Abstract
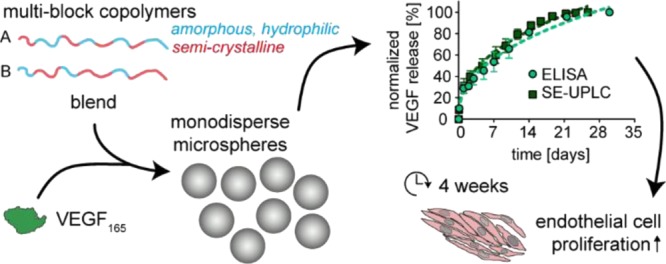
Vascular endothelial growth factor (VEGF) is the major regulating factor for the formation of new blood vessels, also known as angiogenesis. VEGF is often incorporated in synthetic scaffolds to promote vascularization and to enhance the survival of cells that have been seeded in these devices. Such applications require sustained local delivery of VEGF of around 4 weeks for stable blood vessel formation. Most delivery systems for VEGF only provide short-term release for a couple of days, followed by a release phase with very low VEGF release. We now have developed VEGF-loaded polymeric microspheres that provide sustained release of bioactive VEGF for 4 weeks. Blends of two swellable poly(ε-caprolactone)–poly(ethylene glycol)–poly(ε-caprolactone)-b-poly(l-lactide) ([PCL–PEG–PCL]-b-[PLLA])-based multiblock copolymers with different PEG content and PEG molecular weight were used to prepare the microspheres. Loading of the microspheres was established by a solvent evaporation-based membrane emulsification method. The resulting VEGF-loaded microspheres had average sizes of 40–50 μm and a narrow size distribution. Optimized formulations of a 50:50 blend of the two multiblock copolymers had an average VEGF loading of 0.79 ± 0.09%, representing a high average VEGF loading efficiency of 78 ± 16%. These microspheres released VEGF continuously over 4 weeks in phosphate-buffered saline pH 7.4 at 37 °C. This release profile was preserved after repeated and long-term storage at −20 °C for up to 9 months, thereby demonstrating excellent storage stability. VEGF release was governed by diffusion through the water-filled polymer matrix, depending on PEG molecular weight and PEG content of the polymers. The bioactivity of the released VEGF was retained within the experimental error in the 4-week release window, as demonstrated using a human umbilical vein endothelial cells proliferation assay. Thus, the microspheres prepared in this study are suitable for embedment in polymeric scaffolds with the aim of promoting their functional vascularization.
1. Introduction
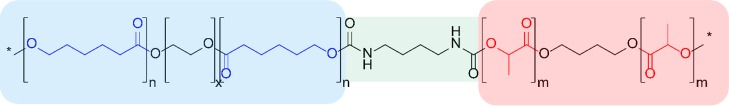
Tissue engineering aims at developing bioartificial implants which can be used for replacement or repair of damaged tissues.1−3 Different categories of such engineered tissues can be distinguished: full synthetic biomaterials, (decellularized) scaffolds from natural origins, and hybrid biomaterials that consist of both synthetic and biological or cellular components.4−6 When the implanted material contains cells or when it will be infiltrated by cells after it has been transplanted, one can consider such biomaterial as an artificial tissue or organ.7 One of the major challenges of constructing cellularized biomaterials is the sufficient supply of nutrients and oxygen from the systemic circulation into the implant.8 Incorporation of growth factors into the tissue-engineered construct can locally stimulate angiogenesis towards the implant, thereby providing vascularization of the construct.9,10 Vascular endothelial growth factor (VEGF) is the most prominent pro-angiogenic growth factor and stimulates angiogenesis by binding to the VEGF receptor present on endothelial cells.11 Stable vascularization of an implant depends on the dose of VEGF and the time period of VEGF release at the site of implantation.10,12 The current literature suggests that a constant dose of VEGF for around 4 weeks leads to sufficient vascularization in rodent models.13,14 Formulation of VEGF into a drug delivery system ideally offers control of the amount of VEGF released and the time span of VEGF release into the adjacent tissue.15,16 Drug delivery systems such as hydrogels, viscous liquids, and microspheres have been developed for sustained release of VEGF.17−19 Particularly, polymer-based microspheres present an attractive delivery platform for proteins due to their tailorable polymer-dependent release profile and enhanced stability of the encapsulated cargo.20−22 Several groups have formulated VEGF in microspheres based on PLGA, which is the most widely applied polymer used for the design for controlled release formulations.23−27 Release of VEGF from PLGA matrices, however, is often biphasic with a high initial burst within the first few hours followed by a relatively slow continuous release in the following weeks.28−30 This release profile is not ideal for functional vascularization of biomaterials as a more sustained elevation of VEGF is needed for the stimulation of blood vessel growth.14,31 Commonly, burst release from PLGA-based microspheres is not controlled by erosion of the polymer particles, but by surface-bound cargo and protein molecules that are released from pores present in the particles that allow rapid diffusion and release of biopharmaceutical drugs.32,33 Another limitation of PLGA-based systems is the retention of acidic degradation products within the polymeric matrix, resulting in a pH decrease in the microspheres34,35 that can have a negative impact on the stability of proteins.23,36 In order to obtain tailorable release of biopharmaceutical protein drugs, Kazazi-Hyseni et al. prepared PLGA microspheres with differences in porosity by varying formulation parameters such as polymer concentration and oil/water ratios in a membrane emulsification process.37 An alternative approach for tailoring the release of pharmaceutical proteins from polymeric microspheres is the use of phase-separated multiblock copolymers.38,39 SynBioSys® multiblock copolymers composed of amorphous poly(ε-caprolactone)–poly(ethylene glycol)–poly(ε-caprolactone) (PCL–PEG–PCL) blocks and semicrystalline poly(l-lactic acid) (PLLA) blocks (as shown in Figure 1) are more hydrophilic than for example PLGA, due to the presence of PEG. The well-controlled swelling of these [PCL–PEG–PCL]-b-[PLLA] polymers allows continuous release of encapsulated molecules through diffusion with low burst release.40−42 The swelling degree of these [PCL–PEG–PCL]-b-[PLLA] polymers is dependent on the weight fraction and molecular weight of PEG.42,43 We hypothesized that the release characteristics of VEGF from multiblock copolymeric microspheres can be tailored by blending multiblock copolymers with different swelling degrees.
Figure 1.
General chemical composition of multiblock copolymers used in this study. In blue shading: amorphous, hydrophilic block, n: PCL, x: PEG. In green shading: urethane linker, in red shading: semicrystalline block, m: poly(l-lactic acid). The two polymers used in this study differ in their block weight fraction (hydrophilic block–semicrystalline block), PEG chain length, and total PEG weight fraction.
In the present study, VEGF was formulated in multiblock copolymer microspheres using a double emulsion-based membrane emulsification method. With this method, monodisperse microspheres with a narrow, well-defined size distribution, are obtained, which is a determining parameter for well-defined and reproducible controlled release systems.44,45 Furthermore, membrane emulsification is advantageous due to its low batch-to-batch variability, decreased mechanical stress on the loaded protein, and high encapsulation efficiency.21,46,47 To the best of our knowledge, this is the first occasion in which monodisperse VEGF-loaded microparticles are prepared by membrane emulsification, in which we furthermore aim at a sustained release profile of several weeks. The release of VEGF from microspheres was measured by two analytical methods, namely size exclusion ultra-performance liquid chromatography (SE-UPLC) and enzyme-linked immunosorbent assay (ELISA). Finally, the bioactivity of VEGF released during the entire release period was assessed by a human umbilical vein endothelial cells (HUVEC) proliferation assay.
2. Results and Discussion
2.1. Selection of Suitable Blend Composition
Microsphere batches were prepared with a target VEGF loading of 0.2 wt % and different blend ratios of multiblock copolymers A and B in order to obtain a microsphere formulation with the desired release profile, that is, a minimal burst followed by a sustained release for 4 weeks. These polymers were selected based on the previous work of Teekamp et al. who achieved a 2 week controlled release profile of human serum albumin (HSA) from microspheres based on multiblock copolymers A and B.48 The inner water phase of the emulsified droplets consisted of 5 mM succinate buffer pH 5, which is similar to the buffer used by Cleland et al. for the preparation of solid VEGF microparticles by spray-drying, which were subsequently encapsulated into PLGA microparticles by solid-in-oil emulsification.19 Microspheres were prepared by the double emulsion method in which a water-in-oil (w1/o) primary emulsion was processed over a stainless steel membrane with 20 μm pores. The obtained microspheres were collected after extraction and evaporation of the organic solvent, washed and without further sieving or fractionating freeze-dried. The freeze-dried microspheres consisted of uniformly sized microparticles with average diameters ranging between 42 and 51 μm and narrow size distribution [12–28% coefficient of variance (CV), Table S2], characteristic for membrane emulsification.46 The diameter of the obtained particles is approximately twice that of the pores in the membrane, a common observation with membrane emulsification. At high dispersed phase flow rates, the extra dispersed phase is pressed into the formed droplet with an initial size equal to the pore diameter before it detaches, resulting in a larger droplet diameter.46
Scanning electron microscopy (SEM) analysis (Figure S2) showed differences in the morphology of the microspheres depending on the polymer blend composition. Microspheres prepared with polymer A or a blend of polymer A and B were porous, whereas microspheres prepared with polymer B only had a smooth surface with scattered visible pores.
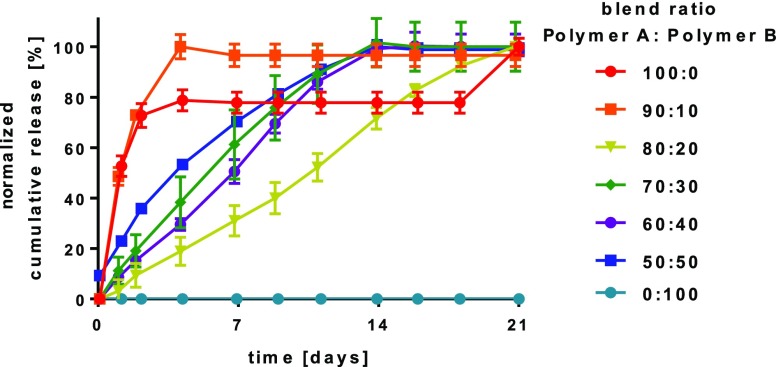
Microspheres were screened based on their 3 week release pattern, as the growth factor release pattern in this time period is crucial for vascularization of biomaterial implants.13 VEGF release was measured by SE-UPLC and is plotted as normalized cumulative VEGF. Total cumulative release after 21 days is assumed to represent the complete release of encapsulated VEGF (with the exception of 0:100 blend ratio)fig2.
