Abstract
Purpose of review:
There is a perceived shortage of evidence-based treatment programs for adults on the autism spectrum. This article reviews the recent research literature on psychosocial / behavioral interventions targeting social functioning in autistic adults without intellectual disability.
Recent findings:
We identified only 41 peer-reviewed studies published from 1980 through 2017 that tested intervention programs focused on one or more of the behavioral components of social functioning (i.e. social motivation, social anxiety, social cognition, and social skills) in more than one adult with autism spectrum disorder (ASD). The studies demonstrated substantial variability in treatment objectives, intervention procedures, assessment methods, and methodologic quality.
Summary:
The results indicate a strong need for additional research to develop and rigorously test interventions for autistic adults that target the many behavioral components of social functioning and that include procedures to promote generalization of knowledge and skills to community settings.
Keywords: autism, adult, social behavior, interventions, review
Introduction
Social functioning deficits – including difficulties with reciprocal social communication and with forming, maintaining, and understanding relationships – are core symptoms of autism spectrum disorder (ASD). These symptoms are particularly important and challenging to address for autistic adults, because adult relationships are more complex and subtler than childhood interactions, and there is less community tolerance for social “mistakes” in adults (1–8). There is a need for both greater community understanding and acceptance of autistic adults, as well as the development and testing of programs to support autistic adults in social functioning (9–12).
Social functioning comprises a complex repertoire of behaviors that need to be tailored to the social context. Pallathra and colleagues (13) argue that there are at least four broad categories of behavior that underlie social functioning, each of which may be disrupted in adults with ASD to varying degrees: social motivation, social anxiety, social cognition, and social skills. We have argued that these four components of social functioning should be regarded as core treatment targets, as disruption of any one of these components could impair social functioning (13). Therefore, our present review uses these components as a framework for reviewing the published treatment literature.
The first component – reduced social motivation, i.e. reduced motivation to interact with others – is observed in many individuals with ASD (1, 14, 15). Social motivation is a complex construct that comprises five main subcomponents, any of which may be affected in ASD: prioritizing and attending to social stimuli (social orienting), endorsing an interest in interaction (social interest), seeking out social interaction (social approach), taking pleasure in interactions (social liking), and engaging in relationships with others over a sustained period of time (social maintaining) (14, 15). Second, many adults with ASD have debilitating social anxiety or social avoidance (16–18). Third, many adults with ASD have impairments in social cognition, which comprises the abilities to identify and interpret verbal and nonverbal social information (19–21). Finally, deficits in social skills are well documented in individuals with ASD both in childhood and adulthood (14, 22). Our data indicate that adults with ASD (13) show only modest correlations in measures across these categories (social motivation, anxiety, cognition, and skills), with a more consistent pattern of correlations between social motivation and most other categories. These data suggest that no single category determines functioning in all others; that interventions targeting social functioning may be most effective if they include modules targeting all 4 categories, including social motivation.
We sought to systematically review the research literature between 1980 and 2017, to determine the number of intervention studies targeting social functioning in autistic adults and the number that target more than one behavioral component of social functioning. We also sought to determine how many of these interventions included an opportunity for adults to generalize and apply knowledge and skills to their everyday lives in the community. Finally, we sought to determine the overall methodologic quality of these studies.
Methods
Search Procedure
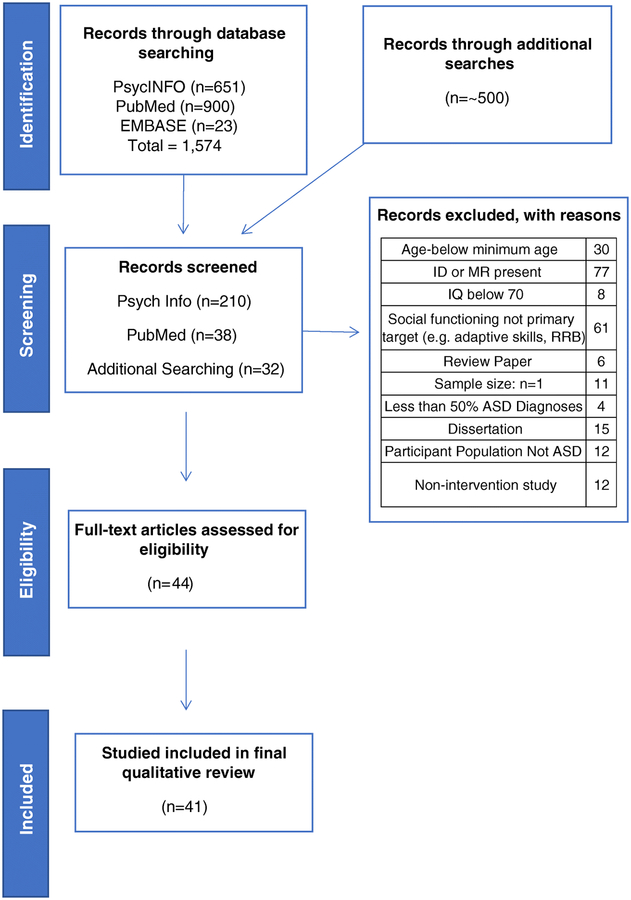
A systematic literature search was executed to identify published treatment studies that include autistic adults, using three online databases (PsycINFO, PubMed, EMBASE on OVID). The search focused on terms related to adults with ASD but without intellectual disability. The search concentrated on psychosocial or behavioral interventions related to social skills or social functioning. Search terms related to intellectual disability, biological studies, or animal models (e.g. gene, linked, drug, mouse, rat, pharmacology) were used to exclude studies (See Supplementary Material). Additional studies were identified through systematic analysis of the citations listed in review papers found in the standardized searches (Figure 1).
Fig. 1.
Manuscript identification process
Inclusion and Exclusion Criteria
All articles reviewed were required to meet the following pre-determined criteria in order to be included: 1) they report peer-reviewed research published in English between January 1980 and December 2017; 2) they describe the execution and detailed methods of a psychosocial or behavioral intervention aimed at improving social functioning, rather than a descriptive study (studies evaluating supported employment methods or methods to teach tasks specifically related to employment were excluded); 3) they include at least one outcome measure that assessed skills, understanding, or affective state related to social functioning; 4) they have sample sizes of greater than one participant, with all participants being 16 years of age or older and at least 50% of participants being 18 years of age or older; 5) at least 50% of each study’s sample must have been diagnosed with ASD without intellectual disability (i.e. full-scale IQ > 70) (Figure 1).
