Abstract
Background:
We evaluated furosemide on attenuating lung injury and/or edema during coarctation repair surgery. We evaluated dynamic lung compliance. We measured the degree of lung edema by means of lung ultrasound (LUS). We recorded the (PaO2/FiO2 ratio) as an indicator for oxygenation.
Materials and Methods:
A study was conducted on 56 patients. Patients were divided into two groups: control group (Group C) which did not receive furosemide and furosemide group (Group F) at a dose of 1 mg/kg at induction of anesthesia. Dynamic lung compliance was calculated at induction (Cdyn 1) and at the end of the surgery (Cdyn 2). The (PaO2/FiO2 ratio) was calculated at start and end of surgery as (PF 1) and (PF 2), respectively. LUS was performed after induction (LUS 1) and at the end of the surgery. LUS 2 using the 12 regions method plotting the results on scale from 0 to 36. Mechanical ventilation days were recorded.
Results:
Administering furosemide attenuated the lung injury/edema and other pulmonary complications. Furosemide administration improved the dynamic lung compliance in the F Group compared to the C Group. Furthermore, it increased the (PaO2/FiO2 ratio) in the F Group compared to the C Group. LUS scale values were lower in the F Group compared to the C Group. There was also less postoperative mechanical ventilation days.
Conclusions:
The use of furosemide was accompanied by improved lung injury/edema profile as indicated by a much less drop in dynamic lung compliance, better oxygenation, a more favorable LUS scale with less parenchymal lung affection.
Keywords: Coarctation, furosemide, lungs
Introduction
Postoperative pulmonary complications (PPCs) refer to a group of complications that affect the respiratory system following surgery and are leading cause of morbidity and mortality.[1,2] Coarctation of the aorta is a common congenital abnormality of the cardiovascular system. Coarctation of the aorta is a condition that requires early interference.[3,4] Management options include surgery or interventional catheterization. Surgery is usually done through lateral thoracotomy in the left lateral position and usually entails resection of the stenosed segment and reanastomosis.[4,5] Surgery for coarctation is often followed by a drop in lung compliance and decreased arterial Pao2 values which may be partly attributed to mechanical compression and trauma to the ipsilateral lung (the nondependent lung) together with the potential for increased blood flow with subsequent congestion in the contralateral-dependent lung. Furosemide; a loop diuretic which acts by blocking the Na+ - K+ - 2 Cl− cotransport mechanism in the thick ascending part of the loop preventing Na+, K+, and Cl− from entering the tubular cells. Like all loop diuretics, it is highly potent and effective. Furosemide has long been used to treat lung edema of variable etiologies. Mechanisms include preload reduction and decrease in lung water.[6,7] Lung ultrasonography is a reliable tool that was recently introduced for the assessment of the lungs for early diagnosis of lung edema, atelectasis, and/or parenchymal lung changes.[8,9,10,11,12,13]
Materials and Methods
This study was a prospective randomized study, and it was conducted in the specialized Pediatric Hospital of Cairo University.
The study is registered on ClinicalTrials.gov with an ID NCT03364842.
A written informed consent from the patient parents and approval from the Ethical Committee of the department of anesthesia was obtained. A total of 56 patients with simple coarctation of the aorta aged (1–18 months) risk adjustment for congenital heart surgery-1 category 1[14] who required coarctation repair surgery were enrolled in the study. Patients were randomly assigned using computer-generated randomization into two groups: Group C (control) and Group F (furosemide).
Group F received furosemide 1 mg/kg immediately after induction.
The exclusion criteria included pneumonia (absence of fever, normal total leukocytic count, and normal C-reactive protein [CRP]), active heart failure, associated other cardiac defects, renal impairment (creatinine >1.5 mg/dl), and bleeding diathesis.
Preoperative fasting guidelines were followed.
All patients were premedicated with oral midazolam 0.5 mg/kg 1 h before anesthesia.