Figure 2.
Cumulative release of VEGF from microspheres based on various blends of multiblock polymer A and B (shown in legend) and target VEGF loading of 0.2 wt %. The release was performed at 37 °C in PBS pH 7.4 supplemented with 0.025% Tween 20 and 0.02% NaN3. Released VEGF was quantified by SE-UPLC.
Microspheres based on a 90:10 blend of polymer A and B and of 100% polymer A showed a high initial VEGF release during the first 2 days followed by a period of 19 days without any further release. As we aimed for a formulation demonstrating the continuous release for several weeks, these formulations were not suitable for our purposes. In contrast, only microspheres based on polymer B did not release VEGF during the three-week timespan of the release experiment. Possibly, these microspheres had a low VEGF loading efficiency and therefore no VEGF release was observed. This observation is in line with the release study published by Teekamp et al. who also observed no release of HSA in the 2 weeks from when the microspheres were prepared with polymer B.48 This microsphere formulation also did not meet our release profile target. Lastly, the release profiles of VEGF from microspheres based on various blends of polymer A and B (i.e., 80:20, 70:30, 60:40, and 50:50) showed continuous release for around 2 weeks with minimal burst release. However, the differences between release profiles from microspheres based on 80:20, 70:30, and 60:40 blends were minimal. The average release rate of these blends was approximately 5–7% release per day for a continuous period of at least 14 days, which met our initial selection criteria for release kinetics. Slight differences in sustained release pattern are likely an interplay between the total PEG content and PEG chain lengths of each polymer. Previous studies with similar multiblock copolymers have shown that the release of proteins from these polymers is governed by the PEG content which leads to swelling of the microspheres, and subsequent diffusion of protein through water-filled pores.41−43
For further development, the 50:50 blend of polymer A and B was selected due to its preferred release kinetics, that is, continuous release without significant burst release, which was also the blend that had been selected by Teekamp et al. for delivery of pPB-HSA.48
2.2. In Vitro Degradation Study of Microspheres Prepared with the 50:50 Blend Ratio
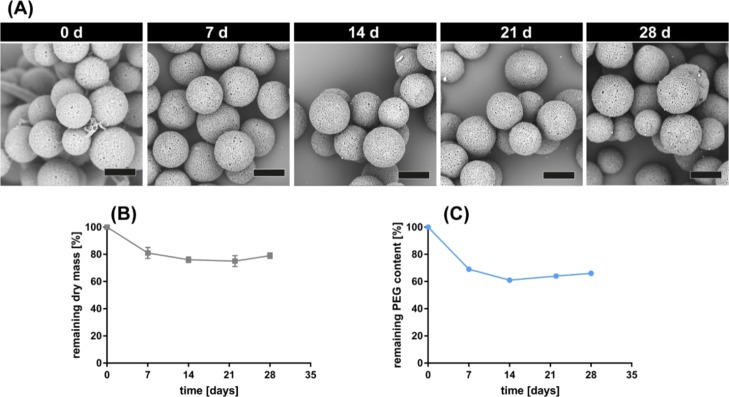
The degradation properties of microspheres based on a 50:50 blend of polymer A and B was studied with nonloaded placebo microspheres. These microspheres had a porous morphology (Figure 3a, left image “0 d”) and a narrow size distribution (40 ± 6 μm) comparable to VEGF-loaded microspheres prepared with the same polymer blend (Table S2 and Figure S2). During incubation in IVR buffer for 28 days, the microspheres retained their spherical shape and porous morphology, as shown in Figure 3a, indicating that hardly any erosion took place.
Figure 3.
In vitro degradation of placebo microspheres prepared with polymer A: polymer B blend of 50:50 after incubation at 37 °C in PBS pH 7.4, supplemented with 0.025% Tween 20, and 0.02% NaN3. (A) SEM images before and after incubation. Scale bars represents 30 μm. The time of incubation (d: days) is stated above each image, whereby “0 d” shows freshly prepared microspheres before incubation. (B) Remaining microsphere dry mass after 28 days and (C) remaining PEG content in the microsphere samples, as determined by 1H NMR.
This observation is in line with the degradation data as shown in Figure 3b, which shows that after a slight decrease in mass of ∼20% after 7 days, the remaining dry mass did not change the next 21 days. The composition of degrading microspheres over time was analyzed for the PEG content. Figure 3c shows that the PEG content decreased by 30% within 7 days, and then no further changes occurred up to 28 days. Gel permeation chromatography (GPC) analysis of degradation samples showed that the molecular weight of the polymers was reduced significantly after 7 days of incubation (Figure S3). From 7 to 28 days, a further slow reduction in molecular weights of the polymers was observed. These results indicate that in the first 7 days, a small fraction of PEG was cleaved resulting in chain scissions in the polymers and diffusion of PEG out of the polymer matrix. This observation is in agreement with previous studies reporting that PEG is shed specifically during the early stages of degradation because of preferential cleavage of the ester bonds that connect PEG and PCL units.49−52 Analysis by 1H NMR before and after addition of shift reagent trichloroacetylisocyanate (TAIC) showed that the constitution of the polymers remained similar during degradation of up to 28 days (Figures S4 and S5). The almost constant weight of the degrading samples and their stable composition between 7 and 28 days demonstrate that hydrolysis of ester bonds in the PCL and PLLA blocks hardly occurred. All in all, our results show that the slight initial loss in mass after 7 days of incubation is likely due to the hydrolysis of PEG–PCL bonds, resulting in the loss of a small fraction of PEG and causing a decrease in the molecular weight of the degrading polymers. Afterwards, molar composition of the polymers remained unchanged until the end of the degradation study. Therefore, no extensive degradation occurred during the 28 days of incubation.
2.3. Optimized Microsphere Formulation Based on the 50:50 Polymer Blend
For further studies, three microsphere batches with a higher target loading (1.0 wt %) were prepared with a 50:50 blend of polymer A and B. The preparation method was slightly modified by increasing batch size and VEGF/polymer ratio (Table 3, Experimental Section). These modifications aimed at increasing VEGF loading content and loading efficiency (as discussed in Section 2.1). The loading content of VEGF of microspheres prepared with a 0.2 wt % target loading could not be accurately analyzed, as VEGF concentrations in the samples were below the detection limit of the developed assay. Possible modifications such as increasing the amount of microspheres used for the protocol were not feasible, as it would have required dissolving ∼380 mg microspheres in 0.5 mL dimethyl sulfoxide (DMSO) in order to fall within the calibration curve of the assay (assuming a loading efficiency of 20%).
Table 3. Composition of the Water and Oil Phases Used for the Preparation of Microspheres.
| |
target VEGF loading |
|||
|---|---|---|---|---|
| formulation parameters | Placebo | 0.2 wt % | 1.0 wt % | |
| w1-phase | VEGF concentration | n.a.a | 2 mg/mL | 15–20 mg/mL |
| o-phase | polymer concentration in DCM | 10 wt % | 10 wt % | 15–20 wt % |
| ratio VEGF/polymer | n.a. | 1:500 | 1:100 | |
| w2-phase | continuous phase | 0.4 wt % PVA, 5 wt % NaCl | 0.4 wt % PVA, 5 wt % NaCl | 4 wt % PVA, 5 wt % NaCl |
n.a. = not applicable.
Microspheres prepared with a 1.0 wt % target loading had a narrow size distribution (Table 1, average sizes between 44 and 52 μm, CV between 15 and 30%, size distribution plots shown in Figure S6). SEM analysis of the obtained microspheres showed a smooth surface with small pores (Figure 4). Table 1 summarizes the characteristics of the obtained microspheres, per microsphere batch and average values for the three individually prepared batches. The batch yields ranged from 65 to 74%. VEGF loading was determined by BCA protein assay after destruction of the particles and corresponded to a high average loading efficiency of 78 ± 16%. The increased encapsulation efficiency as compared to microspheres with a target loading of 0.2 wt % (as described in Section 2.1) can be explained by the introduced modifications, in line with previous experiments.53−56 An increased polymer concentration of the oil phase leads to a shorter time of solidification as less solvent has to be removed. This in turn decreases the diffusion of the protein into the continuous phase and thereby increases the loading efficiency.53 All in all, three microsphere batches were prepared with similar characteristics regarding yield, VEGF loading and loading efficiency, thereby demonstrating low batch-to-batch variation and good batch reproducibility.
Table 1. Formulation Characteristics of Three Batches of VEGF-Loaded Microspheres Prepared with a 50:50 Blend Ratio of Polymer A and B, per Batch and Average Values ± SD for Each Formulation Characteristic.
| batch | yield [%] | average size [μm]; CV [%] | feed loading [wt %] | actual loading [wt %]a | loading efficiency [%] |
|---|---|---|---|---|---|
| 1 | 74 | 51; 15 | 1.00 | 0.72 | 72 |
| 2 | 73 | 52; 30 | 0.93 | 0.90 | 96 |
| 3 | 65 | 44; 17 | 1.13 | 0.76 | 67 |
| average ± SD | 71 ± 5 | 49 ± 4 | 1.02 ± 0.10 | 0.79 ± 0.09 | 78 ± 16 |
Loading of VEGF in microspheres was determined after destruction of loaded microspheres in DMSO and NaOH. VEGF content was quantified by BCA protein assay.
Figure 4.
