Abstract
The goal of this work was to study the phenotypic susceptibility and resistance determinants of N. gonorrhoeae isolates to beta-lactam antimicrobials (benzylpenicillin and ceftriaxone). A total of 522 clinical isolates collected in Russia in 2015–2017 were analysed for susceptibility using the agar dilution method. DNA loci involved in antimicrobial resistance were identified using DNA microarray analysis and sequencing. Resistance to benzylpenicillin remained high, with 7.7% of isolates resistant (MICpen > 1 mg/L) and 47.5% of isolates showing intermediate susceptibility (MICpen = 0.12–1 mg/L). The most frequent resistance determinant (72.4% isolates) was the Asp345 insertion in penA, both as a single mutation and in combination with other mutations, particularly with the substitution Leu421Pro in ponA (39.0%). Mutations affecting the influx and efflux of drugs were also found, including amino acid substitutions in PorB (26.8% isolates) and delA in the promoter region of mtrR (22.8%). The accumulation of mutations in chromosomal genes (penA, pon, porA, and mtrR) led to a stepwise increase in MICpen to values characteristic of intermediate resistance. The presence of blaTEM plasmids was found in 25 isolates (4.8%), resulting in a strong increase in resistance to penicillin (MICpen > 16 mg/L) compared with the chromosomal mutations; 23 plasmids were of the African type with TEM-1 beta-lactamase, and two plasmids were of the Toronto/Rio type with TEM-135 beta-lactamase. Only three isolates were found with reduced susceptibility to ceftriaxone, with MICcef = 0.12–0.25 mg/L. Sequencing of penA did not reveal mutations associated with resistance to third-generation cephalosporins, and the gene structure was non-mosaic. The majority of isolates (21 of 25) carrying the blaTEM plasmid also contained the conjugative plasmid with tetM (resistance to tetracyclines), consistent with previously reported data that the presence of the conjugative plasmid facilitates the transfer of other plasmids associated with antimicrobial resistance.
Introduction
Gonorrhoea is a sexually transmitted infection caused by the gram-negative bacterium Neisseria gonorrhoeae. A distinctive feature of N. gonorrhoeae is its ability to rapidly accumulate different mutations to acquire resistance against the antibiotics used for its treatment [1,2]. The WHO has declared drug resistance in N. gonorrhoeae to be an emerging threat that has the potential to move gonorrhoea to the category of incurable infections [3].
Benzylpenicillin, a beta-lactam antibiotic, along with penicillins of subsequent generations, was used in the Russian Federation until the beginning of the 21st century. However, due to the development of a high resistance level in the population, it is no longer used for gonorrhoea treatment. At present, the antibiotics recommended for the treatment of gonorrhoea in Russia are ceftriaxone, a 3rd-generation cephalosporin, and spectinomycin. Unlike in European countries, azithromycin has never been recommended for gonorrhoea treatment in Russia, and cefixime has not yet been introduced into medical practice.
N. gonorrhoeae isolates that demonstrate resistance to 3rd-generation cephalosporins have recently appeared all over the world, including the H041 and F89 isolates, with MICcef ≥ 1 mg/L [4–8]. The susceptibility level of N. gonorrhoeae to beta-lactam antibiotics is under constant surveillance in the Russian Federation [9–11].
The molecular determinants associated with the resistance of N. gonorrhoeae to penicillins involve both chromosomal mutations and the presence of the blaTEM plasmid encoding beta-lactamases (penicillinases) [1,4,12]. The chromosomal determinants include mutations in penA that result in a decrease in the affinity of the penicillin-binding protein (PBP2), such as the insertion of an Asp codon between positions 345 and 346 (insAsp345); mutations in the C-terminal region of PBP2 have also been described [13,14]. PBP2 types are designated by Roman numerals from I to XXXVIII based on substitution profiles at 82 amino acid positions [15–17]. The recently developed NG-STAR program (https://ngstar.canada.ca) summarizes the currently known PBP2 types. NG-STAR classification uses the entire penA sequence and combines the historical nomenclature for penA types with novel nucleotide sequence designations. It currently includes 49 penA types, 21 historical and 28 novel amino acid profiles, and 80 penA alleles [18].
Mutations in ponA, which encodes penicillin-binding protein 1 (PBP1), e.g., the Leu421Por substitution, lead to a decrease in the rate of penicillin acylation [19]. Mutations causing an increase in the expression of the MtrCDE efflux pump also result in increased penicillin resistance; the main mutations are insertions of T and TT and deletion of A in the promoter region of mtrR. The Gly45Asp substitution in the coding region of mtrR is much less frequent [20,21]. Mutations in porB, which encodes the porin protein PorB1b, at residues Gly120 and Ala121 [22] in the presence of mutations in mtrR [19] result in a change in the permeability of the cell membrane and a decrease in the influx of antimicrobials into bacterial cells. The accumulation of mutations leading to an increase in the MICpen has also been described; N. gonorrhoeae isolates with increased MICpen values of up to 1.0 mg/L were obtained in the laboratory by the stepwise addition of mutations in penA, ponA, mtr, and porB [19].
Plasmid-mediated TEM beta-lactamases catalyse the hydrolysis of the cyclic amide bond of penicillin, resulting in degradation of the antibiotic. The family of N. gonorrhoeae blaTEM plasmids includes the following types: Asian (7426 bp), African (5599 bp), Toronto/Rio (5154 bp), Nimes (6798 bp), New Zealand (9309 bp), Johannesburg (4865 bp) and Australian (3269 bp) [23–26]. The Asian plasmid is considered to be a general ancestor from which plasmids of other types evolved by means of deletions and insertions [23, 25]. Five variants of plasmid beta-lactamases are known: TEM-1 (plasmids of all types), TEM-135 has the Met182Thr change in the amino acid sequence of the protein (usually typical of Toronto/Rio plasmids), TEM-220 contains the Met182Thr and Ala185Thr substitutions (Toronto/Rio plasmids), and enzymes with Glu110Lys and Gly228Ser substitutions occur among African plasmids [24, 26]. Although the described N. gonorrhoeae beta-lactamases cannot destroy third-generation cephalosporins, the emergence of extended-spectrum cephalosporin resistance in N. gonorrhoeae isolates is worrisome. TEM-135 beta-lactamase differs from TEM-1 by a single nucleotide (T→C in position 539, leading to the amino acid substitution Met182Thr). One additional specific SNP may lead to the Gly238Ser substitution, thus changing TEM-135 into the TEM-20 beta-lactamase, which is capable of destroying extended-spectrum cephalosporins [27,28].
