Abstract
Purpose of Review
The emotional memory and learning model of PTSD posits maladaptive fear conditioning, extinction learning, extinction recall, and safety learning as central mechanisms to PTSD. There is increasingly convincing support that sleep disturbance plays a mechanistic role in these processes. The current review consolidates the evidence on the relationships between emotional memory and learning, disturbed sleep, and PTSD acquisition, maintenance, and treatment.
Recent Findings
While disrupted sleep prior to trauma predicts PTSD onset, maladaptive fear acquisition does not seem to be the mechanism through which PTSD is acquired. Rather, poor extinction learning/recall and safety learning seem to better account for who maintains acute stress responses from trauma versus who naturally recovers; there is convincing evidence that this process is, at least in part, mediated by REM fragmentation. Individuals with PTSD had higher “fear load” during extinction, worse extinction learning, poorer extinction recall, and worse safety learning. Evidence suggests that these processes are also mediated by fragmented REM. Finally, PTSD treatments that require extinction and safety learning may also be affected by REM fragmentation.
Summary
Addressing fragmented sleep or sleep architecture could be used to increase emotional memory and learning processes and thus ameliorate responses to trauma exposure, reduce PTSD severity, and improve treatment. Future studies should examine relationships between emotional memory and learning and disturbed sleep in clinical PTSD patients.
Keywords: PTSD, Sleep disorders, Emotional learning, Emotional memory, Treatment
Introduction
Posttraumatic stress disorder (PTSD) is characterized by exposure to trauma, distressing re-experiencing of traumatic memory, avoidance of cues associated with the traumatic event, alterations in negative cognitions and mood, and hyperarousal symptoms [1]. PTSD affects approximately 5.2 million adults in the USA [2] and is associated with numerous negative physical and mental health consequences [3, 4]. While there are several effective evidence-based interventions for PTSD, there are still a significant proportion of non-responders or partial responders to treatment [5]. Advancing our understanding of mechanisms that influence PTSD acquisition, maintenance, and treatment can help guide interventions to decrease PTSD onset and severity and create more effective treatment interventions.
The emotional memory and learning model of PTSD posits dysfunctional or maladaptive Pavlovian fear conditioning [6, 7], fear extinction learning [8, 9••], fear extinction recall [10], and safety learning (the ability to differentiate safe from unsafe cues [11]) as central mechanisms to PTSD. Exaggerated acquisition of conditioned fear as well as impairments in safety learning and extinction processes are hypothesized to be critical factors in the development and maintenance of PTSD (e.g., [12]). Additionally, safety learning and extinction are hypothesized mechanisms for evidence-based PTSD treatment (e.g., [11, 13]). Examining modifiable factors that relate to both PTSD and emotional learning and memory mechanisms, such as disrupted sleep, may offer additional insight into processes relevant in the initiation and maintenance of PTSD as well as guide treatment interventions.
Sleep disturbances have been linked to both PTSD and emotional learning and memory processes. For example, there is evidence that sleep disturbances predict PTSD acquisition (e.g., [14]), severity (e.g., [15]), and treatment response (e.g., [16•]). Additionally, sleep disturbances are linked to emotional memory and learning processes [17, 18]. However, there is a dearth of information examining the relationships between sleep, emotional memory and learning process, and PTSD together. Our paper reviews the most recent literature on the relationship between fear/extinction/safety processes, sleep, and PTSD. We discuss gaps in the extant literature and make suggestions on utilizing evidence-based sleep treatments to decrease the incidence of PTSD and increase treatment effectiveness.
Sleep and PTSD
Comorbidity of PTSD and sleep disorders is staggeringly high, with 70–91% of individuals with PTSD reporting disturbed sleep [19, 20, 21•]. The most common sleep disorders include insomnia [19, 22], obstructive sleep apnea (OSA) [23, 24•], and nightmares [22], with prevalence rates in PTSD that are considerably higher than in unaffected individuals. Although sleep disturbances are symptoms of PTSD, they are best considered co-occurring and independent disorders [25•, 26, 27••]. While OSA, nightmares, and insomnia are fully separate disorders, they may all influence PTSD and sleep stages through shared effects including sleep fragmentation.
There is evidence that sleep disturbances predict PTSD acquisition, severity, and treatment. For instance, insomnia was shown to precede trauma and predict the development of PTSD [14, 28–32]. For example, rapid eye movement (REM) fragmentation within 1 month after a traumatic event was shown to predict PTSD symptom severity 6 weeks later [33]. These effects may be heightened in military populations where short sleep duration and irregular sleep patterns and trauma exposure are common [34, 35]. Sleep disturbances also affect PTSD severity, including impaired daytime functioning [15], negative long-term health consequences [36], and suicide risk [15]. Finally, sleep disturbances may compromise underlying mechanisms used in trauma-focused PTSD treatment (e.g., [37, 38]), although the evidence in inconclusive with some studies showing baseline insomnia interfering with PTSD [16•, 39•] and some showing it does not interfere [40•, 41•].
Sleep disturbances may affect PTSD acquisition, severity, and treatment through the mechanisms of emotional memory and learning, so we now turn to these processes.
Fear/Extinction/Safety Learning and PTSD
Fear conditioning, extinction, and safety learning are fundamental components of an organism’s survival system. Fear and safety learning processes help animals to pair new environmental cues with physical danger, remember those cues in novel environments, differentiate safe from unsafe cues and environments, and learn new cues that signal when the danger is over. The role of trauma and threat cue context may play a role in modulating fear memory and learning processes (e.g., seeing a gun in a dark alley versus seeing a gun at a gun range). Dysfunctional or maladaptive fear and safety learning processes are integral in PTSD acquisition, maintenance, and treatment [42••].
Fear Conditioning and PTSD
Fear conditioning is the process by which animals and humans pair a feared response to an external cue. Based on Pavlovian conditioning [43], fear conditioning occurs when there is a repeated pairing of a neutral conditioned stimulus (CS; e.g, colored light) with an aversive unconditioned stimulus (US; e.g., shock). With repeated presentations of the neutral CS with the aversive US, the CS, by itself, will elicit a conditioned fear response (conditioned response; CR). However, repeated pairings of the US and CS may not be necessary if the emotional intensity of the US is strong enough (e.g., trauma; [44]).
In terms of PTSD, an individual exposed to death, threat of death, serious injury, or sexual violence may begin to associate previously neutral cues with a heightened conditioned response from the traumatic experience. For example, an individual in a severe car accident may pair driving in a car (a previously neutral stimulus) with heightened anxiety (a conditioned fear response) and subsequently experience anxiety whenever driving. Combat PTSD may have a multifaceted fear acquisition process through training (e.g., repeatedly being told to “be on guard”), repeated engagement of high-risk situations (e.g., repeated patrolling of known insurgent hideouts), or heightened emotional responses to a single or multiple traumas (e.g., improvised explosive device; IED). Further, once someone has PTSD, fear conditioning may play a role in the maintenance of PTSD through “second-order conditioning”, the pairing of new, previously neutral cues, to the anxiety response [45]. For example, a sexual assault survivor goes out to a restaurant with his friends, experiences an intense fear response, and may now pair the restaurant with heightened fear, further maintaining PTSD symptoms.
