Abstract
Background
The role of acculturation in dietary behaviors among Hispanics/Latinos in the United States remains unclear. Discrepancies may be explained by variations in acculturation constructs or ethnicity-specific dynamics.
Objective
We aimed to compare relations between 3 different acculturation constructs with dietary quality and patterns among Puerto Ricans in the mainland United States.
Methods
We analyzed cross-sectional data with 1194–1380 Puerto Ricans, aged 45–75 y. Acculturation was measured with the use of a language-based scale (0–100; higher score denotes more English use), a psychological-based scale (0–50; higher score denotes stronger US orientation), and years living in the mainland United States. Diet quality scores (higher scores denote healthier diet) were defined with the use of the Alternate Healthy Eating Index-2010 (AHEI) and the Mediterranean Diet Score (MeDS). Three dietary patterns were previously derived with the use of principal components analysis. Adjusted multivariable regression models tested the association of each acculturation construct with diet quality score or pattern. Interaction terms were included for income or education status.
Results
Psychological-based acculturation, but not the other constructs, was positively associated with AHEI (β ± SE: 0.013 ± 0.004; P = 0.002) and MeDS (0.009 ± 0.005; P = 0.041). Income, but not education, moderated this association (P = 0.03), with higher diet quality observed with higher income (>$25,000) and stronger US orientation. All constructs were inversely associated with a traditional dietary pattern, with the language-based scale being stronger (z score β ± SE: −0.160 ± 0.032; P < 0.0001) than the psychological-based scale (−0.097 ± 0.028; P = 0.001) or years living in the mainland United States (−0.058 ± 0.028; P = 0.041). No associations were observed for the Western or sweets/desserts patterns.
Conclusions
In Puerto Rican adults, stronger psychological US orientation was associated with higher diet quality, particularly with higher income. More Spanish use, stronger psychological Puerto Rican orientation, and shorter length of mainland-US residency were associated with traditional dietary patterns. Appropriate diet-related acculturation constructs should be carefully considered among Hispanics/Latinos. This trial was registered at clinicaltrials.gov as NCT01231958.
Keywords: dietary acculturation, acculturation constructs, language acculturation, psychological acculturation, Hispanics/Latinos, Puerto Ricans, diet quality, dietary patterns, immigrants
Introduction
Acculturation is the process of cultural transition that occurs when 2 distinct cultures interact regularly and can transpire at either the group or the individual level (1). Among Hispanics/Latinos in the United States, higher acculturation has been generally associated with poor health (2, 3). One pathway in which this may occur is through dietary acculturation, or the “process by which immigrants adopt the dietary practices of the host (dominant culture) country” (4). Challenges to determine this include a lack of appropriate measurement of dietary acculturation, limited used of acculturation theory, and common use of single-item or proxy measures (e.g., length of residence, language preference) (5), which assume that the amount of time exposed to a new culture means incorporation into the culture or that gaining the majority culture is ideal while ignoring potentially protective aspects of the origin culture (5, 6).
Investigators advocate the use of bi- or multidimensional acculturation measures that capture different domains of both origin and new cultures (6), including language use, attitudes, values, and ethnic interactions (5), because they provide clearer, more nuanced information about the complex process of acculturation and its association with health (6, 7). Yet, most studies have only assessed language proficiency, or other proxy unidimensional measures, which does not fully capture the process of cultural adaptation (5). The use of bi- or multidimensional scales can capture both overt behavioral change and internal identity change (8), and can help to untangle the complexity of dietary acculturation.
Findings on the relation of acculturation with diet intake in Hispanics/Latinos, for which the majority of studies on acculturation in the United States have been done, have been inconsistent, with some studies showing that increasing acculturation is associated with poorer intake of some foods and nutrients (3, 9), but not others (9), and may depend on the acculturation construct used and the specific Hispanic/Latino heritage (9, 10). For example, among Hispanic/Latinos who participated in the California Health Interview Survey, greater acculturation (measured with a unidimensional scale) was associated with higher intake of fast food among Mexicans, Central Americans, and Puerto Ricans, but not among other Hispanic/Latino heritages (11). In addition, most studies have included predominately Hispanics/Latinos of Mexican heritage (10, 12), limiting the external validity of findings to other Hispanic/Latino heritages that may exhibit differential acculturation processes (3). For example, stringent migration policies along the Mexico-US border have made circular migration for Mexican immigrants more difficult, which has resulted in increased cultural isolation for this group (13); conversely Puerto Ricans may easily return to their country of origin given that it is a US territory. Other differences in income, educational attainment, and English proficiency at time of migration by Latin American country of origin have been reported (14), which may launch disparate acculturation paths. Differentiating by heritage may provide further insights into the inconsistent associations between acculturation and diet (7).
Puerto Ricans living in the United States are of particular concern, because they have lower diet quality than other Hispanic/Latino heritages (15). Because the Commonwealth of Puerto Rico is a US territory, Puerto Ricans may have a distinct acculturation process. The interconnection between the 2 cultures may allow for fluid and hybrid identities of Puerto Ricans in both sites (16). Language use may also be a flexible process; Spanish was used at home but not as the exclusive or dominant language among a Puerto Rican community in Massachusetts (17). However, because of the different constructs used to assess acculturation and dietary behaviors, the association between these 2 factors in mainland Puerto Ricans remains unclear. For example, young adult mainland Puerto Ricans appear to be more acculturated to the mainland United States, as defined by longer length of residency in the mainland United States or higher English use, and to consume more unhealthy foods and less healthy foods than other Hispanics/Latinos (18). For middle-aged and older mainland Puerto Ricans, the opposite was observed, because greater English use assessed with a bidimensional language-based acculturation scale was associated with consumption of fewer ethnic foods and more healthy foods or those aligned with eating patterns of non-Hispanic whites (19). In this same Puerto Rican population, longer time residing in the United States (a unidimensional construct) seemed to shift macronutrient consumption to a level similar to non-Hispanic whites (19, 20). The inconsistent conclusions raise the question of which acculturation construct may provide a stronger association with dietary outcomes in Puerto Rican adults, namely overall health quality of the diet as well as dietary patterns marked by traditional foods compared with US foods (independent of diet quality).
Socioeconomic conditions and educational attainment may modify the associations between acculturation and nutrition, especially among groups with persistent low socioeconomic status (21), such as mainland Puerto Rican adults (22, 23). In the cohort of middle-aged and older mainland Puerto Ricans, poverty status partially moderated some of the observed associations, such that greater language-based acculturation was associated with lower dietary glycemic index, lower starch intake, and greater servings of fruit and nonstarchy vegetables only among individuals above the poverty line (19), reiterating the importance of considering the intersection of socioeconomic status and acculturation (3, 4, 24).
Adequate multidimensional acculturation measures (7, 25) and comparison of different acculturation constructs (26, 27) are needed to better conceptualize and assess dietary acculturation. Thus, the aim of this study was to compare 3 different bidimensional and unidimensional acculturation constructs (psychological-based, language-based, years living in the mainland United States) with regard to their association with nutrient intake, diet quality, and dietary patterns among Puerto Rican adults in Boston, MA. Contrasting different dietary outcomes may help elucidate how acculturation relates to different dietary frameworks (healthfulness compared with food patterns clustered by cultural orientation).
Methods
Participants
We analyzed data from the baseline visit (2004–2007) of the Boston Puerto Rican Health Study (BPRHS), a longitudinal study of psychosocial stress, acculturation, nutrition, and disease development. Detailed recruitment and data collection methods were previously published (22). Study eligibility requirements included self-identifying as Puerto Rican, being between 45 and 75 y old, being able to respond to questions in either English or Spanish, and living in the Boston, MA metropolitan area at the time of the study. Recruitment of eligible adults occurred through door-to-door enumeration and community outreach strategies. Participants provided written consent to participate in study activities, which were administered in the participant's home by trained bilingual interviewers. The Tufts Medical Center Institutional Review Board and the Northeastern University Institutional Review Board approved the study. This study was registered at clinicaltrials.gov as NCT01231958.
Questionnaires inquired about age, sex, marital status, household income, educational attainment, employment status, migration between the US mainland and Puerto Rico, food insufficiency, participation in federal food assistance programs, health insurance, smoking history, alcohol use, and physical activity with the use of a modified Paffenbarger questionnaire of the Harvard Alumni Activity Survey that assessed levels of activities (heavy, moderate, light, or sedentary activity, and sleeping) within a 24-h period. Participants self-reported medically diagnosed health conditions, medication use, perceived stress, difficulty performing activities of daily living, and depressive symptoms with the use of the Center for Epidemiology Studies Depression scale. Physical examinations included blood samples for laboratory assays, and anthropometric measures (including waist and hip circumference) via standardized methods.