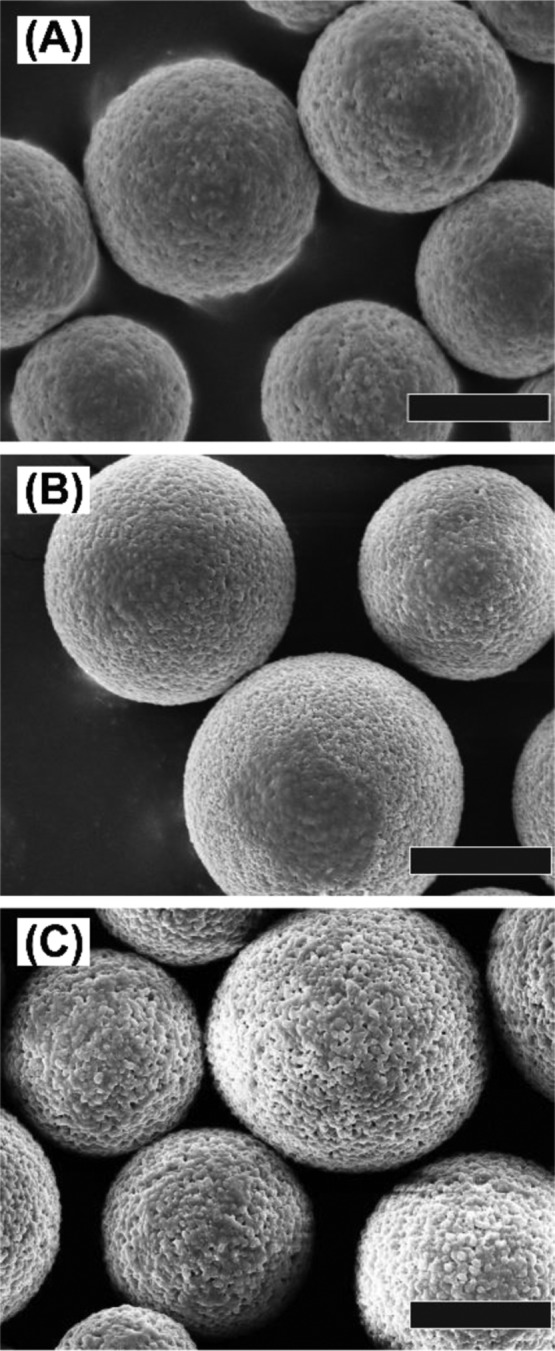
Morphology of VEGF-loaded microspheres (three individually prepared batches) prepared with a 50:50 blend of polymer A and B and a target loading of 1.0 wt % (see Table 1). SEM images; (A) batch 1, (B) batch 2, and (C) batch 3. Scale bar represents 20 μm.
2.3.1. In Vitro VEGF Release
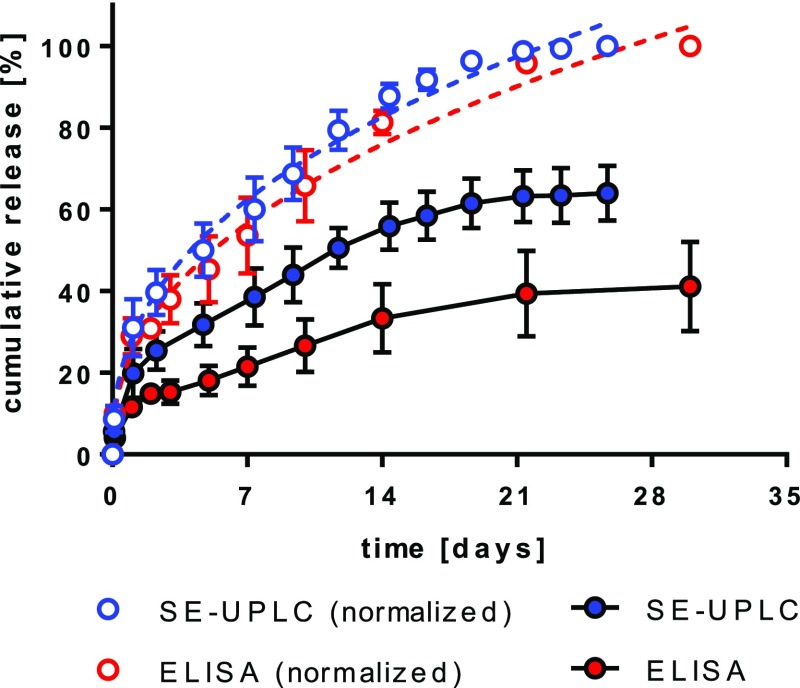
VEGF release from the obtained microspheres was measured by SE-UPLC and ELISA, as shown in Figure 5. Both cumulative release profiles were normalized based on the cumulative release at the end of the release study (day 30 for ELISA data and day 25 for SE-UPLC data). Microspheres of the 50:50 polymer blend released VEGF continuously over a period of ∼4 weeks with a low burst release. Normalized release profiles for both methods are in good agreement (Figure 5, blue and red circles). These release curves were fitted using the Korsmeyer–Peppas model (Figure 5, blue and red dotted lines).57,58 The calculated parameters, that is, diffusional exponent, 95% confidence interval, and correlation coefficient, of this fit are shown in Table 2. Both ELISA and SE-UPLC release data show a good fit for this model [R2: 0.97 (SE-UPLC data) and 0.96 (ELISA data)]. The diffusional exponents n were 0.41 ± 0.02 for SE-UPLC release data and 0.42 ± 0.02 for ELISA release data, suggesting the diffusion-related release. Taking the release profiles and the results of the degradation study (Section 2.2) together, it can be concluded that VEGF release from microspheres occurs via diffusion of VEGF through a water-filled porous network, caused by the hydrophilicity of PEG within the multiblock copolymer, as no extensive polymer erosion occurs.
Figure 5.
Cumulative release of VEGF from microspheres based on a 50:50 blend and a target VEGF loading of 1.0 wt %. The release was performed at 37 °C in PBS pH 7.4 supplemented with 0.025% Tween 20 and 0.02% NaN3. Released VEGF was measured by ELISA (red) and SE-UPLC (blue), and plotted as cumulative release (filled blue and red circles, connected by a black line) and as a normalized cumulative release (blue and red circles). Normalized cumulative release data were fitted using the Korsmeyer–Peppas model (blue and red dotted lines). Parameters of this fit are listed in Table 2.
Table 2. Korsmeyer–Peppas Model Fit Parameters for Normalized Cumulative Release Curves of SE-UPLC and ELISA Data, as Shown in Figure 5 as Blue and Red Dotted Lines, Respectively.
| normalized
cumulative release |
||
|---|---|---|
| Parametersa | SE-UPLC | ELISA |
| n | 0.41 ± 0.02 | 0.42 ± 0.02 |
| 95% CI | 0.37 – 0.44 | 0.39 – 0.46 |
| R2 | 0.97 | 0.96 |
n: diffusional exponent, 95% CI: 95% confidence interval, R2: correlation coefficient.
Based on loading determination with the BCA assay, VEGF was released up to 60% based on SE-UPLC data (Figure 5). In contrast, cumulative VEGF release by ELISA was ∼40% (Figure 5), most likely due to the numerous dilution steps towards the working range of the ELISA kit (31.3–2000 pg/mL) which might have resulted in protein loss due to the aspecific adsorption onto materials the protein is exposed to during sample handling. Similar underestimation of the VEGF levels were observed with freshly prepared VEGF solutions in IVR buffer and with IVR samples spiked with a defined VEGF concentration (Tables S3 and S4). In previous publications on VEGF-loaded PLGA-based microspheres, VEGF release quantified by ELISA reached cumulative release of >50% after 4 weeks.28,29,59 Because the formulations of the mentioned studies were prepared at much lower VEGF target loading (up to 100-fold lower as compared to our target loading of 1.0 wt %), those studies did not require extensive dilution for ELISA purposes. Nevertheless, the observed release profiles of our microspheres determined either by SE-UPLC or ELISA correlate well, corroborating the integrity of the released VEGF. To the best of our knowledge, our study is unique in comparing two analytical methods to measure protein release from microspheres.
The VEGF release profile of microspheres based on a 50:50 blend of polymer A and B (Figure 5) differs substantially from the published release curves of VEGF from PLGA microparticles. Several groups have reported biphasic release profiles with a high burst release (around 60% of the loading), followed by the sustained release of VEGF for 4 weeks accumulating 70–75% of the loaded amount.28,29 Similarly, the sustained release of VEGF from PLGA microspheres of ∼60% up to 7 days has been reported, followed by slow VEGF release reaching 70% after 28 days.59 In contrast to this, the VEGF-loaded microspheres used in this study, which are based on the swellable multiblock copolymers A and B in a ratio of 50:50, showed a low burst release and sustained release for nearly 4 weeks reaching 60% (as measured by SE-UPLC). The difference between release profiles of PLGA-based and [PCL–PEG–PCL]-b-[PLLA]-based microspheres can be explained by the surface-bound protein and protein close to the surface of PLGA-based microspheres that is released nearly completely within the first day “burst”, before the onset of erosion. In contrast, microspheres based on [PCL–PEG–PCL[-b-[PLLA] polymers release their encapsulated cargo via diffusion through a water-filled polymer matrix, caused by the hydrophilic PEG blocks.
2.4. Storage Stability at −20 °C
An important aspect of developing microspheres is preventing protein degradation and aggregation during preparation, storage, and release.23,24,60 It is essential that the release pattern of VEGF from freshly prepared microspheres and after long-term storage remains unchanged. Although previous studies have shown that the addition of cryoprotectants, such as trehalose, increases the stability of proteins formulated in PLGA nanoparticles after freeze-drying, the repeated storage, and long-term storage at −20 °C has not been investigated.61,62 In contrast, the freeze-thaw stability and long-term storage of aqueous protein formulations is well studied, showing that the frozen storage of aqueous protein formulations can cause degradation and aggregation of proteins.63,64 We therefore investigated the storage stability at −20 °C of VEGF-loaded microspheres by comparing the VEGF release profiles from freshly prepared microspheres with the VEGF release profiles from microspheres exposed to repeated freezing and storage at −20 °C as well as long-term storage at −20 °C.
