Abstract
Background
Men who have sex with men (MSM) in Brazil are deferred from donation for 1-year since last sexual contact. Legal proceedings in front of the Brazilian Supreme Court could compel blood collection agencies to discontinue use of sexual orientation questions.
Methods
Data from male participants in a completed HIV risk factor case-control study were used to evaluate whether it is possible to differentiate donors at lower and higher risk for HIV using two analytical approaches latent class and random forest analyses.
Results
Male blood donors were divided into three distinct risk profile classes: Class-1 with donors who are heterosexual (96.4%), HIV− (88.7%), have a main partner (99.4%), and practice unprotected sex (77.8%). Class-2 with donors who are MSM/bisexuals’ donors (100.0%), HIV+ (97.4%), and were not aware of their sexual partners’ HIV status (80.3%). Class-3 with donors who were heterosexual (84.1%), practicing unprotected vaginal/anal heterosexual sex (66.8% vs 40.9%), and were both HIV+ and HIV− (49.5% vs. 50.5%). We also found that asking donors about their partner(s) HIV serostatus could replace asking about donor’s sexual orientation and types of partners with relatively minor shifts in sensitivity (0.76 vs. 0.58), specificity (0.89 vs. 0.94) and positive predictive value (PPV) (0.85 vs. 0.88).
Conclusion
Sexual orientation questions on the donor questionnaire could be replaced without great loss in the sensitivity, specificity and PPV. Social and sexual behaviors of donors and their partners are proxies for HIV risk and can help to develop modified questions that will need controlled trials to be validated.
Keywords: Blood donor screening, HIV, Men having sex with men, Social and behavioral factors
INTRODUCTION
Regulations governing blood donation and transfusion in Brazil are very similar to those in the US and Europe, and internationally accepted procedures and guidelines are used as reference in the development of Brazilian rules and practice guidelines. However, the risk of HIV transmission by blood transfusion persists in Brazil and remains higher than in the US and most European countries (1)
As in Australia, Canada, USA, and several European countries, The Brazilian Ministry of Health changed the regulation for permanent deferral from donation for men who have sex with men (MSM) to be a 1-year deferral since last sexual contact (2, 3). In the UK, MSM donation deferral is now three months after the last sexual contact. Countervailing to the easing of policies, Spain is considering changing their MSM non-deferral policy to a temporary deferral based on individual risk assessments due to the potential risk. In Brazil, there are proceedings in front of the Supreme Court at this time that would compel all blood collectors in the country to change some predonation interview criteria, including not allowing blood centers to ask donors whether their sexual partners are the same or opposite sex, or inquiring about other aspects of the donor’s sexual partners. There are no available data to understand what possible alternative questions would be appropriate to reduce the risk of donation by persons with high risk for infection.
HIV/AIDS is a global epidemic that is dynamic and changing, so the risk is not evenly distributed, varying by risk profile (4, 5). While the routes of HIV infection acquisition are known, the contextual factors such as how and where persons meet their sexual partners, sexual attitudes and the impact of the numbers and different type of partners are less well known. Several studies of risk factors for HIV infection conducted in the Brazilian population report sexual transmission as the main cause of cases of HIV/AIDS, with most cases attributed to unprotected sex between MSM. However, there are also other routes of acquisition observed in Brazil, including intravenous drug use and unprotected heterosexual sex (6). Risk factor studies in blood donors have shown that MSM remains the strongest determinant of HIV status among HIV positive blood donors (1, 6–9).
We analyzed data from a HIV behavioral risk factor case-control study from the Retrovirus Epidemiology Donor Study – II (REDS-II) to assess whether it is possible to identify high-risk behaviors among HIV positive donors and their partners and to assess alternative questions that could predict if a blood donor is at risk of being HIV positive, regardless of sexual orientation. Our study sought to assess whether surrogate risk behavior questions can predict if a blood donor is likely to be HIV-positive or negative. Additionally, the social and sexual behavior of blood donors and their partners were also evaluated to better understand risk behaviors for HIV infection.
MATERIALS AND METHODS
Study Description and Sites
The REDS-II HIV case-control study was conducted from April 2009 to March 2011 in four large Brazilian blood centers - Fundação Pró-Sangue in São Paulo, Fundação Hemominas in Belo Horizonte, Fundação Hemorio in Rio de Janeiro and Fundação Hemope in Recife. More details about the original study design and methods for participant selection, testing and interview procedures can be found in previously published manuscripts (6–8). Together, there are nearly 600,000 blood donations given to these four blood centers per year, or 15% of all blood donations in Brazil. These four Brazilian hemocenters have a wide geographic distribution, are diverse in the socioeconomic characteristics of the donor base, and are located in regions with high rates of HIV. In 2016, 44% of the new HIV infections of the country occurred in these regions (10).In this analysis we focused on the risk behavior questionnaire responses for males because of: (1) Differences in behavior between males and females observed in previous analyses; (2) The fact that the majority of blood donors are male at these blood centers sites; (3) The focus of the donor eligibility debate in Brazil is on male donors.
