Abstract
Introduction:
Prescription opioids were responsible for approximately 17,000 deaths in the U.S. in 2016. One in five prescription opioid deaths also involve alcohol. Drinkers who misuse prescription opioids (i.e., use without a prescription or use only for the experience or feeling it caused) are at heightened risk of overdose. However, little is known about the relationship between drinking patterns and prescription opioid misuse.
Methods:
Data were analyzed from the 160,812 individuals (aged ≥12 years) who responded to questions about prescription opioid misuse and alcohol consumption in the 2012, 2013, or 2014 National Survey on Drug Use and Health (analyzed in 2017–2018). The prevalence of self-reported past 30-day prescription opioid misuse was assessed by sociodemographic characteristics, other substance use (i.e., cigarettes, marijuana), and drinking patterns. Multiple logistic regression was used to calculate AORs.
Results:
From 2012 to 2014, 1.6% (95% CI=1.5, 1.7) of all individuals aged ≥12 years (estimated 4.2 million) and 3.5% (95% CI=3.3, 3.8) of binge drinkers (estimated 2.2 million) reported prescription opioid misuse. Prescription opioid misuse was more common among binge drinkers than non-drinkers (AOR=1.7, 95% CI=1.5, 1.9). Overall, the prevalence of prescription opioid misuse increased significantly with binge drinking frequency (p-value <0.001).
Conclusions:
More than half of the 4.2 million people who misused prescription opioids during 2012–2014 were binge drinkers, and binge drinkers had nearly twice the odds of misusing prescription opioids compared with non-drinkers. Widespread use of evidence-based strategies for preventing binge drinking might reduce opioid misuse and overdoses involving alcohol.
INTRODUCTION
Prescription opioids were involved in approximately 17,000 deaths in the U.S. in 2016,1 tripling since 1999.2,3 The number of opioid prescriptions written also tripled during this time, substantially increasing opioid availability.4 In addition, prescription opioid overdose, abuse, and dependence cost the U.S. $78.5 billion in 2013, including healthcare claims, substance use disorder treatment, criminal justice costs, and lost productivity.5 Consequently, the opioid overdose epidemic has been declared a public health emergency.6
Compared with those who use opioids as prescribed, people who misuse prescription opioids (defined in this analysis as using an opioid without a prescription, or using these drugs only for the experience or feeling it caused) may consume higher doses of these drugs, use them more frequently, or both, increasing the risk of non-fatal and fatal overdoses.7–9 One study analyzed data from the Drug Abuse Warning Network on emergency department (ED) visits and found that there were 305,900 ED visits due to prescription opioid misuse in 2008, which was double the number reported in 2004.10
An important, though generally underrecognized risk factor for opioid misuse is alcohol consumption, particularly excessive drinking. For example, a study using 2006 data from the National Survey on Drug Use and Health (NSDUH) found that, compared with non-drinkers, men and women who consumed alcohol during the previous year were 70% and 90% more likely to misuse opioids during the previous year, respectively.11 However, the authors did not assess the association between prescription opioid misuse and alcohol use by sociodemographic characteristics other than gender, nor did they examine this relationship by drinking patterns (e.g., binge drinking). Another study using the 2001–2002 National Epidemiologic Survey on Alcohol Related Conditions found that 1.1% of past-year drinkers who did not binge drink, and 2.2% of binge drinkers who did not have alcohol abuse or dependence, misused prescription opioids during the past year.12 After controlling for sex, age, and race or ethnicity, past-year drinkers who did not binge drink, and binge drinkers who did not meet DSM-IV criteria for alcohol abuse or dependence, were 1.8 and 3.6 times more likely to report past-year prescription opioid misuse than non-drinkers, respectively. However, the authors did not assess this relationship by sociodemographic characteristics, nor did they control for differences in annual household income, which has been shown to be associated with both binge drinking and prescription opioid misuse.13,14 In addition, the authors were unable to fully assess the relationship between binge drinking and prescription opioid misuse because of the exclusion of respondents who met DSM-IV criteria for alcohol abuse or dependence from their binge drinking population.
Alcohol consumption has also been associated with prescription opioid overdoses. In 2010, one in five opioid-involved deaths in the U.S. also involved alcohol.15 In addition, alcohol was involved in 18% of the prescription opioid-involved ED visits in 2010, and more than 40% of these prescription opioid-involved overdoses were among ED patients aged 30–54 years.15 Similarly, in 2008, a nationwide study found that 20% of hospitalizations for prescription opioid overdoses among young adults aged 18–24 years involved excessive alcohol use (i.e., ICD-9-CM codes 980, E860, 303.0, 305.0, or 790.3), which is similar to the proportion of opioid overdoses among people in this age group that involved excessive alcohol use in 1999 (17%).16 The concurrent use of alcohol and prescription opioids is concerning because both have a depressant effect on the central nervous system, and the concurrent use of these drugs could therefore lead to a dangerous drug interaction that could significantly increase the risk of respiratory depression and death.17–21
The purpose of this study is to assess the association between past 30-day drinking patterns (e.g., current, non-binge drinking and binge drinking) and prescription opioid misuse among U.S. adults and adolescents. In addition, this study seeks to examine the relationship between binge drinking frequency and prescription opioid misuse.
METHODS
Study Sample
The NSDUH is a nationally representative, cross-sectional household survey of the non-institutionalized U.S. adult and adolescent population aged ≥12 years residing in the 50 states and the District of Columbia that is conducted annually by the Substance Abuse and Mental Health Services Administration. For each state and the District of Columbia, a multistage probability sample was independently determined. A computer-assisted personal interview and audio computer-assisted self-interview (to improve respondents’ privacy during visits to households and group living residences) were used to collect survey data. Respondents were given $30 as compensation for their participation in the survey. More details on the NSDUH methods are available elsewhere.22
Data for this study were pooled from the 2012, 2013, and 2014 NSDUH public use files to smooth out random fluctuations in self-reported alcohol use and prescription opioid misuse, particularly when assessing prescription opioid misuse by drinking patterns and sociodemographic characteristics. Weighted response rates were 73.0% (2012), 71.7% (2013), and 71.2% (2014). There was a total of 204,048 survey respondents during the 3-year study period. The study sample included the 160,812 (78.8%) of the total respondents who answered questions about the misuse of prescription opioids and alcohol consumption.