Induction was done by inhaled sevoflurane 4% in oxygen through face mask followed by insertion of a peripheral line.
This was followed by giving 1–2 μg/kg fentanyl and 0.5 mg/kg atracurium to facilitate endotracheal intubation to be repeated during surgery as required. Atropine was omitted except for marked bradycardia (heart rate <60/min). General anesthesia was maintained with sevoflurane 2% in oxygen and atracurium increments at 0.1 mg/kg every 20 min.
Ventilation was set as PCV to achieve a tidal volume (VT) of (8–10 ml/kg), and the respiratory rate was adjusted to maintain end-tidal CO2 35–45 mmHg.
All monitors were applied including electrocardiogram, pulse oximetry, noninvasive BP capnography, temperature, and a urinary catheter. A 4F central venous catheter was inserted. An arterial line was inserted for both invasive ambulatory blood pressure monitoring and arterial blood pressures sampling.
The patients were placed in the left lateral position. After induction, patients of Group F received furosemide at a dose 1 mg/kg. All patients received ringer acetate solution at 10 ml/kg/h. Blood loss was replaced with blood products accordingly.
Dynamic lung compliance was calculated at induction (Cdyn 1) and at the end of the surgery (Cdyn 2) using the VT and the peak inspiratory pressure (PIP), and the positive end-expiratory pressure (PEEP) values using the equation Cdyn = VT/(PIP-PEEP). The ratio of arterial oxygen partial pressure to fractional inspired oxygen (Pao2/Fio2 ratio) was calculated also at start and end of surgery as (PF 1) and (PF 2), respectively. Lung ultrasound (LUS) was performed after induction (LUS 1) for baseline reference and at the end of the surgery (LUS 2) using the 12 region method plotting the results on scale from 0 to 36.
Days of mechanical ventilation were recorded in both study groups.
Lung ultrasound assessment
One of the very basic concepts of lung ultrasonography is “lung sliding.” Sliding represents the layer of visceral pleura sliding on that of the parietal pleura lubricated by a small amount of pleural fluid (<50 ml normally). During respiration (spontaneous or mechanical), expansion of the lungs creates a sliding movement between the 2 pleural layers. US cannot identify a specific pleural layer. Lung sliding can be seen all over the lung surface where visceral pleura is directly adherent to the chest wall. Loss of lung sliding denotes that the 2 layers are no more sliding over each other. Clear identification of lung sliding excludes pneumothorax.[15]
Lung parenchyma that is normally filled with air is not directly visualized by sonography but shows a characteristic pattern of an artefact referred to as A-lines that are hyperechoic lines parallel to the pleural line. Another artifactual pattern is B-lines (also known as lung comets or comet-tail artefacts) are hyperechoic lines arising from and running perpendicular to the pleura up to the deep edge of the sonographic image, without fading, and obliterating the A-lines where they cross [Figure 1]. Initial reports suggested that the increase in B-lines come from thickened, edematous interlobular septa. Yet, recently, it was thought that they do not originate from distinct anatomical structural abnormalities, but rather from air-fluid interfaces produced in the lung parenchyma by neighboring fluid and air-filled structures such as alveolar air and the interstitium that correspond to increase in extravascular lung water (EVLW) or decrease in aeration. Although occasional B-lines are seen in normal lung, especially in dependent zones, a distinct increase in the amount and density of B-lines is considered pathological. Three or more separate B-lines visualized simultaneously or when they become confluent (also referred to as compact B-lines) are interpreted as thickening of the interlobular septae due to increased interstitial fluid or infiltration.
Figure 1.
