Abstract
Introduction
While a large body of literature suggests that tobacco control legislation—including fiscal measures such as excise taxes—effectively reduces tobacco smoking, the long-run (10+ years) relationship between cigarettes excise taxes and life expectancy has not been directly evaluated. Here, we test the hypothesis that increases in state cigarette excise taxes are positively associated with long-run increases in population-level life expectancy.
Methods
We studied age-standardised life expectancy among all US counties from 1996 to 2012 by sex, in relation to state cigarette excise tax rates by year, controlling for other demographic, socioeconomic and county-specific features. We used an error-correction model to assess the long-run relationship between taxes and life expectancy. We additionally examine whether the relationship between cigarette taxes and life expectancy was mediated by changes to county smoking prevalence and varied by the sex, income and rural/urban composition of a county.
Results
For every one-dollar increase in cigarette tax per pack (in 2016 dollars), county life expectancy increased by 1 year (95% CI 0.60 to 1.40 years) over the long run, with the first 6-month increase in life expectancy taking 10 years to materialise. The association was mediated by changes in smoking prevalence and the magnitude of the association steadily increased as county income decreased.
Conclusions
Results suggest that increasing cigarette excise tax rates translates to consequential population-level improvements in life expectancy, with larger effects in low-income counties.
INTRODUCTION
Identifying policies that can improve life expectancy and reduce income-based and geographic-based inequalities in life expectancy is of major interest.1 Tobacco smoking is a leading preventable risk factor for death in the USA.2 Tobacco control measures—including fiscal measures such as excise taxes—reduce tobacco smoking through reduced smoking initiation and increased smoking cessation.3–10 A major uncertainty is whether cigarette excise taxes improve population-level life expectancy,11 despite widespread smoking and its profound mortality impact.
A significant gap in the literature has been to empirically assess the long-run (10+ years) relationship between cigarette taxes and life expectancy, particularly because a suitable methodological approach to studying the relationship has been elusive. Life expectancy is not expected to change immediately following an increase in tobacco taxation. There is a strong inertial component to life expectancy, as generational cohorts with gradually changing exposures over their life-courses experience gradual attrition from the population, which makes period life expectancy at time t-1 a strong predictor of life expectancy at t, and hence a crucial part of statistically modelling relations between a policy and life expectancy. Additionally, unlike discrete state-level policies, taxes are best measured on a continuous scale (ie, US$/pack, rather than as a dichotomous measure indicating the presence/absence of a tax), and change in multiple years within most states, making analysis difficult through more commonly used methods that assume that the time series are stationary.12 Finally, because life expectancy and state cigarette taxes are both non-stationary, standard regression techniques may lead to spurious correlations.13,14
To overcome these barriers to inference, we use an error-correction model,15 which separately estimates the short-run and long-run associations between an exposure and an outcome when both variables are non-stationary. The short-run relationship reflects the association between a change in cigarette taxes and a change in life expectancy in the following year. Because lagged changes in life expectancy affect future changes, the short-run change sets off a dynamic process such that life expectancy continues fluctuating in subsequent periods. The long-run relationship reflects the association between changes in cigarette taxes and life expectancy after the effects of previous short-run fluctuations die out. We test the hypothesis that increases in cigarette taxes are associated with long-run increases in period age-standardised life expectancy at the county level. We additionally examine whether the relationship between cigarette taxes and life expectancy varies by sex, or by the income level of the county or the rural/urban composition of the county, and whether the relationship is mediated by changes to county smoking prevalence.
METHODS
Study design and reporting was based on the Strengthening the Reporting of Observational studies in Epidemiology Statement, a standardised, evidence-based set of recommendations for reporting observational studies.16
Data
Data on age-standardised life expectancy by sex across all US counties between 1996 and 2012 were obtained from the Institute for Health Metrics and Evaluation (IHME).17 IHME used small-area estimation methods to produce annual life tables and calculate age-specific mortality risk at the county level, by counting de-identified death records collated by the National Centre for Health Statistics, adjusted for population denominator counts from the US Census Bureau. Neither state and local cigarette tax rates were used in the IHME small area estimates for mortality or smoking prevalence, respectively. In a sensitivity analysis, we used data from the Health Inequality Project,18 which derived annual race-adjusted life expectancy estimates at age 40 by gender between 2001 and 2014 from Social Security Administration death records for the 100 most populated commuting zones in the USA.