Acculturation constructs
The 3 constructs of acculturation contrasted in this study were 2 bidimensional constructs (a language-based questionnaire and a psychological-based questionnaire) as well as a unidimensional proxy measure of acculturation (years living in the mainland United States). The language-based questionnaire was adapted from the Bi-dimensional Acculturation Scale for Hispanics (28), assessing bidirectional preferences in language use (Spanish or English) during 7 different daily activities, including at work, when speaking (with neighbors, friends, and family), watching television, reading newspapers/books, and listening to the radio. The scale recognizes multiple language-related (but not psychosocial) acculturative areas across both cultural domains. Response options were on a 5-point Likert scale, from 1 (“only Spanish”) to 5 (“only English”). A summary score from 0 to 100 demonstrated the level of language acculturation such that lower scores indicated less acculturation (more Spanish) and higher scores indicated more acculturation (more English).
The psychological-based questionnaire used an adapted 10-item Psychological Acculturation Scale that assesses individuals’ psychological negotiation of the 2 cultural entities, with particular attention to subjective sense of belonging and emotional attachment to each culture, through questions pertaining to differing cultural contexts, including beliefs and values, shared identity, feelings of comfort, shared ways of thinking, cultural pride, cultural ways of accomplishing tasks and behaving, shared understanding, situational expectations, and knowledge of history and traditions (29). Response options were on a 5-point Likert scale, from 1 (“only Puerto Rican”) to 5 [“only U.S. (American)”], with a bicultural orientation as a midpoint option. Responses were summed to create a score ranging from 0 to 50, with lower scores indicative of more Puerto Rican psychological orientation and higher scores indicative of more US-American psychological orientation. Construct validity conducted among adults showed that the psychological acculturation scores were highly correlated with all the cultural behavior and cultural preference scores, with weaker relations with language use (29).
Years living in the mainland United States was the calculated length of time from year of first arrival to the United States to time of study enrollment, accounting for periods of circular migration between the US mainland and Puerto Rico. Circular migration included residence in Puerto Rico for >3 mo at a time, after initial immigration to the US mainland. Each acculturation construct was reported as a continuous variable and as tertiles.
Dietary intake assessment and dietary measures
An adapted version of the National Cancer Institute Block-FFQ assessed dietary intake during the home interview (30). Modifications of the original FFQ included Puerto Rican–appropriate foods and portion sizes. The adapted semiquantitative FFQ was validated for this population, demonstrating a more accurate representation of intake compared with the original FFQ (30). Participants with implausible energy intakes (<400 or >4800 kcal/d) and/or >10 questions left blank were excluded (n = 67).
The Alternate Healthy Eating Index-2010 (AHEI) and the Mediterranean Diet Score (MeDS) assessed diet quality, and were previously described in this cohort (31, 32). The AHEI score provided a measure of overall diet quality according to evidence for the association between dietary factors and lower chronic disease risk (33). The total score ranged from 0 (lowest diet quality) to 110 (highest diet quality) and reflected 11 food groups and nutrients (vegetables, whole fruit, whole grains, sugar-sweetened beverages/fruit juice, nuts/legumes, red/processed meat, trans fat, omega-3 fatty acids, PUFAs, sodium, and alcohol) based on predefined cutoffs. The MeDS measured adherence to a Mediterranean diet by summing scores of 9 dietary components (vegetables, fruits, nuts and legumes, whole grains, fish, meat and meat products, dairy and dairy products, alcohol, and monounsaturated-to-saturated fats ratio). A point was assigned for being above the healthy population- and sex-specific median cutoff, expressed per 1000 kcal/d; points were summed and total scores ranged from 0 (low adherence) to 9 (high adherence). AHEI and MeDS were reported as continuous scores.
Dietary patterns in this cohort were previously established with the use of factor analysis (34, 35), with the PROC FACTOR procedure in SAS (version 9.2, SAS Institute, Cary, NC). The factors were rotated orthogonally with the varimax option. The sum of food group intakes (entered into principal components analysis as percentage of total energy) for each factor was weighted by its factor loading, providing a pattern score for each participant. A 3-factor solution was retained because it had the most consistent eigenvalues, scree plots, and factor loadings as assessed in random split samples; the 3 identified patterns were: 1) Western pattern (meat, processed meats, and French fries); 2) traditional pattern (rice, beans, and oils); and 3) sweets, sugary beverages, and dairy desserts pattern.
Statistical analysis
Of the 1500 enrolled participants, complete baseline acculturation data were available for 1394 (years living in the United States), 1415 (psychological-based scale), and 1421 (language-based scale) participants, and valid dietary data were available for 1194 (MeDS), 1337 (AHEI), and 1380 (dietary patterns and nutrient data) participants. Spearman correlations between the acculturation constructs were assessed. We analyzed differences in baseline characteristics by tertile categories of each acculturation construct, using ANOVA for continuous variables and chi-square tests for categoric variables. General linear regression models were fitted to predict mean intake of nutrients representative of those primarily consumed in the diet by tertile categories of each acculturation construct, adjusted for age, sex, and energy. Separate multivariable linear regression models tested the association between each acculturation construct as continuous scores, with diet quality (AHEI, MeDS) and with dietary patterns (Western, traditional, sweets and dairy desserts) as continuous outcomes. The models were also run with the z scores of the acculturation constructs for direct comparison of the magnitude of association strength. All multivariable models were adjusted for age, sex, household income, smoking (in packs per year), educational attainment, physical activity score, frequency of eating out, receipt of the Supplemental Nutrition Assistance Program, and energy intake (except for MeDS, because it is already expressed per 1000 kcal/d). Additional models were adjusted for variables considered as confounders in previous studies or hypothesized to be potential confounders in the acculturation-diet association [i.e., household composition, marital status, working status, diabetes diagnosis, waist circumference, perceived stress score, depressive symptomatology, and activities of daily living (i.e., physical function)], but none of these potential confounders changed the models or results and thus were not included in the final models. Sensitivity analyses were conducted to adjust each model for the other acculturation constructs. We also used multivariable linear regression models to separately test interactions between acculturation and income or educational attainment on the associations with diet quality, adjusting for the same confounders mentioned above and using Tukey's procedure to adjust for multiple comparisons. Results are presented as β coefficients and SEs, or adjusted means and SEs. P < 0.05 was used as the significance level.
Results
All acculturation constructs were significantly correlated with one another (all P < 0.0001): psychological-based scale and language-based scale (r = 0.51), language-based scale and years living in the United States (r = 0.25), and years living in the United States and psychological-based scale (r = 0.17). Participants’ characteristics differed across the tertile categories of each acculturation construct (Table 1). Those with the highest tertile of the language-based scale (i.e., more English use) tended to be younger, male, single, with higher educational attainment, more physically active, and less likely to be under the poverty line or to receive food assistance, but more likely to currently work, currently smoke, and eat out >1 time/wk than those with the lowest tertile of the language-based scale (i.e., more Spanish use). Significantly different characteristics for the highest tertile of the psychological-based scale (i.e., more US orientation) were similar to those of the language-based scale except for sex, marital status, and smoking status. Participants in the highest tertile of years living in the United States (>40 y) tended to be older and male and less likely to receive food assistance, but more likely to have health insurance, to have migrated back to Puerto Rico, and to have never smoked, compared with those in the lowest tertile (<32 y).
TABLE 1.