The genetic determinant that is most often associated with N. gonorrhoeae resistance to cephalosporins is a mosaic structure of penA, which results from interspecies genetic recombination among N. gonorrhoeae, N. cinerea and N. perflava [16, 17]. Mosaic alleles can contain more than 70 amino acid changes compared with the wild-type protein that influence acylation by PBP2 [1]. Cephalosporin-resistant isolates with mosaic penA alleles often do not harbour the Asp345 insertion, which provides resistance to penicillins [16,29]. The Gly545Ser, Ile312Met, Val316Thr [30], Gly542Ser, Pro551Ser and Pro551Leu substitutions [31] in mosaic PBP2 genes have been suggested as mutations affecting cephalosporin resistance, but their role is not fully confirmed. Resistance to cephalosporins is also associated with non-mosaic alleles carrying substitutions of the Ala501 residue and mutations in mtrR and porB causing increased efflux and decreased influx of antimicrobials [5,20,22]. For example, two N. gonorrhoeae strains with high-level resistance to 3rd-generation cephalosporins that were isolated in Europe have a mosaic penA, type XXXIV, with an additional Ala501Pro substitution [32,33].
The goal of this work was to study the susceptibility of the current population (2015–2017) of N. gonorrhoeae isolates from the Russian Federation to beta-lactam antibiotics and to identify genetic determinants of resistance to these drugs, including investigation of the types of blaTEM plasmid genes and beta-lactamase variants.
Materials and methods
N. gonorrhoeae clinical isolates
According to the Ethics Committees of the State Research Center of Dermatovenerology and Cosmetology, this research does not require ethical approval. All specimens used in this study were anonymous samples that omitted personal information about the patients, particularly their name or address.
N. gonorrhoeae clinical isolates were collected by the State Research Center of Dermatovenerology and Cosmetology, Russian Ministry of Health, Moscow, within the framework of the Russian Gonococcal Antimicrobial Surveillance Programme (RU-GASP) [9,10]. The collection included 522 isolates obtained in 2015–2017 from 16 regions of the Russian Federation, with centres in Arkhangelsk, Astrakhan, Bryansk, Cheboksary, Chelyabinsk, Irkutsk, Kaluga, Kazan, Moscow, Novosibirsk, Omsk, Penza, Pskov, Ryazan, Stavropol, and Tomsk (S1 Table).
The samples were obtained from clinical specimens (urethral specimens from men and cervical/urethral specimens from women) of patients with diagnosed primary symptomatic uncomplicated gonorrhoea who attended specialized dermatovenereological clinics. The patients had not used antibiotics for the treatment of gonorrhoea or other diseases during the last 12 months.
Primary N. gonorrhoeae identification was performed in regional clinics using Gram staining and the rapid oxidase reaction. Gram-negative and oxidase-positive culture samples were frozen in cryomedium-Trypticase soy broth containing 20% glycerol (Becton, Dickinson BBL, Sparks, MD, USA) and transported on dry ice to the State Research Center of Dermatovenerology and Cosmetology, Moscow. The cultures were then plated on GC-agar enriched with 1% IsoVitaleX and 1% VCAT selective supplement (Becton Dickinson, USA) and verified by tests for biochemical activities with NH ID cards on a VITEK 2 Compact Analyser (bioMérieux, France). For the cultures identified as N. gonorrhoeae with a probability of less than 95%, mass spectrometric studies were carried out using a MALDI Microflex (Bruker Daltonics GmbH, Germany).
The cultures were preserved in Trypticase soy broth with 20% glycerol at –70°C. Isolation of DNA from N. gonorrhoeae pure cultures was carried out using express kits for DNA isolation (Lytekh, Moscow, Russia). DNA was stored at –20°C.
N. gonorrhoeae antimicrobial susceptibility testing
Benzylpenicillin and ceftriaxone susceptibility testing of N. gonorrhoeae isolates and determination of MIC were carried out using the agar dilution method on GC-agar enriched with 1% IsoVitaleX. The obtained MIC values were compared with breakpoints from The European Committee on Antimicrobial Susceptibility Testing (EUCAST) [34].
Isolates tested for susceptibility to benzylpenicillin were categorized as S (susceptible, MICpen ≤ 0.06 mg/L), I (intermediate, 0.12 < MICpen ≤ 1 mg/L), and R (resistant, MICpen > 1 mg/L).
For ceftriaxone, according to the EUCAST criteria, isolates with MICcef ≤ 0.125 mg/L were considered susceptible, and isolates with MICcef > 0.125 mg/L were considered resistant.
For comparison, the US Clinical and Laboratory Standards Institute (CLSI) criteria [35] were also used. The CLSI criteria are less strict: N. gonorrhoeae isolates are considered penicillin resistant if MICpen ≥ 2 mg/L; for ceftriaxone, susceptible strains are strains with MICcef ≤ 0.25 mg/L.
All N. gonorrhoeae isolates were tested for the presence of beta-lactamases by a nitrocefin test using nitrocefin discs (Cefinase, bioMérieux).
Genetic analysis of N. gonorrhoeae
Identification of genetic determinants of antimicrobial resistance
The detection of genetic determinants of N. gonorrhoeae resistance to antimicrobials was carried out using a hydrogel low-density oligonucleotide microarray. The microarray was previously developed for the identification of causative agents of human reproductive tract infections, including N. gonorrhoeae, and for the simultaneous detection of genetic markers of resistance to different antimicrobial drugs [36]. The microarray consisted of elements with immobilized oligonucleotides for the detection of different mutations and other determinants associated with resistance to beta-lactams: mutations in penA resulting in the insertion of Asp in the 345 position in PBP2 (insAsp345), mutations in ponA resulting in the amino acid substitution Leu421Pro in PBP1, the blaTEM plasmid and Met182Thr and Gly238Ser substitutions in the gene encoding beta-lactamase, mutations in porB leading to the amino acid changes Gly120Lys/Asp/Asn/Thr and Ala121/Asp/Asn/Gly/Ser in the porin protein, and deletion A (delA) and insertions T and TT (insT and insTT) in the promoter region of mtrR.
The microarray also allowed the simultaneous identification of mutations associated with resistance to other antimicrobials [1,12,36]: fluoroquinolones (mutations in gyrA and parC), tetracyclines (mutations in the 16S rRNA and rpsJ, plasmid tetM), macrolides (mutations in the 23S rRNA and mefA), and spectinomycin (mutations in the 16S rRNA). All the results obtained with the microarray are presented in S1 Table, although only the genetic determinants of resistance to beta-lactam antibiotics are discussed in this paper.
For isolates with reduced susceptibility to ceftriaxone, the sequence of penA was determined using a 3730xl Genetic Analyzer (Applied Biosystems, USA).
Sequencing of porB and tbp for N. gonorrhoeae multiantigen sequence typing (NG-MAST) was performed according to a conventional protocol [37] using a 3730xl Genetic Analyzer.
