Abstract
Objective:
To determine the characteristics of community-dwelling older adults receiving fall-related rehabilitation.
Design:
Cross-sectional analysis of the fifth round (2015) of the National Health and Aging Trends Study (NHATS). Fall-related rehabilitation utilization was analyzed using weighted multinomial logistic regression with SEs adjusted for the sample design.
Setting:
In-person interviews of a nationally representative sample of community-dwelling older adults.
Participants:
Medicare beneficiaries from NHATS (N = 7062).
Interventions:
Not applicable.
Main Outcomes Measures:
Rehabilitation utilization categorized into fall-related rehabilitation, other rehabilitation, or no rehabilitation.
Results:
Fall status (single fall: odds ratio [OR] = 2.96; 95% confidence interval [CI], 1.52–5.77; recurrent falls: OR= 14.21; 95% CI, 7.45–27.10), fear of falling (OR = 3.11; 95% CI, 1.90–5.08), poor Short Physical Performance Battery scores (score 0: OR = 6.62; 95% CI, 3.31–13.24; score 1–4: OR = 4.65; 95% CI, 2.23–9.68), and hip fracture (OR = 3.24; 95% CI, 1.46–7.20) were all associated with receiving fall-related rehabilitation. Lower education level (less than high school diploma compared with 4-y college degree: OR =.21; 95% CI, .11–.40) and Hispanic ethnicity (OR = .37; 95% CI, .15–.87) were associated with not receiving fall-related rehabilitation.
Conclusions:
Hispanic older adults and older adults who are less educated are less likely to receive fall-related rehabilitation. Recurrent fallers followed by those who fell once in the past year were more likely to receive fall-related rehabilitation than are older adults who have not had a fall in the past year.
Keywords: Accidental falls, Aged, Rehabilitation
Twenty-nine percent of adults older than 65 years fall every year.1,2 Twenty percent of falls result in a serious injury, including fractures and head trauma.2 One third of Medicare beneficiaries who fall seek medical care.3 The Centers for Disease Control and Prevention estimates the annual cost of falls in the United States to be around $31 billion.1 Identifying fall risk factors and effective fall prevention programs has been the primary research focus on falls.4–7 Poor balance and strength, visual impairments, use of medications affecting balance, and fear of falling have all been studied as fall risk factors in older adults.2–4
Effective fall interventions include review and management of medications, optimizing vision, and home modifications delivered by an occupational therapist.8 Extensive research on fall prevention programs for older adults suggests a reduction in the rate of falls after single interventions and multicomponent exercise in-terventions.8 Specifically, Tai Chi has been shown to reduce the risk of falls in community-dwelling older adults.8 Multifactorial interventions, which are tailored to an individual’s risk, also reduce the rate of falls.8 Stopping Elderly Accidents, Deaths and Injuries is a growing effort by the Centers for Disease Control and Prevention to offer guidance for health care providers in fall risk screening, assessment, and intervention.9
Longstanding services such as physical and occupational therapy are shown to increase strength and functional ability, improve balance, and decrease a fear of falling.10,11 Studies10,11 have evaluated rehabilitation services in adults who have had a hip fracture or a stroke. When patients are discharged from a hospital, they are often sent to a skilled nursing facility, an inpatient rehabilitation facility, or home with physical and occupational therapy.12,13 There have been several studies13–17 to address management of falls in skilled nursing homes and inpatient rehabilitation facilities. Research on rehabilitation utilization for falls exists for Asian and European populations; however, much less is known about rehabilitation utilization of community-dwelling adults recovering from falls in the United States.13–17
A recent study18 reported on the characteristics of rehabilitation use in the National Health and Aging Trends Study (NHATS), focusing on rehabilitation services in general but not falls-related rehabilitation. It is uncertain whether recurrent fallers receive more rehabilitation than other older adults, and whether utilization of rehabilitation services for falls specifically varies across demographic groups including race, sex, and socioeconomic status.6
The purpose of this study was to determine the characteristics of those who receive fall-related rehabilitation, using data from NHATS. We hypothesized that fall-related rehabilitation utilization not only depends on whether adults are single or recurrent fallers, but also differs by race, sex, age, and socioeconomic status.
Methods
Population
The NHATS longitudinal cohort study has collected data annually and is sponsored by the National Institute on Aging and conducted by Johns Hopkins Bloomberg School of Public Health.19 Data have been collected since 2011 for a nationally representative sample of Medicare beneficiaries aged ≥65 years in the United States. There are 5 rounds in this longitudinal study to date. Participants were randomly sampled from the Medicare enrollment database and replenished in round 5.20 In both rounds 1 and 5, participants were selected using a stratified 3-stage sample design, with the same primary sampling units used in both rounds and the secondary sampling units selected in the same manner. Each age-race group was sampled at a lower rate in round 5 than the continuing sample.20 A total of 8245 older adults were enrolled in the first round of NHATS. At sample replenishment in round 5, 8334 interviews were completed (4152 subjects enrolled at round 1, and 4182 new subjects enrolled in round 5). The round 5 interview included a new section with questions regarding rehabilitation services.
