Abstract
Background:
One in five adolescents and emerging adults have reported prescription opioid misuse (POM), posing significant risks for opioid-related adverse outcomes. Devising prevention strategies requires a better understanding of the decisional factors underlying risky misuse behavior. This research examined the associations between past opioid use behavior, opioid risk knowledge and perceptions, and intentional POM decisions.
Methods:
Participants aged 15–23 years completed surveys assessing past prescription opioid use and misuse, opioid risk knowledge, opioid risk perceptions, and pain relief preferences (i.e., analgesic benefit vs. risk aversion preference). The outcome, Willingness to Misuse (i.e., intentional decisions to use a prescription opioid in a non-compliant manner) was measured using hypothetical pain decision scenarios.
Results:
Surveys were completed by 972 adolescents and young adults. In total, 44% had taken a prescription opioid and 32% of these reported past POM. Willingness to Misuse was significantly associated with lower opioid misuse risk perceptions (β = .75 [95% CI .66–.86]) and past opioid misuse (β = 1.81 [95% CI 1.13–2.91]) but not simple risk knowledge (β = .81 [95% CI .58–1.11]. The probability of future misuse was highest for those who reported past opioid misuse and had low risk perceptions (58.7% [95% CI 51.3–65.8]) and high pain relief preferences (53.4% [95% CI 45.3%–61.3%]).
Conclusions:
Findings suggest that simple knowledge of prescription opioid risks is insufficient to curtail misuse among adolescents and emerging adults. Rather, it may be important to heighten opioid risk perceptions and strengthen opioid risk aversion values when prescribing opioid analgesics to better prevent future misuse in this high risk population.
Keywords: Opioid misuse, Pain, Risky decision-making, Adolescents, Young adults
The number of prescription opioids dispensed to adolescents and young adults in the United States quadrupled over just one decade [1], likely due to an emphasis on pain management during that period. This surge in prescribing was accompanied by increased rates of opioid-related adverse events [2–4], poisonings [5], opioid misuse [6], and opioid use disorder [7]. These adverse event rates have continued to soar despite the recent plateauing and even declining prescribing rates for children and adolescents [8], suggesting a lingering and worrisome undertow of the prescription opioid epidemic. Exposure to prescribed opioids for medical reasons poses both immediate and long-term risks. Following surgery or injury, 5%–12.5% of opioid-naïve children and adolescents persistently or recurrently use a prescribed opioid [9,10] presenting a high risk for ongoing opioid-related adverse events and dependence. Furthermore, legitimate use during adolescence has been associated with higher rates of opioid misuse and substance use disorder symptoms during adulthood [11,12]. The term prescription opioid misuse (POM) encompasses several risky behaviors including “medical misuse” (e.g., non–compliant use such as taking larger or more frequent doses or taking it for an unintended purpose), “non–medical misuse” (e.g., taking someone else’s prescription), and “diversion” (sharing with others) [13]. Each of these subtypes of misuse poses increased risk for serious adverse outcomes including drug dependence (when drugs are taken longer than intended or over time), drug addiction and accidental overdose, particularly when the inherent risks of prescribed opioids are not known or are underestimated.
A primary motivation for POM for a majority (84%–88%) of adolescents and young adults is to treat pain [14], and 71% of those motivated by self-treatment of pain reported using a past personal prescription [15]. While these and other less common motivations for POM are well described, the decisional factors that may help explain these risky behaviors have not been well explored. Since many misusers are motivated by a desire to self-treat pain, it may be that a large portion of misuse behavior reflects a deliberative process involving a consideration of expected benefits (e.g., pain relief) and expected risks [16]. Higher perceptions of benefit, which are common among adolescents considering risky behavior [16], combined with lower risk perceptions may, thus, promote opioid misuse. Such deliberations are likely influenced by past experiences and the mental models formed in response [16,17]. For instance, experience with opioid use or misuse might leave an impression of the subjective benefits (“I used it this way before”, “Something good happened”) and lessen the perception of risk, particularly if no negative consequences occurred [16,17]. A better understanding of the cognitive and experiential factors associated with POM decisions is needed to optimize interventions to prevent future misuse. This observational, cross-sectional study, therefore, examined the associations between adolescents’ and young adults’ prescription opioid risk knowledge, risk perceptions, their past experiences with prescription opioids, and their decisions to misuse a prescription opioid to treat pain. We hypothesized that (1) greater knowledge of serious opioid-related risks and higher risk perceptions would be associated with less willingness to misuse an opioid, and (2) past experience with prescription opioid use and misuse would be associated with an increased willingness toward future misuse.
