Abstract
Melanoma is a rare malignancy that invades the skin and the mucosa. Research has been conducted on melanoma incidence and the survival of patients with melanoma; however, no studies in melanoma incidence and the survival spanning 40 years and based on a large population have thus far been reported. We obtained data on patients with melanoma for each decade from 1974 to 2013 from the Surveillance, Epidemiology, and End Results (SEER) database. Disparities in survival by decade, age group, gender, race, site, and socioeconomic status (SES) within the aforementioned period were analyzed by comparison of Kaplan-Meier curves. We collected data on 133,996 melanoma patients in 18 SEER registry regions for the period 1974-2013. Our study found that the melanoma incidence increased continuously for the total population as well as for most age groups. The survival of patients with melanoma (except mucosal melanoma) also increased. This study showed increases in incidence and survival in melanoma across four decades in a large sample; meanwhile, the survival rates for mucosal melanoma decreased in the latter three decades, suggesting the need to improve melanoma diagnosis, broaden melanoma awareness among health care providers, and initiate the development of more effective treatments than the existing ones.
Keywords: Melanoma, incidence, relative survival, trends
Introduction
Melanoma, one of malignant skin tumors, ranks fifth as the most common cancer in men and seventh in women. Melanoma incidence has continuously risen worldwide, particularly in people with light complexion [1,2]. Although typically diagnosed in patients aged 50 on the average [3], melanoma can also occur in young adults and children [3]. The incidence of melanoma, particularly mucosal melanoma, in the United States has also increased significantly at a rate faster than that for any other solid tumor in recent years [1]. The survival rates of patients with advanced melanoma remain low; specifically, the 5-year survival rate in patients with stage IV melanoma is ≈6% [4]. Thus, it is not only necessary but also useful to analyze the clinical data of melanoma.
Methods and materials
All data used in the current study were obtained from the SEER program of the National Cancer Institute in the United States. The incidence data on melanoma spanning four decades were obtained for patients from the original nine SEER sites only (the states of Connecticut, Iowa, New Mexico, Utah, and Hawaii and the metropolitan areas of Atlanta, Detroit, San Francisco-Oakland, and Seattle-Puget Sound), whereas the survival data on melanoma were obtained for patients from the original 18 SEER sites (the original 9 sites plus Los Angeles, San Jose-Monterey,
Rural Georgia, the Alaska Native Tumor Registry, Greater California, Kentucky, Louisiana, New Jersey, and Greater Georgia).
Patients with melanoma were analyzed in the SEER registries by the norm, which was set up by the World Health Organization International Classification of Diseases for Oncology. Our research objects were melanoma patients diagnosed from 1974 to 2013, which were selected using ICD-O-3 site codes (C00.0-C14.0, C20-C22, 8C44.0-C44.9, C51-C64) and ICD-O-3 histology codes (8720-8790) [5-8]. The data included melanoma incidence and the relative survival rates (RSRs) of patients. Those diagnosed by autopsy or merely reported as having died from the disease in death certificates were excluded. The socioeconomic status of the area was determined using the county poverty rate [9,10], which is the percentage of persons in the county living below the national poverty threshold in Census 2000 (County attributes 2000s.% Persons below poverty 2000 of low-poverty: 0-999, County attributes 2000s.% Persons below poverty 2000 of medium-poverty: 1000-1999, County attributes 2000s.% Persons below poverty 2000 of high-poverty: 2000-5692, these can be selected in the SEER*Stat software). The patients in the current study were classified by socioeconomic status (SES) (low-poverty, medium-poverty, high-poverty), sex, race (White, Black, and others), and age at diagnosis (0-39, 40-54, 55-69, 70-84, and 85+y).
Data on cancer patient survival were analyzed from the date of diagnosis to the date of death. Period analysis was conducted to calculate the RSRs, which indicated the deaths attributable to melanoma either directly or indirectly. The RSRs were computed as the ratio of the absolute survival rate of melanoma patients divided by the expected survival rate for a group of age-, sex-, and race-matched individuals in the general population. This experiment was designed to identify trends in the clinical outcomes of patients over time. Relative survival point estimates (expressed as percentages), means, and standard errors were computed in the SEER*Stat software in accordance with the standard statistical methodology using the Ederer II method. Kaplan-Meier curves were constructed to estimate the overall survival, and differences between the curves were assessed using the two-tailed logrank test. Stata 12.0 (StataCorp) was used for analysis as well. The difference (p value < 0.01) was considered statistically significant.
Results
Trends in melanoma incidence at the nine original SEER sites over four decades
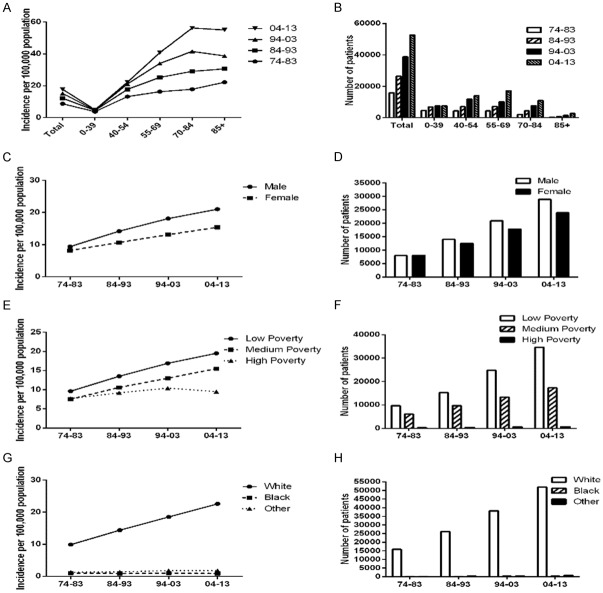
A total of 133,996 patients diagnosed with melanoma between 1974 and 2013 in the SEER program of the National Cancer Institute at the nine original registry sites were collected. As indicated in Figure 1 and Table 1, the melanoma incidence in the four decades continually increased (8.7 per 100,000 from 1974 to 1983, 12.2 per 100,000 from 1984 to 1993, 15.2 per 100,000 from 1994 to 2003, 17.8 per 100,000 from 2004 to 2013). Similar trends were observed in the four decades for almost all age groups (meanwhile, melanoma incidence for the 85+ group decreased from 1994 to 2013). Compared with females, males exhibited a markedly higher melanoma incidence per 100,000 (Figure 1).
Figure 1.
Summary incidences of patients diagnosed with melanoma between 1974 and 2013 at the original nine SEER sites. Incidence and number of melanoma cases are shown by age group (total and ages 0-39, 40-54, 55-69, 70-84 and 85+ years) and calendar period. Incidence (A, C, E, G) and number (B, D, F, H) of melanoma cases are grouped by sex, SES, and race, respectively.