Measures
Respondents were categorized into three drinking categories (i.e., non-drinkers, current/non-binge drinkers, and binge drinkers) on the basis of responses to the following questions: (1) During the past 30 days, on how many days did you drink one or more drinks of an alcoholic beverage?; (2) During the past 30 days, that is since [datefill], on how many days did you have 5 or more drinks on the same occasion? By “occasion,” we mean at the same time or within a couple of hours of each other. (question for males); and (3) During the past 30 days, that is since [datefill], on how many days did you have 4 or more drinks on the same occasion? (question for females). Non-drinking was defined as not consuming an alcoholic drink on any day during the past 30 days, including lifetime abstainers. Current drinking was defined as consuming one or more alcoholic drinks on ≥1 days during the past 30 days. Binge drinking was defined as consuming five or more drinks (for males) or four or more drinks (for females), per occasion, on ≥1 day during the past 30 days. Current/non-binge drinking was defined as current drinking below binge levels. Binge drinking frequency was defined as the number of days a respondent consumed five or more drinks (for males) or four or more drinks (for females) per occasion during the past 30 days.
In the survey section on use of prescription medications, the NSDUH interviewers asked a series of questions about use of specific types of opioids (e.g., codeine, hydrocodone, and morphine). This study assessed prescription opioid misuse on the basis of responses to the following question: How long has it been since you last used any prescription pain reliever that was not prescribed for you or that you took only for the experience or feeling it caused? Prescription opioid misuse was defined as the use of an opioid without a prescription, or the use of these drugs only for the experience or feeling it caused at least one time during the past 30 days.
Statistical Analysis
The prevalence of past 30-day prescription opioid misuse, non-drinking, current/non-binge, and binge drinking were assessed overall and by sociodemographic characteristics and other substance use (i.e., past 30-day cigarette use or marijuana use). Prescription opioid misuse was also assessed by drinking pattern, sociodemographic characteristics, and other substance use. The relationship between binge drinking frequency and prescription opioid misuse was assessed overall and by age group. NSDUH survey weights and design variables were used to compute prevalence estimates and 95% CIs. A new population weight was created for this 3-year dataset by dividing the single-year dataset weights by three. P-values were calculated using Pearson’s chi-square tests (p-values <0.05 were used to assess statistical significance). When measuring the association between prescription opioid misuse and binge drinking, multiple logistic regression was used to adjust ORs for potential confounders, including age group, sex, race or ethnicity, total annual family income, rural or urban status,22 cigarette use,23,24 and marijuana use.23–25
Respondents who were missing data on sociodemographic characteristics or on drinking patterns were excluded from item-specific analyses (missing data were <3%). Data were analyzed using Stata, version 14.2 (analyses were conducted in 2017–2018).
RESULTS
During 2012–2014, 1.6% (95% CI=1.5, 1.7) of U.S. adults and adolescents, or an estimated 4.2 million people, reported past 30-day prescription opioid misuse (Table 1). Prescription opioid misuse was most common among males (1.9%, 95% CI=1.7, 2.1), those aged 18–25 years (2.9%, 95% CI=2.7, 3.1) and 26–34 years (2.8%, 95% CI=2.4, 3.1), among those with an annual family income of <$20,000 (2.3%, 95% CI=2.1, 2.6), and among those with no health insurance coverage (2.9%, 95% CI=2.6, 3.2). Current/non-binge drinking was most common among adults aged ≥50 years (33.4%, 95% CI=32.6, 34.3); white, non-Hispanic adults (31.1%, 95% CI=30.5, 31.6); college graduates (43.4%, 95% CI=42.5, 44.4); and those with an annual family income of >$75,000 (36.9%, 95% CI=36.1, 37.6). Binge drinking was most common among males (29.6%, 95% CI=29.0, 30.2); those aged 18–25 years (40.4, 95% CI=39.7, 41.1) and 26–34 years (38.8%, 95% CI=38.0, 39.7); white, non-Hispanic adults (25.8%, 95% CI=25.3, 26.3); and adults with some college education (28.7%, 95% CI=28.0, 29.5).
Table 1.
Prevalence of Past-30 Day Prescription Opioida Misuse and Drinking Patterns by Characteristics
| Characteristics | Prescription opioid misusera (n=160,812) |
Weighted total population who misused prescription opioidsa |
Non-drinkersb (n=89,898) |
Current/non-binge drinkersc (n=30,296) |
Binge drinkersd (n=40,618) |
||||
|---|---|---|---|---|---|---|---|---|---|
| Weighted % (95% CI) |
p-value | N | Weighted % (95% CI) |
p-value | Weighted % (95% CI) |
p-value | Weighted % (95% CI) |
p-value | |
| Overall | 1.6 (1.5, 1.7) | 4,196,285 | 48.7 (48.2, 49.1) | 27.0 (26.6, 27.5) | 24.3 (23.9, 24.7) | ||||
| Sex | <0.001 | <0.001 | 0.003 | <0.001 | |||||
| Male | 1.9 (1.7, 2.1) | 2,335,637 | 44.0 (43.4, 44.6) | 26.4 (25.8, 27.0) | 29.6 (29.0, 30.2) | ||||
| Female | 1.4 (1.3, 1.5) | 1,860,648 | 53.1 (52.4, 53.7) | 27.7 (27.0, 28.3) | 19.3 (18.8, 19.8) | ||||
| Age group, years | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| 12–17 | 1.7 (1.5, 1.8) | 402,186 | 89.3 (89.0, 89.7) | 4.5 (4.3, 4.8) | 6.1 (5.8, 6.5) | ||||