Data on state cigarette excise taxes (US$ per pack) by year over the same time course were obtained from the US Centers for Disease Control and Prevention State System, Tobacco Legislation Tax Database,19 which we adjusted to 2016 dollars using regional (West, Midwest, Northeast, South) Consumer Price Indices from the Bureau of Labor Statistics.20
Data on annual county and state-level smoking prevalence by sex over the same time course were obtained from the IHME.21 For a sensitivity analysis to help establish a causal interpretation of the results, data on annual county age-standardised mortality rates by cause of death (cardiovascular disease, chronic respiratory disease, cancer and other) over the same time course were also obtained from the IHME.22–24
We merged inflation-adjusted income per capita, population composition (% female, aged under 18 years and over 65 years), racial composition (% black), ethnic composition (% Hispanic) and educational attainment (% completing high school) at the county level for all years of the study from the American Community Survey,25 with missing values linearly interpolated and county urban/rural status from the US Department of Agriculture.26 Per US Department of Agriculture methodology, counties with a population <20 000 residents were considered rural.27
Statistical analysis
Our main specification was a multilevel dynamic panel regression model with fixed effects for county (Stata command ‘xtpmg, dfe’28–33; see Supplementary Materials for details). The dependent variable is county annual life expectancy at birth; the independent variables are state annual cigarette tax rates in 2016 dollars by year, and a set of time-varying county-year covariates on population demographics, educational attainment and income as specified above. We clustered SEs at the state-level using the non-parametric, cluster-robust ‘sandwich’ estimator (Stata option ‘vce(cluster)’) to account for serial correlation in life expectancy over time within counties, intracluster correlation in life expectancy across counties within states and loss of degrees-of-freedom from imputation of covariates.34
Annual life expectancy, smoking prevalence and cigarette taxes each have means, variances and/or covariances that change over time. They follow a unit root autoregressive process and are thus non-stationary variables. When estimating the relationship between two variables that are both non-stationary, standard regression techniques will often find spurious associations.13,14 Cointegration analysis provides a framework for unbiased estimation of the relationship between non-stationary variables, conditional on the assumption that the variables share a common stochastic trend, as captured by the fact that they follow unit root processes.
We used an error-correction model, a type of cointegration analysis, which allows for separate analysis of the short-run and long-run relationships between tobacco taxes and life expectancy. The link between the short-run and long-run relationships is the error-correction term, which allows us to estimate in calendar time the half-life of the long-run response of life-expectancy to a ‘shock’ in the tax rate (calculated as ln (2) times the inverse of the coefficient on the error-correction term (; see Supplementary Materials for details). Hence, the meaning of ‘long-run’ is estimated empirically, allowing the model to indicate to us how long it takes for a tax increase to manifest in an increase in life expectancy.
Further testing and sensitivity analyses were performed to avoid spurious associations between life expectancy (or, in mediator analysis, smoking prevalence) and cigarette taxes, given they are non-stationary variables.13,14 We confirmed there is a cointegrating relationship that ties the stochastic trends of life expectancy (or smoking prevalence) and cigarette taxes together, such that they cannot wander away from each other for an extended period of time.35,36 We additionally checked whether the model’s residuals were normal and stationary, to ensure assumptions for model coefficient interpretation were fulfilled.
In additional analyses, we replaced the dependent variable (life expectancy) with county annual smoking prevalence, to assess whether the observed association between cigarette taxes and life expectancy was plausibly related to changes in smoking prevalence. To further assess the plausibility that the associations we observed reflected causal relationships, we examined the direct relationship between smoking prevalence and life expectancy and the relationship between cigarette taxes and county mortality rates by cause of death. If smoking prevalence acts as an important mediating variable, it should have a statistically significant error-correction term that is more negative (reflecting a shorter half-life of the adjustment process) than the error-correction term for the relationship between cigarette taxes and life expectancy.
In sensitivity analyses, we first examined whether the selection of lag order qualitatively influenced our results. Second, we fit a generalised method of moments dynamic panel estimator developed by Blundell and Bond,37 which relaxes the assumption of strongly exogenous covariates and was designed for small-T, large-N datasets. Third, we restricted analysis to the 43 out of 51 (counting the District of Columbia) states where there is no local government taxation of tobacco.38 Fourth, we included state-year workplace, bar and restaurant smoking restrictions from The National Adult Tobacco Survey39 and 41 other state-year smoking-related policy measures from the Centers for Disease Control and Prevention19 as time-varying covariates in the main analysis. Fifth, we repeated the analysis using annual life expectancy estimates for the 100 most populated US community zones derived from official death records. Sixth, we conducted a falsification test of the association between future, not-yet-announced cigarette taxes (5 years in the future) and current life expectancy and current smoking prevalence.
RESULTS
Cigarette tax changes over time
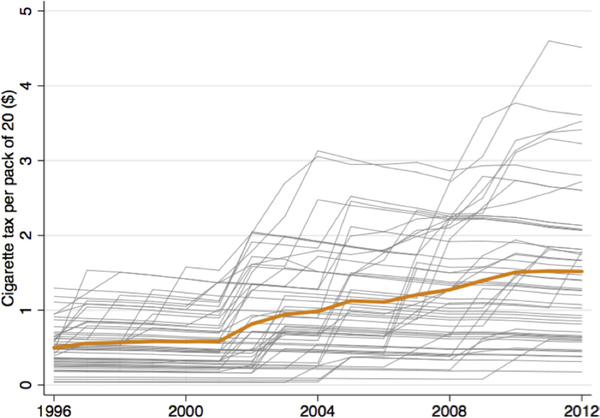
Cigarette taxes increasedd from a national mean of US$0.43 to US$1.19 per pack (in 2016 dollars) between 1996 and 2012 (figure 1), with large variations between states (online supplementary figure S1). States in the Northeast and Western regions generally had higher taxes than those in the Midwest and South, supporting the use of a fixed effects model to account for time-invariant unobserved/unmeasured confounders that differ between states and could otherwise correlate with both cigarette taxes and life expectancy. Consistent with this, there were significant differences in the measured characteristics across counties with above versus below median cigarette taxes during the study period (table 1).