Freeze-dried VEGF-loaded microspheres prepared with the 50:50 blend of polymer A and B, as characterized in Figures 4 and 5 and Tables 1 and 2, were frozen and stored at −20 °C overnight and subsequently incubated at room temperature for 3 h multiple times. After incubation at room temperature, a microsphere sample was removed for analyzing VEGF release with SE-UPLC. The remaining microspheres were returned to −20 °C storage. As shown in Figure S8a, release profiles of VEGF from microspheres repeatedly frozen (up to 5 times) remained highly similar to the release profile of freshly prepared microspheres, which was confirmed by similarity index f2 values of >70 (Table S5).65
Microspheres were also stored at −20 °C for 1, 2, 3, 6, and 9 months. At these time periods, microspheres were incubated at room temperature for at least 3 h, dispersed in IVR buffer and incubated at 37 °C. Released VEGF was quantified by SE-UPLC. VEGF release profiles from freshly prepared microspheres and from microspheres stored at −20 °C up to 9 months are shown in Figure S8b. No distinct differences between release profiles can be seen, confirmed by a similarity factor f2 of >50 (Table S6).65 Neither repeated storage at −20 °C nor long-term −20 °C storage of microspheres altered the release profile of VEGF from microspheres, as compared to release profiles from freshly prepared microspheres. Therefore, microspheres based on a 50:50 blend ratio of polymer A and B and loaded with VEGF present excellent storage stability.
2.5. Bioactivity of Released VEGF
It is crucial that the released VEGF from the microspheres over the 4 week period retained its bioactivity as this is necessary for stable blood vessel formation.31Figure 6 shows the bioactivity of released VEGF as compared to the native nonformulated VEGF, expressed as relative cell proliferation. The released protein at different time points led to relative cell proliferation of around 3. All released VEGF samples fall within the responsive range of the assay (1–3.5 relative cell proliferation). Supernatants of placebo microspheres served as controls. These control samples, containing possible degradation products of placebo microspheres such as PEG (as discussed above with Figure 3), did not induce proliferation.
Figure 6.
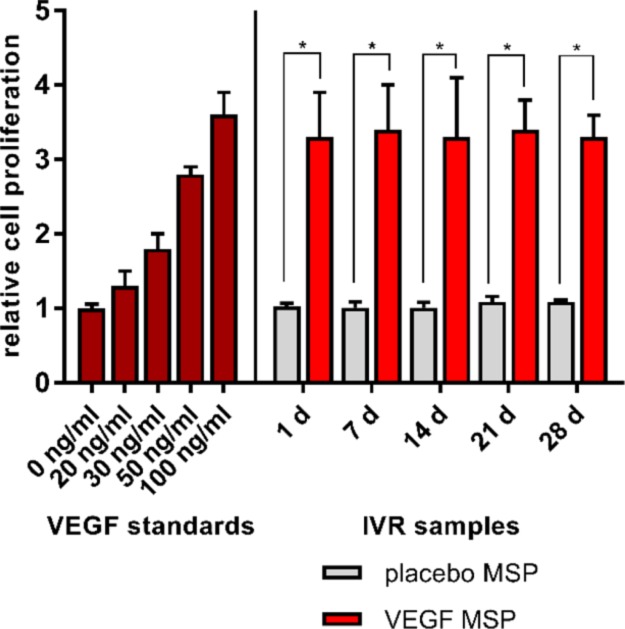
Bioactivity of released VEGF expressed as relative cell proliferation. On the left side of the graph (dark red bars): responsive range of VEGF standards between 0 and 100 ng/mL (n = 3 per concentration). On the right side of the graph (red and gray bars): relative cell proliferation of endothelial cells incubated with IVR supernatants collected from VEGF-loaded microspheres (“VEGF MSP”, red bars) or placebo microspheres (“placebo MSP”, gray bars). Microspheres had been stored at −20 °C for several months and have been exposed to several freezing cycles prior to the bioactivity assay. Supernatants of each time point were diluted in the culture medium and incubated in triplicate wells (bars represent average ± SD of n = 3). *p < 0.05 VEGF MSP versus placebo MSP.
The IVR buffer used for these cell-based bioactivity experiments was supplemented with bovine serum albumin (BSA) and antibiotics (bioactivity IVR buffer), instead of Tween 20 and sodium azide (components of IVR buffer for release studies in Figures 2 and 5), as these materials inhibited cell proliferation (data not shown). As a consequence, the VEGF concentration in the released supernatants could not be determined by SE-UPLC, as BSA interfered with the VEGF peak of the SE-UPLC chromatogram. The concentrations were therefore estimated with ELISA and normalized based on the cumulative release by SE-UPLC as presented in Section 2.3.1. ELISA release data had a good Korsmeyer–Peppas model fit (R2: 0.98) and a diffusional exponent of 0.36 ± 0.05 (95% confidence interval: 0.22–0.55), comparable to the ELISA release data in standard IVR buffer (as discussed in Section 2.3.1, Figure S9). Our results demonstrate that bioactivity of released VEGF was fully retained within the experimental error of the bioactivity assay. In several previous studies, the bioactivity of released VEGF was determined by similar HUVEC viability-based assays, however, these studies reported the bioactivity of VEGF released in the beginning of the release period only, that is up to 1 week.59,66 In contrast, we assessed the bioactivity of VEGF that is released throughout the entire release period, including between week 2, 3, and 4 of release. Precisely the later period of release, that is between 2 and 4 weeks, is critical for stable blood vessel formation.14,31 The bioactivity assay has been performed with VEGF microspheres that have been stored for several months at −20 °C and subjected to several freezing cycles. We therefore conclude that VEGF formulated in the microspheres remains bioactive for prolonged time.
Based on the data shown in this study, we estimate that a dose of 1 mg VEGF microspheres will provide an average release rate of 150 ng VEGF/day for 4 weeks, which has been shown to be sufficient for vascularization of a 0.1 mL biomaterial implant.14
3. Conclusions
In this study, we have developed monodisperse VEGF-loaded microspheres that exhibit sustained release kinetics for 4 weeks. This release profile is considered optimal for successful vascularization of a tissue-engineered construct. The developed VEGF-loaded microspheres were prepared with blends of [PCL–PEG–PCL]-b-[PLLA] multiblock copolymers with various PEG molecular weight and content, using a solvent extraction-based membrane emulsification process. The microspheres had a VEGF loading of 0.79 wt % and loading efficiency of 78%. VEGF release is governed by diffusion through the water-swollen polymer matrix. Released VEGF remained fully bioactive over the entire release period of 4 weeks. Therefore, microspheres based on multiblock copolymers and loaded with VEGF are an attractive vascularization platform for incorporation into tissue engineered constructs.
4. Experimental Section
4.1. Materials
Recombinant human VEGF165 was purchased from PeproTech Inc. (Rocky Hill, NJ, USA). Polyvinyl alcohol (PVA 5–88, 85–89% hydrolyzed) and sodium chloride (NaCl) were purchased from Merck (Germany). Disodium succinate, sodium dodecyl sulphate (SDS), TAIC, and BSA were purchased from Sigma-Aldrich (Germany). DMSO, Tween 20, sodium azide, potassium dihydrogen phosphate (KH2PO4), and dipotassium hydrogen phosphate (Na2HPO4) were purchased from Fisher Scientific (The Netherlands). Sodium hydroxide (NaOH) was purchased from VWR (The Netherlands). Gibco Dulbecco’s phosphate buffered saline (DPBS, 10×, composition 27 mM KCl, 15 mM H2PO4, 1.4 M NaCl, 81 mM Na2HPO4 × 7 H2O) was purchased from Thermo Fisher Scientific (The Netherlands). PEG standards for GPC analysis were purchased from PSS Polymer Standards Services (Germany).
4.2. Methods
4.2.1. Polymer Synthesis and Characterization
Multiblock copolymers A and B (general chemical composition shown in Figure 1) were synthesized and characterized based on procedures described by Stanković et al. and Teekamp et al.40,48 Polymer A consisted of 30 wt % of an amorphous, hydrophilic PCL–PEG3000–PCL block with a molecular weight of 4000 g/mol and 70 wt % of a semicrystalline poly(l-lactide) (PLLA) block with a molecular weight of 4000 g/mol. The total PEG weight fraction of polymer A is 22.5%. Polymer B consisted of 50 wt % of PCL–PEG1000–PCL (Mw: 2000 g/mol) and 50 wt % of the PLLA block (Mw: 4000 g/mol), resulting in a PEG weight fraction of 25%. The molecular weights of polymer A and B are reported in the Supporting Information.
4.2.2. Preparation of Monodisperse Microspheres
Polymeric microspheres were prepared by a membrane emulsification-based double emulsion method. Table 3 shows the compositions of the different water and organic phases used for the preparation of the different formulations.
Polymers A and B at different weight ratios (Table 4) were dissolved in dichloromethane (DCM) to yield a 10–20 wt % solution (see Table 3). Lyophilized carrier-free VEGF was reconstituted in 5 mM succinate buffer pH 5 (see Table 3 for concentrations), added to the polymer solution (final VEGF target loading 0.2 or 1.0 wt % versus total mass of polymer/ratio 1:10 volume w1-phase to volume o-phase) and homogenized for 40 s at 21 600 rpm using an ULTRA-TURRAX mixer (T25 Basic, IKA, Wilmington, USA). The obtained primary emulsion was subsequently pressed through a stainless steel membrane with a pore size of 20 μm (20 μm × 200 μm hydrophilic ringed stainless-steel membrane, Micropore Technologies, Redcar, United Kingdom) into a continuous phase consisting of 0.4 wt % PVA, 5 wt % NaCl or 4 wt % PVA, 5 wt % NaCl. Next, the secondary emulsion was stirred at 200 rpm with a magnetic stirrer for 3 h to evaporate DCM. Subsequently, the particles were washed with 0.05% Tween 80 and water, and were collected on a 5 μm filter before lyophilization overnight. After freeze-drying, microspheres were stored at −20 °C. Placebo microspheres were prepared by single emulsion, that is, pressing a 10 wt % polymer solution in DCM (polymer A and B blend ratio 50:50) directly through a stainless steel membrane (as described above, for formulation parameters see Table 3).