Rating of Methodological Quality
Methodology, participant demographics, and behavioral category target were determined for each article (Table 1). Regarding methodology, articles were classified as a randomized controlled trials (RCT), quasi-experimental studies (quasi), or non-controlled experiments (NCE). RCT studies were defined as those involving random assignment of participants to either an experimental group or a control group. Quasi studies assigned participants to experimental or control groups but did not use strictly-defined randomization to do so. NCE studies did not utilize a control group in their procedures.
Table 1.
Summary of studies included in review
| Study | Treatment (Tx) Name | Design | Total (n) | Tx (n) | Control (n) | Frequency | Duration | Delivery Format | Primary Social Domain Target (s) | Quality Rating |
|---|---|---|---|---|---|---|---|---|---|---|
| Baker-Ericzén (2017) | Supported Employment, Comprehensive Cognitive Enhancement, and Social Skills (SUCCESS) | NCE | 8 | 8 | - | 1.5 hours per session | 25 sessions | Group | Social Cognition; Social Skills | 1 |
| Bölte (2002) | - | Quasi | 10 | 5 | 5 | 2 hours per week | 5 weeks | Individual, Computer-Based | Social Cognition | 5 (E:4; D:l), Low |
| Bonete (2014) | Interperson al Problem Solving for Workplace Adaptation Programme | NCE | 100 | 50 | 50 (TDC) | 75 minutes per week | 10 weeks | Group | Social Cognition | 1 |
| Cunningham (2016) | RelationshiP Enhancement | RCT | 30 | 19 | 19 | 2 hours per week | 8 weeks | Group | Social Skills | 5, Moderate |
| Eack (2013) | Cognitive Enhancement Therapy | NCE | 14 | 14 | - | 60–75 minutes per week | 18 month s | Individ ual, Compu ter-Based and Group | Social Cognition | 1 |
| Eack (2017) | Cognitive Enhancement Therapy | RCT | 54 | 21 | 20 | 90 minutes per week | 18 months | Individual, Computer-Based and Group | Social Cognition | 5, Moderate |
| Eckman (2015) | Cognitive Behavioral Therapy with Visualization | NCE | 18 | 18 | - | 45–60 minutes per session | 15 sessions | Individual | Social Anxiety | 1 |
| Faja (2008) | - | Quasi | 10 | 5 | 5 | 30–60 minutes per session | 8 sessions | Individual, Computer-Based | Social Cognition | 9 (E:8; D:1), Low |
| Faja (2012) | STAART | NCE | 13 | 13 | - | NR | 5–8 sessions | Individual, Computer-Based | Social Cognition | 1 |
| Fullerton (1999) | Putting Feet on My Dreams | NCE | 23 | 23 | - | 2–3 hours per session | 10 sessions | Group | Social Skills | 1 |
| Gantman (2011) | PEERS® for Young Adults | RCT | 17 | 9 | 8 | 90 minutes per week | 14 weeks | Group | Social Skills | 2.5, Weak |
| Golan (2006) | - | Quasi | 31 (Exp 1); 26 (Exp 2) | 19 (Exp 1); 13 (Exp 2) | 22 (Exp l); 13 (Exp 2) | 2 hours per week | 10 weeks | Individual, Computer-Based | Social Cognition | 10.5 (E:8; D:2.5), Low |
| Hesselmark (2014) | Cognitive Behavioral Therapy (CBT) | RCT | 68 | 34 | 34 | 3 hours per week | 36 weeks | Group | Social Cognition; Social Skills | 6, Strong |
| Hillier (2007) | Aspiration Program | NCE | 49 | 49 | - | 60 minutes per week | 8 weeks | Group | Social Skills | 1 |
| Hillier (2011) | Aspiration Program | NCE | 13 | 13 | - | 60 minutes per week | 8 weeks | Group | Social Skills | 1 |
| Howlin (1999) | - | NCE | 10 | 10 | - | 2.5 hours per month | 12 months | Group | Social Skills | 1 |
| Kandalaft (2012) | Virtual Reality Social Cognition Training | NCE | 8 | 8 | - | 60 minutes twice a week | 5 weeks | Individual, Computer-Based | Social Cognition; Social Skills | 1 |
| Kiep (2014) | Mindfulness-Based Therapy for Individuals on the Autism Spectrum | NCE | 50 | 50 | - | 2.5 hours per week | 9 weeks | Group | Social Anxiety | 1 |
| Koch (2014) | Dance Movement Therapy | Quasi | 31 | 16 | 15 | 60 minutes per week | 7 weeks | Group | Social Skills; Social Cognition | 13 (E:9, D:4), High |
| Koegel (2013) | - | NCE | 3 | 3 | - | 60 minutes per week | 33 weeks | Individual | Social Skills | 1 |
| Koegel (2015) | - | NCE | 5 | 5 | - | 10 minutes per week | 4–8 weeks | Individual | Social Skills | 1 |
| Koegel (2016) | - | NCE | 3 | 3 | - | 40 minutes per week | 5–9 weeks | Individual | Social Skills | 1 |
| Koehne (2015) | Imitation and Synchroniz ation Based Dance / Movement | Quasi | 51 | 27 | 24 | 90 minutes per session | 10 sessions | Group | Social Cognition | 12 (E:9; D:3.5), Acceptable |
| Laugeso n (2015) | PEERS® for Young Adults | RCT | 22 | 12 | 10 | 90 minutes per week | 16 weeks | Group | Social Skills | 2.5, Weak |
| Lovett (2014) | - | NCE | 3 | 3 | - | 30–45 minutes , 1–3 sessions per week | 4–6 weeks | Group | Social Cognition | 1 |
| Mason (2012) | - | NCE | 2 | 2 | - | 50 minutes , 2 sessions per week | weeks | Group, Video Modeling | Social Skills | 1 |
| McGillivray (2014) | Think Well, Feel Well, and Be Well | Quasi | 32 | 26 | 16 | 2 hours per week | 9 weeks | Group | Social Anxiety | 14 (E:9, D:5), High |
| McVey (2016) | PEERS® for Young Adults | RCT | 53 | 29 | 24 | 90 minutes per week | 16 weeks | Group | Social Skills | 3, Weak |
| Morgan (2014) | Interview Skills Curriculum | RCT | 24 | 12 | 12 | 90 minutes per week | 12 weeks | Group | Social Skills | 3.5, Weak |
| Palmen (2008) | - | NCE | 9 | 9 | - | 60 minutes per week | 3 weeks | Group | Social Skills | 1 |
| Pugliese and White (2013) | Problem Solving Skills 101 | NCE | 5 | 5 | - | 1 session per week | 9 weeks | Group | Social Cognition | 1 |
| Retherford (2015) | Camp Campus | NCE | NR | NR | - | 15 hours/day | 1 week | Group | Social Cognition; Social Skills | 1 |
| Saban-Bezalel (2015) | - | RCT | 51 | 16 | 13 (ASD);22 (TDC) | 30–45 minutes per week | 5 weeks | Group | Social Cognition | 2, Weak |