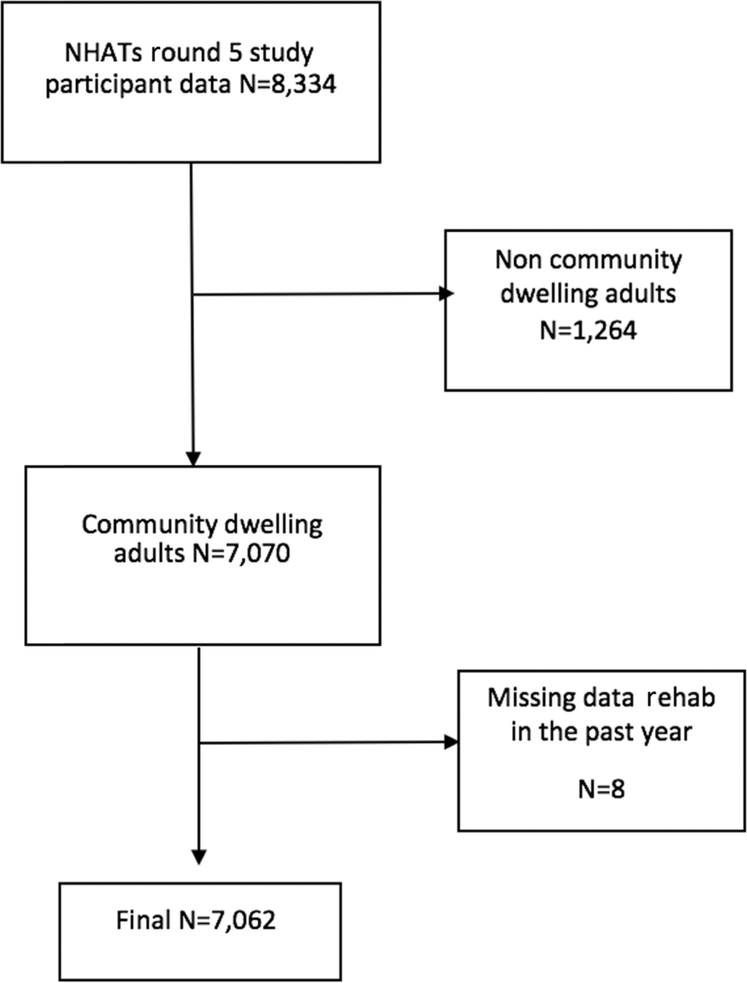
Older adults living in non-nursing home residential care settings or in nursing homes (1264 older adults) were excluded. There were 7070 community-dwelling adults in round 5 of the NHATS study (fig 1). Older adults who did not respond to the question regarding rehabilitation in the past year were further excluded (see fig 1), leaving a study sample of 7062 community-dwelling older adults.
Fig 1.
Population flow diagram.
Demographics
Respondents’ race, sex, and age were collected in the NHATS round 5 survey and used to determine who received fall-related rehabilitation. Education level was recorded in NHATS round 1 for participants followed up since the first round and in round 5 for the replenished sample. Race was categorized into 4 categories: non-Hispanic white, non-Hispanic black, Hispanic, and other. Age of respondents was broken into 5 categories: 65 to 69, 70 to 74, 75 to 79, 80 to 85, and >85 years. Education level was broken into 4 categories: less than high school; high school diploma; some college; and bachelor’s degree or higher. Seventy-five percent of participants either reported their annual income, including retirement, savings, and social security, or picked the category that best fit their annual income. The remaining 25% of missing income was imputed based on answers from other survey questions (see NHATS technical paper 15 for a more detailed explanation21). Income was categorized into 5 categories: less than $33,000 per year; between $33,000 and $43,000; between $43,000 and $66,000; between $66,000 and $109,000; and above $109,000.21
Outcome
Fall-related rehabilitation in the past year was determined by a participant’s response to the question, “Have you received rehabilitation in the past year?” Respondents who answered yes to rehabilitation in the past year were asked specifically for the reason they received rehabilitation and provided with a list of potential options, including to improve problems with falls. Three rehabilitation utilization categories were created: (1) respondents who reported receiving rehabilitation in the past year and specified that this rehabilitation was for improving problems with falls; (2) respondents who reported no rehabilitation in the past year; and (3) respondents who received rehabilitation in the past year but chose a rehabilitation reason other than fall-related problems.
Falls
Falls were categorized into 3 discrete categories: (1) nonfallers in the past year; (2) 1 fall in the past year; and (3) >1 fall in the past year. This was derived from 2 survey questions that asked whether respondents had a fall in the past year (yes/no) and whether respondents had more than 1 fall in the past year (yes/no).
