Abstract
Quantitative biomechanical characterization of pelvic supportive structures and functions in vivo is thought to provide insight into the pathophysiology of pelvic floor disorders including pelvic organ prolapse (POP). An innovative approach - vaginal tactile imaging - allows biomechanical mapping of the female pelvic floor to quantify tissue elasticity, pelvic support, and pelvic muscle functions. The objective of this study is to explore an extended set of 52 biomechanical parameters to characterize pelvic floor changes with age, parity, and subject weight for normal pelvic floor conditions. 42 subjects with normal pelvic conditions (no POP, no stress urinary incontinence) were included in the data analysis from an observational, case-controlled study. The Vaginal Tactile Imager (VTI) was used with an analytical software package to automatically calculate 52 biomechanical parameters for 8 VTI test procedures (probe insertion, elevation, rotation, Val-salva maneuver, voluntary muscle contractions in 2 planes, relaxation, and reflex contraction). The ranges, mean values, and standard deviations for all 52 VTI parameters were established. 12 VTI parameters were identified as statistically sen-sitive (p < 0.05; t-test) to the subject age; 9 parameters were identified as statistically sensitive (p < 0.05; t-test) to the subject parity; no sensitivity was found to subject weight. Among the 12 parameters sensitive to women’s age, 6 parameters show changes (decrease) in tissue elasticity and 6 parameters show weakness in pelvic muscle functions with age. Among the 9 parameters sensitive to parity, 5 parameters show changes (decrease) in tissue elasticity and 4 parameters show weakness in pelvic muscle functions after giving birth. The biomechanical mapping of the female pelvic floor with the VTI provides a unique set of parameters characterizing pelvic changes with age and parity. These objectively measurable biomechanical transformations of pelvic tissues, support structures, and functions may be used in future research and practical applications.
Keywords: Biomechanical mapping, Female pelvic floor, Aging, Parity, Tactile imaging, Tissue elasticity, Pelvic sup-port, Pelvic function, Elastography
INTRODUCTION
Many pelvic floor disorders including POP, stress urinary incontinence (SUI), sexual dysfunction, congenital anomalies, and others are clearly manifested in the mechanical properties of pelvic organs 1–4. Therefore, biomechanical mapping of the response to applied pressure or loads within the pelvic floor opens up new possibilities in biomechanical assessment and monitoring of pelvic floor conditions. The newly developed vaginal tactile imaging technique allows biomechanical mapping of the female pelvic floor including assessment of tissue elasticity, pelvic support, and pelvic muscle functions in high definition 5,6
Previously, we reported the intra- and inter-observer reproducibility of vaginal tactile imaging 7 and proposed interpretation of biomechanical mapping of the female pelvic floor 8 The new mechanistic parameters were introduced for assessment of the vaginal 9 and pelvic floor conditions 10.
The objective of this study is to identify an extended set of Vaginal Tactile Imager (VTI) parameters for biomechanical mapping of the female pelvic floor, to establish parameter ranges, and to explore their sensitivity to age, parity and patient weight for normal pelvic floor conditions.
MATERIALS AND METHODS
Definitions
Tactile Imaging is a medical imaging modality translating the sense of touch into a digital image 9. The tactile image is a function of P(x, y, z), where P is the pressure on soft tissue surface under applied deformation and x, y and z are the coordinates where P was measured. The tactile image is a pressure map on which the direction of tissue deformation must be specified.
Functional Tactile Imaging translates muscle activity into dynamic pressure pattern P(x, y, t) for an area of interest, where t is time and x and y are coordinates where pressure P was measured. It may include: (a) muscle voluntary contraction, (b) involuntary reflex contraction, (c) involuntary relaxation, and (d) specific maneuvers.
Biomechanical Mapping = Tactile Imaging + Functional Tactile Imaging
A tactile imaging probe has a pressure sensor array mounted on its face that acts similar to human fingers during a clinical examination, deforming the soft tissue and detecting the resulting changes in the pressure pattern on the surface. The sensor head is moved over the surface of the tissue to be studied, and the pressure response is evaluated at multiple locations along the tissue. The results are used to generate 2D/3D images showing pressure distribution over the area of the tissue under study.
Generally, an inverse problem solution for tactile image P(x, y, z) would allow the reconstruction of tissue elasticity distribution (E) as a function of the same coordinates E(x, y, z). Unfortunately, the inverse problem solution is hardly possible for most real objects because it is a non-linear and ill-posed problem. However, the tactile image P(x, y, z) per se reveals tissue or organ anatomy and elasticity distribution because it maintains the stress-strain relationship for deformed tissue 11,12. Thus the spatial gradients ∂P(x, y, z)/ ∂x, ∂P(x, y, z)/ ∂y, and ∂P(x, y, z)/ ∂z can be used in practice for soft tissue elasticity mapping, despite structural and anatomical variations 6
Vaginal Tactile Imager
The VTI, model 2S (Advanced Tactile Imaging, Inc., NJ), was used in all test procedures. The VTI probe, as shown in Figure 1, is equipped with 96 pressure (tactile) sensors spaced at 2.5 mm consecutively on both sides of the probe, an orientation sensor, and temperature controllers to provide the probe temperature close to a human body before the examination. During the clinical procedure, the probe is used to acquire pressure responses from two opposite vaginal walls along the vagina. The VTI data are sampled from the probe sensors and displayed on the VTI monitor in real time. The resulting pressure maps (tactile images) of the vagina integrate all the acquired pressure and positioning data for each of the pressure sensing elements. Additionally, the VTI records the dynamic contraction for pelvic floor muscles with resolution of 1 mm. A lubricating jelly is used for patient comfort and to provide reproducible boundary/contact conditions with deformed tissues.
Figure 1.-.
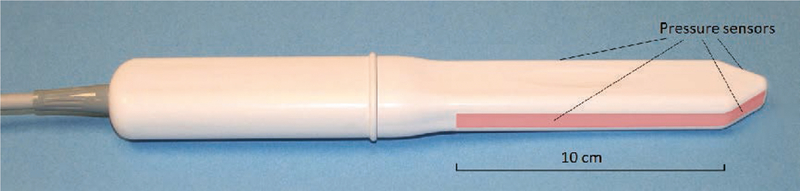
Vaginal Probe. Pressure sensors are aligned on the outer surfaces of the probe (highlighted in the image).