Figure 1.
Average and state-specific trends in state cigarette tax rates, 1996–2012. Inflation-adjusted (2016 dollars) changes in national average (orange) and state-specific cigarette taxes per pack of 20 during the study period.
Table 1.
Demographic characteristics of counties in states with above vs below median cigarette taxes during the study period
|
States where the average cigarette tax during the study period is: |
|||||
|---|---|---|---|---|---|
|
Below the median |
Above the median |
||||
| County-level variable | Mean | (SD) | Mean | (SD) | Std. Diff |
| Cigarette tax (per pack in 2016 dollars) | |||||
| Share female (%) | 0.52 | (0.08) | 0.54 | (0.14) | −0.21 |
| Change<18 years (%) | 0.27 | (0.13) | 0.31 | (0.21) | −0.25 |
| Share>65 years (%) | 0.17 | (0.15) | 0.22 | (0.23) | −0.25 |
| Share black (%) | 0.16 | (0.23) | 0.12 | (0.27) | 0.15 |
| Share Hispanic (%) | 0.04 | (0.06) | 0.17 | (0.29) | −0.63 |
| Share completing high school (%) | 0.78 | (0.09) | 0.83 | (0.09) | −0.56 |
| Income per capita (US$) | 34 836 | (533) | 34 794 | (531) | 0.08 |
Cointegration assumption
Online supplementary figure S2 suggests that life expectancy and cigarette taxes rates share a common trend, making them candidates for belonging to a cointegrating relationship. Panel data unit root tests confirmed life expectancy and cigarette tax rates are non-stationary in level and stationary for the first difference (online supplementary table S1). Using the Johansen cointegration test on the time series of annual life expectancy and cigarette taxes averaged across states, we rejected the null hypothesis of no cointegrating equations at the 1% level for rank=0 and failed to reject the null hypothesis of no cointegrating equations at the 5% level for rank=1. Using the Johansen cost-integration test for each county, in 97% of counties we rejected the null hypothesis of no cointegrating equations at the 1% level for rank=0 and failed to reject the null hypothesis of no cointegrating equations at the 5% level for rank=1 (Stata command ‘vecrank’40); this was also confirmed using the panel cointegration tests developed by Westerlund41 (Stata command ‘xtwest’42). Finally, a regression of life expectancy on cigarette taxes produced normally distributed and stationary residuals (online supplementary figure S3 and table S1).
Lag-order selection
We based lag order selection on the distribution of Akaike information criterion statistics for vector autoregressions of order 1–5 for each county (Stata command ‘ardl’43). Across counties, the optimal lag order had a mean of 3.27, indicating a model of lag order three was the most parsimonious.
Speed of adjustment to equilibrium
For life expectancy, the estimated coefficient of the error-correction term was −0.07 (95% CI −0.09 to −0.05) (table 2). The negative sign is consistent with a stable long-run equilibrium relationship between cigarette taxes and life expectancy. The magnitude indicates that the half-life of the adjustment process back to the long-run relationship between cigarette taxes and life expectancy after a short-run fluctuation (the time it takes for half of the complete adjustment back to the long run to take place) was 9.90 years (95% CI 7.70 to 13.86 years; equal to ). For smoking prevalence, the coefficient was −0.21 (95% CI −0.24 to −0.17), indicating the half-life of the adjustment to the long-run relationship between cigarette taxes and smoking prevalence was 3.30 years (95% CI 2.89 to 4.08 years).
Table 2.
Long-run association of cigarette tax and county-level life expectancy
| County-level life expectancy (years) | |||
|---|---|---|---|
| Variables | Overall | Male | Female |
| Cigarette tax (long run) (US$/pack) | 1.00 | 1.17 | 0.81 |
| (95% CI) | (0.61 to 1.39) | (0.68 to 1.66) | (0.52 to 1.10) |
| Speed of adjustment | −0.07 | −0.07 | −0.10 |
| (95% CI) | (−0.09 to –0.05) | (−0.09 to –0.05) | (−0.12 to –0.08) |
| Lag 1 of life expectancy (years) | −0.14 | −0.29 | −0.16 |
| (95% CI) | (−0.16 to –0.12) | (−0.31 to –0.27) | (−0.20 to –0.12) |
| Lag 2 of life expectancy (years) | 0.05 | −0.08 | 0.11 |
| (95% CI) | (0.03 to 0.07) | (−0.10 to –0.06) | (0.09 to 0.13) |
| Lag 3 of life expectancy (years) | 0.00 | −0.05 | 0.09 |
| (95% CI) | (−0.02 to 0.02) | (−0.07 to –0.03) | (0.07 to 0.11) |