Comorbidities
Comorbidities were self-reported physician-diagnosed conditions: myocardial infarction, cardiovascular disease, hypertension, arthritis, osteoporosis, diabetes, lung disease, stroke, dementia/Alzheimer disease, cancer, or hip fracture.22 Hip fracture and stroke were examined individually because of potential overlap with fall-related rehabilitation. The other comorbidities were added together to create a composite comorbidity score. Each individual received 1 point for each comorbidity reported, not including dementia, hip fracture, or stroke. Dementia was categorized into 3 categories: no dementia, possible dementia, and probable dementia. Because no clinical diagnosis was ascertained in the NHATS cohort, this measure of dementia used reports of diagnoses, a proxy assessment instrument, and scores on 3 different cognitive tests to classify dementia status. Further information regarding this scoring can be found in NHATS technical paper 5.23 Body mass index (BMI) was calculated by dividing current weight by height squared and categorized into 4 categories: underweight (BMI <18.5); normal (BMI between 18.5 and 24.9); overweight (BMI between 25 and 29.9); and obese (BMI ≥30).24
Physical health measures
Other self-reported variables included use of an assistive device (walker, cane, wheelchair, none), mobility disability, problems with balance, and fear of falling. Physical performance was measured by the participant’s score on the Short Physical Performance Battery (SPPB) during the round 5 interview. This battery measures lower extremity functioning and balance and includes repeated chair stands, balance stands, and walking speed, and uses scoring quartiles that are based on the NHATS sample distribution.25 Respondents who were unable to complete the SPPB for safety reasons received a score of 0 for the SPPB. Respondents who were missing the SPPB score for other reasons not involving safety reasons were coded as missing.25
Respondents were asked what their favorite activity was, and these verbatim responses were coded into 52 categories based on those in the American Time Use Study.26 Of these categories, Szanton et al27 selected 12 categories as involving physical activity. In our analysis, routine physical activity was dichotomized into either yes, or no if respondents reported other activities as their favorite. Vision was categorized as follows: wears glasses or contacts; no glasses or contacts; or blind. Living arrangement was dichotomized into lives alone or lives with someone else.
Statistical analysis
All analysis used weighted data. Replicate weights provided for the NHATS sample were used, which employ the modified balance repeated replication method to adjust for variance estimates resulting from the complex survey design.28 Univariate and bivariate analysis of fall-related rehabilitation by the previously mentioned variables (fall status, demographic variables, comorbidities, physical health measures) was conducted using Rao-Scott chi-square tests to account for weights. Variables were assessed for collinearity using Pearson chi-square tests. Multinomial logistic regression was used to model rehabilitation utilization by the characteristics. The multinomial regression model was fitted using Wald tests, due to the weights, to include only variables that were significantly associated with fall-related rehabilitation. Statistical significance was defined by an alpha level of .05. Analysis was conducted using SAS 9.4.a
Results
Table 1 presents the demographic characteristics of the NHATS population in round 5. The survey percentages are reported with their corresponding 95% confidence intervals (CIs) that represent the true percentages in the U.S. population. Overall, about 30% of the cohort was between 65 and 70 years of age. Eighty percent of this cohort identifies as white, non-Hispanic, and 35% makes less than $33,000 per year including retirement funds. Eighty-three percent of the population has at least a high school diploma, and 28% has at least a bachelor’s degree (see table 1). Thirty-four percent of this cohort reported a mobility disability. Twenty-eight percent reported problems with balance, and 26% reported being worried about falling. Sixty-nine percent of participants reported no falls in the past year. Eighteen percent of respondents reported falling once in the past year, and 13% reported recurrent falls in the past year (see table 1).
Table 1.
Characteristics of Medicare beneficiaries, NHATS 2015
| Characteristics | n | % (95% CI)* |
|---|---|---|
| Sex (7062)† | ||
