Abstract
Objective:
The purpose of this study was to quantify how dialysis dietitians spend their time, and whether the activities that were most frequent varied based on patient: full time equivalent (FTE)dietitian ratio.
Design:
Cross-sectional, observational, time and motion study using WOMBAT software/method for time recording
Setting:
Fourteen dialysis centers in [location redacted]
Subjects:
Fourteen registered dietitian nutritionists; mean time in dietetics of 26.6±8.5 years
Intervention:
None
Main outcome measure:
Percent of time in direct care (e.g. patient interaction) vs indirect care (e.g. documentation and plans of care, professional communication) vs other responsibilities (e.g. administrative work, education of self or others).
Results:
The mean number of tasks recorded per 3 hour observation session was 38.3±14.0 including 18.5±7.7 indirect care tasks, 7.7±6.2 direct care tasks, and 9.7±5.4 other tasks. The mean number of unique patients seen per observation session was 6.9±5.4; the mean amount of direct care time per patient encounter was 6.95±4.05 minutes. Indirect care took the highest proportion of observed time, 56.0±22.2%, followed by direct care, 24.9±18.8%. Increasing patient: FTE ratio had a moderate negative correlation with percent of time in direct patient care (r=−0.35, p=0.21), but there was no relationship between patient: FTE ratio and direct care time per patient (r=0.02, p=0.94).
Conclusion:
About 25% of dietitian time was available for direct patient care. This is much less than that reported in previous studies and may not be sufficient to improve nutritional status. Limitations of our study include a small sample size from a single region. Further work is needed to understand the balance of responsibilities among renal dietitians and their impact on patient outcomes.
Introduction
Previous research demonstrates that dietitians in dialysis units are often responsible for more than the KDOQI recommended 100 patients1. Surveys suggest mean patient: full time equivalent (FTE) dietitian ratios between 104.9±48.32 and 115.5±38.43. Administrative data from the Dialysis Annual Facility Reports generate lower estimates: mean patient: FTE dietitian ratios between 564 and 90±345. Research over a period of 10 years suggest that these high patient: FTE staff ratios leave dietitians without the time to follow the KDOQI guidelines for nutrition assessment and intervention 2,6.
In the dialysis units, dietitians see patients at least once a month to review their lab values7, and spend time on Centers for Medicare and Medicaid Services (CMS) mandates including Plans of Care8,9, documenting quality measures, and participating in Quality Assurance Performance Improvement (QAPI) activities 10. Many dietitians assist the Interdisciplinary Team (IDT) to manage anemia, metabolic bone disease and kinetic (adequacy) modeling as well as providing nutrition counseling or education and monitoring the response7,9,10. Additionally, dietitians and other health professionals have been suggested as substitutes when inadequate physician time is available11, which may leave dietitians with non-nutrition responsibilities. Dietitians report frequently being used as administrative personnel to maintain the units’ regulatory status and as pharmacy benefits managers, responsible for moving patients to the company pharmacy3.
Previous studies provide some insight into the job responsibilities of renal dietitians, but are limited by self-report and the lack of objective time data. Direct observation can overcome these limitations and provide quantitative data on the time consumed by renal dietitian responsibilities to understand what types of responsibilities are prioritized within the time limitations of high patient:staff ratios. Therefore, the purpose of this study was to use direct observation to quantify how dietitians at different dialysis facilities spend their time, and whether the activities that were most time consuming varied based on patient: FTE dietitian ratio.
Methods
We used a cross-sectional direct observation time and motion study of dietitians employed at dialysis facilities within 50 miles of [location redacted]. We received approval to recruit dietitians from two of the three dialysis chains in this area: one local and non-profit and one national and for-profit, and IRB approval from [location redacted] University. Because the data collected on dietitian activities had the potential to be sensitive and could be used for performance reviews or other job related evaluations, corporate letters of support stated that they had waived their right to examine the raw data collected in this study. Dialysis dietitians were recruited via email or by phoning dialysis facilities.
Inclusion criteria were:
Registered and [location redacted] Licensed dietitian
Work at least 8 hours per week at an outpatient dialysis facility
Provide at least 8 hours per week of clinical care to dialysis outpatients
In current position and at current facility for at least six months prior to observation
Willing to provide informed consent and be observed
Dietitians were asked to participate in between two and four observation sessions per facility. They could choose to be observed at one or more facilities, if applicable. If more than one dietitian worked at a facility, each eligible dietitian could participate. Each observation session lasted three hours. Attempts were made to schedule the observation sessions on different days of the week and different weeks of the month to attempt to capture variability of routine.
Dietitians were given both a $25.00 amazon.com gift card and a $25.00 Nasco gift card for each observation session they completed. Nasco is an educational supply company selling nutrition related products (e.g. food models and handouts) that can be used for nutrition education.
Facility and dietitian characteristics
At the start of the first scheduled observation session, dietitians provided informed consent and completed a brief written survey (Online Supplemental Material 1) to obtain descriptive characteristics about themselves (years of experience, education, specialty certifications, work schedule) and their facility (number of patients, other dietitians, facility protocols, and type of medical record). The observer also recorded date and day of the week of the observation, the week of the calendar month and the dialysis facility’s lab cycle (i.e. was it a week when lab specimens were being collected or a week when lab results had been received back and the dietitians were reviewing the results with patients), the number of unique patients with whom the dietitian interacted, and whether the dietitian considered the day to be typical. Some facilities had two scheduled lab draws per month. In these facilities, we classified the cycle based on the first set of labs.
