Abstract
Introduction:
We conducted a systematic review of the literature on cigar research on youth to identify potential future research agenda to generate evidence to inform cigar regulations to prevent cigar use among youth.
Methods:
We searched articles on Medline, EMBASE, and PsycINFO in April 2017 to identify articles relevant to cigars and adolescents. Two independent coders examined 48 articles to determine eligibility: 1) published between 2000-April 2017; 2) published in English; 3) conducted in the United States; 4) published in a peer-review journal; 5) examined cigars, cigarillos, or little cigars; 6) included youth (12-18 years old); and 7) included empirical data. Three independent coders reviewed the included articles (n=48) to identify whether the studies addressed FDA’s Research Priorities.
Results:
The studies addressed FDA’s Research Priorities of “behavior” (n=48), “communications” (n=4), “marketing influences” (n=1), and “impact analysis” (n=1). Studies on “behavior” underscored the need for improvements in measurement, such as using brand names and distinguishing cigar products. The review revealed the need for restrictions on cigar flavors, development of media campaigns and interventions, increasing the cost (via taxation), and evaluating the impact of cigar policies.
Conclusions:
The studies mostly focused on surveillance of behaviors and use patterns, which revealed cigar specific issues to address in policies to decrease cigar use among youth. The lack of studies addressing other FDA’s research priorities highlighted the critical need for future studies that inform prevention of youth cigar use.
Keywords: Cigars, Cigarillos, Little Cigars, Youth, Adolescents, Review
1. INTRODUCTION
Cigars (defined as large or little cigars or cigarillos) are tobacco products consisting of tobacco that is wrapped in leaf tobacco or in a paper wrapper that contains tobacco, in comparison to cigarettes, which are wrapped in a paper that does not contain tobacco. Cigars come in different sizes and are referred to by different names (CDC, 2014b). Traditional large cigars contain aged, fermented tobacco and take about one to two hours to smoke. Cigarillos are longer and slimmer (about 3-4 inches) than cigarettes. They sometimes come with wood or plastic tip filters or without any filters. Little cigars are typically the same size as cigarettes and may contain a filter.
Cigars are popular among youth in the United States (US). Prevalence of past-30-day cigar use among US youth is double the use rate observed among US adults (12.6% vs. 5.4%; CDC, 2014c), and lifetime use of cigars is high at 30.5% among high school (HS) students and 8.9% among middle school (MS) students (CDC, 2013).
Cigars may appeal to youth because they come in appealing flavors (King, Tynan, Dube, & Arrazola, 2014) and have lower per-unit cost than cigarettes (Delnevo, Hrywna, Giovenco, Miller Lo, & O'Connor, 2016). Another characteristic that appeals to youth is the ability to manipulate cigars to create blunts (i.e., hollowing out tobacco in cigar to replace it with marijuana) (Schauer, Rosenberry, & Peters, 2017). Cigar use among youth is concerning because cigar use is not a safe alternative to cigarette use. Indeed, cigars are more toxic than cigarettes, and sustained use causes cancers of the lung and upper aerodigestive tract (Baker et al., 2000). However, in contrast to the large body of research on cigarettes, and more recently on e-cigarettes, less is known about cigars.
Accumulating epidemiological studies, which indicate the high prevalence of cigar use among youth, coupled with adverse health consequences of cigar smoking, demonstrate an urgent need to develop comprehensive tobacco control policies and programs focused on preventing cigar use among youth. Cigars have not been regulated until recently, when in May, 2016 the Food and Drug Administration (FDA) released the final rules regarding deeming tobacco products (FDA, 2016). This historic rule extends the FDA’s authority over all tobacco products, including cigars. However, this rule continues to be challenged. The FDA is currently reconsidering exempting premium cigars from their regulatory authority (FDA, 2018a). It is imperative that cigar products, like cigarillos and little cigars, are regulated because these products have characteristics that appeal to youth (e.g., flavors, cheap cost).
To inform the FDA’s regulation of tobacco products, including cigars, FDA’s Center for Tobacco Product (CTP) defined the following research priority areas to understand: 1) toxicity: how tobacco products cause tobacco-related harm; 2) addiction: the effect of tobacco product characteristics on abuse and liability; 3) health effects: the short- and long-term health effects of tobacco products; 4) behavior: the attitudes, knowledge, and behaviors related to tobacco product use and tobacco product characteristics; 5) communications: how to communicate to the public regarding nicotine and health effects of tobacco products; 6) marketing influences: how people initiate and continue to use tobacco products via exposure to tobacco product advertisements; and 7) impact analysis: the impact of FDA’s regulatory actions (FDA, 2018b).
There has not yet been a thorough examination of the literature to assess to what extent research studies have addressed FDA’s Research Priorities specifically related to cigars research on youth. Thus, the goal of this study was to conduct a systematic review of the literature on cigar research on youth published between 2000 and April 2017 using a US sample (FDA has jurisdiction over only the US) to assess whether the existing research addressed any of the FDA’s Research Priority areas, and to set future research agenda aimed at informing a comprehensive effort to reduce youth cigar use.