Methods
With approval from the Institutional Review Board at the University of Michigan (IRB-MED; HUM119543), trained research assistants approached healthy individuals aged 15–23 years in common areas (e.g., coffee shops, study areas) on and nearby the University of Michigan campus. All were approached independent of race, sex, or ethnicity, and STROBE guidelines [18] were followed. Following a brief study description and screen for age, verbal consent/assent was obtained and participants used an iPad to complete a Qualtrics survey. No personal identifiers were recorded to ensure anonymity and encourage honest disclosure.
Survey and measures
The survey assessed past pain experiences, pain relieving treatments, and sources of analgesics and information (see the Appendix for key measures). Both the generic and common brand names for all analgesics of interest were included (e.g., hydrocodone [Vicodin/Norco] and oxycodone [OxyIR/Roxicodone/Percocet]). Demographics and an assessment of recent substance use using specific screening items from the Screening to Brief Intervention Tool [19] (i.e., How frequently have you used…tobacco, alcohol, marijuana, and illegal drugs) were elicited.
Main measures
Past prescription opioid misuse.
This measure was modified from the widely cited Secondary Student Life Survey and Monitoring the Future items that assess lifetime medical misuse and non–medical misuse [20]. Specifically, we asked participants, “Have you ever, at least once taken more of the opioid pain medicine than was prescribed or recommended (higher or more frequent dose, taken for a reason other than prescribed)”. In the same manner as previous surveys, we followed a positive response to past POM with the question, “Please provide the reason(s) why” and provided a list of potential motives for doing so.
Pain relief preference.
This instrument assesses the relative importance that individuals place on obtaining analgesic benefit (pain relief) versus the importance of avoiding analgesic risks (risk aversion) [21]. This survey is similar to those that assess the values and preferences that individuals place on medical treatments which, in turn, have been associated with treatment adherence [22]. Participants ranked six risk-benefit items (e.g., “Pain relief is more important than the side effects of prescription pain drugs”) from strongly disagree (−2) to strongly agree (+2), yielding a summary score from −12 (strongly risk avoidant) to +12 (strongly pain relief [i.e., benefit] preferent). Scores of 0 reflect a relative ambivalence. This tool has demonstrated internal consistency (Cronbach’s alpha.763) [21] and yields two factors (i.e., benefit vs. risk avoidant preferent) that explain 57% of the variance in total score (KMO sampling adequacy >.64; p< .001) [23].
Opioid risk knowledge.
This tool assesses awareness of common (e.g., nausea, constipation) and serious (i.e., excessive sedation, slowed breathing and addiction) opioid-related adverse effects. Items have established content validity and were demonstrated to have predictive validity for opioid decision-making among adults [24]. For the purpose of this study, we summarized participant awareness of the serious opioid-related risks (addiction, over-sedation, and slowed breathing) into the opioid risk knowledge variable, where 1 = aware of all three serious effects and 0 = no or partial awareness.
Medical use and misuse risk perceptions.
To get a general sense of opioid risk perceptions, we asked participants to rate their perceptions of seriousness of adverse effects from 0 to 5, where 0 = not serious and 5 = extremely serious and to rate the overall riskiness over the counter and opioid analgesics [24,25]. Perceived seriousness of adverse effects has been shown to have predictive validity toward parental opioid decision-making [24]. Finally, similar to a recent study that measured perceived harmfulness of non-medical misuse from no risk to great risk, [26] we asked participants to rate the risk of taking a previously prescribed opioid for a new condition (medical misuse) and of sharing one’s own prescribed opioid with a friend (non–medical misuse or diversion). The measure POM Risk Perception was imputed from these later two items and yielded a score ranging from 0 (not risky) to 5 (extremely risky).
Outcome measure
Willingness to misuse an opioid.
Similar to previous studies of opioid decision-making, we used scenarios to assess misuse intent. Scenario-based questions have been successfully used to assess variability in analgesic decision-making based on differing situational pain signals [25]. The scenarios used here were assessed among six undergraduate college students who supported their face validity as measures of misuse intent. Each scenario described a hypothetical pain situation after which participants were asked to decide among several choices (e.g., “Take 2 of the prescribed Vicodin”…”Take 1 Advil”…”Take nothing”) or to write in an action not listed. The first scenario assessed participants’ decisions to medically misuse (i.e., take their own opioid prescribed a year ago for wisdom teeth extraction for a new, unrelated condition-unrelieved headache). The second assessed decisions to medically misuse for unrelieved oral surgery pain (i.e., take a higher dose of their own currently prescribed Vicodin) or non–medically misuse (i.e., take a friend’s offered oxycodone). The last scenario assessed participants’ willingness to divert (i.e., share a prescribed opioid with a friend). The Willingness to Misuse binary variable reflects any reported misuse intent.