Observation and timing of tasks
Recording was accomplished using the validated Work Activity Measurement By Activity Timing (WOMBAT) method, which uses software on a tablet computer to automatically time stamp each task entry12,13. This software captures the complexity of clinical work by capturing interruptions and simultaneous tasks, as well as with whom and with what a task is completed12,13. Field testing of WOMBAT with nurses on inpatient wards12,14, physicians in emergency departments15, and the multidisciplinary team in intensive care units16 has demonstrated that it is a time efficient method for direct observation12, and that it is not influenced by the Hawthorne effect16.
Dietitian activities were recorded using the activity categories and tasks listed in online supplemental material 2. The tasks were based on responsibilities identified in a previous survey of renal dietitians3 and task categories that have been used in previous WOMBAT studies of nurses, physicians, and respiratory therapists16. They were not validated, but were reviewed by a panel expert renal dietitians who agreed on the importance of each task and that the definitions were appropriately descriptive. In addition, we recorded with whom and with what equipment dietitians completed activities (online supplemental material 2). When a computer was in use, the observer stood or sat where the computer screen was visible so that the task could be identified (for example, email vs work in electronic medical record). In cases where clarification was required, the observer asked the subject to describe the current or just completed task to clarify whether it was coded correctly; however, clarification was not requested during patient interactions. A single observer (XXX), who is also a dietitian, conducted all observation sessions; therefore, no inter-observer reliability assessment was required.
The observations did include the potential for the investigator to observe patient interactions and patient information but patient information was not recorded as a part of the observation. During an observation, if the dietitian interacted with a patient, the dietitian introduced the observer and explained that they were collecting data on the dietitian only16.
Statistical analysis—Facility and dietitian characteristics
The statistical analysis was primarily descriptive. We calculated the number of dietitian hours scheduled at the facility and converted to FTE, using the definitions of Yoder et al4: full time is >32 hours/week and part time as one-half FTE, and then established patient: FTE dietitian ratio at each facility. We searched each facility on Dialysis Facility Compare and recorded the star rating and whether the facility’s hospitalization admission rate and mortality rate were better, worse, or as expected.
We used mean and standard deviation or number and percent, as appropriate, to describe the characteristics of the facilities and the dietitians; analysis used SPSS version 24 (IBM Inc. Armonok NY). Because of the small sample size we did not perform statistical comparisons based on facility ownership type.
Statistical analysis—Observation and timing data
We downloaded the timed observation session data from WOMBAT into excel and analyzed it in SPSS. Using the observation session as the unit of analysis, we calculated the number of times each task type was recorded and the total time spent on that task type. Then we calculated the mean and standard deviation of percent of each observation session spent on the four a priori defined activity groups (direct patient care, indirect patient care, other, and non-work) (Table 1).
Table 1:
Activity categories and tasks for observation of renal RDN responsibilities. The far left column indicates the groupings that were used for classifying direct vs indirect vs other time.
| Activity Category | Tasks | Inclusions/Description | Exclusions | |
|---|---|---|---|---|
| Direct Care | Direct patient care | Patient/Caregiver conversation | • Providing feedback on lab results • Rapport building • Reinforcing medications • Assessing medication adherence |
• Gathering information (nutrition assessment) • Providing nutrition advice (nutrition intervention) |
| Nutrition assessment | • Asking patient for information on nutrition intake, appetite, GI symptoms, access to food • Nutrition focused physical exam |
|||
| Nutrition intervention | • Education on nutrition • Recommendation of specific foods to include or modify • Providing supplement samples or recommendations |
Ordering supplements or completing paperwork for supplements | ||
| Patient rounds (with patient present) | Discussing patient with other team members while patient present | Discussion of patient when not present | ||
| Plan of care meetings with patient present | Discussing patient with other team members in order to complete the plan of care documentation while patient present | |||
| Indirect care | Indirect patient care | Medical record review | • Reviewing medical record for specific piece of information • Reviewing patient chart for general updates |
• Writing/recording in chart • Creating lab reports |
| Plan of care meetings without patient present | Discussing patient with other team members in order to complete the plan of care documentation without the presence of the patient | |||
| Reviewing patient lab values to create monthly reports | Developing reports or reviewing lab values, generally for a group of patients in a systematic manner at a designated timeframe of the month | Communicating results to patients | ||
| Assessing dialysis adequacy | Calculation and assessment of dialysis adequacy generally for a group of patients in a systematic manner at a designated timeframe of the month | Communicating results to team members | ||
| Nutrition education development | • Developing or locating handouts for nutrition education • Developing or constructing bulletin boards or activities for nutrition education |
Providing diet instruction to individual patients | ||
| Medication | Insurance communication | • Communicating with insurance companies about nutrition related medication coverage or • Obtaining oral nutrition supplements |
Communicating with patients or other health care professionals about these conversations | |
| Pharmacy benefits management | Ordering medications to be used as part of a bundled payment | Requesting insurance coverage for medications | ||
| Clinical protocols | • Adjusting medications according to a protocol based on patient lab results including anemia and bone mineral protocols • Development of clinical protocols |
|||
| Documentation | Patient care documentation | • Recording nutrition information in the medical chart • Sharing information with other health professionals in a written format |
||
| Documenting plans of care | • Completing nutrition section of plan of care form | Coordinating other health professionals to complete other sections of plan of care | ||
| Professional Communication | (Not further categorized) | • Discussing a specific patient with another health care professional/s (in the facility or off site) • Work related conversation with other dialysis center employees/health care professionals • Corridor contacts/consults with other health care professional |
• Rounds • Plan of care meetings |
|
| Other | In transit | (Not further categorized) | Movement between office and patient care areas | |
| Administrative | Maintaining patient rolls or schedules | • Updating patient contact information • Coordinating/tracking patient transfers • Modifying patient dialysis schedules • Modifying patient lab schedules |
Modifying personal schedule | |
| Quality improvement projects | Conducting or coordinating quality improvement efforts | |||
| CMS data reporting | • Gathering data required by CMS • Inputting data into recording system (eg CROWNweb) |
|||
| Plan of care organization | • Organizing plan of care meetings • Ensuring other team members complete plans of care on timely basis |
Completing plans of care | ||
| Facility or corporate meetings not related to individual patient care | Meetings (in person or virtual) regarding new initiatives, policies | Patient care meetings | ||
| Personal scheduling | • Organizing day • Personal scheduling including time off and time between facilities |
|||
| Supervision/Education | Professional education | Education for self, including webinars/journal reading/journal club | • Educating others • Educating patients |
|
| Research | Conducting research projects | Quality improvement | ||
| Educating other healthcare professionals | • Educating other staff on nutrition • Training students, interns and/or new RDNs |
Patient education | ||
| Non-clinic consumer education | • Educational programs for nursing homes, nearby hospitals, charity screening events | Clinic based consumer education | ||
| Publication | • Writing articles for newsletters, other professional publications | |||
| Non-work | Non-work time | (not further categorized) | • Lunches • Breaks • Staff social events • Non-work conversations • Personal phone calls |
Rapport building with patients |
CMS-Centers for Medicare and Medicaid Services, CROWNWeb-Consolidated Renal Operations in a Web-Enabled Network, RDN-registered dietitian nutritionist
We calculated an average time per patient encounter by dividing the direct patient care time in an observation session by the patient encounter count for that observation session. We compared the percent of direct care time based on week of the lab cycle for the observation session using ANOVA.
