Abstract
Aim
To evaluate the effect of the addition of conventional ceramics on the physical, rheological and mechanical properties of conventional glass ionomer luting cement.
Materials and methods
5%, 10%, 15% and 20% (w/w) of Enamel and Body conventional ceramic additives (E44 Enamel and B96/c4 Body) were reinforced in the two commercially available glass ionomer luting cement – GC Fuji I (GC Corporation Tokyo, Japan) and Ketac Cem Radiopaque (3M ESPE AG). Setting time, film thickness and compressive strength of the cement was measured according to the American Dental Association Specification number 96 for luting cement. Enthalpy change of the cement reaction was measured with the help of Differential Scanning Calorimetry analysis. Compatibility between the sizes of powder particles was measured with the help of a particle size analyzer.
Results
5% of ceramic additive could not improve much of the compressive strength. Compressive strength increased significantly (p < 0.05) with the addition of 10% of ceramic additive, beyond which, there was a gradual decrease in strength. Although the setting time and film thickness were also shown to increase due to the additive, the former did not exceed the limit specified by the American Dental Association Specification number 96 (2–8 min for setting time and 25 microns for film thickness).
Conclusion
Addition of 10% of conventional ceramics resulted in a significant increase in the compressive strength of GIC Luting Cement without any significant compromise in its setting time. The substantial increase in film thickness is a major limitation. Use of ceramic additives with physical properties compatible with that of the glass ionomer cement may aid in increasing the compressive strength without compromising its setting time or film thickness.
Keywords: Materials science, Ketac cem, Compressive strength, Film thickness, Glass ionomer cements, Fuji-ionomer
1. Introduction
Dental cement was designed to retain restorations, appliances, and posts and cores in the oral environment in a stable and long-lasting position [1]. Given the increasing use of fixed partial dentures, the emphasis has been given to improving the physical and mechanical properties of luting materials. Luting agents can be definitive or provisional, depending on their physical properties and planned longevity of the restoration [2]. For acceptable performance, cement must have adequate resistance to dissolution in the oral environment. It should have high strength in tension, shear and compression and fracture toughness capable of resisting the stresses at the restoration-tooth interface. It should develop a strong bond through mechanical interlocking and adhesion [3]. Good manipulation properties, such as adequate working and setting times are also essential for its successful use [4].
Till date Glass ionomer cement [GIC] is the most widely used cement in dental practice. Conventional GICs are formed by the acid-base reaction of an ion-leachable fluoro-alumino-silicate glass with an aqueous solution of poly (acrylic acid) (PAA). Their main advantages are relative ease of use, chemical bonding to tooth substrate, long-term fluoride ion release, low coefficient of thermal expansion and acceptable esthetic quality. On the other hand, they exhibit moisture sensitivity and desiccation during the initial setting stages and relatively poor physical properties [5]. Their wear resistance is less than other aesthetic materials, such as composites and ceramics. Hence, considerable attention has been directed at improving strength, toughness, and resistance to wear by improving the technology of manufacturing of the cement constituents. More recently, ceramic-reinforced GIC (CR-GIC) has attracted some attention, due to their superior aesthetic appeal [6, 7].
The adhesive strength of the cement depends largely on the materials inherent strength. Glass ionomer luting cement possesses a maximum strength of 75 MPa thus limiting its adhesive properties. It has been suggested that increasing the compressive strength of the cement may improve its use as an adhesive [8, 9, 10, 11, 12, 13].
Several studies in recent years have attempted to enhance the GICs properties. Gavic L et al in 2016 studied the effect of the application of thermo-light curing on the microhardness of GICs. Moshaverinia M et al in 2016 evaluated the effects of addition of Nanoparticles fluorapatite (Nano-FA) on microhardness and fluoride release of Glass Ionomer restorative Cement. Gorseta K et al in 2017 studied the effect of different thermo-light polymerization on flexural strength of glass ionomer cement. Gorseta et al had extended the study to a clinical trial wherein they evaluated the effectiveness of new generation Glass Carbomer fissure sealant compared to the conventional resin-based sealant [14, 15, 16, 17]. Although these studies have improved various properties of GIC, the applications of the modified cement varied widely ranging from effective fluoride release to enhance its use as a sealant. The present study focused on improving the compressive strength of the GIC using hybridization for the sole purpose of improving its application as a luting cement.
