Abstract
[Purpose] The purpose of this review is to compare the effect of McKenzie and stabilization exercises in reducing pain and disability in individuals with chronic nonspecific low back pain. [Methods] A systematic literature review of randomized controlled trials (RCTs) were performed using 6 databases. The quality of reviewed articles were assessed by the risk of bias using the Cochrane collaboration’s tool. [Results] A total of 829 articles were found from the databases, of which 10 were finally selected to be included in this review. The overall risk of bias assessment indicated that the risk of bias was low in one study and high in the other nine studies. One study reported reduced pain and two studies reported reduced functional disability in the McKenzie exercise group compared to other exercises. Two studies reported reduced pain and three studies reported reduced functional disability in the stabilization exercise group compared to other exercises. In two studies, the stabilization exercise group was as effective as McKenzie exercise group in reducing pain and functional disability in patients with chronic nonspecific low back pain. [Conclusion] Only two studies compared stabilization and McKenzie exercises in the management of chronic nonspecific low back pain. Therefore, insufficient evidence is available to draw any conclusive comparison on the effects of McKenzie and stabilization exercises in chronic nonspecific low back pain. However, both McKenzie and stabilization exercises was better than conventional exercise programs in reducing functional disability in patients with chronic nonspecific low back pain.
Keywords: Low back pain, McKenzie exercises, Stabilization exercises
INTRODUCTION
Low Back Pain (LBP) is considered as one of the commonest problems, in which pain felt in the lumbosacral spinal and paraspinal regions which encompass the buttocks and upper thigh1). LBP is one of most common medical problems that lead to absence from work, the disability arising from this pain resulting in significant economic impact2). In addition, LBP can lead to activity restrictions such as carrying objects, sitting or standing for a long time, twisting and squatting, which can result in participation limitation (work, recreation activities, family and community) and functional disability3). A previous systematic review4) reported the point prevalence of LBP is estimated at 21−33% and 22–65% for one-year prevalence. It has been reported that lifetime prevalence of low back pain globally is as high as 84%5). Homaid et al.6) reported that global prevalence of LBP is 45% in Saudi Arabia, and the prevalence of LBP is estimated to be 18%. Heyman and Dekel7) stated that back pain problems occur more in adults and detailed that the frequency of low back pain amongst females is more than males and increases with age across both genders.
Previous study defined chronic low back pain (CLBP) as a “back pain problem that has persisted for at least three months and has resulted in pain on at least half the days in the past 6 months”8). Only few cases of CLBP have specific causes of pain and they are defined as symptoms caused by a known pathophysiologic mechanism, for instance infection, herniated nuclei pulposus, rheumatoid arthritis, osteoporosis, tumor or fracture9,10,11). However, patients in the other group with no specific pathophysiologic mechanism are commonly known as “nonspecific LBP”12). Many clinical guidelines reported that patients can control and deal with chronic LBP by patient instruction and help with self-care13,14,15,16). Moreover, there was strong emphasis on encouraging patients to be active partners in the treatment of their health situation, for instance, during instruction and exercise programmes17). However, treatment that focuses on exercise and education instead of medication is amongst the best of treatments18). Furthermore, active rehabilitation programmes can help in enhancing body function, decreasing pain, reducing disability, improving walking and self-efficacy19, 20). Although there are many methods to treat or manage chronic low back pain (CLBP), the current study bases its focus on two methods.
The first is McKenzie exercises, devised by Robin McKenzie21), also known as diagnostic and mechanical therapy22). This is a common method used among physiotherapists as a treatment method for handling back pain23). Additionally, Kuppusamy et al.3) reported that the McKenzie exercises are considered to be frequently used by physiotherapists in the treatment of LBP. Improvement in symptoms is successively measured in terms of ‘centralization’, a phenomenon that has been commonly used24). It combines recurrent end range actions by examination; the classification of direction for exercise is contingent upon the patient’s response to those recurring actions. Posture correction ensuring the maintaining of the correction is a vital characteristic of the McKenzie exercise3).
The second method is stabilization exercises because the decrease in spinal stability it is one of the major causes of recurrent LBP25). As a result, there is more emphasis on training the localized stabilizer muscles; transverse abdominis (TrA) and multifidus muscles (MF)26). Moreover, people with CLBP are more likely to have inadequate control in TrA muscles and atrophy has been found in the MF muscle27). The main goals of the stabilization exercises are deep motor control of deep trunk muscles (TrA and MF) restoration and increase in thickness of these stabilizer muscles that result in improved spine stability27). A study was carried out by O’Sullivan et al.28) on patients with CLBP and showed that the pain intensity in patients in receipt of TrA and MF muscle training for 10 weeks decreased and that functional disability, in turn, improved.