| Δ Cigarette taxt (short run) (US$/pack) | −0.01 | −0.02 | −0.01 |
| (95% CI) | (−0.07 to 0.05) | (−0.08 to 0.04) | (−0.05 to 0.03) |
| Share female (%) | 0.46 | −0.62 | 0.07 |
| (95% CI) | (−0.79 to 1.71) | (−2.11 to 0.87) | (−0.79 to 0.93) |
| Share under 18 (%) | −0.11 | −0.21 | 0.16 |
| (95% CI) | (−0.64 to 0.42) | (−0.90 to 0.48) | (−0.39 to 0.71) |
| Share over 65 (%) | 0.32 | 0.28 | 0.53 |
| (95% CI) | (0.05 to 0.59) | (−0.03 to 0.59) | (0.20 to 0.86) |
| Share black (%) | −2.40 | −2.64 | −1.58 |
| (95% CI) | (−3.83 to –0.97) | (−4.52 to –0.76) | (−2.72 to –0.44) |
| Share Hispanic (%) | −0.10 | −0.12 | −0.06 |
| (95% CI) | (−0.14 to –0.06) | (−0.16 to –0.08) | (−0.10 to –0.02) |
| Share completing high school (%) | 0.46 | 0.29 | 0.09 |
| (95% CI) | (−0.01 to 0.93) | (−0.16 to 0.74) | (−0.22 to 0.40) |
| Income per capita (US$) | 0.00 | 0.00 | 0.00 |
| (95% CI) | (0.00 to 0.00) | (0.00 to 0.00) | (0.00 to 0.00) |
| Constant | 5.44 | 5.15 | 7.72 |
| (95% CI) | (4.09 to 6.79) | (3.86 to 6.44) | (6.05 to 9.39) |
| Observations | 59 660 | 59 660 | 59 660 |
Changes in life expectancy from the main regression analysis with adjustment for county-year income per capita, share female, share black, share over 65, share under 18 and share with high school, and fixed effects for county. 95% CIs reflect Huber-White robust SEs clustered at the state level. Positive values represent increases in life expectancy. Cigarette tax dollars are inflation-adjusted to 2016 year dollars. Speed of adjustment to the long-term equilibrium, or the error-correction speed, is a direct estimate of the speed at which county life expectancy returns to equilibrium after any disturbance from long-run cointegrating relationship.
Long-run (cointegrating) relationship with life expectancy
Overall
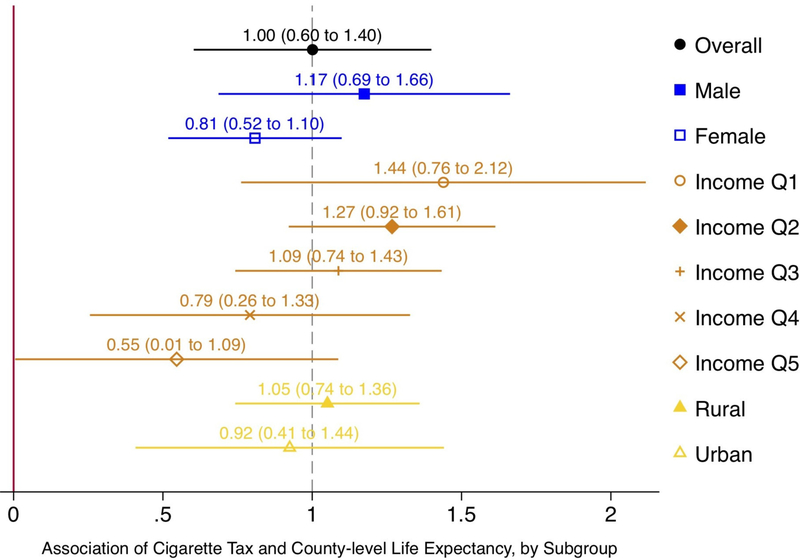
A one-dollar increase in the cigarette tax per pack of 20 cigarettes was associated in the long run with an increase in life expectancy of 1.00 years (95% CI 0.60 to 1.40; figure 2, table 2; Stata command ‘xtpmg, dfe’,29 see Supplementary Materials for derivation of the long-run coefficient). Formulating the same linear model in logs rather than levels, by replacing the dependent variable with the log of life expectancy and main predictor with the log of cigarette taxes, yielded an elasticity of 0.01 (95% CI 0.01 to 0.02) (online supplementary table S2), suggesting a doubling in cigarette taxes per pack (a 100% increase from a mean of US$0.80 to US$1.60) increases life expectancy by 1% (equal to 0.77 years). The error correction model’s residuals were normal and stationary for both specifications (online supplementary table S2 and figure S4).
Figure 2.
Long-run association of cigarette taxes and county-level life expectancy. Long-run changes in life expectancy at the county level by subgroup from the main regression analysis with adjustment for county-year income per capita, share female, share black, share over 65, share under 18 and share with high school, and fixed effects for county. 95% CIs reflect Huber-White robust SEs clustered at the state level. Positive values represent increases in life expectancy. Cigarette tax dollars are inflation-adjusted to 2016 year dollars. Income Q1–5 correspond to quintiles of county income per capita. Vertical dashed line is overall average effect.
By gender
Among men and women, a one-dollar increase in the cigarette tax per pack was associated in the long run with an increase in life expectancy of 1.17 years (95% CI 0.69 to 1.66; figure 2, table 2) and 0.81 years (95% CI 0.52 to 1.10 years; figure 2, table 2), respectively.
By income
Across county income quintiles, a one-dollar increase in the cigarette tax per pack was associated in the long run with an increase in life expectancy of 1.44 years (95% CI 0.76 to 2.12 years) for the lowest income quintile to 0.55 years (95% CI 0.01 to 1.09 years) for the highest income quintile. There was a significant negative linear trend in the long-run coefficients by income quintile (−0.23 years/US$1 cigarette tax increase; 95% CI −0.28 to −0.18) (figure 2 online supplementary table S3). The differences in the long-run coefficients between income quintile 1 vs income quintiles 2, 3, 4 and 5 were −0.17, −0.35, −0.65 and −0.89 years, respectively.
