al.51 revealed that increased drug mortality resulted primarily from heroin and synthetic opioids among young people, whereas prescription opioids and unspecified drugs were bigger contributors among middle-aged persons. We speculate that the key change among young people was a shift to more lethal drugs (e.g., synthetic opioids), which increased the probability of overdosing even if there was little change in the prevalence of abuse; in contrast, among older individuals, we suspect that higher drug mortality resulted from an increase in drug abuse. Our findings showing a bigger period difference in drug abuse at lower socioeconomic status is consistent with a prior study that demonstrated growing educational disparities in drug poisoning mortality rates.52
One prior US survey indicated increased prevalence of alcohol use disorder over recent years,53 whereas another survey showed a decline.54 Similarly, our results are mixed regarding the question of whether the overall prevalence of alcohol abuse has increased. Prior work indicated bigger increases over time in alcohol use disorder at older ages (45+) than at younger ages (18–44),53 which is consistent with our results. Neither our study nor the other study53 find a clear pattern by SES.
Behavioral economics may help explain why subjective measures of economic distress are more strongly associated with drug abuse than objective measures. Behavioral economists argue that decision-making is not based purely on rational choice, but rather is influenced by emotional, social, and cultural factors. Subjective measures may better reflect the myriad factors that shape financial well-being than standard economic indicators like income, employment, and wealth.
Unlike prior studies,29,30,32–34 we find little evidence that alcohol abuse is strongly associated with either subjective or objective measures of economic distress. One explanation is that alcohol abuse may be more sensitive than drug abuse to procyclical influences (i.e., mechanisms by which economic decline benefits health), which offset countercyclical effects (i.e., negative effects of economic decline on health). For example, a decrease in income may reduce substance use if alcohol/drugs are viewed as a discretionary expense.29 Ruhm et al.56,57 found that heavy alcohol consumption declined during economic downturns. To the extent that we find associations between income/wealth and alcohol abuse, our results are also consistent with procyclical effects. Given more limited research on substances other than alcohol and cigarettes,29,30 it is less clear whether there are similar procyclical influences on drug abuse. We can only speculate that once addicted, drug abusers may be less able to self-regulate even if it costs them everything. Ruhm suggests that during difficult economic times, consumers switch to cheaper sources of alcohol.56 Given restrictions on access to prescription and illicit drugs, switching to a cheaper drug may difficult.
Finally, our findings speak to the question: is there a rising tide of economic distress at the root of increasing deaths of despair? If so, we would expect to find similar results for both drug and alcohol abuse. Instead, we find perceived economic distress accounts for part of the period trend in drug abuse, but the results are not clear for alcohol abuse. Admittedly, the increase in alcohol-related mortality has been much less dramatic than the spike in drug-related mortality, and as noted earlier, results are mixed regarding the trend in alcohol abuse. Thus, we may lack sufficient statistical power to detect what could be a small effect. A second possibility is that substance use relates to psychological distress more generally, rather than economic distress per se. A prior study suggested that, over this same time period, mental health has deteriorated among Americans with low socioeconomic status.58
A major limitation of this work is that we cannot determine the direction of causation: is economic distress a cause or a consequence of increased drug use? There are probably causal effects in both directions. For example, a review of prior studies suggests that substance abuse increases the likelihood of unemployment, but most studies that address reverse-causality also find unemployment to be a risk factor for substance abuse.30 Secondly, we must acknowledge the potential for reporting bias. Self-reported drug and alcohol abuse almost certainly under-estimates true prevalence. Furthermore, the MIDUS questions regarding drug abuse are limited to non-medical use of drugs. Thus, some drug usage is omitted by design, even though it could have adverse consequences. In addition, respondents may be less likely to acknowledge non-medical drug use. Accuracy of reporting may also vary across sub-groups, which could bias our results. For example, results based on the CIDI-SF suggest that better educated respondents and those with higher income are more likely to abuse alcohol than their less advantaged counterparts. Yet, the sensitivity of this relationship to the choice of alcohol-related problems used to define abuse casts doubt on its validity. Perhaps this result is an artifact of differential reporting.
