Abstract
Purpose:
Young age has been shown to be an independent predictor of poor outcome in breast cancer. In human epidermal growth factor receptor 2 (HER2)-positive breast cancer, the effects of aging remain largely unknown.
Patients and Methods:
4,547 patients were included (3,132 from North Central Cancer Treatment Group [NCCTG] N9831 and 1,415 from National Surgical Adjuvant Breast and Bowel Project [NSABP] B-31). Pathologic stromal tumor infiltrating lymphocyte (sTIL) and molecular tumor infiltrating lymphocyte (mTIL) signatures were evaluated.
Results:
In NCCTG N9831, comparable benefit of trastuzumab was observed in all patients (age ≤40; hazard ratio [HR], 0.43; 95% CI, 0.28-0.66; P<0.001; and age >40; HR, 0.56; 95% CI, 0.45-0.69; P<0.001). Similar results were observed in NSABP B-31 (age ≤40; HR, 0.45; 95% CI, 0.29-0.68; P<0.001; and age >40; HR, 0.42; 95% CI, 0.33-0.54; P<0.001). Among patients who received chemotherapy alone, younger age was associated with poor outcome in the hormone receptor-positive subset, but not the hormone receptor-negative subset, in both trials. While there was no association between sTIL and age, a small, but significant increase in mTIL CD45 and some immune subset signatures were observed. Among patients who received chemotherapy alone, patients over 40 years of age with lymphocyte-predominant breast cancer had excellent outcome, with 95% remaining recurrence-free at 15 years.
Conclusions:
Among patients treated with trastuzumab, there was no significant difference in outcome related to age. Our study suggests that trastuzumab can negate the poor prognosis associated with young age.
Keywords: HER2-positive breast cancer, age, immune landscape
Introduction
Breast cancer is among the most common malignancies afflicting women worldwide (1). While breast cancer is generally a disease of aging, a number of patients develop breast cancer at a young age. In developed countries, breast cancer is the leading cause of cancer-related death among women younger than 40 years of age(2), and approximately 6.6% of breast cancer occurs in patients younger than 40 (3). Several studies consistently demonstrated that young age is an independent factor associated with adverse outcome (4–7), which can only partly be attributed to aggressive phenotypes. Breast cancers in young patients are more likely to have hormone receptor negativity, lymphovascular invasion, and high histologic grade compared to those in older patients.(8) Nevertheless, after adjustment for these known aggressive phenotypes, young age continues to be an independent predictor of recurrence and poor outcome (7).
Early genomic studies established that breast cancers arising in younger patients are different from those occurring in older patients. One of the gene sets that differs in breast cancers occurring in younger patients is the immune function-related gene set (4). Still, the immune architecture of breast cancers arising in younger patients compared to older patients has not been elucidated to date. Furthermore, given that breast cancer is a heterogeneous disease comprised of multiple subtypes, it is critical to discern the immune architecture for each intrinsic subtype of breast cancer. Human epidermal growth factor receptor 2 (HER2)-positive breast cancer is a unique subset, accounting for approximately 15% to 30% of breast cancers (9,10). Historically, HER2 overexpression conferred poor outcome, with high rates of disease recurrence, metastasis, and death. However, with the advent of treatments targeting HER2, particularly trastuzumab, the outcome of patients with HER2-positive breast cancer has drastically improved in the past 2 decades (11).
Trastuzumab, a monoclonal antibody against the extracellular domain of HER2, is thought to exert its activity via several mechanisms, including inhibition of downstream signaling of HER2 (12) as well as immune-mediated tumor cell killing, particularly by antibody-dependent cellular cytotoxicity (13,14). To date, the effects of patients’ preexisting immune response according to age and benefit of trastuzumab have not been elucidated. In the previous study from the Herceptin Adjuvant (HERA) trial, age of 40 years or younger at study entry was not associated with risk of early recurrence (15). However, the median follow-up of this study was only 2 years. Therefore, we sought to evaluate the long-term outcome and immune landscape of adjuvant trastuzumab-treated HER2-positive breast cancer patients aged 40 years or younger compared to older patients. Patients in this study were accrued to the N9831 trial from North Central Cancer Treatment Group (NCCTG), now part of Alliance for Clinical Trials in Oncology, and the B-31 trial from National Surgical Adjuvant Breast and Bowel Project (NSABP), now part of NRG.
Materials and Methods
Patient Population
The NCCTG N9831 trial is a randomized, multicenter, phase III trial that enrolled women with primary, operable, node-positive or high-risk node-negative HER2-positive breast cancer who were eligible for adjuvant chemotherapy. Patients were randomly assigned to 1 of 3 arms: arm A received only standard adjuvant chemotherapy with doxorubicin and cyclophosphamide followed by weekly paclitaxel (AC-T); arm B patients received AC-T followed by trastuzumab after completion of chemotherapy; and arm C patients received AC-T concurrently with trastuzumab (AC-TH). NSABP B-31 trial is a 2-arm, randomized, phase III trial that enrolled patients with operable, node-positive, HER2-positive breast cancer. Eligible patients were randomly assigned to AC-T, with paclitaxel either every 3 weeks or weekly, or to AC-TH. The study has been performed in accordance with the Declaration of Helsinki and good clinical practice guidelines. Each participant signed an Institutional Review Board-approved, protocol-specific informed consent document in accordance with federal and institutional guidelines. The primary results of these two trials were previously published in 2005,(16) 2011,(17,18) and 2014 (19).
Pathologic Quantification of Tumor Infiltrating Lymphocytes
Data regarding pathologic quantification of stromal tumor-infiltrating lymphocytes (sTILs) were available in a subset of patient samples from AC-T and AC-TH arms of the NCCTG N9831 trial, as previously reported in Perez et al. (20). sTIL quantification was not available in the NSABP B-31 trial. Histopathologic analysis of sTILs was performed with a single hematoxylin-eosin-stained section using the method previously described by Loi et al. (21), Denkert et al. (22), Adams et al. (23), and Salgado et al. (24). The degree of sTILs was collected in deciles, and similar to the previous publication by Loi et al. (25), lymphocyte-predominant breast cancer (LPBC) was defined as tumors with 50% or more sTILs.
