Abstract
Background and purpose:
We aimed to evaluate the current practice patterns, safety and outcomes of patients who receive endovascular therapy (EVT) having mild neurological symptoms.
Methods:
From Jan 2010 to Jan 2018, 127,794 ischemic stroke patients were enrolled in the Florida-Puerto Rico Stroke Registry. Patients presenting within 24 hours of symptoms who received EVT were classified into mild (NIHSS ≤ 5) or moderate/severe (NIHSS > 5) categories. Differences in clinical characteristics and outcomes were evaluated using multivariable logistic regression.
Results:
Among 4,110 EVT patients (median age 73 (IQR=20), 50% women), 446 (11%) had NIHSS≤5. Compared to NIHSS>5, those with NIHSS≤5 arrived later to the hospital (median 138 vs. 101 min), were less likely to receive intravenous alteplase (30% vs. 43%), had a longer door to puncture time (median 167 vs. 115 min) and more likely treated in South Florida (64% vs. 53%). In multivariable analysis younger age, private insurance (vs. Medicare), history of hypertension, prior independent ambulation and hospital size were independent characteristics associated with NIHSS ≤5. Amongst EVT patients with NIHSS≤5, 76% were discharged home/rehabilitation and 64% were able to ambulate independently at discharge as compared to 53% and 32% of patients with NIHSS>5. Symptomatic ICH occurred in 4% of mild stroke EVT patients and 6.4% in those with NIHSS>5.
Conclusion:
Despite lack of evidence-based recommendations, 11% of patients receiving EVT in clinical practice have mild neurological presentations. Individual, hospital and geographical disparities are observed amongst endovascularly treated patients based on the severity of clinical symptoms. Our data suggest safety and overall favorable outcomes for EVT patients with mild stroke.
Keywords: Endovascular Therapy, Mild Stroke, Large Vessel Occlusion
Introduction
Endovascular therapy (EVT) is an effective method to achieve revascularization in patients with acute ischemic stroke related to a large vessel occlusion (LVO). In 2015, the results of five randomized controlled trials established superiority of EVT to standard of care in achieving functional independence in selected acute ischemic stroke patients.1–5 The results of these trials have now been implemented into clinical practice and EVT has become the standard of care in appropriately selected patients with moderate to severe ischemic stroke.6 Patients with mild neurological symptomatology (NIHSS ≤ 5) were either excluded1, 3, 4 or under-represented2, 5 in these trials. Similarly, mild stroke patients were entirely excluded from the recently completed trials which supported EVT for a select group of patients up to 24 hours from symptom onset.7, 8 Nevertheless, the meta-analysis of the 2015 trials showed that the beneficial effect of EVT on reducing disability at 90 days was observed across the entire NIHSS severity range.9 Similarly, a recent systematic review of all published studies of EVT and thrombolysis in mild stroke showed that odds of achieving good functional outcomes were four times higher in patients who received any form of reperfusion treatment relative to those untreated.10 However, these studies had variable methodologies and did not systematically evaluate the safety and efficacy of EVT in this low NIHSS population.
To date, no large study has evaluated the utilization, trends, characteristics and short-term outcomes of patients who are endovascularly treated while presenting with mild neurological symptomology. In the Florida-Puerto Rico Collaboration to Reduce Stroke Disparities (FL-PR CReSD) study, we evaluated all patients who received EVT and aimed to identify the characteristics associated with mild symptomatology and discharge outcomes compared to those who receive this treatment for more severe ischemic strokes.
Methods
Data Availability Statement
Anonymized data will be shared by the corresponding author upon written request from any qualified investigator.
Study population
A total of 127,794 patients were enrolled in the registry with a final diagnosis of ischemic stroke between January 2010 through January 2018 from 80 hospitals in Florida and 14 in Puerto Rico. Amongst 69,714 who presented within 24 hours of symptom onset, 4,110 patients received EVT and were included in the study. EVT was defined as the use of any form of mechanical thrombectomy devices for treatment of acute LVO with or without the use of intra-arterial thrombolysis. EVT Patients were categorized into mild (NIHSS ≤ 5), moderate-severe (NIHSS>5) and missing NIHSS subgroups (Figure 1).