This VTI probe allows 3 – 15 mm tissue deformation at the probe insertion (Tests 1), 20 – 45 mm tissue deformation at the probe elevation (Test 2), 5 – 7 mm deformation at the probe rotation (Test 3) and recording of dynamic responses at pelvic muscle contractions (Tests 4 – 8). The probe maneuvers in Tests 1 – 3 allow accumulation of multiple pressure patterns from the tissue surface to compose an integrated tactile image for the investigated area using a proprietary image composition algorithm similar to the imaging of the prostate and breast 11,12 The spatial gradients ∂P (x, y) / ∂y for anterior and posterior compartments are calculated within the acquired tactile images in Tests 1 and 2; y-coordinate is directed orthogonally from the vaginal channel, x-coordinate is located on the vaginal channel. The VTI software includes data analysis tools and reporting functions. It visualizes the anatomy, pressure maps, and calculates (automatically) 52 VTI parameters for eight test procedures. The VTI examination procedure consists of eight tests: 1) probe insertion, 2) elevation, 3) rotation, and 4) Valsalva maneuver, 5) voluntary muscle contraction, 6) voluntary muscle contraction (left versus right side), 6) involuntary relaxation, and 8) reflex muscle contraction (cough). Tests 1 – 5 and 7 – 8 provide data for anterior/posterior compartments; test 7 provides data for left/right sides.
The VTI absolute measurement accuracy is as follows: ±0.2 kPa within 10 kPa range, ±0.5 kPa at 25 kPa, ±1.0 kPa at 60 kPa. The VTI relative pressure measurement accuracy lies in the range between ±0.05 kPa to ±0.1 kPa. The VTI pressure measurement resolution is 0.001 kPa. The VTI absolute measurement accuracy for probe orientation is ±0.5 degree and ±0.1°C for measuring the temperature inside the probe on the surface of the pressure sensors. The VTI probe was calibrated immediately before every subject examination; it was cleaned and disinfected between the patients.
Biomechanical Mapping Parameters
Table 1 lists 52 biomechanical parameters being calculated for every participating subject based on VTI data recorded in tests 1 – 8. Anatomical assignment of the targeting/contributing pelvic structures into the specified parameters is based on published data 1, 3, 4, 13–15
Table 1.
VTI Biomechanical Parameters.
| No. | VTI Test |
Parameters Abbreviation |
Units | Parameter Description | Parameter Interpretation | Parameter Class | Targeting/Contributing Pelvic Structures |
|---|---|---|---|---|---|---|---|
| 1 | 1 | Fmax | N | Maximum value of force measured during the VTI probe insertion [9] | Maximum resistance of anterior vs posterior widening; tissue elasticity at specified location (capability to resist to applied deformation) | Maximum vaginal tissue elasticity at specified location | Tissues behind the anterior and posterior vaginal walls at 3–15 mm depth |
| 2 | 1 | Work | mJ | Work completed during the probe insertion (Work = Force × Displacement) [9] | Integral resistance of vaginal tissue (anterior and posterior) along the probe insertion | Average vaginal tissue elasticity | Tissues behind the anterior and posterior vaginal walls at 3–15 mm depth |
| 3 | 1 | Gmax_a | kPa/mm | Maximum value of anterior gradient (change of pressure per anterior wall displacement in orthogonal direction to the vaginal channel) | Maximum value of tissue elasticity in anterior compartment behind the vaginal at specified location | Maximum value of anterior tissue elasticity | Tissues/structures in anterior compartment at 10–15 mm depth |
| 4 | 1 | Gmax_p | kPa/mm | Maximum value of posterior gradient (change of pressure per posterior wall displacement in orthogonal direction to the vaginal channel) | Maximum value of tissue elasticity in posterior compartment behind the vaginal at specified location | Maximum value of posterior tissue elasticity | Tissues/structures in anterior compartment at 10–15 mm depth |
| 5 | 1 | Pmax_a | kPa | Maximum value of pressure per anterior wall along the vagina | Maximum resistance of anterior tissue to vaginal wall deformation | Anterior tissue elasticity | Tissues/structures in anterior compartment |
| 6 | 1 | Pmax_p | kPa | Maximum value of pressure per posterior wall along the vagina | Maximum resistance of posterior tissue to vaginal wall deformation | Posterior tissue elasticity | Tissues/structures in posterior compartment |
| 7 | 2 | P1max_a | kPa | Maximum pressure at the area of pubic bone (anterior, A1 in Figure 2) | Proximity of pubic bone to vaginal wall and perineal body strength | Anatomic aspects and tissue elasticity | Tissues between vagina and pubic bone; perineal body |
| 8 | 2 | P2max_a | kPa | Maximum pressure at the area of urethra (anterior, A2 in Figure 2) | Elasticity/mobility of urethra | Anatomic aspects and tissue elasticity | Urethra and surrounding tissues |
| 9 | 2 | P3max_a | kPa | Maximum pressure at the cervix area (anterior, A3 in Figure 2) | Mobility of uterus and conditions of uterosacral and cardinal ligaments | Pelvic floor support | Uterosacral and cardinal ligaments |
| 10 | 2 | P1max_p | kPa | Maximum pressure at the perineal body (posterioir, see P1 in Figure 2) | Pressure feedback of Level III support | Pelvic floor support | Puboperineal, puborectal muscles |
| 11 | 2 | P2max_p | kPa | Maximum pressure at middle third of vagina (posterioir, see P2 in Figure 2) | Pressure feedback of Level II support | Pelvic floor support | Pubovaginal, puboanal muscles |
| 12 | 2 | P3max_p | kPa | Maximum pressure at upper third of vagina (posterioir, see P3 in Figure 2) | Pressure feedback of Level I support | Pelvic floor support | Iliococcygeal muscle, levator plate |
