Abstract
Background
Human papillomavirus (HPV) infection causes cervical cancer. More than 80% of those diagnosed with cervical cancer live in low- and middle-income countries (LMICs). The World Health Organization recommends vaccination as a public health measure against cervical cancer. Communication interventions are able to change how people think about vaccination and are thus instrumental in addressing vaccine hesitancy. Our aim was to provide a broad scoping overview of the available evidence on communication with adolescents, parents, and other stakeholders around HPV vaccination for adolescents, with a specific focus on LMICs.
Methods
We conducted a systematic scoping overview of systematic reviews addressing a range of questions regarding communication around HPV vaccination. We considered reviews published between 2007 and 2018 focusing on communication around HPV vaccination and that searched for qualitative or quantitative studies for inclusion. We searched the Epistemonikos database which includes reviews from multiple electronic databases. Two overview authors screened titles and abstracts and examined potentially eligible reviews in full text. Data extraction was performed by one overview author and verified by a second. We assessed the reliability of the included reviews using an adapted version of AMSTAR 2.
Results
We included twelve reviews in our overview. Four reviews assessed the effectiveness of communication interventions. These interventions intended to inform or educate about HPV and HPV vaccination, such as videos and fact sheets, or to remind or recall, such as text message reminders. Eight reviews assessed factors associated with HPV vaccination uptake, including communication-related factors such as whether the vaccine was recommended by a physician and people’s knowledge regarding the vaccine. Nine reviews searched for studies from LMICs, but most found only a small number of studies from these countries.
Conclusions
The small number of studies identified from LMICs is of concern as these countries face the largest burden of disease related to HPV. This scoping overview also found and excluded a number of reviews because of important methodological limitations, highlighting the need for future reviews to use appropriate methods. The overview indicates areas in which further primary studies are needed on HPV vaccination communication in LMICs.
Systematic review registration
Open Science Framework https://osf.io/agzb4/
Electronic supplementary material
The online version of this article (10.1186/s13643-019-1100-y) contains supplementary material, which is available to authorized users.
Keywords: HPV, Human papillomavirus, Vaccine, Communication, Intervention, Adolescents, Low-income countries, Middle-income countries, Low- and middle-income countries, Systematic scoping overview of systematic reviews
Background
Cervical cancer is the fourth most frequent cancer among women worldwide. Around 530,000 women are diagnosed with cervical cancer and around 265,000 women die from the disease every year [1]. Human papillomavirus (HPV) infection causes cervical cancer and there is growing evidence of HPV being a relevant factor in other anogenital and head and neck cancers. More than 80% of those diagnosed with cervical cancer live in low- and middle-income countries (LMICs) [1] where it is one of the leading causes of death by cancer. In Africa, cervical cancer is the primary cause of cancer death [1].
The HPV vaccine has one of the highest estimated per-person impacts on mortality of all vaccines [2] and is anticipated to prevent death in over 15 per 1000 persons vaccinated [3]. The World Health Organization (WHO) recommends the vaccination of 9–13-year-old girls as the most cost-effective public health measure against cervical cancer. The WHO also recommends investing in an HPV vaccine communication strategy at a country level that reflects the vaccine’s unique characteristics, including the newness of the vaccine, the fact that it is targeted at adolescents and pre-adolescents, and that it protects against a sexually transmitted disease [2].
Communication interventions can impact how people think and feel about vaccination and can be used to address aspects or factors contributing to vaccine hesitancy [2, 4]. It is therefore important to understand communication needs and gaps in relation to HPV vaccination and how these gaps are being addressed. It is also important to understand stakeholders’ views of these strategies; including those of adolescents, parents, other caregivers, and communities. Understanding these communication needs and gaps is especially important where the burden of cervical cancer and the need for implementation of HPV vaccination are highest. This systematic scoping overview of reviews, commissioned to inform discussion at a meeting of stakeholders in the WHO Africa Region, therefore, focuses on LMICs as defined by the World Bank [5].
Our findings can be used to prioritize areas where new or updated systematic reviews are needed on communication around HPV vaccination for adolescents, especially in LMICs. The findings can also be used to quickly identify reviews in this field. However, scoping overviews are not intended to synthesize results from the included reviews and this type of synthesis is therefore not presented in this overview. To our knowledge, no overviews of reviews have been conducted that summarize the available evidence on this topic.
Aim
Our aim was to undertake a systematic scoping overview of systematic reviews of the available evidence on communication with adolescents, parents, and other stakeholders around HPV vaccination for adolescents.
Our specific objectives were to do the following:
Identify systematic reviews on communication around HPV vaccination for adolescents
Briefly describe and summarize the scope of each review and the evidence identified, considering specifically the relevance of these reviews for LMICs
Identify areas in which new or updated systematic reviews are needed on communication around HPV vaccination for adolescents
As this was a scoping overview of reviews, we did not aim to synthesize the findings of the included systematic reviews.
Methods
This systematic scoping overview of systematic reviews used methods adapted from those used for scoping reviews of individual studies [6, 7]. Like scoping reviews, this scoping overview “aim[s] to map rapidly the key concepts underpinning a research area and the main sources and types of evidence available” [8]. Its methods are reported according to the PRISMA Extension for Scoping Reviews, and the PRISMA-ScR checklist is included as Additional file 1.
Criteria for considering reviews for this overview
Types of reviews
We included systematic reviews that focused on communication around HPV vaccination for male and female adolescents and addressed at least one of the following topic areas:
Reviews of quantitative and/or qualitative studies of HPV vaccination communication issues or problems identified by any of the stakeholders (see below). This could include issues such as people’s HPV information needs and how they would like to receive that information
Reviews of descriptive studies of the types of HPV vaccination communication interventions or strategies being used in different settings
Reviews of qualitative and/or quantitative studies of stakeholders’ views of different HPV vaccination communication interventions or strategies, as well as factors affecting the implementation of these interventions
Reviews of quantitative studies of the effectiveness of HPV vaccination communication interventions or strategies
Reviews of quantitative studies of the costs or cost-effectiveness of HPV vaccination communication interventions or strategies
Exclusion criteria are the following:
Reviews published before 2007 as we aimed to only include reviews published after the implementation of HPV vaccination programs [1]
Reviews published in languages other than English, Norwegian, Swedish or Danish as we did not have the capacity within the team to extract data from these reviews. We kept a list of those reviews that appeared eligible but were not published in these languages
Reviews that did not have a “Methods” section with explicit selection criteria for the inclusion of primary studies, or that had other important methodological limitations, as assessed using the approach described below
We did not exclude reviews that labeled themselves as scoping or rapid reviews.
Types of participants
Participants included one or both of the following groups:
Adolescents (defined as aged 10–26 years for the purposes of this review). Where the ages of participants were not disaggregated, we included reviews where there was explicit mention that at least 70% of participants were between the ages of 10–26 years
Other stakeholders such as parents, caregivers, families, communities, health care providers, and health service managers and policy-makers involved in HPV vaccination for adolescents
Types of outcomes and other types of information
We included reviews of the effectiveness and cost-effectiveness of communication strategies that measured any of the following outcomes:
Knowledge of HPV, the HPV vaccine, and HPV vaccine services
Attitudes towards HPV, the HPV vaccine, and HPV vaccine services
HPV vaccination status
Participants’ involvement in decision-making regarding HPV vaccination
Participants’ confidence in the decision made regarding HPV vaccination
Participants’ satisfaction with the health care provider
Unintended effects linked to HPV vaccination interventions
Health care provider outcomes (such as satisfaction with their involvement in the HPV vaccination communication program)
Social outcomes such as school enrollment
We included other types of reviews that reported on any of the following types of information:
Different types of HPV vaccination communication problems or interventions
Participants’ attitudes towards and views regarding HPV vaccination (the term “attitudes” covers beliefs about vaccination, and may include intention to vaccinate) and HPV vaccination communication interventions or strategies
Factors affecting the implementation of HPV vaccination communication interventions or strategies
The outcomes and other types of information were selected by three of the overview authors (HSF, AO, and SL) as the most relevant outcomes and other types of information in relation to providing an overview of the topic. As this was a systematic scoping overview of systematic reviews, we wanted to be as broad as possible regarding outcomes and other types of information.
