Abstract
Background:
Due to demographic changes the world's population is progressively ageing. The physiological decay of the elderly adult may lead to a reduction in the ability to balance and an increased risk of falls becoming an important issue among the elderly. In order to counteract the decay in the ability to balance, physical activity has been proven to be effective. The aim of this study is to systematically review the scientific literature in order to identify physical activity programs able to increase balance in the elderly.
Methods:
This review is based on the data from Medline-NLM, Pubmed, ScienceDirect, and SPORTDiscuss and includes randomized control trials that have analyzed balance and physical activity in healthy elderly over 65 years of age during the last decade. A final number of 8 manuscripts were included in the qualitative synthesis, which comprised 200 elderly with a mean age of 75.1 ± 4.4 years. The sample size of the studies varied from 9 to 61 and the intervention periods from 8 to 32 weeks.
Results:
Eight articles were considered eligible and included in the quantitative synthesis. The articles investigated the effects of resistance and aerobic exercise, balance training, T-bow© and wobble board training, aerobic step and stability ball training, adapted physical activity and Wii Fit training on balance outcomes. Balance measures of the studies showed improvements between 16% and 42% compared to baseline assessments.
Conclusions:
Balance is a multifactorial quality that can be effectively increased by different exercise training means. It is fundamental to promote physical activity in the aging adult, being that a negative effect on balance performance has been seen in the no-intervention control groups.
Keywords: balance, balance training, elderly, risk of falling, strength
1. Introduction
The age distribution of the world's population stands in a constant change. An increase in the number of elderly people and a simultaneous decline in the number of younger people is a trending factor worldwide.[1] Since the natural process of aging is defined as continuous and irreversible, a high life expectancy does not only entail advantages. Aging is associated with a reduction in both physical and cognitive functions of the human body, which also involves the likeliness in the occurrence of age-related diseases.[2] Reduction in muscle strength and coordination of the lower extremities accompanied by decreased gait assurance and balance control are the result of a physical deterioration in an older body.[3,4] Together with decreased cognitive functions, these impairments lead to a higher risk of falling among the elderly.[5,6] Over 30% of people aged 65 or older, which is conventionally the chronological age that defines a person to be elderly,[7] experience on average 1 fall a year.[8] In order to prevent further consequences of such events, it is crucial to reduce the risk of falling among this population. Inactivity is meant to be a factor that accelerates the decrease of bodily functions[9] with a negative impact on balance control.[10,11] Physical activity has been therefore proven to counteract this phenomenon.[12] There is however still uncertainty in which type of exercise may be the most effective to this purpose.[13,14] Higher levels of physical activity reduce the overall morbidity and mortality and the risk of falling between 30% and 50%.[15–18] Especially leg strength training and balance training have been identified as eligible methods to reduce the risk of falls. However, balance is the foundation of the ability to stand upright and move along, therefore balance training should also have an important role in fall prevention.[19] It has been also proven that seniors with deteriorated balance are more likely to experience a fall than seniors with unimpaired postural control, which underlines the importance of balance training among the elderly.[20] Almost all studies which investigate the risk of falling among elderly conclude that physical activity, even leisure exercises, are effective methods in order to maintain an intact balance control and prevent falls.[2,8,21] Various studies have examined different kinds of exercise, from Pilates, stair climbing, vibration training to dancing.[17,22–27] These have all found significant improvements in the ability to balance and provide evidence that physical activity can reduce the risk of falling. As most of them address only 1 specific kind of exercise or 1 kind of balance (either static, dynamic or intended as postural control), it is unsure which form of physical activity can provide the most beneficial effect. Therefore, the aim of this systematic review was to analyze different typologies of exercise directed to increase static balance in elderly adults and try to understand which of them is able to effectively promote such ability and may be of support in order to prevent the risk of falling.
2. Materials and methods
2.1. Research strategy
The PRISMA guidelines for conducting a systematic review were adopted.[28] This systematic review examines the effects of different typologies of physical exercise programs on static balance in elderly people. The literature search was considered in line with ethical principles for medical research involving human subjects. No approval was needed for the present review. The inclusion criteria comprised articles in English language, which were published within the last decade. All articles had to analyze the effects of physical activity on balance on samples of elderly, aging at least 65 or older. Participants had to be healthy without any disabling, physical, neurological, or mental disease and were excluded whether living in a nursing home. Both genders were considered. In order to find articles that met all criteria the following keywords were used in different combinations: balance, exercise, elderly, training. Research was conducted in the following electronic databases: Medline-NLM, Pubmed, Science Direct, and SPORTDiscuss. All the retrieved articles were transferred into the Endnote software (Vers. X6 for Windows 7, © Thomson Reuters).
2.2. Study selection
The first range of articles was selected by title screening of the manuscripts. In this phase, articles matching the search terms and inclusion criteria were collected. Out of this first selection, the abstracts of the papers were read, followed by excluding those that did not meet the inclusion criteria. After duplicate removal, we proceeded with a qualitative synthesis of the full texts of the studies included. Two independent investigators conducted the literature search and performed the synthesis as follows: Study design; Sample (n); Intervention; and main results. The 2 independent investigators, in case of disagreements, resolved article inclusion by negotiation. Finally, full texts were read and a decision upon included articles was made. The included studies were all randomized controlled trials.
2.3. Statistical analysis
In the qualitative synthesis, the comparison of the intervention effect between the exercise and control groups was analyzed for each manuscript according to post-intervention data, or where accessible, the rate of pre-post improvement (i.e., mean differences or percentage change, %Δ). Subsequently, 95% confidence intervals (CIs) were calculated in order to increase homogeneity for the quantitative synthesis. The effect of the balance interventions was interpreted based on standardized mean differences and statistical significance between the exercise intervention group and the control group.