Table 1.
The incidence of melanoma according to age group and decade within sex, SES, and race groups from 1974 to 2013 at the nine original SEER sites. Data are incidence per 100,000 people by year of diagnosis, with the number of patients in parentheses
| Variable | Age Groups | Decade | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| 1974-1983 | 1984-1993 | 1994-2003 | 2004-2013 | |||
| Total | ||||||
| 0-85+ | 8.7 (16032) | 12.2 (26441) | 15.2 (38772) | 17.8 (52751) | ||
| 0-39 | 3.7 (4669) | 4.5 (6898) | 4.7 (7584) | 4.9 (7667) | ||
| 40-54 | 13.2 (4396) | 17.7 (7031) | 21.1 (11818) | 22.2 (14086) | ||
| 55-69 | 16.3 (4375) | 25.3 (7205) | 34 (10226) | 40.8 (17286) | ||
| 70-84 | 17.8 (2156) | 29 (4478) | 41.6 (7701) | 56.3 (10945) | ||
| 85+ | 22.2 (436) | 30.6 (829) | 38.7 (1443) | 55.1 (2767) | ||
| Sex | Male | |||||
| 0-85+ | 9.4 (7983) | 14.2 (13951) | 18.1 (20948) | 21 (28891) | ||
| 0-39 | 3.2 (1988) | 3.8 (2896) | 3.6 (2923) | 3.6 (2784) | ||
| 40-54 | 13.8 (2251) | 19.4 (3772) | 22.6 (6240) | 22 (6935) | ||
| 55-69 | 19.9 (2497) | 33.1 (4420) | 44.8 (6402) | 53.1 (10733) | ||
| 70-84 | 23 (1097) | 40.7 (2524) | 61.2 (4691) | 82.6 (6924) | ||
| 85+ | 25.1 (150) | 44.8 (339) | 63 (692) | 92.4 (1515) | ||
| Female | ||||||
| 0-85+ | 8.2 (8049) | 10.7 (12490) | 13.1 (17824) | 15.4 (23860) | ||
| 0-39 | 4.2 (2681) | 5.1 (4002) | 5.9 (4661) | 6.3 (4883) | ||
| 40-54 | 12.6 (2145) | 16.1 (3259) | 19.7 (5578) | 22.5 (7151) | ||
| 55-69 | 13.2 (1878) | 18.5 (2785) | 24.3 (3824) | 29.6 (6553) | ||
| 70-84 | 14.5 (1059) | 21.2 (1954) | 27.8 (3010) | 36.3 (4021) | ||
| 85+ | 21 (286) | 25.1 (490) | 28.5 (751) | 37.1 (1252) | ||
| Race | White | |||||
| 0-85+ | 9.9 (15788) | 14.4 (26085) | 18.5 (38118) | 22.6 (51889) | ||
| 0-39 | 4.4 (4621) | 5.5 (6817) | 6.1 (7460) | 6.8 (7532) | ||
| 40-54 | 15.3 (4339) | 21.2 (6956) | 26.2 (11647) | 29 (13873) | ||
| 55-69 | 18.4 (4296) | 29.6 (7107) | 41.1 (10050) | 51 (17031) | ||
| 70-84 | 19.4 (2110) | 32.6 (4398) | 48.3 (7566) | 68.1 (10743) | ||
| 85+ | 23.4 (422) | 33.3 (807) | 42.7 (1395) | 63.8 (2710) | ||
| Black | ||||||
| 0-85+ | 1 (119) | 0.9 (146) | 1 (210) | 0.9 (251) | ||
| 0-39 | 0.1 (13) | 0.1 (26) | 0.2 (41) | 0.2 (32) | ||
| 40-54 | 1.1 (31) | 0.7 (27) | 0.8 (48) | 0.7 (56) | ||
| 55-69 | 2.1 (41) | 1.8 (42) | 2.2 (57) | 2.1 (85) | ||
| 70-84 | 3.5 (24) | 4 (40) | 3.4 (44) | 3.9 (59) | ||
| 85+ | 11.2 (10) | 7.2 (11) | 9.1 (20) | 6.2 (19) | ||
| Other | ||||||
| 0-85+ | 1.3 (125) | 1.4 (210) | 1.8 (444) | 1.8 (611) | ||
| 0-39 | 0.4 (35) | 0.4 (55) | 0.5 (83) | 0.5 (103) | ||
| 40-54 | 1.3 (26) | 1.5 (48) | 2.2 (123) | 2 (157) | ||
| 55-69 | 2.7 (38) | 2.6 (56) | 4 (119) | 3.5 (170) | ||
| 70-84 | 4.4 (22) | 4.6 (40) | 5.7 (91) | 6.6 (143) | ||
| 85+ | 5.8 (4) | 8.6 (11) | 11.5 (28) | 8.2 (38) | ||
| SES | Low Poverty | |||||
| 0-85+ | 9.6 (9662) | 13.5 (16216) | 16.9 (24751) | 19.5 (34646) | ||
| 0-39 | 4 (2726) | 4.9 (4109) | 5.3 (4773) | 5.6 (4998) | ||
| 40-54 | 15 (2779) | 19.8 (4448) | 23.4 (7648) | 24.3 (9384) | ||
| 55-69 | 18.3 (2668) | 28.3 (4446) | 38 (6546) | 44.6 (11274) | ||
| 70-84 | 19.1 (1245) | 31.9 (2719) | 45.9 (4887) | 61.5 (7131) | ||
| 85+ | 22.3 (244) | 32.3 (494) | 40.6 (897) | 59.4 (1859) | ||
| Medium Poverty | ||||||
| 0-85+ | 7.5 (6044) | 10.6 (9702) | 13 (13305) | 15.5 (17309) | ||
| 0-39 | 3.4 (1867) | 4 (2663) | 4 (2686) | 4.2 (2608) | ||
| 40-54 | 10.9 (1530) | 15.1 (2464) | 18 (3962) | 19.4 (4527) | ||
| 55-69 | 13.8 (1610) | 21.8 (2624) | 29.1 (3485) | 36.1 (5724) | ||
| 70-84 | 16.2 (860) | 25.1 (1642) | 35.9 (2660) | 49.4 (3592) | ||
| 85+ | 21.2 (177) | 27.5 (309) | 35.5 (512) | 48.2 (858) | ||
| High Poverty | ||||||
| 0-85+ | 7.7 (292) | 9.2 (458) | 10.4 (671) | 9.5 (756) | ||
| 0-39 | 2.3 (68) | 2.9 (107) | 3 (115) | 1.5 (58) | ||
| 40-54 | 11.1 (78) | 11.4 (104) | 14.1 (191) | 10.4 (166) | ||
| 55-69 | 16 (88) | 17.3 (119) | 22.2 (188) | 22.8 (267) | ||
| 70-84 | 19.1 (45) | 30.5 (107) | 31.5 (146) | 37.7 (217) | ||
| 85+ | 39.5 (13) | 39 (21) | 37.3 (31) | 43.9 (48) | ||
Abbreviation: SES, socioeconomic status.