Determination of blaTEM plasmid types and beta-lactamase variants
The type of blaTEM plasmid was determined by multiplex PCR followed by electrophoresis in a 1% agarose gel. PCR was carried out with the primers previously described by Palmer et al. [38]: BL1, 5′-TACTCAATCGGTAATTGGCT-3′; BL2, 5′-CACCTATAAATCTCGCAAG C-3′; BL3, 5′-CCATAGTGTTGAGTATTGCGAA-3′; BL4, 5′-TCATTCGTGCGTTCTAGGA-3′. The PCR product sizes were BL2 + BL3 = 958 bp (Asian plasmid), BL1 + BL3 = 1191 bp (African plasmid), and BL2 + BL4 = 650 bp (Toronto/Rio plasmid).
The presence of mutations in the beta-lactamase gene of N. gonorrhoeae that result in Met182Thr, Ala185Thr, and Gly238Ser substitutions was checked by sequencing with the primers 6617GGCACTGGTGCAACGGAAAT6636 and 446GGTCTGACGCTCAGTGGAAC465, GenBank ID NC_002098.1.
Statistical analysis
The significance of the differences between groups was assessed using a non-parametric Kruskal-Wallis test (significance level α < 0.05) in IBM SPSS Statistics V23 software. Then, multiple pairwise comparisons of groups (with the control group) were carried out using Dunn’s Q criterion. Dunn’s criteria were calculated, and p values were determined using previously defined critical values [39]. The critical value for the Q criterion was 3.90 for the number of groups under study.
Phylogenetic analysis of nucleotide sequences
The Bayesian information criterion was used for the selection of the nucleotide substitution models in MEGA7 software [40]. For the NG-MAST gene locus, the evolutionary history was inferred using the maximum likelihood method based on the Hasegawa-Kishino-Yano model [41] with invariant sites. The initial tree(s) for the heuristic search were obtained automatically by applying the neighbour-joining and BIONJ algorithms to a matrix of pairwise distances estimated using the maximum composite likelihood approach and then selecting the topology with the superior log likelihood value. The tree was drawn to scale with branch lengths measured in number of substitutions per site.
Results
Penicillin resistance in N. gonorrhoeae isolates
The analysis of phenotypic characteristics in the recent (2015–2017) population of gonococcal infections in Russia revealed 40 isolates (7.7%) resistant to benzylpenicillin (with MICpen > 1 mg/L), 248 isolates (47.5%) with intermediate susceptibility (MICpen 0.12–1 mg/L) and 234 (44.8%) susceptible isolates. Microarray hybridization and sequencing revealed 396 isolates that bore different determinants associated with resistance to penicillins, including 25 isolates carrying the blaTEM plasmid (Table 1). The isolate characteristics of the obtained dataset (522 samples), including susceptibility (MIC values), mutations revealed using microarrays and results of NG-MAST typing, are summarized in S1 Table (in addition to penicillins, the microarray results include detection of resistance determinants to fluoroquinolones, tetracyclines, azithromycin, and spectinomycin). Isolates carrying chromosomal mutations demonstrated mostly intermediate susceptibility to benzylpenicillin, whereas isolates with the blaTEM plasmid had high levels of resistance (Table 1), confirming the previously described correlation between the presence of plasmid beta-lactamases and a high level of penicillin resistance in N. gonorrhoeae [26,42].
Table 1. Genetic determinants and susceptibility of N. gonorrhoeae isolates to benzylpenicillin.
Mutations: penA–ins345Asp, ponA–Leu421Pro, mtrR (promoter region)–-35delA, porB–Gly120Lys/Asp/Asn/Thr and/or Ala121/Asp/Asn/Gly/Ser.
| № | Mutations in genes | MICpen (mg/L) / number of isolates with the corresponding MICpen | Median MICpen (mg/L) |
Number of susceptible (S), intermediate (I) and resistant (R) isolates | Comparison with the wild-type isolatec | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0.015 | 0.03 | 0.06 | 0.12 | 0.25 | 0.5 | 1 | 2 | 8 | 16 | ≥ 32 | S (≤ 0.06) | I (0.12–1) |
R (> 1) | Total | Dunn’s criterion Q | p value | |||
| 1 | No mutationsa | 85 | 13 | 11 | 11 | 4 | 2 | – | – | – | – | – | 0.015 | 109 | 17 | – | 126 | – | – |
| 2 | penA | 20 | 17 | 40 | 34 | 14 | 4 | 1 | 1 | – | – | – | 0.06 | 77 | 53 | 1 | 131 | 5.45 | < 0.001 |
| 3 | ponA | – | – | 1 | – | 2 | – | – | – | – | – | – | 0.25 | 1 | 2 | – | 3 | 2.08 | > 0.5 |
| 4 | mtrR | – | 1 | – | – | 1 | – | – | – | – | – | – | 0.14 | 1 | 1 | – | 2 | 1.21 | > 0.5 |
| 5 | porB | 2 | – | 1 | – | – | 2 | – | – | – | – | – | 0.06 | 3 | 2 | – | 5 | 1.69 | > 0.5 |
| 6 | penA and mtrR | 2 | 2 | 1 | 1 | 1 | – | – | 1 | – | – | – | 0.045 | 5 | 2 | 1 | 8 | 1.83 | > 0.5 |
| 7 | ponA and mtrR | 1 | – | – | – | 1 | – | 1 | – | – | – | – | 0.25 | 1 | 2 | – | 3 | 2.01 | > 0.5 |
| 8 | penA and ponA | 3 | 4 | 11 | 13 | 14 | 6 | 1 | 1 | – | – | – | 0.12 | 18 | 34 | 1 | 53 | 6.69 | < 0.001 |
| 9 | penA and porB | 1 | – | 3 | 3 | 6 | 6 | 2 | – | – | – | – | 0.25 | 4 | 17 | – | 21 | 6.15 | < 0.001 |
| 10 | penA, ponA, and mtrR | 2 | 4 | – | 3 | 7 | 13 | 9 | – | – | – | – | 0.5 | 6 | 32 | – | 38 | 8.69 | < 0.001 |
| 11 | penA, ponA, and porB | – | 1 | 4 | 2 | 14 | 7 | 9 | 3 | – | – | – | 0.25 | 5 | 32 | 3 | 40 | 9.48 | < 0.001 |
| 12 | ponA, mtrR, and porB | – | – | – | – | – | – | 2 | 1 | – | – | – | 1 | – | 2 | 1 | 3 | 4.12 | < 0.001 |
| 13 | penA, mtrR, and porB | 2 | – | – | 1 | 3 | 3 | 1 | 1 | – | – | – | 0.25 | 2 | 8 | 1 | 11 | 4.58 | < 0.001 |
| 14 | penA, ponA, mtrR, and porB | – | – | 2 | 4 | 5 | 22 | 13 | 7 | – | – | – | 0.5 | 2 | 44 | 7 | 53 | 12.13 | < 0.001 |
| 15 | Presence of blaTEMb | 1 | 8 | 16 | ≥ 32 | – | – | 25 | 25 | 12.17 | < 0.001 | ||||||||
| Total number of isolates | 234 | 248 | 40 | 522 | |||||||||||||||
a No mutations in chromosomal genes and no blaTEM plasmids were found.
b Mutations in chromosomal genes are not indicated here for isolates with blaTEM.