Using the dietitian as the unit of analysis, we calculated the number of times each task type was recorded and the total time spent on each task type. Then we calculated the mean and standard deviation of percent of each dietitian’s observed time spent on each task type and the four a priori defined activity groups (direct patient care, indirect patient care, other, and non-work) (Table 1). We described the rank frequency, in terms of percent of observed minutes, of the tasks within the activity groups, and of the tasks overall.
We used Spearman’s correlation to determine whether there was a relationship between the patient: FTE dietitian ratio or length of dietitian experience and the average percent of observed minutes spent on each activity, and the average amount of time spent in the patient care area.
As a result of conversations with dietitians during the observations, we conducted a post hoc sensitivity analysis to determine whether observation sessions with home care patients were different to those with only in center hemodialysis patients, with the hypothesis that home care patients had longer interactions with dietitians.
Results
Facility and dietitian characteristics
We conducted 48 observations with 14 dietitians at 14 facilities. We observed two dietitians at different facilities, and at two facilities we observed multiple dietitians. Two observations were deleted due to technical difficulties that prevented portions of data from being recorded.
Characteristics of the facilities were similar between for-profit and non-profit facilities, with the exceptions that for-profit facilities where observations occurred were on average twice as far from the center of the 50-mile radius for recruiting and non-profit facilities were larger (mean 110±60, vs 72±25 patients) and had higher patient: FTE dietitian ratios (mean 132.3±54.0 vs 113.7±18.4) (Table 2).
Table 2:
Characteristics of participating facilities and dietitians
| All | Non-profit chain | For-profit chain | |
|---|---|---|---|
| Facilitya | n=14 | n=7 | n=7 |
| Mean±SD | |||
| Observation sessions per facility | 3.4±1.2 | 3.6±1.5 | 3.3±1.0 |
| Patient census | 90.9 ±48.3 | 109.7±60.0 | 72.0±25.0 |
| Dietitian hours at facility | 28.7±15.4 | 35.2±18.4 | 22.1±8.8 |
| FTE dietitians by Yoder FTE | 0.79±0.43 | 0.93±0.53 | 0.64±0.24 |
| Patient: FTE dietitian ratio (FTE calculated with Yoder4 formula) | 123.0±40.0 | 132.3±54.0 | 113.7±18.4 |
| number (%) | |||
| Location | |||
| City of [location redacted] | 3 (21%) | 2 (29%) | 1 (14%) |
| [location redacted] County | 8 (57%) | 5 (71%) | 3 (43%) |
| [location redacted]County | 1 (7%) | 0 | 1 (14%) |
| [location redacted] County | 1 (7%) | 0 | 1 (14%) |
| [location redacted] County | 2 (14%) | 0 | 2 (29%) |
| [location redacted] County | 2 (14%) | 2 (29%) | 0 |
| More than 1 dietitian works at facility | 3 (21%) | 2 (29%) | 1 (14%) |
| Three Star Rating | 7 (50%) | 3 (43%) | 4 (57%) |
| Mortality as expected | 13 (93%) | 6 (86%) | 7 (100%) |
| Hospital admission frequency as expected | 12 (86%) | 6 (86%) | 6 (86%) |
| Dietitiansb | n=14 | n=8 | n=6 |
| Mean±SD | |||
| Years as dietitian | 26.6±8.5 | 30.4±8.0 | 21.7±6.9 |
| Years in renal nutrition | 16.2±10.1 | 14.9±12.1 | 18.0±7.2 |
| Years at current employer | 11.1±8.8 | 12.6±11.5 | 9.0±2.9 |
| Hours worked per week (across all facilities) | 35.8±5.4 | 33.2±6.0 | 39.2±1.6 |
| Number of observation sessions per dietitian | 3.4±1.2 | 3.1±1.1 | 3.8±1.3 |
| n(%) | |||
| Work at multiple facilities | 10 (72%) | 5 (63%) | 5 (83%) |
| % with Masters | 8 (57.1%) | 4 (50%) | 4 (67%) |
| % with specialty certificationc | 3 (21%) | 2 (25%) | 1 (17%) |
| Observed at multiple facilities | 2 (14%) | 1 (13%) | 1 (17%) |
--Each facility is represented once in the table, even if multiple dietitians were observed at a single facility.