| 13 | 2 | G1max_a | kPa/mm | Maximum gradient at the area of pubic bone (anterior, see A1 in Figure 2) | Vaginal elasticity at pubic bone area | Anterior tissue elasticity | Tissues between vagina and pubic bone; perineal body |
| 14 | 2 | G2max_a | kPa/mm | Maximum gradient at the area of urethra (anterior, see A2 in Figure 2) | Mobility and elasticity of urethra | Urethral tissue elasticity | Urethra and surrounding tissues |
| 15 | 2 | G3max_a | kPa/mm | Maximum gradient at the cervix area (anterior, see A3 in Figure 2) | Conditions of uterosacral and cardinal ligaments | Pelvic floor support | Uterosacral and cardinal ligaments |
| 16 | 2 | G1max_p | kPa/mm | Maximum gradient at the perineal body (posterioir, see P1 in Figure 2) | Strength of Level III support (tissue deformation up to 25 mm) | Pelvic floor support | Puboperineal, puborectal muscles |
| 17 | 2 | G2max_p | kPa/mm | Maximum gradient at middle third of vagina (posterioir, see P2 in Figure 2) | Strength of Level II support (tissue deformation up to 35 mm) | Pelvic floor support | Pubovaginal, puboanal muscles |
| 18 | 2 | G3max_p | kPa/mm | Maximum gradient at upper third of vagina (posterioir, see P3 in Figure 2) | Strength of Level I support (tissue deformation up to 45 mm) | Pelvic floor support | Iliococcygeal muscle, levator plate |
| 19 | 3 | Pmax | kPa | Maximum pressure at vaginal walls deformation by 7 mm [9] | Hard tissue or tight vagina | Vaginal tissue elasticity | Tissues behind the vaginal walls at 5–7 mm depth |
| 20 | 3 | Fap | N | Force applied by anterior and posterior compartments to the probe [9]. | Integral strength of anterior and posterior compartments | Vaginal tightening | Tissues behind anterior/ posterior vaginal walls. |
| 21 | 3 | Fs | N | Force applied by entire left and right sides of vagina to the probe [9]. | Integral strength of left and right sides of vagina | Vaginal tightening | Vaginal right/left walls and tissues behind them. |
| 22 | 3 | P1_l | kPa | Pressure response from a selected location (irregularity 1) at left side (see S1 in Figure 2) | Hard tissue on left vaginal wall | Irregularity on vaginal wall | Tissue/muscle behind the vaginal walls on left side. |
| 23 | 3 | P2_l | kPa | Pressure response from a selected location (irregularity 2) at left side (see S2 in Figure 2) | Hard tissue on left vaginal wall | Irregularity on vaginal wall | Tissue/muscle behind the vaginal walls on left side. |
| 24 | 3 | P3_r | kPa | Pressure response from a selected location (irregularity 3) at right side (see S1 in Figure 2) | Hard tissue on right vaginal wall | Irregularity on vaginal wall | Tissue/muscle behind the vaginal walls on right side. |
| 25 | 4 | dF_a | N | Integral force change in anterior compartment at Valsalva maneuver | Pelvic function* at Valsalva maneuver | Pelvic function | Multiple pelvic muscle* |
| 26 | 4 | dPmax_a | kPa | Maximum pressure change in anterior compartment at Valsalva maneuver. | Pelvic function* at Valsalva maneuver | Pelvic function | Multiple pelvic muscle* |
| 27 | 4 | dL_a | mm | Displacement of the maximum pressure peak in anterior compartment | Mobility of anterior structures* Valsalva maneuver | Pelvic function | Urethra, pubovaginal muscle; ligaments* |
| 28 | 4 | dF_p | N | Integral force change in posterior compartment at Valsalva maneuver | Pelvic function* at Valsalva maneuver | Pelvic function | Multiple pelvic muscle* |
| 29 | 4 | dPmax_p | kPa | Maximum pressure change in posterior compartment at Valsalva maneuver. | Pelvic function* at Valsalva maneuver | Pelvic function | Multiple pelvic muscle* |
| 30 | 4 | dL_p | mm | Displacement of the maximum pressure peak in posterior compartment | Mobility of posterioir structures* Valsalva maneuver | Pelvic function | Anorectal, puborectal, pubovaginal muscles; ligaments* |
| 31 | 5 | dF_a | N | Integral force change in anterior compartment at voluntary muscle contraction | Integral contraction strength of pelvic muscles along the vagina | Pelvic function | Puboperineal, puborectal, pubovaginal and ilicoccygeal muscles; uretra |
| 32 | 5 | dPmax_a | kPa | Maximum pressure change in anterior compartment at voluntary muscle contraction | Contraction strength of specified pelvic muscles | Pelvic function | Puboperineal, puborectal and pubovaginal muscles |
| 33 | 5 | Pmax_a | kPa | Maximum pressure value in anterior compartment at voluntary muscle contraction. | Static and dynamic peak support of the pelvic floor | Pelvic function | Puboperineal and puborectal muscles* |
| 34 | 5 | dF_p | N | Integral force change in posterior compartment at voluntary muscle contraction | Integral contraction strength of pelvic muscles along the vagina | Pelvic function | Puboperineal, puborectal, pubovaginal and ilicoccygeal muscles |
| 35 | 5 | dPmax_p | kPa | Maximum pressure change in posterior compartment at voluntary muscle contraction | Contraction strength of pelvic muscles at specified location | Pelvic function | Puboperineal, puborectal and pubovaginal muscles |
| 36 | 5 | Pmax_p | kPa | Maximum pressure value in posterior compartment at voluntary muscle contraction. | Static and dynamic peak support of the pelvic floor | Pelvic function | Puboperineal and puborectal muscles* |
| 37 | 6 | dF_r | N | Integral force change in right side at voluntary muscle contraction | Integral contraction strength of pelvic muscles along the vagina | Pelvic function | Puboperineal, puborectal, and pubovaginal muscles |
| 38 | 6 | dPmax_r | kPa | Maximum pressure change in right side at voluntary muscle contraction | Contraction strength of specific pelvic muscle | Pelvic function | Puboperineal or puborectal or pubovaginal muscles |