2. METHODS
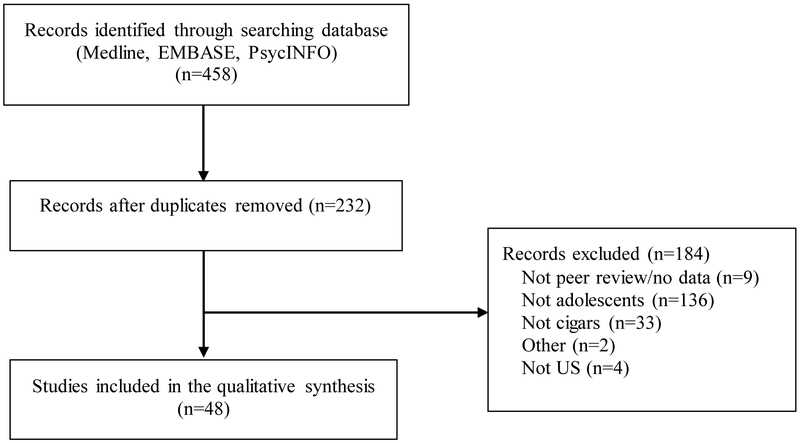
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for this systematic review (Moher, Liberati, Tetzlaff, Altman, & Group, 2009). We searched the terms “cigar” or “cigarillo,” and “adolescents” limited to articles published in English between 2000 and April 2017 (when the search was conducted) on Medline, PsycINFO, and EMBASE. Two independent reviewers reviewed the abstracts of the identified articles to determine eligibility. See Figure 1 for the number of articles included/excluded and reasons for exclusion. Any discrepancies between the coders were amended. To be included, the articles had to 1) be peer-reviewed, 2) contain empirical data (e.g., review articles and commentaries were excluded); 3) have a sample from the US (FDA’s regulatory authority only applies to the US); 4) have a sample of adolescents between the ages of 12 and 18, and if older age groups were in the study, results had to be stratified by the adolescent age group; and 5) include data on traditional cigars, little cigars, or cigarillos.
Figure 1. Flowchart of study selection.
Note: Studies may have been excluded for more than one reason, but reasons for exclusions were tabulated in the order presented.
Next, two coders independently reviewed all included articles and then compared their codes to resolve any discrepancies; a third coder reviewed the coding of all included articles. To better understand the tobacco control domains in context, the articles were first coded for study characteristics (i.e., the study design, the location where the study was conducted) and sample characteristics (i.e., demographics). The included articles were then coded for FDA’s Research Priorities.
3. RESULTS
Forty-eight studies were included in this systematic review. Please see supplementary material for the full references of the reviewed articles. The average publication year was 2011 (SD = 4.72 years, Min = 2000, Max = 2017). Study design and location and sample characteristics were summarized below and listed in detail in Supplementary Table 1. In brief, 27 studies used cross-sectional surveys, ten studies used cross-sectional surveys over time, five studies used longitudinal surveys, two studies used qualitative studies (i.e., focus groups, interviews), and four studies used mixed-method studies (e.g., surveys/focus groups).
In terms of the sample characteristics, 19 studies had a sample that represented different racial/ethnic backgrounds (e.g., White, Black, Hispanic), 19 studies assessed race but did not report race for the overall sample, three studies had predominantly White participants, three studies had predominantly Black participants, three studies did not report race/ethnicity, and one study had all American Indian/Alaskan Native participants.
3.1. FDA’s Research Priorities
The included studies examined the FDA’s Research Priority domains of “behavior,” “communications,” “marketing influence,” and “impact analysis.” These domains are described below in the order of most examined to least examined.
3.1.1. Behavior:
All studies included in this review addressed the research domain of “behavior” by assessing behaviors and perceptions related to cigar use. Thirty-seven studies defined the term “cigar” as an encompassing term that included cigars, little cigars, and cigarillos; seven studies did not specify how cigars were defined; and four studies specified and examined only cigarillos. We also use the word “cigars” in this review as an encompassing word to include cigars, little cigars, and cigarillos, as the studies have done to summarize their findings, unless otherwise specified.
3.1.1.1. Use Behaviors:
Studies assessing cigar use (n=43) were further categorized into 1) correlates/predictors of use (n=36); 2) prevalence of use over time (n=12); 3) prevalence of use with the addition of brand names (n=6); 4) prevalence of use compared to prevalence of blunt/marijuana use (n=4); 5) prevalence of flavored cigar use (n=3); and 6) other (n=2).
A total of 36 studies examined correlates/predictors of cigar use; such as, sociodemographic variables, substance use, and tobacco use characteristics (e.g., susceptibility, age at initiation, dependence). Of the studies (n=12) that examined changes in prevalence of cigar use over time, five studies reported that prevalence of cigar use decreased over time, whereas six studies reported that prevalence of cigar use increased over time, and one study did not provide changes in prevalence of cigar use among the total sample.
Use rates varied depending on a variety of factors such as the definition of cigar use (e.g., past 30 days, lifetime), the characteristics of the sample (e.g., age, tobacco use status); survey location (e.g., national, local), and the description of the product (e.g., using brand names to describe the product, cigar type). Cigar use was high if lifetime-use definition was used, if the sample was older, used other tobacco products, or if brand names were provided.
Interestingly, 17 studies examined race differences in cigar use rates. Of these studies, 10 studies observed that cigar use was higher among Black youth relative to the reference group of either White or non-Black youth, three studies observed that cigar use was higher among White youth than other race groups, and four studies did not observe differences in cigar use by race.
Six studies examined use rates after adding a brand name to the question assessing cigar use. All of these studies observed that adding a brand name to the question increased cigar use rates compared to when a brand name was not used in the question. Four of these studies observed that this increase was higher among Black youth. Four studies reported prevalence of cigar use and prevalence of blunt or marijuana use. These studies reported high concordance between marijuana/blunt use and cigar use. Of note, youth had difficulty differentiating between cigars and blunts, and blunt users did not view themselves to be cigar users. Three studies reported prevalence of flavored cigar use. These studies observed that flavored cigar use was high among youth and that youth who used flavored little cigars had lower intentions to quit tobacco use than youth who used non-flavored little cigars.