Figure 1:
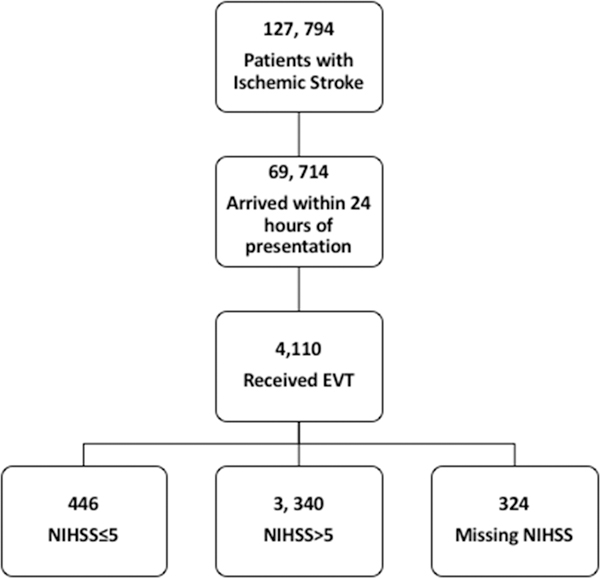
Flowchart of patients included in the study.
The primary outcome was to determine the characteristic associated with mild neurological symptomatology (NIHSS≤5) amongst endovascularly treated patients. Three categories of variables including clinical (demographic, vascular risk factors, time and mode of arrival), hospital (size, experience and academic status), and geographic characteristics (four Florida regions and PR) were studied. Temporal trends in ratio of mild to moderate-severe stroke, treatment time metrics, hospital discharge outcomes and treatment complications were studied.
Case Identification and Data Abstraction
The FL-PR Stroke Registry consists of hospitalized deidentified patient data collected from participating hospitals in Florida and Puerto Rico and includes patients with the primary diagnosis of ischemic stroke, transient ischemic attack (TIA), subarachnoid hemorrhage, intracerebral hemorrhage and stroke not otherwise specified. Briefly, FL-PR CReSD is a National Institute of Neurological Disorders (NINDS) funded multicenter initiative, as part of the Get with The Guidelines Stroke (GWTG-S) program11, to create high impact, culturally tailored interventions to identify disparities in delivery of stroke care among a diverse population of patients with significant Hispanic representation.12, 13
The University of Miami’s institutional review board approved this study. Each participating center received institutional ethics approval to enroll cases in the FL‐PR Stroke Registry without requiring individual patient consent under the common rule or a waiver of authorization and exemption from subsequent review by their institutional review board.
Information collected included patient demographics, clinical characteristics (vascular risk factors and relevant prior medical history), arrival characteristics (mode of hospital arrival (via emergency medical services (EMS) from home/scene, private transport, transfer from other hospital, unknown), presenting NIHSS and presenting neurological symptoms (to identify disability producing symptoms not captured by the NIHSS), the onset-to-door time (time from stroke onset to arrival in the emergency department, OTD), assessment characteristics (time from arrival to the initial head computed tomography (door to CT, DTC), time from hospital arrival to initiation of intravenous alteplase (door-to-needle, DTN time), hospital arrival to the initiation of EVT (door -to-puncture, DTP time) and hospital-level characteristics (number of beds, academic status, annual stroke volume and number of years in GWTG-S).
Short-term outcomes at discharge included discharge to home or to a rehabilitation center, ability to walk independently, and in-hospital mortality. Treatment complications included the rate of symptomatic intracerebral hemorrhage (ICH) defined as clinical deterioration by 4 points in the NIHSS attributed to CT-evident intracranial hemorrhage within 36 hours of treatment; and life threatening or serious systemic hemorrhage defined as bleeding within 36 hours of reperfusion treatment requiring transfusion of more than 3 units of blood.
Statistical Analysis
The level of statistical significance was set at p<0.05. For patient characteristics, continuous variables were summarized as median with interquartile range (IQR) and categorical variables were presented as frequencies with percentages. For continuous variables, differences were assessed using the Student t test (mean comparison) if normally distributed, or Wilcoxon–Mann–Whitney test (median comparison). For categorical variables, the Pearson chi-square test was used to compare the distributions between groups. Univariate analysis was performed to identify the specific characteristics associated with NIHSS≤5 among all EVT patients. To reduce multi-collinearity amongst the correlated factors, we first conducted step-wise logistic regression to select the independent factors. We then conducted multivariable analysis with generalized estimating equations (GEE) to account for clustering effect within each hospital and evaluated the associations between factors and mild stroke symptoms. Potential interactions between hospital characteristics and race-ethnicity, region and arrival time were also examined by including their interaction terms in the regression model.
Most variables had missing values in fewer than 5% of cases, except for door to CT time, (16.7% missing) and the location of the LVO (50.1% missing). The location of LVO was therefore not included in this analysis. The complete case approach and the missing indicator approach were used to include the full sample for variables with a large proportion of missingness as previously described.14 All statistical analyses were performed using SAS Version 9.3 software (SAS Institute).