Statistical analysis
We used SPSS (version 24, IBM Corporation, Armonk, NY) for analyses. We characterized the sample and assessed normality using descriptive statistics and then compared parametric and non–parametric data with unpaired t and chi square tests, respectively. To test the hypotheses, we used a logistic regression model to regress the outcome onto subject characteristics, opioid risk knowledge and perception variables, and past opioid experience. p Values of <.05 were considered significant. Data are presented as odds ratios (OR) or mean differences (MD) with 95% confidence intervals (CI). To more clearly depict the effect of risk perceptions and analgesic preferences on the outcome, we used a posthoc generalized mixed effects logistic regression models (accounting for repeated measures and subject effects) to describe the estimated predicted probabilities of willingness to misuse for (1) the group overall, (2) the group adjusted for high and low pain relief preferences (i.e., benefit vs. risk avoidant preferent), and (3) the group adjusted for high and low risk perceptions. This description enhances the interpretability of the effects of these factors.
Based on previous census data, we estimated that 33,000 adolescents and young adults aged 15–23 years live in the Ann Arbor campus area. Using standard survey methodology, we determined that 1,000 respondents was more than sufficient to provide a representative sample to calculate estimates of prescription opioid use and misuse with a confidence level of 95% and a confidence interval (margin of error) of ±4% [27]. This sample was deemed more than sufficient to detect a modest effect size (OR 1.7; power .8, significance .05) for our main factors of interest on the outcome (expected proportion 10% [28]) [29].
Results
Sample description
One thousand thirteen volunteers were surveyed from May through September 2017, but 41 (4%) were incomplete due to Internet connection problems or time constraints, leaving 972 for analyses. Our convenience sample was representative of the community at large with the exception of sex (69% female in our sample compared to 52% for the community; that is, 2015 university census demographics include 52% female, 13% Asian, 5% black, 5% Hispanic, 66% white, 4% >two, and 7% other/unknown; City of Ann Arbor 2016 data include 49% female, 16% Asian, 7% black, 4% Hispanic, 68% white, 4% >two, and 1% other/unknown).
Table 1 depicts the past pain history and analgesic preferences of respondents who had previously used a prescribed opioid compared to those who did not. Notably, 90% of respondents overall reported at least monthly pain and 96% reported past analgesic use (mostly over-the-counter nonopioids).
Table 1.
Characteristics of the sample (n = 972)
| Previously used a prescription opioid (n = 432) | Never used a prescription opioid (n = 540) | Univariate comparisons between groups | |
|---|---|---|---|
| Age (years) | 19.91 ± 1.3 | 19.4 ± 1.5 | MD −0.51 (CI −.69 to −.33) |
| Female sex | 289 (67%) | 381 (71%) | OR .84 (CI .64–1.12) |
| Race | |||
| White | 342 (79%) | 331 (61%) | OR 2.4 (CI 1.8–3.2) versus all |
| Asian | 42 (10%) | 130 (24%) | Others |
| Black | 15 (4%) | 33 (6%) | |
| Hispanic | 14 (3%) | 23 (4%) | |
| Other | 19 (4%) | 23 (4%) | |
| Substance use within 30 days | |||
| Tobacco | 78 (18%) | 62 (12%) | OR 1.71 (CI 1.19–2.45) |
| Alcohol | 380 (89%) | 379 (71%) | OR 3.37 (CI 2.36–4.81) |
| Illegal drugs | 127 (30%) | 131 (24%) | OR 1.31 (CI .98–1.75) |
| Pain and analgesic use history | |||
| Pain types | |||
| Headache | 393 (91%) | 469 (87%) | OR 1.53 (CI 1.01–2.31) |
| Abdominal | 342 (79%) | 415 (77%) | OR 1.15 (CI .84–1.56) |
| Muscular-Skeletal | 371 (86%) | 384 (71%) | OR 2.47 (CI 1.78–3.43) |
| Frequent analgesica use (≥once or twice a month) | 365 (85%) | 374 (69%) | OR 2.42 (CI 1.76_3.32) |
| Used marijuana for pain | 69 (16%) | 39 (7%) | OR 2.43 (CI 1.6_3.7) |
| Pain relief preference score (normally distributed) | −47 ± 3.87 | −1.22 ± 3.67 | MD −.77 (CI −1.23 to −.28) |
MD = Mean difference; OR = Odds ratio; CI = 95% confidence interval.