Our findings have several implications. First, efforts to address drug abuse may need to pay more attention to patterns of abuse in older individuals and should concentrate efforts among those with low SES. Second, the contradictory results between other national surveys53,55 regarding trends in alcohol abuse, along with our own mixed results for different definitions of alcohol abuse, suggest that minor differences in measurement of alcohol abuse may have a notable effect on the results. To understand inconsistencies between trends in alcohol abuse and alcohol-related mortality, we may need more sensitive measures of alcohol abuse that can distinguish between the type of abuse that poses high risk for mortality versus abuse that may be less deadly albeit still have serious social consequences. Third, our results suggest that the rise in drug abuse among midlife Americans may relate to perceived economic distress that is not captured by standard economic measures. Prior tests of the “despair hypothesis” that rely solely on objective measures may be missing part of the puzzle because despair is, by definition, subjective.
While our results suggest a link between increased economic distress and rising drug abuse, a crucial question remains unresolved: does that relationship arise because economic distress encourages drug abuse or because drug abuse exacerbates economic distress? Efforts to stem the flood of opioids will not solve the problem if drug abuse is merely a symptom of a larger underlying issue as proposed by the despair hypothesis. Alternatively, it is possible that the drug epidemic is being driven entirely by supply: increased access and availability of drugs fueled rising drug abuse, which in turn may have amplified economic despair, alcohol-related mortality, and suicide rates. Identifying the root causes of the US mortality crisis will be crucial for designing effective interventions to address the problem.
HUMAN SUBJECTS APPROVAL STATEMENT
The MIDUS survey obtained written, informed consent from all participants and received human subjects approval from the institutional review board at the University of Wisconsin, Madison.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by the National Institute on Aging [grant numbers P01 AG020166, U19AG051426] and the Graduate School of Arts and Sciences, Georgetown University.
Footnotes
CONFLICT OF INTERERT DISCLOSE STATEMENT
The authors declare they have no conflict of interest.
REFERENCES
- 1.University of California B, Max Planck Institute for Demographic Research. Human Mortality Database. www.mortality.org .Updated 2019 Accessed January 9, 2019.
- 2.Arias E, Heron M, Xu JQ. United States Life Tables, 2014. Table 19 - Estimated life expectancy at birth, in years, by race, Hispanic orgin, and sex: death-registration states, 1900–1928, and United States, 1929–2014 NCHS Data Brief. 2017;National Vital Statistics Reports, Vol. 66, No. 4. [PubMed] [Google Scholar]
- 3.Xu JQ, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2015. NCHS Data Brief. 2016;NCHS Data Brief, No. 267. [PubMed] [Google Scholar]
- 4.Kochanek KD, Murphy SL, Xu JQ, Arias E. Mortality in the United States, 2016. NCHS Data Brief. 2017;NCHS Data Brief, No. 293. [PubMed] [Google Scholar]
- 5.Murphy SL, Xu JQ, Kochanek KD, Arias E. Mortality in the United States, 2017. NCHS Data Brief. 2018;NCHS Data Brief, No. 328. [PubMed] [Google Scholar]
- 6.Muennig PA, Reynolds M, Fink DS, Zafari Z, Geronimus AT. America’s Declining Well-Being, Health, and Life Expectancy: Not Just a White Problem. Am J Public Health. 2018:e1–e6. doi: 10.2105/AJPH.2018.304585 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernstein L. U.S. life expectancy declines again, a dismal trend not seen since World War I. Washington Post. November 29, 2018. 2018;Health and Science. Available from: https://www.washingtonpost.com/national/health-science/us-life-expectancy-declines-again-a-dismal-trend-not-seen-since-world-war-i/2018/11/28/ae58bc8c-f28c-11e8-bc79-68604ed88993_story.html?utm_term=.50f09cacfb4a.
- 8.Stein R Life Expectancy Drops Again As Opioid Deaths Surge In U.S. NPR Web site. https://www.npr.org/sections/health-shots/2017/12/21/572080314/life-expectancy-drops-again-as-opioid-deaths-surge-in-u-s. Published December 21, 2017. Updated 2017. Accessed April 16, 2019.