3. Results
A total of 1305 records have been identified through the preliminary database search. One hundred twelve studies were selected through title screening and 64 of these records were excluded after abstract analysis. Of the 48 records remaining, which the full texts were analyzed, 26 were excluded for not complying to the inclusion criteria. Twenty-two studies were considered potentially relevant and compliant with all the inclusion criteria. Subsequent to the retrieval of the %Δ between pre and post-intervention, calculated on the experimental group, 95% CIs were calculated for the articles included in the qualitative synthesis (C.I. based on the balance improvement after the interventions: CI lower 15.71 – CI upper 43.01) and based on such criteria a total of 8 studies were finally included in the quantitative synthesis. Figure 1 shows the selection process of the studies in detail.
Figure 1.
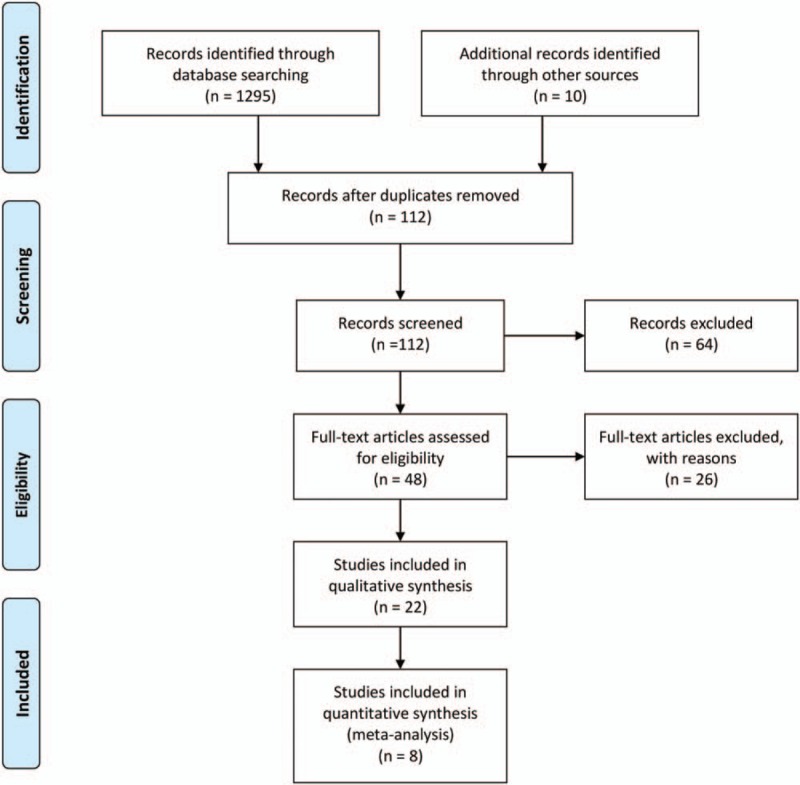
Preferred Reporting Items for Review and Meta-Analyses (PRISMA) flow diagram illustrating the different phases of study inclusion.
A total number of 200 elderly subjects were analyzed across the studies, with a mean age of 75.1 ± 4.4 years. The sample size of the studies varied from 9 to 61 and the intervention periods from 8 to 32 weeks. All 8 studies investigated the effects of different kinds of physical exercise on balance together with other variables. The following typologies of exercises were analyzed: resistance and aerobic exercise,[29,30] balance training,[31,32] T-bow© and wobble board training,[33,34] aerobic step and stability ball training,[35] and adapted physical activity and Wii Fit training.[36] The descriptive characteristics of the retrieved studies are shown in Table 1.
Table 1.
Characteristics of studies included in the quantitative synthesis.
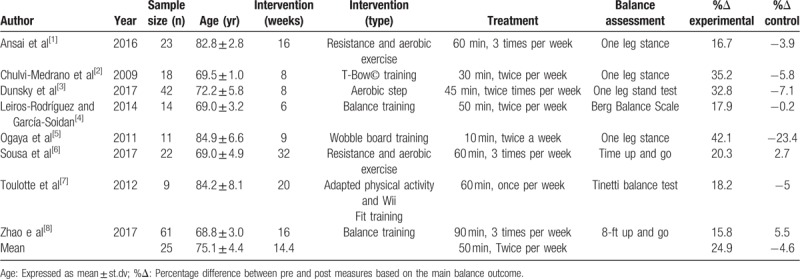
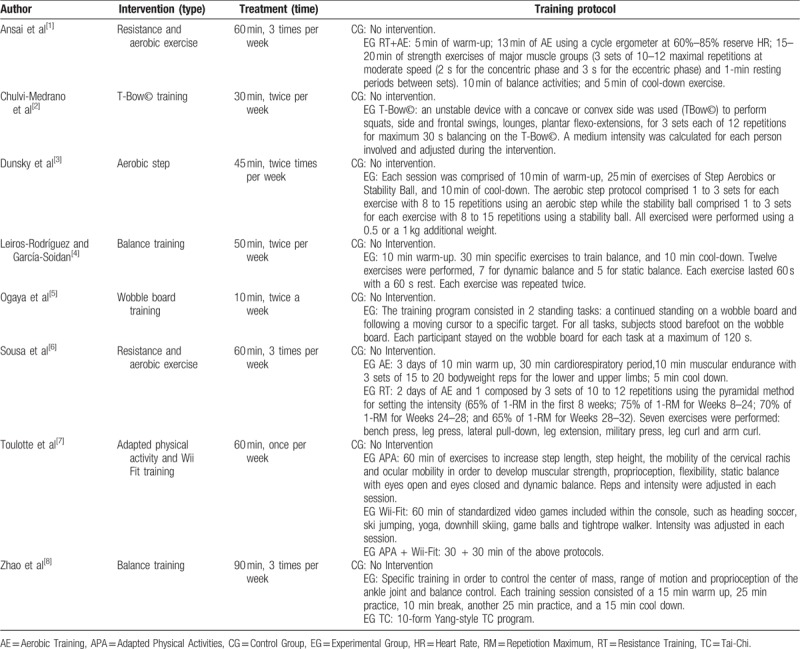
All analyzed studies exhibited improvements in the balance measures between pre and post intervention. The exercise protocol of each intervention is summarized in Table 2. The following section provides an overview of all studies followed by the main results.