According to the concept of hybridization, a material can be blended with another material having desired properties keeping in mind that both the materials should be compatible and inert to each other [18, 19, 20, 21]. The present study has been done based on the same grounds where Type I glass ionomer cement is blended with a ceramic material to increase its compressive strength and bond strength.
Ceramic materials are designed as strong restorative materials. They are used on a wide scale in dentistry owing to their esthetic and strength properties [6, 7]. Along with their own cohesive strength, they can reinforce the matrix of the cement in which it is added.
The present study analyzed the effect of adding varying concentrations of ceramic powder to conventional Glass Ionomer Luting Cement. We hypothesized that the ceramic additive would increase the physical and mechanical properties of the cement.
2. Materials and Methods
Two conventional glass ionomer cements GC Gold Label glass ionomer Luting and Lining cement (GC Corporation Tokyo, Japan) and Ketac Cem radiopaque Glass ionomer luting cement (3M ESPE AG) and two conventional ceramics, Spectrum porcelain (E 44 Enamel) and Spectrum porcelain (B96/c4 Body) by Dentsply was used in the study.
Both the cement were chemically cured and set by the acid-base reaction. Ketac Cem was water settable cement containing freeze-dried polyacrylic acid in powder and liquid consisting of only water and tartaric acid.
2.1. Setting time measurement
The mould (8 mm × 75 mm x 100mm) was conditioned at 23 ± 1 °C and was filled with mixed cement to the surface level. After 60 s (sec) of mixing, the mould was placed in the cabinet. The cabinet was maintained at a temperature of 37 ± 1 °C for 90 s. The indenter was carefully lowered vertically onto the surface of the cement and was in place for 5 s. The indenter used in the study was relatively heavier and the procedure was repeated every 30 s. Indentations were made until complete circular indentations were failed to be viewed. The needle was cleaned between the indentations to remove any debris. The process was repeated, with lighter indenter to calculate the final setting time. The lighter indenter was used at 10 s intervals. The net setting time was calculated from the end of mixing time till the time when needle stops making a complete circular indentation in the cement. The test was repeated three times [22].
2.2. Film thickness measurement
The combined thickness of the two optically flat glass plates having a contact surface area of 200mm ± 25mm2 stacked in contact was measured to an accuracy of ±1.25 μm (reading A). The upper plate was removed and 0.1 ml ± 0.05 ml of the mixed cement was placed in the center of the lower plate and this was placed centrally below the loading device of 150N ± 2 N on the lower plate. The second glass plate was replaced in the same orientation in the center on the cement. 10 sec prior to the end of stated working time by the manufacturer, the force was generated vertically to the center of the specimen via the top plate while ensuring that the space between the glass plates is completely filled by the cement. After 10 min of load application, the plates were removed from the loading device and second reading of the combined thickness of two glass plates and cement film was taken (reading B). The difference between the two readings was recorded as the thickness of the film. The test was repeated three times [22].
2.3. Compressive strength measurement
The split mould plates (with internal dimensions of 6 mm ± 0.l mm high and 4 mm ± 0.l mm diameter) and screw clamp were conditioned at a temperature of 23 ± 1 °C. Within 60 s of the completion of mixing, the cement was packed, into the split mould. The cement was placed in the mould in large proportions to avoid trapping air. The cement was filled more than the mould and placed on the bottom plate with some pressure. Bulk extruded cement was removed and the top metal plate was placed in position on the mould and squeezed together. The mould and plates were put in the screw clamp and tightened. 120 seconds after the completion of mixing, the whole assembly was transferred to the cabinet maintained at 37 ± 1 °C and relative humidity of 90%. After 1 h of the completion of mixing, the plates were removed and the specimen was ground at ends to make it flat at right angles to its long axis. After being removed from the mould, the specimen was checked visually without magnification for any air-voids or chipped edges. Defective specimens were discarded [22].
Twenty-four hours after the end of mixing, specimens were placed with flat ends between the plates of the mechanical tester (Instron), which was operated at a cross-head speed of 0.5 mm/min ±0.20 mm/min or at a loading rate of 50 N/min ±16 N/min. The compressive load was applied in the long axis of the specimen. When the specimen fractures the load applied was noted and the compressive strength, C, was calculated in megapascals, using the formula:
| C = 4p/pixd2 |
where;
p was the maximum load applied in Newton;
d was the diameter of the specimen, in millimeters.