By rural versus urban county
A one-dollar increase in the cigarette tax per pack was associated in the long run with an increase in life expectancy of 1.05 years (95% CI 0.73 to 1.36) for rural counties compared with 0.92 years (95% CI 0.41 to 1.44) for urban counties (figure 2, online supplementary table S4).
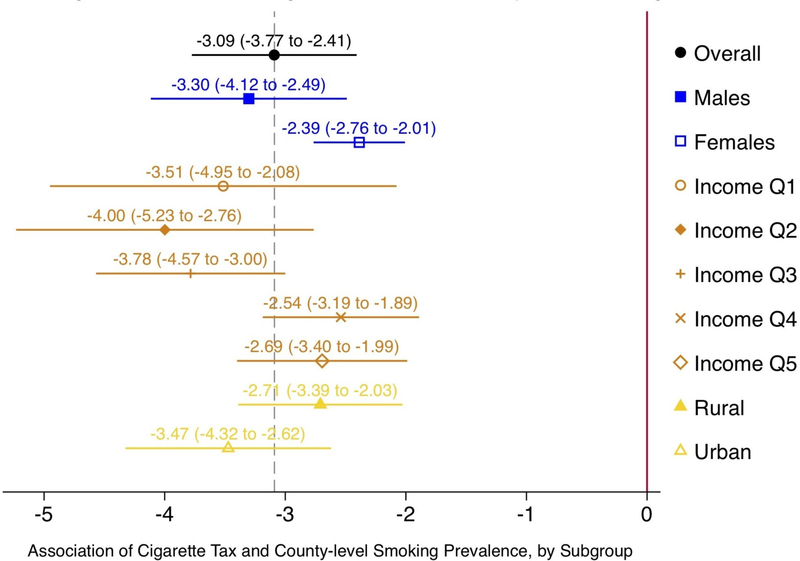
Long-run relationship with smoking prevalence
A one-dollar increase (in 2016 dollars) in the cigarette tax per pack was associated with a 3.09% (95% CI −3.77 to −2.41) absolute reduction in smoking prevalence over the long run (figure 3, online supplementary table S5), from a mean prevalence over the study period of 25.91%. Similar to the pattern for life expectancy, the estimated reduction in smoking prevalence was greater in magnitude among men and in low-income counties (figure 3, online supplementary table S6). In contrast to the pattern for life expectancy, the reduction in smoking prevalence was greater in magnitude for urban versus rather than rural counties (figure 3, online supplementary table S7), although the difference was not significantly different from the null of no difference. The pattern of urban versus rural results persisted after removing states where local cigarette taxes were in effect (online supplementary table S7, panel B).
Figure 3.
Long-run association of cigarette taxes and smoking prevalence. Long-run changes in smoking prevalence at the county level by subgroup from the main regression analysis with adjustment for county-year income per capita, share female, share black, share over 65, share under 18 and share with high school, and fixed effects for county. 95% CIs reflect Huber-White robust SEs clustered at the state level. Positive values represent increases in life expectancy. Cigarette tax dollars are inflation-adjusted to 2016 year dollars. Income Q1–5 correspond to quintiles of county income per capita. Vertical dashed line is overall average effect.
Long-run relationship with mortality rates by cause of death
Among causes of death related to cardiovascular diseases, a one-dollar increase in the cigarette tax per pack of 20 cigarettes was associated in the long run with a significant reduction in mortality rates for deaths caused by ischaemic heart disease, followed in magnitude by cerebrovascular disease and ischaemic stroke (online supplementary figure S5, panel A). Among causes of death related to cancer, the largest mortality rate reduction was observed for deaths caused by tracheal, bronchus and lung cancers (online supplementary figure S5, panel B). Among causes of death related to respiratory disease, the largest mortality rate reduction was observed for deaths caused by chronic obstructive pulmonary disease (online supplementary figure S5, panel C). We note that rates of mortality due to self-harm increased (online supplementary figure S5, panel D). Most of the mortality reductions for tobacco-related causes of death remained statistically significantly different from zero after adjustment for multiple tests (online supplementary table S8).
Sensitivity analyses
First, we examined whether the selection of lag order qualitatively influenced our results; we found the results were robust for lag lengths across the tested span of 1–5 years (online supplementary table S9).
Second, we fit a generalised method of moments dynamic panel estimator developed by Blundell and Bond,37 which relaxes the assumption of strongly exogenous covariates by using lags (of order 2 and greater) as instrumental variables and which was designed for small-T, large-N datasets. Results were robust to the error-correction model’s results (online supplementary table S10), indicating that the weak correlation between the explanatory variables (county-year share female, under 18, over 65, black, Hispanic, completing high school and income per capita) and the residuals of the main error-correction model (<0.11 in absolute value for all covariates; see online supplementary table S11) did not generate a non-stationary error process, such as feedback from the dependent variable to explanatory variables.
Third, because we used state-year cigarette taxes, we also conducted an analysis restricted to the 43 out of 51 (counting the District of Columbia) states where there is no local government taxation of tobacco.38 Results were again robust (online supplementary table S12).