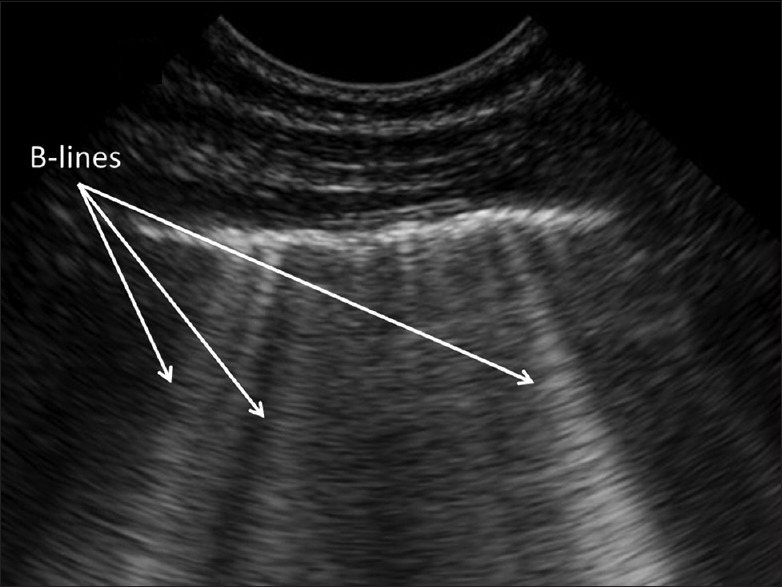
Ultrasound image from in a 2-year-old boy showing multiple and confluent B-lines in a single view
Although B-lines occur during congestion/edema and with parenchymal diseases like infection; yet US can still differentiate between both conditions. Infective and inflammatory conditions cause fluid to displace air. When this comes to the pleural surface, it can be visualized with sonography, usually as a hypoechoic subpleural area with some features. These features include: (a) loss of pleural line echogenicity over the area of consolidation and the absence of A-lines, (b) increased B-lines surrounding the consolidation area, (c) B-lines arise from the deep edge of the consolidation rather than from the pleura, and (d) sonographic air bronchograms seen as multiple hyperechoic punctate areas within the segment of consolidation or branching tree-like structures. Large consolidations tend to have a characteristic liver-like appearance, referred to as hepatization. In addition infection is often associated with other nonsonographic features such as fever, cough, leukocytosis, and elevated CRP.[16]
For our study, LUS was done using Sonosite M turbo ultrasound system (frequency 5 Hz; FUJIFILM Sonosite, Inc., Washington, US) with the ordinary convex probe. Sonography was done using the 12 regions method. Each side of the chest is divided into six regions (anterior, lateral and posterior each comprises upper and lower regions). The intercostal spaces of the 12 regions were examined. Four aeration patterns can be recognized: (a) normal aeration (N): lung sliding sign with respiratory movement or <3 B lines; (b) moderate loss of aeration: a clear number of multiple visible B-lines with horizontal spacing between adjacent B lines ≤7 mm (B1 lines); (c) severe loss of aeration: multiple B lines fused together that were difficult to count with horizontal spacing between adjacent B lines ≤3 mm, including “white lung” (B2 lines); and (d) pulmonary consolidation (C), hyperechoic lung tissue with dynamic air bronchogram. Each of the 12 regions was given a value as n = 0, B1 = 1, B2 = 2, and C = 3.[13]
The patient's LUS was the sum of all regional values with a score (ranging from 0 to 36). Ultrasound was done by a physician who is blind to the group to which the patient belongs.
Statistical analysis
Sample sizing was based on results obtained from previous studies.
Calculation of the sample size revealed that at least 24 patients in each group were needed to detect a difference in LUS score and a difference in compliance as small as 1.5 times its standard deviation (SD) with a power of 0.9 and a significance level of 0.05. The sample size was increased by four patients in each group (i.e., 28 patients in each group) to compensate for dropouts.
Statistical analysis was performed using statistical package for social science version 23.0, (IBM Corporation, Armonk, New York, USA). Normally distributed continuous data were represented as mean, and SD One-way analysis of variance was used to test the difference between means at different time points. The Mann–Whitney U test was used for nonparametric data. P < 0.05 was considered statistically significant.
Results
The study included 56 patients presented for surgical repair of coarctation who were divided into two equal groups – Group C and Group F.