Characteristics by tertile of acculturation construct for Puerto Rican adults living in Boston, MA1
| Language-based acculturation scale (n = 1421) | Psychological-based acculturation scale (n = 1415) | Years living in the mainland United States (n = 1394) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| More Spanish | Bilingual | More English | More Puerto Rican | Bicultural | More US | <32 y | 32–40 y | >40 y | |
| n | 462 | 503 | 456 | 495 | 425 | 495 | 463 | 470 | 461 |
| Age, y | 59.7 (7.8) | 57.3 (7.0) | 54.5 (7.1)**** | 58.7 (7.6) | 57.3 (7.6) | 55.7 (7.5)**** | 54.8 (7.6) | 56.2 (6.5) | 60.2 (7.6)**** |
| Sex | |||||||||
| Female | 78.8 | 73.8 | 62.3**** | 73.5 | 71.8 | 69.9 | 75.2 | 73.4 | 65.7** |
| Male | 21.2 | 26.2 | 37.7 | 26.5 | 28.2 | 30.1 | 24.8 | 26.6 | 34.3 |
| Marital status | |||||||||
| Married | 26.9 | 35.8 | 35.5**** | 32.5 | 31.4 | 34.5**** | 32.0 | 33.9 | 33.2 |
| Single | 12.4 | 13.1 | 16.8 | 13.8 | 13.9 | 14.6 | 14.9 | 14.2 | 13.5 |
| Divorced | 40.6 | 38.4 | 40.6 | 37.7 | 40.1 | 41.6 | 40.7 | 39.1 | 39.3 |
| Widowed | 20.2 | 12.7 | 7.1 | 16.0 | 14.6 | 9.3 | 12.3 | 12.9 | 14.1 |
| Education status | |||||||||
| 8th grade or less | 72.3 | 46.7 | 20.8**** | 60.4 | 44.9 | 34.3**** | 44.3 | 47.2 | 47.3 |
| Some high school/GED | 24.0 | 42.9 | 46.1 | 33.1 | 39.3 | 41.2 | 40.2 | 37.2 | 36.9 |
| ≥High school | 3.7 | 10.3 | 33.1 | 6.5 | 15.8 | 24.4 | 15.6 | 15.5 | 15.8 |
| Household income, $ | |||||||||
| <10,000 | 59.3 | 47.5 | 34.0 | 53.3 | 46.6 | 41.0 | 47.1 | 47.9 | 44.9 |
| 10,000–25,000 | 34.9 | 39.0 | 36.6 | 36.4 | 36.7 | 37.4 | 35.9 | 35.3 | 40.1 |
| ≥25,000 | 5.8 | 13.5 | 29.4 | 10.3 | 16.7 | 21.6 | 17.1 | 16.8 | 15.0 |
| Below 100% federal poverty line | 72.8 | 61.0 | 40.9**** | 64.3 | 61.8 | 49.3**** | 61.1 | 60.0 | 53.6 |
| Currently working | 6.4 | 15.7 | 39.8**** | 12.4 | 19.0 | 31.0**** | 22.6 | 22.1 | 20.1 |
| Food insufficiency2 | 12.6 | 10.3 | 11.8 | 10.9 | 10.4 | 12.7 | 12.5 | 10.6 | 11.3 |
| Government food assistance3 | 36.8 | 28.8 | 25.9** | 30.5 | 35.5 | 26.5* | 34.8 | 27.3 | 29.5* |
| Health insurance | 96.8 | 95.4 | 93.6 | 96.0 | 94.8 | 94.2 | 95.9 | 92.8 | 97.0** |
| Circular migration | 36.7 | 41.0 | 37.3 | 40.9 | 36.6 | 37.8 | 27.4 | 40.9 | 48.0**** |
| Smoking status | |||||||||
| Never | 50.7 | 48.6 | 37.3**** | 49.8 | 45.2 | 42.2 | 52.2 | 46.3 | 38.8*** |
| Former | 28.8 | 30.5 | 30.9 | 29.0 | 30.4 | 30.9 | 23.4 | 29.6 | 36.9 |
| Current | 20.6 | 20.9 | 31.8 | 21.3 | 24.5 | 26.9 | 24.5 | 24.1 | 24.3 |
| Physical activity score4 | 30.4 (3.9) | 31.0 (4.0) | 33.0 (5.5)**** | 30.8 (4.4) | 31.6 (4.7) | 31.9 (4.8)** | 31.7 (4.5) | 31.5 (4.8) | 31.2 (4.8) |
| Frequency eating out | |||||||||
| Never/rarely | 33.8 | 31.5 | 20.0**** | 37.1 | 24.0 | 24.2**** | 28.9 | 26.7 | 28.7 |
| <1 time/wk | 49.1 | 49.8 | 43.7 | 44.1 | 52.9 | 46.7 | 47.9 | 47.8 | 47.5 |
| ≥1 time/wk | 17.0 | 18.8 | 36.3 | 18.9 | 23.1 | 29.1 | 23.2 | 25.4 | 23.8 |
| Perceived stress score5 | 23.9 (9.7) | 23.6 (9.0) | 23.3 (9.7) | 24.4 (8.8) | 23.0 (9.3) | 23.2 (10.1) | 24.1 (9.6) | 23.8 (9.3) | 22.8 (9.3) |
1Values are proportions (%) or means (SE). Analyses included ANOVA for continuous variables and chi-square test (or Fisher's exact test when appropriate) for categoric variables. The language-based questionnaire assesses Spanish compared with English language use and ranges from 0 to 100, with lower scores indicative of less acculturation (more Spanish) and higher scores indicative of more acculturation (more English). The psychological-based questionnaire assesses subjective sense of belonging and emotional attachment to US and Hispanic/Latino cultures and ranges from 0 to 50, with lower scores indicative of more Puerto Rican psychological orientation (lower acculturation) and higher scores indicative of more US-American psychological orientation (higher acculturation). Categories for language-based, psychological-based, and years living in the mainland United States are based on sample tertiles; the corresponding tertile score ranges are: language-based scale: 0–8.2 for more Spanish, 8.3–34.9 for bilingual, and 35–100 for more English; psychological-based scale: 0–15 for more Puerto Rican; 15–20 for bicultural; and 21–50 for more US. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001.
2Defined as responding “sometimes not enough to eat” or “often not enough to eat” to the USDA 10-item adult food security survey module screener question, “Which of these statements best described the food eaten in your household in the last 12 months?”
3Government food assistance is participation in the Supplemental Nutrition Assistance Program (SNAP), formerly food stamps.
4Physical activity scores were the sum of reported hours spent in typical activities over a 24-h period, multiplied by appropriate weighting factors associated with activity intensity/oxygen consumption. Higher scores indicate greater levels of physical activity.
5Higher scores on the Perceived Stress Scale (range 0–40) indicate higher perceived stress in life.
Dietary intake differed across tertiles of the language-based and psychological-based acculturation scales, but less so for years living in the mainland United States (Table 2). After adjusting for sex, age, and energy intake, participants in the highest (compared with lowest) tertile of the language-based scale (i.e., more English use) had higher intakes of saturated fat, trans fat, alcohol, vitamin D, calcium, magnesium, vegetables, and whole grains, and lower intakes of polyunsaturated fats, starches, starchy vegetables, and meat and poultry; they also adhered less to a traditional dietary pattern. Participants in the highest (compared with lowest) tertile of the psychological-based scale (i.e., more US orientation) tended to adhere less to the traditional dietary pattern while having higher AHEI and MeDS scores, higher intake of magnesium and vegetables, and lower intake of polyunsaturated fats and meat and poultry. Participants living in the United States >40 y had lower intakes of starchy vegetables compared with those living in the United States <32 y.
TABLE 2.