Analysis Overview
A cross-sectional Latent Class Analysis (LCA) was used to identify patterns of behavior based on the participants’ as well as their sexual partners’ characteristics. LCA was performed to identify latent population subgroups defined by distinct behavior patterns on multiple risk factors. In this analysis, LCA provides a multidimensional description of how risk factors may work together to increase or decrease the likelihood of acquiring HIV, using methods similar to those reported in other LCA analyses (11). Random forest classifiers are an intuitive and interpretable method for data classification (12). The generated algorithm enables the estimation of each variable’s contribution to classification performance by permutation. The random forest analysis was used to define which questions could better predict if a blood donor has higher or lower risk of being HIV-positive.
HIV Case-Control Study
Questionnaire and Measures
In the original case-control study, the risk behavior questionnaire was implemented using an audio computer assisted structured interview (ACASI) conducted in a private setting. ACASI was chosen to maximize reporting of potentially stigmatizing behaviors (13). In the LCA and decision tree analyses, we included sexual orientation based on the behavior reported during the past 12 months. Donors were defined as heterosexual if the participant did not report any same sex partner, MSM/bisexual if the participant reported to have had at least one same sex partner, or if the donor self-declared MSM or bisexual. Number of sexual partners in the past 12 months were grouped as 0–1, 2–5 or ≥6. For the analysis, responses of ‘don’t know’ and item response refusals were considered as missing. Participant demographics included age in years, education, and marital status. Variables that identified the blood center (Fundação Pró-Sangue, Hemominas, Hemorio and Hemope) and the HIV status of the blood donors were included. HIV-positive blood donors were tested by two EIA and confirmed by Western blot and the HIV-negative blood donors were negative for all the screening serologic markers for infectious diseases applied by the blood centers, including HCV, HBV, HTLV-1/2, syphilis, and T. cruzi.
Sexual Matrix
The characteristics of the sexual partners were assessed as binary (yes/no) responses for respondent’s self-report on up to five sexual partners in the year before donation. Questions captured age disparity in sexual partnerships of ≥10 years for ≥1 partners, type of partners (main partner, friend, acquaintance, one time, anonymous, sex worker), intravenous drug use (IVDU, if donor was an ever IVDU or had a partner who was an ever IVDU), MSM partner, and if the respondent knew the HIV status of his partners. We also evaluated the venues where each respondent met his partners. In addition, we asked about unprotected vaginal or anal intercourse. Response categories are NOT mutually exclusive, since any blood donor who had more than one partner may have had different sexual behaviors or partners with different characteristics.
Statistical Analysis
Latent Class Analysis
We tested models with 2 to 4 latent classes. The results are presented with the distribution of respondent and partner characteristics according to the classes obtained by the best-fit model. The analysis was performed using the poLCA package (14) of R software version 3.4.3, and a significance level of 5% was used.
Random Forest
In this analysis variable importance was calculated following the construction of a random forest with variables listed in Table 1. Additionally, random forests were generated by removing variables and accuracies, sensitivities, specificities, positive predictive values (PPV) were compared. Sub-setting of the HIV negative subjects was used to balance class size and avoid classification bias (15).
Table 1:
Descriptive analysis for the 838 male blood donors from four large Brazilian blood centers from 2009 to 2011.