| 18–25 | 2.9 (2.7, 3.1) | 980,231 | 41.1 (40.7, 41.7) | 18.5 (18.0, 19.1) | 40.4 (39.7, 41.1) | ||||
| 26–34 | 2.8 (2.4, 3.1) | 1,005,464 | 35.1 (34.1, 36.1) | 26.1 (25.2, 27.1) | 38.8 (38.0, 39.7) | ||||
| 35–49 | 1.7 (1.5, 1.9) | 996,565 | 40.3 (39.3, 41.2) | 30.6 (29.7, 31.4) | 29.2 (28.4, 30.1) | ||||
| ≥50 | 0.8 (0.6, 1.0) | 811,839 | 51.3 (50.4, 52.1) | 33.4 (32.6, 34.3) | 15.3 (14.6, 16.0) | ||||
| Race or ethnicity | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| White, non-Hispanic | 1.7 (1.5, 1.8) | 2,757,801 | 43.2 (42.6, 43.8) | 31.1 (30.5, 31.6) | 25.8 (25.3, 26.3) | ||||
| Black, non-Hispanic | 2.0 (1.7, 2.3) | 598,615 | 57.2 (56.0, 58.3) | 21.6 (20.6, 22.7) | 21.2 (20.4, 22.0) | ||||
| Hispanic or Latino | 1.6 (1.4, 1.8) | 634,783 | 58.6 (57.3, 60.0) | 17.0 (16.0, 18.0) | 24.4 (23.4, 25.3) | ||||
| Othere | 1.1 (0.8, 1.3) | 205,087 | 61.7 (60.2, 63.2) | 21.8 (20.3, 23.3) | 16.5 (15.4, 17.7) | ||||
| Educationf | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Less than high school | 2.3 (2.0, 2.6) | 710,396 | 65.9 (64.4, 67.4) | 11.8 (11.0, 12.7) | 22.3 (21.1, 23.5) | ||||
| High school graduate | 1.8 (1.6, 2.0) | 1,204,632 | 51.1 (50.2, 52.0) | 22.0 (21.2, 22.8) | 26.9 (26.1, 27.7) | ||||
| Some college | 1.8 (1.6, 2.0) | 1,101,217 | 40.9 (39.8, 41.9) | 30.4 (29.4, 31.4) | 28.7 (28.0, 29.5) | ||||
| College graduate | 2.3 (2.1, 2.6) | 777,854 | 31.6 (30.7, 32.5) | 43.4 (42.5, 44.4) | 25.0 (24.3, 25.7) | ||||
| Family income (annual) | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| <$20,000 | 2.3 (2.1, 2.6) | 1,079,547 | 60.6 (59.6, 61.6) | 15.1 (14.3, 15.8) | 24.3 (23.5, 25.1) | ||||
| $20,000–<$50,000 | 1.8 (1.6, 1.9) | 1,414,192 | 54.7 (53.9, 55.4) | 22.2 (21.5, 23.0) | 23.1 (22.5, 23.7) | ||||
| $50,000–<$75,000 | 1.4 (1.2, 1.6) | 603,652 | 46.0 (44.9, 47.2) | 29.5 (28.4, 30.6) | 24.5 (23.7, 25.3) | ||||
| ≥$75,000 | 1.3 (1.1, 1.5) | 1,098,894 | 37.8 (37.1, 38.6) | 36.9 (36.1, 37.6) | 25.3 (24.6, 26.0) | ||||
| Rural or urban statusg | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Large metropolitan | 1.7 (1.5, 1.8) | 2,310,371 | 46.5 (45.8, 47.1) | 28.6 (28.0, 29.2) | 24.9 (24.4, 25.5) | ||||
| Small metropolitan | 1.8 (1.6, 2.0) | 1,372,597 | 49.1 (48.0, 50.2) | 26.6 (25.8, 27.4) | 24.3 (23.6, 25.1) | ||||
| Nonmetropolitan | 1.3 (1.1, 1.4) | 513,317 | 55.4 (54.2, 56.4) | 22.5 (21.7, 23.4) | 22.2 (21.4, 23.0) | ||||
| Health insuranceh | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Private | 1.3 (1.2, 1.4) | 2,136,255 | 42.9 (42.4, 43.4) | 32.1 (31.5, 32.6) | 25.0 (24.6, 25.5) | ||||
| Public | 1.9 (1.7, 2.2) | 954,184 | 67.1 (66.1, 68.1) | 16.9 (16.1, 17.7) | 16.0 (15.3, 16.7) | ||||
| Other | 2.0 (1.5, 2.6) | 94,362 | 47.9 (45.1, 50.7) | 20.5 (18.3, 23.0) | 31.5 (29.2, 34.0) | ||||
| No coverage | 2.9 (2.6, 3.2) | 1,011,484 | 50.2 (48.9, 51.4) | 18.4 (17.4, 19.4) | 31.5 (30.3, 32.6) | ||||
| Other substance use | |||||||||
| Cigarettei | 4.0 (3.7, 4.3) | <0.001 | 2,163,917 | 35.8 (34.9, 36.7) | <0.001 | 19.3 (18.5, 20.1) | <0.001 | 44.9 (44.1, 45.7) | <0.001 |
| Marijuanaj | 8.7 (8.0, 9.5) | <0.001 | 1,681,373 | 19.0 (18.0, 20.2) | <0.001 | 21.3 (20.1, 22.6) | <0.001 | 59.6 (58.2, 61.0) | <0.001 |
Notes: Boldface indicates statistical significance (p<0.05).
Used an opioid pain reliever without a prescription or use only for the experience or feeling it caused ≥1 time in the past 30 days.
Did not consume an alcoholic drink on any day in past 30 days, including lifetime abstainers.
Consumed ≥1 alcoholic drink on ≥1 day but did not consume ≥5 drinks (men) or ≥4 drinks (women), per occasion, on ≥1 day in the past 30 days.
Consumed ≥5 drinks (men) or ≥4 drinks (women), per occasion, on ≥1 day in the past 30 days.
Including Asian, American Indian, Alaskan Native, Native Hawaiian or other Pacific Islander, or more than one race or ethnicity.
Includes adults aged ≥18 years only.
Based on the “Rural/Urban Continuum Codes” developed in 2003 by the U.S. Department of Agriculture. Large metropolitan counties have a total population of 1 million or more. Small metropolitan counties have a total population of fewer than 1 million. Nonmetropolitan areas include counties in micropolitan statistical areas as well as counties outside of both metropolitan and micropolitan statistical areas.19
Respondents could indicate more than one type of health insurance. Public includes Medicaid, Medicare, Children’s Health Insurance Program (CHIP), CHAMPUS, TRICARE, CHAMPVA, the VA, or military health care.
Smoked part or all of a cigarette in the past 30 days.
Used marijuana or hashish in the past 30 days.
The prevalence of prescription opioid misuse was similar among non-drinkers (1.0%, 95% CI=0.9, 1.2) and current/non-binge drinkers (1.0%, 95% CI=0.9, 1.2), but was 3.5 times higher among binge drinkers (3.5%, 95% CI=3.3, 3.8; Table 2). This translates to an estimated 2.2 million binge drinkers engaging in prescription opioid misuse in the past 30 days. Across all sociodemographic groups, prescription opioid misuse was more common among binge drinkers than among non-drinkers and current/non-binge drinkers. Prescription opioid misuse was most common among non-drinkers aged 18–25 years (1.5%, 95% CI=1.3, 1.8) and 26–34 years (1.7%, 95% CI=1.4, 2.2), current/non-binge drinkers aged 12–17 years (3.6%, 95% CI=2.8, 4.7), and binge drinkers aged 12–17 years (8.1%, 95% CI=6.8, 9.7). However, about 1.4 million (65%) of the estimated 2.2 million binge drinkers, who reported misusing prescription opioids, were aged ≥26 years.