Dietary intake characteristics by tertile of acculturation construct for Puerto Rican adults living in Boston, MA1
| Language-based acculturation scale | Psychological-based acculturation scale | Years living in the mainland United States | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | More Spanish | Bilingual | More English | More Puerto Rican | Bicultural | More US | <32 y | 32–40 y | >40 y |
| Total energy, kcal/d | 2182 (44) | 2247 (40) | 2204 (42) | 2176 (41) | 2265 (43) | 2193 (40) | 2233 (43) | 2213 (42) | 2210 (42) |
| Total fat, g/d | 77.7 (0.7) | 75.9 (0.7) | 76.6 (0.7) | 76.8 (0.7) | 76.7 (0.7) | 76.2 (0.7) | 76.3 (0.7) | 77.6 (0.7) | 77.0 (0.7) |
| Saturated fat | 23.0 (0.3) | 22.6 (0.3) | 23.8 (0.3)* | 22.7 (0.3) | 23.2 (0.3) | 23.4 (0.3) | 23.2 (0.3) | 23.3 (0.3) | 23.2 (0.3) |
| PUFA | 21.6 (0.3) | 20.9 (0.3) | 20.0 (0.3)* | 21.3 (0.3) | 20.8 (0.3) | 20.2 (0.3)* | 20.6 (0.3) | 21.1 (0.3) | 21.0 (0.3) |
| MUFA | 26.7 (0.3) | 26.2 (0.3) | 26.7 (0.3) | 26.5 (0.3) | 26.5 (0.3) | 26.5 (0.3) | 26.3 (0.3) | 27.0 (0.3) | 26.6 (0.3) |
| ω-3 | 1.7 (0.02) | 1.7 (0.02) | 1.7 (0.02) | 1.7 (0.02) | 1.7 (0.02) | 1.7 (0.02) | 1.7 (0.02) | 1.7 (0.02) | 1.7 (0.02) |
| trans Fat | 2.6 (0.1) | 2.6 (0.1) | 2.8 (0.1)* | 2.7 (0.1) | 2.7 (0.1) | 2.7 (0.1) | 2.6 (0.1) | 2.7 (0.1) | 2.7 (0.1) |
| Protein g/d | 89.5 (0.9) | 88.4 (0.8) | 88.0 (0.8) | 89.3 (0.8) | 88.7 (0.9) | 87.5 (0.8) | 88.9 (0.9) | 89.0 (0.8) | 88.8 (0.8) |
| Animal protein | 61.6 (0.9) | 59.6 (0.8) | 59.2 (0.9) | 60.9 (0.8) | 60.4 (0.9) | 58.7 (0.8) | 60.6 (0.9) | 60.5 (0.9) | 59.8 (0.9) |
| Plant protein | 27.9 (0.3) | 28.8 (0.3) | 28.8 (0.3) | 28.3 (0.3) | 28.2 (0.3) | 28.8 (0.3) | 28.3 (0.3) | 28.4 (0.3) | 29.0 (0.3) |
| Total carbohydrates, g/d | 264 (2.1) | 268 (2.0) | 264 (2.1) | 265 (2.0) | 265 (2.1) | 265 (2.0) | 269 (2.1) | 265 (2.1) | 265 (2.1) |
| Dietary fiber | 20.7 (0.3) | 21.1 (0.3) | 20.9 (0.3) | 20.7 (0.3) | 21.0 (0.3) | 20.9 (0.3) | 20.7 (0.3) | 21.1 (0.3) | 21.0 (0.3) |
| Added sugars | 56.2 (1.9) | 55.2 (1.8) | 57.3 (1.9) | 55.3 (1.8) | 57.7 (1.9) | 55.8 (1.8) | 56.2 (1.9) | 57.3 (1.9) | 55.9 (1.9) |
| Starch | 124 (1.4) | 125 (1.3) | 119 (1.4)* | 124 (1.3) | 121 (1.4) | 121 (1.3) | 122 (1.4) | 122 (1.4) | 123 (1.4) |
| Alcohol, g/d | 4.2 (0.8) | 5.0 (0.8) | 6.9 (0.8)* | 4.5 (0.8) | 5.2 (0.8) | 6.5 (0.8) | 4.6 (0.8) | 5.4 (0.8) | 6.3 (0.8) |
| Micronutrients | |||||||||
| Vitamin D, µg/d | 6.3 (0.2) | 6.7 (0.2) | 7.2 (0.2)* | 6.5 (0.2) | 6.7 (0.2) | 7.0 (0.2) | 6.7 (0.2) | 6.9 (0.2) | 6.6 (0.2) |
| Vitamin B-12, µg/d | 10.3 (0.3) | 9.6 (0.3) | 10.0 (0.3) | 10.3 (0.3) | 9.4 (0.3) | 10.0 (0.3) | 9.7 (0.3) | 10.0 (0.3) | 10.1 (0.3) |
| Vitamin B-6, µg/d | 2.6 (0.1) | 2.6 (0.1) | 2.7 (0.1) | 2.6 (0.1) | 2.6 (0.1) | 2.6 (0.1) | 2.6 (0.1) | 2.7 (0.1) | 2.6 (0.1) |
| Folate, µg/d | 524 (8.7) | 544 (8.1) | 551 (8.4) | 541 (8.2) | 528 (8.7) | 547 (8.1) | 531 (8.6) | 543 (8.4) | 549 (8.5) |
| Calcium, mg/d | 930 (23) | 962 (21) | 1033 (22)* | 946 (211) | 976 (23) | 1003 (22) | 989 (23) | 981 (22) | 969 (22) |
| Magnesium, mg/d | 321 (4.7) | 336 (4.4) | 349 (4.5)* | 327 (4.4) | 336 (4.7) | 343 (4.4)* | 331 (4.7) | 342 (4.5) | 337 (4.6) |
| Sodium, mg/d | 4835 (57) | 4766 (53) | 4747 (55) | 4811 (53) | 4768 (57) | 4727 (53) | 4710 (56) | 4869 (55) | 4800 (55) |
| Potassium, mg/d | 3011 (33) | 3130 (30) | 3124 (31) | 3095 (31) | 3131 (33) | 3131 (30) | 3179 (32) | 3119 (31) | 3098 (32) |
| Iron, mg/d | 20.1 (0.3) | 20.3 (0.3) | 20.2 (0.3) | 20.4 (0.3) | 19.8 (0.3) | 20.3 (0.3) | 20.0 (0.3) | 20.2 (0.3) | 20.6 (0.3) |
| Diet quality/food groups | |||||||||
| AHEI2 | 52.6 (0.5) | 53.7 (0.4) | 53.9 (0.4) | 52.7 (0.4) | 53.0 (0.5) | 54.6 (0.4)* | 53.5 (0.5) | 53.3 (0.4) | 53.7 (0.4) |
| MeDS3 | 4.2 (0.1) | 4.4 (0.1) | 4.5 (0.1) | 4.3 (0.1) | 4.4 (0.1) | 4.6 (0.1)* | 4.3 (0.1) | 4.3 (0.1) | 4.5 (0.1) |
| Vegetables, ser/d | 2.0 (0.1) | 2.2 (0.1) | 2.3 (0.1)* | 2.0 (0.1) | 2.2 (0.1) | 2.3 (0.1)* | 2.2 (0.1) | 2.3 (0.1) | 2.2 (0.1) |
| Starchy vegetables, ser/d | 0.6 (0.02) | 0.5 (0.02) | 0.4 (0.02)* | 0.5 (0.02) | 0.5 (0.02) | 0.5 (0.02) | 0.5 (0.02) | 0.5 (0.02) | 0.4 (0.02)* |
| Fruit, ser/d | 0.7 (0.03) | 0.7 (0.03) | 0.7 (0.03) | 0.7 (0.03) | 0.7 (0.03) | 0.8 (0.03) | 0.7 (0.03) | 0.7 (0.03) | 0.7 (0.03) |
| Whole grains, ser/d | 0.8 (0.1) | 1.0 (0.04) | 1.0 (0.04)* | 0.9 (0.04) | 0.9 (0.1) | 0.9 (0.04) | 0.8 (0.1) | 0.9 (0.04) | 1.0 (0.04) |
| Dairy, ser/d | 0.8 (0.1) | 0.9 (0.04) | 0.9 (0.1) | 0.8 (0.1) | 0.9 (0.1) | 0.9 (0.04) | 0.8 (0.1) | 0.9 (0.01) | 0.9 (0.1) |
| Fish, ser/d | 1.2 (0.1) | 1.2 (0.1) | 1.2 (0.1) | 1.2 (0.1) | 1.2 (0.1) | 1.3 (0.1) | 1.2 (0.1) | 1.3 (0.1) | 1.2 (0.1) |
| Meat and poultry, ser/d | 1.0 (0.04) | 0.9 (0.03) | 0.9 (0.03)* | 1.0 (0.03) | 1.0 (0.03) | 0.9 (0.03)* | 1.0 (0.03) | 0.9 (0.03) | 0.9 (0.03) |
| Nuts, ser/d | 0.6 (0.03) | 0.6 (0.03) | 0.6 (0.03) | 0.6 (0.13) | 0.6 (0.03) | 0.6 (0.03) | 0.6 (0.03) | 0.6 (0.03) | 0.6 (0.03) |
| Sugary beverages, ser/d | 1.4 (0.1) | 1.6 (0.1) | 1.5 (0.1) | 1.5 (0.1) | 1.5 (0.1) | 1.5 (0.1) | 1.6 (0.1) | 1.5 (0.1) | 1.5 (0.1) |
| Dietary pattern score | |||||||||
| Traditional pattern | 0.12 (0.1) | 0.11 (0.1) | −0.18 (0.1)* | 0.11 (0.1) | 0.03 (0.1) | −0.11 (0.1)* | 0.05 (0.1) | 0.03 (0.1) | −0.03 (0.1) |
| Western pattern | 0.18 (0.1) | 0.06 (0.04) | 0.10 (0.1) | 0.17 (0.04) | 0.11 (0.1) | 0.06 (0.04) | 0.09 (0.1) | 0.10 (0.1) | 0.15 (0.1) |
| Sweets and desserts pattern | 0.05 (0.1) | −0.01 (0.1) | −0.09 (0.1) | 0.02 (0.1) | −0.02 (0.1) | −0.07 (0.1) | −0.05 (0.1) | −0.05 (0.1) | 0.03 (0.1) |
1Presented as means (SEs), adjusted for age, sex, and energy (except total energy intake). The language-based questionnaire assesses Spanish compared with English language use and ranges from 0 to 100, with lower scores indicative of less acculturation (more Spanish) and higher scores indicative of more acculturation (more English). The psychological-based questionnaire assesses subjective sense of belonging and emotional attachment to US and Hispanic/Latino cultures and ranges from 0 to 50, with lower scores indicative of more Puerto Rican psychological orientation (lower acculturation) and higher scores indicative of more US-American psychological orientation (higher acculturation). Categories for language-based, psychological-based, and years living in the mainland United States are based on sample tertiles; corresponding tertile score ranges are: language-based scale: 0–8.2 for more Spanish, 8.3–34.9 for bilingual, and 35–100 for more English; psychological-based scale: 0–15 for more Puerto Rican; 15–20 for bicultural; and 21–50 for more US. Overall sample size was 1194 (for MeDS and food groups), 1337 (for AHEI), and 1380 (for dietary patterns and nutrient data). *P < 0.05. AHEI, Alternate Healthy Eating Index-2010; MeDS, Mediterranean Diet Score; ser/d, servings per day.