The current systematic review aimed to assess the efficacy of the McKenzie exercises in comparison with the stabilization exercises in individuals with chronic nonspecific low back pain by systematically and critically assessing the research evidence.
METHODS
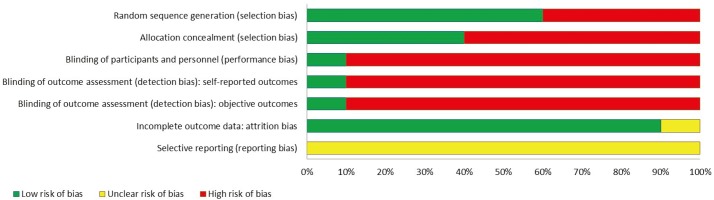
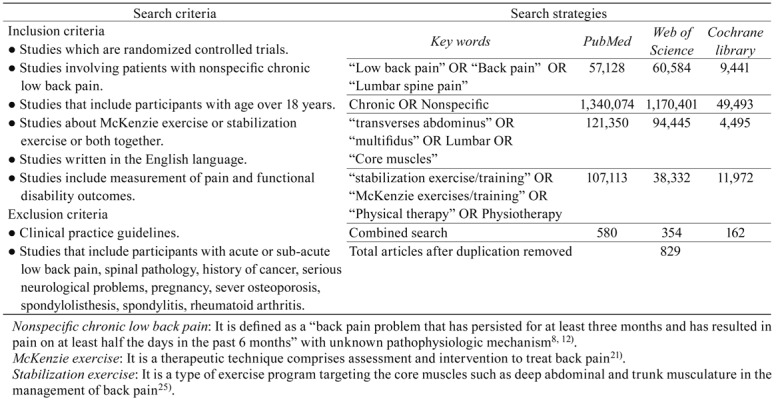
Six databases were used to attain high quality resources, guarantee the dependability and check the rationality of studies and references found. Moreover, the use of these databases is crucial as they contain health and social care and medical journals. These databases include Web of Science, PubMed/ MEDLINE, Cochrane Library online, National Rehabilitation Information Centre (NARIC), ProQuest Medical Library, and PEDro during the period from its inception to current date. Search terms and Boolean operators that are utilized by the author are “chronic” AND “nonspecific” AND “low back pain” OR “lumbar spine” AND “stabilization” OR/AND “McKenzie” AND “exercise” OR “method” OR “training” OR “therapy” AND “transverses abdominus” AND “multifidus”. Search strategies for three databases including PubMed, Web of Science, and Cochrane library were given in Table 1 . All the articles that have been selected depend on the following specific inclusion and exclusion criteria (Table 1). Two reviewers participated All studies that have been selected in this literature review are RCTs. The risk of bias was evaluated with the Cochrane collaboration’s tool. The allocation concealment, sequence generation, blinding, absence of selective outcome reporting, and completeness of outcome data domains were assessed. Risk of bias was indicated as low, high, and unclear in each domain.
Table 1. Search strategies and criteria.
RESULTS
A total of 829 articles were identified in the title search after excluding the duplicates (n=407) (Fig. 1). A total of 10 articles were included in this qualitative review. Table 2 details the study characteristics. All 10 studies are RCTs; additionally, all of these trials target people that have chronic nonspecific low back pain. All of them are comparison trials that compared McKenzie exercise with other kinds of exercises, compare stabilization with other kinds of treatments and compare McKenzie exercise with stabilization. For instance, there are five studies which compared McKenzie exercise with other sorts of exercises, such as Back School exercise, mat-based Pilates, intensive strengthening training, manual therapy and electrophysical methods3, 29,30,31,32), while two studies compared McKenzie exercise with stabilization exercise33, 34). Furthermore, three studies compared stabilization exercise to other types of exercises. For instance, dynamic strengthening exercises for lumbar region, stretching and general exercise27, 35, 36).
Fig. 1.
Results and process of literature search.