| Characteristics | Valid n (n = 838) | Frequency n (%) |
|---|---|---|
| Donor’s Characteristics | ||
| Age (years) | 838 | 33.6 ± 9.9 |
| Educational level | 833 | |
| Illiterate / Inc. Elementary School/Adult Literacy | 86 (10.3) | |
| Complete Elementary/High/Technician School | 596 (71.5) | |
| Graduation/MD/PhD | 151 (18.1) | |
| Marital status | 838 | |
| Married / living with | 433 (51.7) | |
| Unmarried | 405 (48.3) | |
| Sexual History | 812 | |
| Heterosexual | 618 (76.1) | |
| MSM/Bisexual | 194 (23.9) | |
| Lifetime Number of partners | 838 | |
| 0 – 1 | 243 (29.0) | |
| 2 – 5 | 250 (29.8) | |
| ≥ 6 | 345 (41.2) | |
| Center ID | 838 | |
| Fundação Pró-Sangue – São Paulo | 242 (28.9) | |
| Hemominas – Minas Gerais | 159 (19.0) | |
| Hemope – Pernambuco | 175 (20.9) | |
| Hemorio – Rio de Janeiro | 262 (31.3) | |
| Characteristics of the last five partners* | ||
| Partner’s age | ||
| Age disparity of ≥10 years for one or more partners | 799 | 78 (9.8) |
| Type of partner | ||
| Main partner | 799 | 599 (75.0) |
| Friend partner | 799 | 133 (16.6) |
| Acquaintance partner | 799 | 132 (16.5) |
| One time partner | 799 | 102 (12.8) |
| Anonymous partner | 799 | 82 (10.3) |
| Sex worker partner | 799 | 15 (1.9) |
| Anonymous or sex worker partner | 799 | 93 (11.6) |
| Intravenous drug use (IVDU)† | ||
| IVDU or partner IVDU | 799 | 31 (3.9) |
| Partner’s MSM | ||
| Yes | 799 | 104 (13.0) |
| Partner’s HIV Status | ||
| Don’t know partner’s HIV status | 799 | 286 (35.8) |
| HIV positive partner | 799 | 32 (4.0) |
| Venue where met their partners | ||
| Bar or Carnival | 799 | 160 (20.0) |
| Street, park, library, public transportation | 799 | 144 (18.0) |
| Social/political parties in clubs or church | 799 | 239 (29.9) |
| Dating service (internet/newspaper ads) | 799 | 87 (10.9) |
| Some other way or work | 799 | 374 (46.8) |
| Unprotected sexual intercourse | ||
| Unprotected vaginal sex | 799 | 533 (66.7) |
| Unprotected heterosexual anal sex | 797 | 217 (27.2) |
Partner’s characteristics were based on the criteria of having at least one partner with such characteristic
IVDU was defined as lifetime intravenous drug users or lifetime sexual partners of intravenous drug users
Ethical considerations
The case control study was reviewed and approved by Ethical Committees in Brazil and Institutional Review Boards in the USA. Specific approval for this secondary data analysis was not obtained because the dataset has been de-identified.
RESULTS
The REDS-II Brazil HIV case-control study population includes 838 male respondents whose data were used in this analysis. Descriptive statistics for all of the 838 male donors, including the subset of 799 with ACASI questionnaire responses are provided (Table 1). Respondents had a mean age of 33.6 years, 596 (71.5%) completed elementary school, 433 (51.7%) were married, and 666 (79.5%) reported heterosexual partnerships in the past 12 months and, 90 (10.7%) reported having 6 or more partners in the past 12 months. Of the 799, 793 answered the questions from the sexual matrix on their recent sexual partners (Figure 1). About 10% had at least one partner with a ten or more years’ difference of age. Most of blood donors reported to have a main partner (75.0%). Four percent reported IVDU or being a sex partner of an IVDU. Thirteen percent reported having at least one MSM partner among the last five partners. More than one-third (35.8%) reported that they did not know about their partner’s HIV status and 4.0% answered that they had at least one HIV-positive partner in the last 12 months. Thirty percent of the respondents disclosed that they met their partner(s) at social/political events, in clubs, or church. More than two-thirds (66.7%) reported unprotected vaginal sexual encounter and more than one quarter (27.2%) reported unprotected heterosexual anal sex with at least one of the last five partners in the last 12 months.
Figure 1.
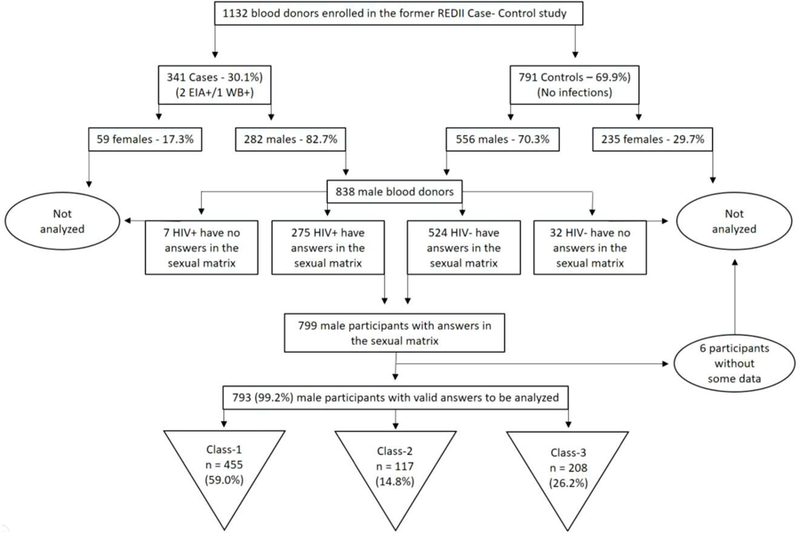
Flowchart showing the enrollment since the beginning of the former REDS-II Case control study until the selection of the male sample for the analysis performed in the present study.