| 39 | 6 | Pmaxa_r | kPa | Maximum pressure value in right side at voluntary muscle contraction | Specified pelvic muscle contractive capability and integrity | Pelvic function | Puboperineal or puborectal muscles |
| 40 | 6 | dF_l | N | Integral force change in left side at voluntary muscle contraction | Integral contraction strength of pelvic muscles along the vagina | Pelvic function | Puboperineal, puborectal, and pubovaginal muscles |
| 41 | 6 | dPmax_l | kPa | Maximum pressure change in left side at voluntary muscle contraction | Contraction strength of specific pelvic muscle | Pelvic function | Puboperineal or puborectal or pubovaginal muscles |
| 42 | 6 | Pmaxa_l | kPa | Maximum pressure value in left side at voluntary muscle contraction | Specified pelvic muscle contractive capability and integrity | Pelvic function | Puboperineal or puborectal muscles |
| 43 | 7 | dPdt_a | kPa/s | Anterior absolute pressure change per second for maximum pressure at involuntary relaxation | Innervation status of specified pelvic muscles | Innervations status | Levator ani muscles |
| 44 | 7 | dPcdt_a | %/s | Anterior relative pressure change per second for maximum pressure at involuntary relaxation | Innervation status of specified pelvic muscles | Innervations status | Levator ani muscles |
| 45 | 7 | dPdt_p | kPa/s | Posterior absolute pressure change per second for maximum pressure at involuntary relaxation | Innervation status of specified pelvic muscles | Innervations status | Levator ani muscles |
| 46 | 7 | dPcdt_p | %/s | Posterior relative pressure change per second for maximum pressure at involuntary relaxation | Innervation status of specified pelvic muscles | Innervations status | Levator ani muscles |
| 47 | 8 | dF_a | N | Integral force change in anterior compartment at reflex pelvic muscle contraction (cough) | Integral pelvic function* at reflex muscle contraction | Pelvic function | Multiple pelvic muscle* |
| 48 | 8 | dPmax_a | kPa | Maximum pressure change in anterior compartment at reflex pelvic muscle contraction (cough). | Contraction strength of specified pelvic muscles | Pelvic function | Multiple pelvic muscle* |
| 49 | 8 | dL_a | mm | Displacement of the maximum pressure peak in anterior compartment | Mobility of anterior structures* at reflex muscle contraction | Pelvic function | Urethra, pubovaginal muscle; ligaments* |
| 50 | 8 | dF_p | N | Integral force change in posterior compartment at reflex pelvic muscle contraction (cough) | Integral pelvic function* at reflex muscle contraction | Pelvic function | Multiple pelvic muscle* |
| 51 | 8 | dPmax_p | kPa | Maximum pressure change in posterior compartment at reflex pelvic muscle contraction (cough). | Contraction strength of specified pelvic muscles | Pelvic function | Multiple pelvic muscle* |
| 52 | 8 | dL_p | mm | Displacement of the maximum pressure peak in posterior compartment | Mobility of anterior structures* at reflex muscle contraction | Pelvic function | Anorectal, puborectal and pubovaginal muscles; ligaments* |
requires further interpretation
Population Description
42 subjects with normal pelvic conditions (no POP, no SUI) were inlcuded in the data analysis from multi-site observational, case-controlled study (clinical trial identifier NCT02294383). The subject age, height, weight, and parity distribution data are present in Table 2. Prior to the VTI examination, a standard physical examination was performed, including a bimanual pelvic examination and Pelvic Organ Prolapse Quantification (POP-Q) 16. None of the analyzed subjects had a prior history of pelvic floor surgery. The clinical protocol was approved by the Institutional Review Board and all women provided written informed consent to be enrolled into the study. This clinical research was done in compliance with the Health Insurance Portability and Accountability Act. The VTI examination data for eight Tests were obtained and recorded at the time of the scheduled routine urogynecologic visits.
Table 2.
Biomechanical Parameters for two age groups: Group 1 of 26 subjects ≤52 y.o., Group 2 of 16 subjects >52 y.o.
| H | p | Units | Average Group 1 |
Average Group 2 |
SD Group 1 |
SD Group 2 |
||
|---|---|---|---|---|---|---|---|---|
|
Height →
Weight → Age → Parity (P) → |
0 | 0.315 | cm | 163.1 | 159.3 | 10.1 | 14.3 | |
| 0 | 0.177 | kg | 60.4 | 80.8 | 6.8 | 6.1 | ||
| 1 | 1 × 10−12 | y.o | 40.7 | 68.3 | 8.3 | 9.0 | ||
| 0 | 0.117 | - | 1.23 | 1.75 | 0.99 | 1.06 | ||
|
Parameters
number ↓ |
Test ↓ | |||||||
| 1 | 1 | 1 | 0.016 | N | 1.46 | 0.90 | 0.80 | 0.48 |
| 2 | 1 | 1 | 0.009 | mJ | 49.23 | 31.14 | 23.41 | 15.79 |
| 3 | 1 | 0 | 0.103 | kPa/mm | 2.82 | 1.67 | 2.65 | 0.84 |
| 4 | 1 | 0 | 0.196 | kPa/mm | 1.74 | 1.29 | 1.21 | 0.78 |
| 5 | 1 | 0 | 0.263 | kPa | 43.10 | 33.48 | 29.90 | 20.24 |
| 6 | 1 | 1 | 0.047 | kPa | 26.07 | 17.07 | 16.27 | 8.15 |
| 7 | 2 | 0 | 0.490 | kPa | 26.96 | 30.33 | 14.04 | 17.02 |
| 8 | 2 | 0 | 0.534 | kPa | 12.44 | 10.89 | 8.21 | 6.98 |
| 9 | 2 | 0 | 0.648 | kPa | 8.96 | 7.78 | 6.70 | 10.03 |
| 10 | 2 | 0 | 0.077 | kPa | 15.86 | 10.45 | 11.19 | 5.14 |
| 11 | 2 | 0 | 0.914 | kPa | 9.45 | 9.68 | 7.23 | 5.03 |
| 12 | 2 | 0 | 0.198 | kPa | 8.14 | 4.99 | 9.22 | 3.24 |
| 13 | 2 | 0 | 0.488 | kPa/mm | 1.74 | 2.12 | 1.74 | 1.54 |
| 14 | 2 | 0 | 0.794 | kPa/mm | 0.76 | 0.83 | 0.76 | 0.99 |
| 15 | 2 | 0 | 0.610 | kPa/mm | 0.62 | 0.51 | 0.58 | 0.81 |
| 16 | 2 | 0 | 0.057 | kPa/mm | 0.93 | 0.39 | 1.06 | 0.40 |
| 17 | 2 | 0 | 0.763 | kPa/mm | 0.40 | 0.43 | 0.29 | 0.32 |
| 18 | 2 | 0 | 0.107 | kPa/mm | 0.56 | 0.25 | 0.74 | 0.18 |