2The AHEI score was defined as a measure of overall diet quality based on 11 components with predefined recommended intakes and with overall scores ranging from 0 to 110, with higher scores indicative of better diet quality.
3The MeDS was defined as a measure of overall diet quality relative to the Mediterranean diet, based on population sex-specific median intake of 9 components. Overall scores range from 0 to 9, with high scores indicative of higher compliance with the Mediterranean diet.
In adjusted multivariable linear regression models, the language-based scale, psychological-based scale, and years living in the mainland United States were all inversely associated with a traditional dietary pattern, such that lower acculturation to the United States, as marked by any of the constructs, was associated with higher intake of the traditional rice, beans, and oils pattern (Table 3). The z score indicates that the strongest association with the traditional dietary pattern was observed for the language-based scale (β coefficient ± SE): −0.160 ± 0.032, followed by the psychological-based scale (−0.014 ± 0.004) and years in the United States (−0.005 ± 0.002). Only the psychological-based acculturation scale was significantly associated with the 2 diet quality scores, with positive associations with the AHEI (0.114 ± 0.037) and MeDS (0.015 ± 0.007) (i.e., higher psychological-based acculturation—or stronger US orientation—denoted better diet quality scores). No significant associations were observed for any of the acculturation constructs and the Western or the sweets and dairy desserts dietary patterns. Results were similar when adjusting for the other acculturation constructs in the model (data not shown).
TABLE 3.
β-Coefficients and SEs for associations between 3 different acculturation constructs and diet quality indexes or pattern scores for Puerto Rican adults living in Boston, MA1
| Language-based scale | Psychological-based scale | Years living in the mainland United States | ||||
|---|---|---|---|---|---|---|
| Diet score | β ± SE | P | β ± SE | P | β ± SE | P |
| AHEI2 | 0.002 ± 0.013 | 0.90 | 0.114 ± 0.037 | 0.002 | −0.005 ± 0.021 | 0.82 |
| z Scores | 0.004 ± 0.033 | 0.088 ± 0.029 | −0.006 ± 0.029 | |||
| MeDS3 | 0.0008 ± 0.003 | 0.75 | 0.015 ± 0.007 | 0.041 | 0.008 ± 0.004 | 0.05 |
| z Scores | 0.011 ± 0.034 | 0.063 ± 0.031 | 0.059 ± 0.031 | |||
| Traditional pattern | −0.007 ± 0.001 | <0.0001 | −0.014 ± 0.004 | 0.001 | −0.005 ± 0.002 | 0.041 |
| z Scores | −0.160 ± 0.032 | −0.097 ± 0.028 | −0.058 ± 0.028 | |||
| Western pattern | 0.0005 ± 0.001 | 0.71 | −0.007 ± 0.004 | 0.06 | 0.002 ± 0.002 | 0.28 |
| z Scores | 0.011 ± 0.029 | −0.048 ± 0.026 | 0.028 ± 0.026 | |||
| Sweets and desserts pattern | −0.003 ± 0.001 | 0.05 | −0.005 ± 0.004 | 0.20 | 0.002 ± 0.002 | 0.30 |
| z Scores | −0.061 ± 0.031 | −0.035 ± 0.028 | 0.029 ± 0.028 | |||
1Values are β-coefficients ± SEs presented for original scores, with the same models shown below using the z scores for direct comparison of the β-coefficients. Adjusted for age, sex, income, smoking status, education, physical activity, frequency of eating out, Supplemental Nutrition Assistance Program receipt, and energy intake (except for MeDS, which is already energy-adjusted). Overall sample size was 1194 (for MeDS), 1337 (for AHEI), and 1380 (for dietary patterns). AHEI, Alternate Healthy Eating Index-2010; MeDS, Mediterranean Diet Score.
2The AHEI score was defined as a measure of overall diet quality based on 11 components with predefined recommended intakes and with overall scores ranging from 0 to 110, with higher scores indicative of better diet quality.
3The MeDS was defined as a measure of overall diet quality relative to the Mediterranean diet, based on population median intake of whole cereals, nuts/legumes, fruit, vegetables, olive oil, fish, meat, sodium, and alcohol. Overall scores range from 0 to 9, with high scores indicative of higher compliance with the Mediterranean diet.
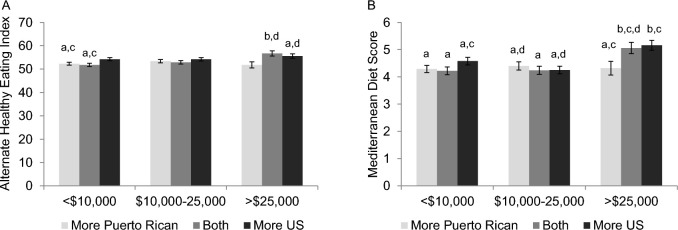
To test for potential effect modification of the associations between acculturation and diet by socioeconomic status or educational attainment, we included interaction terms between the acculturation constructs and education and income in association with diet quality. No significant interactions were observed for the language-based scale and education (AHEI, P-interaction = 0.60; MeDS, P-interaction = 0.66) or income (AHEI, P-interaction = 0.47; MeDS, P-interaction = 0.94), nor for years living in the mainland United States and education (AHEI, P-interaction = 0.70; MeDS, P-interaction = 0.44) or income (AHEI, P-interaction = 0.74; MeDS, P-interaction = 0.55). Educational attainment did not moderate the relation between the psychological-based scale and diet quality (AHEI, P-interaction = 0.45; MeDS, P-interaction = 0.57), but income did show significant interaction (AHEI, P-interaction = 0.033; MeDS, P-interaction = 0.034). After adjusting the interaction terms’ means for multiple comparisons, participants with higher household income (>$25,000) tended to have higher diet quality scores than those with lower household income (<$10,000), but only among those with bicultural or more US orientation; dietary quality was not greater with higher income among those with more Puerto Rican orientation (Figure 1 and Supplemental Table 1). Specifically, being in the highest income category (>$25,000) and classifying as bicultural (equal Puerto Rican and US orientation) or more US orientation was associated with the highest AHEI (mean ± SE: 56.7 ± 1.1 and 55.6 ± 0.92, respectively), unlike those in the same income category classifying as mostly Puerto Rican (51.8 ± 1.3; Figure 1A). Being in the lowest income category (<$10,000) and classifying mostly with US culture was associated with higher AHEI (54.2 ± 0.67) than being in the lowest income category and classifying as bicultural (51.8 ± 0.68) or mostly Puerto Rican (52.3 ± 0.64). Similar trends were observed for the MeDS (Figure 1B).
FIGURE 1.