Latent Class Analysis
There were no substantial differences between 3- or 4-class models, so based on parsimony we chose the 3-class model. The demographic characteristics of blood donors according to three classes are described (Table 2). Also, the last five partnerships characteristics are shown in table 3. Class-1 was the largest, with 59.0% of the sample having the probability of being in this class, and was represented by older donors (median 35.7±9.8 years), who were heterosexual (96.4%) and married (70.9%). Class-1 were in majority represented by HIV-negative (88.7%) blood donors. Compared to the other classes, Class-2 was younger (28.8±7.5) and unmarried blood donors (77.8%), who reported to have at least one MSM partnership (100%) and two thirds of the individual of this class (65.8%) had six or more sex partners in the past 12 months. HIV-positive donors are almost 98% of this class. Class-3 is represented by primarily heterosexual individuals (84.1%) who reported six or more sexual partners (44.7%) and 33 (15.9%) donors who were MSM. Class 3 and is almost equally represented by HIV-positive (50.5%) and negative (49.5%) donors, however the majority of HIV positive donors reported male-male-sex (63.6% - data not shown in tables). Table 3 shows a comparison of demographic characteristics, use of illicit drugs, venues where partners were met and sexual practices with their partners among the three classes. Donors from the Class-1 had significantly higher chance of having a main sex partner (99.4%) and to have had at least one unprotected vaginal sex encounter (77.8%). Class-2 was characterized by those donors who reported having had at least one partner with 10 years or more difference in age (34.2%), and having had at least one anonymous or sex worker partner (40.2%). About 80% of the individuals of the Class-2 disclosed that they didn’t know their partner(s) HIV status, while 17.1% had at least one known HIV-positive partner. Almost half of those in the Class-2 reported meeting their partners in a bar or carnival (46.2%), and more than two thirds (36.8%) met partners using an online dating app or service (internet/ads). The Class-3 was defined by those donors who had at least one unprotected vaginal and/or anal heterosexual intercourse encounter (66.8% and 40.9%, respectively).
Table 2.
Demographic characteristics, sexual history, number of partners and HIV status of 793 male blood donors who answered all the social matrix questions, according to the 3 classes.
| Characteristics | Class-1 | Class-2 | Class-3 |
|---|---|---|---|
| n=468 (59.0%) | n=117 (14.8%) | n=208 (26.2%) | |
| Age* | 35.7 ± 9.8 | 28.8 ± 7.5 | 32.1 ± 9.7 |
| Center ID* | |||
| Fundação Pró-Sangue – São Paulo | 107 (22.9) | 39 (33.3) | 81 (38.9) |
| Hemominas – Minas Gerais | 110 (23.5) | 17 (14.5) | 24 (11.5) |
| Hemope - Pernambuco | 97 (20.7) | 30 (25.6) | 40 (19.2) |
| Hemorio – Rio de Janeiro | 154 (32.9) | 31 (26.5) | 63 (30.3) |
| Educational level* | |||
| Illiterate / Inc. Elementary School/Adult Literacy | 45 (9.6) | 6 (5.1) | 31 (14.9) |
| Complete Elementary/High/Technician School | 338 (72.2) | 75 (64.1) | 152 (73.1) |
| Graduation/MD/PhD | 85 (18.2) | 36 (30.8) | 25 (12) |
| Marital status* | |||
| Married / living with | 332 (70.9) | 26 (22.2) | 61 (29.3) |
| Unmarried | 136 (29.1) | 91 (77.8) | 147 (70.7) |
| Sexual orientation based on the reported sex partners in the last 12 months* | |||
| Heterosexual | 451 (96.4) | - | 175 (84.1) |
| MSM/Bisexual* | 17 (3.6) | 117 (100.0) | 33 (15.9) |
| Number of partners in the last 12 months* | |||
| 0 to 1 | 142 (30.3) | 11 (9.4) | 62 (29.8) |
| 2 to 4 | 156 (33.3) | 29 (24.8) | 53 (25.5) |
| ≥ 6 | 170 (36.3) | 77 (65.8) | 93 (44.7) |
| HIV status* | |||
| HIV negative | 415 (88.7) | 3 (2.6) | 103 (49.5) |
| HIV positive | 53 (11.3) | 114 (97.4) | 105 (50.5) |
Difference between classes (p<0.05)
Table 3.
Demographic characteristics, drug use, venues and sexual practices with the sex partners* from 793 male blood donors who answered all the social matrix questions, according to the three classes.