| 19 | 3 | 0 | 0.562 | kPa | 33.27 | 30.37 | 15.42 | 15.99 |
| 20 | 3 | 0 | 0.120 | N | 4.40 | 3.45 | 2.14 | 1.34 |
| 21 | 3 | 0 | 0.073 | N | 1.37 | 0.90 | 0.90 | 0.60 |
| 22 | 3 | 1 | 0.003 | kPa | 11.43 | 5.60 | 7.10 | 2.02 |
| 23 | 3 | 1 | 0.012 | kPa | 5.87 | 3.42 | 3.52 | 1.55 |
| 24 | 3 | 1 | 0.001 | kPa | 12.29 | 5.91 | 6.93 | 2.48 |
| 25 | 4 | 0 | 0.128 | N | 1.44 | 1.02 | 0.94 | 0.53 |
| 26 | 4 | 0 | 0.717 | kPa | 11.28 | 9.90 | 12.38 | 9.07 |
| 27 | 4 | 0 | 0.558 | mm | 2.31 | 1.28 | 4.68 | 5.47 |
| 28 | 4 | 0 | 0.094 | N | 1.46 | 0.94 | 1.06 | 0.56 |
| 29 | 4 | 0 | 0.350 | kPa | 7.73 | 5.76 | 7.02 | 4.78 |
| 30 | 4 | 0 | 0.299 | mm | 1.44 | 3.44 | 4.46 | 6.49 |
| 31 | 5 | 0 | 0.248 | N | 1.71 | 1.35 | 1.09 | 0.79 |
| 32 | 5 | 0 | 0.124 | kPa | 25.15 | 17.58 | 16.43 | 12.79 |
| 33 | 5 | 0 | 0.259 | kPa | 43.52 | 36.54 | 20.97 | 15.76 |
| 34 | 5 | 0 | 0.070 | N | 2.11 | 1.39 | 1.36 | 0.96 |
| 35 | 5 | 1 | 0.024 | kPa | 16.45 | 9.66 | 10.58 | 5.98 |
| 36 | 5 | 1 | 0.009 | kPa | 26.06 | 17.39 | 11.59 | 6.51 |
| 37 | 6 | 0 | 0.056 | N | 1.03 | 0.63 | 0.62 | 0.59 |
| 38 | 6 | 1 | 0.019 | kPa | 9.70 | 5.04 | 6.33 | 4.80 |
| 39 | 6 | 1 | 0.004 | kPa | 16.62 | 8.99 | 8.41 | 6.16 |
| 40 | 6 | 0 | 0.110 | N | 1.01 | 0.64 | 0.70 | 0.67 |
| 41 | 6 | 1 | 0.031 | kPa | 8.61 | 4.71 | 5.57 | 4.80 |
| 42 | 6 | 1 | 0.002 | kPa | 15.81 | 7.86 | 8.48 | 5.51 |
| 43 | 7 | 0 | 0.501 | kPa/s | −1.45 | −1.08 | 1.82 | 1.37 |
| 44 | 7 | 0 | 0.618 | %/s | −3.36 | −2.76 | 3.79 | 3.31 |
| 45 | 7 | 0 | 0.195 | kPa/s | −1.27 | −0.68 | 1.60 | 0.87 |
| 46 | 7 | 0 | 0.785 | %/s | −4.26 | −3.91 | 4.24 | 3.37 |
| 47 | 8 | 0 | 0.138 | N | 2.59 | 1.83 | 1.44 | 1.33 |
| 48 | 8 | 0 | 0.990 | kPa | 13.91 | 13.97 | 14.27 | 16.30 |
| 49 | 8 | 0 | 0.530 | mm | 6.99 | 5.91 | 3.91 | 5.66 |
| 50 | 8 | 0 | 0.062 | N | 2.68 | 1.69 | 1.42 | 1.46 |
| 51 | 8 | 0 | 0.096 | kPa | 13.55 | 8.66 | 7.94 | 8.01 |
| 52 | 8 | 0 | 0.723 | mm | 4.01 | 3.19 | 6.03 | 6.90 |
Total study workflow comprised of the following steps: (1) Recruiting women who routinely undergo vaginal examination as a part of their diagnostic treatment of concerned areas; (2) Acquisition of clinical diagnostic information related to the studied cases by standard clinical means; (3) Performing a VTI examination in lithotomic position; (4) Analyzing VTI data and assessment of the VTI parameters for pelvic floor characterization.
Statistical Analysis
52 biomechanical parameters were calculated automatically per each of the 42 analyzed VTI examinations or cases (one VTI examination per each subjects). In some rare cases the parameter calculation required a manual correction of the anatomical location where the parameters must be calculated. Unpaired t-tests between two subject groups with thresholds by age, parity or subject weight were completed per parameter to determine whether the parameter showed dependence on the age, parity or subject weight. For visual evaluation of the analyzed clinical data distributions we used notched boxplots 17 showing a confidence interval for the median value (central horizontal line), 25% and 75% quartiles. The spacing between the different parts of the box helps to compare variance. The boxplot also determines skewness (asymmetry) and outlier (cross). The intersection or divergence of confidence intervals for two patient samples is a visual analog of the t-test. The MATLAB (MathWorks, MA) statistical functions were used for the data analysis. The MATLAB (MathWorks, MA) statistical functions were used for the data analysis.
RESULTS
To illustrate the approach and location used in calculating the biomechanical parameters, the VTI examination data for all eight tests, as they observed by an operator in real time, are displayed in Figures 4 - 11 (see Supplementary material). Table 2 displays the calculated statistics (hypothesis testing outcome H- and p-value) for two age groups with threshold of 52 y.o. Average values for 52 biomechanical parameters and standard deviations (SD) for both groups are presented. Table 4 presents the calculated statistics (hypothesis testing outcome H- and p-value) for nulliparous versus parous (Parity > 0) woment, two parity groups average values and standard deviations for 52 biomechanical parameters.
Calculated statistics (hypothesis testing outcome H- and p-value) for two weight groups with threshold of 69 kg demonstrated no sensitivity to women weight; H = 0 and p > 0.316 for all 52 biomechanical parameters.
The t-tests for the age groups demonstrate that 12 out of 52 parameters have statistically significant differences between the groups and that these parameters have the potential to be used for identification of age-related changes in the female pelvic floor (see Table 2). The analysed groups, statistically, have the same subject height, weight, and parity distributions (H = 0, p>0.05). The t-tests for the parity groups demonstrate that 9 out of 52 parameters have statistically significant differences between the groups and that these parameters have the potential to be used for the identification of parity changes in the female pelvic floor (see Table 3). The analysed groups also statistically have the same subject height, weight and age distributions (H = 0, p>0.05). The t-tests for the weight groups demonstrate that o out of 52 parameters have statistically significant differences between the groups; nothing changes with women’s weight (see Table 3). The analysed groups thus statistically have the same subject height, age and parity distributions (H = 0, p>0.05).
Table 3.
Biomechanical Parameters for two groups: Group 1 of 11 nulliparous subjects, Group 2 of 31 subjects with parity ≥1.