--Each dietitian is represented once in the table, even if observed at multiple facilities.
—one each of Board Certified Specialist in Gerontologic Nutrition (CSG), Board Certified Specialist in Renal Nutrition (CSR), and Certified Nutrition Support Clinician (CSNC)
FTE-full time equivalent, SD-Standard Deviation
Dietitians were very experienced, with mean time in dietetics of 26.6±8.5 years (Table 2). Dietitians at the non-profit facilities were more experienced in general but dietitians at the for-profit facilities were more experienced in renal nutrition. Dietitians employed by the for-profit company were more likely to work at multiple facilities (83%), and to work more hours in total per week (Table 2).
The most frequent protocols at facilities were nutrition supplementation and mineral bone disease treatment (100%), followed by dry weight and emergency preparedness (11, 79%). The majority of dietitians reported having primary responsibility for the implementation of nutrition supplementation (12, 86%) and MBD protocols (11, 79%). No dietitians reported primary responsibility for anemia, dry weight, or dialysis adequacy protocols. 71% of dietitians reported that their facilities used only electronic medical records, 29% reported that they used both paper and electronic.
Task counts and time per observation
The mean number of tasks recorded per 3 hour observation session was 38.3±14.0 including 18.5±7.7 tasks within the indirect care activity group, 7.7±6.2 tasks within the direct care activity group, and 9.7±5.4 tasks within the other activity group. The mean number of unique patients seen per observation session was 6.9±5.4, with a range from 0-21. The higher number of tasks within the direct care activity group than patients seen represents the fact that some patients required 2 tasks—an initial conversation followed by a return to the office to get a handout followed by a second task within the direct care activity group. The mean amount of direct care time per patient encounter was 6.95±4.05 minutes, with a minimum of 1.22 minutes and a maximum of 19.05 minutes.
Tasks in the indirect care activity group took up the highest proportion of time per observation, on average 56.0±22.2%. Tasks in the direct care activity group were next highest, 24.9±18.8%. This aligns with the finding that 29.4±21.4% of time was spent in patient care areas, with the additional 5% likely representing communication with other healthcare providers in patient care areas.
Task counts and time per dietitian
The following tasks were never observed: assessing dialysis adequacy, non-clinic consumer education, CMS data reporting, writing publications. The most time-consuming task in each activity group was as follows: direct care activity group—patient/caregiver interaction, indirect care activity group—professional communication, other activity group—in transit (Table 3). Examining recorded time overall, the most time consuming specific tasks were patient/caregiver interaction (24.9±11.5%), professional communication (20.9±6.7%) and reviewing labs (13.5±10.9%) (Figure 1). Patient care documentation (10.1±6.9%) and in transit (7.5±3.3%) rounded out the top five time consuming tasks.
Table 3:
Rank order of percent time per dietitian spent on tasks within activity group.
| Activity Group | Activity Category | Tasks | N of RDNs with task | Mean ± SD % time within group | Rank by % time, within group |
|---|---|---|---|---|---|
| Direct Care | Direct patient care | Patient/Caregiver conversation | 14 | 98.0±3.8 | 1 |
| Nutrition assessment | |||||
| Nutrition intervention | |||||
| Patient rounds (with patient present) | 1 | 0.9±3.4 | 3 | ||
| Plan of care meetings (with patient present) | 1 | 1.2±4.6 | 2 | ||
| Indirect care | Indirect patient care | Medical record review | 13 | 7.8±6.6 | 5 |
| Plan of care meetings without patient present | 5 | 4.0±8.8 | 6 | ||
| Reviewing patient lab values to create monthly reports | 14 | 22.6±15.9 | 2 | ||
| Nutrition education development | 7 | 3.1±6.9 | 7 | ||
| Medication | Insurance communication | 4 | 1.6±3.6 | 9 | |
| Pharmacy benefits management | 6 | 1.7±3.5 | 8 | ||
| Clinical protocols | 13 | 10.8±16.3 | 4 | ||
| Documentation | Patient care documentation | 13 | 19.1±13.2 | 3 | |
| Documenting plans of care | 5 | 1.1±2.6 | 10 | ||
| Professional Communication | (Not further categorized) | 14 | 37.7±10.6 | 1 | |
| Other | In transit | (Not further categorized) | 14 | 58.5±29.6 | 1 |
| Administrative | Maintaining patient rolls or schedules | 2 | 4.4±12.8 | 7 | |
| Quality improvement projects | 4 | 5.7±11.4 | 6 | ||
| CMS data reporting | 0 | ||||
| Plan of care organization | 5 | 8.2±14.2 | 4 | ||
| Facility or corporate meetings not related to individual patient care | 5 | 12.4±20.8 | 3 | ||
| Personal scheduling | 13 | 18.7±15.3 | 2 | ||
| Supervision/Education | Professional education | 7 | 6.0±7.4 | 5 | |
| Research | 1 | 0.37±1.4 | 9 | ||
| Educating other healthcare professionals | 1 | 2.3±8.7 | 8 |
SD-Standard Deviation, CMS-Centers for Medicare and Medicaid Services
Figure 1:
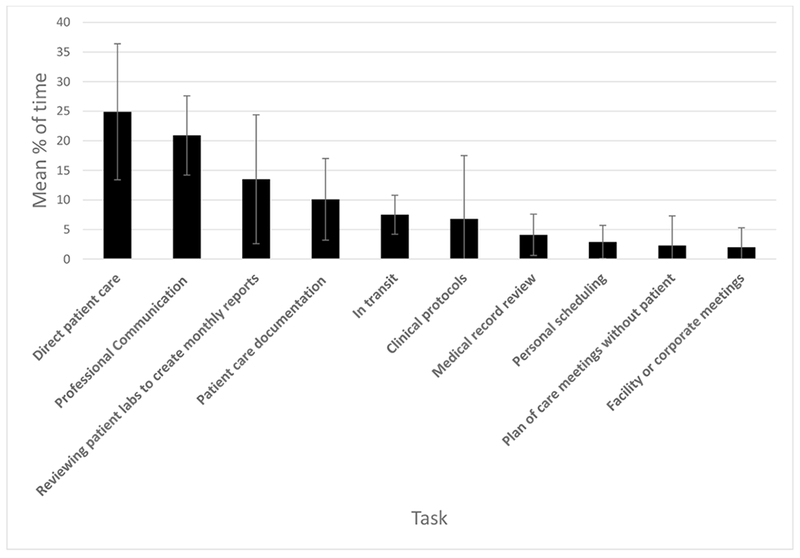
Top ten most time consuming tasks observed based on mean % of time per dietitian.