Table 2.
Prevalence of Past-30 Day Prescription Opioid Misusea by Drinking Pattern and by Characteristics
| Characteristics | Non-drinkersb (n=89,898) |
Current/non-binge drinkersc (n=30,296) |
Binge drinkersd (n=40,618) |
Weighted population of binge drinkers who misused prescription opioids |
|||
|---|---|---|---|---|---|---|---|
| Weighted % (95% CI) |
p- value |
Weighted % (95% CI) |
p- value |
Weighted % (95% CI) |
p- value |
N | |
| Overall | 1.0 (0.9, 1.2) | 1.0 (0.9, 1.2) | 3.5 (3.3, 3.8) | 2,179,386 | |||
| Sex | 0.060 | 0.197 | 0.385 | ||||
| Male | 1.2 (1.0, 1.4) | 1.1 (0.9, 1.5) | 3.6 (3.3, 3.9) | 1,319,366 | |||
| Female | 0.9 (0.8, 1.1) | 0.9 (0.8, 1.1) | 3.4 (3.1, 3.7) | 860,019 | |||
| Age group, years | <0.001 | <0.001 | <0.001 | ||||
| 12–17 | 1.1 (1.0, 1.3) | 3.6 (2.8, 4.7) | 8.1 (6.8, 9.7) | 120,781 | |||
| 18–25 | 1.5 (1.3, 1.8) | 2.1 (1.8, 2.5) | 4.7 (4.3, 5.2) | 639,454 | |||
| 26–34 | 1.7 (1.4, 2.2) | 1.7 (1.2, 2.3) | 4.4 (3.8, 5.1) | 625,088 | |||
| 35–49 | 1.2 (1.0, 1.5) | 1.1 (0.8, 1.4) | 3.0 (2.5, 3.5) | 511,513 | |||
| ≥50 | 0.6 (0.5, 0.9) | 0.6 (0.4, 0.9) | 1.8 (1.4, 2.4) | 282,550 | |||
| Race or ethnicity | 0.163 | 0.014 | 0.025 | ||||
| White, non-Hispanic | 1.1 (0.9, 1.2) | 1.0 (0.8, 1.2) | 3.5 (3.2, 3.8) | 1,485,165 | |||
| Black, non-Hispanic | 1.2 (0.9, 1.5) | 1.6 (1.1, 2.3) | 4.6 (3.7, 5.6) | 292,410 | |||
| Hispanic or Latino | 1.1 (0.9, 1.4) | 1.0 (0.7, 1.4) | 3.1 (2.6, 3.7) | 304,823 | |||
| Othere | 0.7 (0.5, 1.0) | 0.6 (0.4, 1.0) | 3.0 (2.2, 4.1) | 96,987 | |||
| Educationf | 0.306 | <0.001 | <0.001 | ||||
| Less than high school | 1.2 (0.9, 1.5) | 2.1 (1.5, 3.0) | 5.7 (4.8, 6.7) | 391,773 | |||
| High school graduate | 1.0 (0.9, 1.3) | 1.2 (0.9, 1.5) | 3.7 (3.2, 4.2) | 670,387 | |||
| Some college | 1.1 (0.9, 1.5) | 1.2 (0.9, 1.6) | 3.3 (2.9, 3.7) | 587,635 | |||
| College graduate | 0.8 (0.5, 1.2) | 0.6 (0.4, 1.0) | 2.3 (1.9, 2.8) | 408,810 | |||
| Family income (annual) | 0.004 | 0.007 | <0.001 | ||||
| <$20,000 | 1.4 (1.1, 1.6) | 1.7 (1.3, 2.3) | 5.1 (4.4, 5.8) | 575,338 | |||
| $20,000–<$50,000 | 1.1 (0.9, 1.3) | 1.2 (0.9, 1.7) | 3.8 (3.4, 4.3) | 710,241 | |||
| $50,000–<$75,000 | 1.0 (0.7, 1.4) | 0.7 (0.5, 1.0) | 3.0 (2.4, 3.6) | 309,855 | |||
| ≥$75,000 | 0.7 (0.5, 0.9) | 0.9 (0.7, 1.2) | 2.7 (2.3, 3.1) | 583,952 | |||
| Rural or urban statusg | <0.001 | 0.183 | 0.236 | ||||
| Large metropolitan | 1.1 (0.9, 1.3) | 1.1 (0.9, 1.4) | 3.4 (3.1, 3.7) | 1,163,677 | |||
| Small metropolitan | 1.3 (1.0, 1.5) | 0.9 (0.7, 1.2) | 3.8 (3.4, 4.4) | 712,754 | |||
| Nonmetropolitan | 0.6 (0.5, 0.8) | 0.8 (0.6, 1.1) | 3.4 (2.8, 4.0) | 302,955 | |||
| Health insuranceh | <0.001 | <0.001 | <0.001 | ||||
| Private | 0.8 (0.7, 1,0) | 0.9 (0.7, 1.0) | 2.6 (2.4, 2.9) | 1,103,411 | |||
| Public | 1.4 (1.2, 1.7) | 1.2 (0.8, 1.6) | 5.0 (4.2, 6.0) | 394,563 | |||
| Other | 0.6 (0.3, 1.0) | 2.2 (1.2, 4.0) | 4.0 (2.7, 5.9) | 59,998 | |||
| No coverage | 1.4 (1.2, 1.7) | 2.1 (1.5, 3.0) | 5.6 (4.9, 6.4) | 621,414 | |||
| Other substance use | |||||||
| Cigarettei | 2.6 (2.2, 3.0) | <0.001 | 3.1 (2.4, 3.9) | <0.001 | 5.6 (5.1, 6.0) | <0.001 | 1,348,826 |
| Marijuanaj | 6.6 (5.4, 7.9) | <0.001 | 6.6 (5.3, 8.3) | <0.001 | 10.1 (9.3, 11.1) | <0.001 | 1,166,856 |
Notes: Boldface indicates statistical significance (p<0.05).