The evidence of trait-like maladaptive or dysfunctional fear conditioning prior to a trauma (e.g., faster fear acquisition or more intense physiological responses) is limited (e.g., [46]). Rather, extant research supports the notion that differences between individuals with PTSD and those without PTSD seem to occur after fear learning occurs [47–51]. For example, a prospective study examining Marines prior to deployment examined pre-deployment baseline fear-potentiated startle (FPS), without fear condition, and found that the magnitude of FPS was associated with current PTSD symptoms, but did not predict post-deployment PTSD symptoms [50••].
Further, it also seems that individuals with PTSD do not acquire fear learning faster than controls. For example, participants with PTSD had the same startle magnitude at each “block” of acquisition (i.e., early, middle, late) compared to controls [52]. Individuals with PTSD did not have more intense reactions during acquisition than individuals without PTSD [53]. However, there is some evidence that higher magnitude of startle during fear acquisition mediated the relationship between traumatic brain injury (TBI) and PTSD symptoms following military deployment [54•].
Taken together, it appears that while the fear learning paradigm is a valid analogue to the PTSD acquisition process, there is minimal evidence that maladaptive fear learning processes predict who develops PTSD or accounts for PTSD severity.
Extinction Learning and PTSD
Extinction learning is the process through which humans learn that a previously feared cue is no longer dangerous. Extinction learning occurs when the CS is repeatedly presented without the US; after repeated presentations without the US, the CS will no longer elicit the previously learned CR. Extinction learning is a separate learning process than acquisition, which is in competition to inhibit the learned CS/US relationship [55, 56]. Extinction recall is the ability to recall this inhibitory learning after some delay in time, such that low-fear responses to the previously threatening CS are consolidated and retained.
One of the diagnostic criteria for PTSD is that symptoms last longer than 1 month; any criteria that last less than a month are considered acute stress disorder [1]. A majority of individuals who experience a trauma will have an acute stress response immediately following trauma exposure but will have their symptoms decrease in less than a month; only a subset of individuals will go on to develop PTSD [57–59]. Research suggests that impaired extinction of conditioned fear is critical in PTSD acquisition and maintenance [9••, 60, 61]. For example, while it is common to have a heightened fear response following a traumatic event, it is the individual who fails to create new extinction memories who goes on to develop clinical PTSD.
Further, extinction is a key mechanism in prolonged exposure (PE) PTSD treatment [13], one of the gold-standard PTSD treatments. PE specifically uses extinction to reduce PTSD severity through repeated exposure to safe but distress-producing cues [62, 63]. For example, an individual with PTSD may go to a busy grocery store every day, to allow new learning to occur. At first, the individual will have a heightened response, but over time, the response will decrease as they learn the grocery store is not dangerous. Individuals who have dysfunctional or maladaptive extinction learning may have a more difficult time benefitting from PE.
The literature examining PTSD and extinction learning/recall paradigms suggest there is evidence of impaired fear extinction in patients with PTSD [48, 52, 64•, 65, 66, 67••]. Several studies have shown that individuals with PTSD have slower extinction learning [66, 68–70]. Additionally, while the evidence that individuals experience heightened startle magnitude is equivocal [71], individuals with PTSD may have an over-expression of conditioned fear during the early stages of extinction learning, often called “fear load” [52, 72••], that may interfere with extinction. There is also evidence that individuals with PTSD had higher fear expression throughout the extinction process [52, 68–70, 73••]. This is confirmed in a large FPS study that demonstrated (1) high-fear-load class, (2) impaired-extinction class, and (3) normal extinction class [74•].
Some studies have shown that little or no differences in within-session extinction learning between PTSD subjects and controls, but rather, there was poor recall of extinction memories in those with PTSD 24 h after extinction learning [17, 49, 75]. This suggests it is the consolidation of extinction memories that leads to recall the newly learned extinction.
Safety Learning and PTSD
Safety learning is the ability to differentiate safe from unsafe cues. Within a learning paradigm, safety learning is when a neutral stimulus (CS+; e.g., blue light) is repeatedly paired with a US (e.g., shock), while a second neutral stimulus (CS−; e.g., yellow light) is never paired with the US [11]. In this case, the CS− is a cue that represents safety and does not elicit an anxious reactive response. Safety learning is associated with extinction learning through an inability to inhibit fear responses in the presence of safety cues, thus never allowing extinction learning to occur [11].
Safety learning is associated with PTSD acquisition, maintenance, and treatment. For example, a combat veteran with PTSD may experience heightened fear in response to previously learned fearful cues (e.g. crowded marketplaces), even when surrounded by many cues that signal safety (e.g. being far away from a war zone, being with friends and family, seeing local restaurants/storefronts). The ability to differentiate safe from unsafe cues is an essential process in facilitating the extinction process. For example, an individual with PTSD’s ability to scan a local restaurant and see no life-threatening cues can allow any anxious reactive response to decrease (i.e., the CS can decrease a CR). In addition, safety learning is integral to PTSD treatment. In order for treatment to be successful, patients must be able to differentiate safe and threatening cues and to use safe cues to inhibit fear responses, allowing extinction to occur.
The literature provides compelling evidence for the role of impaired safety learning in PTSD acquisition and maintenance. Individuals with PTSD, when compared to controls, show a lack of discrimination between danger and safety cues [69, 73••], and do not show inhibited fear when presented with the safety cues [10, 76]. These findings were confirmed in a meta-analysis [77••]. During the extinction phase, when compared to trauma-exposed controls without PTSD, individuals with PTSD demonstrated a robust psychophysical increase in arousal to the safety signal [52, 66]. Another study found that while safety discrimination (magnitude of response to fear cue minus magnitude of response to safety cue) was not associated with PTSD severity, the inability to inhibit the fear response when exposed to both safety and fear cues did predict the persistence of PTSD symptoms [48].
Contextual Learning and PTSD
It is useful to consider the role of context processing in fear and extinction learning and memory. Fear responses may be conditioned to the environment in which the aversive event occurred. This is typically termed context conditioning. Thus, a person robbed in a dark alley may come to fear and avoid the environment “dark alley,” which is itself made up of a number of discrete cues (e.g., trash bins, gun, smells). Further, cued fear conditioning and extinction learning may be modulated by context. For example, after a robbery, a person may learn to fear “gun,” a discrete cue, in a dark alley-like environment, but seeing a gun in the context of a shooting range would not elicit the same response. An example of contextual modulation of fear extinction learning is the well-known renewal effect (Bouton, 1993). If an individual learns to fear a CS in context A, and then is given extinction learning trials in a different context (B) so that they no longer fear the CS, that fear response may return when the organism is returned to the original context (A), or even when exposed to the CS in a different context altogether (C).