Interactions with individuals and use of equipment during tasks
EHR use was not one of our equipment variables, but time using the EHR can be approximated by the amount of time in task variables “medical record review” and “documentation” (15.9±7.1%, low end) or the equipment variable “desktop computer” (25.5±9.6%, high end, since this also includes email time).
Overall, 17.9% of tasks took place with a patient and 17.2% of tasks were recorded as taking place with the dietitian alone. Nurses were the next most frequent (11.1% of tasks); they were particularly common in the communication tasks. Interaction with a dietetic intern was never observed, nor was use of a pager. Just over one quarter of tasks took place in a patient care area. 14.6% of tasks used a desktop computer, but 25.5±9.6% of time was spent on a desktop computer.
Week-to-week variation in tasks
The largest number of observation sessions (41.3%) were during lab result distribution week, when dietitians are most likely to interact with patients. 26.1% of observation sessions occurred in the week after lab passing, and 15.2 % and 17.4% occurring in the 3rd, and final week of the lab cycle, respectively.
Although there were not statistically significant differences, it did appear that the mix of activity groups varied based on the week of the lab cycle (Figure 2). The indirect care activity group was the most time consuming during all weeks, but tasks in the other activity group overtook direct care as the second most time consuming during week 3 (Figure 2). The final weeks, when preparations begin to collect lab specimens had a very high proportion of activities in the indirect care group (72.2±24.9%) and much less time in the direct care or other activity groups.
Figure 2:
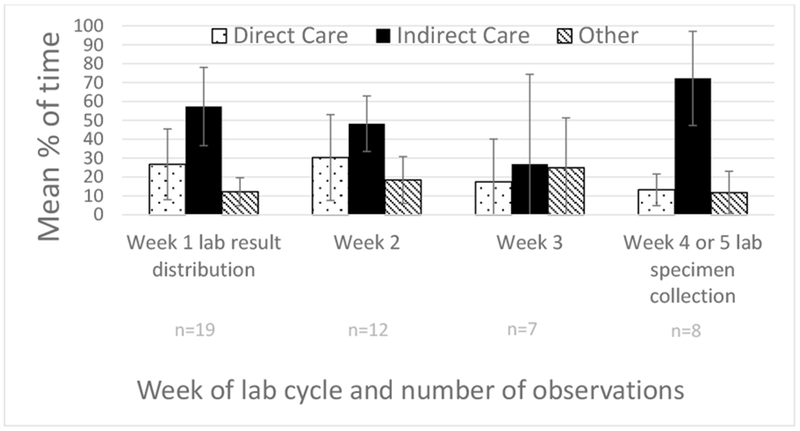
Comparing mean and standard deviation percent of time per observation session in direct care, indirect care, and other activities based on week of lab cycle.
Dietitian characteristics and tasks
Experience in renal nutrition had a small positive, but not statistically significant, association with longer time with each patient (r=0.22, p=0.46) (Table 4). Increasing patient: FTE ratio had a moderate negative correlation with percent of time in patient care area and percent of time on the direct patient care activity group(r=−0.32, p=0.27 and r=−0.35, p=0.21, respectively), but there was no relationship between patient: FTE ratio and direct care time per patient encounter. There were moderate positive correlations between patient: FTE ratio and percent of time in the other activity group and years in renal nutrition (r=0.32, p=0.27 and r=0.24, p=0.41, respectively. The lack of statistical significance may have been due to the small sample size.
Table 4:
Spearman’s Correlation between dietitian characteristics and % of time spent in activity groups.