Results
We included 4,110 patients who received EVT during the study period. Median age was 73 (IQR=20), 50% were women, 60% NHW, 15% NHB, 25% Hispanic. A total of 446 (11%) patients had a presenting NIHSS ≤ 5 and 324 (8%) had a missing baseline NIHSS. Baseline characteristics of patients were compared between the NIHSS≤ 5 and NIHSS> categories (Table 1). EVT patients with NIHSS ≤ 5 were younger, more likely to be male, more likely with private insurance, current smokers and had pre-existing hypertension (HTN) and less likely to have a history of atrial fibrillation as compared to those with NIHSS>5.
Table 1.
Demographic and hospital level characteristics of patients who received endovascular treatment (EVT) in the FL-PR Stroke Registry by NIHSS severity.
| Clinical Characteristics | EVT Patients NIHSS ≤5 (n=446) |
EVT Patients NIHSS >5 (n=3,340) |
p value |
|---|---|---|---|
| Age (yrs), median (IQR) | 68±19 | 74±19 | <0.0001 |
| Sex (male), % | 256 (57.4) | 1617 (48.4) | 0.0004 |
| Ethnicity, % NH- white NH- black FL-Hispanic PR-Hispanic |
276 (61.8) 63 (14.1) 107 (23.9) 0 |
2022 (60.5) 517 (15.4) 788 (23.5) 13 (0.3) |
0.5 |
| Medical Insurance, % Private* Medicare Medicaid/No Insurance** Unknown |
205 (45.9) 106 (23.7) 48 (10.7) 87 (19.5) |
1164 (34.8) 1175 (35.1) 303 (9.1) 698 (20.9) |
<0.0001 |
| Vascular Risk Factor, % | |||
| Current smoker, % | 78 (17.4) | 470 (14) | 0.05 |
| Hypertension, % | 311 (69.7) | 2149 (64.3) | 0.02 |
| Diabetes mellitus, % | 97 (21.7) | 780 (23.3) | 0.45 |
| Dyslipidemia, % | 164 (36.7) | 1092 (32.6) | 0.08 |
| Medical History, % | |||
| Atrial fibrillation, % | 113 (25.3) | 1271 (38.0) | <0.0001 |
| CAD/prior MI, % | 97 (21.7) | 694 (20.7) | 0.63 |
| Previous stroke/TIA, % | 106 (23.7) | 665 (19.9) | 0.057 |
| Arrival Time (%) On –hours Off- hours |
225 (50.4) 221 (49.5) |
1555 (46.5) 1785 (53.4) |
0.12 |
| Hospital Arrival Time from Onset in minutes (median, IQR) |
138 (307) | 101 (219) | <0.0001 |
| Patients based on arrival Time from Onset, % < 4.5 hrs 4.5– 6 hrs 6–12 hrs 12–24 hrs. |
297 (66.5) 36 (8.07) 69 (15.4) 44 (9.8) |
2525 (75.6) 247 (7.4) 377 (11.2) 191 (5.7) |
<0.0001 |
| NIHSS (median), IQR | 3 (2) | 17 (9) | <0.001 |
| Clinical Signs/symptoms, % | |||
| Weakness | 203 (45.5) | 2152 (64.4) | <0.0001 |
| Aphasia | 156 (34.9) | 1662 (49.7) | <0.0001 |
| Altered level of Consciousness | 32 (7.1) | 838 (25.0) | <0.0001 |
| Other Neurological Signs/symptoms | 88(19.7) | 778(23.2) | 0.09 |
| Large Vessel Occlusion, % Yes Missing |
200(44.8) 246(55.2) |
1698(50.8) 1642(49.2) |
<0.0001 |
|
Mode of Arrival EMS, n (%) |
351 (78.7) |
3158 (94.5) |
<0.0001 |
| Door to CT time, min (median, IQR) |
15 (19) |
13(14) |
<0.001 |
| Door to CT time, % <25 min missing |
272 (61) 71 (15.9) |
2232 (66.8) 561 (16.8) |
0.0005 |
| Intravenous Thrombolysis n, (%) | 135 (30.2) | 1409 (42.9) | <0.0001 |
| Door to Needle Time, min (median, IQR) | 46 (36) | 42 (31) | 0.14 |
| Door to Puncture Time, min (median, IQR) | 167 (70) | 115 (90) | <0.0001 |
| CT to puncture time | 151 (175) | 105(83) | <0.0001 |
| Hospital Characteristics | |||
| Hospital Size (beds median/IQR) Small (<250) Mid (250–450) Large (>450) |
672 (316) 5 (1.1) 95 (21.3) 346 (77.6) |
716(431) 35 (1.05) 522 (15.6) 2783 (83.3) |
<0.0001 |
| Academic hospital, % | 131 (29.3) | 1188 (25.5) | 0.009 |
| Years in GWTG, median (IQR) | 12 (4) | 12 (2) | 0.08 |