Used an opioid pain reliever without a prescription or used only for the experience or feeling it caused ≥1 time in the past 30 days.
Did not consume an alcoholic drink on any day in past 30 days, including lifetime abstainers.
Consumed ≥1 alcoholic drink on ≥1 day but did not consume ≥5 drinks (men) or ≥4 drinks (women), per occasion, on ≥1 day in the past 30 days.
Consumed ≥5 drinks (men) or ≥4 drinks (women), per occasion, on ≥1 day in the past 30 days.
Including Asian, American Indian, Alaskan Native, Native Hawaiian or other Pacific Islander, or more than one race or ethnicity.
Includes adults aged ≥18 years only.
Based on the “Rural/Urban Continuum Codes” developed in 2003 by the U.S. Department of Agriculture. Large metropolitan counties have a total population of 1 million or more. Small metropolitan counties have a total population of fewer than 1 million. Nonmetropolitan areas include counties in micropolitan statistical areas as well as counties outside of both metropolitan and micropolitan statistical areas.19
Respondents could indicate more than one type of health insurance. Public includes Medicaid, Medicare, Children’s Health Insurance Program (CHIP), CHAMPUS, TRICARE, CHAMPVA, the VA, or military health care.
Smoked part or all of a cigarette in the past 30 days.
Used marijuana or hashish in the past 30 days.
Among binge drinkers, prescription opioid misuse was most common among black, non-Hispanic people (4.6%, 95% CI=3.7, 5.6; Table 2). Among binge drinkers, having no health insurance coverage (prevalence of prescription opioid misuse: 5.6%, 95% CI=4.9, 6.4) or having public health insurance (prevalence of prescription opioid misuse: 5.0%, 95% CI=4.2, 6.0) was also associated with a higher prevalence of prescription opioid misuse, whereas having private health insurance coverage was associated with a lower rate of prescription opioid misuse (2.6%, 95% CI=2.4, 2.9). The prevalence of prescription opioid misuse was inversely related to education and family income across all drinking categories, but was similar among males and females. Across all drinking categories, prescription opioid misuse was more common among those who used marijuana than those who smoked cigarettes. Prescription opioid misuse was also more common among binge drinkers who smoked cigarettes (5.6%, 95% CI=5.1, 6.0) or used marijuana (10.1%, 95% CI=9.3, 11.1) than among non-drinkers and current/non-binge drinkers who used these substances, respectively.
After adjusting for potential confounders, binge drinkers had 1.7 times greater odds (95% CI=1.5, 1.9, p-value <0.001) of reporting prescription opioid misuse than non-drinkers (Table 3). Current/non-binge drinking was not associated with prescription opioid misuse (AOR=1.0, 95% CI=0.8, 1.1, p-value=0.580).
Table 3.
Odds of Reporting Past-30 Day Prescription Opioid Misusea by Drinking Pattern and Characteristics
| Drinking pattern and characteristics | Unadjusted ORs | AORse | ||
|---|---|---|---|---|
| OR (95% CI) | p-value | AOR (95% CI) | p-value | |
| Drinking pattern | ||||
| Non-drinkingb | ref | ref | ||
| Current drinking/non-bingec | 1.0 (0.8, 1.2) | 0.869 | 1.0 (0.8, 1.1) | 0.580 |
| Binge drinkingd | 3.4 (3.0, 3.9) | <0.001 | 1.7 (1.5, 1.9) | <0.001 |
| Sex | ||||
| Male | 1.3 (1.2, 1.5) | <0.001 | 1.0 (0.9, 1.2) | 0.871 |
| Female | ref | ref | ||
| Age group, years | ||||
| 12–17 | 2.1 (1.7, 2.7) | <0.001 | 2.2 (1.7, 2.8) | <0.001 |
| 18–25 | 3.8 (3.1, 4.6) | <0.001 | 1.7 (1.4, 2.1) | <0.001 |
| 26–34 | 3.5 (2.8, 4.5) | <0.001 | 2.0 (1.6, 2.6) | <0.001 |
| 35–49 | 2.1 (1.7, 2.7) | <0.001 | 1.6 (1.3, 2.1) | <0.001 |
| ≥50 | ref | ref | ||
| Race or ethnicity | ||||
| White, non-Hispanic | 1.6 (1.3, 2.0) | <0.001 | 1.4 (1.1, 1.8) | <0.01 |
| Black, non-Hispanic | 1.9 (1.4, 2.5) | <0.001 | 1.5 (1.1, 2.1) | <0.01 |
| Hispanic or Latino | 1.5 (1.2, 2.0) | <0.01 | 1.3 (1.0, 1.8) | <0.05 |
| Otherf | ref | ref | ||
| Family income (annual) | ||||
| <$20,000 | 1.8 (1.5, 2.2) | <0.001 | 1.3 (1.1, 1.5) | <0.01 |
| $20,000–<$50,000 | 1.4 (1.2, 1.6) | <0.001 | 1.2 (1.0, 1.4) | 0.111 |
| $50,000–<$75,000 | 1.1 (0.9, 1.3) | 0.332 | 1.0 (0.8, 1.2) | 0.993 |
| ≥$75,000 | ref | ref | ||
| Rural or urban statusg | ||||
| Large metropolitan | 1.3 (1.1, 1.6) | <0.01 | 1.3 (1.1, 1.6) | <0.01 |
| Small metropolitan | 1.4 (1.2, 1.7) | <0.001 | 1.4 (1.2, 1.6) | <0.001 |
| Nonmetropolitan | ref | ref | ||
| Other substance use | ||||
| Cigaretteh | 4.1 (3.7, 4.5) | <0.001 | 2.1 (1.9, 2.4) | <0.001 |
| Marijuanai | 8.8 (7.8, 10.0) | <0.001 | 4.6 (4.0, 5.3) | <0.001 |
Notes: Boldface indicates statistical significance (p<0.05).
Used an opioid pain reliever without a prescription or used only for the experience or feeling it caused ≥1 time in the past 30 days.
Did not consume an alcoholic drink on any day in past 30 days, including lifetime abstainers.
Consumed ≥1 alcoholic drink on ≥1 day but did not consume ≥5 drinks (men) or ≥4 drinks (women), per occasion, on at ≥1 day in the past 30 days.
Consumed ≥5 drinks (men) or ≥4 drinks (women), per occasion, on ≥1 day in the past 30 days.