Table 2. Study characteristics.
| Study design | Participants | Interventions | Outcome | Findings | |
|---|---|---|---|---|---|
| Muretzani et al. (2015)32) | Assessor blinded RCT | N=271 Inclusion criteria: Aged between 18–56 years, chronic nonspecific low back pain |
Group 1 (n=134): McKenzie therapy. Exercises repeated
five times per day, 10 to 15 repetitions; participants got seven sessions
treatment as maximum. Session lasted to 10 hours. Group 2 (n=137): Electro-physical agents (EPAs) treatment for four weeks. |
VAS ODQ FTF ROM |
Although the findings between two groups stated that there is significant improvement between both groups, improvement in McKenzie group was more than EPAs group in all the parameters. |
| Garcia et al. (2013)31) | Assessor blinded RCT | N=148 Inclusion criteria: Aged between 18 and 80 years, nonspecific chronic low back pain |
Group 1 (n=74): McKenzie method. Patients were
provided with information regarding spinal care and asked to do specific exercises
according to movement preference direction movement. Group 2 (n=74): Treatment in this group depends on exercise programme in order to enhance mobility, strength and flexibility. |
NRS RMDQ ROM WHOQOL-BREF |
There is no significant difference between groups in pain intensity. However, there is important improvement in disability in McKenzie but not in pain. |
| Moon et al. (2013)36) | Assessor blinded RCT | N=24 Inclusion criteria: Nonspecific chronic LBP |
Group 1 (n=12): Lumber stabilization exercises.
Comprised of 16 exercises, intended to reinforce the deep lumbar stabilizing
muscles. Group 2 (n=12): Conventional lumber dynamic strengthening exercise. comprised of 14 exercises, which triggered the extensor (erector spinae) and flexor (rectus abdominis) muscle groups. |
VAS ODQ |
Pain reduced considerably after treatment; although, the variations were not notably altered between the groups. Disability enhanced notably in the stabilization exercise group only. |
| Hosseinifar et al. (2013)34) | Assessor blinded RCT | N=30 Inclusion criteria: Patients aged between 18–50 and chronic low back pain with or without leg pain. |
Group 1 (n=15): Stabilization exercises. Patients
asked to do stabilization exercises in six steps: Group 2 (n=15): McKenzie Exercise. Individuals were requested to carry out six exercises: four extension-type exercises and two flexion-type exercises. |
VAS FRI |
After interventions, the pain score reduced in the two groups. The disability score reduced, but only in the stabilization group. |
| Franca et al. (2012)27) | Assessor blinded RCT | N=30 Inclusion criteria: Chronic LBP |
Group 1 (n=15): Segmental stabilisation exercise (SS).
Concentrated on the TrA and LM muscles. Group 2 (n=15): Muscular stretching exercises (ST). Focused on erector spinae (ES), hamstring (HS), and triceps surae (TS) muscles stretching and connective tissues posterior to column were conducted. |
VAS MPQ ODQ |
As compared with baseline, the two treatments were essential in relieving pain and bettering disability. Those in the SS group had expressively higher gains for all variables. |
| Paatelma et al. (2008)30) | RCT | N=134 Inclusion criteria: Aged between 18–65 years, employed people with non-specific low back pain. |
Group 1 (n=45): Orthopedic manual therapy. Patients
received three techniques of treatment such as spinal manipulation, specific
mobilization, and muscle stretching. Group 2 (n=52): McKenzie method. Treatment includes an educational module supported with book (year book on back) and an active therapy section, which delivered instructions in exercises repeated several times a day. Group 3 (n=37): Advice only. Patients received 45–60 min counselling from a physiotherapist concerning the good prognosis for LBP. |
VAS RMDQ |
At the 3-month follow-up, substantial improvements were observed in all groups. However, no significant differences were noted between the groups. At the 6-month follow-up, greater improvement was observed in the McKenzie group compared to the advice only group. At 1-year follow-up, the McKenzie group were noted to have had a better disability index than the advice only group. |
| Miller et al. (2005)33) | RCT | N=30 Inclusion criteria: Chronic low back pain. |