| Intravenous Alteplase treated patients/year (n) Low volume center (<20) High volume center (≥20) |
89(19.9) 357 (80.04) |
337 (10.09) 3003 (89.9) |
<0.0001 |
| Stroke Center Type Comprehensive Stroke Center Primary Stroke Center Not primary/Comprehensive |
414 (92.8) 32 (7.17) 0 (0) |
3145 (94.1) 186 (5.57) 9(0.27) |
0.22 |
| State Florida Puerto Rico |
446 (100) 0 (0) |
3327 (99.6) 13 (0.39) |
0.19 |
| Region in Florida South East Central West Central North and Panhandle |
287 (64.35) 59 (13.23) 57 (12.78) 43 (9.64) |
1770(52.9) 452(13.5) 759(22.7) 346 (10.3) |
<0.0001 |
CAD= Coronary Artery Disease, MI=Myocardial Infarction. NH-White= Non-Hispanic White, NH-black= Non-Hispanic black. EMS= Emergency Medical Services.
Includes Private insurance, VA and other.
Includes Medicaid, self-pay and No insurance.
Amongst EVT patients, those with mild symptoms arrived later to the hospital (138 min vs. 101 min) and were less likely to arrive via EMS (78.7% vs. 94.5%) compared to more severe strokes. Similarly, NIHSS≤ 5 patients had a longer assessment time in the emergency room (median DTC time 15 min vs. 13 min) and were less likely to receive IV alteplase as compared to those with NIHSS >5 (30% vs. 42.5%). Treatment times were delayed in this subgroup with longer DTN (46 min vs. 42 min) and DTP (167 min vs. 115 min). Mild stroke EVT patients were more likely treated in a mid-sized hospital (21.3% vs. 15.6%) and at academic hospitals (29.3% vs. 25.5%) compared to more severe strokes. The treatment was predominantly completed at hospitals that have comprehensive stroke center designation for both mild and moderate-severe strokes. Only 13 patients received EVT in Puerto Rico during the study period which did not include any mild stroke patients. Within Florida, EVT patients were more likely to have NIHSS≤ 5 in South Florida and less likely to have a mild presentation in West Central Florida (Table 1).
After step-wise logistic regression age, history of diabetes mellitus, atrial fibrillation, insurance status, door to CT time, arrival via EMS and hospital size (number of beds) were retained for inclusion in multivariable analysis. In the final multilevel-multivariable model (supplemental Table I), younger age (OR=2.02, 95% CI 1.45–2.82), private insurance vs. Medicare (OR= 1.48, 95% CI 1.1–2.0), prior history of Hypertension (OR=1.55, 95% CI 1.17–2.05), No known history of atrial fibrillation (OR=1.34, 95% CI 1.04, 1.71), small hospital vs. large (OR=1.73, 95% CI 1.10, 7.39), prior independent ambulation (OR=2,95% CI 1.2–3.5) were independent characteristics associated with low NIHSS ≤5. In contrast, arrival by EMS (OR=0.18 95% CI 0.12, 0.29), and motor weakness (OR=0.54 95% CI 0.40–0.74) were inversely associated with mild symptoms amongst those treated with EVT.
The absolute number of patients receiving EVT steadily increased over the study period (Figure 2). However, the ratio of mild to moderate/severe stroke patients remained stable over time. Discharge outcomes and treatment complications of EVT patients with mild and moderate/severe stroke are detailed in Table 2. In total, 76% of patient with EVT treated patients with NIHSS≤5 were discharged to either home or to a rehabilitation center and 64% were able to ambulate independently at discharge as compared to 53% and 32% of patients with NIHSS>5 respectively.