It is important to note that eight studies did not examine cigars as a central topic area but rather as a predictor of other areas of interest, such as other tobacco use behaviors and risk behaviors.
3.1.1.2. Perceptions:
In general, cigars were viewed as being harmful to health, but health perceptions relative to cigarettes varied, with some youth perceiving cigars to have lower risk than cigarettes and some perceiving that cigars did not contain nicotine or tobacco. Other perceptions include cigars being easy to obtain and using them primarily for blunts. One survey study examined subjective experiences of cigar products, along with other tobacco products, at first use. This study observed that positive subjective experience of feeling buzzed at initial use was associated with current use of cigars.
3.1.2. Communications:
Four studies addressed the research domain of “communications.” Three of these studies reported findings related to media prevention campaigns. Syu, Huang, and Huang (2010) evaluated a cigarillo media campaign delivered over the radio, television, billboards, internet, and signage in public locations (e.g., subway stations) for 18 months in Baltimore, MD. They observed that compared to the control group, the exposed group reported fewer number of cigarillos smoked per day. Malone, Yerger, and Pearson (2001) assessed youth’s exposure to cigar prevention programs through the use of focus groups and found that youth did not recall being exposed to cigar prevention programs, but they were able to recall seeing cigarette prevention campaigns. Ringel, Wasserman, and Andreyeva (2005) examined exposure to anti-tobacco campaigns as one aspect of the comprehensive state tobacco control policies (see Impact Analysis). Finally, Kowitt, Jarman, Ranney, and Goldstein (2017) examined believability of cigar health warning labels using an experimental study. In this study, youth were exposed to one of three health warning messages regarding cigar smoking and then reported on believability of those warning messages. The results identified that certain messages, such as messages about cigar smoking causing lung cancer and heart diseases, were found to be most believable.
3.1.3. Marketing Influences:
One study addressed the research domain of “marketing influences.” Portnoy, Wu, Tworek, Chen, and Borek (2014) study observed that tobacco advertisement exposure, even if not specific to cigars, was associated with curiosity to use cigars (and use of other tobacco products) among youth who did not use tobacco products.
3.1.4. Impact analysis:
One study addressed “impact analysis” by examining cigar-related policies, such as exposure to anti-tobacco campaigns, youth access restrictions, direct restrictions on cigar use (i.e., clean indoor air law), and taxation. Ringel et al. (2005) showed that the increase in the price of cigars was associated with a decrease in cigar use; youth were two to three times more responsive to tobacco price changes than adults. However, state control policies (e.g., purchase law, possession of use law, clean indoor air law, state-sponsored media campaigns) were not associated with decreasing youth cigar use.
4. DISCUSSION
This is the first systematic review to examine whether cigar research on youth has addressed FDA’s Research Priority areas and to identify future research agenda to prevent youth cigar use. We observed that all of the identified studies examined FDA’s Research Priority of “behavior,” which includes use patterns and perceptions. Surveillance of behaviors and perceptions related to tobacco use is important to examine because it can identify specific problematic use behaviors and perceptions related to tobacco use that could be addressed through interventions and policy changes. Furthermore, surveillance is also important in assessing the implementation and outcome of policy changes and impact over time (CDC, 2014a).
While all studies examined the research area of “behavior,” very few studies examined other research priority areas. Of the included studies, four studies examined “communications,” one study examined “marketing influences,” and one study examined “impact analysis.” Notably, no studies examined the research areas of “toxicity,” “addiction,” or “health effects.” Our review underscores the need for diversity in cigar research that addresses all of the FDA’s Research Priorities.
In the following sections, we discuss our research findings in the context of developing a future research agenda to inform cigar policies to prevent youth cigar use.
4.1. “Behavior”: Cigar use rates
Studies reporting on youth cigar use rates showed varying rates of use, suggesting that use rates depend on several important factors: the sample examined, the brand names used, the terms used to refer to cigars, and blunt use.
Overall, studies assessing behaviors and perceptions related to cigars examined diverse ethnic/racial youth populations covering a range of geographic regions within the US. Some studies observed racial differences. For instance, studies observed that cigar use is higher among Black youth than among non-Black youth, particularly when a brand name is used to refer to cigars. For example, Corey et al. (2014) observed that the addition of brand names in the 2012 national survey yielded a lifetime cigar use rate that was 43% higher among Black youth, compared to the 2011 survey that did not use the brand name, whereas no changes were observed when the brand name was not used. Our review findings support findings that brand names should be used when assessing cigars.
Use rates also varied by different cigar product type (e.g., cigarillos, little cigars, large cigars) and frequency of use (e.g., lifetime use, past-30-day use) examined. The majority of studies used the term “cigars” as an all-encompassing term, which included large cigars, little cigars, and cigarillos. However, the grouping of these disparate products into a single broad cigar product is problematic because these products have unique characteristics and could even be considered disparate products (Henningfield, Fant, Radzius, & Frost, 1999). Furthermore, use patterns and perceptions are specific to each cigar product, so grouping all of them together may obfuscate these differences. For instance, youth are more likely to use machine made, cigarette-sized little cigar products and other popular cigar brands such as Black and Mild, and perceive premium cigars as a product used by wealthy and older adults (Cullen et al., 2011; Malone et al., 2001). Future studies should distinguish between different cigar products.