| Percent indirect care time | Percent direct care time | Percent other time | Percent non-work time | Direct care time per patient | Years in renal nutrition | Patients per FTE dietitiana | ||
|---|---|---|---|---|---|---|---|---|
| Percent of time in patient care area | Correlation Coefficient | −0.49 | 0.87** | −0.08 | −0.70** | 0.27 | −0.10 | −0.32 |
| Sig. (2-tailed) | 0.08 | <0.001 | 0.78 | 0.008 | 0.36 | 0.75 | 0.27 | |
| Percent indirect care time | Correlation Coefficient | −0.50 | −0.68** | 0.29 | −0.40 | 0.19 | 0.07 | |
| Sig. (2-tailed) | 0.07 | 0.007 | 0.34 | 0.16 | 0.52 | 0.82 | ||
| Percent direct care time | Correlation Coefficient | 0.01 | −0.73** | 0.31 | −0.22 | −0.35 | ||
| Sig. (2-tailed) | 0.96 | 0.005 | 0.27 | 0.46 | 0.21 | |||
| Percent other time | Correlation Coefficient | −0.005 | 0.38 | −0.12 | 0.32 | |||
| Sig. (2-tailed) | 0.99 | 0.19 | 0.67 | 0.27 | ||||
| Percent non-work time | Correlation Coefficient | −0.50 | 0.14 | 0.05 | ||||
| Sig. (2-tailed) | 0.09 | 0.64 | 0.87 | |||||
| Direct care time per patient | Correlation Coefficient | 0.22 | 0.02 | |||||
| Sig. (2-tailed) | 0.46 | 0.94 | ||||||
| Years in renal nutrition | Correlation Coefficient | 0.24 | ||||||
| Sig. (2-tailed) | 0.41 |
indicates significance at the p<0.05 level
indicates significance at the p<0.01 level
Bold indicates important correlation (Spearman’s r>0.1)
-for the two dietitians who were observed at multiple facilities, we used the patient:FTE dietitian ratio at the facility where they worked more hours
Post hoc analysis of home care visits
A total of 15 homecare patient visits were observed during seven observation sessions with four dietitians. There was a moderate correlation between number of home care patients observed and direct care time per patient, Spearman’s r=0.414, p=0.006. The mean direct care time per patient encounter in observation sessions without a home care visit was 6.25±3.62 minutes vs. 10.6±4.46 minutes in observation sessions with one or more home care visits, which was significant at p=0.008 (equal variances assumed). The percentages of time spent on each task varied slightly when observations including homecare patients were excluded from the analysis, but not enough to change the rank order. This is probably because even in observations when there were homecare patients, homecare patients were not the sole patient type seen for the day. Thus our sensitivity analysis suggests that the inclusion of some homecare visits did not skew our results.
Discussion
Based on our direct observation sessions, we estimate that patients are seen approximately 3 times per month, for an average of 20.9 minutes per patient per month. There was a trend towards less direct patient care time in the final weeks of the lab cycle, but this was not statistically significant. Dietitians spent about one-tenth of their time on documentation, and about 7% of their time on various protocols, such as oral nutrition supplement protocols.
We estimated half as much time was available for direct patient care compared to previous studies on renal dietitians: Burrowes et al2 estimated 50% of time on direct patient care based on self-reported survey data, whereas our observations suggested 25% direct patient care time. This amount of patient care time is concerning in comparison to the estimates of time required to generate nutritional status change. Ford et al17 demonstrated that changes in serum phosphorus required 20-30 minutes solely on this topic per month for 6 months, while Sevick et al18 provided more than 100 minutes per month of counseling on sodium and fluid restriction and still did not achieve an improvement in interdialytic weight gain. If dietitians are only able to speak with patients for 20 minutes per month, then there may not be enough time to achieve behavior change and improve outcomes.
While dietitians frequently queried patients as to recent changes in food consumption that might explain changes in the lab report, formal diet assessment, using a 24-hour recall or diet record, was never observed. This aligns with previous survey results indicating dietitians do not have time to complete diet assessment with the frequency and methods recommended by the KDOQI guideline6.
Increasing electronic health record functionality has been associated with increased physician burnout and time pressures for care19. Our estimate of EHR time was lower than that of other professions: medical/surgical nurses spend 33% of time on documentation20, and physicians spend 50% of time on EHR and deskwork21.
Every facility included in our direct observation had a protocol for oral nutrition supplementation during dialysis for patients with hypoalbuminemia, aligning with ISRNM recommendations22. Staff burden is one argument leveled against intradialytic supplementation22 but our results suggest that the time spent on protocols is limited.
Study strengths
Use of direct observation is a strength of our study. Direct observation is useful for quantifying the activities of health professionals and uncovering elements of work that may not be otherwise recognized. It eliminates some of the bias of self-reported data, for example surveys suggest that searching for medical records is time-consuming, but direct observation shows that it is not15. Our study demonstrates that Plan of Care meetings are less time consuming than reported via surveys, but that transit time within facilities is significant.
Study limitations
Several limitations should be considered in interpreting our results. We only collected the number of hours the dietitian was scheduled to work, therefore failing to capture any additional time spent working beyond scheduled hours, which many dietitians report in conversation. The high proportion of observation sessions during lab passing week was a limitation, as many dietitians requested observation sessions during these weeks because they were the “most interesting.” However, our analysis does not demonstrate differences in percent of time on specific tasks based on week of lab passing cycle. This may be due to a lack of power to detect a statistically significant difference. We were also unable to determine whether variation was due to cyclic trends or because of dietitian, facility, or facility ownership characteristics. We did not conduct purposive sampling so we cannot determine whether subjects were representative and/or whether dietitian time patterns varied based on facility characteristics. Our facility sample included facilities in [location redacted] urban core as well as first and second ring suburbs and outlying areas, which should include a spectrum of patient characteristics. The facilities were representative in terms of publicly available quality measures. We did not adjust for clustering of observations within RDNs or facilities, and did not determine the variability within or between these clusters. Observation sessions included some homecare patients who tended to get longer visits, and whose visits are also more private and conducive to longer conversations. However, our sensitivity analysis did not suggest that the inclusion of home care visits skewed our results. Previous research has similarly identified that the inclusion of facilities that provide home care does not change results regarding staffing4. We also did not have an equipment category for fax machine, which was used frequently to send labs to RDNs at other facilities (eg long term care).
Study implications
Our findings have implications for patients, dietitians, researchers and policy makers. From a patient’s perspective23: “If nephrologists and medical and industry professionals are serious about encourage [sic] patient participation in their own care, they must sit down with patients for a long, uninterrupted conversation about what truly matters…Inadequate communication between patient and doctor, patient and nurse, patient and administrator, and so on is the primary barrier. For the most part, it is the medical professional talking and the patient listening.” If dietitians only have time to spend 7 minutes with each patient per encounter, the long uninterrupted conversations will never happen. Future practice innovations, should focus on new models to allow more time for these conversations, including potentially group counseling24 and telehealth interventions25.