Table 4. Polymer A and B Blend Ratios and Calculated PEG Content [%]a.
| weight fraction polymer A | weight fraction polymer B | PEG 1 kDa [wt %] | PEG 3 kDa [wt %] | total PEG [wt %] |
|---|---|---|---|---|
| 100 | 0 | 0.0 | 22.5 | 22.5 |
| 90 | 10 | 2.5 | 20.3 | 22.8 |
| 80 | 20 | 5.0 | 18.0 | 23.0 |
| 70 | 30 | 7.5 | 15.8 | 23.3 |
| 60 | 40 | 10.0 | 13.5 | 23.5 |
| 50 | 50 | 12.5 | 11.3 | 23.8 |
| 0 | 100 | 25.0 | 0.0 | 25.0 |
Blend ratio 50:50 was selected for preparation of placebo microspheres and microspheres with a 1.0 wt % target VEGF loading (in bold).
4.2.3. Characterization of Microspheres
Average size and size distribution of the obtained microspheres were measured with an optical particle sizer (Accusizer 780, Santa Barbara, California, USA for placebo microspheres and 0.2 wt % target loading microspheres; Coulter Counter, Beckman Coulter, Woerden, the Netherlands for 1.0 wt % target loading microspheres). The volume–weight mean microsphere diameter (vol–wt mean) is reported as the particle size. The CV [%] was calculated by dividing the standard deviation (SD) by the mean diameter, according to eq 1.
| 1 |
The morphology of the microspheres was analyzed with SEM (Phenom, FEI Company, The Netherlands or JEOL JCM-5000 NeoScope, JEOL Ltd., Japan). Lyophilized microspheres were transferred onto aluminum specimen stubs using double-sided adhesive tape (Agar Scientific Ltd., England or JEOL Ltd., Japan). Prior to analysis, the microspheres were coated with a thin metal layer using an ion coater under vacuum. The sample was then introduced into the microscope, vacuum was applied and the microspheres were imaged using an electron beam.
VEGF loading and encapsulation efficiency was determined by dissolving 10 mg of microspheres in 0.5 mL of DMSO. The samples were heated at 80 °C until complete dissolution. Subsequently, 2.5 mL of 0.05 M NaOH containing 0.5% SDS was added to each sample, similar to Sah and Ghassemi et al.67,68 The samples were incubated overnight at room temperature for 16 h under gentle agitation. Subsequently, 100 μL of the sample was transferred into a glass tube and analyzed for protein content by the BCA protein assay (Fisher Scientific, The Netherlands). The amount of VEGF per sample was calculated using a calibration curve of VEGF. Known amounts of VEGF in solution were transferred into glass tubes and evaporated to dryness. These tubes were further treated as samples, as described above. Addition of the polymer to the calibration standards did not affect the accuracy of the method (data not shown). VEGF loading is expressed as mg VEGF encapsulated per mg of the solid material in weight percentage (wt %) (eq 2). Loading efficiency was calculated by dividing the actual loading of VEGF by the initial weight % of VEGF versus the total dry weight of added materials % [%] (eq 3).
| 2 |
| 3 |
4.2.4. In Vitro Polymer Degradation
The degradation of placebo microspheres of a 50:50 blend of polymer A and B was studied by suspending 10 mg of accurately weighed freeze-dried microspheres in 1 mL of in vitro release (IVR) buffer (Dulbecco’s PBS pH 7.4 (0.2 μm filtered), 0.025% Tween 20, 0.02% NaN3) in 1.5 mL Eppendorf tubes. The samples were incubated at 37 °C for 7, 14, 21, or 28 days under gentle agitation. At these time points, the samples were centrifuged at 2000g for 5 min. After removal of the supernatant, the microspheres were washed three times with 900 μL reverse osmosis water and subsequently freeze-dried overnight. The weight of freeze-dried microspheres was noted, and the remaining dry mass per time point was calculated with eq 4, essentially as described previously.42,43,69
| 4 |
The remaining PEG content of degraded samples was determined by 1H NMR analysis, as described by Sandker et al. and Ramazani et al.43,691H NMR samples were prepared by dissolving approximately 5 mg of degraded microspheres in 0.6 mL of deuterated chloroform (CDCl3). The spectrum was recorded from 0 to 8 ppm with an Agilent 400 MHz NMR spectrometer (Agilent Technologies, USA) at 298 K. The weight percentage of PEG in degraded polymers was calculated from the methine group of l-lactide at δ 5.4–5.1 and the methylene groups of PEG δ 3.6–3.7. The molar composition of degradation study samples was further studied by adding the shift reagent TAIC to the samples, as described previously by Petit et al. and by De Vos and Goethals.70,71 After the reaction of free hydroxyl-end groups of PEG with TAIC, the methylene group next to the urethane-containing end group shifts around 1 ppm higher, that is ∼δ 4.5, than that of integrated PEG.
GPC was used to analyze the molecular weights of degraded polymers. GPC was carried out on a Waters Alliance system, with a Waters 2695 separating module and a Waters 2414 refractive index detector. Two PL-gel 5 μm mixed-D columns fitted with a guard column (Polymer Labs, Mw range 0.2–400 kg/mol) were used. The mobile phase consisted of DMF supplemented with 10 mM LiCl and calibration was done with PEG standards.
4.2.5. In Vitro Release Studies
Release studies with VEGF-loaded microspheres were performed at 37 °C. In vitro release buffer (“IVR buffer”) consisted of Dulbecco’s PBS pH 7.4 (0.2 μm filtered), 0.025% Tween 20, and 0.02% NaN3. Accurately weighed samples of 10 mg of lyophilized microspheres were transferred into 1.5 mL Eppendorf tubes and suspended in 900 μL of IVR buffer. The samples were incubated at 37 °C under gentle agitation in a rotating shaker. At predetermined time points, the samples were centrifuged at 2000g for 5 min and 800 μL of the supernatant was removed and replaced by fresh IVR buffer. The samples were stored at 4 °C until the analysis of VEGF content by SE-UPLC and ELISA as described below.
Similarly performed release studies from microspheres stored at −20 °C for several months (and exposed to several freezing cycles) were conducted in sterilized release buffer (“bioactivity IVR buffer”) that did not contain sodium azide and Tween 20. This buffer consisted of Dulbecco’s PBS pH 7.4, 0.2 μm filtered (as stated above), 0.5% BSA, 30 μg/mL gentamicin, and 15 ng/mL amphotericin. VEGF concentrations in the collected supernatants were measured by ELISA (see Section 4.2.5.2). The bioactivity of released VEGF was determined by the endothelial cell proliferation assay. Details of these procedures are given in Section 4.2.7.
To obtain more information on the mechanism of release, the release data obtained from SE-UPLC and ELISA analysis were fitted using the Korsmeyer–Peppas model, where Qt is the amount of drug released from microspheres at time point t, Q0 is the initial amount of drug in microspheres, n is the diffusional exponent indicative of the transport mechanism, and Kp is the Korsmeyer–Peppas constant incorporating structural and geometric characteristics of the dosage form (eq 5).58 The diffusional exponent n was calculated from the fitted linear regression lines of log (% drug released) versus log (time) (eq 6).
| 5 |
| 6 |
4.2.5.1. VEGF Analysis by SE-UPLC
The samples were analyzed without dilution using SE-UPLC on a Waters Acquity H-class UPLC system (Waters, Milford, USA) with a FLR-detector, operated at λex: 276 nm, λem: 310 nm. The system was equipped with a Waters Acquity UPLC Protein BEH SEC column (150 mm × 4.6 mm; 1.7 μm) maintained at 25 °C. The mobile phase consisted of a 50 mM phosphate, 0.4 M perchlorate buffer pH 6.3/acetonitrile (90:10, v/v), and was operated at a flow rate of 0.30 mL/min. Sample aliquots of 10 μL were automatically injected. The VEGF retention time under these conditions was 4.5 min. The linear range of the VEGF calibration curve was 2 μg/mL (detection limit)–200 μg/mL VEGF.
4.2.5.2. VEGF Analysis by ELISA
In vitro release samples were analyzed by a sandwich ELISA (Human VEGF DuoSet ELISA, R&D Systems, Abingdon, United Kingdom) according to the manufacturer’s protocol. The VEGF stock solution of the ELISA kit was used for calibration in the concentration range of 31–2000 pg/mL. Release samples were diluted with the reagent diluent to fall within the working range of the assay and measured in duplicate. ELISA plates were read at 450 nm using a SPECTROstar Nano plate reader (BMG Labtech, Ortenberg, Germany).
4.2.5.3. Comparison VEGF Detection by ELISA and SE-UPLC
VEGF detection by ELISA and SE-UPLC was compared by quantifying fresh, nonformulated VEGF in solution with defined concentrations. A 1 mg/mL VEGF solution in IVR buffer was prepared by reconstituting 1 mg of freeze-dried VEGF, as received by PeproTech, in 1 mL of IVR buffer (Dulbecco’s PBS pH 7.4 (0.2 μm filtered), 0.025% Tween 20, 0.02% NaN3, see Section 4.2.5). This solution was diluted further in IVR buffer to VEGF solutions of 6, 60, and 160 μg/mL. VEGF was quantified by ELISA and SE-UPLC. Similarly, the IVR samples from microspheres (as described in Section 4.2.5) were spiked with 50 μg/mL of fresh, nonformulated VEGF in IVR buffer. The samples were measured by SE-UPLC and ELISA.