| H | p | Units | Aver Group 1 | Aver Group 2 | SD Group 1 |
SD Group 2 |
||
|---|---|---|---|---|---|---|---|---|
|
Height →
Weight → Age → Parity (P) → |
0 | 0.843 | cm | 161.1 | 161.9 | 13.8 | 11.3 | |
| 0 | 0.587 | kg | 147.5 | 152.6 | 25.1 | 27.2 | ||
| 0 | 0.185 | y.o | 45.6 | 53.1 | 15.2 | 16.1 | ||
| 1 | 1 × 10−11 | - | 0.0 | 1.9 | 0.0 | 0.7 | ||
|
Parameters
number ↓ |
Test ↓ | |||||||
| 1 | 1 | 1 | 0.034 | N | 1.65 | 1.10 | 1.08 | 0.53 |
| 2 | 1 | 0 | 0.141 | mJ | 50.95 | 39.29 | 29.43 | 19.08 |
| 3 | 1 | 0 | 0.072 | kPa/mm | 3.41 | 2.01 | 3.18 | 1.66 |
| 4 | 1 | 0 | 0.651 | kPa/mm | 1.69 | 1.52 | 0.61 | 1.21 |
| 5 | 1 | 0 | 0.347 | kPa | 46.04 | 37.09 | 36.63 | 22.61 |
| 6 | 1 | 0 | 0.291 | kPa | 26.61 | 21.24 | 11.45 | 15.14 |
| 7 | 2 | 0 | 0.497 | kPa | 25.54 | 29.20 | 5.00 | 17.35 |
| 8 | 2 | 0 | 0.427 | kPa | 10.24 | 12.42 | 6.22 | 8.20 |
| 9 | 2 | 0 | 0.511 | kPa | 7.12 | 9.00 | 4.79 | 8.92 |
| 10 | 2 | 0 | 0.321 | kPa | 16.31 | 12.91 | 9.10 | 9.82 |
| 11 | 2 | 0 | 0.826 | kPa | 9.16 | 9.67 | 6.88 | 6.35 |
| 12 | 2 | 0 | 0.397 | kPa | 8.64 | 6.34 | 12.46 | 5.11 |
| 13 | 2 | 1 | 0.020 | kPa/mm | 0.90 | 2.23 | 0.44 | 1.79 |
| 14 | 2 | 0 | 0.100 | kPa/mm | 0.43 | 0.92 | 0.44 | 0.92 |
| 15 | 2 | 0 | 0.343 | kPa/mm | 0.41 | 0.63 | 0.28 | 0.76 |
| 16 | 2 | 0 | 0.579 | kPa/mm | 0.86 | 0.68 | 0.73 | 0.96 |
| 17 | 2 | 0 | 0.221 | kPa/mm | 0.51 | 0.38 | 0.38 | 0.26 |
| 18 | 2 | 0 | 0.197 | kPa/mm | 0.64 | 0.37 | 1.03 | 0.36 |
| 19 | 3 | 0 | 0.464 | kPa | 35.15 | 31.10 | 15.42 | 15.65 |
| 20 | 3 | 0 | 0.332 | N | 4.52 | 3.86 | 2.00 | 1.89 |
| 21 | 3 | 0 | 0.061 | N | 1.59 | 1.05 | 0.81 | 0.80 |
| 22 | 3 | 0 | 0.144 | kPa | 11.63 | 8.35 | 5.98 | 6.36 |
| 23 | 3 | 1 | 0.006 | kPa | 7.09 | 4.17 | 4.16 | 2.32 |
| 24 | 3 | 1 | 0.042 | kPa | 13.22 | 8.67 | 6.16 | 6.19 |
| 25 | 4 | 0 | 0.218 | N | 1.55 | 1.14 | 1.14 | 0.66 |
| 26 | 4 | 0 | 0.891 | kPa | 11.10 | 10.48 | 13.25 | 10.25 |
| 27 | 4 | 0 | 0.284 | mm | 3.51 | 1.31 | 5.04 | 4.99 |
| 28 | 4 | 0 | 0.505 | N | 1.40 | 1.16 | 1.23 | 0.78 |
| 29 | 4 | 0 | 0.960 | kPa | 6.90 | 6.77 | 7.11 | 5.86 |
| 30 | 4 | 0 | 0.541 | mm | 3.45 | 2.06 | 4.69 | 5.79 |
| 31 | 5 | 0 | 0.216 | N | 1.89 | 1.46 | 1.51 | 0.73 |
| 32 | 5 | 1 | 0.047 | kPa | 30.17 | 19.46 | 21.62 | 11.79 |
| 33 | 5 | 0 | 0.064 | kPa | 50.08 | 37.58 | 22.65 | 17.14 |
| 34 | 5 | 0 | 0.313 | N | 2.17 | 1.72 | 1.74 | 1.06 |
| 35 | 5 | 0 | 0.360 | kPa | 16.17 | 13.04 | 12.72 | 8.36 |
| 36 | 5 | 0 | 0.322 | kPa | 25.55 | 21.76 | 12.30 | 10.18 |
| 37 | 6 | 1 | 0.034 | N | 1.27 | 0.74 | 0.87 | 0.51 |
| 38 | 6 | 0 | 0.096 | kPa | 10.88 | 6.80 | 7.34 | 5.55 |
| 39 | 6 | 0 | 0.093 | kPa | 17.71 | 12.11 | 7.65 | 8.25 |
| 40 | 6 | 1 | 0.008 | N | 1.42 | 0.69 | 1.13 | 0.45 |
| 41 | 6 | 1 | 0.044 | kPa | 10.39 | 5.97 | 7.05 | 4.76 |
| 42 | 6 | 0 | 0.072 | kPa | 17.03 | 11.09 | 8.73 | 7.82 |
| 43 | 7 | 0 | 0.975 | kPa/s | −1.31 | −1.29 | 1.55 | 1.68 |
| 44 | 7 | 0 | 0.993 | %/s | −3.11 | −3.10 | 3.22 | 3.70 |
| 45 | 7 | 0 | 0.868 | kPa/s | −0.94 | −1.03 | 0.80 | 1.47 |
| 46 | 7 | 0 | 0.666 | %/s | −4.64 | −3.96 | 3.65 | 3.94 |
| 47 | 8 | 0 | 0.406 | N | 2.63 | 2.13 | 1.15 | 1.51 |
| 48 | 8 | 0 | 0.153 | kPa | 20.51 | 11.74 | 8.12 | 16.14 |
| 49 | 8 | 0 | 0.796 | mm | 6.90 | 6.39 | 3.20 | 5.16 |
| 50 | 8 | 0 | 0.437 | N | 2.61 | 2.12 | 1.31 | 1.56 |
| 51 | 8 | 0 | 0.404 | kPa | 13.55 | 10.70 | 6.20 | 8.78 |
| 52 | 8 | 1 | 0.049 | mm | 7.44 | 2.39 | 9.71 | 4.32 |
Figure 3 displays the boxplots for select parameters for the age groups presented in Table 2 (panels A - D) and for parity groups presented in Table 3 (panels E - H).
Figure 3.-.