Table 2.
Description of the training protocols.
3.1. Resistance and aerobic exercise
Two of the retrieved records used resistance exercise as a form of exercise to increase balance in the elderly.[29,30] The study of Ansai et al[29] used a randomized, 3-arm controlled trial, in which a group of elderly performed a multicomponent exercise intervention which comprised a combination of aerobic and resistance exercise, another group performed a resistance exercise protocol and a control group which received no-intervention. The resistance exercise group carried out 3 sets of 10 to 12 maximal repetitions at moderate speed with a 1 minute rest between each set, with exercises for both upper and lower limbs. The aerobic component in the combined group consisted in 13 minutes on a cycle ergometer at an intensity of 60% to 85% of reserve heart rate (the protocol consisted of intensity increases and decreases every 3 minutes), adjusted for age and gender. The balance measure taken into account was the one leg stance, measured in seconds. The results indicated that after a 16 week intervention period both the multicomponent (pre 7.1 ± 8.6 s, post 11.1 ± 11.7 s) and resistance exercise intervention (pre 6.0 ± 6.7 s, post 6.7 ± 7.4 s) increased the balance measures compared to the control group which instead showed a decrease (pre 5.1 ± 6.5 s, post 5.5 ± 5.9 s). Also, the number of reported falls measured by the authors decreased after the intervention period (Multicomponent pre 10, post 2, Resistance exercise pre 7, post 1, control pre 8, post 5). It has to be noted that the multicomponent exercise intervention showed greater results compared to the resistance exercise protocol alone.
Similar research design has been carried out by Sousa et al,[30] where aerobic exercise alone has been compared to a combined aerobic and resistance exercise protocol to a control group in order to improve risk factors for fall preventions in the elderly. The combined exercise comprised an aerobic session once a week and a resistance exercise session once a week. The resistance training comprised 3 sets of 10 to 12 repetitions using a pyramidal method with increasing intensity from the first to the eighth training week. As in the study of Ansai et al, the exercises targeted both the upper and lower limbs. The aerobic component was composed of a 30 min brisk walking protocol. The time up and go test was used to assess balance performance. The results reported that both the aerobic and the combined intervention showed positive increases in the balance measures with a greater magnitude in the combined exercise program (Aerobic pre 7.7 ± 1.1, post 7.0 ± 0.8; Combined pre 7.4 ± 1.0, post 5.9 ± 0.7). The control group showed a mild decrease in the functional measures (pre 7.5 ± 0.7, post 7.7 ± 1.3).
3.2. Balance training
Two of the retrieved records used balance protocols[31,32] to increase balance and reduce the fall rate in the elderly. The study of Leiros-Rodríguez and García-Soidan was a randomized control trial with an experimental group of 14 elderly women. The experimental group underwent a balance exercise intervention twice a week for 50 minutes for each session in which each participant performed 12 specific balance exercises simulating movements that the participants found instable in ordinary life tasks. The exercises were specific for static and dynamic balance. Each exercise lasted 60 seconds with a 60 second rest between each exercise and it was then repeated twice. When the tasks were deemed not demanding the investigators modified the size and characteristics of the support base surface of the elderly participants. The balance assessment was performed with the Berg Balance scale. At the end of the 6-week intervention, the experimental group increased the balance measure (Pre 45.86 ± 2.91; Post 54.07 ± 1.98), whereas a decrease was observed in the control group (Pre 47.79 ± 3.38; Post 47.71 ± 2.89).
Zhao et al[32] evaluated the effects of a specific balance protocol compared to a tai-chi intervention and a no-intervention group on balance measures. The experimental group underwent specific training in order to control the center of mass, range of motion and proprioception of the ankle joint and balance control. The tai-chi group performed a 10 form-yang-style tai-chi program, whereas the control group received no treatment. The chair stand test was used to assess balance and this was a component of the fall risk test to evaluate the risk of falling. An increase of 15.8% and 15.2% was achieved after the intervention in the balance measure in the experimental group and tai-chi group, respectively. An increase of around 5% was also achieved by the control group. There were no significant differences between the 2 groups regarding the balance measure. It is noteworthy that the experimental group also increased aerobic capacity, which was not achieved neither in the tai- chi nor the control group. Nevertheless, aerobic capacity is not a variable that has been considered in this review.