4.2.6. Storage Stability: Reproducibility of Release Profiles
4.2.6.1. Stability after Repeated Freezing and Storage at −20 °C
To study the effect of repeated storage at −20 °C on the in vitro release profile, 90 mg of freshly prepared freeze-dried microspheres (as described in Section 4.2.2, 1.0 wt % target VEGF loading) were accurately weighed, transferred into a 1.5 mL Eppendorf tube, and stored at −20 °C for a minimum of 16 h. Next, the microsphere sample was taken out of the freezer and incubated at room temperature for at least 3 h. A 10 mg microsphere sample was removed and subjected to an in vitro release study, as described in Sections 4.2.5 and 4.2.5.1 (release measured by SE-UPLC). The remaining microsphere sample was placed back into the −20 °C freezer. This procedure was repeated five times. VEGF release profiles, obtained after repeated freezing to and storage at −20 °C, were compared to the release profiles from freshly prepared microspheres (t = 0).
4.2.6.2. Long-Term Storage Stability at −20 °C
The stability of VEGF-loaded microspheres was assessed for storage durations of 1, 2, 3, 6, and 9 months at −20 °C. In detail, 90 mg of freeze-dried VEGF-loaded microsphere samples (prepared as described in Section 4.2.2, 1.0 wt % target VEGF loading) were accurately weighed, transferred into a 1.5 mL Eppendorf tube, and stored at −20 °C. After the indicated storage period, the samples were removed from the freezer and were incubated at room temperature for at least 3 h. Afterwards, the microsphere samples were subjected to an in vitro release study, as described in Sections 4.2.5 and 4.2.5.1 (release measured by SE-UPLC). The release profiles (obtained after various storage duration at −20 °C) were compared to the release profile of freshly prepared freeze-dried microspheres (t = 0).
4.2.6.3. Similarity Factor f2
The SE-UPLC release curves of microspheres after storage at −20 °C (Sections 4.2.6.1 and 4.2.6.2) were compared by calculation of the similarity factor f2. The differences of the amount of drug released from a reference batch (R) and from a test batch (T) at time point t are further transformed according to eq 7. Two release curves are regarded to be similar when f2 is between 50 and 100, whereby a f2 value of 50 represents a 10% difference and 100 represents fully equal release curves. Two release curves are regarded different if f2 < 50.57,65
| 7 |
4.2.7. Bioactivity of VEGF
The bioactivity of released VEGF was determined using an in-house developed Alamar Blue proliferation assay with HUVEC.72−74 HUVECs (Lonza, Switzerland) were cultured until passage 2–5 in the EBM-2 complete medium (Lonza CC-3162) supplemented with a growth factor bullet kit. Actual proliferation assays were performed in a growth-factor poor medium (bioactivity medium). Addition of VEGF to the medium was able to enhance proliferation approximately 3.5-fold. VEGF standards (10–100 ng/mL) were prepared in the M199 medium supplemented with 2.5% fetal bovine serum (bioactivity medium). Release samples were collected at different time points (1, 7, 14, 21, and 28 days) and diluted 500 times in order to fall within the (linear) proliferation range for nonformulated VEGF (10–100 ng/mL). Prior to the experiment, 96-well plates (Greiner Bio-One, The Netherlands) were coated overnight at 4 °C with 100 μL of coating solution consisting of 50 μg/mL collagen I, rat tail (Corning 354236, USA) in 20 mM acidic acid. On the day of the experiment, the plates were washed twice with PBS before seeding of the cells. Subsequently, the wells were filled with 100 μL of the sample or VEGF standard and 4000 cells suspended in 100 μL of the bioactivity medium (making a total of 200 μL per well). Wells without cells and filled with 200 μL of the bioactivity medium served as controls. The cells were incubated at 37 °C/5% CO2 for 92 h, after which 20 μL of the Alamar Blue reagent was added to the wells. The plates were incubated for another 4 h, before measuring the fluorescence (λex 530 nm and λem 600 nm) with a microplate reader (Berthold Mithras LB 940, Germany). The results are expressed as relative cell proliferation, which is the proliferation in % normalized by the proliferation of cells that were incubated without VEGF.
4.2.8. Statistical Analysis
Data are presented as average with SD. Statistical analysis was performed with GraphPad Prism7 using the one-way analysis of variance (ANOVA) and Tukeys multicomparison test. Differences between the analyzed groups were considered significant if p < 0.05.
Acknowledgments
This research is funded by European Union’s Horizon 2020 research and innovation program under grant agreement number 645991 (DRIVE). The authors thank Christine Hiemstra, Prachi Desai, and Sjaak Jong for their contribution to this work. Yan Wang is greatly acknowledged for the GPC analysis, as well as Mies van Steenbergen for 1H NMR analysis.
Glossary
Abbreviations
- VEGF
vascular endothelial growth factor
- HUVEC
human umbilical vein endothelial cells
- PLGA
poly-lactic-co-glycolic acid
- SE-UPLC
size exclusion ultra-performance liquid chromatography
- ELISA
enzyme-linked immunosorbent assay
- PEG
polyethylene glycol
- DCM
dichloromethane
- PCL
polycaprolactone
- PLLA
poly-l-lactic acid
- FBS
fetal bovine serum
- SDS
sodium dodecyl sulfate
- GPC
gas permeation chromatography
- 1H NMR
proton-nuclear magnetic resonance
- TAIC
trichloroacetylisocyanate
- HSA
human serum albumin
- IVR
in vitro release
Supporting Information Available
The Supporting Information is available free of charge on the ACS Publications website at DOI: 10.1021/acsomega.9b01272.
Polymer composition by 1H NMR and GPC analysis, microsphere characterization (SEM and size distribution measurements), release data, and SE-UPLC chromatogram (PDF)
The authors declare no competing financial interest.
Supplementary Material
References
- Langer R.; Vacanti J. Tissue engineering. Science 1993, 260, 920–926. 10.1126/science.8493529. [DOI] [PubMed] [Google Scholar]
- Khademhosseini A.; Langer R. A decade of progress in tissue engineering. Nat. Protoc. 2016, 11, 1775–1781. 10.1038/nprot.2016.123. [DOI] [PubMed] [Google Scholar]
- Berthiaume F.; Maguire T. J.; Yarmush M. L. Tissue engineering and regenerative medicine: history, progress, and challenges. Annu. Rev. Chem. Biomol. Eng. 2011, 2, 403–430. 10.1146/annurev-chembioeng-061010-114257. [DOI] [PubMed] [Google Scholar]
- Crapo P. M.; Gilbert T. W.; Badylak S. F. An overview of tissue and whole organ decellularization processes. Biomaterials 2011, 32, 3233–3243. 10.1016/j.biomaterials.2011.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stratton S.; Shelke N. B.; Hoshino K.; Rudraiah S.; Kumbar S. G. Bioactive polymeric scaffolds for tissue engineering. Bioact. Mater. 2016, 1, 93–108. 10.1016/j.bioactmat.2016.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ovsianikov A.; Khademhosseini A.; Mironov V. The synergy of scaffold-based and scaffold-free tissue tngineering strategies. Trends Biotechnol. 2018, 36, 348–357. 10.1016/j.tibtech.2018.01.005. [DOI] [PubMed] [Google Scholar]
- Llames S.; García E.; Otero Hernández J.; Meana Á. Tissue bioengineering and artificial organs. Adv. Exp. Med. Biol. 2012, 741, 314–336. 10.1007/978-1-4614-2098-9_20. [DOI] [PubMed] [Google Scholar]
- Novosel E. C.; Kleinhans C.; Kluger P. J. Vascularization is the key challenge in tissue engineering. Adv. Drug Deliv. Rev. 2011, 63, 300–311. 10.1016/j.addr.2011.03.004. [DOI] [PubMed] [Google Scholar]
- Fu J.; Wang D.-A. In situ organ-specific vascularization in tissue engineering. Trends Biotechnol. 2018, 36, 834–849. 10.1016/j.tibtech.2018.02.012. [DOI] [PubMed] [Google Scholar]
- Rouwkema J.; Rivron N. C.; van Blitterswijk C. A. Vascularization in tissue engineering. Trends Biotechnol. 2008, 26, 434–441. 10.1016/j.tibtech.2008.04.009. [DOI] [PubMed] [Google Scholar]
- Ylä-Herttuala S.; Rissanen T. T.; Vajanto I.; Hartikainen J. Vascular endothelial growth factors: biology and current status of clinical applications in cardiovascular medicine. J. Am. Coll. Cardiol. 2007, 49, 1015–1026. 10.1016/j.jacc.2006.09.053. [DOI] [PubMed] [Google Scholar]