When assessing use rates, blunt use should be considered. Youth have difficulty differentiating between cigars and blunts, and some blunt users do not view themselves as cigar users (e.g., Delnevo, Bover-Manderski, & Hrywna, 2011). More research is needed on blunt use among youth; research could examine cigar features that make marijuana use appealing and the role of cigar use in maintaining marijuana use, as well as the role of marijuana in maintaining cigar and other tobacco product use. Although marijuana is not under FDA’s regulatory purview, effective regulations of cigar products must take marijuana into consideration because youth use cigars to smoke marijuana in the form of blunts.
In sum, these findings indicate the need for improvements in cigar use measurement. Efforts should also focus on continued surveillance of cigar use in the context of marijuana use.
4.2. “Behaviors”: Flavored cigar use
While flavors, excluding menthol and tobacco, are banned from cigarettes, they are still permitted in cigars (FDA, 2015). Flavored little cigars comprise over 80% of overall cigar sales (FTC, 1999), and 95% of cigars sold in retail tobacco outlets are flavored products (Cantrell et al., 2013). Despite the well-established evidence that flavors, which can mask the natural harshness and taste of tobacco, increase appeal to youth (Carpenter, Wayne, Pauly, Koh, & Connolly, 2005; Klein et al., 2010), the research on flavored cigars is still an understudied domain according to our study. Future studies should examine whether banning flavors on cigars would discourage young initiates. It is particularly important to focus research on flavored cigars because the FDA has recently announced their plans to prevent youth access to flavored tobacco products and ban menthol flavors in cigarettes and cigars (FDA, 2019).
4.3. “Communications”: Prevention Campaigns
We only identified one study that developed and evaluated a media prevention campaign that focused specifically on cigarillo use (Syu et al., 2010), which indicates a strong need for more effective cigar prevention campaigns focused on youth. Youth-focused cigar prevention campaigns are important because mass media campaigns have shown to be successful in reducing youth cigarette smoking (National Cancer Institute, 2008; Wilson et al., 2012). Importantly, the FDA has the authority to develop and launch comprehensive mass media campaigns (FDA, May 10, 2016); thus, more comprehensive research is needed to assess the unique themes that could be used in youth cigar prevention/education campaigns.
Our study findings suggest that cigar prevention campaigns could include an educational component that discusses the health risks of cigar use in the context of blunt use, because youth have difficulty differentiating between cigars and blunts and the popularity of blunt use among youth (e.g., Stephens, Ogunsanya, Ford, Bamgbade, & Liang, 2015). For instance, these prevention messages could inform youth that using blunts increases the risk of developing addiction to both substances and increases exposure to health risks. Additionally, these campaigns should target and tailor the prevention messages to vulnerable populations of youth, such as Black youth who have higher cigar use rates (e.g., Nasim, Blank, Berry, & Eissenberg, 2012).
4.4. “Communications”: Health Warning Messages
Only one study examined the domain of health warning messages specific to cigars. Kowitt et al. (2017) examined believability of cigar-specific health warning messages and observed that youth found certain health messages more believable than others. Health warning messages that aim to prevent youth cigar use should identify targeted messages that are relevant for youth. For example, studies on cigar perceptions included in this study showed that youth had misconceptions of cigars, such as cigars have lower health risks than cigarettes and cigars do not contain nicotine. Such misconceptions could be addressed through the development of effective and believable health warning messages.
4.5. “Marketing Influences”: Advertisement Restrictions
Advertisement restrictions, including point-of-sale marketing, are domains that are important in tobacco regulation, but which have not been sufficiently examined in the studies included in this review. Only one study examined this domain and observed that tobacco advertising exposure was associated with curiosity to use cigars among non-tobacco using youth (Portnoy et al., 2014). More studies on this domain are needed as innovations in tobacco advertisements, particularly on social media, continue to grow without any regulatory oversight.
4.6. “Impact Analysis”
One study (i.e., Ringel et al., 2005) was an in-depth analysis of various cigar-related policies, such as exposure to anti-tobacco campaigns, youth access restrictions, direct restrictions on cigar use (i.e., clean indoor air law), and taxation. This study showed that among these various policies, the policy to increase the price of cigars was most effective in decreasing youth cigar use. Cigars are currently taxed at a lower rate and are cheaper than cigarettes (Campaign for Tobacco-Free Kids, 2016). In states with high cigarette tax, a pack of 20 little cigars may cost half as much as a pack of 20 cigarettes (Delnevo, Hrywna, Foulds, & Steinberg, 2004). Furthermore, small flavored cigars are sold in a single or a double unit pack for very low prices (e.g., $.99). Youth are more sensitive to price changes than adults (Ross & Chaloupka, 2003). Thus, taxation may be an effective cigar control strategy. Even though taxation is not under FDA’s purview, states can increase taxes on cigar products.
This study also found that policies such as purchase law, possession of use law, clean indoor air law, state-sponsored media campaigns were not associated with decrease in cigar use. However, ongoing evaluation of evolving cigar policies, as well as the effect of non-cigar related tobacco policies on cigar use is needed, as use patterns, marketing practices, and perceptions continue to evolve with the changing tobacco use climate.
There are already some policies aimed at reducing youth access to cigar products. For instance, the FDA instituted a federal rule banning the sale of cigars to minors under the age of 18 years old (FDA, May 10, 2016). Additionally, several states are increasing the age of tobacco sale to 21 years old (i.e., Tobacco 21) (Morain, Winickoff, & Mello, 2016). Although at face value, Tobacco 21 Laws appear to target young adults 18 to 20 years old, Tobacco 21 has the strongest influence on adolescents 15 to 17 years old (Kessel Schneider, Buka, Dash, Winickoff, & Donnell, 2016). However, whether these laws differently influence youth cigar access compared to cigarette or other tobacco product access is unknown. Previous research showed that laws and regulations prohibiting the sale of cigars to minors are not enforced properly (USDHHS, 1999). Indeed, one focus group study that examined youth access to cigars showed that youth reported that cigars were easily obtained at local stores (Malone et al., 2001). Thus, future studies should assess the compliance and enforcement of the restrictions of these laws.