Melanoma incidence by SES and race
The low-poverty group showed a slightly higher melanoma incidence than that of the medium-poverty group, which was higher than that of the high-poverty group. Melanoma incidence per 100,000 in low-and medium-poverty exhibited an increasing trend (from 9.6 to 13.5 to 16.9 to 19.5 in the low-poverty group and from 7.5 to 10.6 to 13.0 to 15.5 in the medium-poverty group). The melanoma incidence in the high-poverty group also increased in the first three decades but decreased in the fourth decade (from 7.7 to 9.2 to 10.4 to 9.5, Table 1; Figure 1E, 1F). As illustrated in Table 1 and Figure 1G, 1H, Whites exhibited a markedly higher melanoma incidence in the four decades, compared with Blacks and other races. In addition, this difference in incidence between Whites and the other groups widened.
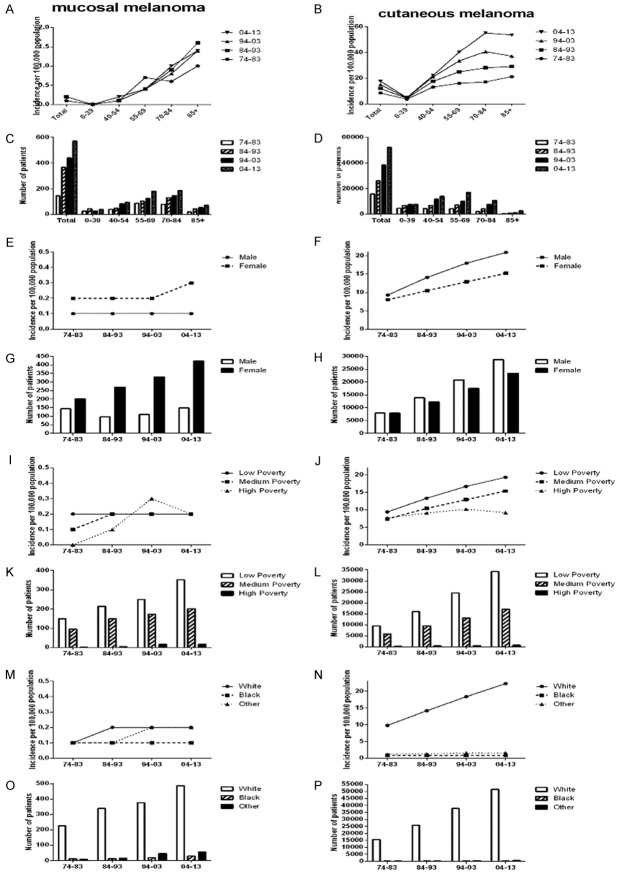
Comparison of the incidence between cutaneous melanoma and mucosal melanoma
The incidence of cutaneous melanoma in males was significantly higher than that in females, whereas the incidence of mucosal melanoma in females was significantly higher than that in males (Figure 2). A considerably large proportion of the incidence of mucosal melanoma was attributed to Whites although the proportion of Blacks and other patients increased significantly (4.4% for mucosal melanoma in Blacks vs. 0.5% for cutaneous melanoma in Blacks; 7.7% for mucosal melanoma in others vs. 0.9% for cutaneous melanoma in others; Tables 2, 3). No apparent differences in SES and age were observed between cutaneous melanoma and mucosal melanoma, and the trends with respect to SES and age were similar for all types of melanoma.
Figure 2.
Summary incidences of patients diagnosed with cutaneous melanoma and mucosal melanoma between 1974 and 2013 at the original nine SEER sites. Incidence and number of two types melanoma cases are shown by age group (total and ages 0-39, 40-54, 55-69, 70-84 and 85+ years) and calendar period. Incidence and number of two types melanoma cases are grouped by sex, SES, and race, respectively (A, C, E, G, I, K, M, O for cutaneous melanoma, while B, D, F, H, J, L, N, P for mucosal melanoma).
Table 2.
The incidence of cutaneous melanoma according to age group and decade within sex, SES, and race groups from 1974 to 2013 at the nine original SEER sites. Data are incidence per 100,000 people by year of diagnosis, with the number of patients in parentheses
| Variable | Age Groups | Decade | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| 1974-1983 | 1984-1993 | 1994-2003 | 2004-2013 | |||
| Total | ||||||
| 0-85+ | 8.5 (15787) | 12 (26074) | 15 (38333) | 17.6 (52180) | ||
| 0-39 | 3.7 (4643) | 4.4 (6854) | 4.7 (7556) | 4.9 (7628) | ||
| 40-54 | 13.1 (4357) | 17.6 (6983) | 21 (11735) | 22.1 (13991) | ||
| 55-69 | 16.1 (4300) | 25 (7103) | 33.6 (10100) | 40.4 (17106) | ||
| 70-84 | 17.1 (2070) | 28.1 (4347) | 40.8 (7553) | 55.3 (10759) | ||
| 85+ | 21.3 (417) | 29.1 (787) | 37.2 (1389) | 53.7 (2696) | ||
| Sex | Male | |||||
| 0-85+ | 9.3 (7940) | 14.1 (13855) | 18 (20838) | 20.9 (28742) | ||
| 0-39 | 3.2 (1986) | 3.8 (2886) | 3.6 (2918) | 3.6 (2773) | ||
| 40-54 | 13.8 (2241) | 19.3 (3756) | 22.5 (6216) | 219 (6901) | ||
| 55-69 | 19.8 (2484) | 32.8 (4385) | 44.6 (6369) | 52.9 (10689) | ||
| 70-84 | 22.7 (1082) | 40.2 (2493) | 60.7 (4653) | 82 (6874) | ||
| 85+ | 24.6 (147) | 44.2 (335) | 62.1 (682) | 91.8 (1505) | ||
| Female | ||||||
| 0-85+ | 8 (7847) | 10.5 (12219) | 12.9 (17495) | 15.2 (23438) | ||
| 0-39 | 4.2 (2657) | 5.1 (3968) | 5.8 (4638) | 6.3 (4855) | ||