Adjusted means ± SEs of diet quality score for the psychological-based acculturation scale, by household income categories for Puerto Rican adults living in Boston, MA. Values are means ± SEs obtained from models adjusted for age, sex, smoking status, education, physical activity, frequency of eating out, Supplemental Nutrition Assistance Program receipt, and energy intake (except for MeDS, which is already energy-adjusted). The AHEI score was defined as a measure of overall diet quality based on 11 components with predefined recommended intakes; overall scores range from 0 to 110, with higher scores indicative of better diet quality. The MeDS was defined as a measure of overall diet quality relative to the Mediterranean diet, based on population median intake of 9 components; overall scores range from 0 to 9, with high scores indicative of higher compliance with the Mediterranean diet. The psychological-based questionnaire assesses subjective sense of belonging and emotional attachment to US and Hispanic/Latino cultures and ranges from 0 to 50, with lower scores indicative of more Puerto Rican psychological orientation (lower acculturation) and higher scores indicative of more US-American psychological orientation (higher acculturation). Categories for the psychological-based scale are based on sample tertiles; the corresponding tertile score ranges are 0–15 for more Puerto Rican; 15–20 for bicultural; and 21–50 for more US. Sample size was 1194 for MeDS and 1337 for AHEI. Labeled means without a common letter differ, P < 0.05, after Tukey's procedure to adjust for multiple comparisons. AHEI, Alternate Healthy Eating Index-2010; MeDS, Mediterranean Diet Score.
Discussion
Among Puerto Rican adults living in the Boston, MA area, higher acculturation, as measured with constructs based on a bidimensional language scale (more English use), bidimensional psychological-based scale (stronger US orientation), or the unidimensional years of living in the mainland United States (longer), was associated with lower adherence to a traditional Puerto Rican dietary pattern. Importantly, results among Puerto Ricans differed by scale use; the language-based scale was more strongly inversely correlated to the traditional pattern. Only the psychological-based scale was positively related to diet quality, primarily at higher income levels. This is in direct contrast to most work on acculturation and diet in the Mexican-American population, where higher acculturation has been consistently associated with poorer diet quality (9, 10, 12). The mixed results indicate that dietary acculturation among Puerto Rican adults varies by acculturation construct and dietary measure. Bidimensional acculturation constructs, rather than single unidimensional proxy measures, may better capture associations with dietary outcomes in Puerto Rican adults.
Language-based acculturation in Puerto Ricans seems to be a fluctuating process that is connected to healthier as well as unhealthier dietary behaviors. Similar to our results, language-based acculturation was positively associated with a fruit and cereal pattern, and negatively with a rice pattern (reflecting a more traditional diet), among Puerto Rican and Dominican older adults living in Boston, MA (36). In contrast, predominately Mexican Hispanics/Latinos have shown poorer healthy food choices with increased English use and preference (9, 37–40). The mixed healthfulness of food and nutrient intake among our sample of Puerto Ricans (e.g., unhealthier fat intake but higher intake of vitamin D, calcium, and magnesium with more English use) may explain why language-based acculturation was not associated with overall diet quality. Moreover, the inconsistent results across Hispanic/Latino heritages suggest that language use may not be a universal marker of dietary acculturation for this group; heritage must be accounted for when selecting an acculturation construct.
In our study, higher psychological acculturation was associated with an overall healthier diet quality, differing from the usual hypothesis of unhealthy dietary behaviors having been gained in the United States (3, 9). The results also contrast to findings that higher US-American orientation was associated with lower diet quality scores in Mexican mothers living in California (41) and that higher ethnic identity was associated with higher intake of fiber and fruit/vegetables in ethnically diverse women with gestational diabetes (42); this highlights the population-specific dynamics of dietary acculturation. In Puerto Ricans, psychological-based scales may capture a distinct acculturation process. For example, a survey among adults in Puerto Rico found that the top reasons for planning to move to the mainland United States were to improve quality of life, to seek employment or for professional and financial reasons, for personal reasons, or to seek health services (43)—all suggestive of beliefs of “a better life” in the United States. A possible explanation may be that Puerto Ricans who have chosen to move to the United States seeking better healthcare or opportunities may be more exposed to health promotion messages or more open to trying healthy US dietary behaviors, and they may have favorable views of the United States, which then reflects as stronger US orientation in the psychological-based scale. A similar theme emerged from a qualitative study among Mexican-American women, for whom perceptions of Mexican foods as unhealthy and US diets as healthier may shape their diet choices during acculturation, even when Mexican foods remained central to maintaining their ethnic identity (44). Although perceptions of healthfulness may not translate into actual healthy eating behaviors for some ethnic groups owing to socio-ecological barriers, future research should further explore if Puerto Ricans with positive links to the US food and health system have healthier behaviors. Measuring psychological-based acculturation may be useful for developing appropriate programs targeting dietary behaviors of immigrant groups (8).
The opposite direction of associations noted in our study between psychological-based acculturation and diet quality compared with traditional dietary patterns suggests that these 2 outcomes capture different dietary frameworks (overall diet healthfulness compared with food patterns clustered by cultural orientation independent of healthfulness), and that the traditional dietary pattern may not correlate with diet quality (the traditional pattern was significantly but weakly correlated with AHEI and MeDS; r = 0.11 and r = 0.11, respectively, both P < 0.001).
Notably, income moderated the psychological acculturation–diet relation. In general, participants with high US orientation had higher diet quality even at low income, whereas those with more Puerto Rican orientation and high income had lower diet quality. In the same cohort, language-based acculturation was positively associated with intake of some healthy foods (i.e., fruit and nonstarchy vegetables) only among Puerto Ricans above the poverty line (19). Education did not moderate the acculturation-diet quality association, suggesting that income and education may influence dietary acculturation differently, despite their correlation. For example, higher education may affect language learning, whereas higher income may increase the affordability of healthy foods. Among mainland Puerto Rican households, lower acculturation has been associated with higher food insecurity (45), also indicative of a role of income in dietary outcomes, because food insecurity has been associated with lower diet quality and higher intake of unhealthy foods among ethnically diverse low-income adults (46–48). In Hispanic/Latino adults participating in the NHANES, interactions between acculturation and poverty:income ratio or education status on health behavior outcomes were not detected (49), suggesting that these income-related dynamics may be heritage-specific.
Lower acculturation, as measured by any of the constructs evaluated, was associated with higher adherence to a traditional dietary pattern, and the language-based scale more strongly denoted this association. For this cohort of Puerto Ricans, language use may be a complex process unrelated to overall diet quality but relevant for traditional food choices. Those who use more Spanish may be more likely to live in predominately Puerto Rican neighborhoods where the heritage's culture and practices can be retained (50), including traditional cooking, access to traditional foods in ethnic stores, or social contact. This, in turn, may reinforce stronger ethnic and cultural preferences for traditional foods, an association that was also noted in our study. Other studies have shown similar environmental influences on dietary acculturation for immigrant groups (51, 52). Living in a neighborhood with a high density of immigrants in Los Angeles County, CA, attenuated the negative association between acculturation and healthy eating behaviors (51). Nonetheless, Puerto Rican women in New York City, compared with Mexican women, had higher adherence to an energy-dense dietary pattern even after controlling for neighborhood linguistic isolation (53), suggesting that Puerto Ricans’ unhealthy habits may be influenced by more than linguistic isolation. Of note, years of living in the mainland United States, a unidimensional proxy measure of acculturation, does not seem to be a strong dietary acculturation construct for Puerto Ricans because it was only associated with a traditional diet pattern and other bidimensional constructs provided stronger associations, even when accounting for circular migration.
Our findings should be considered in the context of overall poor diet quality (15) and unhealthy dietary patterns (34) among US Puerto Ricans. The Western and the sweets and dairy desserts patterns (both unhealthy) were not associated with any acculturation construct in our analysis. It may be possible that some unhealthy behaviors are already present in Puerto Rico and carry through to the mainland United States. Studies indicate that Puerto Rico residents are consuming Western fast foods (54), poor-quality carbohydrates (55), sugar-sweetened beverages, and have low fiber, fruit, and vegetable intake (54, 56, 57). For Puerto Ricans with stronger ethnic orientation who may reside in ethnocentric communities, it may be expected that having continued contact with their native culture could be beneficial for dietary behaviors (58); however, the associations detected here indicate the opposite, suggesting that diets in Puerto Rico may indeed not be as healthy.