4.7. Limitations
This systematic review covered the time period between 2000 and 2017 and did not include recently published studies, or studies which are ongoing. It is important to note that some of the studies were conducted before FDA’s Research Priorities were released, so recent studies may be more responsive to the FDA’s Research Priorities. Our findings related to cigar use should be considered with the understanding that this review focused on US studies. While studies outside of the US could be beneficial in informing regulations within the US, the number of available studies outside of the US was small (n = 4; e.g., Canada, Romania, Argentina). A future review could focus on international studies of cigar use when there are sufficient studies to make meaningful comparisons that consider the unique cultural and tobacco control contexts of studies across countries. Finally, we did not examine prevention/cessation interventions, which is an important tobacco control domain but not part of FDA’s authority. Future studies should focus on developing effective youth-based cigar prevention/cessation interventions.
4.8. Conclusions
Our systematic review of the literature on cigar research on youth demonstrated that all included studies addressed FDA’s Research Priority of “behavior,” which examined themes of correlates/predictors of cigar use, use over time, use with the addition of brand names, use compared to blunt/marijuana use, use of flavored cigar use, and perceptions related to cigars. These findings suggest that the literature on cigar research on youth between 2000 and 2017 focused much on surveillance of behaviors and perceptions. The findings of these studies have been instrumental in enhancing awareness of the growing problem of cigar use among youth and identifying cigar specific issues to address in policies to decrease youth cigar use (e.g., cost, appealing flavors, cigar measurement issues, disparities in vulnerable populations). However, the lack of studies that directly informs prevention of youth cigar use (e.g., mass media campaigns, advertising restrictions) suggests the critical need for future studies to achieve the overall goal of preventing youth combustible tobacco use, including cigar use.
Supplementary Material
Table 1.
FDA Research Priorities identified in the systematic review
| FDA Research Priorities | Number of studies |
|---|---|
| 1. Behavior | 48 |
| a. Use patterns | |
| i. Correlates/predictors of cigar use | 36 |
| ii. Prevalence of use over time | 12 |
| iii. Prevalence of use with the addition of brand names | 6 |
| iv. Prevalence of use compared to blunt /marijuana use | 4 |
| v. Prevalence of flavored cigar use | 3 |
| vi. Other | 2 |
| b. Perceptions | 7 |
| 2. Communications | 4 |
| a. Mass media/public media campaigns | 3 |
| b. Health warning labels | 1 |
| 3. Marketing influences | 1 |
| a. Advertising restrictions | 1 |
| 4. Impact analysis | 1 |
| a. Monetary cost, restrictions on use, youth access | 1 |
| 5. Toxicity | 0 |
| 6. Addiction | 0 |
| 7. Health Effects | 0 |
Note: Studies can be included in more than one category.
Highlights.
Systematic review identified 48 US studies on cigars and adolescents (2000-2017).
100% of the studies addressed the FDA’s research priorities of “behavior.”
8% addressed “communications,” 2% addressed marketing, and 2% addressed impact.
Acknowledgments
FUNDING
This project was completed as part of the collaborative research being conducted by the National Institutes of Health (NIH) and Food and Drug Administration (FDA) Tobacco Centers of Regulatory Science (TCORS) Cigar Measurement Working Group. The research was supported in part by the P50DA036151 from National Institute on Drug Abuse (NIDA) at the NIH and the FDA Center for Tobacco Products (CTP; GK, PS, DAC, KG); grant numbers P50CA180907 (JCR) and P50CA180906 (MRC, JTH) from the National Cancer Institute and the FDA CTP, and NIDA L40 DA042454 (PS). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA.