Indicates overall analgesic use that includes over-the-counter agents.
Importantly, 32% of past prescription opioid users reported POM, and 99% of these did so to relieve pain. Other reasons for past POM included the following: to sleep (n = 33 [8%]), relieve anxiety (n = 7 [2%], get high (n = 8 [2%]), or experiment (n = 6 [1%]). Pain relief preference scores were significantly lower (i.e., more risk averse) for respondents who had never misused a prescription opioid compared to those who had (MD −.76 [95% CI −1.24 to −.28]).
Analgesic knowledge and risk perceptions
Table 2 shows the differences in opioid risk awareness and perceptions between those who had previously used an opioid compared to those who had not. In addition to the noted differences between these groups, the sample overall rated the riskiness of sharing an opioid with others (i.e., diversion) significantly higher than the risk of misusing one’s own past prescription (i.e., medical misuse; MD 2.08 [95% CI 2.01–2.05]). Additionally, participants who reported past POM had significantly lower risk perceptions of medical misuse (i.e., misusing one’s own prescription; MD −0.497 [95% CI −0.76 to −0.24]) and diversion (i.e., MD −0.449 [95% CI −0.68 to −0.22]) compared to those who had never misused.
Table 2.
Opioid risk knowledge and perceptions among past prescription opioid users and nonusers
| Past prescription opioid users (n = 432) | Nonusers (n = 540) | Univariate comparisons between groups | |
|---|---|---|---|
| n (%) | n (%) | Odds ratio (95% confidence interval); p value | |
| Aware of serious opioid-related risks | |||
| Addiction | 362 (84%) | 356 (66%) | 2.71 (2.0–3.71); <.001 |
| Over-sedation | 368 (86%) | 298 (56%) | 4.74 (3.45–6.52); <.001 |
| Slowed breathing | 219 (52%) | 199 (37%) | 1.83 (1.41–2.37); <.001 |
| Know all three | 215 (51%) | 186 (35%) | 1.94 (1.49–2.51); <.001 |
| Risk perceptions (measured from 0 to 5, where 0 = not risky/serious and 5 = most risky/serious) | |||
| Mean ± SD | Mean ± SD | Mean difference (95% confidence interval); p value | |
| Perceived seriousnessa of opioid-related risks | |||
| Addiction | 3.27 ± 2.14 | 3.61 ± 1.92 | .34 (.08–.60); .011 |
| Over-sedation | 2.85 ± 1.48 | 2.56 ± 1.48 | −.29 (−.48 to −.09); .004 |
| Slowed breathing | 3.03 ± 2.02 | 3.21 ± 1.84 | .18 (−.07−.43); .168 |
| Perceived riskinessa of taking over-the-counter analgesics | .84 ± .86 | 1.05 ± .93 | .20 (.09–0.32); .001 |
| Perceived riskinessa of taking a prescribed opioid | 2.02 ± 1.19 | 2.29 ± 1.30 | .26 (.10–.41); .001 |
| Perceived riskinessa of taking one’s own past prescription for an unrelated condition (medical misuse) |
3.81 ± 1.16 | 3.93 ± 1.18 | .12 (−.03−.26); .128 |
| Perceived riskinessa of sharing one’s own opioid left-overs with a friend (diversion) | 4.23 ± 1.04 | 4.26 ± 1.06 | .03 (−.10−.17); .643 |
Seriousness and riskiness rated from 0 (not serious or risky) to 5 (extremely serious or risky).
Willingness to misuse a prescribed opioid
Overall, 249 respondents (26%) indicated a willingness to misuse an opioid for one or more of the scenarios. Past prescription opioid users were significantly more likely to indicate this willingness compared to nonusers (29% vs. 23%; OR 1.34 [95% CI 1.001–1.79]). More specifically, 56 (6%) would medically misuse a prescribed opioid for the first scenario (unrelenting headache), 167 (17%) would medically misuse their own and 55 (6%) would non-medically misuse someone else’s drug for unrelieved toothache in the second scenario, and 25 (3%) would share a prescribed opioid with a friend in pain. In addition, one respondent would use marijuana or “dank kush” for headache, another would use “cold water extraction of the hydrocodone” for either headache or toothache (this latter description coded as willing to misuse).