| 40-54 | 12.5 (2116) | 16 (3227) | 19.4 (5519) | 22.3 (7090) | ||
| 55-69 | 12.8 (1816) | 18.1 (2718) | 23.7 (3731) | 29 (6417) | ||
| 70-84 | 13.5 (988) | 20.1 (1854) | 26.8 (2900) | 35.1 (3885) | ||
| 85+ | 19.8 (270) | 23.2 (452) | 26.8 (707) | 35.3 (1191) | ||
| Race | White | |||||
| 0-85+ | 9.8 (15562) | 14.2 (25747) | 18.4 (37743) | 22.3 (51403) | ||
| 0-39 | 4.4 (4596) | 5.5 (6774) | 6.1 (7436) | 6.8 (7499) | ||
| 40-54 | 15.2 (4305) | 21.1 (6913) | 26.1 (11579) | 28.9 (13797) | ||
| 55-69 | 18.1 (4227) | 29.2 (7014) | 40.7 (9942) | 50.5 (16878) | ||
| 70-84 | 18.7 (2029) | 31.7 (4279) | 47.5 (7435) | 67.1 (10584) | ||
| 85+ | 22.5 (405) | 31.6 (767) | 41.3 (1351) | 62.3 (2645) | ||
| Black | ||||||
| 0-85+ | 0.9 (108) | 0.8 (133) | 0.9 (191) | 0.8 (222) | ||
| 0-39 | 0.1 (12) | 0.1 (26) | 0.2 (40) | 0.1 (30) | ||
| 40-54 | 1 (29) | 0.7 (24) | 0.7 (44) | 0.6 (49) | ||
| 55-69 | 1.9 (38) | 1.7 (39) | 2 (53) | 1.9 (75) | ||
| 70-84 | 2.9 (20) | 3.5 (35) | 3.1 (40) | 3.4 (51) | ||
| 85+ | 10.1 (9) | 5.9 (9) | 6.4 (14) | 5.5 (17) | ||
| Other | ||||||
| 0-85+ | 1.2 (117) | 1.3 (194) | 1.6 (399) | 1.6 (555) | ||
| 0-39 | 0.4 (35) | 0.4 (54) | 0.4 (80) | 0.4 (99) | ||
| 40-54 | 1.1 (23) | 1.4 (46) | 2 (112) | 1.8 (145) | ||
| 55-69 | 2.5 (35) | 2.3 (50) | 3.6 (105) | 3.2 (153) | ||
| 70-84 | 4.2 (21) | 3.8 (33) | 4.9 (79) | 5.7 (124) | ||
| 85+ | 4.3 (3) | 8.6 (11) | 9.8 (24) | 7.3 (34) | ||
| SES | Low Poverty | |||||
| 0-85+ | 9.4 (9514) | 13.3 (16002) | 16.7 (24501) | 19.3 (34294) | ||
| 0-39 | 4 (2710) | 4.8 (4081) | 5.3 (4756) | 5.5 (4974) | ||
| 40-54 | 14.9 (2757) | 19.7 (4423) | 23.3 (7606) | 24.2 (9318) | ||
| 55-69 | 17.9 (2615) | 27.9 (4387) | 37.5 (6468) | 44.2 (11172) | ||
| 70-84 | 18.4 (1199) | 30.9 (2643) | 45.1 (4804) | 60.6 (7023) | ||
| 85+ | 21.3 (233) | 30.6 (468) | 39.3 (867) | 57.7 (1807) | ||
| Medium Poverty | 1 | |||||
| 0-85+ | 7.4 (5949) | 10.4 (9553) | 12.9 (13132) | 15.4 (17108) | ||
| 0-39 | 3.3 (1857) | 4 (2648) | 4 (2676) | 4.2 (2594) | ||
| 40-54 | 10.7 (1513) | 15 (2441) | 17.9 (3925) | 19.3 (4502) | ||
| 55-69 | 13.6 (1589) | 21.5 (2582) | 28.7 (3440) | 35.6 (5651) | ||
| 70-84 | 15.4 (821) | 24.2 (1588) | 35.1 (2600) | 48.4 (3520) | ||
| 85+ | 20.3 (169) | 26.2 (294) | 34.1 (491) | 47.3 (841) | ||
| High Poverty | ||||||
| 0-85+ | 7.7 (290) | 9.1 (454) | 10.2 (655) | 9.2 (739) | ||
| 0-39 | 2.3 (68) | 2.9 (106) | 3 (114) | 1.5 (57) | ||
| 40-54 | 11.1 (78) | 11.4 (104) | 13.8 (187) | 10.1 (162) | ||
| 55-69 | 15.9 (87) | 17.1 (118) | 21.8 (185) | 22.5 (263) | ||
| 70-84 | 18.7 (44) | 30.2 (106) | 30.4 (141) | 36.7 (211) | ||
| 85+ | 39.5 (13) | 37.1 (20) | 33.7 (28) | 42 (46) | ||
Abbreviation: SES, socioeconomic status.
Table 3.
The incidence of mucosal melanoma according to age group and decade within sex, SES, and race groups from 1974 to 2013 at the nine original SEER sites. Data are incidence per 100,000 people by year of diagnosis, with the number of patients in parentheses
| Variable | Age Groups | Decade | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| 1974-1983 | 1984-1993 | 1994-2003 | 2004-2013 | |||
| Total | ||||||
| 0-85+ | 0.1 (145) | 0.2 (367) | 0.2 (439) | 0.2 (571) | ||
| 0-39 | 0 (26) | 0 (44) | 0 (28) | 0 (39) | ||
| 40-54 | 0.1 (39) | 0.1 (48) | 0.1 (83) | 0.2 (95) | ||
| 55-69 | 0.7 (86) | 0.4 (102) | 0.4 (126) | 0.4 (180) | ||
| 70-84 | 0.6 (78) | 0.9 (131) | 0.8 (148) | 1 (186) | ||
| 85+ | 1 (19) | 1.6 (42) | 1.4 (54) | 1.4 (71) | ||
| Sex | Male | |||||
| 0-85+ | 0.1 (43) | 0.1 (96) | 0.1 (110) | 0.1 (149) | ||