Molecular Tumor-Infiltrating Lymphocytes and Immune Subset Signatures
Gene expression data involving immune-related genes were analyzed in 1,378 samples from the NCCTG N9831 trial. There were no data regarding immune-related gene expression in the NSABP B-31 samples. NanoString (NanoString Technologies, Inc.) was used to quantify mRNA in RNA from paraffin-embedded tumor samples from NCCTG N9831. NanoString custom CodeSets were constructed to comprise 1,252 genes, including 5 housekeeping genes (B2M, GAPDH, POLR2A, UBC, YWHAZ) for normalization purposes. Background variation was removed by correcting for the geometric mean of positive spike-in RNAs, and by subtracting the mean plus 2 standard deviations of negative spike-ins. Normalization proceeded by multiplying a patient’s expression profile by a factor scaled to the geometric mean of their housekeeping genes, via the R package NanoStringNorm (26). Molecular tumor-infiltrating lymphocyte (mTIL) signatures were calculated using normalized and log2 transformed data as previously published by Danaher et al. (27). The geometric mean across relevant genes (Supplemental Table 1) was calculated to generate the composite score for each immune subset signature, namely CD45, B cell, CD8 T cell, cytotoxic cell, exhausted CD8, immature dendritic cell (iDC), macrophage, mast cell, neutrophil, natural killer (NK) CD56dim cell, T cell, and regulatory T cell signatures. The score was mean-centered and standardized in all analyses.
Statistical Analysis
For outcome analysis, recurrence-free survival (RFS) was defined as the time from random assignment to breast cancer recurrence (local, regional, or distant recurrence of breast cancer or breast cancer-related death). The time to event for patients who died without recurrence was considered censored at the time of death. Log-rank P values were employed to assess survival differences among groups with more than 2 categories. Cox proportional hazard models were used to generate point estimates of hazard ratios (HRs) and corresponding 95% CIs to assess the benefit of trastuzumab for RFS in each age group, with age treated as both a continuous and dichotomous variable [defined as age ≤ 40 vs >40 years by Partridge et al. (15)]. The effect of age was also assessed in multivariate HRs controlling for hormonal status, breast cancer subtype, and immune subtype scores. Gene Ontology Enrichment Analysis (Gene Ontology Consortium) was used to calculate fold enrichment of biologic processes of genes of interest. All statistical analyses were carried out in R version 3.2.3 (The R Foundation) on a dataset locked on November 14, 2017.
Results
Baseline Characteristics, Age, and Outcome
There were 4,547 patients with available data from both trials, with 3,132 from NCCTG N9831 and 1,415 from NSABP B-31 (Supplemental Figure 1A and B). The median follow-up was 10.3 years in NCCTG N9831 and 8 years in NSABP B-31. The median age was similar in both trials, with 49 years (range 19–82) in NCCTG N9831 and 49.6 years (range 26–77) in NSABP B-31. Across both trials, 3,625 (79.72%) patients were older than 40 years and 922 (20.28%) were 40 years or younger. Patients’ baseline characteristics for both NCCTG N9831 and NSABP B-31 are stratified by age in Table 1, respectively. Similar to the previous report by Partridge et al,(15) younger age (≤ 40) was associated with significantly higher hormone receptor positivity in NCCTG N9831, but not in NSABP B-31 (χ2 P=.02 and P=.78, respectively). Tumor grade was also higher in younger patients (P=.04). However, there was no significant difference in tumor size or nodal status among younger versus older patients (Table 1).
Table 1.
Baseline Characteristics and Age in NCCTG N9831 and NSABP B-31
| NCCTG N9831 Characteristics |
Age ≤ 40 (n=642) |
Age > 40 (n=2,490) |
Total (n=3,132) |
P Value |
|---|---|---|---|---|
| Age | <.0001 | |||
| Median | 36.0 | 52.0 | 49.0 | |
| Mean | 35.4 | 53.2 | 49.5 | |
| Tumor size, No. (%) | .21 | |||
| <2 cm | 265 (41.3) | 985 (39.6) | 1,250 (39.9) | |
| 2.0-4.9 cm | 314 (48.9) | 1,302 (52.3) | 1,616 (51.6) | |
| ≥5 cm | 63 (9.8) | 203 (8.2) | 266 (8.5) | |
| Nodal status, No. (%) | .21 | |||
| N0 | 71 (11.1) | 345 (13.9) | 416 (13.3) | |
| N1 | 535 (83.3) | 1,990 (79.9) | 2,525 (80.6) | |
| N2 | 36 (5.6) | 153 (6.1) | 189 (6.0) | |
| N3 | 0 (0.0) | 2 (<0.1) | 2 (<0.1) | |
| Menopausal status, No. (%) | <.0001 | |||
| Premenopausal or >50 years old | 621 (96.7) | 1,064 (42.7) | 1,685 (53.8) | |
| Postmenopausal or >50 years old | 21 (3.3) | 1,426 (57.3) | 1,447 (46.2) | |
| Histologic grade, No. (%) | .04 | |||
| Low (1-2) | 154 (24.3) | 699 (28.4) | 853 (27.6) | |
| High (3) | 479 (75.7) | 1,759 (71.6) | 2,238 (72.4) | |
| Unknown | 9 | 32 | 41 | |
| Hormonal status, No. (%) | .02 | |||
| Negative | 269 (41.9) | 1,174 (47.1) | 1,443 (46.1) | |
| Positive | 373 (58.1) | 1,316 (52.9) | 1,689 (53.9) | |
| Treatment arm, No. (%) | .04 | |||
| A | 226 (35.2) | 861 (34.6) | 1,087 (34.7) | |
| B | 246 (38.3) | 850 (34.1) | 1,096 (35.0) | |
| C | 170 (26.5) | 779 (31.3) | 949 (30.3) | |
| NSABP B-31 Characteristics |
Age ≤ 40 (n=280) |
Age > 40 (n=1,135) |
Total (N=1,415) |
P Value |
| Age | <.0001 | |||
| Median | 37.0 | 52.0 | 49.0 | |
| Mean | 36.2 | 52.9 | 49.6 | |
| Tumor size, No. (%) | .69 | |||
| <2 cm | 85 (30.4) | 341 (30.0) | 426 (30.1) | |
| 2.0-4.9 cm | 155 (55.4) | 652 (57.4) | 807 (57.0) | |
| ≥5 cm | 40 (14.3) | 142 (12.5) | 182 (12.9) | |
| Missing | 2 | 2 | 4 | |
| Nodal status, No. (%) | .64 | |||
| N0 | 0 | 0 | 0 | |
| N1 | 149 (53.2) | 638 (56.2) | 787 (55.6) | |
| N2 | 89 (31.8) | 344 (30.3) | 433 (30.6) | |
| N3 | 42 (15.0) | 153 (13.5) | 195 (13.8) | |
| Hormonal status, No. (%) | .78 | |||
| Negative | 134 (47.9) | 554 (48.8) | 688 (48.6) | |
| Positive | 146 (52.1) | 581 (51.2) | 727 (51.4) | |
| Treatment arm, No. (%) | .22 | |||
| 1 | 149 (53.2) | 557 (49.1) | 706 (49.9) | |
| 2 | 131 (46.8) | 578 (51.0) | 709 (50.1) |
Abbreviation: NCCTG, North Central Cancer Treatment Group and NSABP, National Surgical Adjuvant Breast and Bowel Project.