Hypothesis tests
Table 3 depicts the adjusted odds for all associations between factors and the outcome, willingness to misuse an opioid. The model supported, in part, the first hypothesis in that higher perceived riskiness of misuse was significantly associated with lower willingness to misuse, whereas greater awareness of the potential serious risks of opioids was not associated with this outcome. The model also supported, in part the second hypothesis, that is, past prescription opioid use itself was not independently associated with the outcome but past misuse was associated with greater willingness to misuse. Indeed, individuals who had misused an opioid in the past were nearly twice as likely as those who had not misused to be willing to misuse again. To better clarify and interpret the effect of risk perceptions and pain relief preferences, Figure 1 shows how the predicted probability of future misuse was highest for individuals (both those who never misused and those who had misused in past) with the lowest misuse risk perceptions and for those with highest pain relief preference (i.e., benefit preferent).
Table 3.
Results from the logistic regression model (chi-square = 77.77; df = 11; p<.001)
| Factors | OR [95% CI]; p value |
|---|---|
| Age | 1.01 [.91–1.13]; .808 |
| Female sex (vs. male) | .74 [.53–1.04]; .085 |
| White race (vs. others) | .86 [.61–1.21]; .387 |
| Pain relief preference | 1.07 [1.03–1.12]; .002 |
| ≥Monthly analgesic use (vs. less frequent to none) | .96 [.65–1.41]; .829 |
| Recent substance usea | 1.67 [1.20–2.33]; .003 |
| Hypothesis 1: Greater knowledge and higher perceived riskiness of opioid misuse predict less willingness to misuse an opioid (i.e., any intent for medical or non–medical misuse or diversion) for pain treatment | |
| Awareness of all serious opioid risks (vs. no awareness) | .81 [.58–1.11]; .187 |
| Perceived riskiness opioid misuse (rank 0–5) | .75 [.66–.86]; <.001 |
| Hypothesis 2: Past opioid use and misuse behaviors increase the willingness to misuse an opioid for pain treatment | |
| Prescribed opioid use (vs. none) | 1.10 [.74–1.61]; .646 |
| Past opioid misuse (vs. none) | 1.81 [1.13–2.91]; .015 |
OR = Odds ratio; CI = Confidence interval, df = Degrees of freedom.
Includes alcohol, illicit drugs, and marijuana.
Figure 1. Predicted probabilities of willingness to misuse among past prescription opioid misusers and nonmisusers.
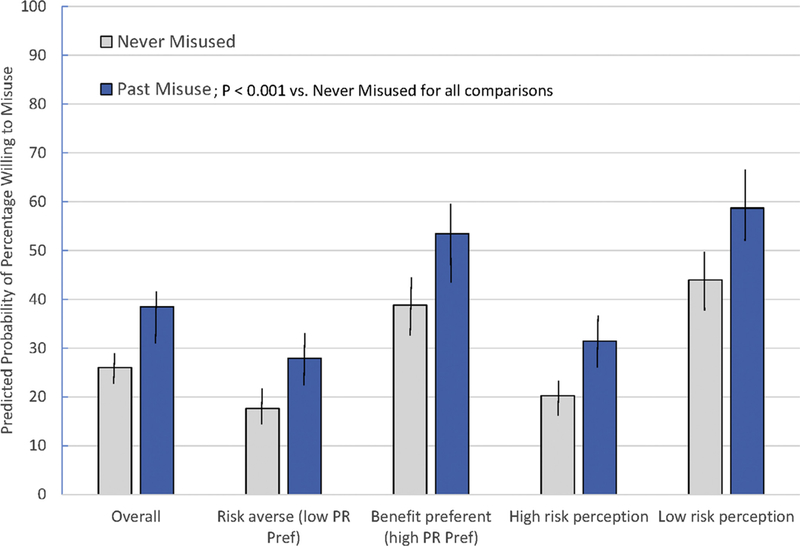
Results are based on five mixed effects logistic regression models where pain relief preference scores were fixed at high (+8) values, and then low (–8) values, and perceived opioid misuse riskiness was fixed at high (5) and low (1) values. In each model, all other continuous variables were fixed at the mean. The estimated marginal means and (95% confidence intervals) are shown.
Discussion
Findings from this large community survey of adolescents and young adults suggest that perceptions of opioid misuse riskiness, pain relief preferences (i.e., analgesic benefit), and past opioid misuse experience help to explain what may be deliberative prescription opioid misuse decisions among those considering self-treatment of pain. These findings have significant implications for strategizing better interventions to mitigate prescription opioid misuse among transitional aged youth.