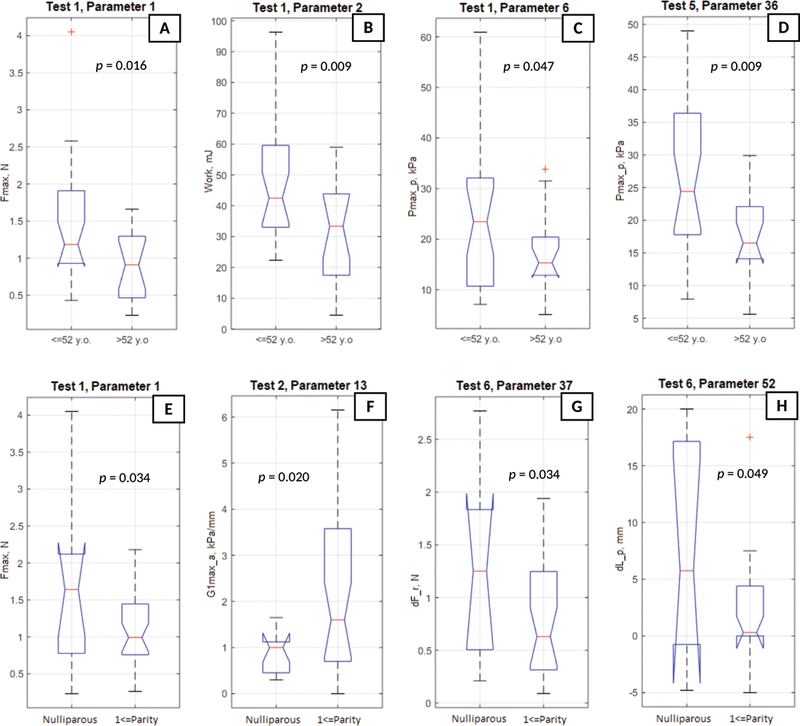
Boxplots A - D for selected biomechanical parameters for the age groups and boxplots E - H for selected biomechanical parameters for the parity groups.
DISCUSSION
The results of this research agree with previously reported data 4–10; however, the current analysis includes the biggest VTI parameter set ever considered. 12 of 52 biomechanical parameters are identified as having statistically significant sensitivity to the women’s age (see Tables 2). Their average changes are from 49.9% to 107.8% (78.2% in average). 9 of 52 biomechanical parameters are identified as having statistically significant sensitivity to women’s parity (see Tables 3). Their average changes are from 49.6% to 211% (83.2% in average). These changes with age and parity clearly outperform possible deviations related to VTI intra- and inter-operator variability which were found on an average of ±15.1% (intra-observer error) and ±18.4 (inter-observer error) 7. These reproducibility errors have value and sign intrinsically by a chance, but we have identified statistically systematic parameter changes by age and parity. No parameter changes were found with the women weight.
Let’s consider the age changes. Test 1 provides three identified age-sensitive parameters (1, 2, 6) related to tissue elasticity; their average values is changed by 52.8% - 67.18% (see panels A - C in Figure 3). No changes in pelvic support, which could be detected by Test 2 parameters were found. Test 3 provides three identified parameters (22, 23, 24) related to the tissue elasticity of side vaginal walls and beyond 3–7 mm (small irregularities); their average values change from 71.6% to 108%. Pelvic muscle contraction Tests 5 and 6 provide six identified parameters (35, 36, 38, 39, 41, 42) related to pelvic function; their average values are changed by 49.9% - 101.2% (see panel D in Figure 3). All these 6 parameters demonstrate a decrease in muscle contractive capabilities in Level I (levator plate muscle) and Level II support (pubovaginal and ilicoccygeal muscles). Valsalva maneuver (Test 4), involuntary muscle relaxation (Test 7), and reflex muscle contraction at cough (Test 8) demonstrated no changes in parameters with age. In total, among the 12 age parameters, 6 parameters are related to decrease in vaginal tissue elasticity and 6 parameters are related to pelvic function - the weakened muscle contractive strength with age. Let’s consider the parity changes. Test 1 provides one parity-sensitive parameter (1) related to tissue elasticity; its average value changes by 49.6% (see panel E in Figure 3). This parameter is the maximum resistance force the VTI probe insertion. This maximum resistance comes from the perineal body which deteriorates after giving birth. No changes in pelvic support (Test 2) were found except for parameter 13, which increased with the parity (see panel F in Figure 3). This, at first sight, is an unexpected result and might be easily explained by significant softening of tissues between the vaginal wall and the pubic bone. As a result, these soft tissues demonstrate an increased pressure gradient to the bone due to their low resistance to displacement versus that of the bone. It means that parameter 13 changes with parity and relates to the tissue elasticity change rather than to pelvic support. Test 3 provides two identified parameters (23, 24) related to tissue elasticity at the side of vaginal walls and beyond 3–7 mm (small irregularities); their average values change by 70.1% and 52.5%. With regards to pelvic muscle contraction, Tests 5 and 6 provides four identified parameters (32, 37, 40, 41) related to pelvic function; their average values are changed by 55.0% - 105.5% (see parameter 37 change in Figure 3, panel G). These changes in pelvic muscle contractive strength must be related to avulsed pu- borectalis 15. Valsalva maneuver (Test 4), involuntary muscle relaxation (Test 7), and the reflex muscle contraction at cough (Test 8) demonstrated no changes with the parity. In total, among the 9 age parameters, 5 parameters are related to a decrease in vaginal tissue elasticity and 4 parameters are related to pelvic function - the weakened muscle contractive strength (avulsion) with the parity
It is important to note that the subject sample analysed in this study with normal pelvic conditions (no POP, no SUI) was composed of the visitors of urogynecological site; these patients may have had some pelvic floor conditions that were not identified in this study. Possibly, the patients from the normal group had pre-prolapse conditions which hadn’t yet transformed into anatomically visible POP This study reasonably proposes that if more subjects with no history of consulting urogynecological clinics would be added to this sample, more significant differences in the VTI parameters with regards to age and parity may be observed.
The next step (which falls beyond the purview of this article) with these biomechanical parameters may include (a) an insight into POP versus normal pelvic conditions, (b) an insight into POP classes (anterior versus posterior versus uterine), (c) analysis for continence versus incontinence conditions, (d) analysis of urogynecological surgical outcomes as a whole as well as per specific surgical procedure, (e) a combination of VTI data with urodynamics, ultrasound, and MRI data, (f) the usage of the VTI and other clinically related data for predicative modelling of outcomes for conservative and surgical procedures (personalized predictive treatment), and (g) maintenance of the objective history of biomechanical transformation of the patient pelvic floor. One of the strengths of this study is that the current VTI offers an opportunity to assess tissue elasticity, pelvic support structures, and pelvic function (muscle and ligaments) in high definition along the entire length of the anterior, posterior, and lateral walls at rest with applied deflection pressures and pelvic muscle contractions. All 52 parameters are calculated automatically in real-time. This allows a large body of measurements to evaluate individual variations in support defects as well as identify specific problematic structures. In addition, the technology provides the opportunity to measure pelvic floor muscle strength at specific locations along the vaginal wall and helps correlate its relative contributions to measured tissue properties. These measurements may provide insight into the functional contribution or relationship between support ligaments and the underlying muscle support. Because VTI testing is relatively easy and inexpensive to obtain, post-treatment follow-up is available to evaluate the surgical impact on functional tissue properties and pelvic floor muscles. This may provide valuable outcome measurements for evaluating current and future treatments.