Fourth, using data on the probability of a county resident being covered by a 100% smokefree law for workplaces, bars or restaurants, respectively, in a given year (compiled previously based on the American Non-smokers’ Rights Foundation Local Ordinance Database44), we confirmed that county-year workplace, bar and restaurant restrictions were not strongly correlated to state-year cigarette tax levels (correlation coefficient <0.28) or predictive of state cigarette tax levels (R2=0.07) (online supplementary table S13, panels A and B). As additional sensitivity analyses, we included state-year workplace, bar and restaurant smoking restrictions from The National Adult Tobacco Survey39 and 41 other state-year smoking-related policy measures from the Centers for Disease Control and Prevention19 as time-varying covariates in the main analysis. Results were unchanged (online supplementary table S13, panel C; online supplementary figure S6).
Fifth, results were consistent when we repeated the analysis using annual life expectancy estimates for the 100 most populated US community zones derived from official death records: a one-dollar increase in cigarette taxes in a community zone (calculated as the population-weighted average of state tax rates) was associated with a long-run increase in life expectancy of 0.78 years (95% CI 0.50 to 1.05) for men and 0.55 years (95% CI 0.37 to 0.73) for women.
Sixth, as a falsification test, we tested and found no association between current year life expectancy (or smoking prevalence) and future, not-yet-announced cigarette taxes 5 years in the future (online supplementary table S14).
DISCUSSION
We examined the long-run association between cigarette excise taxes and life expectancy across US counties between 1996 and 2012. Our central finding was that for every one-dollar increase in cigarette tax per pack (in 2016 dollars), county life expectancy increased by approximately 1 year in the long-run equilibrium relationship. The magnitude of the long-run association of life expectancy and cigarette tax rates steadily increased as county income decreased. The association between cigarette excise taxes and life expectancy was plausibly related to reductions in county smoking prevalence, a mediator that had a similar and faster response to cigarette taxes as observed for life expectancy. Using the same regression model to assess the relationship between cigarette taxes and disease-specific mortality rates showed a decline in deaths caused by tobacco-related diseases (cerebrovascular disease, ischaemic stroke and heart disease, tracheal, bronchus and lung cancers and chronic obstructive pulmonary disease). There was also no detectable relationship for deaths caused by non-tobacco-related diseases. Our empirical estimates suggest that, after a change in the short run, the half-life of the adjustment back to the long-run equilibrium relationship between excise taxes and life expectancy was approximately 10 years. Thus, a 6-month increase in life expectancy would be expected 10 years after a one-dollar increase in the cigarette tax rates, and then an additional 3-month increase would be expected over the following 10 years, and so on, approaching 1 year asymptotically following a permanent change in the tax rate.
Our results provide both empirical and methodological contributions to the tobacco control literature. Contributing to the rich literature showing that increases in cigarette taxes reduce tobacco smoking, our results here additionally show corresponding improvements in overall life expectancy in the context of ongoing debates about how best to reduce income-based and geographic-based inequalities in life expectancy.18 The results are consistent with a simulation model that projected potential life expectancy benefits based on extrapolation of the effects of taxes on smoking and then the effects of smoking on life expectancy.45 Our use of dynamic panel regression models allowed us to empirically partition short-run and long-run components of the relationship between taxes and life expectancy, providing an important tool to public health policy evaluation given that delayed effects are otherwise difficult to assess through traditional strategies such as difference-in-differences analysis. Given (i) the addictive nature of nicotine, which may generate a lagged behavioural response to a tax increase, (ii) that life expectancy is expected to respond slowly to changes in cigarette taxes and (iii) that tobacco tax effects would be expected to accumulate over time, increasing in multiple years and various amounts in most states, studies that do not consider dynamic issues in the modelling process may underestimate the net life expectancy effects of taxation strategies.
That the magnitude of the long-run association of life expectancy and cigarette tax rates steadily increased as county income decreased is consistent with the idea that demand for cigarettes is sensitive to price changes more among consumers with lower rather than higher incomes.46 Our findings contradict the argument—promoted by the tobacco industry and organisations that the industry has a history of financially supporting47,48—that cigarette taxes disproportionately burden low-income smokers because they are regressive. Our results instead suggest that the net benefit of cigarette taxes disproportionately accrue to low-income counties.
Some important limitations of our study should be noted when interpreting the findings. First, we cannot rule out the possibility of residual confounding, particularly with respect to changing tobacco smoking norms over the observation period. To the extent that certain states may be more likely to increase cigarette taxes as a function of changing beliefs about the tobacco-related harms, residents of those states may also be more likely to reduce smoking. This concern is somewhat offset by that fact that at the state level, the impetus to raise tobacco taxes is thought to have been typically based primarily on revenue, rather than public health, priorities.49 Although we include county-year controls on income per capita and population composition, as well as county-level fixed effects to control for time-invariant unobservable differences across counties with varying changes in cigarette tax rates, it remains possible that time-varying county-level changes that are not correlated with income per capita or the compositional changes we controlled for, but that are correlated with both cigarette tax increases and life expectancy, are influencing our estimates. Furthermore, while there is significant variation in the degree to which states implemented various tobacco control policies, prior literature suggests that these policies tend to be clustered.44 Although the findings did not change after we incorporated annual data on over 40 state smoking-related laws as control variables in our model or restricted analysis to the 42 states without local government taxation of tobacco,38 we cannot rule out the influence of other tobacco control policies (eg, smokefree air laws, youth prevention, mass media campaigns and marketing restrictions) if they were frequently implemented during the same periods as increased taxes, although we would expect that most of effect from these will be absorbed in the county-specific intercept.