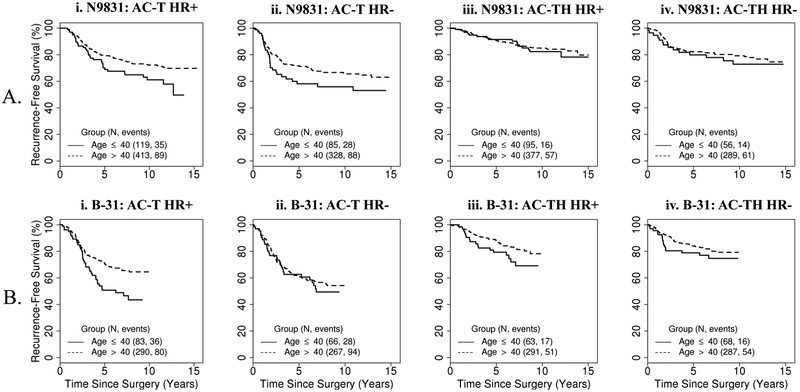
Comparing younger versus older patients, similar survival benefit of trastuzumab was observed in both age groups (age by treatment interaction P= 0.1; P=.27 for NCCTG N9831 and P=.82 for NSABP B-31). In the combined analysis of both NSAPB B-31 and NCCTG N9831 trials, age was a significant predictor of poor outcome only in patients who received chemotherapy alone (P<0.001) and not in patients who received trastuzumab-based chemotherapy (P=.12). In NCCTG N9831, 8-year RFS rate was 63.5% with AC-T versus 83.1% with AC-TH in younger patients (HR, 0.43; 95% CI, 0.28–0.66; P<0.001; Figure 1A). In older patients, 8-year RFS rate was 71.1% in the AC-T arm versus 83.4% in the AC-TH arm (HR, 0.56; 95% CI, 0.45–0.69; P<0.001; Figure 1B). In NSABP B-31, 8-year RFS rate was 46.3% with AC-T versus 72.0% with AC-TH in younger patients (HR, 0.45; 95% CI, 0.29–0.68; P<0.001; Figure 1C) and 60.3% and 80.3%, respectively, in older patients (HR, 0.42; 95% CI, 0.33–0.54; P<0.001; Figure 1D).
Figure 1.
Kaplan-Meier Curves of Recurrence-Free Survival Comparing Chemotherapy Alone and Concurrent Trastuzumab Arms. A, NCCTG N9831 patients ≤ 40 years old; B, NCCTG N9831 patients > 40 years old; C, NSABP B-31 patients ≤ 40 years old; D, NSABP B-31 patients > 40 years old. AC-T indicates adjuvant chemotherapy followed by paclitaxel; AC-TH, adjuvant chemotherapy followed by paclitaxel with concurrent trastuzumab; NCCTG, North Central Cancer Treatment Group; NSABP, National Surgical Adjuvant Breast and Bowel Project.
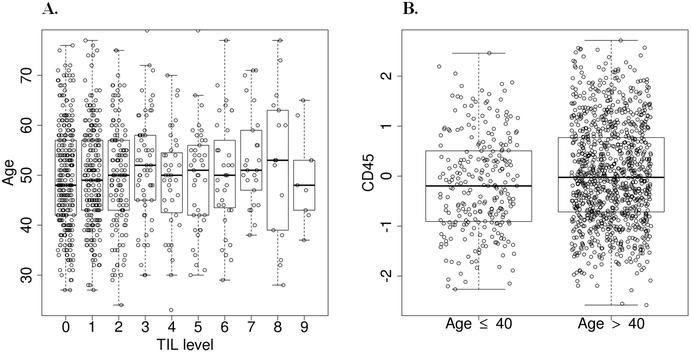
Given that previous studies of HER2-positive breast cancer demonstrated differential complete pathologic response to neoadjuvant chemotherapy among patients with hormone receptor-positive (HR+) versus hormone receptor-negative (HR−) disease,(28,29) we evaluated outcome as a function of HR status. Furthermore, to match NSABP B-31 trial, which only included patients with lymph node involvement, we only analyzed patients with lymph node involvement in the NCCTG N9831 trial (N = 2,716). We observed a significant difference in outcome among younger versus older patients with HR+ disease receiving AC-T (P=.04, Figure 2Ai), though HR− patients did not reach this threshold (P=.09, Figure 2Aii; interaction p-value > 0.1). Similar results were observed in NSABP B-31 (P=.01, Figure 2Bi and P=.60, Figure 2Bii; interaction p-value > 0.1). However, there was no significant difference in outcome between younger and older patients who received AC-TH in either trial, regardless of their hormone receptor status (Figures 2Aiii, 2Aiv, 2Biii, and 2Biv).