Search methods for identification of studies
We searched for relevant systematic reviews in the Epistemonikos database of systematic reviews (https://www.epistemonikos.org/), published between 2007 and 2018 (database searched 31 May 2018). The following databases are searched to populate the Epistemonikos database, with no language or publication status restrictions: Cochrane Database of Systematic Reviews (CDSR), PubMed, Embase, CINAHL (The Cumulative Index to Nursing and Allied Health Literature), PsycINFO, LILACS (Literatura Latinoamericana y del Caribe en Ciencias de la Salud), Database of Abstracts of Reviews of Effects (DARE), The Campbell Collaboration online library, JBI Database of Systematic Reviews and Implementation, and EPPI-Centre Evidence Library. The full search strategy is provided in Additional file 2.
Data collection and analysis
Selection of reviews
Two overview authors independently screened titles and abstracts to identify potentially eligible reviews. We conducted a pilot screening of 20 full-text reviews to ensure agreement on our interpretation of the inclusion and exclusion criteria. Two overview authors examined potentially eligible reviews in full text to make a final decision on inclusion. Discrepancies were resolved either by a third overview author deciding on inclusion or through discussion between the two overview authors. Additional file 3 provides a complete list of reviews assessed in full text with reasons for exclusion. Table 1 provides a complete list of reviews excluded after data extraction for having important methodological limitations, using the approach described below.
Table 1.
Table of reviews excluded from data synthesis due to important methodological limitations
| Review | Methodological limitations (criterion number1) | Geographic settings of the included studies |
|---|---|---|
| Allen et al., 2010 [9] | Twelve minor limitations (2, 3, 4, 5, 7, 9, 10, 12, 13, 14, 15, 16) | U.S. (41 studies), Australia (5), Belgium (3), Brazil (2), Canada (n = 4), Columbia (n = 1), Finland (n = 1), Germany (n = 1): Hong Kong (n = 2), Iceland (n = 1), Mexico (n = 2), Netherlands (n = 1), Sweden (n = 1), Turkey (n = 1), UK (n = 10), and Vietnam (n = 1). Not specified: 2 |
| Brewer et al., 2007 [10] | One major limitation (9). Ten minor limitations (2, 3, 4, 6, 7, 10, 12, 13, 14, 15). | USA |
| Catalan-Matamoros et al., 2017 [11] | One major limitation (9). Nine minor limitations (4, 5, 6, 7, 10, 12, 13, 15, 16). |
Print media: US (n = 27), UK (n = 5), Canada (n = 8), Australia (n = 3), Israel (n = 1), Panama (n = 1), India (n = 1), China (n = 1), and Iran (n = 1). Television: US (n = 9). Radio: Australia (n = 1). Combination of media: US (n = 4) and Italy (n = 1) |
| Chan et al., 2012 [12] | One major limitation (9). Eleven minor limitations (2, 4, 5, 6, 7, 10, 12, 13, 14, 15). | Studies were conducted in Asia (n = 11), North America (n = 15), UK (n = 2), Europe (n = 6), and Australia (n = 2) |
| Crocker-Buque et al., 2017 [13] | One major limitation (9). Seven minor limitations (3, 6, 7, 10, 12, 13, 15). | US (n = 31), UK (n = 5), Canada (n = 3) and Australia (n = 2) |
| Cunningham et al., 2014 [14] | One major limitation (9). Nine minor limitations (2, 4, 5, 6, 10, 12, 13, 14, 15). | SSA: Botswana (1), South Africa (2), Nigeria (2), Kenya (3), Ghana (1), Uganda (1), Mali (1), Zambia (1), Tanzania (1) and Malawi (1) |
| Das et al., 2016 [15] | One major limitation (9). Nine minor limitations (2, 3, 4, 7, 10, 11, 12, 14, 15). | HICs. |
| Francis et al., 2017 [16] | One major limitation (9). Nine minor limitations (2, 4, 6, 7, 10, 12, 13, 15, 16). | USA |
| Galbraith et al., 2016 [17] | One major limitation (9). Eight minor limitations (2, 4, 5, 6, 7, 10, 13, 14). | N/R2 |
| Gilkey et al., 2016 [18] | One major limitation (9). Eight minor limitations (2, 4, 5, 6, 7, 10, 12, 14). | N/R2 |
| Holman et al., 2014 [19] | Two major limitations (4, 9). Nine minor limitations (1, 2, 5, 7, 10, 11, 12, 13, 14). | N/R2 |
| Hyde et al., 2012 [20] | One major limitation (9). Eleven minor limitations (2, 4, 5, 6, 7, 8, 10, 12, 13, 14, 16). | 97 (75%) were from high-income countries, 21 (16%) were from middle-income countries, and 4 (3%) were from low-income countries. |
| Kabakama et al., 2016 [21] | One major limitation (9). Nine minor limitations (2, 4, 5, 6, 7, 8, 10, 12, 13). | 37 low- and middle-income countries |
| Karafillakis et al., 2017 [22] | One major limitation (9). Eleven minor limitations (2, 3, 4, 5, 6, 7, 8, 10, 12, 13, 14). | The majority of articles included were from the UK (35.2%), the Netherlands (11.7%), France (11.7%), Germany (8.3%), Greece (7.6%), and Sweden (6.2%). |
| Kessels et al., 2012 [23] | Eight minor limitations (2, 3, 4, 5, 6, 7, 10, 16). | Mostly USA |
| Loke et al., 2017 [24] | Two major limitations (9, 13). Seven minor limitations (2, 3, 4, 5, 7, 10, 15). | Information only provided for 28 studies. Geographic settings such as countries or cities: 17, secondary schools: 4, unspecified schools: 4, health center or community clinic: 3, colleges: 1. One study had both random digit dialing as their study setting for mothers and schools for adolescents as their setting. |
| Mishra, 2011 [25] | Two major limitations (9, 13). Eight minor limitations (2, 4, 5, 6, 7, 10, 12, 14, 16). | N/R2 |
| Niccolai et al., 2015 [26] | One major limitation (9). Nine minor limitations (2, 3, 4, 5, 7, 10, 12, 13, 14). | USA |
| Paul et al., 2014 [27] | Two major limitations (4, 9). Eight minor limitations (2, 5, 6, 7, 10, 12, 13, 16). | Seventeen countries from Africa, Asia, Australia, Europe, Latin America, and North America are represented |
| Perlman et al., 2014 [28] | One major limitation (9). Nine minor limitations (2, 4, 5, 6, 7, 10, 12, 13, 14). | Cameroon: 5. Nigeria: 5. South Africa: 4. Tanzania: 4. Uganda: 3. Kenya: 2. Botswana: 1. Ghana: 1. Lesotho: 1. Mali: 1. Rwanda: 1. Zambia: 1. Zimbabwe: 1 |
| Rosen et al., 2018 [29] | One minor limitation (9). Nine minor limitations (2, 4, 5, 6, 7, 10, 12, 14, 15). | USA |
| Ryan et al., 2018 [30] | One major limitation (9). Eight minor limitations (2, 3, 4, 7, 10, 12, 13, 16). | Appalachian states and also all states including Appalachian regions (USA) |
| Small et al., 2014 [31] | One major limitation (9). Nine minor limitations (2, 4, 5, 6, 7, 10, 12, 13, 14). | USA |
| Smulian et al., 2016 [32] | Two major limitations (4, 9). Ten minor limitations (2, 3, 5, 6, 7, 10, 12, 13, 14, 15). | N/R2 |
| Walling et al., 2016 [33] | One major limitation (11). Seven minor limitations (2, 4, 5, 7, 10, 12, 14). | N/R2 |
| Wigle et al., 2013 [34] | One major limitation (9). Ten minor limitations (2, 4, 5, 6, 7, 8, 10, 12, 13, 14). | Items identified by the search included studies and experiences from individual countries (Peru, Vietnam, Uganda, India, Rwanda, Ghana, Tanzania, Malaysia, Indonesia, Kenya, Bhutan, Bolivia, Cambodia, Haiti, Lesotho and Nepal) and broad world regions. |
| Young, 2010 [35] | One major limitation (9). Eight minor limitations (2, 4, 5, 6, 10, 12, 14, 16). | The 18 articles selected for inclusion in this review represent nine countries. Australia (n = 6) and China (n = 4) accounted for over half of the studies; India, Korea, Malaysia, New Zealand, Taiwan, Thailand, and Vietnam were also represented. |
1As numbered in Additional file 4 which lists the criteria for assessing the reliability of reviews, adapted from AMSTAR 2
2N/R: not reported
Assessment of the reliability of included reviews
One overview author assessed the reliability of the individual reviews using an adapted version of A MeaSurement Tool to Assess systematic Reviews (AMSTAR 2) [36]. A second overview author verified the assessments. We adapted AMSTAR 2 to allow its application across the range of types of reviews included in this overview and to try to ensure its appropriateness to a scoping overview of this kind. This involved adapting the wording of some questions to allow assessment of reviews of descriptive studies, qualitative studies, surveys, and cost-effectiveness studies as well as reviews of studies of the effects of interventions. Adapting the wording of questions also involved simplifying the tool as we did not attempt to develop revised, comprehensive response categories for the adapted questions, as found in AMSTAR 2.