| Male | 3027 | 45 (45–46) |
| Female | 4035 | 55 (54–55) |
| Age (7062) | ||
| 65–69y | 1032 | 30 (29–31) |
| 70–74y | 1722 | 28 (27–29) |
| 75–79y | 1535 | 19 (18–20) |
| 80–84y | 1307 | 12 (12–13) |
| ≥85y | 1466 | 11 (11–11) |
| Race (6890) | ||
| White, non-Hispanic | 4759 | 80 (78–82) |
| Black, non-Hispanic | 1491 | 9 (8–9) |
| Other, non-Hispanic | 208 | 4 (3–5) |
| Hispanic | 432 | 7 (6–9) |
| Income (7062) | ||
| <$33,000 | 3719 | 35 (34–37) |
| $33,000 to <$43,000 | 1097 | 16 (15–17) |
| $43,000 to <$66,000 | 994 | 19 (17–20) |
| $66,000 to <$109,000 | 727 | 16 (15–18) |
| >$109,000 | 525 | 13 (12–15) |
| Education (6900) | ||
| Less than high school diploma | 1521 | 17 (16–18) |
| High school graduate | 1859 | 26 (25–28) |
| Some college | 1805 | 28 (27–30) |
| Bachelor’s degree or advanced degree | 1715 | 28 (26–30) |
| Falls in past year (7053) | ||
| 0 | 4788 | 69 (68–71) |
| 1 | 1293 | 18 (16–19) |
| >1 | 972 | 13 (12–14) |
| Medical | ||
| BMI (6891) | ||
| Underweight | 141 | 2 (1–2) |
| Normal | 2171 | 29 (28–31) |
| Overweight | 2515 | 37 (36–38) |
| Obese | 2064 | 32 (31–33) |
| Heart attack (7049) | 581 | 9 (8–10) |
| Heart disease (7047) | 1439 | 17 (16–19) |
| High blood pressure (7053) | 4989 | 66 (64–67) |
| Arthritis (7053) | 4318 | 56 (55–58) |
| Osteoporosis (7031) | 1697 | 22 (21–23) |
| Diabetes (7054) | 1999 | 26 (25–28) |
| Lung disease (7054) | 1282 | 17 (16–18) |
| Stroke (7049) | 417 | 6 (5–7) |
| Dementia (7055) | ||
| No dementia | 5871 | 89 (88–89) |
| Possible dementia | 715 | 7 (7–8) |
| Probable dementia | 476 | 4 (3–4) |
| Cancer (7062) | 1103 | 18 (17–20) |
| Hip fracture (7059) | 184 | 2 (2–3) |
| Vision (7049) | ||
| Wears glasses/contacts | 4271 | 61 (60–63) |
| Does not wear glasses/contacts | 2737 | 38 (37–40) |
| Blind | 41 | 0 (0–1) |
| Living arrangement (7062) | ||
| Lives alone | 2202 | 27 (26–29) |
| Walking aid (7061) | ||
| None | 4939 | 78 (77–79) |
| Walker/cane | 1652 | 17 (16–18) |
| Wheelchair | 470 | 5 (4–6) |
| SPPB (6513) | ||
| 0 | 490 | 5 (5–6) |
| 1–4 | 1588 | 16 (15–17) |
| 5–8 | 2412 | 34 (32–35) |
| 9–12 | 2023 | 38 (36–39) |
| Mobility disability (7062) | 3051 | 34 (33–36) |
| Routine physical activity (7062) | 3545 | 53 (52–55) |
| Worried about falling (7055) | 2063 | 26 (25–27) |
| Self-reported balance problems (7058) | 2324 | 28 (27–29) |
Abbreviation: CI, confidence interval.
95% CIs represent percentages in weighted data.
Numbers in parenthesis indicate the number of respondents who responded to each question.
Table 2 shows the percentages of rehabilitation utilization for each characteristic. Percentages were reported with 95% CIs around each percentage, representing the estimated percentages in the weighted population. Two demographic characteristics were associated with fall-related rehabilitation utilization in bivariate analysis: 64% of those receiving fall-related rehabilitation were women, and 82% were white non-Hispanic. A number of clinical characteristics were associated with fall-related rehabilitation: (1) 40% were obese; (2) 66% had ≥3 chronic health conditions; (3) 13% had had a stroke; (4) 8% had probable dementia; (5) 6% had a hip fracture; (6) 48% used a cane or walker; (7) 83% reported a mobility disability; and (8) 39% were physically active (see table 2). With regards to fall-specific characteristics, 73% of fall-related rehabilitation participants had a fear of falling, 80% reported balance problems, and 65% reported more than 1 fall in the past year (see table 2). Twenty-seven percent of participants who reported receiving no rehabilitation had at least 1 fall in the past year (see table 2).
Table 2.
Initial characteristics separated by rehabilitation services received
| Characteristics | Fall-Related Rehab in Past Year % (95% CI) |
Other Rehab in Past Year % (95% CI) |
No Rehab in Past Year % (95% CI) |
P From Rao-Scott χ2 |
|---|---|---|---|---|
| Total (n) | 197 | 1138 | 5727 | |
| Sex | ||||
| Male | 36 (28–44) | 41 (38–45) | 46 (46–47) | .0028 |
| Female | 64 (56–72) | 59 (55–62) | 54 (53–54) | |
| Age | ||||
| 65–69y | 16 (8–23) | 27 (25–30) | 31 (30–32) | <.0001 |
| 70–74y | 26 (19–330) | 29 (26–32) | 28 (27–29) | |
| 75–79y | 22 (16–28) | 19 (17–20) | 19 (18–20) | |
| 80–84y | 22 (16–28) | 13 (11–15) | 12 (11–12) | |
| ≥85y | 15 (11–19) | 12 (10–13) | 11 (10–11) | |
| Race | ||||
| White, non-Hispanic | 82 (76–88) | 85 (83–87) | 79 (77–81) | <.0001 |
| Black, non-Hispanic | 7 (4–10) | 7 (6–8) | 9 (8,9) | |
| Other, non-Hispanic | 1 (0–2) | 3 (2–5) | 4 (3–5) | |
| Hispanic | 10 (4–15) | 5 (4–6) | 8 (6–9) | |