Impaired contextual modulation of fear learning and extinction has been posited as a central factor in the etiology and maintenance of PTSD [78•, 79]. A study of PTSD patients and combat-exposed controls found that when a fear response was extinguished in a different context (safety context) than when it was learned (threat context), PTSD patients were less able to effectively use that contextual information to suppress fear responding in the safety context [80]. Interestingly, they were also unable to use contextual information to enhance fear in the threat context. Overall, these results suggest that patients with PTSD have deficits in the contextual modulation of learned fear that is not accounted for by trauma exposure alone.
Relationship Between Sleep and Emotional Learning Processes
Sleep is generally divided into two types: rapid eye movement (REM) sleep and non-REM (NREM) sleep. NREM sleep is divided into three stages, with each stage representing a deeper level of sleep. Stage N3 sleep is considered “deep sleep,” also called slow-wave sleep (SWS). Each stage of sleep is linked with different patterns of brain activity, neurochemistry, memory consolidation, and emotional processing (see [81] for review). REM sleep is generally associated with processing and formation of emotional memories [82–84], consolidation of emotional memories and learning [85, 86], and fear and extinction memory learning [87••] (See [88••] for review). SWS has also been implicated in learning [89•, 90, 91]. Memory encoding was shown to deteriorate after total sleep deprivation, but not after selective REM sleep deprivation [89•]. The differential findings between REM and NREM sleep may depend on the type of information being encoded, for example, episodic information and context may be more associated with SWS while emotional processing may be more associated with REM.
REM Sleep and Fear Acquisition in Healthy Human Controls
A study examined the relationship between REM sleep and fear acquisition in 17 healthy students and found more time in REM sleep prior to learning task predicted weaker fear-related learning, concluding that REM sleep may be protective against fear learning [92•]. They also suggest that examining REM over multiple nights had a stronger effect on outcome than any single night alone, perhaps suggesting a trait-like relationship between REM and fear acquisition.
REM Sleep and Extinction Learning in Healthy Human Controls
Animal models indicate that sleep disruption interferes with initial extinction learning [93], though findings in humans are more mixed. One night of total sleep deprivation did not interfere with extinction learning [94•], while another recent study comparing healthy controls to individuals with primary insomnia showed delayed neural activation in the brain circuits relevant to extinction learning in the insomnia group [95•]. Sleep deprivation prior to initial fear conditioning was associated with higher subjective and objective fear at the extinction stage compared to a non-sleep-deprived group [96•]. However, most human studies indicate that sleep disruption interferes with extinction recall and generalization. It was reported that participants who slept overnight were better able to generalize fear extinction than participants who remained awake between extinction learning and recall [17]. Additionally, naps [97] and overnight REM deprivation [18] have shown that disrupted REM sleep interferes with recall of extinguished fear. In healthy human control participants, total sleep deprivation prior to extinction learning interfered with extinction recall 24 h later [94•]. Additionally, this study showed REM sleep consolidation was correlated with extinction recall on the final day of testing. These investigations, most of which have been conducted in healthy human control subjects, suggest sleep, and REM sleep in particular, is critical for extinction processes, particularly extinction consolidation and recall.
REM Sleep and Safety Learning in Healthy Human Controls
In addition to demonstrating links between sleep and extinction learning, additional research implicates sleep as a critical factor in safety learning. Research findings from healthy humans corroborate the notion that REM sleep is important for safety signal learning. For example, in one study, 42 healthy control participants underwent a fear conditioning/safety learning paradigm, and then, their sleep was monitored overnight in the laboratory prior to undergoing an extinction learning session the next day [98]. They found that increased safety signal learning during the acquisition phase of the study was associated with more consolidated REM sleep that night. More consolidated REM sleep, in turn, was then associated with better discrimination between the threat and safety signal session 24 h later. This study, which was conducted in healthy human control participants, suggests impaired safety learning is associated with more fragmented REM sleep, which is then subsequently associated with impairments in discrimination between threat and safety cues. Another study had healthy human control participants undergo a fear and safety acquisition session, and then a split-night protocol was used to randomize participants to have a larger or smaller proportion of REM sleep the next night and prior to extinction learning (sleeping the first half of the night leads to relatively less REM sleep and sleeping only the second half of the night leads to more REM) [87••]. Following a night of recovery sleep, participants randomized to have disrupted REM sleep showed worse discrimination of threat and safety signals. This study provides additional evidence suggesting impaired REM sleep is associated with worse ability to discriminate between threatening and safe cues.
REM Sleep and Fear/Safety Processes in PTSD
Despite mechanistic research suggesting associations between REM sleep consolidation, fear and safety processes, and PTSD symptoms, to our knowledge, only one study has examined links between REM sleep and fear conditioning in patients with PTSD [99•]. This small study (n = 13), conducted in military veterans with PTSD, consisted of a 3-day protocol including (1) fear conditioning and safety learning, (2) extinction learning, and (3) a fear and safety recall session. All participants underwent overnight lab-based sleep polysomnography prior to each testing session. This study found no associations between REM sleep and fear or extinction processes. However, participants who learned the safety signal more rapidly during the first testing session showed more efficient REM sleep that night. Additionally, participants who had a higher percentage of REM sleep on the last night showed better safety signal recall on the last testing session. This study extends the research in healthy human control participants by showing associations between REM sleep and safety learning in patients with PTSD. However, the small size and lack of statistical power likely hampered the ability to detect potential relationships between REM sleep and fear conditioning or extinction processes.
Conclusions
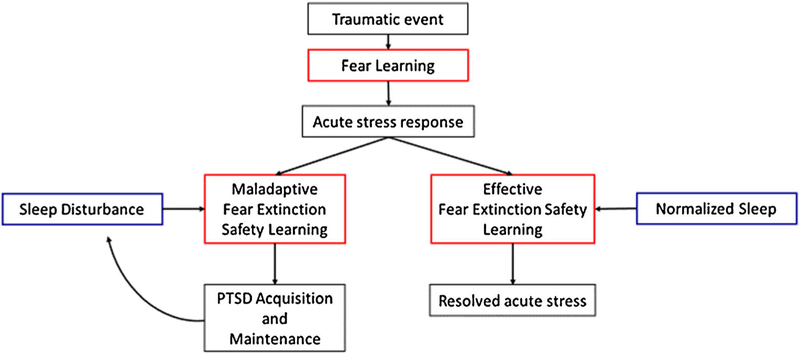
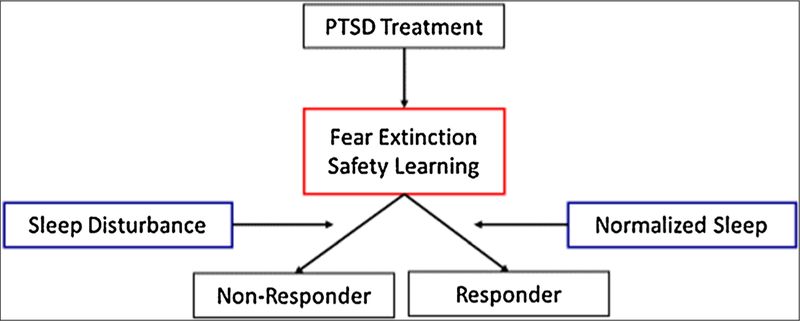
The current review consolidates the evidence on the relationships between emotional memory and learning, disturbed sleep, and PTSD acquisition, maintenance, and treatment (see Figs. 1 and 2 for a graphical depiction based on the literature, and see Table 1 for a summary of key findings). There is increasingly convincing support that emotional memory and learning are critical for PTSD acquisition, maintenance, and treatment and that sleep disturbance plays a mechanistic role in these processes. Further research of sleep and emotional memory and learning in clinical PTSD samples is needed.