2.4. Differential Scanning Calorimetry
The instrument used was DSC-60 (Shimadzu Corp, Japan) with Thermal Analyzer and Operating software of TA 60. The Flow controller was FCL 60. Indium was used as a reference. 5 mg fine powder was used as a sample and was placed in Al pan which was used as the sample holder. It was heated at the rate of 5 °C/min under a Nitrogen atmosphere in the Scanning range of 0–200 °C.
2.5. Particle size analyzer
CILAS 1064 was used to analyze the particle size. The samples were analyzed by dispersing the 5mg of the sample in water which was sonified for 5 min.
Statistical analysis was done with one-way ANOVA with a confidence interval of 99%. Tukey test was used for comparison. A p-value of less than 0.05 was considered statistically significant.
3. Results
3.1. Initial and final setting time
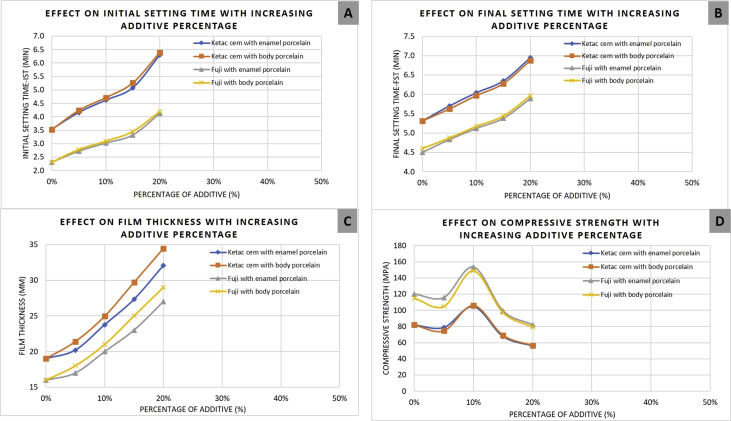
The addition of conventional enamel and body porcelain at concentrations of 5%, 10%, 15%, and 20%, resulted in significantly longer initial and final setting times (p < 0.05) than the control (0%).
Initial setting time for both the cements containing conventional enamel porcelain continued to increase with increasing concentration of ceramic, from 2.31 min for the control to 4.12 min for the powders containing 20% ceramic powder and from 3.53 min for the control to 6.30 min for the powders containing 20% ceramic powder in case of Fuji and Ketac Cem respectively (Fig. 1A). Similarly, initial setting time for Fuji and Ketac Cem cements containing conventional body porcelain continued to increase with increasing concentration of ceramic, from 2.31 min to 4.19 min and from 3.52 to 6.38 respectively (Fig. 1A).
Fig. 1.
A-Effect of Porcelain additives on the initial setting time of Glass Ionomer Luting Cements; B-Effect of Porcelain additives on the final setting time of Glass Ionomer Luting Cements; C-Effect of Porcelain additives on the film thickness of Glass Ionomer Luting Cements; D-Effect of Porcelain additives on Compressive Strength of Glass Ionomer Luting Cements.
Final setting time for both the cement Fuji and Ketac Cem also showed the same trend increasing from 4.50 to 5.89 min and from 5.31 to 6.95 min respectively with the addition of conventional enamel porcelain and from 4.60 to 5.96 min and from 5.31 to 6.88 min respectively with the addition of conventional body porcelain (Fig. 1B).
3.2. Film thickness
The film thickness of the cement showed a significant increase (p < 0.05) with the addition of both enamel and body porcelain. Compared to the control value of 16μ and 19μ in case of Fuji and Ketac Cem respectively film thickness went on increasing with increasing concentration of the additives (Fig. 1C). The maximum value for film thickness was reported at 20% with Fuji having 27μ and Ketac Cem having 32μ in case of enamel porcelain and 29μ and 34μ respectively in case of body porcelain.
3.3. Strength
Addition of conventional enamel porcelain in Fuji and Ketac Cem at 5% did not show any significant change (p > 0.05) compared to control. However, the addition of 10% of the same additive increased the strength value to a significant degree (p < 0.05) of 153.42 MPa and 104.73 MPa for Fuji and Ketac Cem respectively compared to their control value 120 MPa and 81.92 MPa respectively. But with further increase in the concentration of additive to 15 and 20% a significant (p < 0.05) decrease in strength was observed in both the cement (Fig. 1D).