- Cao L.; Mooney D. Spatiotemporal control over growth factor signaling for therapeutic neovascularization. Adv. Drug Deliv. Rev. 2007, 59, 1340–1350. 10.1016/j.addr.2007.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva E. A.; Mooney D. J. Effects of VEGF temporal and spatial presentation on angiogenesis. Biomaterials 2010, 31, 1235–1241. 10.1016/j.biomaterials.2009.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies N.; Dobner S.; Bezuidenhout D.; Schmidt C.; Beck M.; Zisch A. H.; Zilla P. The dosage dependence of VEGF stimulation on scaffold neovascularisation. Biomaterials 2008, 29, 3531–3538. 10.1016/j.biomaterials.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Said S. S.; Pickering J. G.; Mequanint K. Advances in growth factor delivery for therapeutic angiogenesis. J. Vasc. Res. 2013, 50, 35–51. 10.1159/000345108. [DOI] [PubMed] [Google Scholar]
- Lee K.; Silva E. A.; Mooney D. J. Growth factor delivery-based tissue engineering: general approaches and a review of recent developments. J. R. Soc. Interface 2011, 8, 153–170. 10.1098/rsif.2010.0223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelps E. A.; Templeman K. L.; Thulé P. M.; García A. J. Engineered VEGF-releasing PEG-MAL hydrogel for pancreatic islet vascularization. Drug Delivery Transl. Res. 2015, 5, 125–136. 10.1007/s13346-013-0142-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babasola I. O.; Rooney M.; Amsden B. G. Corelease of bioactive VEGF and HGF from viscous liquid poly(5-ethylene ketal epsilon-caprolactone-co-D,L-lactide). Mol. Pharm. 2013, 10, 4552–4559. 10.1021/mp400361m. [DOI] [PubMed] [Google Scholar]
- Cleland J. L.; Duenas E. T.; Park A.; Daugherty A.; Kahn J.; Kowalski J.; Cuthbertson A. Development of poly-(D,L-lactide--coglycolide) microsphere formulations containing recombinant human vascular endothelial growth factor to promote local angiogenesis. J. Control. Release 2001, 72, 13–24. 10.1016/s0168-3659(01)00258-9. [DOI] [PubMed] [Google Scholar]
- Freiberg S.; Zhu X. X. Polymer microspheres for controlled drug release. Int. J. Pharm. 2004, 282, 1–18. 10.1016/j.ijpharm.2004.04.013. [DOI] [PubMed] [Google Scholar]
- Ma G. Microencapsulation of protein drugs for drug delivery: strategy, preparation, and applications. J. Control. Release 2014, 193, 324–340. 10.1016/j.jconrel.2014.09.003. [DOI] [PubMed] [Google Scholar]
- Prajapati V. D.; Jani G. K.; Kapadia J. R. Current knowledge on biodegradable microspheres in drug delivery. Expert Opin. Drug Deliv. 2015, 12, 1283–1299. 10.1517/17425247.2015.1015985. [DOI] [PubMed] [Google Scholar]
- van de Weert M.; Hennink W. E.; Jiskoot W. Protein instability in poly(lactic-co-glycolic acid) microparticles. Pharm. Res. 2000, 17, 1159–1167. 10.1023/a:1026498209874. [DOI] [PubMed] [Google Scholar]
- Schwendeman S. P. Recent advances in the stabilization of proteins encapsulated in injectable PLGA delivery systems. Crit. Rev. Ther. Drug Carrier Syst. 2002, 19, 73–98. 10.1615/critrevtherdrugcarriersyst.v19.i1.20. [DOI] [PubMed] [Google Scholar]
- Giteau A.; Venier-Julienne M. C.; Aubert-Pouëssel A.; Benoit J. P. How to achieve sustained and complete protein release from PLGA-based microparticles?. Int. J. Pharm. 2008, 350, 14–26. 10.1016/j.ijpharm.2007.11.012. [DOI] [PubMed] [Google Scholar]
- Zhang Y.; Wischke C.; Mittal S.; Mitra A.; Schwendeman S. P. Design of controlled release PLGA microspheres for hydrophobic fenretinide. Mol. Pharm. 2016, 13, 2622–2630. 10.1021/acs.molpharmaceut.5b00961. [DOI] [PubMed] [Google Scholar]
- Wu D.; Wang C.; Yang J.; Wang H.; Han H.; Zhang A.; Yang Y.; Li Q. Improving the Intracellular Drug Concentration in Lung Cancer Treatment through the Codelivery of Doxorubicin and miR-519c Mediated by Porous PLGA Microparticle. Mol. Pharm. 2016, 13, 3925–3933. 10.1021/acs.molpharmaceut.6b00702. [DOI] [PubMed] [Google Scholar]
- Rui J.; Dadsetan M.; Runge M. B.; Spinner R. J.; Yaszemski M. J.; Windebank A. J.; Wang H. Controlled release of vascular endothelial growth factor using poly-lactic-co-glycolic acid microspheres: in vitro characterization and application in polycaprolactone fumarate nerve conduits. Acta Biomater. 2012, 8, 511–518. 10.1016/j.actbio.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simón-Yarza T.; Tamayo E.; Benavides C.; Lana H.; Formiga F. R.; Grama C. N.; Ortiz-de-Solorzano C.; Kumar M. N. V. R.; Prosper F.; Blanco-Prieto M. J. Functional benefits of PLGA particulates carrying VEGF and CoQ10 in an animal of myocardial ischemia. Int. J. Pharm. 2013, 454, 784–790. 10.1016/j.ijpharm.2013.04.015. [DOI] [PubMed] [Google Scholar]
- Simón-Yarza T.; Formiga F. R.; Tamayo E.; Pelacho B.; Prosper F.; Blanco-Prieto M. J. PEGylated-PLGA microparticles containing VEGF for long term drug delivery. Int. J. Pharm. 2013, 440, 13–18. 10.1016/j.ijpharm.2012.07.006. [DOI] [PubMed] [Google Scholar]
- Amsden B. G.; Timbart L.; Marecak D.; Chapanian R.; Tse M. Y.; Pang S. C. VEGF-induced angiogenesis following localized delivery via injectable, low viscosity poly(trimethylene carbonate). J. Control. Release 2010, 145, 109–115. 10.1016/j.jconrel.2010.03.029. [DOI] [PubMed] [Google Scholar]
- Allison S. D. Analysis of initial burst in PLGA microparticles. Expert Opin. Drug Deliv. 2008, 5, 615–628. 10.1517/17425247.5.6.615. [DOI] [PubMed] [Google Scholar]
- Fredenberg S.; Wahlgren M.; Reslow M.; Axelsson A. The mechanisms of drug release in poly(lactic-co-glycolic acid)-based drug delivery systems--a review. Int. J. Pharm. 2011, 415, 34–52. 10.1016/j.ijpharm.2011.05.049. [DOI] [PubMed] [Google Scholar]
- Fu K.; Pack D. W.; Klibanov A. M.; Langer R. Visual evidence of acidic environment within degrading poly(lactic-co-glycolic acid) (PLGA) microspheres. Pharm. Res. 2000, 17, 100–106. 10.1023/a:1007582911958. [DOI] [PubMed] [Google Scholar]
- Shenderova A.; Burke T. G.; Schwendeman S. P. The acidic microclimate in poly(lactide-co-glycolide) microspheres stabilizes camptothecins. Pharm. Res. 1999, 16, 241–248. 10.1023/a:1018876308346. [DOI] [PubMed] [Google Scholar]
- Giteau A.; Venierjulienne M.; Marchal S.; Courthaudon J.; Sergent M.; Monteromenei C.; Verdier J.; Benoit J. Reversible protein precipitation to ensure stability during encapsulation within PLGA microspheres. Eur. J. Pharm. Biopharm. 2008, 70, 127–136. 10.1016/j.ejpb.2008.03.006. [DOI] [PubMed] [Google Scholar]
- Kazazi-Hyseni F.; Landin M.; Lathuile A.; Veldhuis G. J.; Rahimian S.; Hennink W. E.; Kok R. J.; van Nostrum C. F. Computer modeling assisted design of monodisperse PLGA microspheres with controlled porosity affords zero order release of an encapsulated macromolecule for 3 months. Pharm. Res. 2014, 31, 2844–2856. 10.1007/s11095-014-1381-8. [DOI] [PubMed] [Google Scholar]
- Kissel T.; Li Y.; Unger F. ABA-triblock copolymers from biodegradable polyester A-blocks and hydrophilic poly(ethylene oxide) B-blocks as a candidate for in situ forming hydrogel delivery systems for proteins. Adv. Drug Deliv. Rev. 2002, 54, 99–134. 10.1016/s0169-409x(01)00244-7. [DOI] [PubMed] [Google Scholar]
- Bonacucina G.; Cespi M.; Mencarelli G.; Giorgioni G.; Palmieri G. F. Thermosensitive self-assembling block copolymers as drug delivery systems. Polymers 2011, 3, 779–811. 10.3390/polym3020779. [DOI] [Google Scholar]
- Stanković M.; de Waard H.; Steendam R.; Hiemstra C.; Zuidema J.; Frijlink H. W.; Hinrichs W. L. Low temperature extruded implants based on novel hydrophilic multiblock copolymer for long-term protein delivery. Eur. J. Pharm. Sci. 2013, 49, 578–587. 10.1016/j.ejps.2013.05.011. [DOI] [PubMed] [Google Scholar]
- Stanković M.; Hiemstra C.; de Waard H.; Zuidema J.; Steendam R.; Frijlink H. W.; Hinrichs W. L. Protein release from water-swellable poly(D,L-lactide-PEG)-b-poly(-caprolactone) implants. Int. J. Pharm. 2015, 480, 73–83. 10.1016/j.ijpharm.2015.01.007. [DOI] [PubMed] [Google Scholar]
- Stanković M.; Tomar J.; Hiemstra C.; Steendam R.; Frijlink H. W.; Hinrichs W. L. Tailored protein release from biodegradable poly(epsilon-caprolactone-PEG)-b-poly(epsilon-caprolactone) multiblock-copolymer implants. Eur. J. Pharm. Biopharm. 2014, 87, 329–337. 10.1016/j.ejpb.2014.02.012. [DOI] [PubMed] [Google Scholar]
- Sandker M. J.; Duque L. F.; Redout E. M.; Chan A.; Que I.; Löwik C. W. G. M.; Klijnstra E. C.; Kops N.; Steendam R.; van Weeren R.; Hennink W. E.; Weinans H. Degradation, intra-articular retention and biocompatibility of monospheres composed of [PDLLA-PEG-PDLLA]-b-PLLA multi-block copolymers. Acta Biomater. 2017, 48, 401–414. 10.1016/j.actbio.2016.11.003. [DOI] [PubMed] [Google Scholar]
- Chen W.; Palazzo A.; Hennink W. E.; Kok R. J. Effect of particle size on drug loading and release kinetics of gefitinib-loaded PLGA microspheres. Mol. Pharm. 2017, 14, 459–467. 10.1021/acs.molpharmaceut.6b00896. [DOI] [PubMed] [Google Scholar]