Importantly, we found no association between simple awareness of serious opioid-related adverse outcomes (e.g., addiction, excessive sedation, respiratory depression) and willingness to misuse a prescription opioid. This finding suggests that provision of simple risk information alone, such as that included in newly mandated opioid consent forms, is likely to be insufficient toward mitigating the potential for later prescription opioid misuse. In contrast, we found that stronger preferences for analgesic benefit (i.e., pain relief) and lower risk perceptions were strongly associated with misuse intention. These findings align with studies of risky decision-making among adolescents and young adults who respond more to the possibility of short-term benefit than to the potential long-term and rare risks, and whose risk perceptions are strongly associated with behavioral willingness [30]. Together, these findings suggest a need to heighten opioid risk perception and strengthen risk aversion preferences.
Of note, past prescription opioid users in our sample ranked the riskiness of addiction (a long-range outcome) lower compared to past nonusers but ranked the excessive sedation risk higher. This risk appraisal may reflect a mental model derived from personal experience with the more immediate adverse effect, sedation. These findings are not surprising since adolescents’ risk perceptions are often reappraised downward after experience with a risky behavior [17,30]. Indeed, longitudinal data show how experience with drinking and driving, unprotected sex, or heroin use together with failure to experience negative outcomes leads to lowered risk perceptions [16,31].
Since adolescents exhibit cognitive appraisal during risky decision-making, some suggest that behaviors may be best modified by discouraging deliberative analysis of risks and benefits and, rather, by enhancing risk perceptions and risk avoidance values [30]. Giving verbatim or quantitative information about low rates of negative outcomes (e.g., overdose, dependence, and addiction) could provide a “rational calculus of risk promotion” that endorses risk-taking and intentions among youth who focus on potential benefits [16]. Conversely, enhancing gist risk perceptions (i.e., simple global perceptions) has been found to decrease risky intentions [16]. Devising the most effective health-risk messaging for adolescents is complex given the impact of “unpunished” experiences and that gist-based risk perceptions develop slowly as experience matures [17]. Novel prevention strategies aimed at strengthening the perceived benefits of health-promoting behaviors may, therefore, end up being more successful in reducing risk-taking among adolescents. For instance, promoting healthier approaches to pain management (e.g., non-opioid analgesics and non-pharmacologic methods) in combination with messages that enhance prescription opioid risk perceptions may better prevent intentional POM for self-treatment of pain.
Notably, more respondents in our sample indicated a willingness to misuse a personal prescription than to use a friend’s or share with a friend (non-medically misuse or diversion), reflecting common misconceptions about the safety of prescribed opioids [32]. Additionally, similar to others [33–35], we found an association between substance use behavior and willingness to misuse a prescription opioid. Together, these findings suggest a need to better assess past prescription opioid behaviors and substance use and to introduce preventive interventions at the time of prescribing before the slippery slope of misuse and subsequent risk reappraisal has the chance to emerge.
Our findings must be considered in light of the following limitations. Our convenience sample was drawn from one university community and our sample included primarily older, white and female adolescents. Thus, our sampling limits the potential generalizability to other population. Next, the data reflect self-report of potentially sensitive information. However, surveys were anonymous and the questions were carefully worded to be nonjudgmental to promote honest disclosure and reduce the potential for response bias. Additionally, our findings are validated, in part, by previous, broader-based community data showing similar rates of self-reported pain [36], analgesic use [37], prescription opioid use (including racial differences in use) and misuse [38]. Despite some external validation, the ability to generalize to other populations of youth is limited by our sampling. Next, although we did not directly measure perceived personal vulnerability, we did find that riskiness of personal opioid misuse was ranked lower than riskiness of sharing or diversion which is in line with data regarding personal invulnerability among youth [39]. Our study explored decisional factors related to intentional risk taking specifically for treatment of pain, and thus, factors related to impulsive POM may differ. Indeed, recent data suggest that perceived harmfulness was not associated with non-medical prescription opioid use in college students who scored high in sensation-seeking [26]. Such differences suggest a need for differing interventional strategies for different target populations. Last, it could be argued that hypothetical decision-making may not align with real-world decision-making. Yet, empirical studies have shown that hypothetical decisions are highly correlated with real behavior and provide the opportunity to manipulate key variables that are otherwise difficult to ascertain in the real world [40].
Despite these limitations, this study identified important risk perception and experiential factors that may contribute to adolescents’ and emerging adults’ risky decisions to misuse prescription opioids. Our findings have important implications given that millions of prescriptions are dispensed to this group annually, posing ongoing and potentially significant risks of misuse and adverse events. Our data can also inform recent policy mandates for parental consent and youth education. We find the likely targets for intervention include the need to heighten opioid misuse risk perceptions (not simple risk awareness alone) and strengthen analgesic risk aversion values when prescribing opioids to treat pain in adolescents and young adults.