Fig. 1.
Theoretical relationship between trauma, emotional memory and learning, and sleep
Fig. 2.
Theoretical relationship between PTSD treatment, emotional memory and learning, and sleep
Table 1.
Summary of key findings
| • Maladaptive fear acquisition processes do not seem to account for PTSD acquisition. |
| • Poor extinction learning, extinction retention, and safety learning predict who maintains acute stress response from trauma versus who naturally recovers. |
| • Safety learning and extinction processes are also integral mechanisms for trauma-focused interventions. |
| • The extant literature suggests poor sleep is a risk factor for developing PTSD, and poor sleep may interfere with trauma-focused interventions. |
| • The relationship between PTSD and emotional memory and learning may be mediated by disrupted sleep, specifically, REM fragmentation. |
| • In healthy humans, REM sleep disruption impairs extinction learning and retention. |
| • In healthy humans, impaired REM sleep is associated with worse safety learning. |
| • One study in PTSD patients demonstrated links between disrupted REM sleep and safety learning. |
| • Clinically addressing fragmented sleep may increase emotional memory and learning processes, and ameliorate responses to trauma exposure, reduce PTSD severity, and improve treatment. |
| • More research is needed in clinical PTSD patients and with PTSD treatment. |
While disrupted sleep prior to trauma predicts PTSD onset, maladaptive fear acquisition processes do not seem to be the mechanism through which PTSD is acquired. Rather, poor extinction learning/recall and safety learning seem to better account for who maintains acute stress responses from trauma versus who naturally recovers; there is convincing evidence that this process is, at least in part, mediated by REM fragmentation. Individuals with PTSD were shown to have higher “fear load” during extinction, worse extinction learning, poorer extinction recall, and worse safety learning. Evidence suggests that these processes are also mediated by fragmented REM, and may account for long-term PTSD maintenance. Finally, PTSD treatments that require extinction and safety learning may also be affected by REM fragmentation, although no studies have specifically examined this hypothesis.
Clinically addressing fragmented sleep or sleep architecture could be used to increase efficient emotional memory and learning processes and thus ameliorate responses to trauma exposure, reduce PTSD severity, and improve treatment. For example, poor sleep predicted PTSD onset [14]. This is consistent with both REM fragmentation within 1 month after a traumatic event predicting PTSD symptom severity 6 weeks later [33] and REM fragmentation being associated with poorer extinction recall [17, 18] and safety learning [98]. This suggests that addressing REM fragmentation through behavioral sleep interventions (e.g., napping/cognitive behavioral therapy for insomnia; CBT-I) or pharmacological treatments (e.g., prazosin) may help consolidate emotional memories and learning and perhaps decrease the incidence of PTSD. Similarly, consolidating sleep may be useful for stress inoculation. For example, a military unit under intense combat training could prioritize quality sleep to help effectively consolidate emotional experiences. Finally, addressing sleep may be useful in increasing PTSD treatment outcomes. For example, REM deprivation did not interfere with extinction learning but rather led to poorer extinction recall, a primary mechanism for PE [18]. This is consistent with the finding that within-session extinction did not predict PE treatment outcome, but rather, between-session extinction (i.e., extinction recall) did predict treatment outcomes [100•]. Another study showed that individuals who slept after spider phobia exposure, compared to a non-sleep group, had better reductions in fear [101]. This finding is showing evidence in the PTSD treatment literature, where there are preliminary positive results suggesting that addressing sleep disturbances prior to PE may increase treatment efficacy [102••]. Overall, targeting treatments of disturbed sleep in the context of PTSD could be a unique and underutilized opportunity to advance clinical care.
There are many sleep disorders associated with PTSD that could cause sleep architecture disruption, which then in turn may interfere with emotional memory and learning. Common sleep disturbances include insomnia [19, 22], obstructive sleep apnea (OSA) [23, 24•], and nightmares [22] with prevalence rates in PTSD that are considerably higher than in unaffected individuals. These sleep disturbances can be further exacerbated by chaotic sleep schedules in the case of military personnel [35]. Accurate sleep assessments and evidence-based interventions are necessary to address sleep disturbances (see [27••] for a thorough review of the sleep treatments in individuals with PTSD), which, in turn, may help PTSD symptom severity and treatment.
While disrupted REM sleep has received the most attention thus far, it is only one aspect of sleep architecture. Other stages of sleep may affect the etiology of PTSD as well. For example, as discussed earlier, contextual fear processing can affect extinction, extinction recall, and safety learning in the etiology of PTSD [79]. It is suggested that SWS may be necessary for consolidating contextual information about that event into memory [103]. If SWS is disrupted following trauma or during treatment, then the contextual fear memory necessary to make future discriminations between actual threat contexts and those that simply contain some of the same elements may be disturbed. However, to date, no studies have examined the effect of sleep disruption on contextual fear memory in humans.
Emotional memory and learning is only one process in the complex etiology of PTSD acquisition, maintenance, and treatment. Future studies should also examine the role of disturbed sleep on other processes involved with PTSD. For example, letting individuals know about fear and safety cues helped them differentiate between safe and unsafe cues [104•]. This suggests that attentional control or awareness of fear cues may affect emotional memory and learning. Another example is that heightened startle or “fear load” may lead to greater behavioral avoidance, thus increasing the negative salience of the feared cue and reinforcing further avoidance responses. This suggests a more nuanced relationship to the magnitude of fear response impacting PTSD maintenance and treatment may involve interoceptive awareness, cognitive interpretation of internal cues, and/or distress tolerance.
Future studies should examine relationships between emotional memory and learning and disturbed sleep in clinical PTSD patients. Additionally, future studies could use a manipulation paradigm to either disrupt REM sleep (e.g., via REM deprivation) or consolidate REM sleep overnight (e.g., via a pharmacological agent), and examine the relationship between REM sleep and extinction processes in PTSD patients. Doing so could provide additional validation that REM sleep quality is an important and modifiable mechanism in PTSD. Future studies should also examine sleep architecture beyond just REM sleep, such as SWS. Finally, future studies would do well to examine how emotional memory and learning and disturbed sleep may affect behaviors (e.g., avoiding or treatment dropout), emotions (e.g., inhibition, stress reactivity), and cognitions (e.g., interpretation/perception, attentional control) that are associated with PTSD maintenance and treatment.