Group 1 (n=15): McKenzie Exercises. Participants
allocated to this group acquired treatment founded on their history and reaction
to the recurrent movement examination after the completion of the McKenzie exam. Group 2 (n=15): Stabilization Exercises. These concentrated on reinforcing the lumbar multifidus and transversus abdominis muscles through performance of a lower abdominal contraction. |
Short-Form MPQ FSQ |
The stabilization group portrayed a statistically
noteworthy enhancement in pain results. The McKenzie group did better in the
current pain index of the SF-MPQ only (p<0.05). Between-group comparisons of alterations in the dependent variable scores showed no statistical alterations between the groups. |
| Koumantakis et al. (2005)35) | Assessor blinded RCT | N=55 Inclusion criteria: Recurrent LBP, Nonspecific LBP |
Group 1 (n=29) Stabilisation and general exercises
group Group 2 (n=26) General exercises only. |
MPQ RMDQ PSEQ TSK PLCS |
There are differences between groups. All of them were improved in pain and disability. |
| Peterson et al. (2002)29) | Assessor blinded RCT | N=230 Inclusion criteria: Low back pain with or without leg pain, aged between 18–60 years, chronic low back pain. |
Group 1 (n=132): McKenzie treatment. Consisted of an
initial physical assessment, followed by self-mobilizing repetitive activities or
sustained positions performed in specific directions, the application of manual
overpressure, and/or mobilization by the physiotherapist. Group 2 (n=128): The strengthening training. Involved 5–10 minutes on a fixed bike followed by 10 minutes of warm up exercises of low intensity for the lumbopelvic muscles. |
MLBPRS | The effectiveness of the McKenzie treatment equaled
that of intensive strengthening training in reducing incapacity and intensity of
pain. However, the McKenzie treatment has some potential, compared to strength training in the treatment of chronic low back pain. |
| Kuppusamy et al. (2013)3) | Assessor blinded RCT | N=30 Inclusion criteria: Aged between 20–65-year chronic low back pain. |
Group 1 (n=15): McKenzie Exercise. After examination,
patients were allocated according to one of four symptom classifications. Group 2 (n=15): Mat Based Pilates Exercise. These exercises were performed in six to 10 repetitions with progressive difficulty if needed and stretches were held for 30 seconds. |
NRS RMDQ ROM |
No significant difference observed between groups and there is improvement in both groups in terms of pain, disability and trunk flexion and trunk extension. |
VAS: Visual analogue scale; ODQ: Oswestry Disability Questionnaire (OSW); FTF: Fingertip-to-Floor Disability; ROM: Range of Motion; NRS: Numerical rating scale; RMDQ: Roland-Morris Disability Questionnaire; WHOQOL-BREF: World Health Organization Quality of Life-BREF; FRI: Functional Rating Index; MPQ: McGill pain Questionnaire; FSQ: Functional Status Questionnaire; SLR: Straight Leg Raising; PSEQ: Pain Self-Efficacy Questionnaire; TSK: Tampa Scale of Kinesiophobia; PLCS: Pain Locus of Control Scale; TrA: Tranverse abdominis; MF: Multifidus; MLBPRS: Manniche’s Low Back Pain Rating Scale.
According to all research that was selected in this review, the outcome measures are the same (Pain intensity and Functional disability). However, the outcome measure tools are different; for example, for pain there are four types of tools (Visual Analogue Scale (VAS), Numeric Rating Scale (NRS), Mannich Low Back Pain Rating Scale and McGill Pain Questionnaire (MPQ) and four kinds for disability (Roland Morris Disability Questionnaire (RMDQ), Oswestry Disability Questionnaire (ODQ), Functional Rating Index (FRI) and Functional status Questionnaire (FSQ).
All the 10 included trials in this review have clear concentrated questions; in addition, clear objectives are reported in these trials. Moreover, all the outcome measures utilized in these selected studies are valid and reliable and all of them were ethically agreed. According to the variance, statistical power, consequence of size and pre-test significance, suitable sample size is assumed to be considered37). In the current study, five out of the 10 studies selected in this review have small sample size according to each study’s author3, 27, 31, 33, 36).