As we aimed to include as many relevant reviews as possible in this descriptive scoping overview, we assessed a review to have important methodological limitations only if it had one or more major methodological limitations or if, in the judgment of the overview authors, it had a large number of minor methodological limitations. A review was categorized as having a major limitation if it did not use a comprehensive literature search strategy, if it did not use a satisfactory technique for assessing the methodological limitations/risk of bias (RoB) for individual studies included in the review, or if it did not account for methodological limitations/RoB in individual studies when interpreting/discussing the results of the review. All other concerns were described as minor limitations. The adapted AMSTAR 2 criteria used in this overview are available in Additional file 4.
Data extraction and management
We designed a data extraction form (included as Additional file 5) and piloted it on two reviews to test the form and ensure agreement on which content was to be extracted.
For each included review, one overview author extracted the following data, which were then verified by a second overview author:
Review characteristics such as review objectives, number of included studies, proposed and included publication range, study designs, populations, geographic and health system settings, interventions, and comparison
Secondly, for reviews that did not have important limitations as assessed using the adapted AMSTAR 2 criteria listed in Additional file 4, we extracted data on the key findings and conclusions relevant to our overview question.
Assessment of the applicability of the evidence to LMICs
We assessed the applicability of the evidence to LMIC settings using an approach similar to that used in several recent Cochrane Effective Practice and Organisation of Care Group (EPOC) overviews of reviews [37]. This approach was also adapted to the range of reviews included in this scoping overview. Our assessment was based on the following questions:
Were some or all of the studies included in the systematic review conducted in LMICs or were the findings in the review consistent across settings or time periods and therefore suggest wide applicability?
Are there important differences in on-the-ground realities and constraints in LMICs, such as people’s access to health services or to communication sources that might substantially alter the feasibility and acceptability of the intervention (where applicable) or raise questions about the applicability of the review findings?
Are there important differences in health system arrangements, such as how HPV vaccination is financed or delivered, that may mean an intervention could not work in the same way in LMICs or review findings may not be applicable to LMICs?
The methods for this scoping overview were specified in a protocol prior to the piloting of the study selection process. It included our overview questions, search strategy, inclusion and exclusion criteria, and the methods for a future reliability assessment. The protocol is available via the Open Science Framework (see https://osf.io/agzb4/).
Results
Our search yielded 461 records. After screening titles and abstracts, we excluded 387 records. We assessed 74 reviews in full text of which 39 were potentially eligible for inclusion. Our assessment of methodological limitations led to the exclusion of a further 27 reviews, resulting in 12 included reviews. Additional file 3 lists the reasons for exclusion for reviews assessed in full text and Table 1 describes the methodological limitations of the reviews excluded because of concerns regarding their reliability (see also Additional file 6 for a list of reviews for which no full text was available). A PRISMA Flow Diagram [38] is included as Fig. 1.
Fig. 1.
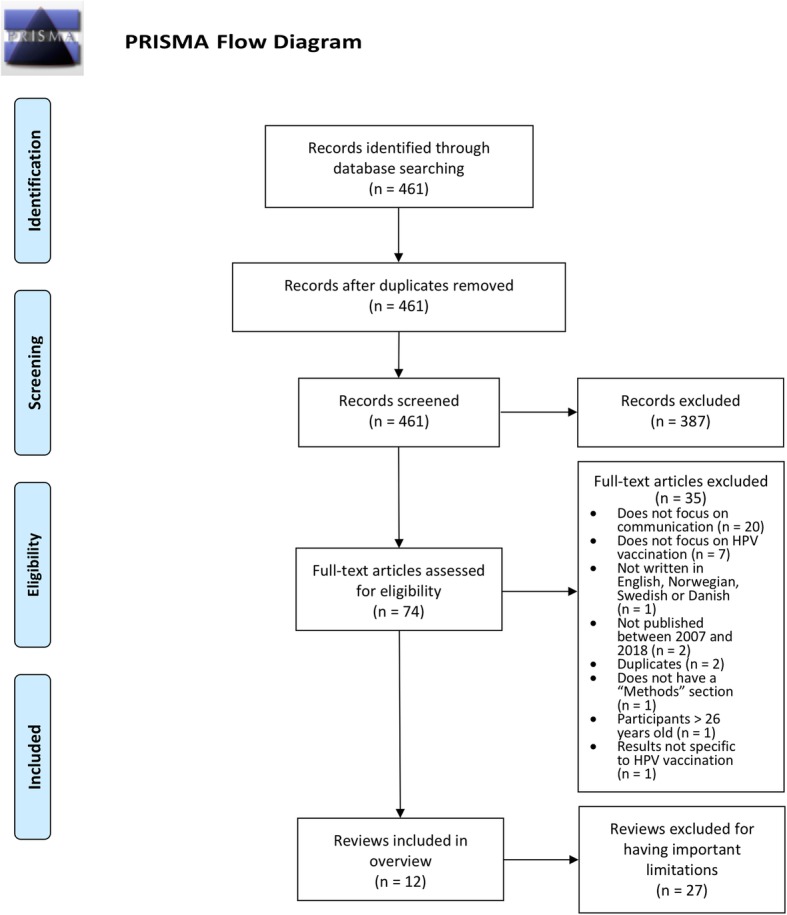
PRISMA Flow Diagram
Summary description of included reviews
A summary of the characteristics of the studies included in the reviews can be found in Table 2. The number of included studies included in the reviews ranged from five to 79, and over half of the reviews included over 20 studies. The years of publication for studies included in the reviews ranged from 1996 to 2017. Over half of the reviews only found eligible studies published after 2008. The types of studies found included quantitative designs, such as randomized controlled trials, quasi-experimental designs, cross-sectional studies and surveys, and studies that used qualitative methods. The types of studies that were included in each review differed based on the review aim. The populations of the studies were mostly adolescent females, but some reviews included other stakeholders such as parents [45, 47, 48]. The geographic settings were mostly high-income countries (HICs) (see Table 2). Where reported, the health systems settings were mostly primary care [4, 40–42, 44, 45, 48, 49]. The reviews also found studies conducted in educational settings such as schools and universities [4, 40–42, 44, 49]. Further information on the funding and conflicts of interests reported for the included reviews is provided in Additional file 7.
Table 2.