3.3. T-Bow© and wobble board training
Other 2 studies applied a form of specific balance training, T-bow© and wobble board training,[33,34] and for this reason these have been classified outside of the more generic “balance training” protocols. The study of Chulvi-Medrano et al[33] applied a t-bow balance intervention on 10 elderly people and compared the results with a control group that did not follow any intervention. The T-bow is a concave board that can be positioned on the floor in a concave or convex position. When the convex side is facing downwards the T-bow will be unstable either laterally or in an anterior-posterior direction. The training program consisted of 5 exercises using the T-Bow©. These were mainly resistance exercises of the lower limbs. The intensity of these exercises was controlled by exposure time and by modifying the support base. Balance exercise intensity was implemented by the time of stance, while balancing on the T-bow. The exercise protocol consisted of 1 to 3 sets of 12 repetitions each. The protocol was implemented for 2 weekly 30-minute sessions, over a period of 8 weeks. The one leg stance was used to assess balance. The results of Chulvi-Medrano et al's study reported an increase of 35.2% in the time balancing in the one leg stance in the exercise group and a decrease of 5.8% in the control group, when compared to the baseline assessments. The second analyzed study, published by Ogaya et al[34] used a wobble board for balance exercise 9 weeks twice a week. The results of such intervention were then compared to a control group that did not receive any intervention. The wobble board used for the intervention was an unstable surface composed by a flat balancing surface with a semi sphere positioned underneath and at the center of the balancing surface. The balance training was performed 10 minutes for each training session. The training program consisted of the following 2 standing tasks:
-
(1)
a continued standing on the wobble board (static balance) and
-
(2)
following a moving cursor on a screen, positioned in front of the participant, to a specific target (dynamic balance).
The one leg stance was used to assess balance. The results indicate that training on a wobble board is able to increase the one leg standing task for a mean 42.1%, whereas the control group decreased the balancing performance by approximately 23%. Both the increase of the experimental group and the decrease exhibited by the control group in Ogaya et al study[34] was the greatest amongst all the analyzed studies. It is however important to note that the cohort analyzed was that presenting the greatest mean age.
3.4. Aerobic step and stability ball
The only retrieved record evaluating aerobic step as a form of intervention to increase balance in the elderly is that of Dunsky et al.[35] The authors implemented 2 protocols compared to a control group. The first using an aerobic step and the second using a stability ball. Both protocols were developed over a 45 minute session, twice a week for 8 consecutive weeks. The aerobic step protocol comprised 1 to 3 sets for each exercise with 8 to 15 repetitions per exercise of slow to medium speed performances using an aerobic step. The exercises were stepping on or over the step, walking around the step, with or without an overload ranging between 0.5 and 1 kg using or not using music to gain a rhythmic movement. The stability ball exercises comprised 1 to 3 sets for each exercise with 8 to 15 repetitions per exercise of slow to medium speed performances using a stability ball. The exercises were resistance exercises against body weight with the addition of a soft ball or a medicine ball of 0.5 or 1 kg. Such interventions might be considered as a form of combined aerobic and resistance exercise. The one leg stance was used to evaluate balance performance. The results of the study indicated that aerobic step was able to increase the one leg stand to a greater extent compared to the stability ball protocol (Aerobic step pre 13.1 ± 10.4 s, post 17.4 ± 11.9 s; Stability ball pre 14.6 ± 9.2 s, post 15.9 ± 11.6 s). Interestingly also in the study of Dunsky et al,[35] the control group presented a decrease of the balance measures (pre 22.9 ± 12.1 s, post 23.0 ± 11.6 s).
It is important to note that also in the above-mentioned protocols (Resistance and Aerobic Exercise and Balance Training) those which showed greater effects were those combining aerobic and anaerobic training, as the aerobic step activity in which anaerobic exercises were used in an aerobic manner.
3.5. Adapted physical activity and Wii Fit training
The only retrieved record evaluating adapted physical activity is that of Toulotte et al.[36] The authors had as main aim to compare adapted physical activity to a Wii Fit training. The study design comprised 4 groups:
-
(1)
An adapted physical activity group,
-
(2)
a Wii Fit training group,
-
(3)
a combined intervention group and
-
(4)
a no-intervention control group.
All participants exercised once a week for 60 minutes for 20 consecutive weeks. The adapted physical intervention consisted of exercises in which the participants were asked to increase the step length, step height, the mobility of the cervical rachis, and ocular mobility in order to develop muscular strength, proprioception, flexibility, static balance with eyes open and eyes closed and dynamic balance. The difficulty increased each training week by implementing the number of repetitions and the tasks required. The Wii Fit training consisted of standardized video games included with this console, such as heading soccer, ski jumping, yoga, downhill skiing, game balls, and tightrope walker. Each participant underwent the difficulty level that best fitted his abilities. The combined group underwent both the above-mentioned interventions with lower repetitions compared to the 2 single interventions alone and the control group underwent no physical activity intervention. Each participant was evaluated through the Tinetti test, the unipedal test, and the Wii Fit test. The results showed for group 1 and 3 that balance increased significantly: The Tinetti test decreased of 13% and 12%, respectively, in static (15%) and dynamic conditions (16%). The unipedal test reported a decreased number of balance losses (Group 1 pre 20, post 8; Group 3 pre 22, post 14) and Wii Fit test an improvement of 44%. The results for the group which underwent the Wii Fit training alone showed an improvement only in the Tinetti test with a reduction of 13% only in the static but not in the dynamic conditions. No significant improvement in the unipedal test and an increase of the measure in the Wii Fit test by 61%.
A decrease in balance of 5% was shown in the control group regarding the Tinetti balance test.
4. Discussion
The aim of this systematic review was to analyze different typologies of exercise aimed at increasing static balance in elderly adults. Of the analyzed studies, all showed improvements in the ability to balance after the intervention period. Resistance and aerobic exercise,[29,30] balance training,[31,32] T-bow© and wobble board training,[33,34] aerobic step and stability ball,[35] and adapted physical activity and Wii Fit training[36] all seem to be effective exercise programs able to increase the ability to balance in the elderly.