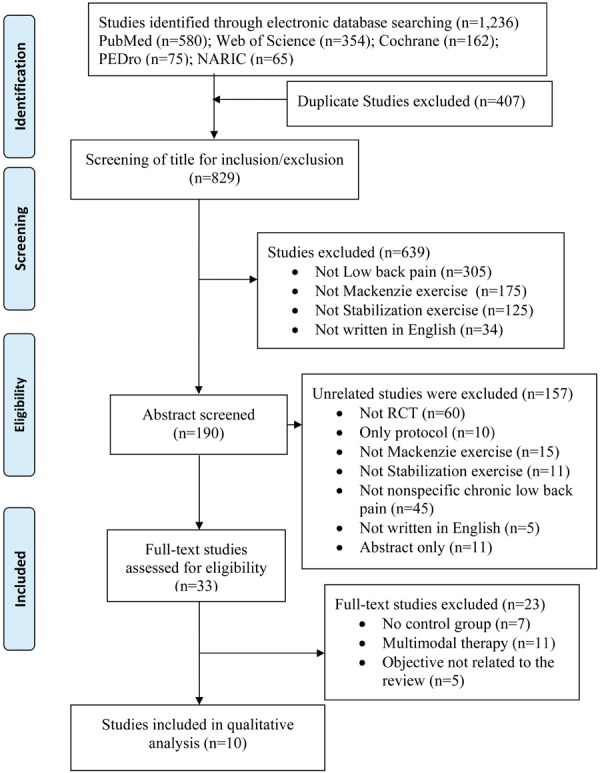
Table 3 details the risk of bias assessment of the included studies. Figure 2 presented risk of bias graph of review authors’ judgments about each risk of bias item presented as percentages across all included studies. The overall risk of bias assessment indicated that the risk of bias was low in 1 study29), and high in other 9 studies3, 27, 30,31,32,33,34,35,36). Bias in the study can be affected by unsuitable masking and inappropriate participants38). Blinding of participants can provide a chance to provide performance bias, particularly in relation to subjective results. Patients masking in a study can aid to avoid the placebo effect; failure to complete this can result in leaning the findings in favor of the treatment39). In all 10 included studies, none of the study fulfils the criteria of complete blinding. However, eight studies have assessor blinding3, 27, 29, 31, 32, 34,35,36) and two of them have no blinding30, 33). If there is poor randomization and inadequate concealed allocation of the contributors in study, bias will be introduced38). Furthermore, the inclusion and exclusion criteria are explained in all the selected studies in this review. Although six studies had concealed allocation27, 29,30,31,32, 36), there are four studies that did not mention any such information3, 33, 34, 36).
Table 3. Risk of bias of included studies (Yes, Low risk of bias; No, High risk of bias).
| Citations | Adequate sequence generation? | Allocation concealment? | Blinding? | Incomplete outcome data addressed? | Free of selective reporting? | Conclusions |
|---|---|---|---|---|---|---|
| Muretzani et al. (2015)32) | Yes | Yes | No | Unclear | Unclear | High risk of bias |
| Garcia et al. (2013)31) | Yes | Yes | No | Yes | Unclear | High risk of bias |
| Franca et al. (2012)27) | No | No | No | Yes | Unclear | High risk of bias |
| Paatelma et al. (2008)30) | Yes | No | No | Yes | Unclear | High risk of bias |
| Koumantakis et al. (2005)35) | Yes | Yes | No | Yes | Unclear | High risk of bias |
| Peterson et al. (2002)29) | Yes | Yes | Yes | Yes | Unclear | Low risk of bias |
| Moon et al. (2013)36) | No | No | No | Yes | Unclear | High risk of bias |
| Kuppusamy et al. (2013)3) | Yes | No | No | Yes | Unclear | High risk of bias |
| Hosseinifar et al. (2013)34) | No | No | No | Yes | Unclear | High risk of bias |
| Miller et al. (2005)33) | No | No | No | Yes | Unclear | High risk of bias |
Fig. 2.
Risk of bias graph: review authors’ judgments about each risk of bias item presented as percentages across all included studies.
One study32) reported reduced pain and two studies31, 32) reported reduced functional disability in the McKenzie exercise group compared to other exercises. In the three studies3, 29, 30), the McKenzie exercise group was as effective as other groups in reducing pain and functional disability in patients with chronic nonspecific low back pain. Two studies27, 35) reported reduced pain and three studies27, 35, 36) reported reduced functional disability in the stabilization exercise group compared to other exercises. In two studies33, 34), the stabilization exercise group was as effective as McKenzie exercise group in reducing pain and functional disability in patients with chronic nonspecific low back pain.
DISCUSSION
In this study, the researcher set out to investigate whether McKenzie exercises are more effective than stabilization exercises in terms of reducing pain and functional disability among individuals with chronic nonspecific low back pain. The researcher reviewed ten different studies that examined the effectiveness of either McKenzie or stabilization exercises, sometimes comparing these training regimens against other types of therapies. In such a study, Murtezani et al.32) found significant improvement in pain and disability scores in both treatment groups with a greater increase in the McKenzie group. On the other hand, a few studies comparing McKenzie exercises and other types of therapies did not reveal any statistically significant differences in outcomes between groups3, 30). For example, studies by Kuppusamy et al.3) and Paatelma et al.30) did not find any significant differences between McKenzie and other exercise-based therapies. In other cases, for instance, Garcia et al.31), McKenzie was more efficient in reducing disability scores than pain intensity. These results agree with others in the literature that showed no significant differences between McKenzie exercises and other such therapies. For example, Ghosh et al.40) did not find any difference in outcomes between groups performing McKenzie exercises and Swiss ball exercises for three months. However, McKenzie exercises seemed to have higher efficiency overall. In studies comparing stabilization exercises and other types of therapies based on physical activities, stabilization exercises emerged more effective than muscular strengthening, general exercises and intensive strengthening. The literature available also supports these findings. For example, Chitra41) found that stabilization exercises reduced pain and disability scores compared to extension activities only.