Increasing cigarette excise tax rates may translate to consequential population-level improvements in overall life expectancy, especially in lower-income counties.
Supplementary Material
What this paper adds.
What is already known on this subject
A large body of literature suggests that tobacco control legislation—including fiscal measures such as excise taxes—effectively reduces tobacco smoking.
The long-run (10+ years) relationship between cigarette taxes and life expectancy has not been directly evaluated.
What this study adds
We find that a one-dollar increase in cigarette tax per pack (in 2016 dollars) translated to an increase in life expectancy of 1 year over the following decades, with the first 6-month increase in life expectancy taking 10 years to materialise.
There was a larger life-expectancy benefit of increases in cigarette excise taxes in lower-income counties compared with higher-income counties, which is evidence against the claim that cigarette taxes are regressive.
Acknowledgements
The authors would like to thank Dr Raj Chetty, Dr David Cutler, Michael Stepner and participants at the National Bureau of Economic Research Retirement Research Center Meeting, Determinants of Life Expectancy by Income and Geography: Implications for Social Security, for helpful comments and suggestions that improved the paper.
Funding This research was supported by the US Social Security Administration through grant RRC08098400-09 to the National Bureau of Economic Research as part of the SSA Retirement Research Consortium and by the National Institutes of Health (National Institute on Drug Abuse R01DA043950 and National Institute on Minority Health and Health Disparities DP2MD010478).
Role of the funding source
None. AB and SA had access to the raw data. The corresponding author had full access to all of the data and the final responsibility to submit for publication.
Footnotes
Competing interests None declared.
Disclaimer The findings and conclusions expressed are solely those of the author(s) and do not represent the views of SSA, the National Institutes of Health, any agency of the Federal Government or the NBER.
Patient involvement
No patients were involved in the creation of this article.
Patient consent for publication Not required.
Ethics approval The analysis was deemed exempt from review by the Icahn School of Medicine Institutional Review Board, Protocol ID# 17-02303.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement Life expectancy, cigarette smoking prevalence and cigarette tax rate data are publicly available and can be downloaded at http://ghdx.healthdata.org/record/united-states-life-expectancy-and-age-specific-mortality-risk-county-1980-2014, http://ghdx.healthdata.org/record/united-states-smoking-prevalence-county-1996-2012 and https://chronicdata.cdc.gov/Legislation/CDC-STATE-System-Tobacco-Legislation-Smokefree-Ind/2snk-eav4, respectively.
REFERENCES
- 1.Chetty R, Cutler D, Stepner M. Effects of local health interventions on inequality in life expectancy: new publicly available data. Am J Public Health 2016;106:2154–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med 2009;6:e1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lantz PM, Jacobson PD, Warner KE, et al. Investing in youth tobacco control: a review of smoking prevention and control strategies. Tob Control 2000;9:47–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaloupka FJ, Yurekli A, Fong GT. Tobacco taxes as a tobacco control strategy. Tob Control 2012;21:172–80. [DOI] [PubMed] [Google Scholar]
- 5.Hu TW, Sung HY, Keeler TE. Reducing cigarette consumption in California: tobacco taxes vs an anti-smoking media campaign. Am J Public Health 1995;85:1218–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilson LM, Avila Tang E, Chander G, et al. Impact of tobacco control interventions on smoking initiation, cessation, and prevalence: a systematic review. J Environ Public Health 2012;2012:1–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mokdad AH, Ballestros K, Echko M, et al. The state of us health, 1990–2016: burden of diseases, injuries, and risk factors among US States. JAMA 2018;319:1444–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laugesen M, Grace RC. Reduced tobacco consumption, improved diet and life expectancy for 1988–1998: analysis of New Zealand and OECD data. N Z Med J 2017;130:46–51. [PubMed] [Google Scholar]
- 9.Jemal A, Ward E, Thun M. Declining death rates reflect progress against cancer. PLoS One 2010;5:e9584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Global Tobacco Economics Consortium. The health, poverty, and financial consequences of a cigarette price increase among 500 million male smokers in 13 middle income countries: compartmental model study. BMJ 2018;361:361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stewart ST, Cutler DM, Rosen AB. Forecasting the effects of obesity and smoking on U.S. life expectancy. N Engl J Med 2009;361:2252–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Basu S, Meghani A, Siddiqi A. Evaluating the health impact of large-scale public policy changes: classical and novel approaches. Annu Rev Public Health 2017;38:351–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Granger CWJ, Newbold P. Spurious regressions in econometrics. J Econom 1974;2:111–20. [Google Scholar]
- 14.Phillips PCB. Understanding spurious regressions in econometrics. J Econom 1986;33:311–40. [Google Scholar]
- 15.Martin V, Hurn S, Harris D. Econometric modelling with time series: specification estimation and testing: Cambridge University Press, 2012. [Google Scholar]
- 16.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 2007;4:e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, et al. Inequalities in life expectancy among us counties, 1980 to 2014: temporal trends and key drivers. JAMA Intern Med 2017;177:1003–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA 2016;315:1750–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.CDC STATE System Tobacco Legislation - Tax. Centers for disease control and prevention, national center for chronic disease prevention and health promotion, office on smoking and health; 2018. [Google Scholar]
- 20.U.S. Bureau of Labor Statistics. Consumer Price Index (CPI) Databases.