| Sizoo (2017) | CBT and Mindfulness Based Stress Reduction | Quasi | 59 | 27 (CBT) | 32 (MBSR) | 90 minutes per week | 13 weeks | Group | Social Anxiety | 11, (E:7; D: 4), Low |
| Smith (2014) | Virtual Reality Job Interview Training (VR-JIT) | RCT | 26 | 16 | 10 | 10 hours over 5 sessions | 2 weeks | Individual, Computer-Based | Social Skills | 4, Modera te |
| Spain (2017) | Group CBT | NCE | 14 | 14 | - | 2 hours per week | 11 weeks | Group MeetingS | Social Anxiety | 1 |
| Spek (2013) | - | RCT | 41 | 20 | 21 | 2.5 hour weekly sessions | 9 weeks | Group | Social Anxiety | 4, Moderate |
| Strickland (2013) | Job TIPS | Quasi | 22 | 11 | 11 | Varied | 10 days | Individual, Computer-Based | Social Skills | 8.5 (E:7; D:1.5), Low |
| Trepagnier (2011) | - | NCE | 16 | 16 | - | 2 sessions | 2 weeks | Individual, Computer-Based | Social Skills | 1 |
| Turner-Brown (2008) | Social Cognition and Interaction Training for HFA Adults (SCIT-A) | Quasi | 11 | 6 | 5 | 50 minutes per week | 18 weeks | Group | Social Cognition | 10 (E:7.5; D:2.5), Low’ |
| White (2016) | Brain-Computer Interface for ASD (BCI-ASD) | RCT | 8 | 4 | 4 | 40 minutes per week | 10–14 sessions | Individual, Computer-Based | Social Cognition; Social Skills; Social Anxiety | 4, Moderate |
Design: RCT randomized controlled trial, Quasi quasi-experimental, NCE non-controlled experiment. NR indicates information was not reported, and “–” indicates the absence of a component described in the column header
All intervention studies were carried out in clinic / university settings, with the exception of the SUCCESS program
The quality of all RCT and quasi articles was assessed using published methodological rating scales as described in Kasari et al. (23). The American Academy of Cerebral Palsy and Developmental Medicine scale was used to assess RCTs by examining participant inclusion criteria, intervention description, measurement, attrition, and analyses. The scale provides an overall rating of ‘weak’ (0–3 points), ‘moderate’, or ‘strong’ (23). Quasi articles were also rated using a scale by Gersten and colleagues (23, 24) that assesses 18 “essential” and “desirable” quality indicators (related to description of participants, implementation of intervention, validity of outcome measures, and data analysis), and provides an overall summary rating of “acceptable” or “high” quality (24). Our review refers to studies not meeting either acceptable or high ratings as “low” quality (Kasari et al., 2014). Finally, NCE articles were rated using a scale that Sackett and colleagues developed to determine the effectiveness of medical interventions (25) based on the quality of the evidence provided. The scale rates interventions at five different levels, the lowest of which is reserved for case series or studies with no controls (25).
All studies were rated by both the first and second authors. Inter-rater reliability (IRR) of these 2 authors, calculated by dividing total number of coded items by the number of agreements (i.e. when each rater agreed within a score of one), was 0.89. Final ratings presented in Table 1 are the average of each rater’s scores. Studies were also assessed to determine which component(s) of social functioning that each intervention targeted. Meta-analytical approaches were not conducted due to the methodological and clinical heterogeneity among all studies.
Results
Search Findings
Initial search terms (see Supplementary Material) yielded 1574 articles (Figure 1). Our process for screening and excluding articles based on our inclusion / exclusion criteria is illustrated in Figure 1. Forty-one studies met our inclusion criteria.
Summary of Methodological Quality
RCT
According to the AACPDM scale, five of the RCT studies were of weak quality (26–30), five were of moderate quality (31–35), and only one was of strong quality (36) (Table 1). Many of the weak quality RCT interventions lacked description of the reliability and validity of their outcome measures, indication of blind assessor, power calculations, and/or reported dropout rate. One study did not provide a well-described randomized assignment procedure (28).
Quasi
The majority of quasi-experimental interventions (37–42) were of low quality, as determined by the criteria of Gersten and colleagues (23, 24) (Table 1). One study was rated as acceptable quality (43) and the remaining two studies were deemed of high quality (44, 45). Many of the low-quality quasi interventions were lacking evidence of reliability and validity of each outcome measure, measures of inter-rater reliability, and/or description of how implementation fidelity was assessed.
Non-Controlled
The 21 non-controlled papers (12, 46–65) all received a very weak rating of 1 on the Sackett 1989 scale (Table 1), primarily because they did not have a control group.
Summary of Treatment Targets and Outcomes
The identified studies varied with regard to which domain(s) of social functioning was directly targeted by the intervention. The majority of the articles described programs targeting social cognition (n=12; (28, 34, 37–39, 42, 43, 47–49, 57, 63)) or social skills (n=17; (26, 27, 29, 30, 33, 35, 40, 46, 50–52, 54–56, 58, 60, 62)). Six studies targeted social anxiety, (31, 41, 44, 61, 64, 65) and only six studies specifically targeted more than one domain of social functioning (12, 32, 36, 45, 53, 59). No studies targeted social motivation as their primary treatment target, which is striking, given recent data on the importance of this component (13–15); however, some studies used assessments of motivation and anxiety as primary or secondary outcome measures (52, 56).