Different studies have linked an increase in muscle strength to an increase in the ability to balance in elderly,[37–39] this due to the intrinsic factors associated to ageing, such as degenerative processes in the nervous and muscular system that lead to muscle weakness and gait instability.[40] Such assumptions have in part been confirmed, Lacroix et al, for example, has proposed a 6 week resistance exercise protocol in healthy older adults, applied in a supervised and non-supervised manner and found that both protocols were able to increase balance (a 68% increase was noted in the supervised protocol compared to the baseline measure), measured through a modified Romberg balance test. It is however interesting to note that the supervised group increased balance to a greater extent than the non-supervised group, underlining that individual cognitive factors might also play a role as a form of motivation for the elderly experiencing the resistance exercise program and that the supervision might help the elderly to perform the exercises at a higher quality. Other study proposed by Marques et al in 2017 has provided both resistance and aerobic exercise to 2 groups of elderly, and found that after the 32 weeks intervention both groups increased their ability to balance. The resistance exercise group increased by 25% the ability to balance during the one leg stance compared to baseline, while the aerobic group increased the balance measure around 31% compared to baseline. Both the studies of Lacroix and Marques reported a decrease of the balance measures in their control groups by 21.9% and 14.9%, respectively. As above reported for other studies, also Marques et al have shown that the group undergoing the aerobic exercise together with the resistance exercise, improved greatly, compared to the other groups, the ability to balance. It is not clear whether such further balance ability is linked to the aerobic capacity developed or to the means used to increase such capacity. Running or swimming, for example, might help elderly people to increase the proprioception of the ankle and knee joint and thus result in an increased ability to balance.[41]
We have also analyzed studies that implemented balance protocols without including specific resistance exercises. The study of Leiros-Rodríguez and García-Soidan[31] comprised of static and dynamic exercises performed by elderly women in a public park for 6 weeks. Similar outcomes are those of Barnett et al[42] which implemented a community-based group exercise program. The training protocol proposed included exercises designed to improve balance, coordination, and aerobic capacity. Balance and co-ordination exercises included modified Tai Chi exercises, stepping practice, change of direction, dance steps, and catching/throwing a ball. The balance of the elderly was measured through body sway and the results underline that the intervention group significantly reduced body sway, whereas the control group, which did not exercise, increased the body sway measure. Such results indicated that after the 1-year intervention proposed, the physiological decay of the elderly adults, together with physical inactivity, significantly decreased the ability to balance, whereas a physical intervention of low intensity might effectively increase balance.
Another common exercise intervention that has been found to increase balance, and which has been also used in the study of Zhao et al,[32] as a comparison intervention, is Tai-Chi training. Different systematic reviews and meta-analysis have analyzed the effects of Tai-Chi on balance in elderly populations[43–45] and all conclude that such kind of exercise if effective to increase balance and functional measures related to quality of life in the elderly, such as flexibility or strength and is also able to reduce the risk of falls.
The same trend has been shown in the study of Zhao et al, where both the Tai-Chi group and the experimental group increased their balance abilities, notwithstanding this latter improved balance to a greater extent.
The T-Bow© device and a wobble board were other 2 devices used to increase balance in the elderly. The first study using the T-Bow© device[33] is however the only 1 published that has actually investigated the effects of a training regimen on elderly to increase balance using the T-Bow© device, and for such it is not possible to compare the results of such study with any other. However, the magnitude of the results seems to be in line with the other analyzed study using an unstable surface.[34] Balancing on unstable surfaces has been seen to increase the brain activity in the supplementary motor area. The unstable activity tasks also increase the sway area in both a medio-later and anterior-posterior sway. The medio-later sway has been also seen to be negatively related to the activation of the supplementary motor area, which means that an increased sensorimotor control of the brain is related to increased balance.[46] However, when directly comparing a training which aims to increase balance through the use of unstable surfaces and resistance training, as the study of Dunsky et al,[35] in which a stability ball has been compared to an aerobic step, this latter seems to be more beneficial. Again, the increase in muscle strength, proposed in the aerobic step protocol, together with the increase in the aerobic capacity, seems to be a crucial component for balance improvement in the elderly. The studies of Chulvi-Medrano et al, Ogaya et al, and Dunsky et al all show a reduction in the balance measures of the control groups analyzed of 5.8, 23.4, and 7.1, respectively, all assessed through the one leg stance.
Toulette et al[36] was the only author to propose an adapted physical activity program compared to a Wii Fit training protocol. The adapted physical activity comprised different elements such as proprioception, muscular strength, and flexibility. Whereas the Wii Fit aimed to increase balance simulating different activities as heading soccer, ski jumping, yoga, downhill skiing, game balls, and tightrope walker. Wii Fit has been seen to only improve activities on static balance in bipedal conditions, contrary to Adapted Physical Activities.
Adapted Physical Activities training alone improves balance and adding Wii Fit does not confer a major additional benefit. Bieryla,[47] similarly to Toulette et al have instead used an Xbox Kinect training to improve clinical measures of balance in older adults. Training was individual play using the Kinect for 30 minutes, 3 times a week for 3 weeks. The training was supervised, though no physical assistance was given. Two Kinect games were used: YourShape: Fitness Evolved and Kinect adventures. After the intervention period the elderly were re-tested for 4 clinical measures of balance: Berg Balance Scale, Fullerton advanced balance scale, functional reach, and the time up and go test. Only the Berg balance scale and the Fullerton advanced balance scale showed improvements after the training period of 8.3 and 21%, respectively. The results indicate that partial increases of balance measures can be achieved through the use of an Xbox Kinect training, as above described through the use of the Wii Fit which was able to increase static but not dynamic balance. It is however unclear if such results are due to the small sample sizes of both studies or due to the restricted time spent training for both groups (10 minutes twice a week for the Wii Fit and 30 minutes 3 times a week for the Xbox Kinect training). Also, in the study undergoing the Wii Fit training, the control group which did not undergo any intervention, showed a decrease in the balance measure of 5%.