Table of characteristics of reviews with only minor methodological limitations
| Review | N | Years of publication of included studies | Study designs1 | Interventions or strategies3 | Populations2 | Geographical settings |
|---|---|---|---|---|---|---|
| Abdullahi et al., 2016 [39] | 18 | 2008–2014 | Cross-sectional: 17. Qualitative: 1 | Sensitization campaigns and communication strategies: 3 |
Adolescent: 9 Parents: 14 Teachers: 2 |
South Africa: 6. Cameroon: 2. Uganda: 2. Nigeria: 2. Kenya: 1. Ghana: 1. Tanzania: 1. Botswana: 1. Mali: 1. Malawi: 1 |
| Badawy et al., 2017 [40] | 19 | 2010–2016 | RCT: 11. Pre-post pilot design: 6. QES: 2 |
Reminder: 15 Mobile phone app platform intervention: 4 |
Adolescents (12-24): 19 | USA: 9. Switzerland: 3. Hong Kong: 2. Colombia: 1. Wales: 1. Italy: 1. New Zealand: 1. Germany: 1 |
| Ferrer et al., 2014 [41] | 41 | 2004–2012 | N/R4 | N/A5 | N/R4 | USA: 24. Uke: 9. Australia: 3. Sweden: 2. Hong Kong. 2. Canada: 1 |
| Fu et al., 2014 [4] | 33 | 2004–2013 |
RCT: 10 N/R4: 23 |
Educational intervention: 15 Comparative message persuasiveness: 18 |
Parents: 12. Parents of girls: 5. Parents of either sex: 2. Adolescents (12-26): 21. Only women: 7. Only men: 3. Both: 3 Adults: 1 |
USA: 21. Canada: 3. Australia: 2. England: 2. China: 1. India: 1. Ireland: 1. Hong Kong: 1. Sweden: 1 |
| Hendry et al., 2013 [42] | 72 | 2004–2011 | Qualitative: 28. Surveys: 44 | N/A5 | Adolescents (7-26) or their parents. Mostly women | USA: 32. UK: 15. Australia: 4. Malaysia: 3. India: 3. Canada: 3. Hong Kong: 2. Sweden: 2. Italy: 2. Thailand: 1. Brazil: 1. Vietnam: 1. Netherlands: 1. Korea: 1. Korea, Taiwan, Thailand and Malaysia: 1 |
| Johnson et al., 2018 [43] | 53 | 1996–2017 |
Cross-sectional: 34 Pre-posttest: 10 RCT: 8 Non-RCT: 1 |
Education strategies: 38 Restructure strategies: 26 Quality strategies: 13 |
N/R4 | Southern Africa: 16. Western Africa: 16. Eastern Africa: 14. Middle Africa: 7 |
| Kang et al., 2018 [44] | 5 | 2013–2016 |
RCT: 3 Cluster RCT: 2 |
Reminders: 5 Reminders and education: 3 |
Mostly female adolescents (9-26) One study included males (11-17) | USA |
| Kim et al., 2017 [45] | 22 | 2009–2015 |
Quantitative: 16 Qualitative 6 |
A culturally tailored Spanish educational radionovela | Parents, mostly of female adolescents: 22 Only mothers (18-64): 15 | USA |
| Newman et al., 2013 [46] | 24 | N/R4 | Cross-sectional studies: 27. Cohort studies: 2 | N/A5 |
Adult men: 21 Boys (14-19): 2 |
USA: 12. Australia: 3. Sweden: 2. Canada: 1. Germany: 1. Netherlands: 1. New Zealand: 1. Philippines: 1. Singapore: 1. South Korea: 1 |
| Newman et al., 2018 [47] | 79 | 2009–2017 |
Cross-sectional: 67 Longitudinal: 7 Cohort: 1 Case-control: 1 QES: 1 Clustered non-RCT: 1 Cluster-RCT: 1 |
N/A5 |
Parents of girls: 45 Parents of boys: 10 Parents of either: 24 Sex of parents: Both: 44. Mothers: 24. Not specified: 11 |
USA: 55. Canada: 4. Denmark: 2. Norway: 2. Puerto Rico: 2. Australia: 1. Fiji: 1. Hong Kong: 1. Italy: 1. Kenya: 1. South Africa: 1. Tanzania: 1. Turkey: 1. United Arab Emirates: 1. Vietnam: 1 |
| Radisic et al., 2016 [48] | 18 | 2010–2015 |
Quantitative: 14 Qualitative: 3 Mixed-methods: 1 |
N/A5 | Parents, mostly of male adolescents (9-26) | USA: 12. Canada: 2. Italy: 2. Denmark: 2 |
| Rambout et al., 2013 [49] | 22 | 2008–2011 |
Quantitative: 19 Qualitative: 1 Mixed-methods: 2 |
N/A5 | Adolescents (26 years or younger) | USA: 21. Canada: 1 |
1The study design terms listed here are those reported in the individual reviews. They are therefore not consistent across reviews
2The ages of the participants have been included when reported
3This column reports only the number of studies of interventions of strategies included in the reviews. Not all reviews included interventions as some focused on stakeholders’ views of communication interventions and of factors affecting their implementation
4N/R: not reported
5N/A: not applicable
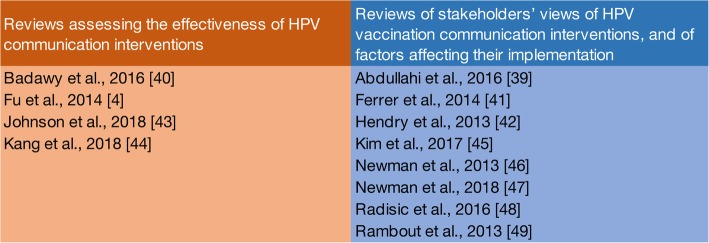
Focus of the included reviews
In relation to our overview objectives, we found that the available evidence from reviews on communication with stakeholders around HPV vaccination for adolescents could be organized into two groups, as shown in Fig. 2.
Fig. 2.
Overview of categorization of reviews
The first group assesses the effectiveness of HPV vaccination communication interventions or strategies and includes four reviews [4, 40, 43, 44]. The second group assesses factors associated with vaccination uptake as part of stakeholders’ views of HPV vaccination communication interventions or strategies and factors affecting their implementation. It includes eight reviews [39, 41, 42, 45–49].
For the following categories defined in the protocol, we found no reviews that met our eligibility criteria:
HPV vaccination communication issues or problems identified by any of the stakeholders, such as people’s information needs and how they would like to receive that information (rather than stakeholders’ views of vaccination communication interventions)
The cost or cost-effectiveness of HPV vaccination communication interventions or strategies
The concepts assessed by the included reviews were often poorly defined, not defined at all or differed across reviews. For example, one review [48] conceptualized vaccination acceptability as “holding a positive intention or willingness towards vaccinating sons in the future (vaccine intention), or by having consented to their sons being vaccinated in the past (vaccine initiation).” Another review [43] defined acceptability as “Perception among implementation stakeholders that a given treatment, service, practice, or innovation is agreeable, palatable, or satisfactory.” Differences such as these made assessing the focus of each review more challenging.
Reviews of the effectiveness of HPV vaccination communication interventions or strategies
Four reviews [4, 40, 43, 44] assessed the effectiveness of communication strategies by assessing their impact on vaccination acceptability, intention, or uptake. Their aims are described in Table 3. One review had a broader focus than HPV vaccination communication and included only a single study addressing HPV vaccination [40].
Table 3.
Aims of the reviews of the effectiveness of HPV vaccination communication interventions or strategies
| Review | Stated aims of the reviews |
|---|---|
| Badawy et al., 2016 [40] | Evaluate the efficacy of text messaging and mobile phone app interventions to improve adherence to preventive behavior, describe intervention approaches |
| Fu et al., 2014 [4] | Focus on educational interventions designed to increase HPV vaccine acceptance |
| Johnson et al., 2018 [43] | Uncover breadth and diversity of implementation strategies used to improve the uptake and sustainability of cervical cancer prevention programs |
| Kang et al., 2018 [44] | Evaluate the impact of interventions implemented after the first dose of HPV vaccination on the rate of HPV vaccine completion |
The communication interventions identified in these reviews were nearly all interventions to inform or educate [50], including written information fact sheets, house-to-house education, and radio [4, 43] (see Table 4). Other communication interventions intended to inform or educate, and remind or recall and included reminder messages and education as well as DVD-based instructions with telephone reminders. Table 4 shows the outcomes assessed by these reviews. Findings regarding the effectiveness of the communication interventions are not discussed in this overview.
Table 4.
Outcomes assessed by reviews on the effectiveness of HPV vaccination communication interventions
| Reviews | Outcomes assessed | Communication intervention purpose1 | Details of intervention |
|---|---|---|---|
| [4] | Vaccine acceptability, uptake | Inform or educate | Written information fact sheets from 1 to 2 pages in length |
| [4] | Not fact sheet based | ||
| [4] | 1-h slide presentation | ||
| [4] | Videos ranging in length from 3 to 10 min | ||
| [4] | Hour-long, live presentations delivered at school | ||
| [4] | An online fact sheet with a question-and-answer section and a self-quiz | ||
| [4] | Spanish-language radio advertisement (referred to as radionovela in the study) | ||
| [43] | Community outreach with lectures, pamphlets, posters, radio messages, and dramas | ||
| [43] | Vaccine uptake | House-to-house education given on a one-on-one basis by community health workers | |
| [43] | Staff training in program policy, sensitize school leadership, community outreach | ||
| [43] | Vaccine acceptability | Educational session to inform adults and adolescents | |
| [44] | Completion rate | Inform or educate and remind or recall | Reminder messages and education |
| [44] | Reminder letters vs. standard care | ||
| [44] | DVD-based instruction with telephone reminder vs. standard care | ||
| [40] | Text messages |
1Categories based on the “Communicate to Vaccinate” taxonomy of communication interventions for childhood vaccination [50]
Reviews of factors associated with HPV vaccination uptake
Eight reviews assessed factors associated with or influencing HPV vaccination uptake [39, 41, 42, 45–49] but did not look at the effectiveness of interventions to improve vaccination uptake. Seven of these reviews found only or mostly quantitative studies or surveys [39, 42, 45–49] while one review only searched for qualitative studies [41]. Some of the factors identified, such as knowledge and awareness, may be categorized as both barriers and facilitators in reviews, which is why we have decided to use the term “factor” to describe these.