Supplementary Material
IMPLICATIONS AND CONTRIBUTION.
This study of adolescents and young adults demonstrates how prescription opioid misuse risk perceptions, analgesic risk avoidance preferences, and past opioid misuse behavior factor into decisions to misuse prescription opioids for pain. These data suggest modifiable targets for interventions when prescribing opioids to mitigate opioid misuse among emerging adults.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors have no potential conflicts of interest to declare, and all have made a substantive contribution to this work. The authors thank the following undergraduate research students who recruited subjects and conducted the surveys for this study: Emily Currier, Trevor de Sibour, Caroline Hyman, Marianna Dorta, Jacqueline Meier, Connor Knowles, and Deontay Walker. This study has not been presented previously.
Footnotes
Conflict of interest: None of the authors have potential conflicts of interest.
References
- [1].Fortuna RJ, Robbins BW, Caiola E, et al. Prescribing of controlled medications to adolescents and young adults in the United States. Pediatrics 2010;126:1108–16. [DOI] [PubMed] [Google Scholar]
- [2].Budnitz DS, Pollock DA, Weidenbach KN, et al. National surveillance of emergency department visits for outpatient adverse drug events. JAMA 2006;296:1858–66. [DOI] [PubMed] [Google Scholar]
- [3].Tadros A, Layman SM, Davis SM, et al. Emergency department visits by pediatric patients for poisoning by prescription opioids. Am J Drug Alcohol Abuse 2016;42:550–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Warner M, Chen LH, Makuc DM. Increase in fatal poisonings involving opioid analgesics in the United States, 1999–2006 Hyattsville: Centers for Disease Control and Prevention; 2009. [PubMed] [Google Scholar]
- [5].Gaither JR, Leventhal JM, Ryan SA, et al. National trends in hospitalizations for opioid poisonings among children and adolescents, 1997 to 2012. JAMA Pediatr 2016;170:1195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Jordan AE, Blackburn NA, Des Jarlais DC, et al. Past-year prevalence of prescription opioid misuse among those 11 to 30years of age in the United States: A systematic review and meta-analysis. J Subst Abuse Treat 2017;77:31–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Martins SS, Segura LE, Santaella-Tenorio J, et al. Prescription opioid use disorder and heroin use among 12–34 year-olds in the United States from 2002 to 2014. Addict Behav 2017;65:236–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Groenewald CB, Rabbitts JA, Gebert JT, et al. Trends in opioid prescriptions among children and adolescents in the United States: A nationally representative study from 1996 to 2012. Pain 2016;157:1021–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Harbaugh CM, Lee JS, Hu HM, et al. Persistent opioid use among pediatric patients after surgery. Pediatrics 2018;141:e20172439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Whiteside LK, Russo J, Wang J, et al. Predictors of sustained prescription opioid use after admission for trauma in adolescents. J Adolesc Health 2016; 58:92–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].McCabe SE, Veliz P, Schulenberg JE. Adolescent context of exposure to prescription opioids and substance use disorder symptoms at age 35: A national longitudinal study. Pain 2016;157:2173–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Miech R, Johnston L, O’Malley PM, et al. Prescription opioids in adolescence and future opioid misuse. Pediatrics 2015;136:e1169–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2016 national survey on drug use and health (HHS publication no. SMA 17–5044, NSDUH series H-52) Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2017. [Google Scholar]
- [14].McCabe SE, West BT, Boyd CJ. Motives for medical misuse of prescription opioids among adolescents. J Pain 2013;14:1208–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].McCabe SE, West BT, Boyd CJ. Leftover prescription opioids and nonmedical use among high school seniors: A multi-cohort national study. J Adolesc Health 2013;52:480–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Reyna VF, Estrada SM, DeMarinis JA, et al. Neurobiological and memory models of risky decision making in adolescents versus young adults. J Exp Psychol Learn Mem Cogn 2011;37:1125–42. [DOI] [PubMed] [Google Scholar]
- [17].Albert D, Steinberg L. Judgment and decision making in adolescence. J Res Adolesc 2011;21:211–4. [Google Scholar]