A similar trend was observed with the addition of conventional body porcelain to both the cement. It showed a maximum value of 148.94 MPa and 106.06 MPa at 10% compared to the control value of 120 MPa and 81.92 MPa for Fuji and Ketac Cem respectively (Fig. 1D).
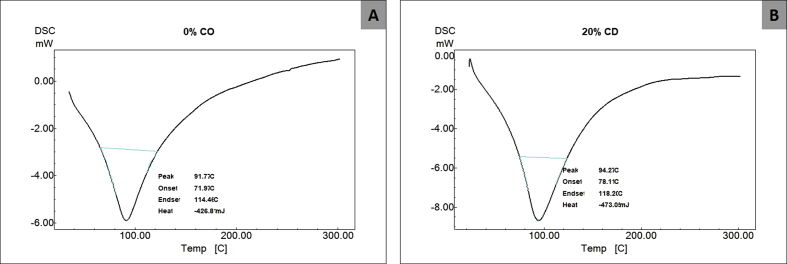
3.4. Differential Scanning Calorimetry
Enthalpy change has been reported from the DSC data which signifies that irrespective of the concentration, the setting of the conventional glass ionomer luting cement was delayed (Figs. 2A and 2B).
Fig. 2.
A- Enthalpy change during setting reaction of GIC without any additive; B-Enthalpy change during setting reaction of GIC with 20% additive.
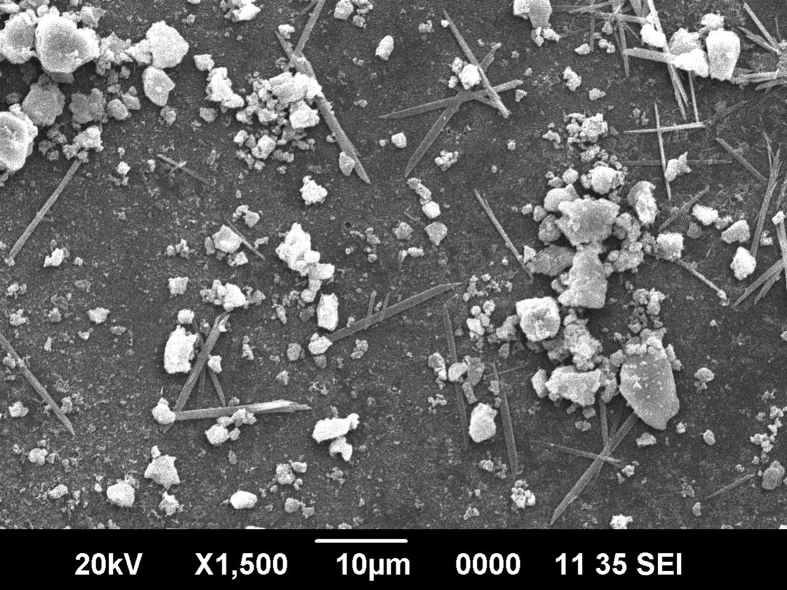
3.5. Particle size analysis
According to the results revealed through particle size analyzer, glass ionomer cement possesses a maximum size of about 18 μ whereas the ceramic additives have the maximum size of 35 μ.
3.6. Scanning electron microscopy
Through SEM again it was confirmed that the particle size of the ceramic additives is more than that of glass ionomer cement and hence acts as a filler (Fig. 3).
Fig. 3.
Particle size analysis of GIC and porcelain additive through SEM.
To summarise the results, the setting time and the film thickness of the cement showed a significant increase (p < 0.05) as the additive concentration was increased. A 10% increase in additive concentration resulted in a significant increase (p < 0.05) in the strength of the cement. On the contrary, further increase or decrease in additive concentration led to relatively decreased cement strength. Supplementary file 1 can be referred for detailed data analysis.
The null hypothesis of the study was that the addition of ceramics will not cause an increase in the strength of the cement. As mentioned above, a 10% increase in additive concentration caused a statistically significant increase in the strength of the cement. Thus, the null hypothesis was rejected.