There was no statistically significant difference between the two groups as regards the demographic data: age, gender, weight, and duration of surgery [Table 1].
Table 1.
Demographic data of both study groups (sex and age)
| C group | F group | |
|---|---|---|
| Sex (%) | ||
| Male | 14 (50) | 15 (53.6) |
| Female | 14 (50) | 13 (46.4) |
| Age (months) | 4.642±2.617 | 3.853±3.289 |
The dynamic lung compliance (Cdyn) was evaluated both intragroup and intergroup comparing (Cdyn) at start and end of the surgery; (Cdyn 1) and (Cdyn 2), respectively, and it was found that (Cdyn 2) was less than (Cdyn 1) in both groups and it decreased more significantly in the C Group (2.176 ± 0.549) than in the F Group (3.089 ± 0.912); (P < 0.05) [Figure 2].
Figure 2.
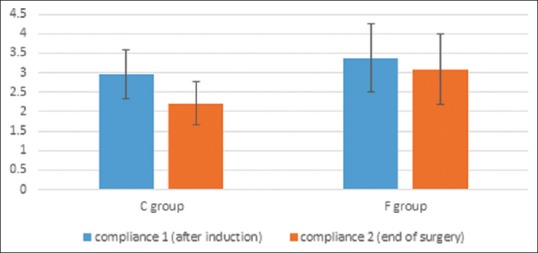
Compliance at induction and at end of surgery in both study groups
The (Pao2/Fio2 ratio) decreased from the baseline in both groups (PF 2 < PF 1) and this decrease was much in the C Group than in the F Group and the drop in the (Pao2/Fio2 ratio) at the end of surgery (PF 2) in Group F was significantly less (160.5 ± 42.057) than in Group C (270.536 ± 18.600); (P < 0.05) [Figure 3].
Figure 3.
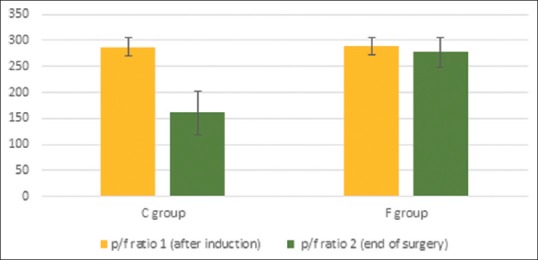
Pao2/Fio2 ratio at induction and at end of surgery in both study groups
Comparing lung sonography scores at start and end of surgery, it was found that score at the end of the surgery (LUS 2) was greater than that at start of surgery (LUS 1) indicating lung affection by edema and/or consolidation. It was found that despite being higher than (LUS 1) in both groups, yet (LUS 2) score was significantly less in the F Group than in the C Group denoting a more favorable lung condition and less affection by edema and/or consolidation [Figure 4].
Figure 4.
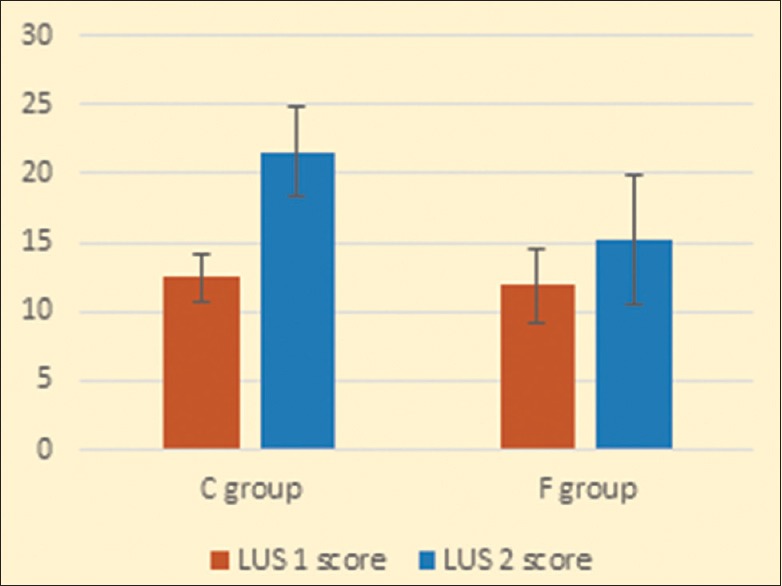
Lung ultrasound score at start and end of surgery in both study groups
The duration of postoperative mechanical ventilation was slightly less in the F Group than in the C Group but with no statistical significance [Table 2].