| 0-39 | 0 (2) | 0 (10) | 0 (5) | 0 (11) | ||
| 40-54 | 0.1 (10) | 0.1 (16) | 0.1 (24) | 0.1 (34) | ||
| 55-69 | 0.3 (15) | 0.3 (35) | 0.2 (33) | 0.2 (44) | ||
| 70-84 | 0.2 (11) | 0.5 (31) | 0.5 (38) | 0.6 (50) | ||
| 85+ | 0.5 (3) | 0.5 (4) | 0.9 (10) | 0.6 (10) | ||
| Female | ||||||
| 0-85+ | 0.2 (202) | 0.2 (271) | 0.2 (329) | 0.3 (422) | ||
| 0-39 | 0 (24) | 0 (34) | 0 (23) | 0 (28) | ||
| 40-54 | 0.1 (29) | 0.2 (32) | 0.2 (59) | 0.2 (61) | ||
| 55-69 | 1.0 (71) | 0.4 (67) | 0.6 (93) | 0.6 (136) | ||
| 70-84 | 0.9 (67) | 1.1 (100) | 1 (110) | 1.2 (136) | ||
| 85+ | 1.2 (16) | 1.9 (38) | 1.7 (44) | 1.8 (61) | ||
| Race | White | |||||
| 0-85+ | 0.1 (226) | 0.2 (338) | 0.2 (375) | 0.2 (486) | ||
| 0-39 | 0 (25) | 0 (43) | 0 (24) | 0 (33) | ||
| 40-54 | 0.1 (34) | 0.1 (43) | 0.2 (68) | 0.2 (76) | ||
| 55-69 | 0.8 (81) | 0.4 (93) | 0.4 (108) | 0.5 (153) | ||
| 70-84 | 0.7 (73) | 0.9 (119) | 0.8 (131) | 1 (159) | ||
| 85+ | 0.9 (17) | 1.6 (40) | 1.3 (44) | 1.5 (65) | ||
| Black | ||||||
| 0-85+ | 0.1 (11) | 0.1 (13) | 0.1 (19) | 0.1 (29) | ||
| 0-39 | 0 (1) | 0 (0) | 0 (1) | 0 (2) | ||
| 40-54 | 0.1 (2) | 0.1 (3) | 0.1 (4) | 0.1 (7) | ||
| 55-69 | 0.6 (4) | 0.1 (3) | 0.2 (4) | 0.3 (10) | ||
| 70-84 | 0.6 (4) | 0.5 (5) | 0.3 (4) | 0.6 (8) | ||
| 85+ | 1.1 (1) | 1.3 (2) | 2.7 (6) | 0.7 (2) | ||
| Other | ||||||
| 0-85+ | 0.1 (8) | 0.1 (16) | 0.2 (45) | 0.2 (56) | ||
| 0-39 | 0 (0) | 0 (1) | 0 (3) | 0 (4) | ||
| 40-54 | 0.1 (3) | 0.1 (2) | 0.2 (11) | 0.2 (12) | ||
| 55-69 | 0.2 (1) | 0.3 (6) | 0.5 (14) | 0.4 (17) | ||
| 70-84 | 0.2 (1) | 0.8 (7) | 0.8 (13) | 0.9 (19) | ||
| 85+ | 1.4 (1) | 0 (0) | 1.6 (4) | 0.9 (4) | ||
| SES | Low Poverty | |||||
| 0-85+ | 0.2 (148) | 0.2 (214) | 0.2 (250) | 0.2 (352) | ||
| 0-39 | 0 (16) | 0 (28) | 0 (17) | 0 (24) | ||
| 40-54 | 0.1 (22) | 0.1 (25) | 0.1 (42) | 0.2 (66) | ||
| 55-69 | 0.4 (53) | 0.4 (59) | 0.5 (78) | 0.4 (102) | ||
| 70-84 | 0.7 (46) | 0.9 (76) | 0.8 (83) | 0.9 (108) | ||
| 85+ | 1 (11) | 1.7 (26) | 1.4 (30) | 1.7 (52) | ||
| Medium Poverty | ||||||
| 0-85+ | 0.1 (95) | 0.2 (149) | 0.2 (173) | 0.2 (201) | ||
| 0-39 | 0 (10) | 0 (15) | 0 (10) | 0 (14) | ||
| 40-54 | 0.1 (17) | 0.1 (23) | 0.2 (37) | 0.1 (25) | ||
| 55-69 | 0.2 (21) | 0.3 (42) | 0.4 (45) | 0.5 (73) | ||
| 70-84 | 0.7 (39) | 0.8 (54) | 0.8 (60) | 1 (72) | ||
| 85+ | 1 (8) | 1.3 (15) | 1.5 (21) | 1 (17) | ||
| High Poverty | ||||||
| 0-85+ | 0 (2) | 0.1 (4) | 0.3 (16) | 0.2 (17) | ||
| 0-39 | 0 (0) | 0 (1) | 0 (1) | 0 (1) | ||
| 40-54 | 0 (0) | 0 (0) | 0.3(4) | 0.3 (4) | ||
| 55-69 | 0.2 (1) | 0.2 (1) | 0.4 (3) | 0.4 (4) | ||
| 70-84 | 0.3 (1) | 0.3 (1) | 1.1 (5) | 1 (6) | ||
| 85+ | 0 (0) | 1.9 (1) | 3.6 (3) | 1.8 (2) | ||
Abbreviation: SES, socioeconomic status.
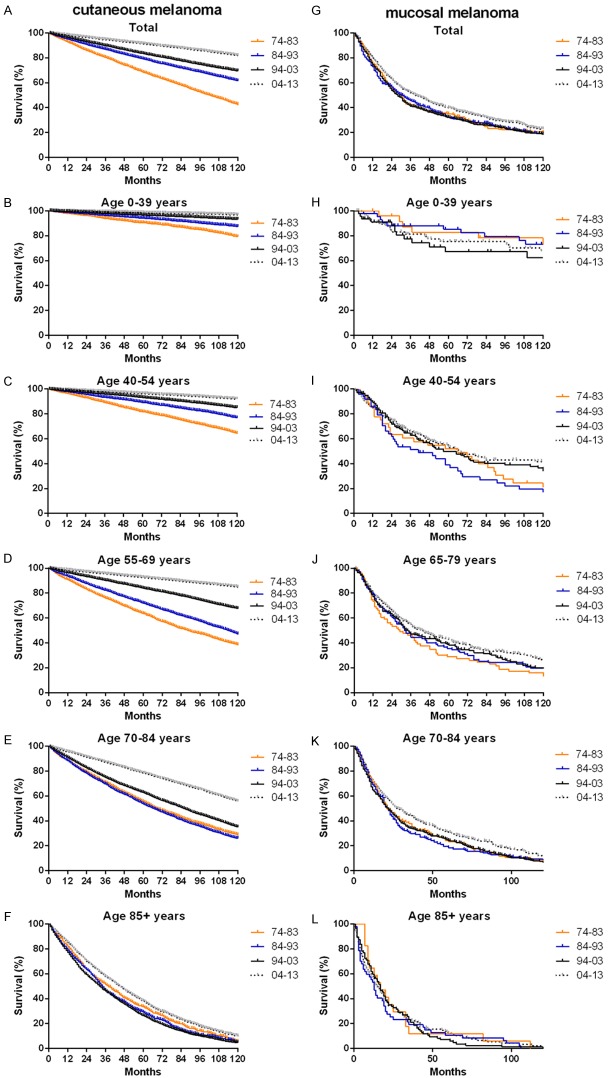
Relative survival estimates for the 18 SEER sites over four decades
The RSRs (Table 4 and Figure 3) and survival times of patients with melanoma across the four decades improved for each age group analyzed. The one-year RSR gradually increased over time (94.40% from 1974 to 1983, 96.30% from 1984 to 1993, 96.90% from 1994 to 2003, and 97.00% from 2004 to 2013; P < 0.0001 for each decade). However, the 1-year survival rate increased very slowly. Kaplan-Meier survival analysis indicated increases in survival time over the four decades for all age groups (Figure 3; Table 4). The 5-year RSR increased from 81.60% to 87.70% to 90.10% to 91.10% over the four decades. The 10-year RSR increased from 76.80% to 84.90% to 87.90% in the first three decades but decreased to 87.80% in the fourth decade.