4. Discussion
Properties of GIC as restorative material have been enhanced by the application of various techniques including thermo-light curing, the addition of nanoparticles fluorapatite and thermolight polymerization [14, 15, 16, 17]. Conventional glass ionomer luting cement properties can also be modified by incorporating various additives. The strength of the cement can be enhanced if the additive does not take part in the reaction and act as a reinforcing material to the matrix. In the present study, the conventional glass ionomer cement has been modified by incorporation of conventional ceramic additive and its effect on various properties of glass ionomer has been evaluated. It has been shown that zirconia forms the major if not the only (crystalline) component of the additive [19]. The foremost thing to consider while increasing the strength of the cement is to avoid any significant compromise on the other properties of the cement. The effect of various additives on both physical and mechanical properties of the cement has been discussed as follows individually:
The standard ADA requirements report the value of final setting time to be not more than 8 min for a luting cement. With the incorporation of ceramic additives, the setting time of both glass ionomer cements Fuji and Ketac Cem has shown to be an extender for a relatively longer duration, but still within the maximum limit of 8 min. As the concentration of additives is increased the setting time of the cement also increased. irrespective of the type of ceramic additive or the type of conventional glass ionomer cement used.
The delay in setting time can be explained with the help of a differential thermal analysis curve [23, 24]. The curve showed that there was an enthalpy change when the ceramic powder has been added to the cement compared to the control without any additive. The change in enthalpy was irrespective of the concentration of the additive used. Ceramic powder might act as a physical barrier in the normal setting of the cement to form a matrix. So, the formation of the matrix got delayed and hence the setting time was increased.
The film thickness is an important rheological property for the luting cement as they must be placed beneath the permanent restorations to seat in them in the proper place for a sufficiently long period of time. If the film thickness of luting cement does not meet the required ADA standards, it would result in the improper seating of the restorations leading to loss of a properly functional and occlusal relationship.
In the present study, film thickness increased significantly, even with the addition of just 5% additive. This increase can be explained based on the particle size analysis. The particles of conventional glass ionomer luting cement powder are very fine in nature exhibiting a particle size of nearly 18μ. While the porcelains exhibit a particle size of nearly 35μ. So, the two powders might not be able to blend properly to an acceptable degree. This might have led to a significant increase in the film thickness [25].
Secondly, the handling characteristics of the cement also got altered on the addition of the ceramic additive. As the concentration of the additive increased, there was a progressive increase in the viscosity of the cement compared to control, which in turn led to an increase in the film thickness [24].
Conventional ceramic was added in the glass ionomer luting cement in a view to enhance the compressive strength of the cement. For the additive to increase the strength of cement, it should be added in an optimum concentration so that it should not interfere with the normal matrix of the cement, rather it should reinforce the formed matrix.
Addition of 5% of additive did not show a significant change in the compressive strength compared to the addition of control. This can be explained on the basis that 5% concentration was not much enough to act as reinforcement for the cement. The value of compressive strength at 5% concentration largely represents the compressive strength of the conventional cement matrix. Thus, at 5% concentration, the additive is neither retarding nor enhancing the compressive strength of the cement [26].
At 10% concentration, the additive increased the compressive strength of the cement to a significant degree compared to the control value. The increase in strength is due to the reinforcement of the conventionally formed a matrix of the cement. The additive was acting as a filler which was confirmed by SEM. Thus 10% could be the optimum concentration for matrix formation and reinforcement [27].
Increasing the concentration of the ceramic further to 15 or 20% resulted in a decrease in the strength to lower than that of conventional glass ionomer cement. With the increase in additive percentage concentration of the cement, there may have been a deficiency of powder. Thus, the normal matrix formation could have been hampered. Reinforcement was present in sufficient amount but the matrix to be reinforced was insufficient [27]. Hence for an increase in the compressive strength, there should be an optimum concentration of conventional glass ionomer cement matrix and ceramic additive.
Addition of 10% of ceramic additive to conventional glass ionomer luting cement leads to a significant increase in the compressive strength of the luting cement. Setting time also increased by 10% but the change was not clinically significant as it was within the ADA specified limits of 8 min for luting cement. However, the film thickness at the same concentration showed a significantly higher value which was unacceptable for their use as luting cement.
Keeping in mind the above results, clinical trials of the cement reinforced with the desired amount of ceramic additive are required further. This would give the better picture of the properties of reinforced cement in a natural oral environment of the patient and also regarding the handling characteristics of the cement with respect to the clinician.