Table 2.
Average duration of postoperative ventilation in both study groups
| C group | F group | |
|---|---|---|
| Ventilation days | 2.286±0.937 | 1.714±0.763 |
On estimating the volume of urine in both groups, it was found that there was a markedly increased urine output (UOP) in F Group than in C Group.
Discussion
PPCs are leading causes of postoperative morbidity and mortality following thoracotomy. This involves several major problems such as pneumonia, bronchitis, atelectasis, lung edema, respiratory failure, and prolonged mechanical ventilation.[1,2] Types and severity of such complications vary with the procedure done and the patient preoperative condition. In our study, we were concerned with lateral thoracotomy. The position of lateral thoracotomy itself alters lung physiology and mechanics through decreasing the functional residual capacity and the forced vital capacity. Additional contributing factors include airway secretions, bleeding, and altered lung parenchyma that occur secondary due to lung ischemia and reperfusion following lung collapse and manipulations, altered capillary permeability, mediators release, and lung injury secondary to mechanical ventilation. In conclusion, several factors make the children more likely to become desaturated during lateral thoracotomy.[17]
Coarctation of the aorta is a common congenital anomaly that accounts for (5%–8%) of all cardiac congenital anomalies. The most common site for coarctation is at the site of attachment of the ductus arteriosus.[3,4] As part of the pathophysiology of coarctation of the aorta; pressure load is exerted on the left ventricle with subsequent hypertrophy which might end up with left ventricular failure.
Furosemide, a loop diuretic that is commonly used for the treatment of hypertension and heart failure has been also used for the treatment of pulmonary edema both of cardiogenic or noncardiogenic origin. The role of loop diuretics in pulmonary edema is mediated through reducing the preload and decompression of the circulation. Therefore, they should be used with extreme caution in patients with potentially depleted intravascular volume.[6,7] In the instance of cardiogenic lung edema, the pathogenesis is primarily increased capillary hydrostatic pressure with subsequent alveolar edema. In the instance of noncardiogenic lung edema, the main pathology is damage to the alveolocapillary membrane together with inflammation resulting in fluid leakage into the alveoli and/or the interstitium. In either condition, the resultant edema reduces lung compliance and interferes with oxygenation therefore treating such edema is of great value to attenuate the severity and improving the outcome.
Surgery for coarctation of the aorta entails putting the patient in the left lateral position, thoracotomy, compressing the lungs, reaching the coarctation segment followed by excision and reanastomosis. This is often associated by mechanical trauma to the ipsilateral lung, lung collapse, and presence of secretions and/or blood within the airways, especially with the technically difficult to use one lung ventilation in young children.[4,5] The contralateral-dependent lung might also suffer secondary to slightly increased blood flow, atelectasis, and spillage of secretions from the upper lung which is more evident during thoracotomy in pediatrics.[5,17] The postoperative course is usually affected by the condition of the lungs peri- and intra-operatively in addition to the extent of the thoracotomy incision. Thoracotomy itself is a type of surgery that is commonly accompanied by PPCs.
LUS has been recently introduced as a tool to evaluate the lungs parenchyma for EVLW and/or congestion.[8,9,10] Many methods have been introduced for quantitative assessment of lung water the most applicable of them is the 12 regions method graded from 0 to 3 for each region and summed collectively to a score from 0 to 36.[13]
In our study, we studied whether using furosemide during coarctation repair surgery would result in decreasing the severity of postoperative lung complications and whether this would affect the overall hospital stay.