Figure 2.
Kaplan-Meier Curves of Recurrence-Free Survival Stratified by Age ≤ 40 Versus > 40 Years Old in Separate Analysis. A, NCCTG N9831 patients with lymph node involvement (N = 2,716): i, HR+ subgroup in chemotherapy alone arm; ii, HR− subgroup in chemotherapy alone arm; iii, HR+ in concurrent trastuzumab arm; and iv, HR− in concurrent trastuzumab arm. B, NSABP B-31 patients with lymph node involvement (N = 1,415): i, HR+ subgroup in chemotherapy alone arm; ii, HR− in chemotherapy alone arm; iii, HR+ subgroup in concurrent trastuzumab arm; and iv, HR− in concurrent trastuzumab arm. AC-T indicates adjuvant chemotherapy followed by paclitaxel; AC-TH, adjuvant chemotherapy followed by paclitaxel with concurrent trastuzumab; HR+, hormone receptor-positive; HR−, hormone receptor-negative; NCCTG, North Central Cancer Treatment Group; and NSABP, National Surgical Adjuvant Breast and Bowel Project.
Immune Landscape in Younger Versus Older Patients
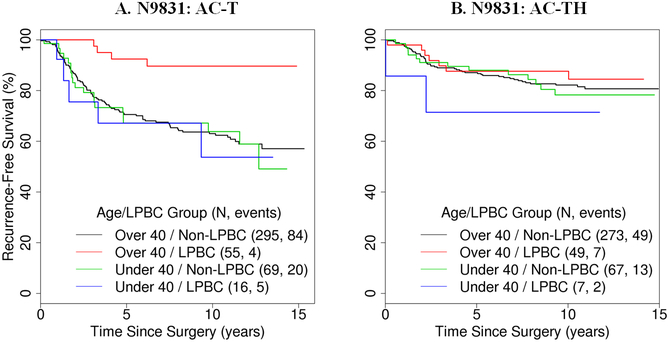
Pathologic quantification of sTIL was available in 831 patients from the NCCTG N9831 trial with 435 patient samples from the AC-T arm and 396 from the AC-TH arm. In this cohort, 159 (19.13%) patients were 40 years old or younger and 672 (80.87%) patients were older than 40. One hundred twenty-seven (15.3%) patient samples had sTIL of 50% or greater and were categorized as LPBC. Overall, there was no significant association between the amount of sTIL by deciles and age in both continuous (P=.19; Figure 3A) and dichotomized analyses (χ2 P=.75). Among younger patients, 14.4% (23/159 patients) had LPBC. Similarly, 15.5% (104/672) of older patients had LPBC. More comprehensive analysis was carried out using gene expression signatures to identify individual immune infiltrates. mTIL used CD45 to estimate total leukocyte infiltration. There was a small but statistically significant increase in mTIL CD45 expression with older age (linear regression, P=.01) (Figure 3B). Similar trends were observed in other mTIL subset signatures (Table 2), including cytotoxic cells (P=.03), exhausted CD8 (P=.02), macrophages (P<0.001), neutrophils (P<0.001), NK CD56dim (P<0.001), T cells (P=.02), and regulatory T cells (P=.04). However, there was no statistically significant difference in B cells (P=.09), CD8 T cells (P=.14), and iDC (P=.17) among younger and older subgroups.
Figure 3.
A, Pathologic quantification of stromal TIL in deciles and age. B, Molecular TIL and age. ER/PR indicates estrogen receptor/progesterone receptor; TIL, tumor infiltrating lymphocytes.
Table 2:
Molecular Tumor Infiltrating Lymphocytes and Immune Subset Signatures Stratified by Age ≤ 40 Versus > 40 Years Old in NCCTG N9831
| mTIL Signatures | Age ≤ 40 (n=281) |
Age > 40 (n=1,111) |
Total (N=1,392) |
Mann-Whitney P Value |
|---|---|---|---|---|
| CD45 | .004 | |||
| Mean | −0.2 | 0.0 | 0.0 | |
| Median (range) | −0.2 (−2.4-2.4) | 0.0 (−2.8-2.9) | −0.1 (−2.8-2.9) | |
| B cells | .09 | |||
| Mean | −0.2 | 0.0 | 0.0 | |
| Median (range) | −0.3 (−2.7-3.4) | −0.1 (−3.0-4.1) | −0.2 (−3.0-4.1) | |
| CD8 T cells | .14 | |||
| Mean | −0.1 | 0.0 | 0.0 | |
| Median (range) | −0.1 (−2.8-2.3) | 0.0 (−3.0-2.5) | 0.0 (−3.0-2.5) | |
| Cytotoxic cells | .03 | |||
| Mean | −0.2 | 0.0 | 0.0 | |
| Median (range) | −0.2 (−3.0-2.8) | 0.1 (−2.9-3.6) | 0.0 (−3.0-3.6) | |
| Exhausted CD8 | .02 | |||
| Mean | −0.1 | 0.0 | 0.0 | |
| Median (range) | −0.1 (−1.3-1.4) | 0.0 (−1.4-2.2) | 0.0 (−1.4-2.2) | |
| iDC | .17 | |||