| Partners’ Characteristics* | Class-1 | Class-2 | Class-3 |
|---|---|---|---|
| n=468 (59.0%) | n=117 (14.8%) | n=208 (26.2%) | |
| Partner’s age | |||
| Age disparity of ≥ ten years for one or more partners | 24 (5.1) | 40 (34.2)† | 12 (5.8) |
| Partner’s type | |||
| Main partner | 465 (99.4)† | 65 (55.6) | 65 (31.2) |
| Friend partner | 29 (6.2) | 41 (35) | 61 (29.3) |
| Acquaintance partner | 7 (1.5) | 45 (38.5) | 80 (38.5) |
| One time partner | 1 (0.2) | 36 (30.8) | 63 (30.3) |
| Anonymous or sex worker partner | - | 47 (40.2)† | 46 (22.1) |
| Intravenous drug user (IVDU)‡ | |||
| IVDU or partner IVDU | 6 (1.3) | 10 (8.5) | 15 (7.2) |
| Partner’s MSM | - | 103 (88.0)† | - |
| Partner’s HIV Status | |||
| Don’t know partner’s HIV status | 56 (12) | 94 (80.3)† | 133 (63.9) |
| HIV positive partner’s | 7 (1.5) | 20 (17.1)† | 4 (1.9) |
| Venue where met their partners | |||
| Meet in the bar/carnival | 42 (9.0) | 54 (46.2)† | 63 (30.3) |
| Meet in the street, park, library, public transportation | 59 (12.6) | 34 (29.1) | 49 (23.6) |
| Meet in a parties, clubs, political function or church | 132 (28.2) | 27 (23.1) | 79 (38) |
| Meet in the date service (Internet/Newspaper ads) | 9 (1.9) | 43 (36.8)† | 34 (16.3) |
| Meet some other way/work | 243 (51.9) | 43 (36.8) | 85 (40.9) |
| Unprotected sexual intercourse | |||
| Unprotected vaginal sex | 364 (77.8)† | 27 (23.1) | 139 (66.8)† |
| Unprotected heterosexual anal sex | 114 (24.4) | 17 (14.5) | 85 (40.9)† |
Partner’s characteristics were based on the criteria of having at least one partner with such characteristic
Variables that most clearly define the profile classes’ profile
IVDU criteria were defined as lifetime intravenous drug users or lifetime sexual partners of intravenous drug users.
Random Forest Analysis
The random forest result showed that with all variables we analyzed (listed in table 4), the sensitivity of these questions would be 0.76, while the specificity would be 0.89. The PPV of this set of questions to identify HIV-positive donors during the predonation interview is 0.85. When we removed the questions about classification of partner type (main, acquaintance, etc.) these values did not change. When we removed questions about sexual orientation, the values of sensitivity, specificity and PPV decreased (to 0.69, 0.84 and 0.78, respectively). When we removed both questions about partner type and sexual orientation together the sensitivity decreased (0.67), but the specificity and PPV remained similar (0.84 and 0.78, respectively). The most important question to predict whether a donor is HIV positive in all models is knowing the HIV status of their sexual partner(s), as we can see in figure 2. When this question was removed, we found the lowest sensitivity (0.58)
Table 4.
Sensitivity, specificity and positive/negative predictive values in random forest permutation, including all 838 cases and controls male blood donor’s answers for the sociodemographic and sexual matrix questions
| Measures/Permutation | All variables | Without Type of partners variables | Without sexual orientation variables | Without both partner’s type and sexual orientation variables | Without partner’s HIV status |
|---|---|---|---|---|---|
| Sensitivity | 0.76 | 0.76 | 0.69 | 0.67 | 0.58 |
| Specificity | 0.89 | 0.89 | 0.84 | 0.84 | 0.94 |
| Positive Predicitive Value | 0.85 | 0.85 | 0.78 | 0.78 | 0.88 |
| Negative Predicitive Value | 0.82 | 0.82 | 0.77 | 0.76 | 0.73 |
Figure 2.
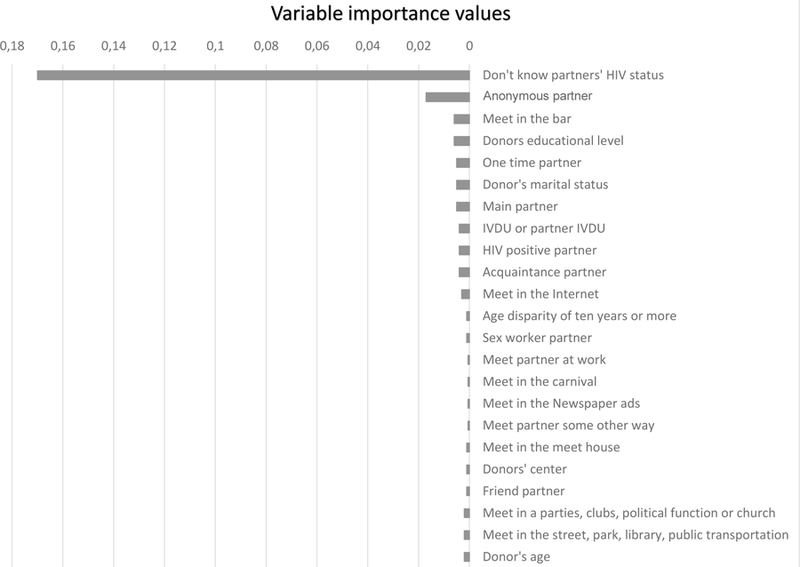
Random forest graphic showing the variable importance chart, including all 838 HIV positive and negative male blood donor’s answers for the sociodemographic and social matrix question, but removing the variables about “Sexual orientation”
DISCUSSION
We evaluated blood donors who tested positive and negative for HIV in blood centers from four locations in Brazil. Latent class analysis revealed three classes, with distinct levels of risk behavior. Two Classes (1 and 2) with differing HIV status were very well described with dissimilar behaviors, but Class 3 with mixed behaviors, had the same proportion of HIV positives and negatives. The Class-3 is predominantly a group of heterosexual, unmarried donors, with multiple sexual partners who are having unprotected sex. Therefore, a closer look at this group is needed, since almost half of these individuals are potentially eligible blood donors and can return for new donation. Some characteristics of donors’ sexual partners such as age, type of partner, as well as where donors met their partners may directly affect the risk of being HIV positive. Thus, an understanding of respondent’s sexual networks may be extremely useful to improve predonation interviews currently used to select eligible blood donors.