| Income | ||||
| <$33,000 | 55 (47–64) | 42 (39–45) | 45 (43–46) | .0099 |
| $33,000 to <$43,000 | 14 (9–19) | 16 (14–18) | 16 (15–18) | |
| $43,000 to <$66,000 | 17 (10–24) | 17 (15–20) | 16 (15–18) | |
| $66,000 to <$109,000 | 7 (3–11) | 14 (11–17) | 13 (12–15) | |
| >$109,000 | 6 (2–11) | 12 (9–14) | 10 (8–11) | |
| Education | ||||
| Less than high school diploma | 16 (10–21) | 13 (11–16) | 18 (16–19) | <.0001 |
| High school graduate | 26 (19–33) | 27 (24–30) | 26 (24–28) | |
| Some college | 28 (20–35) | 25 (23–28) | 29 (27–31) | |
| Bachelor’s degree or advanced degree | 31 (21–40) | 35 (32–38) | 27 (25–29) | |
| Medical | ||||
| BMI | ||||
| Underweight | 7 (2–11) | 2 (1–3) | 2 (1–2) | .0003 |
| Normal | 26 (17–34) | 27 (24–30) | 30 (29–31) | |
| Overweight | 28 (20–36) | 39 (35–43) | 37 (36–38) | |
| Obese | 40 (30–49) | 32 (29–36) | 32 (30–33) | |
| Comorbidities | ||||
| 0–2 | 34 (26–43) | 49 (45–53) | 60 (59–62) | <.0001 |
| ≥3 | 66 (57–74) | 51 (47–55) | 40 (38–41) | |
| Stroke | 13 (8–18) | 9 (7–11) | 5 (4–6) | <.0001 |
| Dementia | 12 (7–17) | 4 (3–5) | 4 (3–4) | <.0001 |
| Hip fracture | 6 (2–10) | 4 (3–5) | 0 | <.0001 |
| Vision | ||||
| Wears glasses/contacts | 62 (53–72) | 64 (61–67) | 61 (59–63) | .1394 |
| Does not wear glasses/contacts | 36 (27–45) | 36 (33–39) | 39 (37–40) | |
| Blind | 1 (0–3) | 0 | 0 | |
| Living arrangement | ||||
| Lives alone | 27 (21–34) | 29 (26–32) | 27 (25–29) | .3708 |
| Walking aid | ||||
| None | 26 (17–34) | 66 (63–69) | 82 (81–83) | <.001 |
| Walker/cane | 48 (39–57) | 25 (22–28) | 15 (14–16) | |
| Wheelchair | 27 (19–34) | 10 (8–11) | 3 (3–4) | |
| SPPB | ||||
| 0 | 19 (13–26) | 9 (7–11) | 5 (4–5) | <.0001 |
| 1–4 | 44 (35–52) | 21 (18–24) | 16 (15–17) | |
| 5–8 | 27 (19–36) | 33 (30–36) | 37 (36–38) | |
| 9–12 | 10 (5–14) | 36 (33–39) | 43 (41,44) | |
| Mobility disability | ||||
| Yes | 83 (77–90) | 46 (43–49) | 31 (29–32) | <.0001 |
| Routine physical activity | ||||
| Yes | 39 (31–48) | 52 (47–56) | 54 (53–56) | .0056 |
| Worried about falling | 73 (65–81) | 34 (31–37) | 23 (22–25) | <.0001 |
| Self-reported balance problems | 80 (73–87) | 36 (33–40) | 25 (23–26) | <.0001 |
| Falls | ||||
| No falls in past 5y | 14 (7–21) | 49 (45–53) | 63 (61–64) | <.0001 |
| History of falls rounds 1—4 | 4 (2–7) | 10 (8–11) | 10 (10–11) | |
| One fall in past year (round 5) | 17 (11–23) | 21 (18–24) | 17 (16–18) | |
| >1 fall in past year | 65 (56–73) | 21 (18–24) | 10 (9–11) | |
NOTE. All percentages are column percentages. The 95% CIs represent percentages in weighted data.
Before modeling, we assessed for collinearity using a correlation greater than 0.4 as the cutoff. Mobility disability, walking aid use, and the SPPB were correlated variables. The SPPB was kept in the model because this measure has been used in numerous studies, while walking aid use and mobility disability were removed.4‘24 Education and income were correlated, as were selfreported balance problems and fear of falling. Education was chosen to remain in the model instead of income. Self-reported balance problems was removed from the model instead of fear of falling because actual balance was measured as part of the SPPB. Stroke, routine physical activity, dementia, weight, vision, and living arrangement were not found to significantly contribute to fall-related rehabilitation utilization and were removed. The final fitted model included self-reported falls, sex, race, fear of falling, hip fractures, age, education, comorbidity count, and the SPPB.
Table 3 presents the results of the fitted multinomial logistic regression model for the outcome: no rehabilitation (referent), fall-related rehabilitation, and other rehabilitation. Our focus was on fall-related rehabilitation compared with no rehabilitation (see table 3, second column). The results for fall-related rehabilitation versus no rehabilitation and other rehabilitation versus no rehabilitation were mostly similar. For the results of other rehabilitation compared with no rehabilitation, refer to table 3. Participants who fell once in the past year had 2.96 (95% CI, 1.52–5.77) times the odds of receiving fall-related rehabilitation versus no rehabilitation compared with someone who had no falls in the past year adjusted for the other variables in the model. The adjusted odds of fall-related rehabilitation versus no rehabilitation for participants who had multiple falls in the past year was 14.21 (95% CI, 7.45–27.10) times the odds of fall-related rehabilitation compared with someone who had not fallen in the past year.