Figure 2:
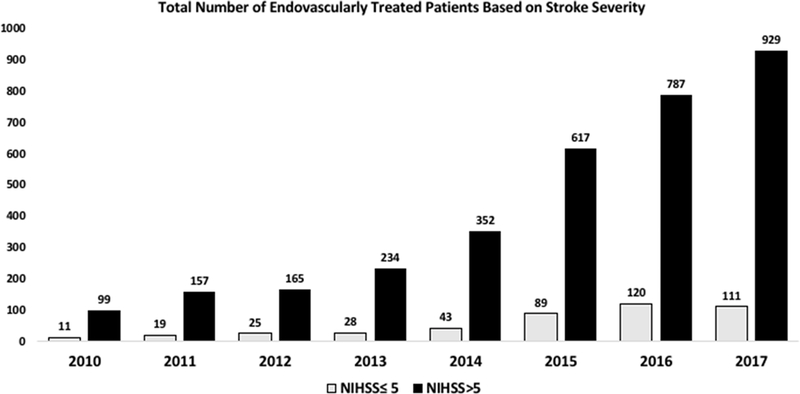
Trends of endovascular treatment by year (2010–2017) stratified by stroke symptom severity.
Table 2.
Outcomes at discharge and treatment complications in stroke patients who received EVT stratified by severity and intravenous (IV) Alteplase use.
|
Short-term Outcomes and Treatment Complications |
EVT Patients NIHSS ≤5 |
EVT patients NIHSS >5 |
||
|---|---|---|---|---|
|
Without IV Alteplase (n=311) |
With IV Alteplase (n=135) |
Without IV Alteplase (n=1931) |
With IV Alteplase (n=1409) |
|
| Discharge home/rehab, % | 232 (74.6) | 106 (78.5) |
934 (48.4) |
834 (59.2) |
|
Independent ambulation, % |
153 (62.2) |
67 (69.8) |
405 (29.1) |
361 (37.8) |
| Symptomatic ICH, % | 13(4.2) | 7 (5.2) |
123 (6.4) |
92 (6.5) |
| Life threatening or serious systemic hemorrhage, % | 2 (0.6) | 1 (0.7) |
20 (1.0) |
11 (0.8) |
| Death, % | 16 (5.1) | 7 (5.2) | 238 (12.3) | 137 (9.7) |
Discharge outcomes were not different in the mild category based on the IV alteplase treatment status, but thrombolysis had a positive effect on discharge outcomes in those with moderate/severe EVT patients (Table 2). In the multivariable model, young age (< 65 years old) (OR=2.29, 95% CI 1.04–5.05) was associated with independent ambulation at discharge among mild EVT patients, while stroke onset to arrival time (every 10 minutes increase, OR=0.99, 95% CI 0.21–1.00), arrival by EMS (OR=0.42, 95% CI 0.75–0.83), motor weakness at presentation (OR=0.46, 95% CI 0.27–0.79) and North and Panhandle region hospitals (compared to the South region, OR=0.30, 95% 0.19–0.48) were negatively associated with independent ambulation at discharge. Mild stroke EVT patients were more likely to be discharged home/rehabilitation center if they were young (<65 years old) (OR=2.88, 95% CI 1.61–5.17) and treated at a large hospital (>250 beds ) OR=1.58, 95% CI 1.01–2.48). Treatment at the West Central hospitals (compared to South, OR=0.52, 95% CI 0.36–0.77) where negatively associated with discharge home/rehabilitation amongst mild stroke EVT patients. The rate of symptomatic intracerebral hemorrhage was 4.5% and that of life threatening, serious systemic hemorrhage was 0.7%, in those with NIHSS≤5 and 6.4% and 0.9% in NIHSS>5 respectively. IV alteplase did not increase hemorrhagic complications amongst those treated with EVT regardless of symptom severity. The rate of in-hospital death was 5% and 11% in the mild and moderate/severe categories.
Conclusion
In this large multi-center cohort of ischemic stroke, over one in ten patients who received EVT had mild neurological symptoms. Multiple clinical, demographic and arrival characteristics were associated with mild neurological symptomatology amongst EVT patients. We identified that mild EVT patients were younger, more privately insured, and more likely to be independent at baseline as compared to treated patients with moderate to severe stroke. An overall favorable outcome pattern was noted amongst EVT patients with mild symptoms with close to two third of patients independently ambulating or being able to return home or to a rehabilitation center at discharge. Young age, early hospital presentation without concurrent motor symptoms were associated with favorable discharge outcomes amongst mild EVT patients. Hospital and geographic characteristics affected the practice patterns and outcomes, as large, academic hospitals in the South Florida region had a larger percentage of patients with mild symptoms among those utilizing EVT and higher odds of favorable outcomes in this population.