In Class-1 most donors informed practicing unprotected sex. However, most also reported to have one main partner, explaining why donors in this class are HIV-negative. Despite unprotected sex representing a source of HIV risk in many contexts, our study shows that this could be viewed as a protective factor by virtue of it being an indicator of lower number of sexual partners in Class-1 members when compared to the other Classes (16).
Class-2 was defined by donors who did not know the HIV status of their partners. Previous studies have shown that a large number of HIV-positive persons, especially young people, engage in unprotected sex with casual partners with unknown HIV status (17–19). The HIV status disclosure to sex partners is very complex and influenced by gender, anticipated support, fear of rejection and sociocultural context such as stigma/rejection (20). The lack of support and fear of rejection are less likely to occur in individuals with main and steady partners, so probably the type and number of sexual partners also contributed to the disclosure of HIV status. In some settings HIV positive persons are encouraged or legally expected to disclose their HIV status to their partners as a strategy to reduce HIV transmission (21, 22). Currently, this is not the situation in Brazil. Nonetheless, more studies are needed to understand the influence of knowledge of HIV status on sexual partnerships and what factors influence the disclosure of HIV status. Class-2 also reported to have met their partners in dating services (internet/ads) or in a bar/carnival, being the only class in which the meeting venue clearly defined the class’ profile. A recent study has pointed out that there are more risky places than others for risk of sexually transmitted infection, and some people gather at these sites to find potential sexual partners. As a cluster, many individuals at risk and who attend these venues constitute the “risk environment” for HIV acquisition (23). This was evident in our study even though it was not defined as an objective of the original REDS-II HIV case-control study.
The random forest analysis showed that the sensitivity values would decrease minimally if direct questions about sexual orientation of blood donors were removed from predonation interviews. When we remove questions about sexual history and partner’s type together but keep the partner’s HIV unknown status in the model, we achieve reasonable values. The knowledge about sexual partner(s) HIV status followed by other questions were a strong predictor for donor’s HIV status. Mathematical models show that HIV status disclosure can directly impact HIV transmission risk and that individuals who disclosure their HIV status are less likely to have multiple sex partners and more likely to use condoms (24–26). Removal of questions about sexual orientation and type of sexual partners does not entail significant losses in sensitivity, specificity and PPV of the models to predict whether donors are HIV positive. However, if the question about HIV status of sexual partners was included as a criterion for donor eligibility, the number of deferrals for persons who do not know their sex partner’s HIV status could potentially increase to an unacceptably high proportion. A previous study suggests that extensive questioning of blood donors about their sexual behavior may lead to the loss of existing donors who may find the process invasive (27).
This study has some limitations. The original case-control study included a convenience sample of HIV cases and a probability sample of controls. The behaviors and characteristics of the respondents may or may not reflect all HIV-positive and infection-negative donors in Brazil. We conducted this analysis for males only, and so the same questions may or may not be capable of predicting HIV-infection risk in females. Because of the context of HIV risk and sexual orientation it was necessary to focus just on male respondents to asses if there are differences within the male blood donors and to measure the impact of the possible changes in the deferral policy for MSM in Brazil. In addition, we have generalized our findings for the participants from the four blood centers in Brazil, assuming they are representative of male donors throughout the country. Despite these limitations, this study represents one of few in the field of sexual networks in blood donors and points out further studies in this domain to guide changes in blood donations selection are necessary.