Mutations in penA and ponA were predominant among the determinants that affected resistance. The most frequent mutation in the samples was the insertion of aspartic acid at codon 345 of penA, both as a single mutation and in combination with other changes. The ins345Asp mutation was observed in 378 of 522 isolates (72.4%). A single ins345Asp mutation did not result in the appearance of benzylpenicillin-resistant isolates, but a statistically significant increase in the median MICpen to 0.06 mg/L was observed. The Leu421Pro substitution in ponA was found in 204 isolates (39.0%). This mutation had a more pronounced effect on benzylpenicillin resistance, resulting in the formation of intermediately susceptible isolates with a median MICpen of 0.25 mg/L (Table 1).
The deletion of adenine (delA) in the promoter region of mtrR was identified in 119 N. gonorrhoeae isolates (22.8%), whereas the insertions described in the literature of thymidine (T) or TT at the -10 position of mtrR were not found.
Mutations in porB were revealed in 140 isolates (26.8%). Substitutions in PorB in the presence of simultaneous mutations in mtrR led to an increase in the median MICpen to 0.25–0.5 mg/L (isolates with intermediate susceptibility). However, there was no statistically relevant difference in resistance level depending on the type of amino acid change at residues 120 and 121 (data not shown).
As a rule, compared with single mutations, the accumulation of several mutations resulted in an increase in the resistance of N. gonorrhoeae isolates: statistically significant differences in median MICpen values were obtained (Table 1). Hence, the median MICpen for the isolates with mutations in two genes increased to 0.25 mg/L, and the simultaneous presence of mutations in four genes (53 samples) led to an increase in the median MICpen to 0.5 mg/L. Table 1 shows Dunn’s Q criterion for the comparison of groups of isolates carrying mutations with the group of wild-type isolates (groups 2–15 compared to group 1). Some scores were found to be statistically non-significant due to the small numbers of samples in groups.
To determine whether the differences in the median MICpen for the sample groups with chromosomal mutations (groups 2–14 in Table 1) were statistically significant, additional pairwise comparisons of groups were carried out. High values of the Q criterion were obtained for group 2 (single mutation in penA) compared with group 10 (mutations in penA, ponA, and mtrR), group 2 compared with group 11 (mutations in penA, ponA, and porB), group 2 compared with group 14 (mutations in penA, ponA, mtrR, and porB), and group 8 (mutations in penA and ponA) compared with group 14 (mutations in penA, ponA, mtrR, and porB). These results indicate that the accumulation of mutations, i.e., mutations in 3 or 4 genes compared with mutations in 1 or 2 genes, led to statistically significant increases in MICpen.
The presence of the blaTEM plasmid was detected in 25 (4.8%) N. gonorrhoeae isolates. All isolates with the blaTEM plasmid demonstrated resistance to benzylpenicillin with MICpen > 8 mg/L; 24 isolates had a MICpen ≥ 16 mg/L (Tables 1 and 2), regardless of mutations in chromosomal genes.
Table 2. Characterization of N. gonorrhoeae isolates carrying blaTEM plasmids.
| Region | NG-MAST type | MICpen, mg/L | Type of blaTEM plasmid | Beta-lactamase variant | Presence of tetM plasmid | MICtet, mg/L |
|---|---|---|---|---|---|---|
| Arkhangelsk (2 isolates) | 14604 | 16 | African | TEM-1 | tetM | 32 |
| Arkhangelsk | 12096 | 16 | African | TEM-1 | tetM | 32 |
| Astrakhan | 14596 | 16 | African | TEM-1 | tetM | 32 |
| Bryansk (7 isolates) |
14826 | ≥ 32 | African | TEM-1 | tetM | 16 |
| Chuvashiya | 10158 | ≥ 32 | Toronto/Rio | TEM-135 | tetM | 8 |
| Kaluga (3 isolates) |
15644 | ≥ 32 | African | TEM-1 | tetM | 64 |
| Kaluga | 15644 | ≥ 32 | African | TEM-1 | – | 1 |
| Kaluga | 16173 | ≥ 32 | Toronto/Rio | TEM-135 | – | 1 |
| Kaluga | 12096 | 16 | African | TEM-1 | tetM | 32 |
| Moscow | 3109 | ≥ 32 | African | TEM-1 | – | 0.5 |
| Moscow | 7848 | 16 | African | TEM-1 | tetM | 32 |
| Moscow | 3109 | 8 | African | TEM-1 | – | 0.25 |
| Novosibirsk | 15748 | ≥ 32 | African | TEM-1 | tetM | 64 |
| Omsk | 14826 | ≥ 32 | African | TEM-1 | tetM | 8 |
| Ryazan | 13336 | 16 | African | TEM-1 | tetM | 32 |
| Ryazan | 14015 | 16 | African | TEM-1 | tetM | 32 |
The type of blaTEM plasmid and the variant of beta-lactamase were identified for the first time in the samples collected in the Russian Federation. The majority (23 of 25) of blaTEM plasmids were of the African type, the most widespread type in the world. Two plasmids were of the Toronto/Rio type. Interestingly, the penicillinase-producing strains in neighbouring Poland contained both the African and Toronto/Rio plasmids (50/50) [26].
The African-type plasmids contained a TEM-1 beta-lactamase gene with a Met residue at position 182, and both Toronto/Rio plasmids carried a TEM-135 beta-lactamase gene with a Met182Thr substitution that was in accordance with previously described data [24,26]. Mutations that can result in the emergence of beta-lactamase activity towards cephalosporins were not found in the analysed N. gonorrhoeae isolates.
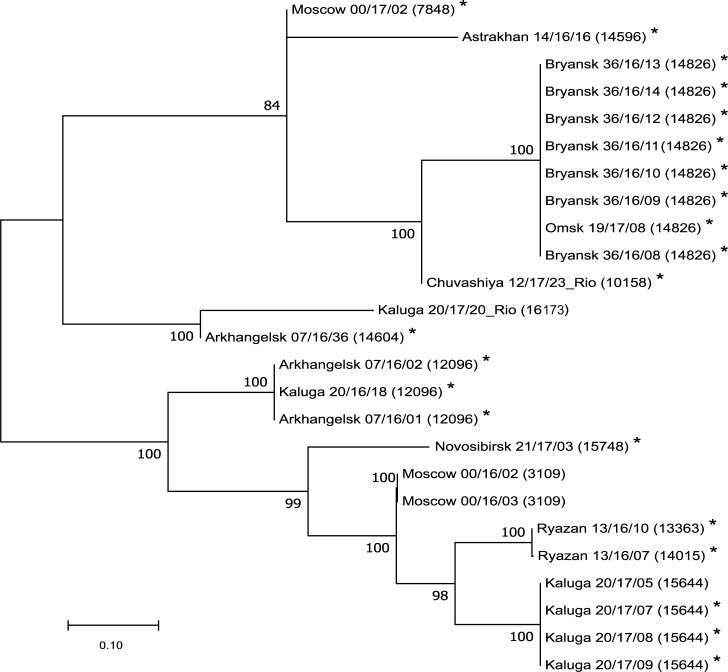
For the N. gonorrhoeae isolates carrying blaTEM plasmids, a maximum likelihood phylogenetic tree was constructed for the loci used for NG-MAST typing (Fig 1). According to the phylogenetic results, the isolates with blaTEM plasmids can be divided into three clusters. The isolates with Toronto/Rio plasmids were located in different clusters. Isolates from nearby regions were often closer to each other than isolates from distant regions, with some exceptions (Arkhangelsk, Kaluga, and Moscow). These results indicate that several parallel processes can be observed: horizontal gene transfer, vertical gene transfer, and migration of people with N. gonorrhoeae.