From the analyzed studies, it is unclear whether 1 specific training regimen may be more beneficial than others in order to increase balance in the elderly. However, all the no-activity groups showed a decline in function. Such crucial finding highlights the need to promote physical activity in the elderly, more than to provide a specific training regimen, not only to allow increases of balance, but also to promote diverse functional measures.[48–50] Physical inactivity has been seen to increase mortality[51] and disease in the elderly, including several forms of cancer, diabetes, hypertension, coronary, and cerebrovascular diseases and increase obesity.[52] For such reasons exercise interventions with the aim to increase strength, balance, and aerobic fitness have been also recommended by the World Health Organization (WHO). In particular, these forms of exercises have been enhanced to allow the elderly to continue with the activities of daily life and limit future medical costs. At least 150 minutes of moderate-intensity aerobic activity a week, 2 to 3 days performing muscle strengthening exercises and 3 or more days practicing balance exercises have been recommended by the WHO as minimum exercise prescription to reduce physical decline in people over 65 years of age.[53]
The analyzed studies provide evidence that a multicomponent approach with resistance training, aerobic, and proprioceptive components may be appropriate to promote balance performance and reduce the risk of falling.
Despite the significant findings, there are different characteristics that vary among the studies that do not allow a direct comparison of the retrieved results. All analyzed studies, for example, used different assessment tools for the evaluation of balance abilities. Four studies used the one leg stance to evaluate static balance, 1 the berg balance scale, 1 the tinetti balance test, 1 the time up and go test, and another 1 the 8-ft up and go. It is doubtful whether certain tests actually assessed balance properly, such as the 8-ft up and go or the time up and go test. These methods are deemed to evaluate balance but may be more selective to observe the increase in strength of the lower limbs combined with aerobic capacities.[32] No equipment was used in more than 1 study and such aspect needs to be kept in mind when comparing the outcomes. Moreover, the sample size of the examined studies varies greatly. The smallest group consisted of 9 participants, the biggest of 61. This makes it hard to represent a general community, as a sample size of 9 is rather small. Furthermore, the manuscript aimed to understand the effects of exercise on static balance in healthy elderly, and due to such specific inclusion criteria a very limited number of studies have been included in this systematic review. It has to be pointed out that different manuscripts include as elderly adults, individuals of 60 years of age, which have not been included in our manuscript. Last, the training status of the participants before the start of the interventions should have been addressed. Most studies did not assess the physical and training status that may have led to a biased conclusion.
5. Conclusion
Although the investigated studies exhibited positive effects on balance, indicating a reduction in the risk of falling, there were some aspects of the studies that do not make a comparison possible. The studies reported a concomitant increase in strength together with balance improvements. Multicomponent exercise with aerobic and anaerobic components seems to provide positive outcomes together with specific balance exercises integrated with resistance exercise means. The control groups which received no intervention, showed a decline in the ability to balance, suggesting that inactivity, more than a specific type of physical activity, plays a pivotal role in the elderly, in the mechanisms involved in maintaining balance. Regular physical activity including aerobic, anaerobic and proprioceptive components may be practiced in order to promote static balance in the elderly as a mean to reduce future risk of falling. There is however the need to compare such results with larger population studies.
Author contributions
Conceptualization: Giuseppe Battaglia, Marianna Bellafiore.
Data curation: Giuseppe Battaglia, Marianna Bellafiore.
Investigation: Ewan Thomas, Jessica Brusa.
Methodology: Ewan Thomas.
Project administration: Antonio Palma.
Resources: Vincenza Leonardi.
Supervision: Antonio Palma.
Visualization: Jessica Brusa.
Writing – original draft: Ewan Thomas, Antonino Patti.
Writing – review & editing: Ewan Thomas, Antonio Palma, Marianna Bellafiore.
Footnotes
Abbreviations: CI = confidence intervals, PRISMA = Preferred Reporting Items for Review and Meta-Analyses, WHO = World Health Organization.
The authors declare no conflict of interest.