Acknowledgments
The writing was supported by VA RR&D CDA Grant no. 1lK2Rx002120–01 (Dr. Colvonen) and by the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs (Dr. Straus). The editors would like to thank Dr. Bradley Gaynes for taking the time to review this manuscript.
Footnotes
Compliance with Ethical Standards
Conflict of Interest Peter J. Colvonen, Laura D. Straus, Dean Acheson, and Philip Gehrman declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer The contents do not represent the views of the U.S. Department of Veterans Affairs or the US Government.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.APA. Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub; 2013. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62(6):617–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boscarino JA. A prospective study of PTSD and early-age heart disease mortality among Vietnam veterans: implications for surveillance and prevention. Psychosom Med 2008;70(6):668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. J Consult Clin Psychol 2003;71(4):692. [DOI] [PubMed] [Google Scholar]
- 5.Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry: Interpersonal and Biological Processes 2008;71(2):134–68. [DOI] [PubMed] [Google Scholar]
- 6.Elzinga BM, Bremner JD. Are the neural substrates of memory the final common pathway in posttraumatic stress disorder (PTSD)? J Affect Disord 2002;70(1):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson LR, McGuire J, Lazarus R, Palmer AA. Pavlovian fear memory circuits and phenotype models of PTSD. Neuropharmacology 2012;62(2):638–46. [DOI] [PubMed] [Google Scholar]
- 8.Myers KM, Davis M. Mechanisms of fear extinction. Mol Psychiatry 2007;12(2):120–50. [DOI] [PubMed] [Google Scholar]
- 9. ••.Pace-Schott EF, Germain A, Milad MR. Effects of sleep on memory for conditioned fear and fear extinction. Psychol Bull 2015;141(4):835.This review paper identifies both animal and human studies that demonstrate the importance of sleep, REM specifically, on processes of conditioned fear and fear extinction.
- 10.Jovanovic T, Norrholm SD, Blanding NQ, Davis M, Duncan E, Bradley B, et al. Impaired fear inhibition is a biomarker of PTSD but not depression. Depress Anxiety 2010;27(3):244–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jovanovic T, Kazama A, Bachevalier J, Davis M. Impaired safety sign al learn i ng may b e a biomark e r o f P TS D. Neuropharmacology 2012;62(2):695–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.VanElzakker MB, Dahlgren MK, Davis FC, Dubois S, Shin LM. From Pavlov to PTSD: the extinction of conditioned fear in rodents, humans, and anxiety disorders. Neurobiol Learn Mem 2014;113:3–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foa E, Hembree E, Rothbaum BO. Prolonged exposure therapy for PTSD: emotional processing of traumatic experiences therapist guide: Oxford University Press; 2007. [Google Scholar]
- 14.Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. J Anxiety Disord 2010;24(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep 2011;34(1):93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. •.López CM, Lancaster CL, Gros DF, Acierno R. Residual sleep problems predict reduced response to prolonged exposure among veterans with PTSD. Journal of Psychopathology and Behavioral Assessment 2017;39(4):755–63This study found that greater residual sleep symptoms were predictive of smaller treatment gains and changes in sleep were significant predictors of PTSD and depression symptom reduction above and beyond the influence of demographic and therapy engagement factors.
- 17.Pace-Schott EF, Milad MR, Orr SP, Rauch SL, Stickgold R, Pitman RK. Sleep promotes generalization of extinction of conditioned fear. Sleep 2009;32(1):19. [PMC free article] [PubMed] [Google Scholar]
- 18.Spoormaker VI, Schröter MS, Andrade KC, Dresler M, Kiem SA, Goya-Maldonado R, et al. Effects of rapid eye movement sleep deprivation on fear extinction recall and prediction error signaling. Hum Brain Mapp 2012;33(10):2362–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ohayon MM, Shapiro CM. Sleep disturbances and psychiatric disorders associated with posttraumatic stress disorder in the general population. Compr Psychiatry 2000;41(6):469–78. [DOI] [PubMed] [Google Scholar]
- 20.Plumb TR, Peachey JT, Zelman DC. Sleep disturbance is common among servicemembers and veterans of Operations Enduring Freedom and Iraqi Freedom. Psychol Serv 2014;11(2):209. [DOI] [PubMed] [Google Scholar]
- 21. •.Jenkins MM, Colvonen PJ, Norman SB, Afari N, Allard CB, Drummond SP. Prevalence and mental health correlates of insomnia in first-encounter veterans with and without military sexual trauma. Sleep 2015;38(10):1547–54This study compared MST to non-MST veterans. They found that, in the MST subgroup, 60.8% of the participants had insomnia, a number significantly higher than the general population or the non-MST group.
- 22.Neylan TC, Marmar CR, Metzler TJ, Weiss DS, Zatzick DF, Delucchi KL, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Sleep 1998;155(7). [DOI] [PubMed] [Google Scholar]
- 23.Krakow B, Melendrez D, Johnston L, Warner TD, Clark JO, Pacheco M, et al. Sleep-disordered breathing, psychiatric distress, and quality of life impairment in sexual assault survivors. J Nerv Ment Dis 2002;190(7):442–52. [DOI] [PubMed] [Google Scholar]
- 24. •.Colvonen PJ, Masino T, Drummond SP, Myers US, Angkaw AC, Norman SB. Obstructive sleep apnea and posttraumatic stress disorder among OEF/OIF/OND Veterans. J Clin Sleep Med 2015;11(5):513–8This study found high rates of OSA in younger, lower BMI veterans with PTSD, suggesting the classic signs of OSA may not fit for OEF/OIF/OND veterans.
- 25. •.Germain A, McKeon AB, Campbell RL. Sleep in PTSD: Conceptual model and novel directions in brain-based research and interventions. Curr Opin Psychol 2017;14:84–9This review provides evidence that sleep disturbances are a comorbid, rather than a secondary, condition in PTSD.
- 26.Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev 2008;12(3):169–84. [DOI] [PubMed] [Google Scholar]
- 27. ••.Colvonen PJ, Straus LD, Stepnowsky C, McCarthy MJ, Goldstein LA, Norman SB. Recent advancements in treating sleep disorders in co-occurring PTSD. Current Psychiatry Reports 2018;20(7):48.This review highlights evidence-based practices for sleep disturbances commonly found in PTSD including insomnia, nightmares, and OSA. The authors present a flowchart of assessment and treatment.