Fig 1. Phylogenetic tree constructed with the NG-MAST gene loci of N. gonorrhoeae isolates collected in the Russian Federation in 2015–2017 and carrying blaTEM plasmids.
Bootstrap values are shown next to the branches. The origin of each isolate and its sample code are indicated. Isolates harbouring blaTEM (resistance to penicillins) and tetM (resistance to tetracycline) plasmids simultaneously are marked with asterisks.
Simultaneous presence of plasmids associated with resistance to benzylpenicillin and tetracycline
Twenty-two of the 25 N. gonorrhоeae isolates harboured the blaTEM plasmid, and the plasmid with tetM was responsible for high resistance to tetracyclines (MICtet > 8 mg/L) [43] (Table 2). The tetM in N. gonorrhoeae is located on a large (~25 MDa) conjugative plasmid and, as previously shown [44–47], the backbone of this plasmid mobilizes the transfer of the small gonococcal beta-lactamase plasmids (3–6 MDa depending on the plasmid type) to other N. gonorrhoeae strains and other Neisseria species, i.e., it may facilitate the transfer of other plasmids carrying other drug resistance markers into the cell. Because tetracycline was previously actively used for the treatment of gonorrhoea throughout the world, the level of resistance to this drug remains very high. In Russia, 29% of N. gonorrhoeae isolates were tetracycline resistant in 2015–2017, and one-quarter of these isolates contained the plasmid with tetM [43]. As the presence of the tetM plasmid facilitates the acquisition of other plasmids by the cell, there is a danger of the appearance of multiresistant N. gonorrhoeae species with high plasmid-mediated resistance.
Ceftriaxone resistance in N. gonorrhoeae isolates
Only three isolates with decreased susceptibility to ceftriaxone were found in the studied samples collected in Russia in 2015–2017. One isolate showed MICcef = 0.25 mg/L; this isolate is considered resistant according to the EUCAST criteria but susceptible according to the CLSI criteria. Another two isolates had MICcef = 0.125 mg/L, and the other 519 isolates had MICcef values in the range of 0.001–0.06 mg/L. Detailed characteristics of the N. gonorrhoeae isolates with MICcef ≥ 0.125 mg/L are presented in Table 3. The distributions of the ceftriaxone MICs and detected genetic determinants in N. gonorrhoeae isolates are shown in S2 Table.
Table 3. Characterization of the N. gonorrhoeae isolates with the highest ceftriaxone MICs.
| №* | Region (year) |
Sample code | NG-MAST type | MICcef, mg/L | MICpen, mg/L | Chromosomal genetic determinants | blaTEM plasmid | Type of PBP2 encoded by penA | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| penA | ponA | porB | mtrR | ||||||||
| 1 (135) |
Arkhangelsk (2015) | 07/15/49 | 9480 | 0.25 (R) | 0.25 (I) | insAsp345 | no mutations | Gly120Asp | no mutations | – | I |
| 2 (78) |
Arkhangelsk (2016) | 07/16/42 | 9486 | 0.125 | 1 (I) | insAsp345 | no mutations | no mutations | no mutations | – | I |
| 3 (306) |
Kaluga (2017) |
20/17/05 | 15644 | 0.125 | ≥ 32 (R) | insAsp345 | Leu421Pro | no mutations | no mutations | blaTEM-1 | XVI |
* The isolate number in S1 Table is indicated in brackets.
All these isolates carried the Asp insertion in the 345 position of penA. Additional sequencing of penA revealed a non-mosaic structure for all three isolates. The protein sequences encoded by penA in these samples were homologous and belonged to types I and XVI; the amino acid changes that are present in cephalosporin-resistant isolates were not typical of these structure types [16,17]. The chromosomal mutations identified in these isolates were associated with resistance or intermediate resistance to benzylpenicillin; however, they cannot explain the mechanism of ceftriaxone MIC elevation for these isolates.
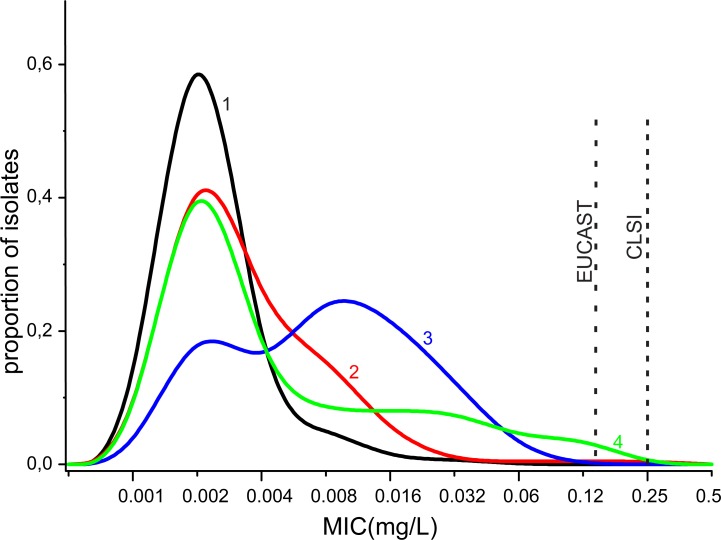
The distribution of mutations in the whole pool of isolates (Fig 2, S2 Table) indicated that mutations in a single gene or simultaneous mutations in two genes (penA, ponA, mtrR (promoter region), and porB) did not result in a change in the median MICcef in comparison with the wild-type isolates (MICcef = 0.002–0.003 mg/L). A statistically significant increase in MICcef to 0.004–0.008 mg/L was observed in the presence of three simultaneous mutations in penA, ponA, and mtrR or penA, ponA, and porB. The occurrence of mutations in four chromosomal genes led to an increase in MICcef to 0.015 mg/L (Fig 2). The accumulation of mutations also resulted in an increase in MICcef, but this increase did not reach the MIC level of ceftriaxone-resistant isolates.
Fig 2. Ceftriaxone MIC distributions of N. gonorrhoeae isolates with different genetic determinant profiles.