Table 4.
Relative survival rates of melanoma patients during the periods of 1974-1983, 1984-1993, 1994-2003 and 2004-2013 at eighteen SEER sites. Data are mean ± standard error of the mean, with number of patients in parentheses
| Age Group | Decade | |||
|---|---|---|---|---|
|
| ||||
| 1974-1983 | 1984-1993 | 1994-2003 | 2004-2013 | |
| 12-Mo RS | ||||
| All | 94.40±0.20 (16461) | 96.30±0.10 (28410)*** | 96.90±0.10 (75353)*** | 97.00±0.10 (139017) |
| 0-39 | 96.80±0.30 (4865) | 97.80±0.20 (7433)** | 98.40±0.10 (14096)** | 98.50±0.10 (18894) |
| 40-54 | 95.60±0.30 (4530) | 97.00±0.20 (7663)*** | 97.50±0.10 (22876) | 97.60±0.10 (37066)* |
| 55-69 | 93.40±0.40 (4454) | 95.80±0.30 (7691)*** | 96.70±0.10 (20200)*** | 96.90±0.10 (45926) |
| 70-84 | 89.90±0.80 (2180) | 94.70±0.50 (4743)*** | 95.60±0.20 (15278)* | 96.40±0.20 (30023)* |
| 85+ | 88.20±2.50 (432) | 89.70±1.70 (880)*** | 93.10±0.90 (2903) | 93.50±0.60 (7108) |
| 60-Mo RS | ||||
| All | 81.60±0.40 | 87.70±0.30*** | 90.10±0.20*** | 91.10±0.10*** |
| 0-39 | 86.90±0.50 | 91.30±0.30*** | 94.20±0.20*** | 95.00±0.20** |
| 40-54 | 83.80±0.60 | 89.00±0.40*** | 91.40±0.20*** | 92.70±0.20*** |
| 55-69 | 79.90±0.70 | 86.90±0.50*** | 90.00±0.30*** | 90.90±0.20* |
| 70-84 | 70.80±1.50 | 82.80±1.00*** | 86.40±0.50*** | 88.10±0.40* |
| 85+ | 61.00±5.20 | 71.30±3.30 | 75.60±2.10 | 80.80±1.70 |
| 120-Mo RS | ||||
| All | 76.80±0.40 | 84.90±0.30*** | 87.90±0.20*** | 87.80±0.24 |
| 0-39 | 82.80±0.60 | 88.50±0.40*** | 92.20±0.20*** | 92.55±0.31 |
| 40-54 | 79.10±0.70 | 85.30±0.50*** | 88.90±0.30 | 89.40±0.32 |
| 55-69 | 74.30±0.90 | 85.20±0.60*** | 88.00±0.40*** | 89.00±0.45 |
| 70-84 | 64.60±2.10 | 79.50±1.40*** | 84.20±0.80** | 86.00±1.00 |
| 85+ | 51.50±9.00 | 66.90±7.90 | 68.90±4.40 | 70.00±6.30 |
Abbreviations: Mo, month; RS, relative survival; SEM, standard error of the mean.
P < 0.01 for comparisons with the preceding decade.
P < 0.001 for comparisons with the preceding decade.
P < 0.0001 for comparisons with the preceding decade.
Figure 3.
Trends in 10-year relative survival rates (A, C, E, G, I, K) and Kaplan-Meier survival analysis (B, D, F, H, J, L) for patients with melanoma at eighteen SEER sites in 1974-1983 (orange), 1984-1993 (blue), 1994-2003 (black) and 2004-2013 (gray) respectively according to age group (total and ages 0-39, 40-54, 55-69, 70-84 and 85+ years).
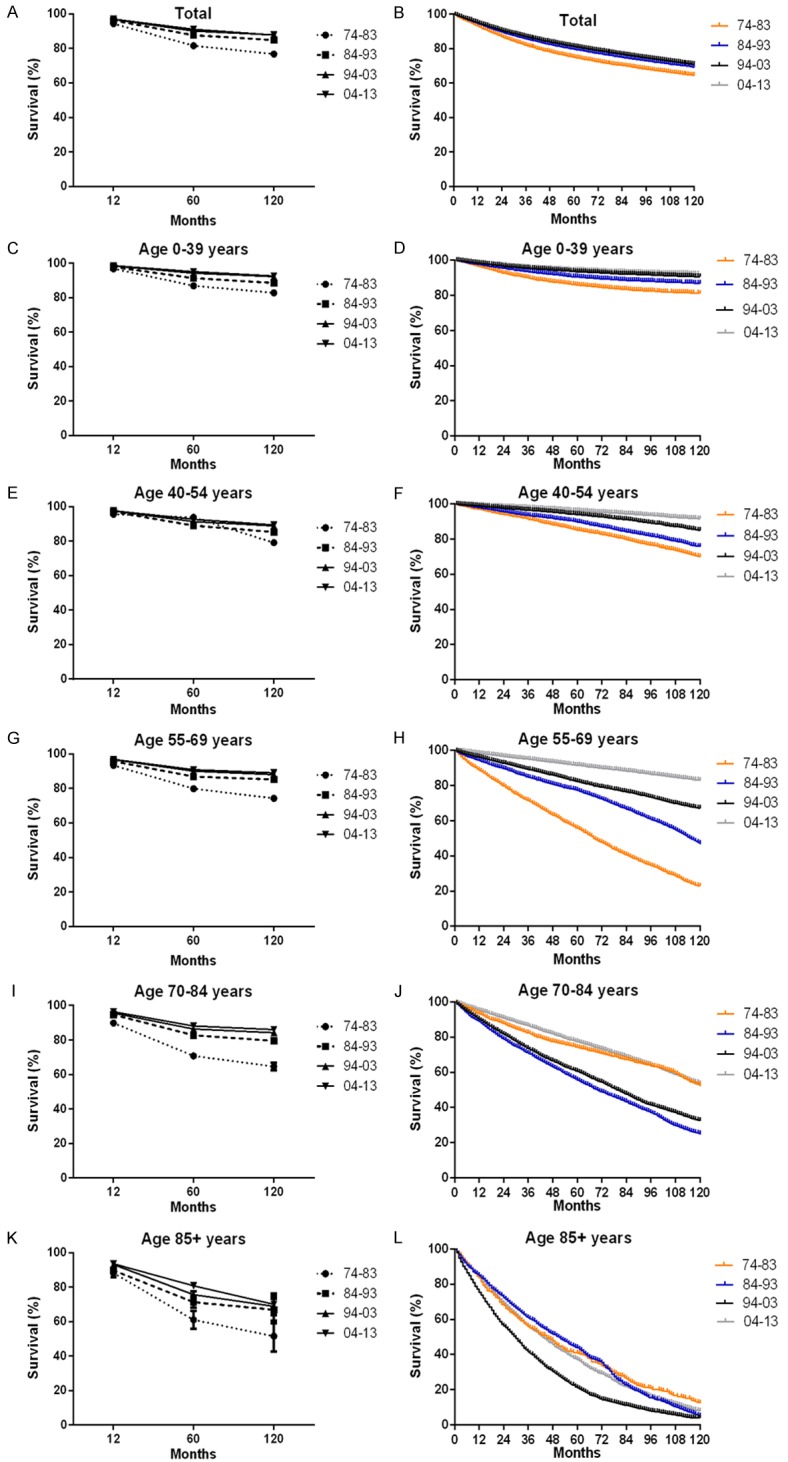
The survival rate in both sexes over the four decades improved (Table 5 and Figure 4A). Females showed a slightly higher 12-month RSR than males (96.00% vs. 92.80%) from 1974 to 1983; in the subsequent three decades, both sexes showed a similar 12-month RSR (97.20% for females vs. 95.50% for males from 1984 to 1993, 97.60% for females vs. 96.40% for males from 1994 to 2003, and 97.70% for females vs. 96.50% for males; Table 5). The same trend was exhibited in the 60-month and 120-month relative survival (Table 6). Kaplan-Meier survival analysis indicated that survival time differed between males and females especially in the 60-month RSR and the 