Our results are similar to prior studies of mild stroke EVT that showed significant outcomes benefit from reperfusion therapy without a substantial increase in the complication rates.15–17. However, small sample size and retrospective nature of prior studies, prevented further analyses with regards to work-flow metrics and characteristics associated with favorable outcomes. The safety and efficacy of EVT is time sensitive.9 Fast imaging to puncture and reperfusion times are robust predictors of good clinical outcomes in EVT patients. 18,19 Correspondingly, workflow modifications to reduce these time metrics in addition to increased clinical experience and use of newer thrombectomy devices have resulted in better EVT related outcomes.20 In our study, the time from symptom onset to hospital presentation was significantly longer in mild as compared to the moderate/severe EVT patients (Figure 3). The delays in hospital presentation are multifactorial and likely attributed to factors such as under-recognition of mild symptoms, underutilization of EMS, and perhaps a natural tendency on the part of patients and their families to minimize the importance of mild neurological symptoms. However, our data also showed significant in-hospital delays in all time-dependent acute performance metrics including DTC, DTN and DTP amongst EVT patients with mild symptoms. Importantly, the modest relative delays in the median DTC (2 min) and the median DTN (4 min) times do not entirely explain the significant relative delays in the median DTP times (52 min) in mild versus more severe EVT patients (Figure 3). In patients with moderate/severe stroke, contributing factors to delays in time-sensitive endovascular metrics include inefficiencies in triage, off-hour presentation, administration of IV alteplase and use of general anesthesia.18, 21 Our results showed a lower rate of IV alteplase use, and similar off-hour presentation rates among mild and moderate/severe EVT patients. Therefore, we believe that in-hospital delays in reperfusion time metrics amongst EVT patients with low NIHSS may be due to longer deliberations on the part of the treating physicians to consider EVT and perhaps acquisition of advanced imaging to improve clinical certainty before offering an aggressive treatment in this subgroup of patients. The fear of potential reperfusion complications including the risk of intracerebral hemorrhage and awaiting early deterioration prior to offering EVT are other possible explanations for these delays. In fact, prior studies reported that almost half of the mild stroke patients received EVT after early in-hospital neurological deterioration.16 In our study the rates of EVT-related hemorrhagic complications were lower in mild compared to the severe stroke population and on par with the recent reports in the literature.20, 22
Figure 3:
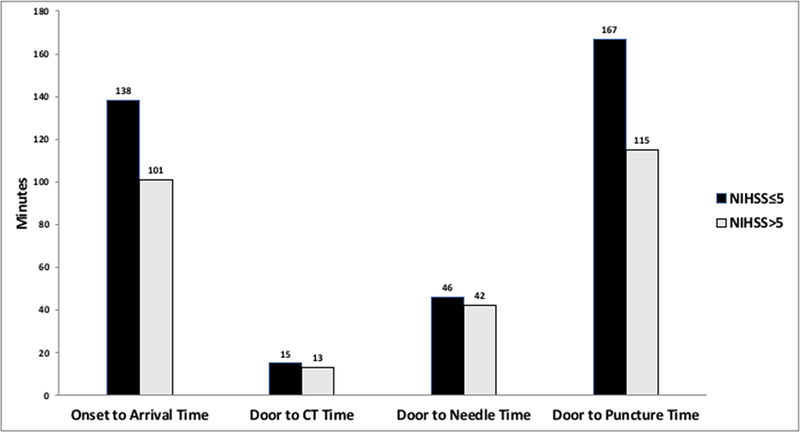
Median time (minutes) from symptom onset to hospital presentation and in hospital reperfusion time metrics amongst patients who received endovascular treatment, stratified by stroke symptom severity.
The role of thrombolysis in patients with low NIHSS is not well understood and the current practice pattern is widely variable.23 The previous observation that thrombolysis alone is a sufficient reperfusion treatment to obtain favorable outcomes for patients with mild symptoms and concurrent LVO 24 is highly contested and not supported by more recently completed studies.16, 25, 26 Our results show that in routine clinical practice, the majority of EVT patient with low NIHSS do not receive concurrent IV alteplase and importantly, no significant outcome differences were noted in mild EVT patients with or without IV alteplase therapy.