Here, we evaluated the severity of lung complications through assessment of the dynamic lung compliance, the Pao2/Fio2 ratio, and LUS. We also recorded the duration of ICU stay and the volume of UOP.
Patients in both study groups showed a reduced lung compliance at the end of the surgery, yet the reduction in compliance was much more profound in the C Group than in the F Group denoting that the lungs are possibly healthier in the F Group.
In the F Group, were we used furosemide; we found that the Pao2/Fio2 ratio was minimally affected at the end of the surgery as compared to the Pao2/Fio2 ratio calculated in the C Group which was markedly and significantly decreased.
These findings were in agreement with the findings of Martin et al. who conducted a study in 2002 and a follow-up study in 2005 where they found that furosemide/albumin combination slightly improved the Pao2/Fio2 ratio, reduced the duration of ventilation, ICU time and hospital stay in acute lung injury/acute respiratory distress (ARDS) patients.[18,19]
Zhao et al. in 2015 validated the correlation between lung ultrasonography and PiCCO in the evaluation of EVLW in the setting of ARDS. They also used LUS as a prognostic tool during ARDS.[13] Volpicelli et al. in 2014 used LUS to evaluate EVLW together with LVEF as indicators for lung congestion in correlation to PAOP measurement in patients who required invasive monitoring.[9]
In 2014, Vitale et al. reviewed the use of lung ultrasonography as a tool for diagnosis of PPCs following cardiac surgery in pediatrics. They found that LUS proved strong correlation to chest radiographs.[20]
Anile et al. in 2017 correlated LUS to PiCCO in evaluating EVLW in critically ill patients requiring ventilation and found that LUS was strongly correlated to the values of PiCCO with an advantage of being noninvasive.[20] For our study, when we have imaged the lungs by sonography, the LUS scale in both study groups at the end of surgery was higher than the LUS scale at initiation of surgery, yet the increase in LUS scale for the C Group was marked and much significant than the very slight increase in such scale in the F Group, [Figure 3]. This can be explained by alveolar and interstitial edema, atelectasis and intraluminal secretions and/or blood clots. Furosemide may contribute to dryness of the lungs and prophylaxis against potential edema in addition to treating already developed edema which may have been developed secondary to manipulations, potential fluid overload or very rarely due to left ventricular failure. Findings of LUS were confirmed by routine chest X-ray on ICU admission and findings were usually in agreement to LUS.
The average duration of mechanical ventilation was compared between both groups, and it was less in the F Group than in the C Group due to less frequently and less severely developed pulmonary complications.
Conclusions
The use of furosemide during coarctation repair surgery through lateral thoracotomy was associated by much less postoperative complications and led to a more favorable outcome as assessed by evaluating dynamic lung compliance, Pao2/Fio2 ratio and noninvasive bedside lung imaging by LUS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rudra A, Sudipta D. Postoperative pulmonary complications. Indian J Anaesth. 2006;50:89–98. [Google Scholar]
- 2.Agostini P, Cieslik H, Rathinam S, Bishay E, Kalkat MS, Rajesh PB, et al. Postoperative pulmonary complications following thoracic surgery: Are there any modifiable risk factors? Thorax. 2010;65:815–8. doi: 10.1136/thx.2009.123083. [DOI] [PubMed] [Google Scholar]
- 3.Kenny D, Hijazi ZM. Coarctation of the aorta: From fetal life to adulthood. Cardiol J. 2011;18:487–95. doi: 10.5603/cj.2011.0003. [DOI] [PubMed] [Google Scholar]