Seven reviews in this group identified studies assessing factors thought to affect vaccination uptake and the association between these factors and uptake of the vaccine [41, 42, 45–49]. One review only identified studies that measured knowledge, attitudes, and practices and did not assess directly the association between these factors and reported uptake of the vaccine [39]. Rather, they hypothesized that these factors would impact on uptake.
The stated aims of the reviews are shown in Table 5. We have divided these reviews into two groups: the first group includes those looking at attitudes, views and preferences, and acceptability with regard to HPV vaccination (n = 4) [39, 42, 46, 48]. The second group includes those reviews focused on factors affecting vaccination uptake (n = 4) [41, 45, 47, 49].
Table 5.
Aims of the reviews looking at factors associated with vaccination uptake
| Systematic reviews looking at attitudes, views and preferences and acceptability with regard to HPV vaccination | Stated aim |
| Abdullahi et al., 2016 [39] | Knowledge, attitudes, and practices among stakeholders |
| Hendry et al., 2013 [42] | Information needs, views, and preferences |
| Newman et al., 2013 [46] | Acceptability and factors correlated with acceptability |
| Radisic et al., 2016 [48] | Factors associated with acceptability in parents of adolescent boys |
| Systematic reviews focusing on factors affecting vaccination uptake | Stated aim |
| Ferrer et al., 2014 [41] | Facilitators and barriers to decision-making by key stakeholders |
| Kim et al., 2017 [45] | Awareness, intention, and uptake among immigrant parents |
| Newman et al., 2018 [47] | Parents’ uptake, examine factors correlated with parents’ uptake, possible moderating influences of sex of child and parent on uptake |
| Rambout et al., 2013 [49] | Barriers and facilitators to vaccination |
In the first group of reviews, two aimed to explore the attitudes, views, or preferences of stakeholders towards HPV vaccination and included mainly survey studies [39, 42]. One of these reviews looked at knowledge, attitudes, and practices among stakeholders [39], while a second review looked at stakeholders’ information needs, views, and preferences [42]. Two more reviews assessed the acceptability of HPV vaccination [46, 48]. One review looked at acceptability in parents of adolescent boys [48] and included mostly survey studies. A second review explored HPV vaccine acceptability, and factors linked to this, among men and included mostly cross-sectional, quantitative studies [46].
The four reviews in the second group looked at factors affecting HPV vaccination uptake [41, 45, 47, 49]. Two of the reviews [45, 49] considered uptake as well as intention to vaccinate and included mostly survey and other cross-sectional studies. One review [41] included only qualitative studies of vaccination decision-making (which we viewed as related to intention to vaccinate), with the aim of providing an understanding of the factors affecting vaccination uptake. The last review [47] included only quantitative studies and found mostly studies using cross-sectional designs. It looked at factors associated with parents’ uptake of HPV vaccines for their children.
Table 6 provides a summary of the range of factors assessed in reviews of stakeholders’ views of HPV vaccination communication interventions and of the factors affecting the implementation of these interventions. The most commonly assessed factors were HPV education, health care provider influence, and the perceived benefits of HPV vaccination.
Table 6.
Summary of the range of factors assessed in reviews of stakeholders’ views of HPV vaccination communication interventions and of factors affecting the implementation of these interventions
| Overview authors’ groupings of factors | Factors as specified in reviews1 | Outcomes used in quantitative studies to measure factors affecting stakeholders’ views and the implementation of HPV vaccination communication2 | Reviews | Number of reviews in this grouping |
|---|---|---|---|---|
| HPV education | Knowledge [39, 48], information needs [42], HPV awareness [46], parents’ HPV-related knowledge and awareness—HPV vaccine knowledge and awareness [47], cervical cancer / HPV knowledge [47] | Level of knowledge [39, 42], acceptability [46, 48], uptake [47] | [39, 42, 46–48] | 5 |
| Health care provider influence | Physician recommendation [42], provider’s influence [45], health care provider recommendation [49] | Positive/negative [49], acceptability [42, 46], intention, uptake [45, 47] | [42, 45–47, 49] | 5 |
| Perceived benefits of HPV vaccination | Perceived HPV vaccine benefits [46–49] | Attitudes, acceptance [46, 48], intention or uptake [49], uptake [47] | [46–49] | 4 |
| Attitudes and beliefs | Parents’ vaccine attitudes—HPV vaccine safety concerns [47], fear of side effects/safety [48] | Acceptability [48], uptake [47] | [47–49] | 3 |
| Anticipatory regret [46, 47] | Attitudes, uptake [46, 47] | [46, 47] | 2 | |
| Feeling that the vaccine was not needed for various reasons [49] | Positive/negative [49] | [49] | 1 | |
| Perceived HPV vaccine effectiveness [46] | Attitudes [46] | [46] | 1 | |
| Fear of needles [46] | Attitudes [46] | [46] | 1 | |
| Belief in vaccines in general | Uptake [47] | [47] | 1 | |
| Structural barriers | Vaccine cost [45–47, 49] | Acceptability [46], intention or uptake [49], uptake [45, 47, 49] | [45–47, 49] | 4 |
| Perceived HPV severity [46] | Acceptability [46] | [46] | 1 | |
| Logistical barriers [46] | Acceptability [46] | [46] | 1 | |
| Need for multiple shots/doses [46] | Acceptability [46] | [46] | 1 | |
| Acceptability | Acceptability [42, 46] | Level of acceptability [42, 46] | [42, 46] | 2 |
| Parent’s vaccine beliefs, attitudes and intentions—intention to vaccinate child for HPV [47] | Uptake [47] | [47] | 1 | |
| Sexual risk behavior | Number of lifetime sexual partners [46] | Acceptability [46] | [46] | 1 |
| Having a current sex partner [46] | Acceptability [46] | [46] | 1 | |
| History of STI [46] | Acceptability [46] | [46] | 1 | |
| Not being sexually active [49] | Positive/negative [49] | [49] | 1 | |
| Other risk behaviors | Smoking cigarettes [46] | Acceptability [46] | [46] | 1 |
| Non-receipt of hepatitis B vaccine [46] | Acceptability [46] | [46] | 1 | |
| Socio-demographic factors | Effects of neighborhoods [45] | Uptake [45] | [45] | 1 |
| Acculturation (e.g., language use, origin of birth) [45] | HPV vaccination [45] | [45] | 1 | |
| Being employed [46] | Acceptability [46] | [46] | 1 | |
| Educational level [46] | Acceptability [46] | [46] | 1 | |
| Non-white (vs white) ethnicity [46] | Acceptability [46] | [46] | 1 | |
| HPV vaccine endorsements | Endorsement from a governmental source [41] | N/A [41] | [41] | 1 |
| Partner thinks one should get the vaccine [46] | Acceptability [46] | [46] | 1 | |
| Other | Cultural sexual health values (such as social norms regarding adolescent sexuality and stigma related to sexually transmitted diseases) [45] | N/A [45] | [45] | 1 |
| Immigration laws [45] | N/A [45] | [45] | 1 | |
| Mother as HPV vaccine decision-maker (vs both parents) [47] | Uptake [47] | [47] | 1 | |
| Social norms [49] | Intention or uptake [49] | [49] | 1 |
1Not all reviews in each group assessed all factors
2Not all reviews in each group assessed all outcomes
Additional file 8 shows the aims of the included reviews, in relation to our overview objectives, and the results as expressed by the review authors. We do not discuss the review results as this falls outside of the scope of this overview.
Applicability of the evidence
Our assessments of the applicability of the evidence in the reviews to LMICs shows that this differs among the included reviews (see Table 7). With two exceptions [39, 43], the reviews included few studies from LMICs. For many reviews, we believe there are likely to be important differences in on-the-ground realities and constraints in LMICs that might alter the feasibility and acceptability of the intervention or raise questions about the applicability of the review findings. For many reviews, we also assessed there to be important differences in health system arrangements that may mean an intervention would not work in the same way in LMICs or review findings may not be applicable to LMICs. The reasoning behind these assessments can be found in Additional file 9.