Abbreviations:
- FDA
Food and Drug Administration
- HS
high school
- MS
middle school
Footnotes
CONFLICTS OF INTEREST
The authors do not have any financial relationships or conflicts of interest relevant to this article to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baker F, Ainsworth SR, Dye JT, Crammer C, Thun MJ, Hoffman D, … Shopland DR (2000). Health risks associated with cigar smoking. JAMA, 284(6), 735–740. doi: 10.1001/jama.284.6.735 [DOI] [PubMed] [Google Scholar]
- Campaign for Tobacco-Free Kids. (2016). State excise tax rates for non-cigarette tobacco products. from https://www.tobaccofreekids.org/research/factsheets/pdf/0169.pdf
- Cantrell J, Kreslake JM, Ganz O, Pearson JL, Vallone D, Anesetti-Rothermel A, … Kirchner TR (2013). Marketing little cigars and cigarillos: Advertising, price, and associations with neighborhood demographics. American Journal of Public Health, 103, 1902–1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter CM, Wayne GF, Pauly JL, Koh HK, & Connolly GN (2005). New cigarette brands with flavors that appeal to youth: Tobacco marketing strategies. Health Affairs, 24, 1601–1610. doi: 10.1377/hlthaff.24.6.1601 [DOI] [PubMed] [Google Scholar]
- Cavazos-Rehg PA, Krauss MJ, Spitznagel EL, Lowery A, Grucza RA, Chaloupka FJ, & Bierut LJ (2014). Monitoring of non-cigarette tobacco use using Google Trends. Tobacco Control. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. (2013). Tobacco product use among middle and high school students-United States, 2011 and 2012. Morbidity and Mortality Weekly Report, 62, 893–897. [PMC free article] [PubMed] [Google Scholar]
- CDC. (2014a). Best Practices for Comprehensive Tobacco Control Programs—2014. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. [Google Scholar]
- CDC. (2014b). Little filtered cigar, cigarillo, and premium cigar smoking among adults — United States, 2012–2013. Morbidity and Mortality Weekly Report (MMWR), 63, 650–654. [PMC free article] [PubMed] [Google Scholar]
- CDC. (2014c). Smoking and tobacco use. Retrieved March 17, 2015, from http://www.cdc.gov/tobacco/data_statistics/fact_sheets/tobacco_industry/cigars/
- Cohn A, Johnson A, Ehlke S, & Villanti AC (2016). Characterizing substance use and mental health profiles of cigar, blunt, and non-blunt marijuana users from the National Survey of Drug Use and Health. Drug and Alcohol Dependence, 160, 105–111. doi: https://doi.Org/10.1016/j.drugalcdep.2015.12.017 [DOI] [PubMed] [Google Scholar]
- Corey CG, Ambrose BK, Apelberg BJ, & King BA (2015). Flavored tobacco product use among middle and high school students --United States, 2014. Morbidity & Mortality Weekly Report (MMWR), 64, 1066–1070. [DOI] [PubMed] [Google Scholar]
- Corey CG, Dube SR, Ambrose BK, King BA, Apelberg BJ, & Husten CG (2014). Cigar smoking among U.S. students: reported use after adding brands to survey items. American Journal of Preventive Medicine, 47(2, Supplement 1), S28–S35. doi: http://dx.doi.Org/10.1016/j.amepre.2014.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen J, Mowery P, Delnevo C, Allen JA, Sokol N, Byron MJ, & Thornton-Bullock A (2011). Seven-year patterns in US cigar use epidemiology among young adults aged 18–25 years: A focus on race/ethnicity and brand. American Journal of Public Health, 101(10), 1955–1962. doi: 10.2105/AJPH.2011.300209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delnevo CD, Bover-Manderski MT, & Hrywna M (2011). Cigar, marijuana, and blunt use among US adolescents: Are we accurately estimating the prevalence of cigar smoking among youth? Preventive Medicine, 52(6), 475–476. doi: 10.1016/j.ypmed.2011.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delnevo CD, Giovenco DP, Ambrose BK, Corey CG, & Conway KP (2014). Preference for flavoured cigar brands among youth, young adults and adults in the USA. Tobacco Control. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delnevo CD, Hrywna M, Foulds J, & Steinberg M (2004). Cigar use before and after a cigarette excise tax increase in New Jersey. Addictive Behaviors, 29(9), 1779–1807. [DOI] [PubMed] [Google Scholar]
- Delnevo CD, Hrywna M, Giovenco DP, Miller Lo EJ, & O'Connor RJ (2016). Close, but no cigar: certain cigars are pseudo-cigarettes designed to evade regulation. Tobacco Control, doi: 10.1136/tobaccocontrol-2016-052935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elfassy T, Yi SS, & Kansagra SM (2015). Trends in cigarette, cigar, and smokeless tobacco use among New York City public high school youth smokers, 2001–2013. Preventive Medicine Reports, 2, 488–491. doi: 10.1016/j.pmedr.2015.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- FDA. (2015). Deeming-Extending Authorities to Additional Tobacco Products. December/10/15, from http://www.fda.gov/TobaccoProducts/Labeling/ucm388395.htm
- FDA. (2016). Deeming Tobacco Products To Be Subject to the Federal Food, Drug, and Cosmetic Act, as Amended by the Family Smoking Prevention and Tobacco Control Act; Restrictions on the Sale and Distribution of Tobacco Products and Required Warning Statements for Tobacco Product. Federal Register, 81. [PubMed] [Google Scholar]
- FDA. (2018a). Regulation of premium cigars, from https://www.federalregister.gov/documents/2018/03/26/2018-06047/regulation-of-premium-cigars
- FDA. (2018b). Research Priorities. Retrieved December/18/18, from https://www.fda.gov/TobaccoProducts/PublicHealthScienceResearch/Research/ucm311860.htm
- FDA. (2019). Menthol and Other Flavors in Tobacco Products. from https://www.fda.gov/tobaccoproducts/labeling/productsingredientscomponents/ucm2019416.htm