| Mean | −0.1 | 0.0 | 0.0 | |
| Median (range) | −0.1 (−3.2-2.0) | 0.1 (−2.6-2.6) | 0.0 (−3.2-2.6) | |
| Macrophages | .0003 | |||
| Mean | −0.2 | 0.0 | 0.0 | |
| Median (range) | −0.2 (−2.2-1.8) | 0.0 (−3.4-3.0) | 0.0 (−3.4-3.0) | |
| Mast cells | .08 | |||
| Mean | 0.1 | 0.0 | 0.0 | |
| Median (range) | 0.2 (−5.3-4.5) | 0.1 (−5.4-4.5) | 0.1 (−5.4-4.5) | |
| Neutrophils | .0005 | |||
| Mean | −0.1 | 0.0 | 0.0 | |
| Median (range) | −0.1 (−2.9-1.7) | 0.0 (−2.7-2.9) | 0.0 (−2.9-2.9) | |
| NK-CD56dim cells | .001 | |||
| Mean | −0.2 | 0.0 | 0.0 | |
| Median (range) | −0.2 (−3.2-2.1) | 0.0, (−2.9-2.9) | 0.0 (−3.2-2.9) | |
| T cells | .02 | |||
| Mean | −0.1 | 0.0 | 0.0 | |
| Median (range) | −0.2 (−2.6-2.4) | 0.0 (−2.9-2.5) | 0.0 (−2.9-2.5) | |
| Treg | .04 | |||
| Mean | −0.1 | 0.0 | 0.0 | |
| Median (range) | −0.1 (−2.0-1.6) | 0.0 (−2.4-2.0) | 0.0 (−2.4-2.0) |
Abbreviations: iDC, immature dendritic cell ; mTIL, molecular tumor infiltrating lymphocyte; NCCTG, North Central Cancer Treatment Group; NK, natural killer; Treg, regulatory T cells
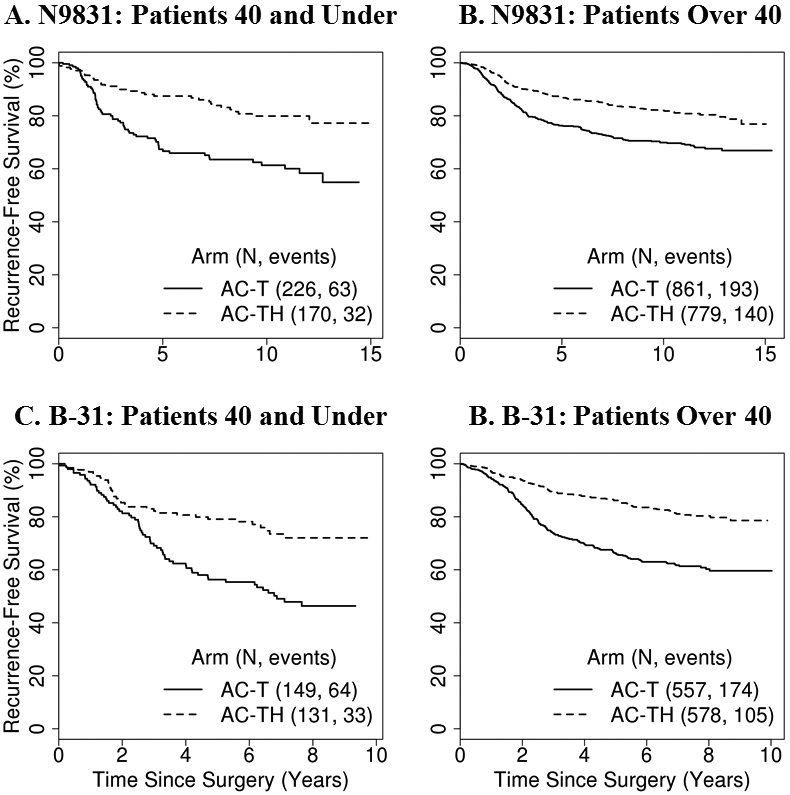
Outcomes Related to Immune Landscape and Age
Patient outcomes related to sTIL and age were further evaluated in the 831-patient cohort with available sTIL data in the NCCTG N9831 trial. In patients with LPBC who received AC-T, there was statistically significant improvement in RFS (HR, 0.18; 95% CI, 0.05–0.7; P=.01; Figure 4A) in patients older than 40 compared to younger than 40. The older patients in this group had excellent outcomes, with 95% remaining recurrence-free at 15 years, despite not receiving adjuvant trastuzumab. However, younger patients had poor RFS when receiving AC-T, regardless of LPBC status. In contrast, among patients who received AC-TH, there was no significant difference in RFS (P=.26; Figure 4B) among younger and older patients stratified by LPBC status. Similar findings were observed using age and sTILs as continuous variables (Supplemental Table 2). In patients who received AC-T, there was no significant difference in RFS when age and sTIL were analyzed as continuous variable (HR, 1.00; 95% CI, 0.97–1.02 ; P=.74 and HR, 1.20; 95% CI, 0.75–1.92 ; P=.44, respectively). Similar findings are observed in in patients who received AC-TH (HR, 1.01; 95% CI, 0.98–1.04 ; P=.52 and HR, 1.25; 95% CI, 0.72–2.18 ; P=.43). Furthermore, the age by sTIL interaction was significant with an age dichotomization of 40 years, but was not for 50 or 60. As shown in Supplemental Figure 2 and Table 3, younger LPBC patients have significantly higher levels of genes enriched in proliferation (P=.02), but lower levels of genes enriched in chemokines related to leukocyte migration and function (P<0.001). In contrast, older patients have significantly higher levels of genes involved in immune suppression and exhaustion, including FOXP3, HAVCR2, LAG3, and ICOS.
Figure 4.
Kaplan-Meier Curves of Recurrence-Free Survival (RFS) and Overall Survival (OS) Stratified by Age ≤ 40 versus > 40 Years Old and LPBC in NCCTG N9831. A, RFS in chemotherapy alone arm. B, RFS in concurrent trastuzumab arm. C, OS in chemotherapy alone arm. D, OS in concurrent trastuzumab arm. AC-T indicates adjuvant chemotherapy followed by paclitaxel; AC-TH, adjuvant chemotherapy followed by paclitaxel with concurrent trastuzumab; LPBC, lymphocyte-predominant breast cancer; NCCTG, North Central Cancer Treatment Group; NSABP, National Surgical Adjuvant Breast and Bowel Project.