Wild-type isolates (1), isolates with mutations in one or two chromosomal genes (2), isolates with mutations in three or four chromosomal genes (3), and isolates carrying blaTEM plasmids (4) are shown.
Thus, a number of isolates with decreased susceptibility to ceftriaxone were found among recent N. gonorrhoeae isolates in Russia, and the analysis did not reveal mutations associated with resistance to third-generation cephalosporins.
Discussion
In this work, the phenotypic susceptibility and genetic determinants of resistance to benzylpenicillin and ceftriaxone were analysed in N. gonorrhoeae clinical isolates collected in Russia in 2015–2017. The low-density oligonucleotide microarray [36] used in this work proved to be a useful and convenient tool for the rapid screening of drug resistance determinants. The limitation of this assay was the restricted number of identified genetic markers relevant to antibiotic resistance. Hence, the microarray did not allow detection of mosaic penA alleles and mutations in mosaic alleles due to the large number of alterations (more than 70 mutations are known to date) and the presence of several SNPs in non-mosaic penA alleles. Therefore, penA was additionally analysed by sequencing.
The recent results of N. gonorrhoeae surveillance in Russia within the framework of the RU-GASP Programme [48] indicated decreasing trends in resistance to the antibiotics previously used for gonorrhoea treatment (benzylpenicillin, tetracycline, and ciprofloxacin). However, the level of resistance to these antibiotics remains high, excluding the possibility of reviving their therapeutic use for gonococcal infection. Isolates with slightly decreased susceptibility to ceftriaxone appeared only sporadically [48]. Among the clinical isolates collected in 2015–2017 in Russia and analysed in this work, 7.7% were resistant to benzylpenicillin, and 47.5% showed intermediate resistance. The accumulation of mutations in chromosomal genes (penA, pon, porA, and mtrR) led to a stepwise increase in penicillin MIC to values characteristic of intermediate resistance (up to 0.5 mg/L).
An additional limitation for penicillin usage is the presence of a blaTEM plasmid that is potentially capable of rapid horizontal transfer in the case of selective pressure related to this antibiotic. Notably, the ratio of plasmid penicillinase-producing N. gonorrhoeae isolates in Russia was 4.8%, which is lower than the average ratio of 14.9% reported for Euro-GASP countries [49].
The study of susceptibility to another beta-lactam antibiotic, ceftriaxone, showed a high indication of susceptibility in the Russian isolates collected in 2015–2017, which is a good reason to maintain the recommendation to use ceftriaxone as a first-line drug for gonorrhoea therapy. It should be noted that the Euro-GASP report indicated stable overall resistance levels to third-generation cephalosporins, both cefixime and ceftriaxone, in European countries at the present time [49]. Only one isolate with MICcef = 0.25 mg/L, which is considered resistant according to the EUCAST criteria, was found among the samples collected in Russia in 2015–2017. Two isolates had MICcef at the resistance breakpoint (0.125 mg/L). The analysis of chromosomal determinants indicated their roles in the shift of MICcef towards increased values, especially with the simultaneous presence of mutations in the target genes (penA and ponA) and the drug delivery (porB) and efflux (mtrR) systems. Additional analysis of samples with maximum MICcef values, including sequencing of penA, did not reveal the mutations associated with resistance to third-generation cephalosporins and showed a non-mosaic structure of penA. It is worth noting that five N. gonorrhoeae samples with a non-mosaic penA allele and decreased susceptibility to extended-spectrum cephalosporins (MICcef = 0.5 mg/L) were found among isolates collected in the USA; it was proposed that the observed phenotype might have resulted from the combined effects of mutations in multiple genes [50].
One of the interesting facts observed in this work was the simultaneous presence of the blaTEM and tetM plasmids associated with high resistance to penicillins and tetracyclines in N. gonorrhoeae isolates. Previous studies [45–47] have shown that the conjugative tetM plasmid in N. gonorrhoeae facilitates the acquisition of other plasmids by the cell. This manner of developing drug resistance should not be underestimated. Thus, analysis of drug resistance determinants in N. gonorrhoeae calls for special attention to isolates resistant to tetracyclines and carrying tetM plasmids, because the presence of this genetic element simplifies the transfer of blaTEM plasmids with penicillin resistance markers and other plasmids containing genes associated with resistance to other antimicrobial drugs.
Supporting information
ST–NG-MAST sequence type, Pen–penicillin, Tet–tetracycline, Cef–ceftriaxone, Cip–ciprofloxacin, Spec–spectinomycin, Azit–azithromycin.
(XLSX)
Mutations: penA–ins345Asp, ponA–Leu421Pro, mtrR (promoter region)–-35delA, porB–Gly120Lys/Asp/Asn/Thr and/or Ala121/Asp/Asn/Gly/Ser.
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the Russian Science Foundation Grant No. 17-75-20039 (Boris Shaskolskiy, Ekaterina Dementieva, Ilya Kandinov, Marina Filippova, Dmitry Gryadunov) and the Ministry of Health of the Russian Federation, Project No. 056-00015-18-00 (Alexey Kubanov). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Unemo M, Shafer WM. Antimicrobial resistance in Neisseria gonorrhoeae in the 21st century: past, evolution, and future. Clin. Microbiol. Rev. 2014; 27(3): 587–613. 10.1128/CMR.00010-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suay-García B, Pérez-Gracia MT. Drug-resistant Neisseria gonorrhoeae: latest developments. Eur. J. Clin. Microbiol. Infect. Dis. 2017; 36(7): 1065–71. 10.1007/s10096-017-2931-x [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Antimicrobial resistance: global report on surveillance Geneva: WHO Press; 2014. [Google Scholar]