- 21.Dwyer-Lindgren L, Mokdad AH, Srebotnjak T, et al. Cigarette smoking prevalence in US counties: 1996–2012. Popul Health Metr 2014;12:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roth GA, Dwyer-Lindgren L, Bertozzi-Villa A, et al. Trends and patterns of geographic variation in cardiovascular mortality among us counties, 1980–2014. JAMA 2017;317:1976–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mokdad AH, Dwyer-Lindgren L, Fitzmaurice C, et al. Trends and patterns of disparities in cancer mortality among us counties, 1980–2014. JAMA 2017;317:388–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, et al. Trends and patterns of differences in chronic respiratory disease mortality among us counties, 1980–2014. JAMA 2017;318:1136–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bureau UC. American community survey. Washington, DC: US Department of Commerce, Economics and Statistics Administration, US Census Bureau, 2010. [Google Scholar]
- 26.USDA. Rural-Urban Commuting Area (RUCA) Codes: US Department of Agriculture Economic Research Services, 2010. [Google Scholar]
- 27.USDA. REPORT ON THE DEFINITION OF “RURAL”: United States Department of Agriculture Rural Development, 2013. [Google Scholar]
- 28.Pesaran MH, Smith R. Estimating long-run relationships from dynamic heterogeneous panels. J Econom 1995;68:79–113. [Google Scholar]
- 29.Blackburne EF, Frank MW. Estimation of nonstationary heterogeneous panels. Stata J 2007;7:197–208. [Google Scholar]
- 30.Baltagi BH, Griffin JM, Xiong W. To pool or not to pool: homogeneous versus heterogeneous estimators applied to cigarette demand. Rev Econ Stat 2000;82:117–26. [Google Scholar]
- 31.Kirchgässner G, Wolters J, Hassler U. Introduction to modern time series analysis: Springer Science & Business Media, 2012. [Google Scholar]
- 32.Hsiao C, Fujiki H. Nonstationary time-series modeling versus structural equation modeling: with an application to japanese money demand. Monetary and Economic Studies 1998;16:57–80. [Google Scholar]
- 33.Identification Hsiao C. and dichotomization of long- and short-run relations of cointegrated vector autoregressive models. Econometric Theory 2001;17:889–912. [Google Scholar]
- 34.Rogers W Regression standard errors in clustered samples. Stata technical bulletin 1994;3. [Google Scholar]
- 35.Aznar A, Salvador M. Selecting the rank of the cointegration space and the form of the intercept using an information criterion. Econometric Theory 2002;18:926–47. [Google Scholar]
- 36.Westerlund J Panel cointegration tests of the Fisher effect. J Appl Econ 2008;23:193–233. [Google Scholar]
- 37.Blundell R, Bond S. Initial conditions and moment restrictions in dynamic panel data models. J Econom 1998;87:115–43. [Google Scholar]
- 38.Consortium TCL. U S. Local Tobacco Tax Authority: A 50-State Review:55105–3076.
- 39.King BA, Dube SR, Tynan MA. Current tobacco use among adults in the united states: findings from the national adult tobacco survey. Am J Public Health 2012;102:e93–e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Corporation S Stata time-series: reference manual: Stata Press, 2004. [Google Scholar]
- 41.Westerlund J Testing for error correction in panel data. Oxf Bull Econ Stat 2007;69:709–48. [Google Scholar]
- 42.Persyn D, Westerlund J. Error-correction–based cointegration tests for panel data. Stata J 2008;8:232–41. [Google Scholar]
- 43.In: Kripfganz S, Schneider D, eds. ardl: Estimating autoregressive distributed lag and equilibrium correction models. 2018. London: Stata ConferenceStata Users Group, 2018. [Google Scholar]
- 44.Song AV, Dutra LM, Neilands TB, et al. Association of smoke-free laws with lower percentages of new and current smokers among adolescents and young adults: an 11-year longitudinal study. JAMA Pediatr 2015;169:e152285–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Global Tobacco Economics Consortium. The health, poverty, and financial consequences of a cigarette price increase among 500 million male smokers in 13 middle income countries: compartmental model study. BMJ 2018;361:k1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gallet CA, List JA. Cigarette demand: a meta-analysis of elasticities. Health Econ 2003;12:821–35. [DOI] [PubMed] [Google Scholar]
- 47.Campbell R, Balbach ED. Mobilising public opinion for the tobacco industry: the Consumer Tax Alliance and excise taxes. Tob Control 2008;17:351–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Campbell RB, Balbach ED. Building alliances in unlikely places: progressive allies and the Tobacco Institute’s coalition strategy on cigarette excise taxes. Am J Public Health 2009;99:1188–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Goldman T Tobacco Taxes. Health Affairs Health Policy Brief 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.