5. Conclusion
Based on the results it can be concluded that addition of ceramic powder at 10% concentration increased the compressive strength of the conventional glass ionomer luting cement without having a significant effect on the setting characteristics of the cement. However, film thickness showed a significant increase which could prove to be a major limitation in its use. Thus, to conclude, future studies must investigate the use of a compatibilizing agent which share properties with glass ionomer cement. Such agents may enhance the mechanical properties of the conventional glass ionomer cement without compromising the setting time and the film thickness.
Limitations of the study: As the study focussed on enhancing GIC properties for the sole purpose of improving its application as a luting cement, several other parameters including fluoride releasing ability, bonding of cement with different surfaces including enamel, dentin, temporary and permanent crowns, and orthodontic brackets, were not evaluated. Future in vitro and in vivo based studies using hybridization on GIC are needed to analyze other key properties of the cement including fluoride release, bonding characteristics.
Data Availability Statement: The raw/processed data required to reproduce these findings cannot be shared at this time due to legal or ethical reasons.
Declarations
Author contribution statement
Archana Gupta: Conceived and designed the experiments; Performed the experiments; Wrote the paper.
Pratiksha Mahajan: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
A Thirumal Raj & Sanjyot Mulay: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
I would like to acknowledge Dr. Nagraj Upadhya and Dr. Kishore Ginjupalli, Dept. of Dental Materials, Manipal College of Dental Sciences, Manipal for their guidance in the study.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.American National Standard/American Dental Association Specification. No. 96 for Dental Water-Based Cement.
- 2.Attar N., Tam L.E., McComb D. Mechanical and physical properties of contemporary dental luting agents. J. Prosthet. Dent. 2003;89(2):127–134. doi: 10.1067/mpr.2003.20. [DOI] [PubMed] [Google Scholar]
- 3.Behr M., Rosentritt M., Loher H., Kolbeck C., Trempler C., Stemplinger B. Changes in cement properties caused by mixing errors: the therapeutic range of different cement types. Dent. Mater. 2008;24:1187–1193. doi: 10.1016/j.dental.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 4.Bjornestal T. Essays.se; 2004. "Biomer": a New Type of Dental Material Obtained through Hybridization between Calcium Aluminates and Glass Ionomer Cement. [Google Scholar]
- 5.Craig R.G. twelfth ed. Mosby Elsevier Health Science Publications; 2006. Restorative Dental Materials; pp. 484–497. [Google Scholar]
- 6.Ewoldsen N., Demke R.S. A review of orthodontic cement and adhesives. Am. J. Orthod. Dentofac. Orthop. Ewoldsen and Demke. 2001;120(1):45–48. doi: 10.1067/mod.2001.117207. [DOI] [PubMed] [Google Scholar]
- 7.Fleming Garry J.P., Farooq Ahmed A., Barralet Jake E. Influence of powder/liquid mixing ratio on the performance of a restorative glass-ionomer dental cement. Biomaterials. 2003;24:4173–4179. doi: 10.1016/s0142-9612(03)00301-6. [DOI] [PubMed] [Google Scholar]
- 8.Gu Y.W., Yap A.U.J., Cheang P., Khor K.A. Effects of incorporation of HA/ZrO2 into glass ionomer cement (GIC) Biomaterials. 2005;26(7):713–720. doi: 10.1016/j.biomaterials.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 9.Ilie N., Hickel R. Mechanical behavior of glass ionomer cement as a function of loading condition and mixing procedure. Dent. Mater. J. 2007;26(4):526–533. doi: 10.4012/dmj.26.526. [DOI] [PubMed] [Google Scholar]
- 10.Kerby R.E., Knobloch L. Strength characteristics of glass-ionomer cements. Oper. Dent. 1992;17(5):170–174. [PubMed] [Google Scholar]
- 11.Mallmann A., Ataide J.C., Amoedo R., Rocha P.V., Jacques L.B. Compressive strength of glass ionomer cements using different specimen dimensions. Braz. Oral Res. 2007;21(3):204–208. doi: 10.1590/s1806-83242007000300003. [DOI] [PubMed] [Google Scholar]