Interventions Targeting Social Cognition and Broader Cognitive Skills
Twelve interventions (28, 34, 37–39, 42, 43, 47–49, 57, 63) focused on improving social cognition. The interventions targeted a variety of sub-domains within social cognition that are challenging for many adults with ASD (e.g. face recognition, emotion recognition, perspective taking).
Face recognition was targeted by two studies and used a combination of explicit rule-based instruction and practice labeling characteristics of faces vs. objects (42, 49). In both studies, the test group and control group significantly improved after training, while in one study, the test group showed significantly greater sensitivity to certain stimuli than the control group (42). Both studies suggest that face processing ability and strategies can be significantly improved through training. However, self-report measures of training experiences revealed that 64% of participants reported no change in social functioning (49), suggesting that participation in face processing training alone may not be sufficient to improve social functioning in the community.
Three studies addressed emotion recognition/inference as their primary treatment target (37, 38, 43). The interactive guide, Mind Reading (66) and a computer-based program (38) were used to teach emotion recognition and identification in faces and voices. Users of both programs demonstrated significant improvement on closely related tasks of complex emotion recognition as compared to the respective control group, but this improvement did not carry over to more distant generalization tasks of mental state recognition. Koehne and colleagues used a dramatically different approach to fostering emotion inference and empathic feelings by evaluating the efficacy of dance/movement intervention (SI-DMI), compared to a control movement intervention (CMI) (43). Participants treated with SI-DMI, which focused on interpersonal movement imitation and synchronization skills, showed significantly larger improvement in emotion inference, but not empathic feelings, than the control group.
Two studies evaluated the effect of interventions targeting the identification of social cues and the use of perspective taking skills (39, 57). Lovett and Rehfeldt implemented multiple exemplar instruction to effectively teach perspective taking skills (57). However, findings showed varying degrees of generalization of skills to more natural social interactions (57). In contrast, Turner-Brown et al. 2008 tested the utility of a group-based cognitive behavioral intervention to improve social cognition in adults with ASD, Social Cognition and Interaction Training for Adults (SCIT-A; (39)). SCIT-A included didactic sessions focusing on three aspects of social cognition: emotion recognition, directing attention in social interactions, and perspective taking. Intervention participants demonstrated significant improvements on primary outcomes measures of face emotion identification and theory of mind as compared to the treatment as usual control group of adults with ASD. Yet, the groups did not differ significantly on a more general measure of social communication skills.
Five studies targeted broader cognitive skills relevant to social functioning as their main treatment focus. Two studies (34, 48) used the same cognitive therapy intervention to treat general impairments in social and non-social information processing and problem solving, called Cognitive Enhancement Therapy (CET). CET combines computer-based neurocognitive training on improving cognition (e.g. processing speed, sustaining attention, increasing cognitive flexibility, managing frustration, etc.) with a structured social-cognitive group curriculum focused on perspective taking, managing emotion, etc. Participants demonstrated significant levels of improvement in composite indices of all four cognitive and behavioral domains assessed (i.e. neurocognition, cognitive style, social cognition, and social adjustment) (48) and were more likely to gain competitive employment than their counterparts in the control group (34). Two similar group-format, manual-based interventions targeted social problem-solving skills in the workplace (47) and in the college setting (63). Both interventions demonstrated significant improvements on a task of social problem-solving skills for some participants (47, 63). Finally, Saban-Bezalel and colleagues tested the effectiveness of a short-term intervention in enhancing the comprehension of irony (28). This specialized intervention included video clips, short stories, and comic strips to teach the recognition of ironic expression and was effective in improving comprehension of irony as well as modifying the pattern of hemispheric processing of irony in the brain.
Interventions Targeting Social Skills
The category of behavior most commonly targeted in the identified studies (n=17) was social skills. The category of “social skills” in itself encompasses a host of different skills. While the majority of these social skills studies reported improvement post-intervention, many of the studies used qualitative data only.
Five studies focused on training specific aspects of conversation. These included skills related to forming and asking relevant and appropriately timed questions (58), reducing use of negative statements (56), forming and employing empathetic responses (55), and maintenance of reciprocal conversation (60, 62). Three out of the five studies employed an applied behavior analysis-style multiple-baseline approach, which included opportunities to practice discrete elements of conversation prior to training (baseline), during training, and during follow-up. Only one study employed a small group design (58) while the rest used a single subject design (55, 56, 60, 62). The majority of these interventions had moderate to substantial success in improving the targeted skills and showed varying degrees of successful maintenance of skills at follow-up. However, a lack of group-based statistical analysis of data from most of the studies limits our understanding of the significance of improvements at a group level. In addition, the lack of generalization data and considerably varied maintenance data provide only limited support for the notion that teaching discrete basics of conversation alone generalizes to the improvement of conversation in natural settings.
Five studies tested the efficacy of an intervention specifically focused on improving relational skills and engagement with peers. Three papers (26, 27, 29) evaluated the effectiveness of The Program for the Education and Enrichment of Relational Skills (PEERS), a caregiver-assisted social skills program for adolescents with ASD but adapted for young adults. Participants attended weekly group sessions while caregivers attended separate concurrent sessions. The primary goal of the intervention was to provide instruction and rehearsal of social skills specifically related to building and maintaining peer relationships. In the original randomized controlled pilot study (26), participants reported significantly less loneliness, improved social skills and social skills knowledge, and increased frequency of get-togethers as compared to the wait-list control group (26), the last three of which were replicated in the RCT study (27). Similar results were replicated in a third study, which also indicated improvements in self-reported social anxiety (29). Koegel and colleagues used a multiple baseline design and individual weekly intervention sessions to focus on social planning related to each participant’s interests. Participants worked on concrete organizational skills (e.g. using a planner, inviting peers to activities) that would enable them to engage socially (54). Participants reported attending more social events, as well as a higher quality of life and greater satisfaction with their college experience and peer interactions. Secondary improvements in grade point averages and successes with employment suggested generalization of skills to other areas of functioning. Finally, Cunningham and colleagues focused on improving social skills useful for navigating romantic relationships (33). Participants in the intervention, Ready for Love, demonstrated improvement on select social skills and empathy (33).