120-month RSR (Figure S1). In some age groups, the difference in survival rate between the sexes was more apparent (Table 5 and Figure 4). For patients aged 0-39 y, the 12-month RSR was significantly higher in females than males in the second decade to the fourth decade (98.2.90% vs. 94.9% from 1974 to 1983, P < 0.001; 98.90% vs. 96.30% from 1984 to 1993, P < 0.0001; 99.00% vs. 97.60% from 1994 to 2003, P < 0.0001; 99.20% vs. 97.50% from 2004 to 2013, P < 0.0001). For patients aged 40-54 y, the 12-month RSR was higher in females than males in each decade (97.50% vs. 93.80% from 1974 to 1983, P < 0.0001; 97.70% vs. 96.50% from 1984 to 1993, P < 0.0001; 98.30% vs. 96.70% from 1994 to 2003, P < 0.0001; 98.60% vs. 96.60% from 2004 to 2013, P < 0.0001). The same tendency was observed in the 55-69 and 70-84 age groups. The differences in survival between males and females were similar for all age groups except the 85+ age group. For patients aged more than 85 y, the survival rates in the last three decades were higher in males than females. Similar disparities in 60-month and 120-month RSRs were found between sexes and age groups (Table 6 and Figure S1).
Table 5.
12-month relative survival rates of melanoma patients according to sex, age group, and calendar period from 1974 to 2013 at eighteen SEER sites. Data are means 6 standard error of the mean, with number of patients in parentheses
| Decade | Age Group | Sex | |
|---|---|---|---|
|
| |||
| Male | Female | ||
| 74-83 | 12-Mo RS | ||
| All | 92.80±0.30 (8198) | 96.00±0.30 (8263)*** | |
| 0-39 | 94.90±0.50 (2074) | 98.20±0.30 (2791)*** | |
| 40-54 | 93.80±0.50 (2316) | 97.50±0.40 (2214)*** | |
| 55-69 | 92.30±0.60 (2553) | 94.80±0.60 (1901)** | |
| 70-84 | 89.90±0.80 (2180) | 89.30±1.20 (1107) | |
| 85+ | 88.20±2.50 (432) | 84.00±4.60 (148) | |
| 84-93 | 12-Mo RS | ||
| All | 95.50±0.20 (15002) | 97.20±0.20 (13408)*** | |
| 0-39 | 96.30±0.30 (3124) | 98.90±0.20 (4309)*** | |
| 40-54 | 96.50±0.30 (4114) | 97.70±0.30 (3549)** | |
| 55-69 | 94.90±0.40 (4733) | 97.30±0.40 (2958)*** | |
| 70-84 | 94.70±0.60 (2669) | 94.60±0.70 (2074) | |
| 85+ | 90.50±2.70 (362) | 89.10±2.10 (518) | |
| 94-03 | 12-Mo RS | ||
| All | 96.40±0.10 (41349) | 97.60±0.10 (34004)*** | |
| 0-39 | 97.60±0.20 (5692) | 99.00±0.10 (8467)*** | |
| 40-54 | 96.70±0.20 (12223) | 98.30±0.10 (10653)*** | |
| 55-69 | 96.60±0.20 (12738) | 96.90±0.20 (7462) | |
| 70-84 | 95.40±0.30 (9324) | 95.90±0.40 (5924) | |
| 85+ | 92.20±1.30 (1435) | 93.90±1.10 (1468) | |
| 04-13 | 12-Mo RS | ||
| All | 96.50±0.10 (77685) | 97.70±0.10 (61332)*** | |
| 0-39 | 97.50±0.20 (7095) | 99.20±0.10 (11799)*** | |
| 40-54 | 96.60±0.10 (18837) | 98.60±0.10 (18229)*** | |
| 55-69 | 96.40±0.10 (28831) | 97.60±0.10 (17095)*** | |
| 70-84 | 96.50±0.20 (18996) | 96.30±0.30 (11027) | |
| 85+ | 95.10±0.80 (3926) | 91.60±0.80 (3182)** | |
Abbreviations: mo, month; RSR, relative survival rate; SEM, standard error of the mean.
P < 0.001 for comparisons with the Male group.
P < 0.0001 for comparisons with the Male group.
Figure 4.