Discussion
Similar to other studies (3,4,30), our study demonstrates that breast cancers arising in younger patients have distinct characteristics and gene expression compared to older counterparts. Overall, breast cancer in younger patients is associated with more aggressive phenotypes. When combining all breast cancer subtypes, previous studies showed younger patients were more likely to have HR− disease, higher HER2 protein expression, larger tumors, pathologic grade 3, lymphovascular invasion, and lymph node involvement compared to older patients (8). In HER2-positive patients, previous HERA trial reported that younger patients are more likely to have estrogen receptor-positive and progesterone receptor-positive disease (15). However, in our study, younger age was associated with higher hormone receptor positivity compared to older age in NCCTG N9831 trial but not in NSABP B-31 trial. These findings signify the importance of evaluating biologic process related to age separately in each breast cancer subtype.
Among patients who received AC-T, our analysis in the NCCTG N9831 and NSABP B-31 trials demonstrated that younger age confers significantly poorer outcomes among patients with HR+ HER2-positive, but not HR− HER2-positive breast cancer. This is in contrast to the HERA trial report (15), which found no significant difference in disease-free survival (HR, 1.16; 95% CI, 0.89–1.51; P=.27) among patients treated with AC-T when comparing between younger and older patients. However, outcome based on hormone receptor status in the context of age was not reported. Furthermore, the median follow-up in that particular report was relatively short, with only 2 years of median follow-up. Nevertheless, the poor outcomes associated with younger age were not observed among patients who received AC-TH. This finding is similar to the HERA trial report, which also showed no significant difference in disease-free survival among patients treated with AC-TH (HR, 1.18; 95% CI, 0.87–1.61, P=.30) (15). To our knowledge, our analysis represents the first study to demonstrate that trastuzumab may mitigate the poor prognosis associated with younger age in patients with early stage HER2+ breast cancer as age was not significantly associated with poor outcome in our combined analysis in patients treated with adjuvant trastuzumab-based chemotherapy. Nevertheless, among patients received trastuzumab in the NSABP B-31 trial, there was numerically more number of older patients without recurrence compared to younger patients (80.3% vs. 72%, respectively). Given the fact that patients in the NSABP B-31 had higher risk disease with more lymph node involvement than patients in the NCCTG N9831, it is possible that the detrimental effect of age may exist in patients with higher risk disease. In addition, our study also shows the difference in outcomes among HR+ versus HR− within HER2-positive disease based on age. However, beneficial effects of trastuzumab on age persist, regardless of hormone receptor status.
One potential explanation for the poorer outcome observed only in younger patients with HR+ HER2+ breast cancer but not HR− HER2-positive breast cancer may be due to the type of adjuvant endocrine therapy used in these trials. The accrual period of our two trials preceded the information from the SOFT and TEXT trials (31), which demonstrated superiority of ovarian suppression in combination with tamoxifen or aromatase inhibitor in premenopausal patient with HR+ disease. The majority of younger premenopausal patients in our two trials were mainly treated with adjuvant tamoxifen and older postmenopausal patients were treated with adjuvant aromatase inhibitors. Giving the fact that aromatase inhibitor confers approximately 30% improvement in the outcome compared to tamoxifen (32), this may explain the poorer outcome observed in younger patients only in the HR+ HER2+ subset.
Using gene set enrichment analysis, a previous large-scale genomic study demonstrated that distinct gene sets that are different in younger patients involve immune function, hypoxia, BRCA1, stem cells, apoptosis, histone deacetylase, and multiple other oncogenic signaling pathways, including MYC, E2F, RAS, and mammalian target of rapamycin (4). While this previous study showed that immune function genes are among the gene sets distinctly different with age, the actual difference in immune-related genes in tumors arising in younger versus older patients remains largely unknown. In general, aging of the immune system is associated with a decline in both humoral and cellular adaptive immune response. This process is termed immune senescence (33). Due to involution of the thymic gland with aging, the number and portion of naïve T cells considerably decrease with aging process (34). Furthermore, there is an increase in the proportion of memory T cells, which may cause defects in cytokine production (35) and accumulation of terminally differentiated T cells that are dysfunctional and have limited T-cell receptor repertoire diversity (36). Nevertheless, the immune landscape of younger versus older patients with breast cancer, specifically with HER2-positive subtype, is not defined. In contrast to a decline in the immune response expected from immune senescence, we observed no statistically significant difference in the amount of sTIL measured by pathologic quantification. However, with more in-depth analysis using gene expression signatures, there were small, but significant increases in mTIL signatures for total lymphocytes, cytotoxic cells, macrophages, neutrophils, NK CD56dim cells, and total T cells. Older patients appeared to have slight increases in exhausted CD8 T cells and regulatory T cells, but there was no statistically significant difference in B cells, CD8 T cells, and iDC.
In our analysis, older patients with LPBC appeared to have excellent outcomes with AC-T, despite not receiving trastuzumab. However, the number of older patients with LPBC was too small with only 55 patients receiving AC-T and 49 patients receiving AC-TH. Therefore, definitive conclusion about the added benefit of trastuzumab cannot be determined. When comparing gene expression among younger and older patients with LPBC, it appears younger patients have lower levels of chemokines critical for immune function. By contrast, older patients appear to have more immune suppression and exhaustion. These findings highlight that immune escape mechanisms may differ between younger and older patients. Therefore, different treatment strategies may be needed to modulate immune response to improve outcomes in these 2 distinct groups of patients.
However, our study has several limitations. One of the limitations is the lack of predetermined statistical analysis plan to evaluate specific association between age and outcome in both of the trials. Furthermore, the data of sTIL and gene expression analysis of immune-related genes were not available in both trials. Currently, the data of sTIL and gene expression analysis of immune-related gene were only available in the NCCTG-N9831 trial and not the NSABP B-31 trial. Therefore, we were unable to further validate these findings from the NCCTG-N9831 trial in the NSABP B-31 trial. Therefore, the results of this analysis should be viewed as hypothesis generation.
Supplementary Material
Supplemental Figure 1: Consort Diagram. A, NCCTG N9831 trial; B, NSABP B-31 trial.
Supplemental Figure 2. A, Genes significantly decreased in LPBC patients ≤ 40 years of age compared to > 40 years old. B, Genes significantly increased in LPBC patients > 40 years of age compared to ≤ 40 years old. FC, fold change; LPBC, lymphocyte-predominant breast cancer.