- [18].von Elm E, Altman DG, Egger M, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007;335:806–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Levy S, Weiss R, Sherritt L, et al. An electronic screen for triaging adolescent substance use by risk levels. JAMA Pediatr 2014;168:822–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Johnson L, O’Malley PM, Bachman J, et al. Monitoring the future national survey results on drug use, 1975–2010 The University of Michigan Institute for Social Research; 2011. [Google Scholar]
- [21].Voepel-Lewis T, Zikmund-Fisher BJ, Smith EL, et al. Parents’ preferences strongly influence their decisions to withhold prescribed opioids when faced with analgesic trade-off dilemmas for children: A prospective observational study. Int J Nurs Stud 2015;52:1343–53. [DOI] [PubMed] [Google Scholar]
- [22].Tibaldi G, Clatworthy J, Torchio E, et al. The utility of the Necessity Concerns Framework in explaining treatment non-adherence in four chronic illness groups in Italy. Chronic Illn 2009;5:129–33. [DOI] [PubMed] [Google Scholar]
- [23].Voepel-Lewis T, Zikmund-Fisher BJ, Boyd CJ, et al. Effect of a scenario-tailored opioid messaging program on parents’ risk perceptions and opioid decision-making. Clin J Pain 2018;34:497–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Voepel-Lewis T, Zikmund-Fisher BJ, Smith EL, et al. Parents’ analgesic trade-off dilemmas: How analgesic knowledge influences their decisions to give opioids. Clin J Pain 2016;32:187–95. [DOI] [PubMed] [Google Scholar]
- [25].Voepel-Lewis T, Zikmund-Fisher B, Smith EL, et al. Opioid-related adverse drug events: do parents recognize the signals. Clin J Pain 2015;31:198–205. [DOI] [PubMed] [Google Scholar]
- [26].Arria AM, Caldeira KM, Vincent KB, et al. Perceived harmfulness predicts non-medical use of prescription drugs among college students: Interactions with sensation-seeking. Prev Sci 2008;9:191–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Bartlett J, Kotrlik J, Higgins C. Organizational research: Determining appropriate sample size in survey research. Inf Technol Learn Perform J 2001;19: 43–50. [Google Scholar]
- [28].Boyd CJ, Young A, Grey M, et al. Adolescents’ nonmedical use of prescription medications and other problem behaviors. J Adolesc Health 2009;45:543–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Demidenko E Sample size determination for logistic regression revisited. Stat Med 2007;26:3385–97. [DOI] [PubMed] [Google Scholar]
- [30].Reyna VF, Farley F. Risk and rationality in adolescent decision making: Implications for theory, practice, and public policy. Psychol Sci Public Interest 2006;7:1–44. [DOI] [PubMed] [Google Scholar]
- [31].Votaw VR, Wittenauer J, Connery HS, et al. Perceived risk of heroin use among nonmedical prescription opioid users. Addict Behav 2017;65:218–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Kenne DR, Hamilton K, Birmingham L, et al. Perceptions of harm and reasons for misuse of prescription opioid drugs and reasons for not seeking treatment for physical or emotional pain among a sample of college students. Subst Use Misuse 2017;52:92–9. [DOI] [PubMed] [Google Scholar]
- [33].McCabe SE, West BT, Boyd CJ. Medical use, medical misuse, and nonmedical use of prescription opioids: Results from a longitudinal study. Pain 2013;154:708–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Vaughn MG, Nelson EJ, Salas-Wright CP, et al. Racial and ethnic trends and correlates of non-medical use of prescription opioids among adolescents in the United States 2004–2013. J Psychiatr Res 2016;73:17–24. [DOI] [PubMed] [Google Scholar]
- [35].Monnat SM, Rigg KK. Examining rural/urban differences in prescription opioid misuse among US adolescents. J Rural Health 2016;32:204–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].King S, Chambers CT, Huguet A, et al. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 2011;152: 2729–38. [DOI] [PubMed] [Google Scholar]
- [37].Fouladbakhsh JM, Vallerand AH, Jenuwine ES. Self-treatment of pain among adolescents in an urban community. Pain Manag Nurs 2012;13:80–93. [DOI] [PubMed] [Google Scholar]
- [38].McCabe SE, West BT, Veliz P, et al. Trends in medical and nonmedical use of prescription opioids among US adolescents: 1976–2015. Pediatrics 2017;139:e20162387. doi: 10.1542/peds.2016-2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Millstein SG, Halpern-Felsher BL. Perceptions of risk and vulnerability. J Adolesc Health 2002;31:10–27. [DOI] [PubMed] [Google Scholar]
- [40].Anderson LR, Mellor JM. Predicting health behaviors with an experimental measure of risk preference. J Health Econ 2008;27:1260–74. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