- 4.Unemo M. Current and future antimicrobial treatment of gonorrhoea–the rapidly evolving Neisseria gonorrhoeae continues to challenge. BMC Infect. Dis. 2015; 15: 364 10.1186/s12879-015-1029-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Unemo M, Nicholas RA. Emergence of multidrug-resistant, extensively drug-resistant and untreatable gonorrhea. Future Microbiol. 2012; 7: 1401–22. 10.2217/fmb.12.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chisholm SA, Unemo M, Quaye N, Johansson E, Cole MJ, Ison CA, van de Laar MJ. Molecular epidemiological typing within the European Gonococcal Antimicrobial Resistance Surveillance Programme reveals predominance of a multidrug-resistant clone. Euro Surveill. 2013; 18(3). pii: 20358. . [PubMed] [Google Scholar]
- 7.Martin I, Sawatzky P, Allen V, Hoang L, Lefebvre B, Mina N., et al. Emergence and characterization of Neisseria gonorrhoeae isolates with decreased susceptibilities to ceftriaxone and cefixime in Canada: 2001–2010. Sex. Transm. Dis. 2012; 39(4): 316–23. 10.1097/OLQ.0b013e3182401b69 [DOI] [PubMed] [Google Scholar]
- 8.Shimuta K, Watanabe Y, Nakayama S, Morita-Ishihara T, Kuroki T, Unemo M, Ohnishi M. Emergence and evolution of internationally disseminated cephalosporin-resistant Neisseria gonorrhoeae clones from 1995 to 2005 in Japan. BMC Infect. Dis. 2015; 15: 378 10.1186/s12879-015-1110-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kubanova A, Frigo N, Kubanov A, Sidorenko S, Lesnaya I, Polevshikova S, et al. The Russian gonococcal antimicrobial susceptibility programme (RU-GASP)–national resistance prevalence in 2007 and 2008, and trends during 2005–2008. Euro. Surveill. 2010; 15(14): pii 19533. . [PubMed] [Google Scholar]
- 10.Kubanova A, Kubanov A, Frigo N, Solomka V, Semina V, Vorobyev D, et al. Russian gonococcal antimicrobial susceptibility programme (RU-GASP)–resistance in Neisseria gonorrhoeae during 2009–2012 and NG-MAST genotypes in 2011 and 2012. BMC Infect. Dis. 2014; 14: 342 10.1186/1471-2334-14-342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kubanov A, Vorobyev D, Chestkov A, Leinsoo A, Shaskolskiy B, Dementieva E., et al. Molecular epidemiology of drug-resistant Neisseria gonorrhoeae in Russia (current status, 2015). BMC Infect. Dis. 2016; 16: 389 10.1186/s12879-016-1688-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shaskolskiy B, Dementieva E, Leinsoo A, Runina A, Vorobyev D, Plakhova X, et al. Drug resistance mechanisms in bacteria causing sexually transmitted diseases and associated with vaginosis. Front. Microbol. 2016; 7: 747 10.3389/fmicb.2016.00747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dowson CG, Jephcott AE, Gough KR, Spratt BG. Penicillin binding protein 2 genes of non-beta-lactamase-producing, penicillin resistant strains of Neisseria gonorrhoeae. Mol. Microbiol. 1989; 3: 35–41. 10.1111/j.1365-2958.1989.tb00101.x [DOI] [PubMed] [Google Scholar]
- 14.Brannigan JA, Tirodimos IA, Zhang QY, Dowson CG, Spratt BG. Insertion of an extra amino acid is the main cause of the low affinity of penicillin-binding protein 2 in penicillin-resistant strains of Neisseria gonorrhoeae. Mol. Microbiol. 1990; 4: 913–19. 10.1111/j1365-2958.1990.tb00664.x [DOI] [PubMed] [Google Scholar]
- 15.Whiley DM, Limnios EA, Ray S, Sloots TP, Tapsall JW. Diversity of penA alterations and subtypes in Neisseria gonorrhoeae strains from Sydney, Australia, that are less susceptible to ceftriaxone. Antimicrob. Agents Chemother. 2007; 51: 3111–16. 10.1128/AAC.00306-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ohnishi M, Golparian D, Shimuta K, Saika T, Hoshina S, Iwasaku K, et al. Is Neisseria gonorrhoeae initiating a future era of untreatable gonorrhea? Detailed characterization of the first strain with high-level resistance to ceftriaxone. Antimicrob. Agents Chemother. 2011; 55: 3538–45. 10.1128/AAC.00325-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zapun A, Morlot C, Taha M. Resistance to beta-lactams in Neisseria ssp. due to chromosomally encoded penicillin-binding proteins. Antibiotics. 2016; 5(4): pii: E35 10.3390/antibiotics5040035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Demczuk W, Sidhu S, Unemo M, Whiley DM, Allen VG, Dillon JR, et al. Neisseria gonorrhoeae sequence typing for antimicrobial resistance, a novel antimicrobial resistance multilocus typing scheme for tracking global dissemination of N. gonorrhoeae strains. J. Clin. Microbiol. 2017; 55(5):1454–68. 10.1128/JCM.00100-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ropp PA, Hu M, Olesky M, Nicholas RA. Mutations in ponA, the gene encoding penicillin-binding protein 1, and a novel locus, penC, are required for high-level chromosomally mediated penicillin resistance in Neisseria gonorrhoeae. Antimicrob. Agents Chemother. 2002; 46: 769–77. 10.1128/AAC.46.3.769-777.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao S, Duncan M, Tomberg J, Davies C, Unemo M, Nicholas RA. Genetics of chromosomally mediated intermediate resistance to ceftriaxone and cefixime in Neisseria gonorrhoeae. Antimicrob. Agents Chemother. 2009; 53: 3744–51. 10.1128/AAC.00304-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Folster JP, Johnson PJ, Jackson L, Dhulipali V, Dyer DW, Shafer WM. MtrR modulates rpoH expression and levels of antimicrobial resistance in Neisseria gonorrhoeae. J. Bacteriol. 2009; 191: 287–97. 10.1128/JB.01165-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olesky M, Zhao S, Rosenberg RL, Nicholas RA Porin-mediated antibiotic resistance in Neisseria gonorrhoeae: ion, solute, and antibiotic permeation through PIB proteins with penB mutations. J. Bacteriol. 2006; 188(7): 2300–308. 10.1128/JB.188.7.2300-2308.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pagotto F, Aman AT, Ng LK, Yeung KH, Brett M, Dillon JA. Sequence analysis of the family of penicillinase-producing plasmids of Neisseria gonorrhoeae. Plasmid. 2000; 43(1): 24–34. 10.1006/plas.1999.1431 [DOI] [PubMed] [Google Scholar]
- 24.Muhammad I, Golparian D, Dillon JA, Johansson A, Ohnishi M, Sethi S, et al. Characterisation of blaTEM genes and types of β-lactamase plasmids in Neisseria gonorrhoeae—the prevalent and conserved blaTEM-135 has not recently evolved and existed in the Toronto plasmid from the origin. BMC Infect. Dis. 2014; 14: 454 10.1186/1471-2334-14-454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Müller EE, Fayemiwo SA, Lewis DA. Characterization of a novel beta-lactamase-producing plasmid in Neisseria gonorrhoeae: sequence analysis and molecular typing of host gonococci. J. Antimicrob. Chemother. 2011; 66(7): 1514–17. 10.1093/jac/dkr162 [DOI] [PubMed] [Google Scholar]