The above results indicated that both McKenzie and stabilization exercises are effective in reducing pain and functional disability scores among individuals suffering from chronic non-specific low back pain. However, a direct comparison of McKenzie and stabilization exercises yielded mixed results. Hosseinifar et al.34) investigated the effect of stabilization and McKenzie exercises on pain, disability and muscles. Pain decreased in both groups, while the disability score declined in the stabilization group only, concluding that McKenzie exercises were better in reducing pain, but not disability scores, as compared to stabilization.
Additionally, there were greater scores achieved in the stabilization group compared to the McKenzie group. On the other hand, Miller et al.33) compared McKenzie and stabilization programmes and concluded that there was no statistical difference between groups in terms of pain and functional disability scores. However, both groups reported reduced pain and functional disability. Although there can be various explanations for the mixed results in the two studies, it is clear that both stabilization and McKenzie exercises have almost similar efficiencies in pain and functional disability reduction and that the two are better than general exercises, advice-only and other therapies that do not directly target the back muscles. These findings agree with other studies available in the literature. An RCT by Halliday et al.23) compared McKenzie exercises and motor control exercises on trunk muscles in individuals with chronic low back pain. The researchers observed no significant differences between groups for pain or function, although perceived sense of recovery was greater in the group undertaking McKenzie exercises. A systematic review by Smith et al.42) gave slightly different findings in favor of stabilization exercises in the long-term treatment of LBP and associated functional disability. However, the researchers found no significant between-group differences and concluded that stabilization exercises might not offer additional benefits over alternative forms of physical activities.
The Fear-avoidance model supports the current systematic review43). According to the model, people’s fear of pain aggravates pain, leading to chronic pain and, ultimately, functional disability. When treating low back pain using McKenzie and stabilization exercises, the focus on directional preference of the TrA and MF muscles, respectively, helps alleviate the pain, which, in turn, helps patients recover physically and psychologically. The exercises counter chronic pain and functional disability through conquering fear and, subsequently, avoidance of pain in patients. In this way, patients report reduced pain and disability scores after undergoing the interventions. The specificity of the exercises helps in managing pain emanating from the strained or wasted back muscles and, therefore, facilitates the healing process. In other words, the exercises help patients confront their pain, leading to recovery.
The current study had some potential limitations. One of the limitations of the current review is the use of studies with diverse follow-up periods and comparisons. Different research studies included in the review had their own particular length of the follow-up period. This could have affected the results of this review, because the respective findings could be different depending on when they were taken. For example, a 3-month follow-up and a 1 year follow-up may yield differing results depending on the commitment of the participants and the efficacy of the treatment. Additionally, different comparisons were used in the individual studies, which make it difficult to compare McKenzie and stabilization exercises. Most of the included studies in this review compared McKenzie and other therapies or stabilization exercises and other therapies. Only two studies directly compared McKenzie and stabilization exercises33, 34). Also, it is imperative to note that, in most of the studies, the researchers did not blind the therapists and participants and, therefore, there was some element of bias. Moreover, the interventions were applied for different durations. In some studies, the participants were subjected to the intervention for a few weeks, while others for months. These difference could have led to a difference in results and difficulties in comparing the two interventions at an equal level. Finally, use of varieties of instrument for assessing pain and disability in the included studies make it difficult for the pooling of data for any quantitative analysis.
In conclusions, only two studies compared stabilization exercise with McKenzie exercises in the management of chronic nonspecific low back pain. Therefore, insufficient evidence is available to draw any conclusive comparison on the effects of McKenzie and stabilization exercises in chronic nonspecific low back pain. However, both McKenzie and stabilization exercises was better than conventional exercise programs in reducing functional disability in patients with chronic nonspecific low back pain.
Funding and Conflict of interest
None reported.