Table 3.
Adjusted association of rehabilitation utilization*
| Category | Fall-Related Rehab Compared With No Rehab OR (95% CI) |
Other Rehab Compared With No Rehab OR (95% CI) |
|---|---|---|
| Falls in past year | ||
| 0 (ref) | NA | NA |
| 1 | 2.96 (1.52–5.77) | 1.45 (1.19–1.75) |
| >1 | 14.21 (7.45–27.10) | 2.08 (1.61–2.69) |
| Sex | ||
| Male (ref) | NA | NA |
| Female | 1.43 (0.95–2.15) | 1.18 (0.97–1.43) |
| Age | ||
| 65–69y (ref) | NA | NA |
| 70–74y | 1.74 (0.75–4.04) | 1.09 (0.86–1.39) |
| 75–79y | 1.84 (0.84–4.02) | 0.99 (0.80–1.23) |
| 80–84y | 2.29 (0.94–5.58) | 1.02 (0.80–1.30) |
| ≥85y | 1.16 (0.50–2.71) | 0.89 (0.69–1.13) |
| Race/ethnicity | ||
| White (ref) | NA | NA |
| African American | 0.89 (0.51–1.57) | 0.72 (0.57–0.91) |
| Hispanic | 0.37 (0.15–0.87) | 0.71 (0.44–1.14) |
| Other | 1.46 (0.64–3.37) | 0.66 (0.49–0.90) |
| Education | ||
| Less than high school | 0.21 (0.11–0.40) | 0.47 (0.35–0.63) |
| High school | 0.40 (0.23–0.70) | 0.63 (0.51–0.78) |
| Some college | 0.51 (0.26–1.01) | 0.59 (0.49–0.72) |
| Bachelor’s or higher (ref) | NA | NA |
| Fear of falling | ||
| Yes | 3.11 (1.90–5.08) | 1.14 (0.92,1.40) |
| No (ref) | NA | NA |
| Hip fracture | ||
| Yes | 3.24 (1.46–7.20) | 2.00 (1.21–3.30) |
| No (ref) | NA | NA |
| SPPB | ||
| 0 | 6.62 (3.31–13.24) | 2.22 (1.53–3.22) |
| 1–4 | 4.65 (2.23–9.68) | 1.44 (1.09–1.91) |
| 5–8 | 2.21 (1.07–4.57) | 1.09 (0.90–1.31) |
| 9–12 (ref) | NA | NA |
| Comorbidities | ||
| 0–2 (ref) | NA | NA |
| ≥3 | 1.29 (0.81–2.06) | 1.41 (1.16–1.71) |
Abbreviations: NA, not applicable; ref, reference.
Multivariable mulitnominal logistic regression of weighted data from the NHATS, 2015.
Sex and age were not significantly related to rehabilitation utilization after adjusting for everything else in the model. Identifying as black non-Hispanic did not seem to be significantly related to fall-related rehabilitation versus no rehabilitation but was related to other rehabilitation versus no rehabilitation (odds ratio [OR] = .72; 95% CI, .57–.91). Those identifying as Hispanic were less likely (OR=.37; 95% CI, .15–.87) to receive fall-related rehabilitation compared with no rehabilitation than those identifying as white non-Hispanic (see table 3).
Higher education was significantly related to utilization of fall-related rehabilitation, as those with less than a high school diploma were less likely to receive fall-related rehabilitation versus no rehabilitation (OR=.21; 95% CI, .11–.40) compared with those with a bachelor’s degree. Participants with a high school diploma were still less likely to receive fall-related rehabilitation versus no rehabilitation than those with at least a bachelor’s degree (OR=.40; 95% CI, .23–.70).
A fear of falling (OR=3.11; 95% CI, 1.90–5.08), hip fracture (OR=3.24; 95% CI, 1.46–7.20), and the SPPB were also associated with fall-related rehabilitation compared with no rehabilitation (SPPB score of 0: OR = 6.62; 95% CI, 3.31 – 13.24; SPPB score of 1–4: OR = 4.65; 95% CI, 2.23–9.68; SPPB score of 5–8: OR = 2.21; 95% CI, 1.07–4.57 compared with those who scored 9–12 on the SPPB). There was less of an association with the SPPB scores for the participants receiving other rehabilitation compared with those receiving no rehabilitation (see table 3). Finally, the number of chronic conditions other than dementia and stroke was not associated with fall-related rehabilitation versus no rehabilitation but was associated with other rehabilitation versus no rehabilitation (OR= 1.41; 95% CI, 1.16–1.71) (see table 3).
Discussion
Hispanics were less likely to receive fall-related rehabilitation than whites. Education played an important role in determining who received fall-related rehabilitation, with participants from lower education levels receiving less fall-related rehabilitation. Not surprisingly, older adults who have experienced 1 or more falls in the past year are more likely to receive fall-related rehabilitation. SPPB score was associated with receiving fall-related rehabilitation, as were fear of falling and hip fracture.