- 26.Mlynarczyk-Bonikowska B, Kujawa M, Mlynarczyk G, Malejczyk M, Majewski S. Susceptibility to ceftriaxone and occurrence of penicillinase plasmids in Neisseria gonorrhoeae isolates isolated in Poland in 2012–2013. Folia Microbiol. (Praha). 2016; 61: 269–73. 10.1007/s12223-015-0434-7 [DOI] [PubMed] [Google Scholar]
- 27.Arlet G., Goussard S., Courvalin P, Philippon A. Sequences of the genes for the TEM-20, TEM-21, TEM-22, and TEM-29 extended-spectrum beta-lactamases. Antimicrob. Agents Chemother. 1999; 43(4): 969–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bradford PA. Extended-spectrum beta-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin. Microb. Rev. 2001; 14(4): 933–51. 10.1128/CMR.14.4.933-951.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lindberg R, Fredlund H, Nicholas R, Unemo M. Neisseria gonorrhoeae isolates with reduced susceptibility to cefixime and ceftriaxone: association with genetic polymorphisms in penA, mtrR, porB1b, and ponA. Antimicrob. Agents Chemother. 2007; 51(6): 2117–22. 10.1128/AAC.01604-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Osaka K, Takakura T, Narukawa K, Takahata M, Endo K., Kiyota H, Onodera S. Analysis of amino acid sequences of penicillin-binding protein 2 in clinical isolates of Neisseria gonorrhoeae with reduced susceptibility to cefixime and ceftriaxone. J. Infect. Chemother. 2008; 14(3): 195–203. 10.1007/s10156-008-0610-7 [DOI] [PubMed] [Google Scholar]
- 31.Whiley DM, Goire N, Lambert SB, Ray S, Limnios EA, Nissen MD, et al. Reduced susceptibility to ceftriaxone in Neisseria gonorrhoeae is associated with mutations G542S, P551S and P551L in the gonococcal penicillin-binding protein 2. J. Antimicrob. Chemother. 2010; 65(8): 1615–18. 10.1093/jac/dkq187 [DOI] [PubMed] [Google Scholar]
- 32.Cámara J, Serra J, Ayats J, Bastida T, Carnicer-Pont D, Andreu A, Ardanuy C. Molecular characterization of two high-level ceftriaxone-resistant Neisseria gonorrhoeae isolates detected in Catalonia, Spain. J. Antimicrob. Chemother. 2012; 67: 1858–60. 10.1093/jac/dks162 [DOI] [PubMed] [Google Scholar]
- 33.Unemo M, Golparian D, Nicholas R, Ohnishi M, Gallay A, Sednaoui P. High-level cefixime- and ceftriaxone-resistant N. gonorrhoeae in France: novel penA mosaic allele in a successful international clone causes treatment failure. Antimicrob. Agents Chemother. 2012; 56: 1273–80. 10.1128/AAC.05760-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 9.0, 2019: pages 55–62. http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_9.0_Breakpoint_Tables.pdf.
- 35.Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing, 24th informational supplement. CLSI Document M100-S24. Wayne, PA: CLSI; 2014.
- 36.Leinsoo AT, Shaskol'skii BL, Dement'eva EI, Gryadunov DA, Kubanov AA, Chestkov AV, et al. Oligonucleotide microchip for the identification of infectious agents of reproductive system with simultaneous analysis of determinants of resistance to antimicrobial substances. Bull. Exp. Biol. Med. 2017; 164(1): 54–60. 10.1007/s10517-017-3925-5 [DOI] [PubMed] [Google Scholar]
- 37.Martin IMC, Ison CA, Aanensen DM, Fenton KA, Spratt BG. Rapid sequence-based identification of gonococcal transmission clusters in a large metropolitan area. J. Infect. Dis. 2004; 189(8): 1497–1505. 10.1086/383047 [DOI] [PubMed] [Google Scholar]
- 38.Palmer HM, Leeming JP, Turner A. A multiplex polymerase chain reaction to differentiate β-lactamase plasmids of Neisseria gonorrhoeae. J. Antimicrob. Chemother. 2000; 45(6): 777–82. 10.1093/jac/45.6.777 . [DOI] [PubMed] [Google Scholar]
- 39.Zar JH. Biostatistical Analysis. Prentice Hall, New York; 2010. [Google Scholar]
- 40.Kumar S, Stecher G, Tamura K. MEGA7: molecular evolutionary genetics analysis version 7.0 for bigger datasets. Mol. Biol. Evol. 2016; 33(7):1870–74. 10.1093/molbev/msw054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hasegawa M, Kishino H, Yano T. Dating the human-ape split by a molecular clock of mitochondrial DNA. J. Mol. Evol. 1985; 22: 160–74. . [DOI] [PubMed] [Google Scholar]
- 42.Ashford WA, Golash RG, Hemming VG. Penicillinase-producing Neisseria gonorrhoeae. Lancet 1976; 2 (7987): 657–658. 10.1016/s0140-6736(76)92467-3 . [DOI] [PubMed] [Google Scholar]
- 43.Shaskolskiy B, Dementieva E, Leinsoo A, Petrova N, Chestkov A, Kubanov A, et al. Tetracycline resistance of Neisseria gonorrhoeae in Russia, 2015–2017. Infect. Genet. Evol. 2018; 63: 236–42. 10.1016/j.meegid.2018.06.003 [DOI] [PubMed] [Google Scholar]
- 44.Roberts MC, Knapp JS. Transfer of beta-lactamase plasmids from Neisseria gonorrhoeae to Neisseria meningitidis and commensal Neisseria species by the 25.2-megadalton conjugative plasmid. Antimicrob Agents Chemother. 1988; 32(9): 1430–32. 10.1128/aac.32.9.1430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Roberts MC. Plasmids of Neisseria gonorrhoeae and other Neisseria species. Clin. Microbiol. Rev. 1989; 2: S18–S23. 10.1128/cmr.2.suppl.s18 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pachulec E, van der Does C. Conjugative plasmids of Neisseria gonorrhoeae. PLoS One 2010; 5: e9962 10.1371/journal.pone.0009962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rotman E, Seifert HS. The genetics of Neisseria species. Annu. Rev. Genet. 2014; 48: 405–31. 10.1146/annurev-genet-120213-092007 [DOI] [PubMed] [Google Scholar]
- 48.Kubanov A, Solomka V, Plakhova X, Chestkov A, Petrova N, Shaskolskiy B et al. Summary and trends of the Russian Gonococcal Antimicrobial Surveillance Programme, 2005–2016. J. Clin. Microbiol., 2019; 5(6): e02024–18. 10.1128/JCM.02024-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.European Centre for Disease Prevention and Control. Gonococcal antimicrobial susceptibility surveillance in Europe, 2016 Stockholm: ECDC; 2018. [Google Scholar]
- 50.Abrams AJ, Kirkcaldy RD, Pettus K, Fox JL, Kubin G, Trees DL. A case of decreased susceptibility to ceftriaxone in Neisseria gonorrhoeae in the absence of a mosaic penicillin-binding protein 2 (penA) allele. Sex Transm. Dis. 2017; 44(8): 492–94. 10.1097/OLQ.0000000000000645 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ST–NG-MAST sequence type, Pen–penicillin, Tet–tetracycline, Cef–ceftriaxone, Cip–ciprofloxacin, Spec–spectinomycin, Azit–azithromycin.
(XLSX)
Mutations: penA–ins345Asp, ponA–Leu421Pro, mtrR (promoter region)–-35delA, porB–Gly120Lys/Asp/Asn/Thr and/or Ala121/Asp/Asn/Gly/Ser.
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.