References
- [1].Peters E, Pritzkuleit R, Beske F, et al. Demografischer Wandel und Krankheitshäufigkeiten. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz 2010;53:417–26. 10.1007/s00103-010-1050-y. [DOI] [PubMed] [Google Scholar]
- [2].Fernandez-Arguelles EL, Rodriguez-Mansilla J, Antunez LE, et al. Effects of dancing on the risk of falling related factors of healthy older adults: a systematic review. Arch Gerontol Geriatr 2015;60:1–8. 10.1016/j.archger.2014.10.003. [DOI] [PubMed] [Google Scholar]
- [3].Owino V, Yang SY, Goldspink G. Age-related loss of skeletal muscle function and the inability to express the autocrine form of insulin-like growth factor-1 (MGF) in response to mechanical overload. FEBS Lett 2001;505:259–63. [DOI] [PubMed] [Google Scholar]
- [4].Daley MJ, Spinks WL. Exercise, mobility and aging. Sports medicine 2000;29:1–2. [DOI] [PubMed] [Google Scholar]
- [5].Zecevic AA, Salmoni AW, Speechley M, et al. Defining a fall and reasons for falling: comparisons among the views of seniors, health care providers, and the research literature. Gerontologist 2006;46:367–76. DOI 10.1093/geront/46.3.367. [DOI] [PubMed] [Google Scholar]
- [6].Kendrick D, Kumar A, Carpenter H, et al. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst Rev 2014;11:CD00984810.1002/14651858.CD009848.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Orimo H, Ito H, Suzuki T, et al. Reviewing the definition of “elderly”. Geriatr Gerontol Int 2006;6:149–58. 10.1111/j.1447-0594.2006.00341.x. [Google Scholar]
- [8].Gillespie LD, Gillespie WJ, Robertson MC, et al. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev 2003;4:CD00034010.1002/14651858.CD000340. [DOI] [PubMed] [Google Scholar]
- [9].Inouye SK, Studenski S, Tinetti ME, et al. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc 2007;55:780–91. 10.1111/j.1532-5415.2007.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Woollacott M, Shumway-Cook A. Attention and the control of posture and gait: a review of an emerging area of research. Gait Posture 2002;16:1–4. [DOI] [PubMed] [Google Scholar]
- [11].Thomas E, Martines F, Bianco A, et al. Decreased postural control in people with moderate hearing loss. Medicine 2018;97:e024410.1097/MD.0000000000010244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Sherrington C, Whitney JC, Lord SR, et al. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc 2008;56:2234–43. 10.1111/j.1532-5415.2008.02014.x. [DOI] [PubMed] [Google Scholar]
- [13].Gine-Garriga M, Roque-Figuls M, Coll-Planas L, et al. Physical exercise interventions for improving performance-based measures of physical function in community-dwelling, frail older adults: a systematic review and meta-analysis. Arch Phys Med Rehabil 2014;95:753–69. e753.10.1016/j.apmr.2013.11.007. [DOI] [PubMed] [Google Scholar]
- [14].Gobbo S, Bergamin M, Sieverdes JC, et al. Effects of exercise on dual-task ability and balance in older adults: a systematic review. Arch Gerontol Geriatr 2014;58:177–87. 10.1016/j.archger.2013.10.001. [DOI] [PubMed] [Google Scholar]
- [15].Bembom O, van der Laan M, Haight T, et al. Leisure-time physical activity and all-cause mortality in an elderly cohort. Epidemiology 2009;20:424–30. 10.1097/EDE.0b013e31819e3f28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;9:CD00714610.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Bellafiore M, Battaglia G, Bianco A, et al. Improved postural control after dynamic balance training in older overweight women. Aging Clin Exp Res 2011;23:378–85. 10.3275/7354. [DOI] [PubMed] [Google Scholar]
- [18].Battaglia G, Bellafiore M, Bianco A, et al. Effects of a dynamic balance training protocol on podalic support in older women. Pilot Study. Aging Clin Exp Res 2010;22:406–11. 10.3275/6713. [DOI] [PubMed] [Google Scholar]
- [19].Melzer I, Benjuya N, Kaplanski J. Postural stability in the elderly: a comparison between fallers and non-fallers. Age Ageing 2004;33:602–7. 10.1093/ageing/afh218. [DOI] [PubMed] [Google Scholar]
- [20].Muir SW, Berg K, Chesworth BM, et al. Modifiable risk factors identify people who transition from non-fallers to fallers in community-dwelling older adults: a prospective study. Physiother Can 2010;62:358–67. 10.3138/physio.62.4.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Rao SS. Prevention of falls in older patients. Am Fam Physician 2005;72:81–8. [PubMed] [Google Scholar]
- [22].Bird ML, Fell J. Positive long-term effects of Pilates exercise on the aged-related decline in balance and strength in older, community-dwelling men and women. J Aging Phys Act 2014;22:342–7. 10.1123/japa.2013-0006. [DOI] [PubMed] [Google Scholar]
- [23].Donath L, Faude O, Roth R, et al. Effects of stair-climbing on balance, gait, strength, resting heart rate, and submaximal endurance in healthy seniors. Scand J Med Sci Sports 2014;24:e93–101. 10.1111/sms.12113. [DOI] [PubMed] [Google Scholar]
- [24].Granacher U, Muehlbauer T, Bridenbaugh SA, et al. Effects of a salsa dance training on balance and strength performance in older adults. Gerontology 2012;58:305–12. 10.1159/000334814. [DOI] [PubMed] [Google Scholar]
- [25].Yang F, King GA, Dillon L, et al. Controlled whole-body vibration training reduces risk of falls among community-dwelling older adults. J Biomech 2015;48:3206–12. 10.1016/j.jbiomech.2015.06.029. [DOI] [PubMed] [Google Scholar]
- [26].Bianco A, Patti A, Bellafiore M, et al. Group fitness activities for the elderly: an innovative approach to reduce falls and injuries. Aging Clin Exp Res 2014;26:147–52. 10.1007/s40520-013-0144-4. [DOI] [PubMed] [Google Scholar]