These results are similar to the findings of Freburger et al,13 who found that racial/ethnic minorities and those with lower socioeconomic status were less likely to receive postacute rehabilitation care after hip fractures. Our results are also similar to the those in the study conducted by Chu et al14 in China, where recurrent fallers were found to have the most rehabilitation utilization. However, Chu14 also found that there were no significant differences between fallers and nonfallers for rehabilitation utilization, whereas the results presented here demonstrate a significant difference between these 2 groups. Gell et al18 found differences in overall rehabilitation utilization among racial and ethnic minorities in the NHATS population, so these racial utilization differences are not isolated to fall-specific rehabilitation.
Study limitations
Because this was a cross-sectional analysis we were unable to determine how long adults had been accessing fall-related rehabilitation. Although we were able to ascertain some significant demographic characteristics in the utilization of fall-related rehabilitation, there are likely other important characteristics behind this association that were not measured in the NHATS cohort. For example, distance from a health care provider or specifically from physical and occupational therapy services likely influences who receives fall-related rehabilitation.10 Additionally, older adults may not always tell their physicians when they have had a fall, leaving physicians unable to refer these patients to rehabilitation services.29 This could lead to differential misclas-sification, since older adults who received fall-related rehabilitation have likely admitted to having a fall in the past. Older adults who have not received fall-related rehabilitation might be less likely to report having fallen. Questions regarding falls in the past year have been shown to be affected by recall bias, generally leading to an underestimation of actual falls.30 This cohort is limited to the Medicare population, although about 96% of the U.S. population aged ≥65 years are enrolled. All Medicare enrollees have at least some coverage for rehabilitation services through Medicare, but costs and service limits will vary depending on supplemental coverage. Further research is needed to assess rehabilitation utilization in older adults with or without particular supplemental coverage.
These findings suggest that while recurrent falls obviously play a role in predicting who will receive fall-related rehabilitation, demographic characteristics also play a role in who uses fall-related rehabilitation, even after accounting for falls. Health care providers should work to support and connect patients with social workers or patient navigators to ensure that these patients are adequately utilizing fall-related rehabilitation services. This is especially true of patients from a lower socioeconomic status who may be unaware of the resources that are available to them. Future research should be conducted to determine whether receiving fall-related rehabilitation actually reduces falls in the NHATS cohort, as well as examining why some ethnic minorities are less likely to receive fall-related rehabilitation compared with others.
Conclusions
Recurrent fallers are the most likely to receive fall-related rehabilitation, followed by older adults who have fallen once in the past year. Falls are not the only relevant characteristic of rehabilitation utilization. Older adults with lower levels of education and ethnic minorities are less likely to utilize fall-related rehabilitation.
Acknowledgments
This work was supported in part by a grant from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention to the Center for Injury Epidemiology and Prevention at Columbia University (grant no. 1 R49 CE002096–01). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention. It was also supported in part by the National Health and Aging Trends Study, which is sponsored by the United States Department of Health and Human Services, National Institutes of Health, National Institute on Aging (grant no. NIA U01AG032947) through an agreement with the Johns Hopkins Bloomberg School of Public Health.
List of abbreviations:
- BMI
body mass index
- CI
confidence interval
- NHATS
National Health and Aging Trends Study
- OR
odds ratio
- SPPB
Short Physical Performance Battery
Footnotes
Supplier
a. SAS 9.4; SAS Institute Inc.
Disclosures: none.
References
- 1.Bergen G, Stevens MR, Burns ER. Falls and fall injuries among adults aged ≥65 years—United States, 2014. MMWR Morb Mortal Wkly Rep 2016;65:993–8. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention. Important facts about falls. Available at: http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Accessed October 25, 2016.