Statement of Translational relevance.
Conventionally, young age has been previously shown to be an independent predictor of poor outcome in patients with breast cancer. However, our study suggests that trastuzumab-based adjuvant chemotherapy can negate the poor prognosis associated with young age in patients with HER2-positive breast cancer.
However, among patients who received chemotherapy alone, younger age was associated with poor outcome in the hormone receptor-positive subset, but not the hormone receptor-negative subset.
In contrast to a decline in the immune response expected from immune senescence with aging process, a small, but significant increase in mTIL CD45 and some immune subset signatures were observed. Our study highlights that immune escape mechanisms may differ between younger and older patients, with younger patients having lower levels of chemokines critical for immune function and older patients having more immune suppression and exhaustion.
Acknowledgments
Support: Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Numbers U10CA180821 and U10CA180882 (to the Alliance for Clinical Trials in Oncology); U10CA180868 (NCTN), UG1CA189867 (NRG NCORP), U10CA180822 (NRG Oncology SDMC [Biostats]), U24CA196067 (BSB) (Lab) (NRG); and U24CA196171. Also supported in part by funds from the Breast Cancer Research Foundation (BCRF-17–161), Bankhead-Coley Research Program (6BC05), the DONNA Foundation, and the Pennsylvania Department of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Presented at American Society of Clinical Oncology Annual Meeting 2017
Conflict of interest: There is no relevant conflict of interest for Dr. Chumsri, Mr. Serie, Drs. Pogue-Geile, Soyano-Muller, Lou, Colon-Otero, Knutson, Moreno-Aspitia, and Thompson. Dr. Perez worked at Genentech, Inc. Mr. Mashadi-Hossein and Dr. Warren worked at NanoString Technologies, Inc.
NRG LAB Disclaimer: "Under a grant from the Pennsylvania Department of Health. The Department specifically disclaims responsibility for any analysis, interpretations, or conclusions."
ClinicalTrials.gov Identifiers: NCT00005970 (NCCTG N9831) and NCT00004067 (NSABP B-31)
References
- 1.2015 April 7, 2017. American Cancer Society. Breast Cancer Facts & Figures 2015–2016. American Cancer Society, Inc <https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2015-2016.pdf>. April 7, 2017.
- 2.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin 2010;60(5):277–300 doi 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 3.Anders CK, Johnson R, Litton J, Phillips M, Bleyer A. Breast cancer before age 40 years. Semin Oncol 2009;36(3):237–49 doi 10.1053/j.seminoncol.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anders CK, Hsu DS, Broadwater G, Acharya CR, Foekens JA, Zhang Y, et al. Young age at diagnosis correlates with worse prognosis and defines a subset of breast cancers with shared patterns of gene expression. J Clin Oncol 2008;26(20):3324–30 doi 10.1200/JCO.2007.14.2471. [DOI] [PubMed] [Google Scholar]
- 5.Albain KS, Allred DC, Clark GM. Breast cancer outcome and predictors of outcome: are there age differentials? J Natl Cancer Inst Monogr 1994(16):35–42. [PubMed] [Google Scholar]
- 6.de la Rochefordiere A, Asselain B, Campana F, Scholl SM, Fenton J, Vilcoq JR, et al. Age as prognostic factor in premenopausal breast carcinoma. Lancet 1993;341(8852):1039–43. [DOI] [PubMed] [Google Scholar]
- 7.Nixon AJ, Neuberg D, Hayes DF, Gelman R, Connolly JL, Schnitt S, et al. Relationship of patient age to pathologic features of the tumor and prognosis for patients with stage I or II breast cancer. J Clin Oncol 1994;12(5):888–94 doi 10.1200/JCO.1994.12.5.888. [DOI] [PubMed] [Google Scholar]
- 8.Colleoni M, Rotmensz N, Robertson C, Orlando L, Viale G, Renne G, et al. Very young women (<35 years) with operable breast cancer: features of disease at presentation. Ann Oncol 2002;13(2):273–9. [DOI] [PubMed] [Google Scholar]
- 9.Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 1987;235(4785):177–82. [DOI] [PubMed] [Google Scholar]
- 10.Owens MA, Horten BC, Da Silva MM. HER2 amplification ratios by fluorescence in situ hybridization and correlation with immunohistochemistry in a cohort of 6556 breast cancer tissues. Clin Breast Cancer 2004;5(1):63–9. [DOI] [PubMed] [Google Scholar]
- 11.Dawood S, Broglio K, Buzdar AU, Hortobagyi GN, Giordano SH. Prognosis of women with metastatic breast cancer by HER2 status and trastuzumab treatment: an institutional-based review. J Clin Oncol 2010;28(1):92–8 doi 10.1200/JCO.2008.19.9844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arteaga CL, Sliwkowski MX, Osborne CK, Perez EA, Puglisi F, Gianni L. Treatment of HER2-positive breast cancer: current status and future perspectives. Nat Rev Clin Oncol 2011;9(1):16–32 doi 10.1038/nrclinonc.2011.177. [DOI] [PubMed] [Google Scholar]
- 13.Scott AM, Wolchok JD, Old LJ. Antibody therapy of cancer. Nat Rev Cancer 2012;12(4):278–87 doi 10.1038/nrc3236. [DOI] [PubMed] [Google Scholar]
- 14.Clynes RA, Towers TL, Presta LG, Ravetch JV. Inhibitory Fc receptors modulate in vivo cytotoxicity against tumor targets. Nat Med 2000;6(4):443–6 doi 10.1038/74704. [DOI] [PubMed] [Google Scholar]
- 15.Partridge AH, Gelber S, Piccart-Gebhart MJ, Focant F, Scullion M, Holmes E, et al. Effect of age on breast cancer outcomes in women with human epidermal growth factor receptor 2-positive breast cancer: results from a herceptin adjuvant trial. J Clin Oncol 2013;31(21):2692–8 doi 10.1200/JCO.2012.44.1956. [DOI] [PubMed] [Google Scholar]