- FDA. (May 10, 2016). Deeming Tobacco Products To Be Subject to the Federal Food, Drug, and Cosmetic Act, as Amended by the Family Smoking Prevention and Tobacco Control Act; Restrictions on the Sale and Distribution of Tobacco Products and Required Warning Statements for Tobacco Products. Federal Register, 21 CFR Parts 1100, 1140, and 1143, 81(90). [PubMed] [Google Scholar]
- FTC. (1999). Federal Trade Commission report to Congress on cigar sales and advertising and promotional expenditures for calendar years 1996 and 1997. Washington, DC: Federal Trade Commission. [Google Scholar]
- Gilreath TD, Leventhal A, Barrington-Trimis JL, Unger JB, Cruz TB, Berhane K, … McConnell R (2016). Patterns of alternative tobacco product use: Emergence of hookah and e-cigarettes as preferred products amongst youth. The Journal of adolescent health : official publication of the Society for Adolescent Medicine, 58(2), 181–185. doi: 10.1016/j.jadohealth.2015.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell PT, Naqvi SMH, Plunk AD, Ji M, & Martins SS (2017). Patterns of youth tobacco and polytobacco usage: The shift to alternative tobacco products. The American Journal of Drug and Alcohol Abuse, 43(6), 694–702. doi: 10.1080/00952990.2016.1225072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henningfield JE, Fant RV, Radzius A, & Frost S (1999). Nicotine concentration, smoke pH and whole tobacco aqueous pH of some cigar brands and types popular in the United States. Nicotine & Tobacco Research, 1, 163–168. [DOI] [PubMed] [Google Scholar]
- Huh J, & Leventhal AM (2016). Progression of poly-tobacco product use patterns in adolescents. American Journal of Preventive Medicine, 51(4), 513–517. doi: 10.1016/j.amepre.2016.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy SM, Caraballo RS, Rolle IV, & Rock VJ (2016). Not just cigarettes: A more comprehensive look at marijuana and tobacco use among African American and White youth and young adults. Nicotine & Tobacco Research, 18(Suppl 1), S65–S72. doi: 10.1093/ntr/ntv202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessel Schneider S, Buka SL, Dash K, Winickoff JP, & Donnell L (2016). Community reductions in youth smoking after raising the minimum tobacco sales age to 21. Tobacco Control, 25(3), 355. doi: 10.1136/tobaccocontrol-2014-052207 [DOI] [PubMed] [Google Scholar]
- King BA, Tynan MA, Dube SR, & Arrazola R (2014). Flavored-little-cigar and flavored-cigarette use among U.S. middle and high school students. Journal of Adolescent Health, 54(1), 40–46. doi: 10.1016/j.jadohealth.2013.07.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein SM, Giovino GA, Barker DC, Tworek C, Cummings KM, & O'Connor RJ (2010). Use of flavored cigarettes among older adolescent and adult smokers: United States, 2004--2005. Nicotine & Tobacco Research, 2008, 1029–1214. doi: 10.1080/14622200802163159 [DOI] [PubMed] [Google Scholar]
- Kowitt SD, Jarman K, Ranney LM, & Goldstein AO (2017). Believability of cigar warning labels among adolescents. The Journal of Adolescent Health, 60(3), 299–305. doi: 10.1016/j.jadohealth.2016.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y, Hebert CJ, Nonnemaker JM, & Kim AE (2015). Youth tobacco product use in the United States. Pediatrics, 135, 409–415. doi: 10.1542/peds.2014-3202 [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Strong DR, Kirkpatrick MG, & et al. (2015). Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA, 314(7), 700–707. doi: 10.1001/jama.2015.8950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malone RE, Yerger V, & Pearson C (2001). Cigar risk perceptions in focus groups of urban African American youth. Journal of Substance Abuse, 13, 549–561. [DOI] [PubMed] [Google Scholar]
- Mantey DS, Harrell MB, Case K, Crook B, Kelder SH, & Perry CL (2017).Subjective experiences at first use of cigarette, e-cigarettes, hookah, and cigar products among Texas adolescents. Drug and Alcohol Dependence, 173, 10–16. doi: 10.1016/j.drugalcdep.2016.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClelland E, Valentine N, & McMillen R (2015). Tobacco use trends among Mississippi youth following the 1997 Settlement of Mississippi's Medicaid Lawsuit and subsequent tobacco prevention initiatives. Journal of the Mississippi State Medical Association, 56, 328–333. [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & Group P (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ, 339, b2535. doi: 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morain SR, Winickoff JP, & Mello MM (2016). Have Tobacco 21 Laws Come of Age? New England Journal of Medicine, 374(17), 1601–1604. doi: 10.1056/NEJMp1603294 [DOI] [PubMed] [Google Scholar]
- Nasim A, Blank MD, Berry BM, & Eissenberg T (2012). Cigar use misreporting among youth: Data from the 2009 Youth Tobacco Survey, Virginia. Preventing Chronic Disease, 9(E42). doi: 10.5888/pcd9.110084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute. (2008). The role of the media in promoting and reducing tobacco use Tobacco Control Monograph. No 19 . Bethesda, MD: US Department of Health and Human Services, National Institutes of Health, National Cancer Institute. [Google Scholar]
- Page JB, & Evans S (2003). Cigars, cigarillos, and youth: Emergent patterns in subcultural complexes. Journal of Ethnicity in Substance Abuse, 2, 63–76. [Google Scholar]
- Parker EM, & Bradshaw CP (2015). Teen dating violence victimization and patterns of substance use among high school students. Journal of Adolescent Health, 57(4), 441–447. doi: 10.1016/j.jadohealth.2015.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesko MF, Hughes JM, & Faisal FS (2016). The influence of electronic cigarette age purchasing restrictions on adolescent tobacco and marijuana use. Preventive Medicine, 87, 207–212. doi: 10.1016/j.ypmed.2016.02.001 [DOI] [PubMed] [Google Scholar]