- 9.Masters RK. Explaining recent mortality trends among younger and middle-aged white Americans. Int J Epidemiol. 2018;47(1):81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ruhm CJ. Deaths of Despair or Drug Problems? National Bureau of Economic Research Working Paper Series. 2018;Working Paper 24188. http://www.nber.org/papers/w24188. doi: 10.3386/w24188. [DOI] [Google Scholar]
- 11.Mars SG, Fessel JN, Bourgois P, Montero F, Karandinos G, Ciccarone D. Heroin-related overdose: The unexplored influences of markets, marketing and source-types in the United States. Soc Sci Med. 2015;140:44–53. doi: 10.1016/j.socscimed.2015.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Unick G, Rosenblum D, Mars S, Ciccarone D. The relationship between US heroin market dynamics and heroin-related overdose, 1992–2008. Addiction. 2014;109(11):1889–1898. doi: 10.1111/add.12664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999–20187. NCHS Data Brief. 2018;No. 329. [PubMed] [Google Scholar]
- 14.Case A, Deaton A. Mortality and morbidity in the 21st century. Brookings Papers on Economic Activity. 2017:397–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khazan O Middle-Aged White Americans Are Dying of Despair. https://www.theatlantic.com/health/archive/2015/11/boomers-deaths-pnas/413971/. Updated 2015. Accessed December 11, 2017. [Google Scholar]
- 17.Case A ‘Deaths of despair’ are killing America’s white working class. https://qz.com/583595/deaths-of-despair-are-killing-americas-white-working-class/. Updated 2015. Accessed December 11, 2017.
- 18.Monnat SM. Deaths of Despair and Support for Trump in the 2016 Presidential Election, The Pennsylvania State University Department of Agricultural Economics, Sociology, and Education Research Brief. . 2016. [Google Scholar]
- 19.Woolf SH, Chapman DA, Buchanich JM, Bobby KJ, Zimmerman EB, Blackburn SM. Changes in midlife death rates across racial and ethnic groups in the United States: systematic analysis of vital statistics. BMJ. 2018;362:k3096. doi: 10.1136/bmj.k3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cherlin AJ. Why are white death rates rising? New York Times. 2016;The Opinion Pages:A19. Available from: http://www.nytimes.com/2016/02/22/opinion/why-are-white-death-rates-rising.html?emc=eta1&_r=0. Accessed June 25, 2016. [Google Scholar]
- 21.Stein EM, Gennuso KP, Ugboaja DC, Remington PL. The Epidemic of Despair Among White Americans: Trends in the Leading Causes of Premature Death, 1999–2015. Am J Public Health. 2017;107(10):1541–1547. doi: 10.2105/AJPH.2017.303941 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cherlin AJ. Labor’s love lost: the rise and fall of the working class family in America. New York: Russell Sage; 2014. [Google Scholar]
- 23.Sasson I Trends in Life Expectancy and Lifespan Variation by Educational Attainment: United States, 1990–2010. Demography. 2016;53(2):269–293. doi: 10.1007/s13524-015-0453-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hayward MD, Hummer RA, Sasson I. Trends and group differences in the association between educational attainment and U.S. adult mortality: implications for understanding education’s causal influence. Soc Sci Med. 2015;127:8–18. doi: 10.1016/j.socscimed.2014.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Olshansky SJ, Antonucci T, Berkman L, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff (Millwood). 2012;31(8):1803–1813. doi: 10.1377/hlthaff.2011.0746 [doi]. [DOI] [PubMed] [Google Scholar]
- 26.Montez JK, Hummer RA, Hayward MD, Woo H, Rogers RG. Trends in the Educational Gradient of U.S. Adult Mortality from 1986 to 2006 by Race, Gender, and Age Group. Res Aging. 2011;33(2):145–171. doi: 10.1177/0164027510392388 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315(16):1750–1766. doi: 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glei DA, Goldman N, Weinstein M. Perception has its own reality: Subjective versus objective measures of economic distress. Popul Dev Rev. 2018;44(4):695–722. doi: 10.1111/padr.12183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Catalano R, Goldman-Mellor S, Saxton K, et al. The health effects of economic decline. Annu Rev Public Health. 2011;32:431–450. doi: 10.1146/annurev-publhealth-031210-101146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Henkel D Unemployment and substance use: a review of the literature (1990–2010). Curr Drug Abuse Rev. 2011;4(1):4–27. [DOI] [PubMed] [Google Scholar]
- 31.Burgard SA, Ailshire JA, Kalousova L. The great recession and health: people, populations, and disparities. Ann Am Acad Pol Soc Sci. 2013;650(1):194–213. [Google Scholar]
- 32.Beenackers MA, Oude Groeniger J, van Lenthe FJ, Kamphuis CBM. The role of financial strain and self-control in explaining health behaviours: the GLOBE study. Eur J Public Health. 2018;28(4):597–603. doi: 10.1093/eurpub/ckx212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shaw BA, Agahi N, Krause N. Are changes in financial strain associated with changes in alcohol use and smoking among older adults? J Stud Alcohol Drugs. 2011;72(6):917–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kalousova L, Burgard SA. Unemployment, measured and perceived decline of economic resources: contrasting three measures of recessionary hardships and their implications for adopting negative health behaviors. Soc Sci Med. 2014;106:28–34. doi: 10.1016/j.socscimed.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 35.Carpenter CS, McClellan CB, Rees DI. Economic conditions, illicit drug use, and substance use disorders in the United States. J Health Econ. 2017;52:63–73. [DOI] [PubMed] [Google Scholar]
- 36.Currie J, Jin JY, Schnell M. US employment and opioids: Is there a connection? National Bureau of Economic Research Working Paper Series. 2018;No. 24440. http://www.nber.org/papers/w24440.