Table 7.
Applicability of the evidence to LMICs
| Review | Were some or all of the studies included in the systematic review conducted in LMICs or were the findings in the review consistent across settings or time periods and therefore suggest wide applicability? [Proportion of studies conducted in LMICs] | Are there important differences in on-the-ground realities and constraints in LMICs that might substantially alter the feasibility and acceptability of the intervention (where applicable) or raise questions about the applicability of the review findings? | Are there important differences in health system arrangements that may mean an intervention could not work in the same way in LMICs or review findings may not be applicable to LMICs? |
|---|---|---|---|
| Abdullahi et al., 2016 [39] | Yes [18/18] | Likely no | Largely not applicable |
| Badawy et al., 2017 [40] | No1 | Likely yes | Yes |
| Ferrer et al., 2014 [41]2 | No | Likely yes | Likely yes |
| Fu et al., 2014 [4]2 | Yes [2/33] | Likely yes | Likely yes |
| Hendry et al., 2013 [42] | Yes [11/72] | Likely no | Likely no |
| Johnson et al., 2018 [43] | Yes [53/53] | Likely no | Likely no2 |
| Kang et al., 2018 [44] | No | Likely yes | Likely yes |
| Kim et al., 2017 [45] | No | Likely no | Likely no |
| Newman et al., 2013 [46] | Yes [2/29] | Likely yes | Likely yes |
| Newman et al., 2018 [47] | Yes [6/79] | Likely no | Likely no |
| Radisic et al., 2017 [48] | No | Yes | Likely yes |
| Rambout et al., 2014 [49]3 | No | Likely yes | Likely yes |
1The review includes one study from a LMIC; however, this study does not focus on HPV
2Difficult to assess due to inadequate reporting of the results
3Did not intend to include studies from LMICs
Methodological limitations of included reviews
All of the 12 included reviews had minor methodological limitations. We assessed 11 reviews to have used only a partially comprehensive literature search strategy. Ten reviews did not contain an explicit statement that the review methods were established prior to the conduct of the review. Ten reviews also did not provide a list of excluded studies or justify their exclusions. Nine of the included reviews did not report on the sources of funding for their included studies. Seven reviews did not perform data extraction in duplicate and five reviews failed to adequately describe or perform study selection in duplicate.
Table 1 summarizes the AMSTAR 2 assessments of the reviews excluded for having major methodological limitations or a large number of minor methodological limitations. Table 8 provides these assessments for the included reviews. Additional file 10 provides the full AMSTAR 2 assessments.
Table 8.
Table of methodological limitations of included reviews
| Review | Number of methodological limitations (criterion numbers1) |
|---|---|
| Abdullahi et al., 2016 [39] | Four minor limitations (3, 4, 10, 14) |
| Badawy et al., 2017 [40]2 | One major limitation (9). Six minor limitations (4, 7, 10, 11, 12, 14) |
| Ferrer et al., 2014 [41] | Seven minor limitations (2, 4, 6, 7, 10, 12, 14) |
| Fu et al., 2014 [4] | Five minor limitations (2, 3, 4, 7, 10) |
| Hendry et al., 2013 [42] | Seven minor limitations (2, 3, 4, 6, 7, 12, 13) |
| Johnson et al., 2018 [43] | Eight minor limitations (2, 3, 4, 6, 7, 9, 10, 14) |
| Kang et al., 2018 [44] | Seven minor limitations (2, 3, 4, 5, 6, 7, 10) |
| Kim et al., 2017 [45] | Eight minor limitations (2, 4, 5, 6, 7, 10, 13, 14) |
| Newman et al., 2013 [46] | Eight minor limitations (2, 3, 4, 5, 6, 7, 10, 15) |
| Newman et al., 2018 [47] | Four minor limitations (2, 3, 4, 7) |
| Radisic et al., 2017 [48] | Six minor limitations (2, 4, 5, 6, 7, 10) |
| Rambout et al., 2014 [49] | Five minor limitations (2, 4, 5, 7, 14) |
1As numbered in Additional file 4 which lists the criteria for assessing the reliability of reviews, adapted from AMSTAR 2
2This review did not include assessments of the methodological limitations of each included study and therefore could be viewed as having a major limitation, according to our assessment tool. However, the overall results from the assessments were reported and the review was therefore included in our overview on this basis
Discussion
Summary of main results
This scoping overview aimed to provide a broad overview of the evidence available on communication with stakeholders around HPV vaccination for adolescents, with a specific focus on LMICs. We included 12 reviews in the overview after excluding 27 eligible reviews because of important methodological limitations. Of these 12 reviews, four reviews [4, 40, 43, 44] assessed the effectiveness of communication strategies by assessing their impact on vaccination acceptability, intention, or uptake. The interventions or strategies described intended to either inform or educate (including videos, live presentations, and fact sheets [4, 43, 44]) or to remind or recall (including text messages, letters, and telephone reminders [40, 44]) regarding HPV vaccination. Eight reviews reported on factors associated with vaccination uptake and which may affect the implementation of communication interventions. The most commonly assessed factors were HPV education, health care provider influence, and the perceived benefits of vaccination. A plain language summary of these results is available in Additional file 11.
We experienced challenges in categorizing the reviews included in this overview because some reviews had more than one aim. In addition, some of the concepts used across reviews, such as attitudes towards HPV vaccination, were defined in different ways in these reviews. Future reviews might benefit from the development of a shared terminology and consistent definitions that can be applied across reviews.
Overall completeness and applicability of evidence
In this scoping overview, we did not find any reviews addressing communication issues or communication problems related to HPV vaccination. Nor did we find any reviews on the cost or cost-effectiveness of HPV vaccination communication interventions or strategies.
Most of the included reviews found few studies from LMICs. Our assessment of the evidence that was identified in the reviews was that its applicability to LMICs differed (Table 7). However, we acknowledge that these assessments are subjective judgments and we recognize that others may reach different conclusions regarding the degree of differences in on-the-ground realities and health systems between high-income countries and LMICs in relation to the reviews assessed. The reasoning behind the assessments in Table 7 can be found in Additional file 9. Overall, the low numbers of studies from LMICs included in the reviews highlight an evidence gap in relation to primary studies of communication around HPV vaccination for adolescents.
Potential biases in the scoping overview process
We conducted a search using the most comprehensive and up-to-date global database of systematic reviews [51] that is, in turn, based on searches of a very large number of other health study databases. However, we may have missed reviews that described their focus using terms other than those included in our search strategy. In addition, we did not hand search the references of the included reviews, identify eligible gray literature, or ask experts in the field for eligible reviews. These limitations mean that we may not have identified all existing eligible reviews.
Although the overview only included reviews written in English, Norwegian, Swedish, or Danish, only one review was excluded at the full-text stage for being published in another language (Portuguese).
One of the included reviews only included one study regarding HPV vaccination. Although this is a deviation from our protocol, we decided to include this review as the included study contributed to the overview aim. However, this could be a potential source of bias as other similar reviews could have been excluded by our inclusion criteria.
Strengths of the overview include the exclusion of reviews with important methodological limitations that may have misleading results and verification by a second overview author of both the data extraction and the adapted AMSTAR 2 assessments.
Agreements and disagreements with other studies or reviews
We did not find any other systematic scoping overviews or other overview of reviews with which we could compare our results.
Conclusions
Twelve reviews were included in this overview: four reviews assessed their effectiveness while eight reviews assessed factors associated with HPV vaccination uptake. Out of the 12 included reviews, nine reviews searched for studies from LMICs. However, most of these found only a small number of studies from these countries. The small number of studies from LMICs is of concern as these countries face the largest burden of disease related to HPV. We excluded a number of existing reviews because of important methodological limitations. This highlights the need for future reviews to use appropriate methods and to adhere to reporting standards such as PRISMA [38].
Our findings suggest that there may still be important knowledge gaps, for example, in relation to educational interventions to increase HPV acceptance and studies of HPV vaccination for males. Further primary research in these areas may be needed. We also identified gaps in relation to reviews of issues or problems identified by any of the stakeholders and regarding the cost or cost-effectiveness of HPV vaccination communication interventions or strategies. New reviews in these areas may be helpful. These reviews may indicate areas in which further primary studies are needed on HPV vaccination communication in LMICs.