- Portnoy DB, Wu CC, Tworek C, Chen J, & Borek N (2014). Youth curiosity about cigarettes, smokeless tobacco, and cigars: Prevalence and associations with advertising. American Journal of Preventive Medicine, 47(2, Supplement 1), S76–S86. doi: 10.1016/j.amepre.2014.04.012 [DOI] [PubMed] [Google Scholar]
- Primack BA, Walsh M, Bryce C, & Eissenberg T (2009). Water-pipe tobacco smoking among middle and high school students in Arizona. Pediatrics, 123, e282–e288. doi: 10.1542/peds.2008-1663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proescholdbell SK, Summerlin-Long SK, & Goldstein AO (2009). Declining tobacco use among North Carolina middle and high school students: 1999-2007. North Carolina Medical Journal, 70, 205–212. [PubMed] [Google Scholar]
- Rait MA, Prochaska JJ, & Rubinstein ML (2016). Reporting of cigar use among adolescent tobacco smokers. Addictive Behaviors, 53, 206–209. doi: 10.1016/j.addbeh.2015.06.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ringel JS, Wasserman J, & Andreyeva T (2005). Effects of public policy on adolescents’ cigar use: evidence from the National Youth Tobacco Survey. American Journal of Public Health, 95, 995–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, Rosario M, Calzo JP, Corliss HL, Frazier L, & Austin SB (2014). Masculine boys, feminine girls and cancer risk behaviors: An 11-year longitudinal study. The Journal of adolescent health : official publication of the Society for Adolescent Medicine, 55(3), 373–379. doi: 10.1016/j.jadohealth.2014.02.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross H, & Chaloupka FJ (2003). The effect of cigarette prices on youth smoking. Health Economics, 12(3), 217–230. doi: 10.1002/hec.709 [DOI] [PubMed] [Google Scholar]
- Saunders C, & Geletko K (2012). Adolescent cigarette smokers’ and non-cigarette smokers’ use of alternative tobacco products. Nicotine & Tobacco Research, 14(8), 977–985. doi: 10.1093/ntr/ntr323 [DOI] [PubMed] [Google Scholar]
- Schauer GL, Rosenberry ZR, & Peters EN (2017). Marijuana and tobacco co-administration in blunts, spliffs, and mulled cigarettes: A systematic literature review. Addictive Behaviors, 64, 200–211. doi: https://doi.Org/10.1016/j.addbeh.2016.09.001 [DOI] [PubMed] [Google Scholar]
- Schuster RM, Hertel AW, & Mermelstein R (2013). Cigar, cigarillo, and little cigar use among current cigarette-smoking adolescents. Nicotine & Tobacco Research, 15(5), 925–931. doi: 10.1093/ntr/nts222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M, Mirhej G, Page JB, Hastings E, Salaheen H, & Prado G (2008). Black 'N Mild and carcinogenic. Journal of Ethnicity in Substance Abuse, 6(3-4), 81–94. doi: 10.1300/J233v06n03-03 [DOI] [PubMed] [Google Scholar]
- Soldz S, Huyser D, & Dorsey E (2003). Youth preferences for cigar brands: rates of use and characteristics of users. Tobacco Control, 12(2), 155–160. doi: 10.1136/tc.12.2.155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soldz S, Huyser Dana J, & Dorsey E (2003). The cigar as a drug delivery device: youth use of blunts. Addiction, 98(10), 1379–1386. doi: 10.1046/j.1360-0443.2003.00492.x [DOI] [PubMed] [Google Scholar]
- Stephens M, Ogunsanya ME, Ford KH, Bamgbade BA, & Liang C (2015). Little cigar and cigarillo beliefs and behaviors among African-American young adults. American Journal of Health Behavior, 39, 519–528. doi: 10.5993/AJHB.39.4.8 [DOI] [PubMed] [Google Scholar]
- Stoltz AD, & Sanders BD (2000). Cigar and marijuana use: Their relationship in teens. The Journal of School Nursing, 16(4), 28–35. [PubMed] [Google Scholar]
- Sutter ME, Nasim A, Veldheer S, & Cobb CO (2016). Associations between unhealthy dieting behaviors and tobacco use among adolescents. Journal of Eating Disorders, 4, 39. doi: 10.1186/s40337-016-0126-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syu FK, Huang MY, & Huang JJ (2010). A Successful Intervention to Reduce Cigarillo Use Among Baltimore Youth. Fooyin Journal of Health Sciences, 2(3–4), 72–84. doi: 10.1016/S1877-8607(11)60002-7 [DOI] [Google Scholar]
- Terchek JJ, Larkin EMG, Male ML, & Frank SH (2009). Measuring cigar use in adolescents: Inclusion of a brand-specific item. Nicotine & Tobacco Research, 11(7), 842–846. doi: 10.1093/ntr/ntp074 [DOI] [PubMed] [Google Scholar]
- Trapl ES, Terchek JJ, Danosky L, Cofie L, Brooks-Russell A, & Frank SH (2011). Complexity of measuring "cigar use" in adolescents: Results from a split sample experiment. Nicotine and Tobacco Research, 13(4), 291–295. doi: 10.1093/ntr/ntq247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trapl ES, Yoder LD, Frank J, Borawski EA, & Abdus S (2016). Individual, parental, and environmental correlates of cigar, cigarillo, and little cigar among middle school students. Nicotine & Tobacco Research, 18, 834–841. doi: 10.1093/ntr/ntv201 [DOI] [PubMed] [Google Scholar]
- USDHHS. (1999). Youth use of cigars: patterns of use and perceptions of risk. Washington, D.C.: US Department of health and Human Services, Office of the Inspector General. [Google Scholar]
- Wilson LM, Tang EA, Chander G, Hutton HE, Odelola OA, Elf JL, … Apelberg BJ (2012). Impact of tobacco control interventions on smoking initiation, cessation, and prevalence: A systematic review. Journal of Environmental and Public Health. doi: 10.1155/2012/961724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yerger V, Pearson C, & Malone RM (2001). When is a cigar not a cigar? African American youths' understanding of "cigar" use. American Journal of Public Health, 91(2), 316–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu M (2011). Tobacco use among American Indian or Alaska Native middle- and high-school students in the United States. Nicotine & Tobacco Research, 13(3), 173–181. doi: 10.1093/ntr/ntq233 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.