During observation sessions it was clear that some dietitians used an approach more similar to nutrition counseling, whereas others used nutrition education, and it will be important to include this systematically in future research studies. Instead of differentiating between conversation, assessment, and intervention within direct care, it may be more important to differentiate direct care with new vs established patients, given that new patient visits tended to be longer. In order to practically increase the sample size in future research, other methods may need to be used, for example, ecological momentary assessment (EMA). Rather than intensive all day coverage; EMA samples repeated, random time points and obtains participants’ real-time reporting of their current state, via a phone application or website26. For example, researchers have used an EMA app to track the time use of undergraduate students, obtaining information about how they spent the previous 15 minutes 27. This type of sampling could also help answer questions about the cyclic nature of work in dialysis facilities. EMA is an acceptable form of time documentation for establishing time and costs of federal contracts/grants 28. Participants do need access to their phones for instant recording when sampled but this is likely less burdensome than whole day diaries.
Given previous research failing to link staffing to patient care5, it seems likely that staffing ratios do not adequately describe the resulting variation in care; therefore, future research should also describe qualitative elements of staffing, including what responsibilities staff are being asked to take on, and elements of the work environment29 such as team cohesiveness and autonomy vs chaos and fragility30. Higher patient: staff ratios could be reflective of fewer administrative responsibilities and subsequently more time for direct patient care10. Given the discrepancy between important work and time-consuming work3, research should investigate assigned responsibilities are the best use of dietitians’ and other professionals’ time. Policy makers should keep in mind that new mandates may decrease patient care time in favor of additional indirect care or administrative time. These activities are often associated with decreased job satisfaction31 and increased burnout32, potentially negatively impacting patient outcomes in multiple ways.
In conclusion, this study demonstrates that a very small proportion of renal dietitian’s time is spent in direct patient care, which may explain why nutrition status changes are difficult to achieve in dialysis practice settings. Innovative approaches are needed to increase the amount of time available for direct patient care to the levels at which improvement in outcomes are observed.
Practical Application
Individual staff members of all dialysis professions can contribute to the understanding of job responsibilities through careful documentation of interactions with patients, including quantitative information about time spent and qualitative information about the interaction characteristics. Innovative approaches are needed to increase the amount of time available for direct patient care to the levels at which improvement in outcomes are observed. Practitioners who implement new approaches should carefully document outcomes and/or collaborate with researchers to measure the effectiveness.
Supplementary Material
Acknowledgements
Thank you to the Renal Practice Group of the Academy of Nutrition and Dietetics for funding this research. Also thank you to the RDNs in Northeast Ohio who participated as subjects and allowed me to observe them. Jerrilynn Burrowes, PhD, RD, CDN; Jessie Pavlinac, MS, RD, CSR, LD; Cathy Goeddeke-Merickel, MS, RDN, LD; Lesley McPhatter, MS, RD, CSR; and Mary Kay Hensley, MS, RD, CSR gave invaluable advice on important variables for observation.
Contributor Information
Rosa K Hand, Department of Nutrition and PhD candidate, Clinical and Translational Science, Case Western Reserve University. 10900 Euclid Ave Cleveland OH 44106. 216-368-3231 (p) rosa.hand@case.edu.
Jeffrey M Albert, Department of Population and Quantitative Health Sciences, Case Western Reserve University.
Ashwini R Sehgal, Center for Reducing Health Disparities, MetroHealth Medical Center, Case Western Reserve University.
References
- 1.Kopple JD. National kidney foundation K/DOQI clinical practice guidelines for nutrition in chronic renal failure. Am J Kidney Dis. 2001;37(1):S66–S70. [DOI] [PubMed] [Google Scholar]
- 2.Burrowes JD, Russell GB, Rocco MV. Multiple factors affect renal dietitians’ use of the NKF-K/DOQI adult nutrition guidelines. J Ren Nutr. 2005;15(4):407–426. doi: 10.1053/j.jrn.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 3.Hand RK, Burrowes JD. Renal dietitians’ perceptions of roles and responsibilities in outpatient dialysis facilities. J Ren Nutr. 2015;25(5):404–411. [DOI] [PubMed] [Google Scholar]
- 4.Yoder LAG, Xin W, Norris KC, Yan G. Patient care staffing levels and facility characteristics in US hemodialysis facilities. Am J Kidney Dis. 2013;62(6):1130–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hand RK, Albert JM, Sehgal AR. Structural equation modeling to explore patient to staff ratios as an explanatory factor for variation in dialysis facility outcomes. J Ren Nutr. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hand RK, Steiber A, Burrowes J. Renal dietitians lack time and resources to follow the NKF KDOQI guidelines for frequency and method of diet assessment: Results of a survey. J Ren Nutr. 2013;23(6):445–449. doi: 10.1053/j.jrn.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Thelen B, Byham-Gray L, Touger-Decker R, O’Sullivan Maillet J, Khan H. Survey of current job functions of renal dietitians. J Ren Nutr. 2009;19(6):450–461. doi: 10.1053/j.jrn.2009.05.009 [doi]. [DOI] [PubMed] [Google Scholar]