- 16.Romond EH, Perez EA, Bryant J, Suman VJ, Geyer CE Jr., Davidson NE, et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med 2005;353(16):1673–84 doi 10.1056/NEJMoa052122. [DOI] [PubMed] [Google Scholar]
- 17.Perez EA, Suman VJ, Davidson NE, Gralow JR, Kaufman PA, Visscher DW, et al. Sequential versus concurrent trastuzumab in adjuvant chemotherapy for breast cancer. J Clin Oncol 2011;29(34):4491–7 doi 10.1200/JCO.2011.36.7045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perez EA, Romond EH, Suman VJ, Jeong JH, Davidson NE, Geyer CE Jr., et al. Four-year follow-up of trastuzumab plus adjuvant chemotherapy for operable human epidermal growth factor receptor 2-positive breast cancer: joint analysis of data from NCCTG N9831 and NSABP B-31. J Clin Oncol 2011;29(25):3366–73 doi 10.1200/JCO.2011.35.0868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perez EA, Romond EH, Suman VJ, Jeong JH, Sledge G, Geyer CE Jr., et al. Trastuzumab plus adjuvant chemotherapy for human epidermal growth factor receptor 2-positive breast cancer: planned joint analysis of overall survival from NSABP B-31 and NCCTG N9831. J Clin Oncol 2014;32(33):3744–52 doi 10.1200/JCO.2014.55.5730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perez EA, Ballman KV, Tenner KS, Thompson EA, Badve SS, Bailey H, et al. Association of Stromal Tumor-Infiltrating Lymphocytes With Recurrence-Free Survival in the N9831 Adjuvant Trial in Patients With Early-Stage HER2-Positive Breast Cancer. JAMA Oncol 2016;2(1):56–64 doi 10.1001/jamaoncol.2015.3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Loi S, Sirtaine N, Piette F, Salgado R, Viale G, Van Eenoo F, et al. Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02–98. J Clin Oncol 2013;31(7):860–7 doi 10.1200/JCO.2011.41.0902. [DOI] [PubMed] [Google Scholar]
- 22.Denkert C, Loibl S, Noske A, Roller M, Muller BM, Komor M, et al. Tumor-associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. J Clin Oncol 2010;28(1):105–13 doi 10.1200/JCO.2009.23.7370. [DOI] [PubMed] [Google Scholar]
- 23.Adams S, Gray RJ, Demaria S, Goldstein L, Perez EA, Shulman LN, et al. Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J Clin Oncol 2014;32(27):2959–66 doi 10.1200/JCO.2013.55.0491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol 2015;26(2):259–71 doi 10.1093/annonc/mdu450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Loi S, Michiels S, Salgado R, Sirtaine N, Jose V, Fumagalli D, et al. Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trial. Ann Oncol 2014;25(8):1544–50 doi 10.1093/annonc/mdu112. [DOI] [PubMed] [Google Scholar]
- 26.Waggott D, Chu K, Yin S, Wouters BG, Liu FF, Boutros PC. NanoStringNorm: an extensible R package for the pre-processing of NanoString mRNA and miRNA data. Bioinformatics 2012;28(11):1546–8 doi 10.1093/bioinformatics/bts188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Danaher P, Warren S, Dennis L, D’Amico L, White A, Disis ML, et al. Gene expression markers of Tumor Infiltrating Leukocytes. J Immunother Cancer 2017;5:18 doi 10.1186/s40425-017-0215-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang HY, Ma D, Liu YR, Hu X, Zhang J, Wang ZH, et al. Impact of hormone receptor status and distant recurrence-free interval on survival benefits from trastuzumab in HER2-positive metastatic breast cancer. Sci Rep 2017;7(1):1134 doi 10.1038/s41598-017-00663-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barton MK. Hormone receptor status affects locoregional control in HER2-positive breast cancer treated with trastuzumab. CA Cancer J Clin 2012;62(5):281–2 doi 10.3322/caac.21152. [DOI] [PubMed] [Google Scholar]
- 30.Johnson RH, Hu P, Fan C, Anders CK. Gene expression in “young adult type” breast cancer: a retrospective analysis. Oncotarget 2015;6(15):13688–702 doi 10.18632/oncotarget.4051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Francis PA, Pagani O, Fleming GF, Walley BA, Colleoni M, Lang I, et al. Tailoring Adjuvant Endocrine Therapy for Premenopausal Breast Cancer. N Engl J Med 2018;379(2):122–37 doi 10.1056/NEJMoa1803164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Early Breast Cancer Trialists’ Collaborative G. Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet 2015;386(10001):1341–52 doi 10.1016/S0140-6736(15)61074-1. [DOI] [PubMed] [Google Scholar]
- 33.Foster AD, Sivarapatna A, Gress RE. The aging immune system and its relationship with cancer. Aging health 2011;7(5):707–18 doi 10.2217/ahe.11.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haynes BF, Markert ML, Sempowski GD, Patel DD, Hale LP. The role of the thymus in immune reconstitution in aging, bone marrow transplantation, and HIV-1 infection. Annu Rev Immunol 2000;18:529–60 doi 10.1146/annurev.immunol.18.1.529. [DOI] [PubMed] [Google Scholar]
- 35.Hakim FT, Flomerfelt FA, Boyiadzis M, Gress RE. Aging, immunity and cancer. Curr Opin Immunol 2004;16(2):151–6 doi 10.1016/j.coi.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 36.Ivory K, Martin R, Hughes DA. Significant presence of terminally differentiated T cells and altered NF-kappaB and I-kappaBalpha interactions in healthy ageing. Exp Gerontol 2004;39(4):567–76 doi 10.1016/j.exger.2003.09.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1: Consort Diagram. A, NCCTG N9831 trial; B, NSABP B-31 trial.
Supplemental Figure 2. A, Genes significantly decreased in LPBC patients ≤ 40 years of age compared to > 40 years old. B, Genes significantly increased in LPBC patients > 40 years of age compared to ≤ 40 years old. FC, fold change; LPBC, lymphocyte-predominant breast cancer.