Five studies evaluated the effectiveness of training programs targeting social-vocational skills such as job interview skills (30, 35, 40, 51, 52). Two studies used computer-based training programs that included Theory of Mind (ToM)-based instructional training, video models, visual supports, and virtual reality practice job interviews (35, 40). The remaining three studies employed traditional group therapy sessions (30, 51, 52). Three studies utilized interventions that emphasized training on job interview-related social skills, such as answering interview questions, conveying oneself as dependable, closing the interview, and following-up with interviewers. (30, 35, 40). They implemented independently-coded mock interviews as primary outcomes measures, which revealed significant improvement in skills in the treatment group relative to the control group across all three studies. However, distal outcome measures, such as social adaptive behaviors and depressive symptoms, were not significantly different across groups in one study (30). The remaining two studies tested The Aspiration Program, a social and vocational skills support group (51, 52). Examples of program topics include employment goals, friendship development, skills for navigating social gatherings, and general problem solving (51). Out of the self-report measures evaluating appraisal of peer relations, ASD traits, and empathy, only a measure of empathy (67) was significantly improved post-intervention (51). The Aspiration Program also resulted in significantly reduced anxiety and depression in participants post-program (52). This intervention was noteworthy for its evaluation of multiple domains of social functioning across studies.
Interventions Targeting Social Anxiety
Six studies directly focused their intervention efforts on reducing social anxiety, depression, and/or avoidance behavior in adults with ASD (31, 41, 44, 61, 64, 65). Three studies used cognitive behavioral therapy (CBT) as their treatment strategy, in order to reduce symptoms of stress, social anxiety, depression, and/or avoidance behavior (44, 64, 65). Two studies used mindfulness-based therapy to target anxiety (31, 61), while the final study directly compared CBT and mindfulness-based stress reduction (MBSR) in reducing anxiety and depression (41).
Each CBT-based intervention demonstrated decreases in target symptoms, to varying degrees. The more traditional CBT intervention targeting depression and stress saw significantly reduced self-reported scores as compared to the waitlist control group (44). The second CBT-based intervention incorporated visualization as a technique to illustrate the “invisible code of social interaction and communication” (65), while the third intervention used a combination of social skills training and CBT techniques in order to target concurrent social anxiety symptoms (64). Both mindfulness-based therapies used an intervention adapted for autistic adults, Mindfulness-Based Therapy-AS (MBT-AS) and demonstrated significant reductions in symptoms of anxiety and depression (31, 61). MBT-AS also led to an increase in positive affect and reduced rumination (31) as well as a reduction in symptoms of agoraphobia and somatization (61). Finally, results from Sizoo & Kuiper (2017) indicate that both MBSR and CBT were associated with reductions in anxiety and depressive symptoms, effects maintained at follow-up, but with no significant differences in efficacy of the two treatments (41).
Interventions Targeting Multiple Domains of Social Functioning
Of the 41 studies that we identified, only 6 directly targeted more than one component of social functioning in their intervention protocol (12, 32, 36, 45, 53, 59). A few studies were unique in their methodology, such as Kandalaft and colleagues who used virtual reality technology to provide an opportunity for participants to engage in realistic social scenarios and receive performance feedback, in addition to receiving training on social cognition concepts (53). White and colleagues also employed technological strategies via a novel computer-assisted intervention, which incorporates both CBT and mindfulness-acceptance based approaches to target social competence (i.e., social cognition and social skills) and self-regulation (including social anxiety/emotion regulation) (32). Finally, Koch and colleagues tested a dance movement therapy intervention targeting the improvement of attunement, which they hypothesized would lead to increased well-being, social cognition, and social skills (45). Hesselmark and colleagues tested the efficacy of CBT in targeting quality of life outcomes as well as measures of cognition and skills (36). The remaining two studies evaluated interventions based in community-settings, such as a vocational training program for software testing (12) and a college campus camp experience (59).
The CBT and dance movement therapy interventions demonstrated significant improvement in quality of life (36), well-being, and social skills (45) in participants post-intervention. White and colleagues’ computer-assisted intervention resulted in inconsistent behavioral outcomes across their small sample size (32), while Retherford and collegues’ college campus intervention showed the weakest findings by only reporting parent and student survey data describing their experience with the program. Baker-Ericzén and colleagues’ SUCCESS intervention resulted in participant employment rates doubling post-intervention, however the authors were cautious to assert causal claims as the intervention was embedded within a vocational training program specifically targeting improved employment rates (12).
Conclusions
Intervention research on social functioning in adults with ASD has been starting to accelerate in recent years, due to emerging recognition of autistic adults and their needs. However, research on intervention programs targeting social functioning in autistic adults is still in early stages of development, with only 41 treatment studies identified that met our inclusion criteria over the past 37 years, of which only 11 were RCTs, including only 1 RCT with strong methodology by AACPDM scale criteria. There is a strong need for more RCTs, which provide the best evidence of treatment effectiveness. Only then can we begin to carry out deeper analysis of the active ingredients of interventions (68).
While our review has been critical of the small number of treatment studies, and less-than-ideal methodological rigor of many studies, we also acknowledge the substantial challenges of carrying out high-quality studies in this field. A first challenge is that social functioning is inherently complex and multifaceted, and therefore not simple to measure. There is a striking lack of well-validated, reliable assessment instruments to measure the components of social functioning in adults with ASD. Many of the available instruments rely on self-report or informant report, rather than more objective measures; few have been developed for adults with ASD specifically; and few have been developed to measure change in response to treatment. Clearly, there is a strong need for development of better assessment instruments in an adult ASD population that have strong psychometric properties and can reliably detect quantitative changes in behaviors or symptoms over the course of treatment. It would be ideal for treatment studies to include measures of all components of social functioning, even for programs not directly targeting each domain, as this could provide better knowledge of how improvement in one component may affect change in other components. It is noteworthy that only 6 of the 41 studies that we identified specifically included primary measures of more than one component of social functioning.
A second major challenge of carrying out high quality treatment studies is the difficulty of promoting generalization of social functioning gains in a uniform way across studies. This is especially difficult given the heterogeneity of functioning among individuals with ASD, as well as the variability of community contexts. In many of the studies reviewed in this paper, participants improved on primary outcome measures that directly assessed knowledge and skills taught in the intervention curriculum. However, many studies did not assess or did not find generalization to social functioning in daily life. This raises an important question of whether, and to what degree, these interventions affect the lives of the participants. It will be important for the field to place greater attention and emphasis on generalization of skills, as well as measuring maintenance and generalization of skills post treatment, to ensure that our treatments are having a positive impact on participants daily lives.