Multivariable logistic regression models adjusted for sex, age group, race or ethnicity, total annual family income, rural or urban status, cigarette use, and marijuana use.
Including Asian, American Indian, Alaskan Native, Native Hawaiian or other Pacific Islander, or more than one race or ethnicity.
Based on the “Rural/Urban Continuum Codes” developed in 2003 by the U.S. Department of Agriculture. Large metropolitan counties have a total population of 1 million or more. Small metropolitan counties have a total population of fewer than 1 million. Nonmetropolitan areas include counties in micropolitan statistical areas as well as counties outside of both metropolitan and micropolitan statistical areas.19
Smoked part or all of a cigarette in the past 30 days.
Used marijuana or hashish in the past 30 days.
The overall prevalence of prescription opioid misuse increased significantly with the frequency of binge drinking (p-value <0.001), ranging from 2.4% (95% CI=2.2, 2.7) among those who reported binge drinking one to two times during the past 30 days to 6.5% (95% CI=5.6, 7.6) among those who reported binge drinking ten or more times (Figure 1). When stratified by age group, the prevalence of presciption opioid misuse increased significantly with the frequency of binge drinking among those aged 12–49 years (p-value <0.001), as well as among adults aged ≥50 years (p-value=0.04). Among adults aged ≥50 years, the prevalence of opioid misuse was similar for those who reported either binge drinking five to nine times (3.2%, 95% CI=1.8, 5.5) or ten or more times (2.8%, 95% CI=1.5, 5.0) during the previous 30 days.
Figure 1.
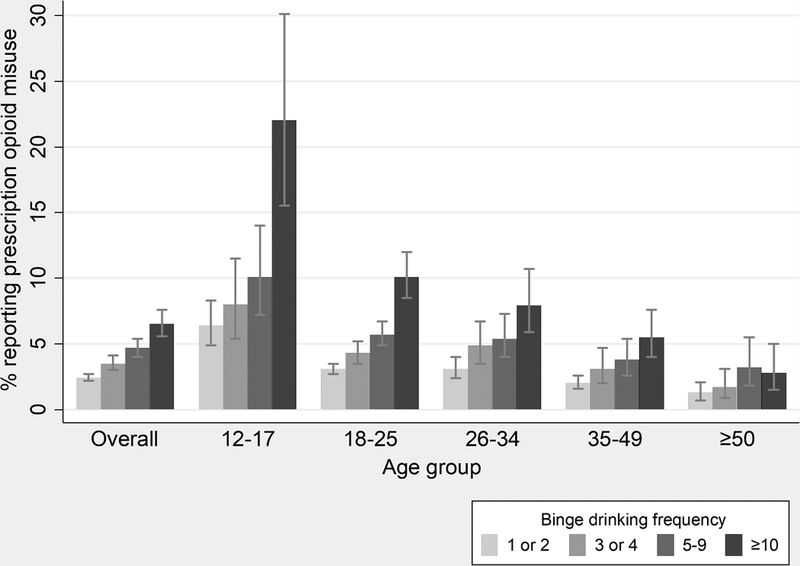
Prevalence and 95% CIa of past 30-day prescription opioid misuseb by age group and binge drinking frequencyc among binge drinkers.
a95% CIs denoted by bracketed lines on each bar.
bUsed a prescription opioid without a prescription or used only for the experience or feeling it caused ≥1 time in the past 30 days.
cNumber of days consuming ≥5 drinks (men) or ≥4 drinks (women), per occasion, in the past 30 days.
DISCUSSION
The results of this study indicate that more than half (2.2 million) of the estimated 4.2 million adolescents and adults who reported past 30-day misuse of prescription opioids during 2012–2014 were binge drinkers. Binge drinkers had nearly twice the odds of misusing prescription opioids compared with non-drinkers, even after controlling for other factors that could affect the relationship between binge drinking and prescription opioid misuse. Prescription opioid misuse was most common among youth aged 12–17 years who binge drank, but about 1.4 million (65%) of the estimated 2.2 million binge drinkers who reported prescription opioid misuse were aged 26 years or older. The prevalence of prescription opioid misuse increased with the frequency of binge drinking, particularly among youth and young adults.
Across drinking categories, this study generally did not find differences in the prevalence of prescription opioid misuse by sex or by rural or urban status. However, among binge drinkers, this study found a higher prevalence of prescription opioid misuse among those with lower levels of education, lower household incomes, and those who were either covered by publicly funded health insurance or were uninsured. This finding is consistent with the findings of other research that has shown that prescription opioid misuse is generally more common among low-income populations, including those on Medicaid.26 It is also consistent with a recent study showing that binge drinkers with lower household incomes consume significantly more total binge drinks per binge drinker annually than those with higher household incomes (532.3 drinks versus 419.0 drinks, respectively).13 However, people with higher household incomes (e.g., $75,000 or more) have a higher prevalence of binge drinking than those with lower household incomes (less than $25,000), underscoring the importance of addressing binge drinking among the entire population.13
The finding that the prevalence of prescription opioid misuse generally increased with binge drinking frequency is consistent with literature showing that the likelihood of engaging in alcohol-related health risk behaviors increases with the number of binge drinking occasions. For example, a study of U.S. high school students found a positive relationship between binge drinking frequency and use of other drugs, including tobacco, marijuana, cocaine, and inhalants (prescription opioid misuse was not assessed).27
Adult binge drinkers tend to binge about once a week on average and consume an average of seven drinks per binge,13 and people who misuse prescription opioids also report doing so about once a week (an average of 54 days a year).7 This is concerning given that the risk of a dangerous interaction between alcohol and opioids is likely to be greatest among those who are misusing opioids and binge drinking frequently and at high intensity.