- Berkland C.; King M.; Cox A.; Kim K.; Pack D. W. Precise control of PLG microsphere size provides enhanced control of drug release rate. J. Control. Release 2002, 82, 137–147. 10.1016/s0168-3659(02)00136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vladisavljević G. T. Structured microparticles with tailored properties produced by membrane emulsification. Adv. Colloid Interface Sci. 2015, 225, 53–87. 10.1016/j.cis.2015.07.013. [DOI] [PubMed] [Google Scholar]
- Tran V.-T.; Benoît J.-P.; Venier-Julienne M.-C. Why and how to prepare biodegradable, monodispersed, polymeric microparticles in the field of pharmacy?. Int. J. Pharm. 2011, 407, 1–11. 10.1016/j.ijpharm.2011.01.027. [DOI] [PubMed] [Google Scholar]
- Teekamp N.; Van Dijk F.; Broesder A.; Evers M.; Zuidema J.; Steendam R.; Post E.; Hillebrands J. L.; Frijlink H. W.; Poelstra K.; Beljaars L.; Olinga P.; Hinrichs W. L. J. Polymeric microspheres for the sustained release of a protein-based drug carrier targeting the PDGFbeta-receptor in the fibrotic kidney. Int. J. Pharm. 2017, 534, 229–236. 10.1016/j.ijpharm.2017.09.072. [DOI] [PubMed] [Google Scholar]
- Samadi N.; van Steenbergen M. J.; van den Dikkenberg J. B.; Vermonden T.; van Nostrum C. F.; Amidi M.; Hennink W. E. Nanoparticles based on a hydrophilic polyester with a sheddable PEG coating for protein delivery. Pharm. Res. 2014, 31, 2593–2604. 10.1007/s11095-014-1355-x. [DOI] [PubMed] [Google Scholar]
- Huang M.-H.; Li S.; Hutmacher D. W.; Schantz J.-T.; Vacanti C. A.; Braud C.; Vert M. Degradation and cell culture studies on block copolymers prepared by ring opening polymerization of epsilon-caprolactone in the presence of poly(ethylene glycol). J. Biomed. Mater. Res., Part A 2004, 69, 417–427. 10.1002/jbm.a.30008. [DOI] [PubMed] [Google Scholar]
- Petit A.; Müller B.; Meijboom R.; Bruin P.; van de Manakker F.; Versluijs-Helder M.; de Leede L. G. J.; Doornbos A.; Landin M.; Hennink W. E.; Vermonden T. Effect of polymer composition on rheological and degradation properties of temperature-responsive gelling systems composed of acyl-capped PCLA-PEG-PCLA. Biomacromolecules 2013, 14, 3172–3182. 10.1021/bm400804w. [DOI] [PubMed] [Google Scholar]
- Zweers M. L. T.; Engbers G. H. M.; Grijpma D. W.; Feijen J. In vitro degradation of nanoparticles prepared from polymers based on DL-lactide, glycolide and poly(ethylene oxide). J. Control. Release 2004, 100, 347–356. 10.1016/j.jconrel.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Ghaderi R.; Sturesson C.; Carlfors J. Effect of preparative parameters on the characteristics ofpoly (D, L-lactide-co-glycolide) microspheres made by the double emulsion method. Int. J. Pharm. 1996, 141, 205. 10.1016/0378-5173(96)04639-x. [DOI] [Google Scholar]
- Ito F.; Fujimori H.; Honnami H.; Kawakami H.; Kanamura K.; Makino K. Control of drug loading efficiency and drug release behavior in preparation of hydrophilic-drug-containing monodisperse PLGA microspheres. J. Mater. Sci. Mater. Med. 2010, 21, 1563–1571. 10.1007/s10856-010-3995-7. [DOI] [PubMed] [Google Scholar]
- Ito F.; Fujimori H.; Makino K. Incorporation of water-soluble drugs in PLGA microspheres. Colloids Surf., B 2007, 54, 173–178. 10.1016/j.colsurfb.2006.10.019. [DOI] [PubMed] [Google Scholar]
- Liu R.; Huang S.-S.; Wan Y.-H.; Ma G.-H.; Su Z.-G. Preparation of insulin-loaded PLA/PLGA microcapsules by a novel membrane emulsification method and its release in vitro. Colloids Surf., B 2006, 51, 30–38. 10.1016/j.colsurfb.2006.05.014. [DOI] [PubMed] [Google Scholar]
- Costa P.; Sousa Lobo J. M. Modeling and comparison of dissolution profiles. Eur. J. Pharm. Sci. 2001, 13, 123–133. 10.1016/s0928-0987(01)00095-1. [DOI] [PubMed] [Google Scholar]
- Ritger P. L.; Peppas N. A. A simple equation for description of solute release II. Fickian and anomalous release from swellable devices. J. Control. Release 1987, 5, 37–42. 10.1016/0168-3659(87)90035-6. [DOI] [PubMed] [Google Scholar]
- Formiga F. R.; Pelacho B.; Garbayo E.; Abizanda G.; Gavira J. J.; Simon-Yarza T.; Mazo M.; Tamayo E.; Jauquicoa C.; Ortiz-de-Solorzano C.; Prosper F.; Blanco-Prieto M. J. Sustained release of VEGF through PLGA microparticles improves vasculogenesis and tissue remodeling in an acute myocardial ischemia-reperfusion model. J. Control. Release 2010, 147, 30–37. 10.1016/j.jconrel.2010.07.097. [DOI] [PubMed] [Google Scholar]
- Teekamp N.; Duque L. F.; Frijlink H. W.; Hinrichs W. L.; Olinga P. Production methods and stabilization strategies for polymer-based nanoparticles and microparticles for parenteral delivery of peptides and proteins. Expert Opin. Drug Deliv. 2015, 12, 1311–1331. 10.1517/17425247.2015.1003807. [DOI] [PubMed] [Google Scholar]
- Fonte P.; Andrade F.; Azevedo C.; Pinto J.; Seabra V.; van de Weert M.; Reis S.; Sarmento B. Effect of the freezing step in the stability and bioactivity of protein-loaded PLGA nanoparticles upon lyophilization. Pharm. Res. 2016, 33, 2777–2793. 10.1007/s11095-016-2004-3. [DOI] [PubMed] [Google Scholar]
- Fonte P.; Araújo F.; Seabra V.; Reis S.; van de Weert M.; Sarmento B. Co-encapsulation of lyoprotectants improves the stability of protein-loaded PLGA nanoparticles upon lyophilization. Int. J. Pharm. 2015, 496, 850–862. 10.1016/j.ijpharm.2015.10.032. [DOI] [PubMed] [Google Scholar]
- Singh S. K.; Kolhe P.; Mehta A. P.; Chico S. C.; Lary A. L.; Huang M. Frozen state storage instability of a monoclonal antibody: aggregation as a consequence of trehalose crystallization and protein unfolding. Pharm. Res. 2011, 28, 873–885. 10.1007/s11095-010-0343-z. [DOI] [PubMed] [Google Scholar]
- Bhatnagar B. S.; Bogner R. H.; Pikal M. J. Protein stability during freezing: separation of stresses and mechanisms of protein stabilization. Pharm. Dev. Technol. 2007, 12, 505–523. 10.1080/10837450701481157. [DOI] [PubMed] [Google Scholar]
- Shah V. P.; Tsong Y.; Sathe P.; Liu J. P. In vitro dissolution profile comparison--statistics and analysis of the similarity factor, f2. Pharm. Res. 1998, 15, 889–896. 10.1023/a:1011976615750. [DOI] [PubMed] [Google Scholar]
- Borselli C.; Ungaro F.; Oliviero O.; d’Angelo I.; Quaglia F.; La Rotonda M. I.; Netti P. A. Bioactivation of collagen matrices through sustained VEGF release from PLGA microspheres. J. Biomed. Mater. Res., Part A 2010, 92, 94–102. 10.1002/jbm.a.32332. [DOI] [PubMed] [Google Scholar]
- Sah H. A new strategy to determine the actual protein content of poly(lactide-co-glycolide) microspheres. J. Pharm. Sci. 1997, 86, 1315–1318. 10.1021/js960363q. [DOI] [PubMed] [Google Scholar]
- Ghassemi A. H.; van Steenbergen M. J.; Talsma H.; van Nostrum C. F.; Crommelin D. J. A.; Hennink W. E. Hydrophilic polyester microspheres: effect of molecular weight and copolymer composition on release of BSA. Pharm. Res. 2010, 27, 2008–2017. 10.1007/s11095-010-0205-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramazani F.; Hiemstra C.; Steendam R.; Kazazi-Hyseni F.; Van Nostrum C. F.; Storm G.; Kiessling F.; Lammers T.; Hennink W. E.; Kok R. J. Sunitinib microspheres based on [PDLLA-PEG-PDLLA]-b-PLLA multi-block copolymers for ocular drug delivery. Eur. J. Pharm. Biopharm. 2015, 95, 368–377. 10.1016/j.ejpb.2015.02.011. [DOI] [PubMed] [Google Scholar]
- Petit A.; Müller B.; Bruin P.; Meyboom R.; Piest M.; Kroon-Batenburg L. M. J.; de Leede L. G. J.; Hennink W. E.; Vermonden T. Modulating rheological and degradation properties of temperature-responsive gelling systems composed of blends of PCLA-PEG-PCLA triblock copolymers and their fully hexanoyl-capped derivatives. Acta Biomater. 2012, 8, 4260–4267. 10.1016/j.actbio.2012.07.044. [DOI] [PubMed] [Google Scholar]
- De Vos R.; Goethals E. J. End group analysis of commercial poly(ethylene glycol) monomethyl ether’s. Polym. Bull. 1986, 15, 547–549. 10.1007/bf00281766. [DOI] [Google Scholar]
- Stone D.; Phaneuf M.; Sivamurthy N.; LoGerfo F. W.; Quist W. C. A biologically active VEGF construct in vitro: implications for bioengineering-improved prosthetic vascular grafts. J. Biomed. Mater. Res. 2002, 59, 160–165. 10.1002/jbm.1229. [DOI] [PubMed] [Google Scholar]
- O’Brien J.; Wilson I.; Orton T.; Pognan F. Investigation of the Alamar Blue (resazurin) fluorescent dye for the assessment of mammalian cell cytotoxicity. Eur. J. Biochem. 2000, 267, 5421–5426. 10.1046/j.1432-1327.2000.01606.x. [DOI] [PubMed] [Google Scholar]
- Musilli C.; Karam J.-P.; Paccosi S.; Muscari C.; Mugelli A.; Montero-Menei C. N.; Parenti A. Pharmacologically active microcarriers for endothelial progenitor cell support and survival. Eur. J. Pharm. Biopharm. 2012, 81, 609–616. 10.1016/j.ejpb.2012.04.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.