- 28.Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep 2010;33(1):69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Germain A, Buysse DJ, Nofzinger E. Sleep-specific mechanisms underlying posttraumatic stress disorder: integrative review and neurobiological hypotheses. Sleep Med Rev 2008;12(3):185–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bonn-Miller MO, Babson KA, Vujanovic AA, Feldner MT. Sleep problems and PTSD symptoms interact to predict marijuana use coping motives: a preliminary investigation. Journal of Dual Diagnosis 2010;6(2):111–22. [Google Scholar]
- 31.Gehrman P, Seelig AD, Jacobson IG, Boyko EJ, Hooper TI, Gackstetter GD, et al. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. Sleep 2013;36(7):1009–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD and depression among Iraq combat veterans. J Clin Psychol 2011;67(12):1240–58. [DOI] [PubMed] [Google Scholar]
- 33.Mellman TA, Bustamante V, Fins AI, Pigeon WR, Nolan B. REM sleep and the early development of posttraumatic stress disorder. Am J Psychiatr 2002;159(10):1696–701. [DOI] [PubMed] [Google Scholar]
- 34.Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil Med 2008;173(3):230–5. [DOI] [PubMed] [Google Scholar]
- 35.Seelig AD, Jacobson IG, Smith B, Hooper TI, Boyko EJ, Gackstetter GD, et al. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep, 2010;33(12):1615–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baran B, Pace-Schott EF, Ericson C, Spencer RM. Processing of emotional reactivity and emotional memory over sleep. J Neurosci 2012;32(3):1035–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Belleville G, Guay S, Marchand A. Persistence of sleep disturbances following cognitive-behavior therapy for posttraumatic stress disorder. J Psychosom Res 2011;70(4):318–27. [DOI] [PubMed] [Google Scholar]
- 38.Gutner CA, Casement MD, Gilbert KS, Resick PA. Change in sleep symptoms across cognitive processing therapy and prolonged exposure: A longitudinal perspective. Behav Res Ther 2013;51(12):817–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. •.Lommen MJ, Grey N, Clark DM, Wild J, Stott R, Ehlers A. Sleep and treatment outcome in posttraumatic stress disorder: results from an effectiveness study. Depression and anxiety 2016;33(7): 575–83This study found that patients with worse comorbid depression and poorer sleep showed smaller decreases in PTSD symptoms with CT-PTSD treatment.
- 40. •.Woodward E, Hackmann A, Wild J, Grey N, Clark DM, Ehlers A. Effects of psychotherapies for posttraumatic stress disorder on sleep disturbances: results from a randomized clinical trial. Behav Res Ther 2017;97:75–85This study found that CT-PTSD, compared to waitlist, improved self-reported sleep duration and nightmares. They found that baseline sleep did not interfere with PTSD treatment outcomes.
- 41. •.Sexton MB, Avallone KM, Smith ER, Porter KE, Ashrafioun L, Arnedt JT, et al. Sleep disturbances as predictors of prolonged exposure therapy effectiveness among veterans with PTSD. Psychiatry Res 2017;256:118–23This study found that higher PSQI scores were related to higher baseline PCL scores. PSQI scores were not associated with reduced effectiveness of PE treatment or slope of PTSD symptom changes.
- 42. ••.Norrholm SD, Jovanovic T. Fear processing, psychophysiology, and PTSD. Harvard review of psychiatry 2018;26(3):129–41This review focuses on fear acquisition and fear extinction and how they are relevant to PTSD and PTSD treatment.
- 43.Pavlov IP. Conditional reflexes: an investigation of the physiological activity of the cerebral cortex 1927. [DOI] [PMC free article] [PubMed]
- 44.Rescorla RA, Wagner AR. A theory of Pavlovian conditioning: variations in the effectiveness of reinforcement and nonreinforcement. Classical conditioning II: Current research and theory 1972;2:64–99. [Google Scholar]
- 45.Rescorla RA, Gillan DJ. An analysis of the facilitative effect of similarity on second-order conditioning. J Exp Psychol Anim Behav Process 1980;6(4):339. [PubMed] [Google Scholar]
- 46.Pole N, Neylan TC, Otte C, Henn-Hasse C, Metzler TJ, Marmar CR. Prospective prediction of posttraumatic stress disorder symptoms using fear potentiated auditory startle responses. Biol Psychiatry 2009;65(3):235–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shalev AY, Peri T, Brandes D, Freedman S, Orr SP, Pitman RK. Auditory startle response in trauma survivors with posttraumatic stress disorder: a prospective study. Am J Psychiatr 2000;157(2): 255–61. [DOI] [PubMed] [Google Scholar]
- 48.Lommen MJ, Engelhard IM, Sijbrandij M, van den Hout MA, Hermans D. Pre-trauma individual differences in extinction learning predict posttraumatic stress. Behav Res Ther 2013;51(2):63–7. [DOI] [PubMed] [Google Scholar]
- 49.Milad MR, Orr SP, Lasko NB, Chang Y, Rauch SL, Pitman RK. Presence and acquired origin of reduced recall for fear extinction in PTSD: results of a twin study. J Psychiatr Res 2008;42(7):515–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. ••.Glenn DE, Acheson DT, Geyer MA, Nievergelt CM, Baker DG, Risbrough VB, et al. High and low threshold for startle reactivity associated with PTSD symptoms but not PTSD risk: Evidence from a prospective study of active duty Marines. Depression and anxiety 2016;33(3):192–202This study suggests that startle reactivity is not a risk marker for developing PTSD; rather, startle reactivity is associated with current PTSD.
- 51.Orr SP, Metzger LJ, Lasko NB, Macklin ML, Hu FB, Shalev AY, et al. Physiologic responses to sudden, loud tones in monozygotic twins discordant for combat exposure: association with posttraumatic stress disorder. Arch Gen Psychiatry 2003;60(3):283–8. [DOI] [PubMed] [Google Scholar]
- 52.Norrholm SD, Jovanovic T, Olin IW, Sands LA, Bradley B, Ressler KJ. Fear extinction in traumatized civilians with posttraumatic stress disorder: relation to symptom severity. Biol Psychiatry 2011;69(6):556–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jovanovic T, Norrholm SD, Fennell JE, Keyes M, Fiallos AM, Myers KM, et al. Posttraumatic stress disorder may be associated with impaired fear inhibition: relation to symptom severity. Psychiatry Res 2009;167(1):151–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. •.Glenn DE, Acheson DT, Geyer MA, Nievergelt CM, Baker DG, Risbrough VB, et al. Fear learning alterations after traumatic brain injury and their role in development of posttraumatic stress symptoms. Depression and anxiety 2017;34(8):723–33This study suggests that TBI may contribute to risk for developing PTSD symptoms because of the association between multiple-hit TBI and increased conditioned fear learning and fear expression.