Our study has several limitations. The FL-PR Stroke Registry is a voluntary program including only GWTG-S participating hospitals, which are generally larger teaching hospitals with higher endovascular experience and volume. It is therefore likely that our data over represents the proportion of mild symptoms amongst EVT patients. Correspondingly, the delays in endovascular treatment may be even greater among hospitals not participating in the FL-PR registry. A total of 324 EVT patients had a missing baseline NIHSS. The characteristics of the patients in the missing category are similar to those in the NIHSS ≤ 5 category (supplemental Table II). It is therefore possible that the majority of the EVT patients in the missing NIHSS category had mild neurological symptoms. This assumption would increase the rate of mild EVT patients (from 11% to 19%) and affect our final results. Brain imaging information is inconsistently documented in the GWTG registry, with high missing rates of the vascular occlusion and its location. Finally, multivariable analysis is only presented for the independent ambulation and discharge disposition outcomes, as this analysis was not possible for the hemorrhagic complications and death due to small number of patients in each category (Table 2). Our results suggest that in the absence of established guidelines, there are significant delays in the delivery of EVT to those with mild symptoms and highlight significant individual, hospital and geographical disparities amongst endovascularly treated patients based on the severity of their clinical symptoms.
In the modern era of acute reperfusion therapies, EVT is increasingly performed for stroke patients with mild neurological symptoms. Prospective registries and randomized controlled trials of EVT in mild stroke are needed to determine the safety and efficacy of EVT in these patients.
Supplementary Material
Acknowledgment
The authors wish to thank the Florida-Puerto Rico participating hospitals. A complete list of FL-PR CReSD Investigators and Collaborators can be found in the supplemental material.
Financial Disclosures
Dr. Sacco- recipient and the primary investigator of the SPIRP cooperative grant from the NIH/NINDs (Grant Number: U54NS081763).
Dr. Rundek- recipient of the women’s supplement from the NIH, Office of Research on Women’s Health and receives salary support from the SPIRP cooperative grant from the NIH/NINDS (Grant Number: U54NS081763–01S1).
Dr. Romano - receives research salary support for grant to the University of Miami for role in Core B of SPIRP grant U54 NS081763. Dr. Romano is the recipient of the Grant from Genentech: Grant to the University of Miami for role as PI of the Mild and Rapidly Improving Stroke Study (MaRISS)
Dr. Koch - receives research salary support from the SPIRP cooperative grant from the NIH/NINDS (Grant Number: U54NS081763).
Dr. Yavagal- has a served as a consultant for Medtronic, Cerenovus, Guidepoint, GLG and Rapid Medical (modest compensation) and has served as a consultant for Neuralanalytics (No Compensation)
Study Funded by the National Institute of Health (NIH)/National Institute of Neurological Disorders (NINDS) through the Stroke Prevention and Intervention Research Program (SPIRP) cooperative grant (Grant Number: U54NS081763) and the Florida Department of Health.
Footnotes
Statistical Analysis conducted by Chuanhui Dong, PhD and Kefeng Wang, MSc
References
- 1.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. The New England journal of medicine. 2015;372:1019–1030 [DOI] [PubMed] [Google Scholar]
- 2.Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. The New England journal of medicine. 2015;372:1009–1018 [DOI] [PubMed] [Google Scholar]
- 3.Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-pa vs. T-pa alone in stroke. The New England journal of medicine. 2015;372:2285–2295 [DOI] [PubMed] [Google Scholar]
- 4.Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. The New England journal of medicine. 2015;372:2296–2306 [DOI] [PubMed] [Google Scholar]
- 5.Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. The New England journal of medicine. 2015;372:11–20 [DOI] [PubMed] [Google Scholar]
- 6.Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 american heart association/american stroke association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: A guideline for healthcare professionals from the american heart association/american stroke association. Stroke; a journal of cerebral circulation. 2015;46:3020–3035 [DOI] [PubMed] [Google Scholar]
- 7.Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. The New England journal of medicine. 2018;378:11–21 [DOI] [PubMed] [Google Scholar]
- 8.Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378:708–718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–1731 [DOI] [PubMed] [Google Scholar]