This study has several notable strengths, including adding to a limited evidence base of dietary acculturation among Hispanics/Latinos beyond those of Mexican heritage or the overall Hispanic/Latino population (9). We also contrasted different acculturation constructs using validated scales or accurate years of living in the United States accounting for circular migration, thus providing new insights into diet-related acculturation measurement tools to help inform future studies on acculturation and dietary or health outcomes, because they seem to differ by construct used. Having various diet-related outcomes—all captured with a validated culture-specific dietary assessment tool—further contributes to the validity of results. Finally, our sample was based on a population at high risk of chronic disease, an important aspect to accurately operationalize acculturation (6).
Limitations of this study include cross-sectional analyses and lack of a mainland US–born comparison group, which may provide insights into how dietary acculturation shapes health factors by place of birth (59). Income (60) or financial hardship (61) may be more accurately represented as a mediator, given that acculturation may drive increases in income which then improves diet. Further longitudinal analysis may be able to ascertain this. Our sample of older Boston-Puerto Rican adults may limit generalizability, especially because middle-aged and older immigrants may be more likely to adhere to traditional diets (62). Future research on diet-related acculturation with Puerto Ricans across the mainland United States should include a greater range of ages, sociodemographic backgrounds, and family and neighborhood contexts. Because our study was not framed within a particular acculturation model, future studies should explore acculturation theories and scales, especially those accounting for biculturalism (50).
In conclusion, it is important to appropriately select dietary acculturation constructs and to differentiate by heritage to account for specific acculturation dynamics (3, 12, 26). Our findings emphasize the need to determine how language compared with cultural orientation may define dietary behaviors in other Hispanic/Latino heritages as well as other ethnic minority groups, and reiterate that dietary acculturation may include both positive and negative behaviors (63). Although the acculturation process cannot be changed, knowing this information can help focus programs and interventions to promote healthier nutrition (9, 58) among Puerto Ricans with higher Spanish use and stronger ethnic orientation, with emphasis on those of low income.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—JM: designed the research question and analyzed the data; ACM: assisted with data analysis and wrote portions of the manuscript; JM and ACM: interpreted the results; SEN, LMF, and KLT: conducted the research study and contributed meaningfully to the interpretation of results; JM: wrote the manuscript, and has primary responsibility for final content; and all authors: read and approved the final manuscript.
Notes
Supported by the National Heart, Lung, and Blood Institute (NHLBI) grant P50-HL105185 (to KLT); National Institute on Aging grants P01-AG023394 and R01-AG055948 (to KLT); a Mentored Career Development Award to Promote Faculty Diversity in Biomedical Research (K01-HL120951) from the NIH/NHLBI (to JM); and NIH/National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) grant K01-AR067894 (to SEN). ACM was supported by an NIH Ruth L. Kirschstein Institutional Training Grant Postdoctoral Fellowship (T32 DK 7703–23).
Supplemental Table 1 is available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/jn/.
Author disclosures: JM, ACM, LMF, SEN, and KLT, no conflicts of interest.
References
- 1. Berry JW, Trimble J, Olmedo EL. Assessment of acculturation. In: Loner WJ, Berry JW, editors. Field methods in cross-cultural research. Beverly Hills, CA: Sage; 1986. [Google Scholar]
- 2. Daviglus ML, Pirzada A, Durazo-Arvizu R, Chen J, Allison M, Aviles-Santa L, Cai J, Gonzalez HM, Kaplan RC, Schneiderman N et al. . Prevalence of low cardiovascular risk profile among diverse Hispanic/Latino adults in the United States by age, sex, and level of acculturation: the Hispanic Community Health Study/Study of Latinos. J Am Heart Assoc 2016;5(8):e003929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Perez-Escamilla R. Acculturation, nutrition, and health disparities in Latinos. Am J Clin Nutr 2011;93(5):1163S–7S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Satia-Abouta J, Patterson RE, Neuhouser ML, Elder J. Dietary acculturation: applications to nutrition research and dietetics. J Am Diet Assoc 2002;102(8):1105–18. [DOI] [PubMed] [Google Scholar]
- 5. Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: a systematic review of public health studies with Hispanic populations in the United States. Soc Sci Med 2009;69(7):983–91. [DOI] [PubMed] [Google Scholar]
- 6. Fox M, Thayer Z, Wadhwa PD. Assessment of acculturation in minority health research. Soc Sci Med 2017;176:123–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Perez-Escamilla R. Dietary quality among Latinos: is acculturation making us sick? J Am Diet Assoc 2009;109(6):988–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Matsudaira T. Measures of psychological acculturation: a review. Transcult Psychiatry 2006;43(3):462–87. [DOI] [PubMed] [Google Scholar]
- 9. Ayala GX, Baquero B, Klinger S. A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. J Am Diet Assoc 2008;108(8):1330–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Arandia G, Nalty C, Sharkey JR, Dean WR. Diet and acculturation among Hispanic/Latino older adults in the United States: a review of literature and recommendations. J Nutr Gerontol Geriatr 2012;31(1):16–37. [DOI] [PubMed] [Google Scholar]
- 11. Van Wieren AJ, Roberts MB, Arellano N, Feller ER, Diaz JA. Acculturation and cardiovascular behaviors among Latinos in California by country/region of origin. J Immigr Minor Health 2011;13(6):975–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lara M, Gamboa C, Kahramanian MI, Morales LS, Hayes Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health 2004;26(1):367–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Abraido-Lanza AF, Echeverria SE, Florez KR. Latino immigrants, acculturation, and health: promising new directions in research. Annu Rev Public Health 2016;37:219–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bodvarsson OB, Van den Berg H. Hispanic immigration to the United States. In: Bodvarsson OB, Van den Berg H, editors. The economics of immigration: theory and policy. Berlin and Heidelberg: Springer-Verlag; 2009. [Google Scholar]
- 15. Mattei J, Sotres-Alvarez D, Daviglus ML, Gallo LC, Gellman M, Hu FB, Tucker KL, Willett WC, Siega-Riz AM, Van Horn L et al. . Diet quality and its association with cardiometabolic risk factors vary by Hispanic and Latino ethnic background in the Hispanic Community Health Study/Study of Latinos. J Nutr 2016;146(10):2035–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Duany J. Nation on the move: the construction of cultural identities in Puerto Rico and the diaspora. American Ethnologist 2000;27:5–30. [Google Scholar]
- 17. Urzúa A, Gómez E. Home style Puerto Rican: a study of language maintenance and use in New England. J Multiling Multicult Dev 2008;29(6):449–66. [Google Scholar]
- 18. Hromi-Fiedler A, Bermudez-Millan A, Segura-Perez S, Perez-Escamilla R. Nutrient and food intakes differ among Latina subgroups during pregnancy. Public Health Nutr 2012;15(2):341–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van Rompay MI, McKeown NM, Castaneda-Sceppa C, Falcón LM, Ordovas JM, Tucker KL. Acculturation and sociocultural influences on dietary intake and health status among Puerto Rican adults in Massachusetts. J Acad Nutr Diet 2012;112(1):64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bermudez OI, Falcón LM, Tucker KL. Intake and food sources of macronutrients among older Hispanic adults: association with ethnicity, acculturation, and length of residence in the United States. J Am Diet Assoc 2000;100(6):665–73. [DOI] [PubMed] [Google Scholar]
- 21. Fitzgerald N. Acculturation, socioeconomic status, and health among Hispanics. NAPA Bulletin 2010;34:28–46. [Google Scholar]
- 22. Tucker KL, Mattei J, Noel SE, Collado BM, Mendez J, Nelson J, Griffith J, Ordovas JM, Falcon LM. The Boston Puerto Rican Health Study, a longitudinal cohort study on health disparities in Puerto Rican adults: challenges and opportunities. BMC Public Health 2010;10:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Center for Puerto Rican Studies. Puerto Ricans in U.S., 2010 socio-economic conditions data sheet. Report Number: Centro DS2010US-01. New York, NY: 2012. [Google Scholar]
- 24. Satia JA. Dietary acculturation and the nutrition transition: an overview. Appl Physiol Nutr Metab 2010;35(2):219–23. [DOI] [PubMed] [Google Scholar]