REFERENCES
- 1.Dissanayaka TD: Level of awareness of body use in young people. IJSRP, 2014, 4: 2250–3153. [Google Scholar]
- 2.Adams MA: Biomechanics of back pain. Acupunct Med, 2004, 22: 178–188. [DOI] [PubMed] [Google Scholar]
- 3.Kuppusamy S, Narayanasamy R, Christopher J: Effectiveness of Mckenzie exercises and mat based pilates exercises in subjects with chronic non-specific low back pain: a comparative study. Int J Prev Treat, 2013, 2: 47–54. [Google Scholar]
- 4.Hoy D, Bain C, Williams G, et al. : A systematic review of the global prevalence of low back pain. Arthritis Rheum, 2012, 64: 2028–2037. [DOI] [PubMed] [Google Scholar]
- 5.Balagué F, Mannion AF, Pellisé F, et al. : Non-specific low back pain. Lancet, 2012, 379: 482–491. [DOI] [PubMed] [Google Scholar]
- 6.Bin Homaid M, Abdelmoety D, Alshareef W, et al. : Prevalence and risk factors of low back pain among operation room staff at a Tertiary Care Center, Makkah, Saudi Arabia: a cross-sectional study. Ann Occup Environ Med, 2016, 28: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heyman E, Dekel H: Ergonomics for children: an educational program for elementary school. Work, 2009, 32: 261–265. [DOI] [PubMed] [Google Scholar]
- 8.Deyo RA, Dworkin SF, Amtmann D, et al. : Report of the NIH Task Force on research standards for chronic low back pain. Spine J, 2014, 14: 1375–1391. [DOI] [PubMed] [Google Scholar]
- 9.Airaksinen O, Brox JI, Cedraschi C, et al. COST B13 Working Group on Guidelines for Chronic Low Back Pain: Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J, 2006, 15: S192–S300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deyo RA, Weinstein JN: Low back pain. N Engl J Med, 2001, 344: 363–370. [DOI] [PubMed] [Google Scholar]
- 11.Koes BW, van Tulder MW, Thomas S: Diagnosis and treatment of low back pain. BMJ, 2006, 332: 1430–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Russo M, Deckers K, Eldabe S, et al. : Muscle control and non-specific chronic low back pain. Neuromodulation, 2018, 21: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waddell G, Feder G, McIntosh A, et al. : Low back pain evidence review London: Royal College of General Practitioners. J Manual Manip Ther, 1998, 6: 151–153. [Google Scholar]
- 14.Jordan KM, Arden NK, Doherty M, et al. Standing Committee for International Clinical Studies Including Therapeutic Trials ESCISIT: EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: report of a task force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis, 2003, 62: 1145–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammond A: Rehabilitation in rheumatoid arthritis: a critical review. Musculoskelet Care, 2004, 2: 135–151. [DOI] [PubMed] [Google Scholar]
- 16.Savigny P, Kuntze S, Watson P, et al. : Low back pain: early management of persistent non-specific low back pain. London: National Collaborating Centre for Primary Care and Royal College of General Practitioners, 2009, 14. [PubMed] [Google Scholar]
- 17.Aitken D, Buchbinder R, Jones G, et al. : Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Aust Fam Physician, 2015, 44: 39–42. [PubMed] [Google Scholar]
- 18.Pencharz JN, Grigoriadis E, Jansz GF, et al. : A critical appraisal of clinical practice guidelines for the treatment of lower-limb osteoarthritis. Arthritis Res, 2002, 4: 36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Baar ME, Dekker J, Oostendorp RA, et al. : The effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a randomized clinical trial. J Rheumatol, 1998, 25: 2432–2439. [PubMed] [Google Scholar]
- 20.Foley A, Halbert J, Hewitt T, et al. : Does hydrotherapy improve strength and physical function in patients with osteoarthritis--a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Ann Rheum Dis, 2003, 62: 1162–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McKenzie R: The lumbar spine: mechanical diagnosis and therapy. Spinal Publications, 1997. [Google Scholar]
- 22.McKenzie R, May S. The lumbar spine: mechanical diagnosis and therapy. Orthopedic Physical Therapy, Waikanae: Spinal Publications, 2003.