Additional files
PRISMA-ScR Checklist. (PDF 82 kb)
Full search strategy. (PDF 13 kb)
List of excluded reviews assessed in full-text with reasons for exclusion. (PDF 47 kb)
Criteria for assessing the reliability of included reviews. (PDF 66 kb)
Data extraction sheet. (XLSX 54 kb)
List of reviews excluded where no full-text was available. (PDF 23 kb)
Table of funding and conflicts of interest as reported in the reviews. (PDF 38 kb)
Summary of the results of each review, in relation to the scoping overview objectives. (PDF 59 kb)
Applicability of the evidence to LMICs, with explanations of assessments. (PDF 56 kb)
Individual AMSTAR 2 assessments. (PDF 770 kb)
Plain language summary of the overview. (PDF 37 kb)
Acknowledgements
We thank the Epistemonikos Foundation for assistance with searches and use of the Collaboratron screening tool; Dr. Marit Johansen, Norwegian Institute of Public Health, for assistance with the search strategy; Dr. Unni Gopinathan, Institute of Health and Society, Faculty of Medicine, University of Oslo, for orchestrating the collaboration among the overview authors in its early stages; and the participants attending a meeting on communication in the context of HPV vaccination in Pretoria, South Africa, on 22 February 2018 who provided feedback on preliminary findings.
Abbreviations
- AMSTAR 2
A MeaSurement Tool to Assess systematic Reviews 2
- EPOC
Cochrane Effective Practice and Organisation of Care Group
- HIC
High-income country
- HPV
Human papillomavirus
- LMICs
Low- and middle-income countries
- N/A
Not applicable
- N/R
Not reported
- NIPH
Norwegian Institute of Public Health
- PRISMA
Preferred Reporting Items for Systematic reviews and Meta-Analyses
- RCT
Randomized controlled study
- WHO
World Health Organization
Authors’ contributions
SL developed the initial idea for the overview. SL, HSF, and AO wrote the protocol for the review and AF and CL commented on this. HSF and AO wrote the search strategy with assistance (see the “Acknowledgements” section). HSF, AO, and SL ran the literature search and independently carried out the abstract review. HSF and AO screened the full texts and SL came in as a third reviewer when necessary. SL developed the data extraction form. HSF performed most of the data extraction and methodological assessments with contributions from AO. AO and SL verified the data extraction and methodological assessments. HSF wrote the first draft of the manuscript. All overview authors contributed to the writing of the manuscript and have read and approved the manuscript. This overview will be a part of the project thesis and degree Candidatus medicinae of HSF at the University of Oslo, Oslo, Norway.
Funding
This systematic overview of reviews received funding from the Norwegian Institute of Public Health (NIPH). A meeting on communication in the context of HPV vaccination held in Pretoria, South Africa, on 22 February 2018 was funded by the Norwegian Agency for Development Cooperation (Norad). The attendees at this meeting provided feedback on the preliminary findings of the overview. This work was also in part financed by the i4C project funded by the Research Council of Norway (project number 234608). SL receives additional funding from the South African Medical Research Council.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its additional files.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bruni L, Barrionuevo-Rosas L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. Human papillomavirus and related diseases in the world. Summary Report. 2017.
- 2.HPV vaccine communication . Special considerations for a unique vaccine: 2016 update. Geneva: World Health Organization; 2017. [Google Scholar]
- 3.Lee LA, Franzel L, Atwell J, Datta SD, Friberg IK, Goldie SJ, Reef SE, Schwalbe N, Simons E, Strebel PM, Sweet S, Suraratdecha C, Tam Y, Vynnycky E, Walker N, Walker DG, Hansen PM. The estimated mortality impact of vaccinations forecast to be administered during 2011–2020 in 73 countries supported by the GAVI Alliance. Vaccine. 2013;31:B61–B72. doi: 10.1016/j.vaccine.2012.11.035. [DOI] [PubMed] [Google Scholar]
- 4.Fu LY, Bonhomme LA, Cooper SC, Joseph JG, Zimet GD. Educational interventions to increase HPV vaccination acceptance: a systematic review. Vaccine. 2014;32(17):1901–1920. doi: 10.1016/j.vaccine.2014.01.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fantom N, Serajuddin U. The World Bank’s classification of countries by Income: Data Group, Development Economics, World Bank Group; 2016.
- 6.Tricco AC, Lillie E, Zarin W, et al. Prisma extension for scoping reviews (prisma-scr): Checklist and explanation. Ann Intern Med. 2018. [DOI] [PubMed]
- 7.Tricco AC, Lillie E, Zarin W, O’Brien K, Colquhoun H, Kastner M, Levac D, Ng C, Sharpe JP, Wilson K, Kenny M, Warren R, Wilson C, Stelfox HT, Straus SE. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16(1):15. doi: 10.1186/s12874-016-0116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 9.Allen JD, Coronado GD, Williams RS, Glenn B, Escoffery C, Fernandez M, Tuff RA, Wilson KM, Mullen PD. A systematic review of measures used in studies of human papillomavirus (HPV) vaccine acceptability. Vaccine. 2010;28(24):4027–4037. doi: 10.1016/j.vaccine.2010.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med. 2007;45(2-3):107–114. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 11.Catalan-Matamoros D, Peñafiel-Saiz C. The use of traditional media for public communication about medicines: a systematic review of characteristics and outcomes. Health communication. 2017:1–9. [DOI] [PubMed]
- 12.Chan ZC, Chan TS, Ng KK, Wong ML. A systematic review of literature about women’s knowledge and attitudes toward human papillomavirus ( HPV) vaccination. Public Health Nurs. 2012;29(6):481–489. doi: 10.1111/j.1525-1446.2012.01022.x. [DOI] [PubMed] [Google Scholar]
- 13.Crocker-Buque T, Edelstein M, Mounier-Jack S. Interventions to reduce inequalities in vaccine uptake in children and adolescents aged <19 years: a systematic review. J Epidemiol Community Health. 2017;71(1):87–97. doi: 10.1136/jech-2016-207572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cunningham MS, Davison C, Aronson KJ. HPV vaccine acceptability in Africa: a systematic review. Prev Med. 2014;69C (Cunningham M.S.; Davison C.; Aronson K.J., aronson@queensu.ca). Kingston: Department of Public Health Sciences, Queen’s University. p. 274–9. [DOI] [PubMed]
- 15.Das JK, Salam RA, Arshad A, Lassi ZS, Bhutta ZA. Systematic review and meta-analysis of interventions to improve access and coverage of adolescent immunizations. J Adolesc Health. 2016;59(4S):S40–SS8. doi: 10.1016/j.jadohealth.2016.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Francis DB, Cates JR, Wagner KP, Zola T, Fitter JE, Coyne-Beasley T. Communication technologies to improve HPV vaccination initiation and completion: a systematic review. Patient Educ Couns. 2017;100(7):1280–1286. doi: 10.1016/j.pec.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 17.Galbraith KV, Lechuga J, Jenerette CM, Moore LTCAD, Palmer MH, Hamilton JB. Parental acceptance and uptake of the HPV vaccine among African-Americans and Latinos in the United States: a literature review. Soc Sci Med. 2016;159:116–126. doi: 10.1016/j.socscimed.2016.04.028. [DOI] [PubMed] [Google Scholar]
- 18.Gilkey MB, McRee AL. Provider communication about HPV vaccination: a systematic review. Hum Vaccin Immunother. 2016;12(6):1454–1468. doi: 10.1080/21645515.2015.1129090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168(1):76–82. doi: 10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hyde T, Dentz H, Wang S, Burchett H, Mounier-Jack S, Mantel C. The New Vaccine Introduction Impact Published Literature Working G. The impact of new vaccine introduction on immunization and health systems: a review of the published literature. Vaccine. 2012;30(45):6347–6358. doi: 10.1016/j.vaccine.2012.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kabakama S, Gallagher KE, Howard N, Mounier-Jack S, Burchett HE, Griffiths UK, Feletto M, LaMontagne DS, Watson-Jones D. Social mobilisation, consent and acceptability: a review of human papillomavirus vaccination procedures in low and middle-income countries. BMC Public Health. 2016;16(1):834. doi: 10.1186/s12889-016-3517-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karafillakis E, Larson HJ. consortium A. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine. 2017;35(37):4840–4850. doi: 10.1016/j.vaccine.2017.07.061. [DOI] [PubMed] [Google Scholar]