- 25. Abraido-Lanza AF, Armbrister AN, Florez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. Am J Public Health 2006;96(8):1342–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Matias SL, Stoecklin-Marois MT, Tancredi DJ, Schenker MB. Adherence to dietary recommendations is associated with acculturation among Latino farm workers. J Nutr 2013;143(9):1451–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Norman S, Castro C, Albright C, King A. Comparing acculturation models in evaluating dietary habits among low-income Hispanic women. Ethn Dis 2004;14(3):399–404. [PubMed] [Google Scholar]
- 28. Marin G, Gamba RJ. A new measurement of acculturation for Hispanics: the Bidimensional Acculturation Scale for Hispanics (BAS). Hisp J Behav Sci 1996;18(3):297–316. [Google Scholar]
- 29. Tropp LR, Erkut S, Coll CG, Alarcon O, Vazquez Garcia HA. Psychological acculturation: development of a new measure for Puerto Ricans on the U.S. mainland. Educ Psychol Meas 1999;59(2):351–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tucker KL, Bianchi LA, Maras J, Bermudez OI. Adaptation of a food frequency questionnaire to assess diets of Puerto Rican and non-Hispanic adults. Am J Epidemiol 1998;148(5):507–18. [DOI] [PubMed] [Google Scholar]
- 31. Ye X, Scott T, Gao X, Maras JE, Bakun PJ, Tucker KL. Mediterranean diet, healthy eating index 2005, and cognitive function in middle-aged and older Puerto Rican adults. J Acad Nutr Diet 2013;113(2):276–81.e1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mattei J, Sotos-Prieto M, Bigornia SJ, Noel SE, Tucker KL. The Mediterranean diet score is more strongly associated with favorable cardiometabolic risk factors over 2 years than other diet quality indexes in Puerto Rican adults. J Nutr 2017;147(4):661–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, Stampfer MJ, Willett WC. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr 2012;142(6):1009–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Noel SE, Newby PK, Ordovas JM, Tucker KL. A traditional rice and beans pattern is associated with metabolic syndrome in Puerto Rican older adults. J Nutr 2009;139(7):1360–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mattei J, Noel SE, Tucker KL. A meat, processed meat, and French fries dietary pattern is associated with high allostatic load in Puerto Rican older adults. J Am Diet Assoc 2011;111(10):1498–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lin H, Bermudez OI, Tucker KL. Dietary patterns of Hispanic elders are associated with acculturation and obesity. J Nutr 2003;133(11):3651–7. [DOI] [PubMed] [Google Scholar]
- 37. Langellier BA, Brookmeyer R, Wang MC, Glik D. Language use affects food behaviours and food values among Mexican-origin adults in the USA. Public Health Nutr 2015;18(2):264–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bolstad AL, Bungum T. Diet, acculturation, and BMI in Hispanics living in southern Nevada. Am J Health Behav 2013;37(2):218–26. [DOI] [PubMed] [Google Scholar]
- 39. Montez JK, Eschbach K. Country of birth and language are uniquely associated with intakes of fat, fiber, and fruits and vegetables among Mexican-American women in the United States. J Am Diet Assoc 2008;108(3):473–80. [DOI] [PubMed] [Google Scholar]
- 40. Yoshida YX, Simonsen N, Chen L, Zhang LU, Scribner R, Tseng TS. Sociodemographic factors, acculturation, and nutrition management among Hispanic American adults with self-reported diabetes. J Health Care Poor Underserved 2016;27(3):1592–607. [DOI] [PubMed] [Google Scholar]
- 41. Martin CL, Tate DF, Schaffner A, Brannen A, Hatley KE, Diamond M, Munoz-Christian K, Pomeroy J, Sanchez T, Mercado A et al. . Acculturation influences postpartum eating, activity, and weight retention in low-income Hispanic women. J Womens Health (Larchmt) 2017;26(12):1333–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Brown SD, Ehrlich SF, Kubo A, Tsai AL, Hedderson MM, Quesenberry CP Jr, Ferrara A. Lifestyle behaviors and ethnic identity among diverse women at high risk for type 2 diabetes. Soc Sci Med 2016;160:87–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mattei J, Tamez M, Rios-Bedoya CF, Xiao RS, Tucker KL, Rodriguez-Orengo JF. Health conditions and lifestyle risk factors of adults living in Puerto Rico: a cross-sectional study. BMC Public Health 2018;18(1):491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ramirez AS, Golash-Boza T, Unger JB, Baezconde-Garbanati L. Questioning the dietary acculturation paradox: a mixed-methods study of the relationship between food and ethnic identity in a group of Mexican-American women. J Acad Nutr Diet 2018;118(3):431–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Dhokarh R, Himmelgreen DA, Peng YK, Segura-Perez S, Hromi-Fiedler A, Perez-Escamilla R. Food insecurity is associated with acculturation and social networks in Puerto Rican households. J Nutr Educ Behav 2011;43(4):288–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mello JA, Gans KM, Risica PM, Kirtania U, Strolla LO, Fournier L. How is food insecurity associated with dietary behaviors? An analysis with low-income, ethnically diverse participants in a nutrition intervention study. J Am Diet Assoc 2010;110(12):1906–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower-income adults. J Acad Nutr Diet 2014;114(12):1943–53.e2. [DOI] [PubMed] [Google Scholar]
- 48. Hanson KL, Connor LM. Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr 2014;100(2):684–92. [DOI] [PubMed] [Google Scholar]
- 49. Mainous AG 3rd, Diaz VA, Geesey ME. Acculturation and healthy lifestyle among Latinos with diabetes. Ann Fam Med 2008;6(2):131–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: implications for theory and research. Am Psychol 2010;65(4):237–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Zhang D, van Meijgaard J, Shi L, Cole B, Fielding J. Does neighbourhood composition modify the association between acculturation and unhealthy dietary behaviours? J Epidemiol Community Health 2015;69(8):724–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Weisberg-Shapiro P, Devine CM. “Because we missed the way that we eat at the middle of the day:” dietary acculturation and food routines among Dominican women. Appetite 2015;95:293–302. [DOI] [PubMed] [Google Scholar]
- 53. Park Y, Neckerman K, Quinn J, Weiss C, Jacobson J, Rundle A. Neighbourhood immigrant acculturation and diet among Hispanic female residents of New York City. Public Health Nutr 2011;14(9):1593–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Colon-Ramos U, Perez-Cardona CM, Monge-Rojas R. Socio-demographic, behavioral, and health correlates of nutrition transition dietary indicators in San Juan, Puerto Rico. Rev Panam Salud Publica 2013;34(5):330–5. [PMC free article] [PubMed] [Google Scholar]
- 55. Mattei J, Malik V, Wedick NM, Hu FB, Spiegelman D, Willett WC, Campos H. Reducing the global burden of type 2 diabetes by improving the quality of staple foods: the Global Nutrition and Epidemiologic Transition Initiative. Global Health 2015;11:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Soltero SM, Palacios C. Association between dietary patterns and body composition in a group or Puerto Rican obese adults: a pilot study. P R Health Sci J 2011;30(1):22–7. [PMC free article] [PubMed] [Google Scholar]
- 57. Colon-Lopez V, Banerjee G, Gertz AM, Ortiz AP, Calo W, Finney-Rutten LJ, Colon-Ramos U, Hesse BW, Tortolero G. Behavioral correlates of fruit and vegetable intake in Puerto Rico: results from the Health Information National Trends Survey. P R Health Sci J 2013;32(4):194–9. [PMC free article] [PubMed] [Google Scholar]
- 58. Andreeva VA, Unger JB. Host society acculturation and health practices and outcomes in the United States: public health policy and research implications worldwide. J Public Health Policy 2014;35(3):278–91. [DOI] [PubMed] [Google Scholar]
- 59. Van Hook J, Quiros S, Frisco ML. The food similarity index: a new measure of dietary acculturation based on dietary recall data. J Immigr Minor Health 2015;17(2):441–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lopez EB, Yamashita T. Acculturation, income and vegetable consumption behaviors among Latino adults in the U.S.: a mediation analysis with the bootstrapping technique. J Immigr Minor Health 2017;19(1):155–61. [DOI] [PubMed] [Google Scholar]
- 61. Allen JD, Caspi C, Yang M, Leyva B, Stoddard AM, Tamers S, Tucker-Seeley RD, Sorensen GC. Pathways between acculturation and health behaviors among residents of low-income housing: the mediating role of social and contextual factors. Soc Sci Med 2014;123:26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Sofianou A, Fung TT, Tucker KL. Differences in diet pattern adherence by nativity and duration of US residence in the Mexican-American population. J Am Diet Assoc 2011;111(10):1563–9.e2. [DOI] [PubMed] [Google Scholar]
- 63. Batis C, Hernandez-Barrera L, Barquera S, Rivera JA, Popkin BM. Food acculturation drives dietary differences among Mexicans, Mexican Americans, and non-Hispanic whites. J Nutr 2011;141(10):1898–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.