- 4.Doshi AR, Syamasundar Rao P. Coarctation of aorta-management options and decision making. Pediatr Therapeut. 2012;S5:6. [Google Scholar]
- 5.Omeje I, Poruban R, Sagát M, Nosál M, Hraška V. Surgical treatment of aortic coarctation. Images Paediatr Cardiol. 2004;6:18–28. [PMC free article] [PubMed] [Google Scholar]
- 6.Pacifici GM. Clinical pharmacology of furosemide in neonates: A review. Pharmaceuticals (Basel) 2013;6:1094–129. doi: 10.3390/ph6091094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buggey J, Mentz RJ, Pitt B, Eisenstein EL, Anstrom KJ, Velazquez EJ, et al. A reappraisal of loop diuretic choice in heart failure patients. Am Heart J. 2015;169:323–33. doi: 10.1016/j.ahj.2014.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Volpicelli G. Lung sonography. J Ultrasound Med. 2013;32:165–71. doi: 10.7863/jum.2013.32.1.165. [DOI] [PubMed] [Google Scholar]
- 9.Volpicelli G, Skurzak S, Boero E, Carpinteri G, Tengattini M, Stefanone V, et al. Lung ultrasound predicts well extravascular lung water but is of limited usefulness in the prediction of wedge pressure. Anesthesiology. 2014;121:320–7. doi: 10.1097/ALN.0000000000000300. [DOI] [PubMed] [Google Scholar]
- 10.Platz E, Lewis EF, Uno H, Peck J, Pivetta E, Merz AA, et al. Detection and prognostic value of pulmonary congestion by lung ultrasound in ambulatory heart failure patients. Eur Heart J. 2016;37:1244–51. doi: 10.1093/eurheartj/ehv745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anile A, Russo J, Castiglione G, Volpicelli G. A simplified lung ultrasound approach to detect increased extravascular lung water in critically ill patients. Crit Ultrasound J. 2017;9:13. doi: 10.1186/s13089-017-0068-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Picano E, Pellikka PA. Ultrasound of extravascular lung water: A new standard for pulmonary congestion. Eur Heart J. 2016;37:2097–104. doi: 10.1093/eurheartj/ehw164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao Z, Jiang L, Xi X, Jiang Q, Zhu B, Wang M, et al. Prognostic value of extravascular lung water assessed with lung ultrasound score by chest sonography in patients with acute respiratory distress syndrome. BMC Pulm Med. 2015;15:98. doi: 10.1186/s12890-015-0091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI, et al. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2002;123:110–8. doi: 10.1067/mtc.2002.119064. [DOI] [PubMed] [Google Scholar]
- 15.Strnad M, Zadel S, Klemenc-Ketis Z, Prosen G. Identification of lung sliding: A basic ultrasound technique with a steep learning curve. Signa Vitae. 2013;8:31–5. [Google Scholar]
- 16.Stadler JA, Andronikou S, Zar HJ. Lung ultrasound for the diagnosis of community-acquired pneumonia in children. Pediatr Radiol. 2017;47:1412–9. doi: 10.1007/s00247-017-3910-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Golianua B, Hammerb GB. Pediatric thoracic anesthesia. Curr Opin Anaesthesiol. 2005;18:5–11. doi: 10.1097/00001503-200502000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Martin GS, Mangialardi RJ, Wheeler AP, Dupont WD, Morris JA, Bernard GR, et al. Albumin and furosemide therapy in hypoproteinemic patients with acute lung injury. Crit Care Med. 2002;30:2175–82. doi: 10.1097/00003246-200210000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Martin GS, Moss M, Wheeler AP, Mealer M, Morris JA, Bernard GR, et al. A randomized, controlled trial of furosemide with or without albumin in hypoproteinemic patients with acute lung injury. Crit Care Med. 2005;33:1681–7. doi: 10.1097/01.ccm.0000171539.47006.02. [DOI] [PubMed] [Google Scholar]
- 20.Vitale V, Ricci Z, Cogo P. Lung ultrasonography and pediatric cardiac surgery: First experience with a new tool for postoperative lung complications. Ann Thorac Surg. 2014;97:e121–4. doi: 10.1016/j.athoracsur.2014.01.060. [DOI] [PubMed] [Google Scholar]