A third challenge is designing studies with sufficient statistical power and relevance to the population. A priority of the field should be larger and more diverse sample sizes, as well as replication studies. Because the 41 studies that we identified had a divergence of treatment methods, modest sample sizes, and most lacked later replications, it is uncertain how many of the reported treatment effects are replicable. Moreover, future studies should include ethnically/socioeconomically diverse sample sizes that include representative groups of autistic adults. While this review has focused on treatments targeting adults without intellectual disability, additional reviews and treatment research are much-needed as well for intellectually disabled adults with ASD. It will be important for investigators to collaborate on treatment studies across sites in order to generate the needed sample size and diversity of participants.
By working together as a field to address these challenges – as well as promoting understanding and acceptance of ASD in the wider society – we can make faster progress toward supporting autistic adults in navigating the social world and empowering these adults to achieve the quality of life that they desire.
Supplementary Material
Funding:
This study was funded by the NIMH (R34MH104407).
Footnotes
Conflict of Interest
Ashley A. Pallathra, Lucero Cordero, Kennedy Wong, and Edward S. Brodkin declare no conflict of interest.
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
† Papers included in this review
* Papers of particular interest and importance, published recently
- 1.Howlin P, Moss P, Savage S, Rutter M. Social outcomes in mid- to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(6):572–81. [DOI] [PubMed] [Google Scholar]
- 2.Howlin P, Moss P. Adults with autism spectrum disorders. The Canadian Journal of Psychiatry. 2012;57(5):275–83. [DOI] [PubMed] [Google Scholar]
- 3.Shattuck PT, Narendorf SC, Cooper B, Sterzing PR, Wagner M, Taylor JL. Postsecondary education and employment among youth with an autism spectrum disorder. Pediatrics. 2012;129(6):1042–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ganz ML. The lifetime distribution of the incremental societal costs of autism. Arch Pediatr Adolesc Med. 2007;161:343–9. [DOI] [PubMed] [Google Scholar]
- 5.Buescher AVS, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatrics. 2014;168(8):721–8. [DOI] [PubMed] [Google Scholar]
- 6.Hurlbutt K, Chalmers L. Adults with autism speak out: perceptions of their life experiences. Autism. 2002;17(2):103–11. [Google Scholar]
- 7.Muller E, Schuler A, Burton BA, Yates GB. Meeting the vocational support needs of individuals with Asperger syndrome and other autism spectrum disorders. Journal of Vocational Rehabilitation. 2003;18(3):163–75. [Google Scholar]
- 8.Shattuck PT, Roux AM, Hudson LE, Taylor JL, Maenner MJ, Trani J-F. Services for adults with an autism spectrum disorder. Canadian Journal of Psychiatry. 2012;57(5):284–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spain D, Blainey SH. Group social skills interventions for adults with high-functioning autism spectrum disorders: A systematic review. Autism. 2015;19(7):874–86. [DOI] [PubMed] [Google Scholar]
- 10.Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2013;43:687–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gates JA, Kang E, Lerner MD. Efficacy of group social skills interventions for youth with autism spectrum disorder: A systematic review and meta-analysis. Clin Psychol Rev. 2017;52:164–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †*12.Baker-Ericzen MJ, Fitch MA, Kinnear M, Jenkins MM, Twamley EW, Smith L, et al. Development of the supported employment, comprehensive cognitive enhancement, and social skills program for adults on the autism spectrum: results of initial study. Autism. 2017;22(1):6–19.Even as prevalence estimates for autism in adulthood have continued to increase, vocational outcomes remain particularly poor for this population. This pilot study investigates the feasibility, acceptability, and initial estimates of outcomes for a newly developed intervention entitled Supported Employment, Comprehensive Cognitive Enhancement, and Social Skills (SUCCESS), a manualized “soft skills” curriculum that targets cognitive and social development in autistic adults.
- *13.Pallathra AA, Calkins ME, Parish-Morris J, Maddox BB, Perez LS, Miller J, et al. Defining behavioral components of social functioning in adults with autism spectrum disorder as targets for treatment. Autism Research. 2018;11(3):488–502.Few studies have evaluated the multidimensional nature of social functioning in autistic adults as a means of identifying treatment targets. This study examined social motivation, social cognition, social skills, and social anxiety in adults with autism spectrum disorder and found varying associations between these behavioral components of social functioning, but relatively robust correlations between social motivation and the other components of social skill and social anxiety. The data suggest that treatments should ideally target the many components of social functioning, particularly including social motivation, which has been relatively neglected in most treatment programs.
- 14.Chevallier C, Kohls G, Troiani V, Brodkin ES, Schultz RT. The social motivation theory of autism. Trends in Cognitive Sciences. 2012;16:231–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *15.Clements CC, Zoltowski AR, Yankowit LD, Yerys BE, Schultz RT, Herrington JD. Evaluation of the social motivation hypothesis of autism: a systematic review and meta-analysis JAMA Psychiatr y 2018;in press.The social motivation hypothesis suggests that individuals with autism spectrum disorder (ASD) find social stimuli less rewarding than typically developing individuals, which leads to downstream effects on the development of social cognition, social skills, and overall functioning in the community. This study evaluated the literature on fMRI studies to examine whether individuals with ASD process rewarding stimuli differently than typically developing individuals and whether previous contradictory findings in the literature might be due to sample characteristics. Results supported the broader hypothesis that individuals with ASD show atypical processing of social and nonsocial rewards.
- *16.Maddox BB, White SW. Comorbid social anxiety disorder in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2015;45(12):3949–60.Social anxiety symptoms commonly co-occur among youth with autism spectrum disorder and without intellectual disability. This study evaluated the co-occurrence of social anxiety disorder in adults with and without ASD, and results illustrated how adults with ASD plus SAD differ from those with ASD without SAD in several key characteristics. This paper suggests that treatments targeting social functioning should include elements to address social anxiety, particularly in those participants with co-occurring SAD.