- 23.Halliday MH, Pappas E, Hancock MJ, et al. : A randomized controlled trial comparing the McKenzie method to motor control exercises in people with chronic low back pain and a directional preference. J Orthop Sports Phys Ther, 2016, 46: 514–522. [DOI] [PubMed] [Google Scholar]
- 24.Aina A, May S, Clare H: The centralization phenomenon of spinal symptoms—a systematic review. Man Ther, 2004, 9: 134–143. [DOI] [PubMed] [Google Scholar]
- 25.George SZ, Childs JD, Teyhen DS, et al. : Rationale, design, and protocol for the prevention of low back pain in the military (POLM) trial (NCT00373009). BMC Musculoskelet Disord, 2007, 8: 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Millisdotter M, Strömqvist B: Early neuromuscular customized training after surgery for lumbar disc herniation: a prospective controlled study. Eur Spine J, 2007, 16: 19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.França FR, Burke TN, Caffaro RR, et al. : Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain: a randomized, controlled trial. J Manipulative Physiol Ther, 2012, 35: 279–285. [DOI] [PubMed] [Google Scholar]
- 28.O’Sullivan PB, Phyty GD, Twomey LT, et al. : Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine, 1997, 22: 2959–2967. [DOI] [PubMed] [Google Scholar]
- 29.Petersen T, Kryger P, Ekdahl C, et al. : The effect of McKenzie therapy as compared with that of intensive strengthening training for the treatment of patients with subacute or chronic low back pain: a randomized controlled trial. Spine, 2002, 27: 1702–1709. [DOI] [PubMed] [Google Scholar]
- 30.Paatelma M, Kilpikoski S, Simonen R, et al. : Orthopaedic manual therapy, McKenzie method or advice only for low back pain in working adults: a randomized controlled trial with one year follow-up. J Rehabil Med, 2008, 40: 858–863. [DOI] [PubMed] [Google Scholar]
- 31.Garcia AN, Costa LC, da Silva TM, et al. : Effectiveness of back school versus McKenzie exercises in patients with chronic nonspecific low back pain: a randomized controlled trial. Phys Ther, 2013, 93: 729–747. [DOI] [PubMed] [Google Scholar]
- 32.Murtezani A, Govori V, Meka VS, et al. : A comparison of mckenzie therapy with electrophysical agents for the treatment of work related low back pain: a randomized controlled trial. J Back Musculoskeletal Rehabil, 2015, 28: 247–253. [DOI] [PubMed] [Google Scholar]
- 33.Miller ER, Schenk RJ, Karnes JL, et al. : A comparison of the McKenzie approach to a specific spine stabilization program for chronic low back pain. J Manual Manip Ther, 2005, 13: 103–112. [Google Scholar]
- 34.Hosseinifar M, Akbari M, Behtash H, et al. : The effects of stabilization and McKenzie exercises on transverse abdominis and multifidus muscle thickness, pain, and disability: a randomized controlled trial in nonspecific chronic low back pain. J Phys Ther Sci, 2013, 25: 1541–1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Koumantakis GA, Watson PJ, Oldham JA: Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther, 2005, 85: 209–225. [PubMed] [Google Scholar]
- 36.Moon HJ, Choi KH, Kim DH, et al. : Effect of lumbar stabilization and dynamic lumbar strengthening exercises in patients with chronic low back pain. Ann Rehabil Med, 2013, 37: 110–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Youssef MA: Effective sample size calculation: how many patients will I need to include in my study? Middle East Fertil Soc J, 2011, 16: 295–296. [Google Scholar]
- 38.Schulz KF, Grimes DA: Multiplicity in randomised trials I: endpoints and treatments. Lancet, 2005, 365: 1591–1595. [DOI] [PubMed] [Google Scholar]
- 39.Turner MK, Hooten WM, Schmidt JE, et al. : Prevalence and clinical correlates of vitamin D inadequacy among patients with chronic pain. Pain Med, 2008, 9: 979–984. [DOI] [PubMed] [Google Scholar]
- 40.Ghosh S, Datta S, Nayak S, et al. : Comparative study of muscle strengthening exercises for treatment of chronic low backache. Medical Journal of Dr. DY Patil Vidyapeeth, 2014, 7: 443–446. [Google Scholar]
- 41.Chitra R: Effect of lumbar stabilization exercise and lumbar extension exercise in the treatment of chronic low back pain. ESJ, 2014, 10: 123–131. [Google Scholar]
- 42.Smith BE, Littlewood C, May S: An update of stabilisation exercises for low back pain: a systematic review with meta-analysis. BMC Musculoskelet Disord, 2014, 15: 416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leeuw M, Goossens ME, Linton SJ, et al. : The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med, 2007, 30: 77–94. [DOI] [PubMed] [Google Scholar]