- 10.Griessenauer CJ, Medin C, Maingard J, Chandra RV, Ng W, Brooks DM, et al. Endovascular mechanical thrombectomy in large-vessel occlusion ischemic stroke presenting with low national institutes of health stroke scale: Systematic review and meta-analysis. World Neurosurg. 2018;110:263–269 [DOI] [PubMed] [Google Scholar]
- 11.Smaha LA, American Heart A. The american heart association get with the guidelines program. American heart journal. 2004;148:S46–48 [DOI] [PubMed] [Google Scholar]
- 12.Sacco RL, Gardener H, Wang K, Dong C, Ciliberti-Vargas MA, Gutierrez CM, et al. Racial-ethnic disparities in acute stroke care in the florida-puerto rico collaboration to reduce stroke disparities study. J Am Heart Assoc. 2017;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Asdaghi N, Romano JG, Wang K, Ciliberti-Vargas MA, Koch S, Gardener H, et al. Sex disparities in ischemic stroke care: Fl-pr cresd study (florida-puerto rico collaboration to reduce stroke disparities). Stroke. 2016;47:2618–2626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li L, Shen C, Li X, Robins JM. On weighting approaches for missing data. Stat Methods Med Res. 2013;22:14–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haussen DC, Bouslama M, Grossberg JA, Anderson A, Belagage S, Frankel M, et al. Too good to intervene? Thrombectomy for large vessel occlusion strokes with minimal symptoms: An intention-to-treat analysis. J Neurointerv Surg. 2017;9:917–921 [DOI] [PubMed] [Google Scholar]
- 16.Messer MP, Schonenberger S, Mohlenbruch MA, Pfaff J, Herweh C, Ringleb PA, et al. Minor stroke syndromes in large-vessel occlusions: Mechanical thrombectomy or thrombolysis only? AJNR Am J Neuroradiol. 2017;38:1177–1179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haussen DC, Lima FO, Bouslama M, Grossberg JA, Silva GS, Lev MH, et al. Thrombectomy versus medical management for large vessel occlusion strokes with minimal symptoms: An analysis from stopstroke and gestor cohorts. J Neurointerv Surg. 2018;10:325–329 [DOI] [PubMed] [Google Scholar]
- 18.Menon BK, Sajobi TT, Zhang Y, Rempel JL, Shuaib A, Thornton J, et al. Analysis of workflow and time to treatment on thrombectomy outcome in the endovascular treatment for small core and proximal occlusion ischemic stroke (escape) randomized, controlled trial. Circulation. 2016;133:2279–2286 [DOI] [PubMed] [Google Scholar]
- 19.Sun CH, Nogueira RG, Glenn BA, Connelly K, Zimmermann S, Anda K, et al. “Picture to puncture”: A novel time metric to enhance outcomes in patients transferred for endovascular reperfusion in acute ischemic stroke. Circulation. 2013;127:1139–1148 [DOI] [PubMed] [Google Scholar]
- 20.Menon BK, Saver JL, Goyal M, Nogueira R, Prabhakaran S, Liang L, et al. Trends in endovascular therapy and clinical outcomes within the nationwide get with the guidelines-stroke registry. Stroke; a journal of cerebral circulation. 2015;46:989–995 [DOI] [PubMed] [Google Scholar]
- 21.Menon BK, Almekhlafi MA, Pereira VM, Gralla J, Bonafe A, Davalos A, et al. Optimal workflow and process-based performance measures for endovascular therapy in acute ischemic stroke: Analysis of the solitaire fr thrombectomy for acute revascularization study. Stroke; a journal of cerebral circulation. 2014;45:2024–2029 [DOI] [PubMed] [Google Scholar]
- 22.Sarraj A, Sangha N, Hussain MS, Wisco D, Vora N, Elijovich L, et al. Endovascular therapy for acute ischemic stroke with occlusion of the middle cerebral artery m2 segment. JAMA Neurol. 2016;73:1291–1296 [DOI] [PubMed] [Google Scholar]
- 23.Asdaghi N, Wang K, Ciliberti-Vargas MA, Gutierrez CM, Koch S, Gardener H, et al. Predictors of thrombolysis administration in mild stroke: Florida-puerto rico collaboration to reduce stroke disparities. Stroke. 2018;49:638–645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Urra X, San Roman L, Gil F, Millan M, Canovas D, Roquer J, et al. Medical and endovascular treatment of patients with large vessel occlusion presenting with mild symptoms: An observational multicenter study. Cerebrovasc Dis. 2014;38:418–424 [DOI] [PubMed] [Google Scholar]
- 25.Heldner MR, Jung S, Zubler C, Mordasini P, Weck A, Mono ML, et al. Outcome of patients with occlusions of the internal carotid artery or the main stem of the middle cerebral artery with nihss score of less than 5: Comparison between thrombolysed and non-thrombolysed patients. J Neurol Neurosurg Psychiatry. 2015;86:755–760 [DOI] [PubMed] [Google Scholar]
- 26.Khatri P, Kleindorfer DO, Devlin T, Sawyer RN, Jr., Starr M, Mejilla J, et al. Effect of alteplase vs aspirin on functional outcome for patients with acute ischemic stroke and minor nondisabling neurologic deficits: The prisms randomized clinical trial. JAMA. 2018;320:156–166 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Anonymized data will be shared by the corresponding author upon written request from any qualified investigator.