The odds of prescription opioid misuse among binge drinkers being nearly twice that of non-drinkers suggests the importance of population-level policies to reduce binge drinking. The U.S. Community Preventive Services Task Force recommends several effective strategies for reducing binge drinking, including increasing alcohol taxes,28 regulating the density of alcohol outlets,29 and having commercial host liability laws.30 In addition, the U.S. Preventive Services Task Force recommends screening and brief intervention for adults as a strategy to reduce excessive alcohol use.31 This intervention may also be effectively administered electronically (also known as e–screening and brief intervention) using computers, tablets, smartphones, and other electronic tools in a variety of settings (e.g., primary care clinics, health departments, and on college campuses).32 Effective strategies to reduce overdoses involving prescription opioids includeexpanding safe, evidence-based pain treatment and decreasing excessive prescribing that may leave unused opioids available for potential misuse, safe prescribing practices, as described in the Centers for Disease Control and Prevention Guideline for Prescribing Opioids for Chronic Pain,33 as well as strategies to prevent and treat opioid use disorder,34 and reverse opioid overdoses.35
Finally, the 2015–2020 U.S. Dietary Guidelines for Americans indicate that some people should not drink at all, including those who are taking medications that could interact with alcohol, as well as youth under age 21 years and women who are pregnant or might be pregnant.36 The U.S. Food and Drug Administration has also advised healthcare professionals to avoid prescribing opioids to patients using alcohol or other central nervous system depressants.17 Therefore, adult drinkers aged 21 years or older should only do so in moderation (i.e., consume up to one drink per day for women and up to two drinks per day for men), or not drink at all, particularly while taking prescription opioids.17,36
Future research examining the relationship between evidence-based alcohol policies (e.g., increasing alcohol taxes28 and regulating the density of alcohol outlets30), total binge drinks per binge drinker, and the risk of opioid overdoses in states could help guide the prevention of opioid misuse and opioid overdoses involving alcohol. In addition, future research could assess whether improved opioid prescribing could also help reduce opioid misuse and opioid overdoses involving alcohol. In addition, future research could assess whether improved opioid prescribing could also help reduce opioid misuse and opioid overdoses involving alcohol.
Limitations
This study has limitations. First, this study was not able to examine whether alcohol and opioids were used concurrently. Second, data were based on self-reports, and therefore, both prescription opioid misuse and alcohol consumption (particularly binge drinking) are likely to have been underreported. However, the NSDUH audio computer-assisted self-interview process assesses the internal consistency of responses, which has been shown to improve the sensitivity of NSDUH estimates of binge drinking among adults.37 Third, because this study was focused on the misuse of prescription opioids, it did not consider the use of illicit opioids, such as heroin and illicitly manufactured fentanyl, which has been increasing,38 including among people who binge drink and people who misuse prescription opioids.39
CONCLUSIONS
Binge drinking is associated with prescription opioid misuse, and the prevalence of prescription opioid misuse increased with the frequency of binge drinking. Binge drinkers who misuse prescription opioids are likely to be at substantially increased risk of overdose because of the combined effect of high blood alcohol levels and prescription opioids on the central nervous system.17 The high prevalence, frequency, and intensity of binge drinking among adults and adolescents in the U.S.,13,40 along with the heightened prevalence of prescription opioid misuse among binge drinkers, emphasizes the importance of adopting a comprehensive and coordinated approach to addressing both binge drinking and prescription opioid misuse to reduce the risk of opioid overdoses.
ACKNOWLEDGMENTS
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or HHS. MB Esser conceptualized the study and led the drafting of the article. G Guy led the data analysis. K Zhang assisted with the data analysis and presentation of the results. RD Brewer drafted sections of the article. All authors contributed to the interpretation of the findings, reviewed and edited drafts of the article, and approved the final version.
Footnotes
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Seth P, Scholl L, Rudd RA, Bacon S. Overdose deaths involving opioids, cocaine, and psychostimulants - United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67(12):349–358. 10.15585/mmwr.mm6712a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC. Wide-ranging Online Data for Epidemiologic Research (WONDER). http://wonder.cdc.gov Published 2016. Accessed December 13, 2017.
- 3.CDC. Annual surveillance report of drug-related risks and outcomes — United States, 2017. Surveillance Special Report 1. CDC, HHS; www.cdc.gov/drugoverdose/pdf/pubs/2017-cdc-drug-surveillance-report.pdf Published August 31, 2017. Accessed March 1, 2018. [Google Scholar]
- 4.Guy GP Jr., Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697–704. 10.15585/mmwr.mm6626a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Florence CS, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54(10):901–906. 10.1097/MLR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.HHS. HHS Acting Secretary Declares Public Health Emergency to Address National Opioid Crisis. www.hhs.gov/about/news/2017/10/26/hhs-acting-secretary-declares-public-health-emergency-address-national-opioid-crisis.html Published October 26, 2017. Accessed March 1, 2018.
- 7.Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003–2013. JAMA. 2015;314(14):1468–1478. 10.1001/jama.2015.11859. [DOI] [PubMed] [Google Scholar]
- 8.Bohnert AS, Logan JE, Ganoczy D, Dowell D. A detailed exploration into the association of prescribed opioid dosage and overdose deaths among patients with chronic pain. Med Care. 2016;54(5):435–441. 10.1097/MLR.0000000000000505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lanier WA, Johnson EM, Rolfs RT, Friedrichs MD, Grey TC. Risk factors for prescription opioid-related death, Utah, 2008–2009. Pain Med. 2012;13(12):1580–1589. 10.1111/j.1526-4637.2012.01518.x. [DOI] [PubMed] [Google Scholar]
- 10.CDC. Emergency department visits involving nonmedical use of selected prescription drugs – United States, 2004–2008. MMWR Morb Mortal Wkly Rep. 2010;59(23):705–709. [PubMed] [Google Scholar]
- 11.Back SE, Payne RL, Simpson AN, Brady KT. Gender and prescription opioids: findings from the National Survey on Drug Use and Health. Addict Behav. 2010;35(11):1001–1007. 10.1016/j.addbeh.2010.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCabe SE, Cranford JA, Boyd CJ. The relationship between past-year drinking behaviors and nonmedical use of prescription drugs: prevalence of co-occurrence in a national sample. Drug Alcohol Depend. 2006;84(3):281–288. 10.1016/j.drugalcdep.2006.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanny D, Naimi TS, Liu Y, Lu H, Brewer RD. Annual total binge drinks consumed by U.S. adults, 2015. Am J Prev Med. 2018;54(4):486–496. 10.1016/j.amepre.2017.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han B, Compton WM, Blanco C, et al. Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 National Survey on Drug Use and Health. Ann Intern Med. 2017;167(5):293–301. 10.7326/M17-0865. [DOI] [PubMed] [Google Scholar]
- 15.Jones CM, Paulozzi LJ, Mack KA. Alcohol involvement in opioid pain reliever and benzodiazepine drug abuse-related emergency department visits and drug-related deaths - United States, 2010. MMWR Morb Mortal Wkly Rep. 2014;63(40):881–885. [PMC free article] [PubMed] [Google Scholar]
- 16.White AM, Hingson RW, Pan IJ, Yi HY. Hospitalizations for alcohol and drug overdoses in young adults ages 18–24 in the United States, 1999–2008: results from the Nationwide Inpatient Sample. J Stud Alcohol Drugs. 2011;72(5):774–786. 10.15288/jsad.2011.72.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Food and Drug Administration. FDA Drug Safety Communication: FDA warns about serious risks and death when combining opioid pain or cough medicines with benzodiazepines; requires its strongest warning. www.fda.gov/Drugs/DrugSafety/ucm518473.htm Published 2016. Accessed July 3, 2017.