- 17.Gotham K, Brunwasser SM, Lord C. Depressive and anxiety symptom trajectories from school age through young adulthood in samples with autism spectrum disorder and developmental delay. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54(5):369–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bishop-Fitzpatrick L, Mazefsky CA, Minshew NJ, Eack SM. The relationship between stress and social functioning in adults with autism spectrum disorder and without intellectual disability. Autism Res. 2015;8(2):164–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kennedy DP, Adolphs R. Perception of emotions from facial expressions in high-functioning adults with autism. Neuropsychologia. 2012;50(14):3313–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Volkmar F Understanding the social brain in autism. Developmental Psychobiology. 2011;53:428–34. [DOI] [PubMed] [Google Scholar]
- 21.Baron-Cohen S, Leslie AM, Frith U. Does the autistic child have a “theory of mind”? Cognition. 1985;21:37–46. [DOI] [PubMed] [Google Scholar]
- 22.Reichow B, Steiner AM, Volkmar F. Cochrane Review: Social skills groups for people aged 6 to 21 with autism spectrum disorders (ASD). Evidence-Based Child Health. 2013;8(2):266–315. [DOI] [PubMed] [Google Scholar]
- 23.Kasari C, Shire S, Factor R, McCracken C. Psychosocial treatments for individuals with autism spectrum disorder across the lifespan: New developments and underlying mechanisms. Curr Psychiatry Rep. 2014;16(11):512. [DOI] [PubMed] [Google Scholar]
- 24.Gersten R, Fuchs LS, Compton D, Coyne M, Greenwood C, Innocenti MS. Quality indicators for group experimental and quasi-experimental research in special education. Exceptional Children. 2005;71(2):149–64. [Google Scholar]
- 25.Sackett DL. Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest. 1989;95(2):2S–4S. [PubMed] [Google Scholar]
- †26.Gantman A, Kapp SK, Orenski K, Laugeson EA. Social skills training for young adults with high-functioning autism spectrum disorders: a randomized controlled pilot study. Journal of Autism and Developmental Disorders. 2012;42:1094–103. [DOI] [PubMed] [Google Scholar]
- †27.Laugeson EA, Gantman A, Kapp SK, Orenski K, Ellingsen R. A randomized controlled trial to improve social skills in young adults with autism spectrum disorder: the UCLA PEERS program. Journal of Autism and Developmental Disorders. 2015;45:3978–89. [DOI] [PubMed] [Google Scholar]
- †28.Saban-Bezalel R, Mashal N The effects of intervention in the comprehension or irony and on hemispheric processing of irony in adults with ASD. Neuropsychologia. 2015;77:233–41. [DOI] [PubMed] [Google Scholar]
- †29.McVey AJ, Dolan BK, Willar KS, Pleiss S, Karst JS, Casnar CL, et al. A replication and extension of the PEERS for young adults social skills intervention: examining effects on social skills and social anxiety in young adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2016;46(12):3739–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †30.Morgan L, Leatzow A, Clark S, Siller M. Interivew skills for adults with autism spectrum disorder: a pilot randomized controlled trial. Journal of Autism and Developmental Disorders. 2014;44:2290–300. [DOI] [PubMed] [Google Scholar]
- †31.Spek AA, van Ham NC, Nyklicek I. Mindfulness-based therapy in adults with an autism spectrum disorder: a randomized controlled trial. Research in Developmental Disabilities. 2013;34(1):246–53. [DOI] [PubMed] [Google Scholar]
- †32.White SW, Richey JA, Gracanin D, Coffman M, Elias R, LaConte S, et al. Psychosocial and computer-assisted intervention for college students with autism spectrum disorder: preliminary support for feasibility. Education and Training in Autism and Developmental Disabilities. 2016;51(3):307–17. [PMC free article] [PubMed] [Google Scholar]
- †33.Cunningham A, Sperry L, Brady MP, Peluso PR, Pauletti RE. The Effects of a Romantic Relationship Treatment Option for Adults With Autism Spectrum Disorder. Counseling Outcome Research and Evaluation. 2017;7(2):99–110. [Google Scholar]
- †34.Eack SM, Hogarty SS, Greenwald DP, Litschge MY, Porton SA, Mazefsky CA, et al. Cognitive enhancement therapy for adult autism spectrum disorder: Results of an 18-month randomized clinical trial. Autism Research. 2018;11(3):519–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †35.Smith MJ, Ginger EJ, Wright K, Wright MA, Taylor JL, Humm LB, et al. Virtual reality job interview training in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2014;44(2450–2463). [DOI] [PMC free article] [PubMed] [Google Scholar]
- †36.Hesselmark E, Plenty S, Bejerot S. Group cognitive behavioural therapy and group recreational activity for adults with autism spectrum disorders: a preliminary randomized controlled trial. Autism. 2014;18(6):672–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †37.Golan O, Baron-Cohen S. Systemizing empathy: Teaching adults with asperger syndrome or high-functioning autism to regonize complex emotions using interactive multimedia. Development and Psychopathology. 2006;18(591–617). [DOI] [PubMed] [Google Scholar]
- †38.Bolte S, Feineis-Matthews S, Leber S, Dierks T, Hubl D, Poustka F. The development and evaluation of a computer-based program to test and to teach the recognition of facial affect. International Journal of Circumpolar Health. 2002;61:61–8. [DOI] [PubMed] [Google Scholar]
- †39.Turner-Brown LM, Perry TD, Dichter GS, Bodfish JW, Penn DL. Brief report: Feasibility of social cognition and interaction training for adults with high functioning autism. Journal of Autism and Developmental Disorders. 2008;38:1777–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †40.Strickland DC, Coles CD, Southern LB. JobTIPS: A transition to employment program for individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2013;43:2472–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †41.Sizoo BB, Kuiper E. Cognitive behavioural therapy and mindfulness based stress reduction may be equally effective in reducing anxiety and depression in adults with autism spectrum disorders. Research in Developmental Disabilities. 2017;64:47–55. [DOI] [PubMed] [Google Scholar]
- †42.Faja S, Aylward E, Bernier R, Dawson G. Becoming a face expert: a computerized face-training program for high-functioning individuals with autism spectrum disorders. Developmental Neuropsychology. 2008;33(1):1–24. [DOI] [PubMed] [Google Scholar]