- 37.Charles KK, Hurst E, Schwartz M. The transformation of manufacturing and the decline in US employment In: NBER Macroeconomics Annual 2018, volume 33 University of Chicago Press; 2018. [Google Scholar]
- 38.Krueger A Where Have All the Workers Gone? An Inquiry into the Decline of the U.S. Labor Force Participation Rate. BPEA Conference Drafts, September 7–8, 2017. Brookings Papers on Economic Activity. 2017:1–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hollingsworth A, Ruhm CJ, Simon K. Macroeconomic conditions and opioid abuse. J Health Econ. 2017;56:222–233. [DOI] [PubMed] [Google Scholar]
- 40.Pierce JR, Schott PK. Trade liberalization and mortality: Evidence from US counties. National Bureau of Economic Research Working Paper Series. 2016;No. 22849. http://www.nber.org/papers/w22849.
- 41.Brim OG, Baltes PB, Bumpass LL, et al. National Survey of Midlife Development in the United States (MIDUS), 1995–1996. ICPSR02760-v11. . 2016. [Google Scholar]
- 42.Ryff C, Almeida D, Ayanian J, et al. Midlife in the United States (MIDUS Refresher), 2011–2014. ICPSR36532-v2. . 2016. [Google Scholar]
- 43.Kessler RC, Andrews G, Mroczek D, Ustun TB, Wittchen H-. The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int J Methods Psychiatr Res. 1998;7(4):171–185. [Google Scholar]
- 44.Selzer ML. The Michigan alcoholism screening test: the quest for a new diagnostic instrument. Am J Psychiatry. 1971;127(12):1653–1658. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- 45.Voydanoff P Economic distress and family relations: a review of the eighties. Journal of Marriage and Family. 1990;52(4):1099–1115. [Google Scholar]
- 46.StataCorp. Stata: Release 14. Statistical Software. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 47.Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999;8(1):3–15. [DOI] [PubMed] [Google Scholar]
- 48.Rubin DB. Multiple imputation after 18+ years (with discussion). J Am Stat Assoc. 1996;91:473–489. [Google Scholar]
- 49.Nadaraya EA. On estimate regression. Theory of Probability and Its Application. 1964;9:141–142. [Google Scholar]
- 50.Watson G Smooth regression analysis. Sankhya Series A. 1964;26:359–372. [Google Scholar]
- 51.Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, Burke DS. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. 2018;361(6408): 10.1126/science.aau1184. doi: eaau1184 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Richardson R, Charters T, King N, Harper S. Trends in Educational Inequalities in Drug Poisoning Mortality: United States, 1994–2010. Am J Public Health. 2015;105(9):1859–1865. doi: 10.2105/AJPH.2015.302697 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001–2002 to 2012–2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911–923. doi: 10.1001/jamapsychiatry.2017.2161 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health. . 2017;HHS Publication No. SMA 17–5044, NSDUH Series H-52. [Google Scholar]
- 55.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health. https://wwwsamhsagov/data/sites/default/files/NSDUH-FFR1-2016/NSDUH-FFR1-2016htm. 2017;HHS Publication No. SMA 17–5044, NSDUH Series H-52.
- 56.Ruhm CJ. Economic conditions and alcohol problems. J Health Econ. 1995;14(5):583–603. doi: 0167629695000240 [pii]. [DOI] [PubMed] [Google Scholar]
- 57.Ruhm CJ, Black WE. Does drinking really decrease in bad times? J Health Econ. 2002;21(4):659–678. doi: S0167–6296(02)00033–4 [pii]. [DOI] [PubMed] [Google Scholar]
- 58.Goldman N, Glei DA, Weinstein M. Declining mental health among disadvantaged Americans. Proc Natl Acad Sci U S A. 2018;115(28):7290–7295. doi: 10.1073/pnas.1722023115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.von Hippel PT, Scarpino SV, Holas I. Robust estimation of inequality from binned incomes. Sociological Methodology. 2016;46(1):212–251. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.