- 23.Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: a systematic review. Vaccine. 2012;30(24):3546–3556. doi: 10.1016/j.vaccine.2012.03.063. [DOI] [PubMed] [Google Scholar]
- 24.Loke AY, Kwan ML, Wong YT, Wong AKY. The uptake of human papillomavirus vaccination and its associated factors among adolescents: a systematic review. J Prim Care Community Health. 2017;2150131917742299. [DOI] [PMC free article] [PubMed]
- 25.Mishra A. Implementing HPV vaccines: public knowledge, attitudes, and the need for education. Int Q Community Health Educ. 2011;31(1):71–98. doi: 10.2190/IQ.31.1.f. [DOI] [PubMed] [Google Scholar]
- 26.Niccolai LM, Hansen CE. Practice- and community-based interventions to increase human papillomavirus vaccine coverage: A Systematic Review. JAMA Pediatr. 2015;169(7):686–692. doi: 10.1001/jamapediatrics.2015.0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paul P, Fabio A. Literature review of HPV vaccine delivery strategies: considerations for school- and non-school based immunization program. Vaccine. 2014;32(3):320–326. doi: 10.1016/j.vaccine.2013.11.070. [DOI] [PubMed] [Google Scholar]
- 28.Perlman S, Wamai RG, Bain PA, Welty T, Welty E, Ogembo JG. Knowledge and awareness of HPV vaccine and acceptability to vaccinate in sub-Saharan Africa: a systematic review. PLoS One. 2014;9(3):e90912. doi: 10.1371/journal.pone.0090912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosen BL, Shepard A, Kahn JA. US health care clinicians’ knowledge, attitudes, and practices regarding human papillomavirus vaccination: a qualitative systematic review. Acad Pediatr. 2018;18:53–65. doi: 10.1016/j.acap.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ryan C, Duvall KL, Weyant EC, Johnson KR, Wood D. Human papillomavirus vaccine uptake, knowledge, and acceptance for youth: a systematic review of Appalachia. J Community Health. 2018;43(3):616–624. doi: 10.1007/s10900-018-0500-6. [DOI] [PubMed] [Google Scholar]
- 31.Small SL, Sampselle CM, Martyn KK, Dempsey AF. Modifiable influences on female HPV vaccine uptake at the clinic encounter level: a literature review. J Am Assoc Nurse Pract. 2014;26(9):519–525. doi: 10.1002/2327-6924.12057. [DOI] [PubMed] [Google Scholar]
- 32.Smulian EA, Mitchell KR, Stokley S. Interventions to increase HPV vaccination coverage: a systematic review. Hum Vaccin Immunother. 2016;12(6):1566–1588. doi: 10.1080/21645515.2015.1125055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Walling EB, Benzoni N, Dornfeld J, Bhandari R, Sisk BA, Garbutt J, Colditz G. Interventions to improve HPV vaccine uptake: a systematic review. Pediatrics. 2016;138(1):1–11. doi: 10.1542/peds.2015-3863. [DOI] [PubMed] [Google Scholar]
- 34.Wigle J, Coast E, Watson-Jones D. Human papillomavirus (HPV) vaccine implementation in low and middle-income countries (LMICs): health system experiences and prospects. Vaccine. 2013;31(37):3811–3817. doi: 10.1016/j.vaccine.2013.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Young A. HPV vaccine acceptance among women in the Asian Pacific: a systematic review of the literature. Asian Pac J Cancer Prev. 2010;11(3):641–649. [PubMed] [Google Scholar]
- 36.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358. [DOI] [PMC free article] [PubMed]
- 37.Ciapponi A, Lewin S, Herrera CA, Opiyo N, Pantoja T, Paulsen E, Rada G, Wiysonge CS, Bastías G, Dudley L, Flottorp S, Gagnon M-P, Garcia Marti S, Glenton C, Okwundu CI, Peñaloza B, Suleman F, Oxman AD. Delivery arrangements for health systems in low-income countries: an overview of systematic reviews. Cochrane Database Syst Rev. 2017;9. [DOI] [PMC free article] [PubMed]
- 38.Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abdullahi LH, Kagina BM, Cassidy T, Adebayo EF, Wiysonge CS, Hussey GD. Knowledge, attitudes and practices on adolescent vaccination among adolescents, parents and teachers in Africa: A systematic review. Vaccine. 2016;34(34):3950–3960. doi: 10.1016/j.vaccine.2016.06.023. [DOI] [PubMed] [Google Scholar]
- 40.Badawy SM, Kuhns LM. Texting and mobile phone app interventions for improving adherence to preventive behavior in adolescents: a systematic review. JMIR MHealth UHealth. 2017;5(4):e50. doi: 10.2196/mhealth.6837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferrer HB, Trotter C, Hickman M, Audrey S. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health. 2014;14:700. doi: 10.1186/1471-2458-14-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hendry M, Lewis R, Clements A, Damery S, Wilkinson C. “HPV? Never heard of it!”: a systematic review of girls’ and parents’ information needs, views and preferences about human papillomavirus vaccination. Vaccine. 2013;31(45):5152–5167. doi: 10.1016/j.vaccine.2013.08.091. [DOI] [PubMed] [Google Scholar]
- 43.Johnson LG, Armstrong A, Joyce CM, Teitelman AM, Buttenheim AM. Implementation strategies to improve cervical cancer prevention in sub-Saharan Africa: a systematic review. Implement Sci. 2018;13(1):28. doi: 10.1186/s13012-018-0718-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kang HS, De Gagne JC, Son YD, Chae S-M. Completeness of human papilloma virus vaccination: a systematic review. J Pediatr Nurs. 2018;39:7–14. doi: 10.1016/j.pedn.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 45.Kim K, LeClaire AR. A systematic review of factors influencing human papillomavirus vaccination among immigrant parents in the United States. Health Care Women Int. 2017:0. [DOI] [PubMed]
- 46.Newman PA, Logie CH, Doukas N, Asakura K. HPV vaccine acceptability among men: a systematic review and meta-analysis. Sex Transm Infect. 2013;89(7):568–574. doi: 10.1136/sextrans-2012-050980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Newman PA, Logie CH, Lacombe-Duncan A, Baiden P, Tepjan S, Rubincam C, Doukas N, Asey F. Parents’ uptake of human papillomavirus vaccines for their children: a systematic review and meta-analysis of observational studies. BMJ Open. 2018;8(4):e019206. doi: 10.1136/bmjopen-2017-019206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Radisic G, Chapman J, Flight I, Wilson C. Factors associated with parents’ attitudes to the HPV vaccination of their adolescent sons : A systematic review. Prev Med. 2017;95:26–37. doi: 10.1016/j.ypmed.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 49.Rambout L, Tashkandi M, Hopkins L, Tricco AC. Self-reported barriers and facilitators to preventive human papillomavirus vaccination among adolescent girls and young women: a systematic review. Prev Med. 2014;58(1):22–32. doi: 10.1016/j.ypmed.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 50.Kaufman J, Ames H, Bosch-Capblanch X, Cartier Y, Cliff J, Glenton C, Lewin S, Muloliwa AM, Oku A, Oyo-Ita A, Rada G, Hill S. The comprehensive ‘Communicate to Vaccinate’ taxonomy of communication interventions for childhood vaccination in routine and campaign contexts. BMC Public Health. 2017;17(1):423. doi: 10.1186/s12889-017-4320-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rada G, Perez D, Capurro D. Epistemonikos: a free, relational, collaborative, multilingual database of health evidence. Stud Health Technol Inform. 2013;192:486–490. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA-ScR Checklist. (PDF 82 kb)
Full search strategy. (PDF 13 kb)
List of excluded reviews assessed in full-text with reasons for exclusion. (PDF 47 kb)
Criteria for assessing the reliability of included reviews. (PDF 66 kb)
Data extraction sheet. (XLSX 54 kb)
List of reviews excluded where no full-text was available. (PDF 23 kb)
Table of funding and conflicts of interest as reported in the reviews. (PDF 38 kb)
Summary of the results of each review, in relation to the scoping overview objectives. (PDF 59 kb)
Applicability of the evidence to LMICs, with explanations of assessments. (PDF 56 kb)
Individual AMSTAR 2 assessments. (PDF 770 kb)
Plain language summary of the overview. (PDF 37 kb)
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its additional files.