- †43.Koehne S, Behrends A, Fairhurst MT, Dziobek I. Fostering social cognition through an imitation and synchronization-based dance/movement intervention in adults with autism spectrum disorder: a controlled proof-of-concept study. Psychotherapy and Psychosomatics. 2016;85:27–35. [DOI] [PubMed] [Google Scholar]
- †44.McGillivray JA, Evert HT. Group cognitive behavioural therapy program shows potential in reducing symptoms of depression and stress among young people with ASD. Journal of Autism and Developmental Disorders. 2014;44(8):2041–51. [DOI] [PubMed] [Google Scholar]
- †45.Koch SC, Mehl L, Sobanski E, Sieber M, Fuchs T. Fixing the mirrors: a feasibility study of the effects of dance movement therapy on young adults with autism spectrum disorder. Autism. 2015;19(3):338–50. [DOI] [PubMed] [Google Scholar]
- †46.Howlin P, Yates P. The Potential Effectiveness of Social Skills Groups for Adults with Autism. Autism. 1999;3(3):299–307. [Google Scholar]
- †47.Bonete S, Calero MD, Fernández-Parra A. Group training in interpersonal problem-solving skills for workplace adaptation of adolescents and adults with Asperger syndrome: a preliminary study. Autism. 2015;19(4):409–20. [DOI] [PubMed] [Google Scholar]
- †48.Eack SM, Greenwald DP, Hogarty SS, Bahorik AL, Litschge MY, Mazefsky CA, et al. Cognitive enhancement therapy for adults with autism spectrum disorder: results of an 18-month feasibility study. Journal of Autism and Developmental Disorders. 2013;43:2866–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †49.Faja S, Webb SJ, Jones E, Merkle K, Kamara D, Bavaro J, et al. The effects of face expertise training on the behavioral performance and brain activity of adults with high functioning autism spectrum disorders. Journal of Autism and Developmental Disorders. 2012;42(2):278–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †50.Fullerton A, Coyne P. Developing skills and concepts for self-determination in young adults with autism. Focus on Autism and other Developmental Disabilities. 1999;14(1):42–52. [Google Scholar]
- †51.Hillier A, Fish T, Cloppert P, Beversdorf DQ. Outcomes of a social and vocational skills support group for adolescents and young adults on the autism spectrum. Focus on Autism and other Developmental Disabilities. 2007;22(2):107–15. [Google Scholar]
- †52.Hillier A, Fish T, Siegel JH, Beversdorf DQ. Social and vocational skills training reduces self-reported anxiety and depression among young adults on the autism spectrum. Journal of Developmental and Physical Disabilities. 2011;23:267–76. [Google Scholar]
- †53.Kandalaft MR, Didehbani N, Krawczyk DC, Allen TT, Chapman SB. Virtual reality social cognition training for young adults with high-functioning autism. Journal of Autism and Developmental Disorders. 2013;43(34–44). [DOI] [PMC free article] [PubMed] [Google Scholar]
- †54.Koegel LK, Ashbaugh K, Koegel RL, Detar WJ. Increasing socialization in adults with asperger’s syndrome. Psychology in the Schools. 2013;50(9):899–909. [Google Scholar]
- †55.Koegel LK, Ashbaugh K, Navab A, Koegel RL. Improving empathic communication skills in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2016;46(3):921–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †56.Koegel LK, Navab A, Ashbaugh K, Koegel RL. Using reframing to reduce negative statements in social conversation for adults With autism spectrum disorder. Journal of Positive Behavior Interventions. 2015;18(3):133–44. [Google Scholar]
- †57.Lovett S, Rehfeldt RA. An evaluation of multiple exemplar instruction to teach perspective-taking skills to adolescents with asperger syndrome. Behavioral Development Bulletin. 2014;19(2):22–36. [Google Scholar]
- †58.Palmen A, Didden R, Arts M. Improving question asking in high-functioning adolescents with autism spectrum disorder: effectiveness of small-group training. Autism. 2008;12(1):83–98. [DOI] [PubMed] [Google Scholar]
- †59.Retherford KS, Schreiber LR. Camp campus: college preperation for adolescents and young adults with high-functioing autism, asperger syndrome, and other social communication disorders. Topics in Language Disorders. 2015;35(4):362–85. [Google Scholar]
- †60.Trepagnier CY, Olsen DE, Boteler L, Bell CA. Virtual conversation partner for adults with autism. Cyberpsychology, Behavior, and Social Networking. 2011;14(1–2):21–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- †61.Kiep M, Spek AA, Hoeben L. Mindfulness-based therapy in adults with an autism spectrum disorder: Do treatment effects last? Mindfulness. 2014;6(3):637–44. [Google Scholar]
- †62.Mason RA, Rispoli M, Ganz JB, Boles MB, Orr K. Effects of video modeling on communicative social skills of college students with Asperger syndrome. Developmental Neurorehabilitation. 2012;15(6):425–34. [DOI] [PubMed] [Google Scholar]
- †63.Pugliese CE, White SW. Brief report: problem solving therapy in college students with autism spectrum disorders: feasibility and preliminary efficacy. Journal of Autism and Developmental Disorders. 2014;44:719–29. [DOI] [PubMed] [Google Scholar]
- †64.Spain D, Blainey SH, Vaillancourt K. Group cognitive behaviour therapy (CBT) for social interaction anxiety in adults with autism spectrum disorders (ASD). Research in Autism Spectrum Disorders. 2017;41>–42:20–30. [Google Scholar]
- †65.Ekman E, Hiltunen AJ. Modified CBT using visualization for Autism Spectrum Disorder (ASD), anxiety and avoidance behavior--a quasi-experimental open pilot study. Scand J Psychol. 2015;56(6):641–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Baron-Cohen S, Golan O, Wheelwright S, Hill JJ. Mind reading: The interactive guide to emotions. London: Jessica Kingsley; 2004. [Google Scholar]
- 67.Baron-Cohen S, Wheelwright S. The empathy quotient: an investigation of adults with Asperger syndrome or high functioning autism, and normal sex differences. Journal of Autism and Developmental Disorders. 2004;34:163–75. [DOI] [PubMed] [Google Scholar]
- 68.Kasari C, Rotheram-Fuller E, Locke J, Gulsrud A. Making the connection: randomized controlled trial of social skills at school for children with autism spectrum disorders. Journal of Child Psychology and Psychiatry. 2012;53:431–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.