- 55.Bouton ME, Westbrook RF, Corcoran KA, Maren S. Contextual and temporal modulation of extinction: behavioral and biological mechanisms. Biol Psychiatry 2006;60(4):352–60. [DOI] [PubMed] [Google Scholar]
- 56.Myers KM, Davis M. Behavioral and neural analysis of extinction. Neuron 2002;36(4):567–84. [DOI] [PubMed] [Google Scholar]
- 57.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52(12):1048–60. [DOI] [PubMed] [Google Scholar]
- 58.Bryant RA. Early predictors of posttraumatic stress disorder. Biol Psychiatry 2003;53(9):789–95. [DOI] [PubMed] [Google Scholar]
- 59.Bryant RA. Acute stress disorder as a predictor of posttraumatic stress disorder: a systematic review. The Journal of Clinical Psychiatry 2011;72(2):233–9. [DOI] [PubMed] [Google Scholar]
- 60.Mineka S, Oehlberg K. The relevance of recent developments in classical conditioning to understanding the etiology and maintenance of anxiety disorders. Acta Psychol 2008;127(3):567–80. [DOI] [PubMed] [Google Scholar]
- 61.Pitman RK, Rasmusson AM, Koenen KC, Shin LM, Orr SP, Gilbertson MW, et al. Biological studies of post-traumatic stress disorder. Nat Rev Neurosci 2012;13(11):769–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McNally RJ. Mechanisms of exposure therapy: how neuroscience can improve psychological treatments for anxiety disorders. Clin Psychol Rev 2007;27(6):750–9. [DOI] [PubMed] [Google Scholar]
- 63.Craske MG, Kircanski K, Zelikowsky M, Mystkowski J, Chowdhury N, Baker A. Optimizing inhibitory learning during exposure therapy. Behav Res Ther 2008;46(1):5–27. [DOI] [PubMed] [Google Scholar]
- 64. •.Rabinak CA, Mori S, Lyons M, Milad MR, Phan KL. Acquisition of CS-US contingencies during Pavlovian fear conditioning and extinction in social anxiety disorder and posttraumatic stress disorder. J Affect Disord 2017;207:76–85In this standard Pavlovian fear conditioning-extinction paradigm, participants with PTSD overestimated the aversive outcomes and did not show successful extinction.
- 65.Orcutt HK, Hannan SM, Seligowski AV, Jovanovic T, Norrholm SD, Ressler KJ, et al. Fear-potentiated startle and fear extinction in a sample of undergraduate women exposed to a campus mass shooting. Front Psychol 2017;7:2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Blechert J, Michael T, Vriends N, Margraf J, Wilhelm FH. Fear conditioning in posttraumatic stress disorder: evidence for delayed extinction of autonomic, experiential, and behavioural responses. Behav Res Ther 2007;45(9):2019–33. [DOI] [PubMed] [Google Scholar]
- 67. ••.Zuj DV, Palmer MA, Hsu CMK, Nicholson EL, Cushing PJ, Gray KE, et al. Impaired fear extinction associated with PTSD increases with hours-since-waking. Depression and anxiety 2016;33(3): 203–10In this study, hours-since-waking was a significant moderator of the relationship between impaired late extinction and PTSD symptoms.
- 68.Wessa M, Flor H. Failure of extinction of fear responses in posttraumatic stress disorder: evidence from second-order conditioning. Am J Psychiatr 2007;164(11):1684–92. [DOI] [PubMed] [Google Scholar]
- 69.Orr SP, Metzger LJ, Lasko NB, Macklin ML, Peri T, Pitman RK. De novo conditioning in trauma-exposed individuals with and without posttraumatic stress disorder. J Abnorm Psychol 2000;109(2):290. [PubMed] [Google Scholar]
- 70.Peri T, Ben-Shakhar G, Orr SP, Shalev AY. Psychophysiologic assessment of aversive conditioning in posttraumatic stress disorder. Biol Psychiatry 2000;47(6):512–9. [DOI] [PubMed] [Google Scholar]
- 71.Zoladz PR, Diamond DM. Current status on behavioral and biological markers of PTSD: a search for clarity in a conflicting literature. Neurosci Biobehav Rev 2013;37(5):860–95. [DOI] [PubMed] [Google Scholar]
- 72. ••.Norrholm SD, Glover EM, Stevens JS, Fani N, Galatzer-Levy IR, Bradley B, et al. Fear load: the psychophysiological overexpression of fear as an intermediate phenotype associated with trauma reactions. Int J Psychophysiol 2015;98(2):270–5In this study, individuals with PTSD were shown to have an overexpression of conditioned fear during the early stages of extinction learning, called “fear load,” that may interfere with extinction.
- 73. ••.Acheson D, Geyer M, Baker D, Nievergelt C, Yurgil K, Risbrough VB, et al. Conditioned fear and extinction learning performance and its association with psychiatric symptoms in active duty Marines. Psychoneuroendocrinology 2015;51:495–505During fear acquisition, the PTSD symptom group exhibited larger startle responses during the safety cue compared to the healthy group. During extinction, the PTSD group showed less reduction in their response to the conditioned stimulus.
- 74. •.Galatzer-Levy IR, Andero R, Sawamura T, Jovanovic T, Papini S, Ressler KJ, et al. A cross species study of heterogeneity in fear extinction learning in relation to FKBP5 variation and expression: implications for the acute treatment of posttraumatic stress disorder. Neuropharmacology 2017;116:188–95Study 1 (in humans) found that FKBP5 and PTSD symptom domains are associated with abnormal fear extinction phenotypes. Study 2 (in mice) found that dexamethasone was associated with increased amygdala FKBP5 following extinction.
- 75.Shvil E, Sullivan GM, Schafer S, Markowitz JC, Campeas M, Wager TD, et al. Sex differences in extinction recall in posttraumatic stress disorder: a pilot fMRI study. Neurobiol Learn Mem 2014;113:101–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jovanovic T, Sakoman AJ, Kozarić-Kovačić D, Meštrović AH, Duncan EJ, Davis M, et al. Acute stress disorder versus chronic posttraumatic stress disorder: inhibition of fear as a function of time since trauma. Depress Anxiety 2013;30(3):217–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. ••.Duits P, Cath DC, Lissek S, Hox JJ, Hamm AO, Engelhard IM, et al. Updated meta-analysis of classical fear conditioning in the anxiety disorders. Depress Anxiety 2015;32(4):239–53This meta-analysis examined differences in fear conditioning between anxiety patients and healthy controls and found robustly increased fear responses to conditioned safety cues in anxiety patients. During extinction, anxiety patients show stronger fear responses to the conditioned danger cue and trend toward increased discrimination learning compared to controls.
- 78. •.Liberzon I, Abelson JL. Context processing and the neurobiology of post-traumatic stress disorder. Neuron 2016;92(1):14–30Propose that dysregulation within contextual processing is a the core of PTSD pathophysiology.