We conclude that LCA methods can assess the interaction of multiple risk factors that place individuals at different levels of risk for acquiring sexual transmitted infections, including HIV. This type of assessment is not possible with regular regression methods, but shows that use of LCA can help to improve clinical screening and blood donor selection. In our study, HIV positive blood donors have a homogeneous pattern of behavior, with very well-known high-risk behaviors. With exception of the Class 3 profile with blood donors that are engaged in mixed high and low-risk behaviors, the study did find compelling results for questions that could reliably differentiate between lower and higher risk blood donors, an unresolved challenge in donor selection. A tendency emerging in some countries, such as Spain, Italy and Portugal, is to select blood donors based on individual risk assessments, that can include partners with unknown risk behaviors, new or multiple partners, and not to consider just if a sexual partner is the same or opposite sex (3, 28). We do not know what the impact of this approach would be in Brazilian blood services. Considering that blood donor selection in Brazil is performed via face-to-face interview and based on epidemiological data about well-known high-risk behaviors, we recognize it would not be easy to change to other approaches to donor eligibility questioning. Research to understand barriers to such change would need to be completed to ensure the adequacy of the blood supply would not be adversely affected. Nonetheless, we conclude that direct or indirect questions about sexual orientation used in the selection of blood donors could be replaced by an inquiry into the knowledge about sexual partner’s HIV status. Thus, while this study shows changes to donor questioning can differentiate between higher and lower risk donors, we believe it is premature to move to new donor eligibility questions in Brazil that have not been studied to assess donor comprehension and acceptability.
Acknowledgements:
The authors thank the support from the University of California, San Francisco’s International Traineeships in AIDS Prevention Studies (ITAPS) and the Blood System Research Institute (BSRI) for their assistance in the preparation of this article. We also would like to thank the blood donors for providing consent and helping the present study. The Retrovirus Epidemiology Donor Study - II (REDS-II), International Component (Brazil) was responsibility of the following persons: Blood Centers: Fundação Pró-Sangue/Hemocentro São Paulo (São Paulo) - Ester C. Sabino, Cesar de Almeida Neto, Alfredo Mendrone Jr., Ligia Capuani and Nanci Salles; Hemominas (Belo Horizonte, Minas Gerais) - Anna Bárbara de Freitas Carneiro-Proietti, Fernando Augusto Proietti, Claudia Di Lorenzo Oliveira and Carolina Miranda; Fundação Hemope (Recife, Pernambuco) - Divaldo de Almeida Sampaio, Silvana Ayres Carneiro Leão and Maria Inês Lopes. Data Warehouse: University of São Paulo (São Paulo) - João Eduardo Ferreira, Márcio Oikawa and Pedro Losco Takecian. US Investigators: Blood Systems Research Institute and University of California San Francisco - M.P. Busch, E.L. Murphy, B. Custer and T. Gonçalez; Coordinating Center: Westat, Inc - J. Schulman, M. King and K. Kavounis; National Heart, Lung, and Blood Institute, NIH - S.A. Glynn.
This study was funded by a grant from a partnership from University of California in San Francisco and the Vitalant Foundation, San Francisco, CA. Also is part of a PhD project financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001”
Footnotes
The authors declare no conflicts of interest
References
- 1.Sabino EC, Gonçalez TT, Carneiro-Proietti AB, Sarr M, Ferreira JE, Sampaio DA, et al. Human immunodeficiency virus prevalence, incidence, and residual risk of transmission by transfusions at Retrovirus Epidemiology Donor Study-II blood centers in Brazil. Transfusion 2012;52(4):870–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brasil. Ministério da Saúde. Portaria 158 de 04 de fevereiro de 2016. Redefine o regulamento técnico de procedimentos hemoterápicos.
- 3.Benjamin RJ, Bianco C, Goldman M, Seed CR, Yang H, Lee J, et al. Deferral of males who had sex with other males. Vox sanguinis 2011;101(4):339–67. [DOI] [PubMed] [Google Scholar]
- 4.Brito AMd, Castilho EAd, Szwarcwald CL. AIDS e infecção pelo HIV no Brasil: uma epidemia multifacetada. Revista da Sociedade Brasileira de Medicina Tropical 2001;34:207–17. [DOI] [PubMed] [Google Scholar]
- 5.Jones A, Cremin I, Abdullah F, Idoko J, Cherutich P, Kilonzo N, et al. Transformation of HIV from pandemic to low-endemic levels: a public health approach to combination prevention. The Lancet 2014;384(9939):272–9. [DOI] [PubMed] [Google Scholar]
- 6.de Almeida Neto C, McFarland W, Murphy EL, Chen S, Nogueira FA, Mendrone A, et al. Risk factors for human immunodeficiency virus infection among blood donors in Sao Paulo, Brazil, and their relevance to current donor deferral criteria. Transfusion 2007;47(4):608–14. [DOI] [PubMed] [Google Scholar]
- 7.Blatyta PF, Custer B, Gonçalez TT, Birch R, Lopes ME, Lopes Ferreira MI, et al. Undisclosed human immunodeficiency virus risk factors identified through a computer-based questionnaire program among blood donors in Brazil. Transfusion 2013;53(11):2734–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Almeida-Neto C, Goncalez TT, Birch RJ, de Carvalho SM, Capuani L, Leão SC, et al. Risk factors for human immunodeficiency virus infection among Brazilian blood donors: a multicentre case-control study using audio computer-assisted structured interviews. Vox Sang 2013;105(2):91–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patavino GM, de Almeida-Neto C, Liu J, Wright DJ, Mendrone-Junior A, Ferreira MI, et al. Number of recent sexual partners among blood donors in Brazil: associations with donor demographics, donation characteristics, and infectious disease markers. Transfusion 2012;52(1):151–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brasil. Ministério da Saúde (MS). Boletim epidemiológico Aids e DST Brasília: MS; 2017.