- 12.Nakajima H., Watkins J.H., Arita K., Hanaoka K., Okabe T. Mechanical properties of glass ionomers under static and dynamic loading. Dent. Mater. 1996;12(1):30–37. doi: 10.1016/S0109-5641(96)80061-3. [DOI] [PubMed] [Google Scholar]
- 13.Pegoraro T.A., da Silva N., Carvalho R.M. Cements for use in esthetic dentistry. Dent. Clin. N. Am. 2007;51:453–471. doi: 10.1016/j.cden.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Gavic L., Gorseta K., Borzabadi-Farahani A., Tadin A., Glavina D., van Duinen R.N. Influence of thermo-light curing with dental light-curing units on the microhardness of glass-ionomer cements. Int. J. Periodontics Restor. Dent. 2016;36(3):425–430. doi: 10.11607/prd.2405. [DOI] [PubMed] [Google Scholar]
- 15.Moshaverinia M., Borzabadi-Farahani A., Sameni A., Moshaverinia A., Ansari S. Effects of incorporation of nano-fluorapatite particles on microhardness, fluoride-releasing properties, and biocompatibility of a conventional glass ionomer cement (GIC) Dent. Mater. J. 2016;35(5):817–821. doi: 10.4012/dmj.2015-437. [DOI] [PubMed] [Google Scholar]
- 16.Gorseta K., Borzabadi-Farahani A., Moshaverinia A., Glavina D., Lynch E. Effect of different thermo-light polymerization on flexural strength of two glass ionomer cements and a glass carbomer cement. J. Prosthet. Dent. 2017;118(1):102–107. doi: 10.1016/j.prosdent.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 17.Gorseta K., Glavina D., Borzabadi-Farahani A., Van Duinen R.N., Skrinjaric I., Hill R.G. One-year clinical evaluation of a Glass Carbomer fissure sealant, a preliminary study. Eur. J. Prosthodont. Restor. Dent. 2014;22(2):67–71. [PubMed] [Google Scholar]
- 18.Prentice L.H., Tyas M.J., Burrow M.F. The effect of particle size distribution on an experimental glass-ionomer cement. Dent. Mater. 2005;21(6):505–510. doi: 10.1016/j.dental.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 19.Prentice L.H., Tyas M.J., Burrow M.F. The effects of boric acid and phosphoric acid on the compressive strength of glass-ionomer cements. Dent. Mater. 2006;22:94–97. doi: 10.1016/j.dental.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 20.Prentice L.H., Tyas M.J., Burrow M.F. The effect of ytterbium fluoride and barium sulfate nanoparticles on the reactivity and strength of a glass-ionomer cement. Dent. Mater. 2006;22:746–751. doi: 10.1016/j.dental.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 21.Prosser H.J., Powis D.R., Wilson A.D. Glass-ionomer cements of improved flexural strength. J. Dent. Res. 1986;65(2):146–148. doi: 10.1177/00220345860650021101. [DOI] [PubMed] [Google Scholar]
- 22.Bansal R.K., Tewari U.S., Singh Parkash, Murthy D.V.S. Influence of cryolite on the properties of polycarboxylate cement. J. Prosthet. Dent. 1995;73:210–213. doi: 10.1016/s0022-3913(05)80163-5. [DOI] [PubMed] [Google Scholar]
- 23.Skrtic D., Antonucci J.M., Eanes E.D., Brunworth R.T. Silica- and zirconia-hybridized amorphous calcium phosphate: effect on transformation to hydroxyapatite. J. Biomed. Mater. Res. 2001:597–604. doi: 10.1002/jbm.10017. [DOI] [PubMed] [Google Scholar]
- 24.Smith D.C. Dental cements current status and future prospects. Dent. Clin. N. Am. 1983;6(3):763–793. [PubMed] [Google Scholar]
- 25.Wilson A.D., Crisp S., Abel G. Characterization of glass-ionomer cements - effect of molecular-weight on physical properties. J. Dent. 1977;5(2):117–120. doi: 10.1016/0300-5712(77)90070-7. [DOI] [PubMed] [Google Scholar]
- 26.Xie D., Park J.G., Faddah M., Zhao J., Khanijoun H.K. Novel amino acid-constructed polyalkenoates for dental glass-ionomer restoratives. J. Biomater. Appl. 2006;21:147–165. doi: 10.1177/0885328206059797. [DOI] [PubMed] [Google Scholar]
- 27.Xie D., Chung I.D., Wu W., Lemons J., Puckett A., Mays J. An amino acid-modified and non - HEMA containing glass-ionomer cement. Biomaterials. 2004;25:1825–1830. doi: 10.1016/j.biomaterials.2003.08.033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.