- 79.Acheson DT, Gresack JE, Risbrough VB. Hippocampal dysfunction effects on context memory: possible etiology for posttraumatic stress disorder. Neuropharmacology 2012;62(2):674–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Garfinkel SN, Abelson JL, King AP, Sripada RK, Wang X, Gaines LM, et al. Impaired contextual modulation of memories in PTSD: an fMRI and psychophysiological study of extinction retention and fear renewal. J Neurosci 2014;34(40):13435–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Van der Helm E, Yao J, Dutt S, Rao V, Saletin JM, Walker MP. REM sleep depotentiates amygdala activity to previous emotional experiences. Curr Biol 2011;21(23):2029–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wagner U, Gais S, Born J. Emotional memory formation is enhanced across sleep intervals with high amounts of rapid eye movement sleep. Learn Mem 2001;8(2):112–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wagner U, Fischer S, Born J. Changes in emotional responses to aversive pictures across periods rich in slow-wave sleep versus rapid eye movement sleep. Psychosom Med 2002;64(4):627–34. [DOI] [PubMed] [Google Scholar]
- 84.Wagner U, Kashyap N, Diekelmann S, Born J. The impact of post-learning sleep vs. wakefulness on recognition memory for faces with different facial expressions. Neurobiol Learn Mem 2007;87(4):679–87. [DOI] [PubMed] [Google Scholar]
- 85.Nishida M, Pearsall J, Buckner RL, Walker MP. REM sleep, prefrontal theta, and the consolidation of human emotional memory. Cereb Cortex 2008;19(5):1158–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nishida M, Pearsall J, Buckner R, Walker M. Prefrontal theta during REM sleep enhances emotional memory. Cereb Cortex 2009;19:1158–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. ••.Menz MM, Rihm JS, Büchel C. REM sleep is causal to successful consolidation of dangerous and safety stimuli and reduces return of fear after extinction. J Neurosci 2016;36(7):2148–60In this study, REM-rich sleep in the second half of the night promoted good discrimination between fear-relevant and neutral stimuli during recall while staying awake the second half of the night led to an increase of discrimination between extinguished and neutral stimuli.
- 88. ••.Tempesta D, Socci V, De Gennaro L, Ferrara M. Sleep and emotional processing. Sleep Med Rev 2017.This review discusses the importance of REM and the protective role of sleep in emotional homeostasis and regulation.
- 89. •.Kaida K, Niki K, Born J. Role of sleep for encoding of emotional memory. Neurobiol Learn Mem 2015;121:72–9In this study, REM sleep deprivation did not affect encoding in general, also REM sleep deprivation distinctly impaired vigilance at the time of encoding, similar to total sleep deprivation.
- 90.Mander BA, Santhanam S, Saletin JM, Walker MP. Wake deterioration and sleep restoration of human learning. Curr Biol 2011;21(5):R183–R4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Van Der Werf YD, Altena E, Vis JC, Koene T, Van Someren EJ. Reduction of nocturnal slow-wave activity affects daytime vigilance lapses and memory encoding but not reaction time or implicit learning. Prog Brain Res 193: Elsevier; 2011. p. 245–55. [DOI] [PubMed] [Google Scholar]
- 92. •.Lerner I, Lupkin SM, Sinha N, Tsai A, Gluck MA. Baseline Levels of Rapid Eye Movement Sleep May Protect Against Excessive Activity in Fear-Related Neural Circuitry. J Neurosci 2017;37(46):11233–44Results from this study indicate that higher baseline levels of REM sleep predict reduced fear-related activity in, and connectivity between, the hippocampus, amygdala, and ventromedial PFC during conditioning.
- 93.Silvestri AJ. REM sleep deprivation affects extinction of cued but not contextual fear conditioning. Physiol Behav 2005;84(3):343–9. [DOI] [PubMed] [Google Scholar]
- 94. •.Straus LD, Acheson DT, Risbrough VB, Drummond SPA. Sleep deprivation disrupts recall of conditioned fear extinction. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging 2017;2(2):123–9This study found that the 36-h pre-extinction total sleep deprivation group demonstrated significantly less extinction recall than the normal sleep group. There was no difference between the normal sleep and post-extinction 36-h total sleep deprivation group.
- 95. •.Seo J, Moore KN, Gazecki S, Bottary RM, Milad MR, Song H, et al. Delayed fear extinction in individuals with insomnia disorder. Sleep 2018;41(8):1–18.This study found that insomnia-disordered invidividuals may show a delayed acquisition of fear extinction memories.
- 96. •.Feng P, Becker B, Feng T, Zheng Y. Alter spontaneous activity in amygdala and vmPFC during fear consolidation following 24 h sleep deprivation. NeuroImage 2018;172:461–9This study found that sleep deprivation increased subjective and autonomic fear responses compared to controls at the stage of fear acquisition. At the stage of fear consolidation, sleep deprivation decreased ventromedial prefrontal cortex activity and increased amygdala activity. The findings suggest that sleep deprivation may weaken the top-down ability of the ventromedial prefrontal cortex to regulate amygdala activity during fear memory consolidation.
- 97.Spoormaker V, Sturm A, Andrade K, Schröter M, Goya-Maldonado R, Holsboer F, et al. The neural correlates and temporal sequence of the relationship between shock exposure, disturbed sleep and impaired consolidation of fear extinction. J Psychiatr Res 2010;44(16):1121–8. [DOI] [PubMed] [Google Scholar]
- 98.Marshall AJ, Acheson DT, Risbrough VB, Straus LD, Drummond SP. Fear conditioning, safety learning, and sleep in humans. J Neurosci 2014;34(35):11754–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. •.Straus LD, Norman SB, Risbrough VB, Acheson DT, Drummond SP. REM sleep and safety signal learning in posttraumatic stress disorder: a preliminary study in military veterans. Neurobiol Stress 2018;20(9):22–8.In a 3-day study of objective sleep and fear-potentiated startle performance, veterans who underwent safety learning more quickly showed more efficient REM sleep that night. Patients with more REM sleep on the last night of the study showed more safety recall.
- 100. •.Sripada RK, Rauch SAM. Between-session and within-session habituation in Prolonged Exposure Therapy for posttraumatic stress disorder: A hierarchical linear modeling approach. J Anxiety Disord 2015;30:81–7This study used hierarchical linear modeling to examine SUDS and found that high responders demonstrated differential between- but not within-session habituation.
- 101.Kleim B, Wilhelm FH, Temp L, Margraf J, Wiederhold B, Rasch B. Sleep enhances exposure therapy. Psychol Med 2014;44(7): 1511–9. [DOI] [PubMed] [Google Scholar]
- 102. ••.Colvonen PJ, Drummond SP, Angkaw AC, Norman SB. Piloting cognitive behavioral therapy for insomnia integrated with prolonged exposure. Psychol Trauma Theory Res PractPolicy 2019;11(1):107–13.The authors examined CBT-I prior to PE in a non-randomized study and found that both sleep and PTSD significantly improved. The authors suggest that addressing insomnia first may help increase efficacy of PE.
- 103.Graves LA, Heller EA, Pack AI, Abel T. Sleep deprivation selectively impairs memory consolidation for contextual fear conditioning. Learn Mem 2003;10(3):168–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. •.Duits P, Richter J, Baas JM, Engelhard IM, Limberg-Thiesen A, Heitland I, et al. Enhancing effects of contingency instructions on fear acquisition and extinction in anxiety disorders. J Abnorm Psychol 2017;126(4):378.This study found that anxiety disorder patients and healthy comparison participants are better able to discriminate between danger and safety cues when they have been explicitly informed about cues that announce a threat situation.