One of the shortcomings of this study is its relatively small sample size. Further studies with larger patient populations, investigating varieties of other pelvic floor conditions and their use in the evaluation of interventions including physical therapy, conservative management options, and surgical correction are needed to further explore the diagnostic values of biomechanical mapping of the female pelvic floor.
CONCLUSIONS
The biomechanical mapping of the female pelvic floor with the VTI provides a unique set of parameters characterizing pelvic changes with age and parity. These objectively measurable biomechanical transformations of pelvic tissues, support structures and functions may be used in future research and practical applications.
Supplementary Material
Figure 2.-.
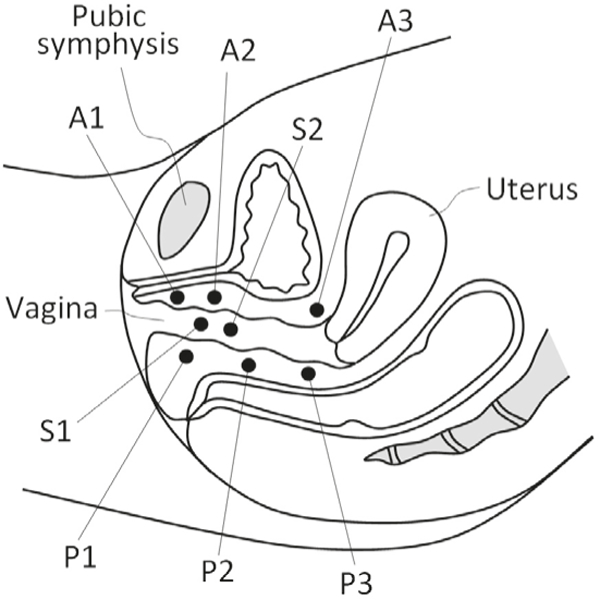
Locations of the VTI parameters within the pelvic floor. A1-A3 are in anterior compartment (Test 2), P1-P3 in posterior compartment (Test 2), and S1, S2 are in lateral compartments (left and right sides, Test 3). Figure 2 shows the locations of the measured VTI parameters for test 2 and 3 in mid-sagittal plane of the female pelvic floor.
ACKNOWLEDGEMENTS
Research reported in this publication was supported by the National Institute On Aging of the National Institutes of Health under Awards Number R44AG034714 and SB1AG034714. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
DISCLOSURE
V. Egorov: CEO and shareholder of Advanced Tactile Imaging, Inc.
H. van Raalte: shareholder of Advanced Tactile Imaging, Inc.
REFERENCES
- 1.Petros P The Female Pelvic Floor: Function, Dysfunction and Management According to the Integral Theory. 3rd ed. Berlin, Germany: Springer; 2010: 1–330. [Google Scholar]
- 2.Siddiqui NY, Gregory WT, Handa VL, DeLancey JOL, Richter HE, Moalli P, Barber MD, Pulliam S, Visco AG, Alperin M, Medina C, Fraser MO, Bradley CS. American Urogynecologic Society Prolapse Consensus Conference Summary Report. Female Pelvic Med Reconstr Surg. 2018. January 5 PMID: [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DeLancey JO. Pelvic floor anatomy and pathology In: Hoyte L, Damaser MS, editors. Biomechanics of the Female Pelvic Floor. 1st ed. London, UK: Elsevier; 2016: 13–51. [Google Scholar]
- 4.Egorov V, van Raalte H, Lucente V. Quantifying vaginal tis¬sue elasticity under normal and prolapse conditions by tactile imaging. International Urogynecology Journal 2012; 23(4): 459–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Egorov V, van Raalte H, Sarvazyan A. Vaginal Tactile Imaging. IEEE Transactions on Biomedical Engineering 2010; 57(7): 1736–1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Egorov V, van Raalte H, Lucente V, Sarvazyan A. Biomechanical characterization of the pelvic floor using tactile imaging In: Biomechanics of the Female Pelvic Floor, Eds. Hoyte L, Damaser MS, 1st Edition, Elsevier, 2016: 317–348. [Google Scholar]
- 7.van Raalte H, Lucente V, Ephrain S, Murphy M, Bhatia N, Sarvazyan N, Egorov V. Intra- and inter-observer reproducibility of vaginal tactile imaging. Female Pelvic Medicine & Reconstructive Surgery 2016; 22(5S): S130–131. [Google Scholar]
- 8.Lucente V, van Raalte H, Murphy M, Egorov V. Biomechanical paradigm and interpretation of female pelvic floor conditions before a treatment. International Journal of Women’s Health 2017; 9: 521–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Raalte H Egorov V Tactile imaging markers to characte¬rize female pelvic floor conditions. Open Journal of Obstetrics and Gynecology 2015; 5: 505–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Egorov V, Murphy M, Lucente V, van Raalte H, Ephrain S, Bhatia N, Sarvazyan N. Quantitative Assessment and Interpretation of Vaginal Conditions. Sexual Medicine 2018; 6(1): 39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Egorov V, Ayrapetyan S, Sarvazyan AP Prostate Mechanical Imaging: 3-D Image Composition and Feature Calculations. IEEE Transactions on Medical Imaging 2006; 25(10): 1329–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Egorov V, Sarvazyan AP. Mechanical imaging of the breast. IEEE Trans Med Imaging 2008; 27(9): 1275–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shobeiri SA. Practical Pelvic Floor Ultrasonography A Multicompartmental Approach to 2D/3D/4D Ultrasonography of the Pelvic Floor, 2nd Edition, Springer International Publishing AG, 2017: 1–368. [Google Scholar]
- 14.Dietz HP. Pelvic Floor Ultrasound. Atlas and Text Book Creative Commons Attribution License. Springwood, Australia; 2016: 1–127. [Google Scholar]
- 15.Hoyte L, Ye W, Brubaker L, Fielding JR, Lockhart ME, Heil¬brun ME, Brown MB, Warfield SK. Segmentations of MRI images of the female pelvic floor: a study of inter- and intra-reader reliability. J Magn Reson Imaging 2011; 33(3): 684–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bump RC, Mattiasson A, Bo K et al. (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. American Journal of Obstetrics and Gynecology, 175, 10–17. [DOI] [PubMed] [Google Scholar]
- 17.McGill R, Tukey JW, Larsen WA (1978) Variations of Box Plots. American Statistician 32:12–16. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