- 18.Levine B, Caplan YH. Pharmacology and toxicology of ethyl alcohol In: Caplan YH, Goldberger BA, editors. Garriott’s Medicolegal Aspects of Alcohol - Sixth Edition Tucson, AZ: Lawyers & Judges Publishing Company, Inc; 2015. [Google Scholar]
- 19.van der Schrier R, Roozekrans M, Olofsen E, et al. Influence of ethanol on oxycodone-induced respiratory depression: a dose-escalating study in young and elderly individuals. Anesthesiology. 2017;126(3):534–542. 10.1097/ALN.0000000000001505. [DOI] [PubMed] [Google Scholar]
- 20.Kandel DB, Hu MC, Griesler P, Wall M. Increases from 2002 to 2015 in prescription opioid overdose deaths in combination with other substances. Drug Alcohol Depend. 2017;178:501–511. 10.1016/j.drugalcdep.2017.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gudin JA, Mogali S, Jones JD, Comer SD. Risks, management, and monitoring of combination opioid, benzodiazepines, and/or alcohol use. Postgrad Med. 2013;125(4):115–130. 10.3810/pgm.2013.07.2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Center for Behavioral Health Statistics and Quality. 2014 National Survey on Drug Use and Health: Methodological summary and definitions. www.samhsa.gov/data/sites/default/files/NSDUH-MethodSummDefs2014/NSDUH-MethodSummDefs2014.htm Published 2015. Accessed February 28, 2019.
- 23.Jarlenski M, Barry CL, Gollust S, et al. Polysubstance use among U.S. women of reproductive age who use opioids for nonmedical reasons. Am J Public Health. 2017;107(8):1308–1310. 10.2105/AJPH.2017.303825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arterberry BJ, Horbal SR, Buu A, Lin HC. The effects of alcohol, cannabis, and cigarette use on the initiation, reinitiation and persistence of non-medical use of opioids, sedatives, and tranquilizers in adults. Drug Alcohol Depend. 2016;159:86–92. 10.1016/j.drugalcdep.2015.11.029. [DOI] [PubMed] [Google Scholar]
- 25.Olfson M, Wall MM, Liu SM, Blanco C. Cannabis use and risk of prescription opioid use disorder in the United States. Am J Psychiatry. 2018;175(1):47–53. 10.1176/appi.ajp.2017.17040413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Song Z Mortality quadrupled among opioid-driven hospitalizations, notably within lower-income and disabled white populations. Health Aff (Millwood). 2017;36(12):2054–2061. 10.1377/hlthaff.2017.0689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller JW, Naimi TS, Brewer RD, Jones SE. Binge drinking and associated health risk behaviors among high school students. Pediatrics. 2007;119(1):76–85. 10.1542/peds.2006-1517. [DOI] [PubMed] [Google Scholar]
- 28.Elder RW, Lawrence B, Ferguson A, et al. The effectiveness of tax policy interventions for reducing excessive alcohol consumption and related harms. Am J Prev Med. 2010;38(2):217–229. 10.1016/j.amepre.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campbell CA, Hahn RA, Elder R, et al. The effectiveness of limiting alcohol outlet density as a means of reducing excessive alcohol consumption and alcohol-related harms. Am J Prev Med. 2009;37(6):556–569. 10.1016/j.amepre.2009.09.028. [DOI] [PubMed] [Google Scholar]
- 30.Rammohan V, Hahn RA, Elder R, et al. Effects of dram shop liability and enhanced overservice law enforcement initiatives on excessive alcohol consumption and related harms two community guide systematic reviews. Am J Prev Med. 2011;41(3):334–343. 10.1016/j.amepre.2011.06.027. [DOI] [PubMed] [Google Scholar]
- 31.Moyer VA, Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159(3):210–218. 10.7326/0003-4819-159-3-201308060-00652. [DOI] [PubMed] [Google Scholar]
- 32.Tansil KA, Esser MB, Sandhu P, et al. Alcohol electronic screening and brief intervention: a Community Guide systematic review. Am J Prev Med. 2016;51(5):801–811. 10.1016/j.amepre.2016.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain - United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- 34.Substance Abuse and Mental Health Services Administration. SAMHSA Opioid Overdose Prevention Toolkit. HHS Publication No. (SMA) 16–4742 2016. https://store.samhsa.gov/product/Opioid-Overdose-Prevention-Toolkit/SMA18-4742 . Accessed August 7, 2018. [Google Scholar]
- 35.National Institute on Drug Abuse. Opioid Overdose Reversal with Naloxone (Narcan, Evzio). www.drugabuse.gov/related-topics/opioid-overdose-reversal-naloxone-narcan-evzio Published 2018. Accessed August 7, 2018.
- 36.HHS, U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th Edition http://health.gov/dietaryguidelines/2015/guidelines Published 2015. Accessed January 7, 2016. [Google Scholar]
- 37.Miller JW, Groferer JC, Brewer RD, et al. Prevalence of adult binge drinking: a comparison of two national surveys. Am J Prev Med. 2004;27(3):197–204. 10.1016/j.amepre.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 38.O’Donnell JK, Gladden RM, Seth P. Trends in deaths involving heroin and synthetic opioids excluding methadone, and law enforcement drug product reports, by Census region - United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(34):897–903. 10.15585/mmwr.mm6634a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jones CM, Logan J, Gladden RM, Bohm MK. Vital signs: demographic and substance use trends among heroin users - United States, 2002–2013. MMWR Morb Mortal Wkly Rep. 2015;64(26):719–725. [PMC free article] [PubMed] [Google Scholar]
- 40.Esser MB, Clayton H, Demissie Z, Kanny D, Brewer RD. Current and binge drinking among high school students - United States, 1991–2015. MMWR Morb Mortal Wkly Rep. 2017;66(18):474–478. 10.15585/mmwr.mm6618a4. [DOI] [PMC free article] [PubMed] [Google Scholar]