- [27].Patti A, Bianco A, Karsten B, et al. The effects of physical training without equipment on pain perception and balance in the elderly: a randomized controlled trial. Work 2017;57:23–30. 10.3233/WOR-172539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e100009710.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Ansai JH, Aurichio TR, Goncalves R, et al. Effects of two physical exercise protocols on physical performance related to falls in the oldest old: a randomized controlled trial. Geriatr Gerontol Int 2016;16:492–9. 10.1111/ggi.12497. [DOI] [PubMed] [Google Scholar]
- [30].Sousa N, Mendes R, Silva A, et al. Combined exercise is more effective than aerobic exercise in the improvement of fall risk factors: a randomized controlled trial in community-dwelling older men. Clin Rehabil 2017;31:478–86. 10.1177/0269215516655857. [DOI] [PubMed] [Google Scholar]
- [31].Leiros-Rodriguez R, Garcia-Soidan JL. Balance training in elderly women using public parks. J Women Aging 2014;26:207–18. 10.1080/08952841.2014.888220. [DOI] [PubMed] [Google Scholar]
- [32].Zhao Y, Chung PK, Tong TK. Effectiveness of a balance-focused exercise program for enhancing functional fitness of older adults at risk of falling: a randomised controlled trial. Geriatr Nurs 2017;38:491–7. 10.1016/j.gerinurse.2017.02.011. [DOI] [PubMed] [Google Scholar]
- [33].Chulvi-Medrano I, Colado JC, Pablos C, et al. A lower-limb training program to improve balance in healthy elderly women using the T-bow device. Phys Sportsmed 2009;37:127–35. 10.3810/psm.2009.06.1719. [DOI] [PubMed] [Google Scholar]
- [34].Ogaya S, Ikezoe T, Soda N, et al. Effects of balance training using wobble boards in the elderly. J Strength Cond Res 2011;25:2616–22. 10.1519/JSC.0b013e31820019cf. [DOI] [PubMed] [Google Scholar]
- [35].Dunsky A, Yahalom T, Arnon M, et al. The use of step aerobics and the stability ball to improve balance and quality of life in community-dwelling older adults - a randomized exploratory study. Arch Gerontol Geriatr 2017;71:66–74. 10.1016/j.archger.2017.03.003. [DOI] [PubMed] [Google Scholar]
- [36].Toulotte C, Toursel C, Olivier N. Wii Fit® training vs. Adapted physical activities: which one is the most appropriate to improve the balance of independent senior subjects? A randomized controlled study. Clin Rehabil 2012;26:827–35. 10.1177/0269215511434996. [DOI] [PubMed] [Google Scholar]
- [37].Marques EA, Figueiredo P, Harris TB, et al. Are resistance and aerobic exercise training equally effective at improving knee muscle strength and balance in older women? Arch Gerontol Geriatr 2017;68:106–12. 10.1016/j.archger.2016.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Lacroix A, Kressig RW, Muehlbauer T, et al. Effects of a supervised versus an unsupervised combined balance and strength training program on balance and muscle power in healthy older adults: a randomized controlled trial. Gerontology 2016;62:275–88. 10.1159/000442087. [DOI] [PubMed] [Google Scholar]
- [39].Lee IH, Park SY. Balance improvement by strength training for the elderly. J Phys Ther Sci 2013;25:1591–3. 10.1589/jpts.25.1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 2006;35Suppl 2:ii37–41. 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- [41].Xu D, Hong Y, Li J, et al. Effect of tai chi exercise on proprioception of ankle and knee joints in old people. Br J Sports Med 2004;38:50–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Barnett A, Smith B, Lord SR, et al. Community-based group exercise improves balance and reduces falls in at-risk older people: a randomised controlled trial. Age Ageing 2003;32:407–14. [DOI] [PubMed] [Google Scholar]
- [43].Liu H, Frank A. Tai chi as a balance improvement exercise for older adults: a systematic review. Arch Gerontol Geriatr 2010;33:103–9. [PubMed] [Google Scholar]
- [44].Maciaszek J, Osinski W. The effects of Tai Chi on body balance in elderly people--a review of studies from the early 21st century. Am J Chin Med 2010;38:219–29. 10.1142/S0192415X10007798. [DOI] [PubMed] [Google Scholar]
- [45].Leung DP, Chan CK, Tsang HW, et al. Tai chi as an intervention to improve balance and reduce falls in older adults: a systematic and meta-analytical review. Altern Ther Health Med 2011;17:40–8. [PubMed] [Google Scholar]
- [46].Herold F, Orlowski K, Bormel S, et al. Cortical activation during balancing on a balance board. Hum Mov Sci 2017;51:51–8. 10.1016/j.humov.2016.11.002. [DOI] [PubMed] [Google Scholar]
- [47].Bieryla KA. Xbox Kinect training to improve clinical measures of balance in older adults: a pilot study. Aging Clin Exp Res 2016;28:451–7. 10.1007/s40520-015-0452-y. [DOI] [PubMed] [Google Scholar]
- [48].Fisher JP, Steele J, Gentil P, et al. A minimal dose approach to resistance training for the older adult; the prophylactic for aging. Exp Gerontol 2017;99:80–6. 10.1016/j.exger.2017.09.012. [DOI] [PubMed] [Google Scholar]
- [49].Souza D, Barbalho M, Vieira CA, et al. Minimal dose resistance training with elastic tubes promotes functional and cardiovascular benefits to older women. Exp Gerontol 2019;115:132–8. 10.1016/j.exger.2018.12.001. [DOI] [PubMed] [Google Scholar]
- [50].Barbalho MSM, Gentil P, Izquierdo M, et al. There are no no-responders to low or high resistance training volumes among older women. Exp Gerontol 2017;99:18–26. 10.1016/j.exger.2017.09.003. [DOI] [PubMed] [Google Scholar]
- [51].Simonsick EM, Lafferty ME, Phillips CL, et al. Risk due to inactivity in physically capable older adults. Am J Public Health 1993;83:1443–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Knight JA. Physical inactivity: associated diseases and disorders. Ann Clin Lab Sci 2012;42:320–37. [PubMed] [Google Scholar]
- [53].Taylor D. Physical activity is medicine for older adults. Postgrad Med J 1059;90:26–32. 10.1136/postgradmedj-2012-131366. [DOI] [PMC free article] [PubMed] [Google Scholar]