- 3.Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the Medicare population: incidence, associated factors, and impact on health care. Phys Ther 2009;89:324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ward RE, Leveille SG, Beauchamp MK, et al. Functional performance as a predictor of injurious falls in older adults. J Am Geriatr Soc 2015; 63:315–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stalenhoef P, Diederiks JP, Knottnerus J, Kester AD, Crebolder HF. A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol 2002;55:1088–94. [DOI] [PubMed] [Google Scholar]
- 6.Hester AL, Wei F. Falls in the community: state of the science. Clin Interv Aging 2013;8:675–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verma SK, Willetts JL, Corns HL, Marucci-Wellman HR, Lombardi DA, Courtney TK. Falls and fall-related injuries among community-dwelling adults in the United States. PLoS One 11:e0150939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;(9):CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention. STEADI (Stopping Elderly Accidents, Deaths, and Injuries): Older adult fall prevention. Available at: https://www.cdc.gov/steadi/. Accessed. [Google Scholar]
- 10.Hauer K, Specht N, Schuler M, Bartsch P, Oster P. Intensive physical training in geriatric patients after severe falls and hip surgery. Age Ageing 2002;31:49–57. [DOI] [PubMed] [Google Scholar]
- 11.Chudyk AM, Jutai JW, Petrella RJ, Speechley M. Systematic review of hip fracture rehabilitation practices in the elderly. Arch Phys Med Rehabil 2009;90:246–62. [DOI] [PubMed] [Google Scholar]
- 12.Buntin MB. Access to postacute rehabilitation. Arch Phys Med Rehabil 2007;88:1488–93. [DOI] [PubMed] [Google Scholar]
- 13.Freburger JK, Holmes GM, Ku LJ. Postacute rehabilitation care for hip fracture: who gets the most care? J Am Geriatr Soc 2012;60:1929–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chu LW, Chiu AY, Chi I. Falls and subsequent health service utilization in community-dwelling Chinese older adults. Arch Gerontol Geriatr 2008;46:125–35. [DOI] [PubMed] [Google Scholar]
- 15.Seematter-Bagnoud L, Wietlisbach V, Yersin B, Bula CJ. Healthcare utilization of elderly persons hospitalized after a noninjurious fall in a Swiss academic medical center. J Am Geriatr Soc 2006; 54:891–7. [DOI] [PubMed] [Google Scholar]
- 16.Stel VS, Smit JH, Pluijm SM, Lips P. Consequences of falling in older men and women and risk factors for health service use and functional decline. Age Ageing 2004;33:58–65. [DOI] [PubMed] [Google Scholar]
- 17.Gilbert R, Todd C, May M, Yardley L, Ben-Shlomo Y. Sociodemographic factors predict the likelihood of not returning home after hospital admission following a fall. J Public Health (Oxf) 2010;32:117–24. [DOI] [PubMed] [Google Scholar]
- 18.Gell NM, Mroz TM, Patel KV. Rehabilitation services use and patient reported outcomes among older adults in the United States. Arch Phys Med Rehabil 2017;98:2221–2227.e3. [DOI] [PubMed] [Google Scholar]
- 19.Kasper JD, Freedman VA. National Health and Aging Trends Study (NHATS) user guide: rounds 1, 2, 3, 4, 5 beta release. Available at: www.NHATS.org. Accessed September 4, 2017. [Google Scholar]
- 20.DeMatteis J, Freedman VA, Kasper JD. National Health and Aging Trends Study round 5 sample design and selection. Baltimore: Johns Hopkins University School of Public Health; 2016. NHATS technical paper no. 16. Available at https://www.nhats.org/scripts/sampleDesign.htm. Accessed September 4, 2017. [Google Scholar]
- 21.DeMatteis JM, Freedman V, Kasper JD. National Health and Aging Trends Study round 5 income imputation. Baltimore: Johns Hopkins University School of Public Health; 2016. NHATS technical paper no. 15. Available at https://www.nhats.org/scripts/TechnicalImputation.htm. Accessed September 4, 2017. [Google Scholar]
- 22.Freedman VA, Kasper JD, Spillman BC. Successful aging through successful accommodation with assistive devices. J Gerontol B Psychol Sci Soc Sci 2017;72:300–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kasper JD, Freedman VA, Spillman B. Classification of persons by dementia status in the National Health and Aging Trends Study. Baltimore: Johns Hopkins University School of Public Health; 2013. Technical paper no. 5. Available at https://www.nhats.org/scripts/TechnicalDementiaClass.htm. Accessed September 4, 2017. [Google Scholar]
- 24.Centers for Disease Control and Prevention Division of Nutrition, Physical Activity, and Obesity. 2017. About adult BMI. Available at: https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Accessed September 4, 2017.
- 25.Kasper JD, Freedman VA, Niefeld MR. Construction of performance-based summary measures of physical capacity in the National Health and Aging Trends Study. Baltimore: Johns Hopkins University School of Public Health; 2012. NHATS technical paper no. 4. Available at https://www.nhats.org/scripts/TechnicalPerfSumMeasure.htm. Accessed September 4, 2017. [Google Scholar]
- 26.Freedman VA, Cornman JC. The panel study of income dynamics, supplement on disability and use of time user guide: release 2009.1. Ann Arbor: University of Michigan, Institute for Social Research; 2009. [Google Scholar]
- 27.Szanton SL, Walker RK, Roberts L, et al. Older adults’ favorite activities are resoundingly active: findings from the NHATS study. Geriatr Nurs 2015;36:131–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.DeMatteis J, Freedman VA, Kasper JD. National Health and Aging Trends Study development of round 5 survey weights. Baltimore: Johns Hopkins University School of Public Health; 2016. NHATS technical paper no. 14. Available at https://www.nhats.org/scripts/TechnicalWeighting.htm. Accessed September 4, 2017. [Google Scholar]
- 29.Lee DC, Day L, Hill K, Clemson L, McDermott F, Haines TP. What factors influence older adults to discuss falls with their health-care providers? Health Expect 2015;18:1593–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ganz DA, Higashi T, Rubenstein LZ. Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. J Am Geriatr Soc 2005;53:2190–4. [DOI] [PubMed] [Google Scholar]