- 11.Alexander J, Rose J, Dierker L, Chan PA, MacCarthy S, Simmons D, et al. It is complicated: sexual partner characteristic profiles and sexually transmitted infection rates within a predominantly African American population in Mississippi. Sex Transm Dis 2015;42(5):266–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trevor Hastie, Tibshirani Robert, Friedman JH. Springerseries in statistics New York, Springer, 2009. Book. 2nd ed.xxii, 745 pages. [Google Scholar]
- 13.Sanchez AM, Schreiber GB, Glynn SA, Bethel J, Kessler D, Chang D, et al. Blood-donor perceptions of health history screening with a computer-assisted self-administered interview. Transfusion 2003;43(2):165–72. [DOI] [PubMed] [Google Scholar]
- 14.Linzer DA, Lewis JB. poLCA: An R package for polytomous variable latent class analysis. J Stat Softw 2011;42:1–29. [Google Scholar]
- 15.Chen C, Liaw A, L B, editors. Using Random Forest to Learn Imbalanced Data2004; University of California, Berkeley. [Google Scholar]
- 16.Boily MC, Baggaley RF, Wang L, Masse B, White RG, Hayes RJ, et al. Heterosexual risk of HIV-1 infection per sexual act: systematic review and meta-analysis of observational studies. Lancet Infect Dis 2009;9(2):118–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Conserve DF, King G. An examination of the HIV serostatus disclosure process among Haitian immigrants in New York City. AIDS care 2014;26(10):1270–4. [DOI] [PubMed] [Google Scholar]
- 18.Tassiopoulos K, Moscicki A-B, Mellins C, Kacanek D, Malee K, Allison S, et al. Sexual risk behavior among youth with perinatal HIV infection in the United States: predictors and implications for intervention development. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2013;56(2):283–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Latkin C, Yang C, Tobin K, Roebuck G, Spikes P, Patterson J. Social Network Predictors of Disclosure of MSM Behavior and HIV-Positive Serostatus Among African American MSM in Baltimore, Maryland. AIDS and Behavior 2012;16(3):535–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lunze K, Cheng DM, Quinn E, Krupitsky E, Raj A, Walley AY, et al. Nondisclosure of HIV Infection to Sex Partners and Alcohol’s Role: A Russian Experience. AIDS and Behavior 2013;17(1):390–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Galletly CL, Glasman LR, Pinkerton SD, Difranceisco W. New Jersey’s HIV exposure law and the HIV-related attitudes, beliefs, and sexual and seropositive status disclosure behaviors of persons living with HIV. American journal of public health 2012;102(11):2135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vu L, Andrinopoulos K, Mathews C, Chopra M, Kendall C, Eisele TP. Disclosure of HIV Status to Sex Partners Among HIV-Infected Men and Women in Cape Town, South Africa. AIDS and Behavior 2012;16(1):132–8. [DOI] [PubMed] [Google Scholar]
- 23.Young LE, Michaels S, Jonas A, Khanna AS, Skaathun B, Morgan E, et al. Sex Behaviors as Social Cues Motivating Social Venue Patronage Among Young Black Men Who Have Sex with Men. AIDS and Behavior 2017;21(10):2924–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Niccolai LM, Dorst D, Myers L, Kissinger PJ. Disclosure of HIV status to sexual partners: predictors and temporal patterns. Sexually transmitted diseases 1999;26(5):281–5. [DOI] [PubMed] [Google Scholar]
- 25.Pinkerton SD, Galletly CL. Reducing HIV Transmission Risk by Increasing Serostatus Disclosure: A Mathematical Modeling Analysis. AIDS and Behavior 2007;11(5):698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kalichman SC, Kalichman MO, Cherry C, Grebler T. HIV Disclosure and Transmission Risks to Sex Partners Among HIV-Positive Men. AIDS Patient Care and STDs 2016;30(5):221–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldman M, Yi QL, Ye X, Tessier L, O’Brien SF. Donor understanding and attitudes about current and potential deferral criteria for high-risk sexual behavior. Transfusion 2011;51(8):1829–34. [DOI] [PubMed] [Google Scholar]
- 28.Suligoi B, Pupella S, Regine V, Raimondo M, Velati C, Grazzini G. Changing blood donor screening criteria from permanent deferral for men who have sex with men to individual sexual risk assessment: no evidence of a significant impact on the human immunodeficiency virus epidemic in Italy. Blood Transfus 2013;11(3):441–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