- 8.Department of Health and Human Services, Centers for Medicare and Medicaid Services. 42 CFR parts 405, 410, 413 et al. medicare and medicaid programs; conditions for coverage for end-stage renal disease facilities; final rule. Federal Register. 2008;73. [PubMed] [Google Scholar]
- 9.Blankschaen SM, Saha S, Wish JB. Management of the hemodialysis unit: Core curriculum 2016. Am J Kidney Dis. 2016;68(2):316–327. [DOI] [PubMed] [Google Scholar]
- 10.Kent PS, McCarthy MP, Burrowes JD, et al. Academy of nutrition and dietetics and national kidney foundation: Revised 2014 standards of practice and standards of professional performance for registered dietitian nutritionists (competent, proficient, and expert) in nephrology nutrition. J Acad Nutr Diet. 2014;114(9):1448–1457.e45. doi: 10.1016/j.jand.2014.05.006 [doi]. [DOI] [PubMed] [Google Scholar]
- 11.Plantinga LC, Fink NE, Sadler JH, et al. Frequency of patient-physician contact and patient outcomes in hemodialysis care. J Am Soc Nephrol. 2004;15(1):210–218. [DOI] [PubMed] [Google Scholar]
- 12.Westbrook JI, Ampt A. Design, application and testing of the work observation method by activity timing (WOMBAT) to measure clinicians’ patterns of work and communication. Int J Med Inform. 2009;78 Suppl 1:S25–33. doi: 10.1016/j.ijmedinf.2008.09.003 [doi]. [DOI] [PubMed] [Google Scholar]
- 13.Westbrook JI, Creswick NJ, Duffield C, Li L, Dunsmuir WT. Changes in nurses’ work associated with computerised information systems: Opportunities for international comparative studies using the revised work observation method by activity timing (WOMBAT). NI 2012 (2012). 2012;2012:448. [PMC free article] [PubMed] [Google Scholar]
- 14.Westbrook JI, Duffield C, Li L, Creswick NJ. How much time do nurses have for patients? A longitudinal study quantifying hospital nurses’ patterns of task time distribution and interactions with health professionals. BMC Health Serv Res. 2011;11:319-6963-11-319. doi: 10.1186/1472-6963-11-319 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Westbrook JI, Ampt A, Kearney L, Rob MI. All in a day’s work: An observational study to quantify how and with whom doctors on hospital wards spend their time. Med J Aust. 2008;188(9):506–509. [DOI] [PubMed] [Google Scholar]
- 16.Ballermann MA, Shaw NT, Mayes DC, Gibney RT, Westbrook JI. Validation of the work observation method by activity timing (WOMBAT) method of conducting time-motion observations in critical care settings: An observational study. BMC Med Inform Decis Mak. 2011;11:32-6947-11-32. doi: 10.1186/1472-6947-11-32 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ford JC, Pope JF, Hunt AE, Gerald B. The effect of diet education on the laboratory values and knowledge of hemodialysis patients with hyperphosphatemia. J Ren Nutr. 2004;14(1):36–44. [DOI] [PubMed] [Google Scholar]
- 18.Sevick MA, Piraino BM, St-Jules DE, et al. No difference in average interdialytic weight gain observed in a randomized trial with a technology-supported behavioral intervention to reduce dietary sodium intake in adults undergoing maintenance hemodialysis in the united states: Primary outcomes of the BalanceWise study. J Ren Nutr. 2016;26(3):149–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: Results from the MEMO study. J Am Med Inform Assoc. 2014;21(e1):e100–6. doi: 10.1136/amiajnl-2013-001875 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hendrich A, Chow MP, Skierczynski BA, Lu Z. A 36-hospital time and motion study: How do medical-surgical nurses spend their time? Perm J. 2008;12(3):25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: A time and motion study in 4 specialties. Ann Intern Med. 2016;165(11):753–760. doi: 10.7326/M16-0961 [doi]. [DOI] [PubMed] [Google Scholar]
- 22.Kistler BM, Benner D, Burrowes JD, et al. Eating during hemodialysis treatment: A consensus statement from the international society of renal nutrition and metabolism. J Ren Nutr. 2018;28(1):4–12. [DOI] [PubMed] [Google Scholar]
- 23.Rosenbloom DL. Surveys and patient centeredness. Nephrol News Issues. 2017(12):25.30408356 [Google Scholar]
- 24.Stein K The group appointment trend gains traction: How dietetics fits into a new model of health care delivery. J Am Diet Assoc. 2011;111(3):340–353. doi: 10.1016/j.jada.2011.01.021 [doi]. [DOI] [PubMed] [Google Scholar]
- 25.Lunney M, Lee R, Tang K, et al. Impact of telehealth interventions on processes and quality of care for patients with ESRD. Am J Kidney Dis. 2018. [DOI] [PubMed] [Google Scholar]
- 26.Stone AA, Shiffman S, Atienza AA, Nebeling L. Chapter 1: Historical roots and rational of ecological momentary assessment (EMA) In: Stone AA, Shiffman S, Atienza AA, Nebeling L, eds. The science of real-time data capture: Self-reports in health research . New York, New York: Oxford University Press; 2007:3. [Google Scholar]
- 27.Runyan JD, Steenbergh TA, Bainbridge C, Daugherty DA, Oke L, Fry BN. A smartphone ecological momentary assessment/intervention “app” for collecting real-time data and promoting self-awareness. PLoS One. 2013;8(8):e71325. doi: 10.1371/journal.pone.0071325 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Office of Management and Budget. Cost principles for state, local, and indian tribal governments. . 2004;A-87.
- 29.Duffield C, Diers D, O’Brien-Pallas L, et al. Nursing staffing, nursing workload, the work environment and patient outcomes. Appl Nurs Res. 2011;24(4):244–255. [DOI] [PubMed] [Google Scholar]
- 30.Nagykaldi Z, Zubialde J, Mold J. Developing a primary care practice fragility index (abstract). NAPCRG PBRN Meeting 2017. [Google Scholar]
- 31.Sullivan C, Leon JB, Sehgal AR. Job satisfaction among renal dietitians. J Ren Nutr. 2006;16(4):337–340. [DOI] [PubMed] [Google Scholar]
- 32.Williams AW. Addressing physician burnout: Nephrologists, how safe are we? Clin J Am Soc Nephrol. 2018;13(2):325–327. doi: 10.2215/CJN.06800617. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