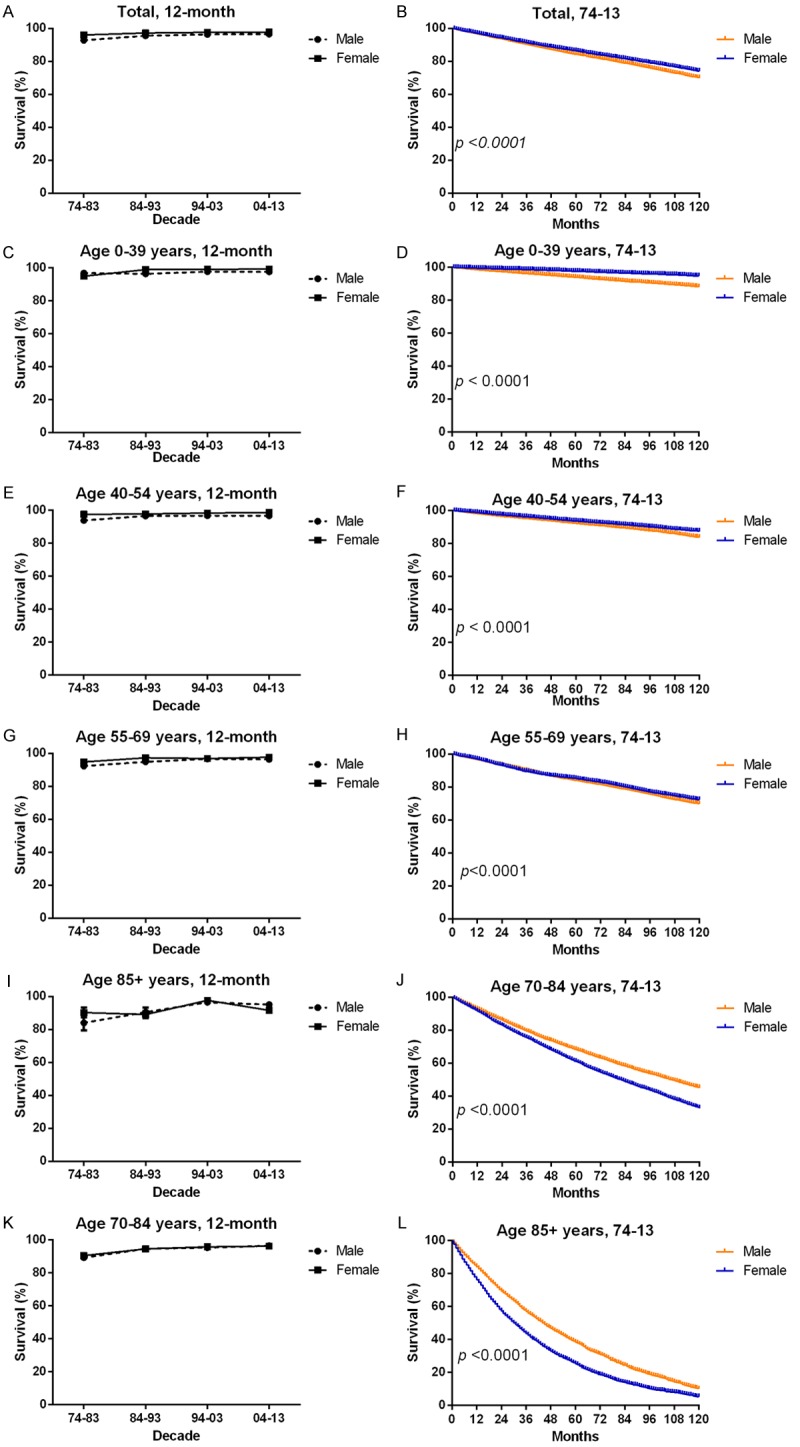
12-month relative survival rates from 1974 to 2013 (A, C, E, G, I, K) and Kaplan-Meier survival analysis from 1974 to 2013 (B, D, F, H, J, L) for male (orange) and female (blue) with melanoma at eighteen SEER sites by age group (total and ages 0-39, 40-54, 55-69, 70-84 and 85+ years).
Table 6.
12-month, 60-month and 120-month relative survival rates of melanoma patients according to sex, age group, and calendar period from 1974 to 2013 at eighteen SEER sites. Data are means ± standard error of the mean, with number of patients in parentheses
| Decade | Age Group | Sex | |
|---|---|---|---|
|
| |||
| Male | Female | ||
| 74-83 | 12-Mo RS | ||
| All | 92.80±0.30 (8198) | 96.00±0.30 (8263)*** | |
| 0-39 | 96.8±0.30 (2704) | 94.9±0.50 (2791) | |
| 40-54 | 93.8±0.50 (2316) | 97.50±0.40 (2214)*** | |
| 55-69 | 92.30±0.60 (2553) | 94.80±0.60 (1901)** | |
| 70-84 | 89.3±1.20 (1107) | 90.5±1.10 (1073) | |
| 85+ | 84.00±4.60 (148) | 90.30±2.90 (284) | |
| 60-Mo RS | |||
| All | 77.30±0.60 | 85.8±0.50*** | |
| 0-39 | 86.90±0.50 | 80.40±0.90*** | |
| 40-54 | 79.50±0.90 | 88.30±0.70*** | |
| 55-69 | 77.3±1.0 | 83.4±1.0*** | |
| 70-84 | 68.80±2.20 | 72.80±1.90 | |
| 85+ | 48.70±9.20 | 66.1±5.1 | |
| 120-Mo RS | |||
| All | 71.9±0.7 | 81.6±0.60*** | |
| 0-39 | 75.10±1.00 | 88.50±0.60*** | |
| 40-54 | 74.5±1.1 | 84.00±0.90*** | |
| 55-69 | 71.2±1.30 | 78.4±1.3*** | |
| 70-84 | 60.8±2.9 | 66.2±2.7 | |
| 85+ | 36.8±16.7 | 55.3±10.7 | |
| 84-93 | 12-Mo RS | ||
| All | 95.50±0.20 (15002) | 97.20±0.20 (13408)*** | |
| 0-39 | 96.30±0.30 (3124) | 98.9±0.2 (4309)*** | |
| 40-54 | 96.50±0.30 (4114) | 97.70±0.30 (3549)** | |
| 55-69 | 94.90±0.40 (4733) | 97.30±0.40 (2958)*** | |
| 70-84 | 94.70±0.60 (2669) | 94.60±0.70 (2074) | |
| 85* | 90.5±2.70 (362) | 89.10±2.10 (518) | |
| 60-Mo RS | |||
| All | 85.10±0.40 | 90.50±0.30*** | |
| 0-39 | 86.80±0.60 | 94.6±0.4*** | |
| 40-54 | 86.20±0.60 | 92.30±0.50*** | |
| 55-69 | 85.1±0.7 | 89.80±0.70*** | |
| 70-84 | 82.60±1.40 | 83.00±1.30 | |
| 85+ | 68.8±5.9 | 72.3±4.1 | |
| 120-Mo RS | |||
| All | 81.90±0.50 | 88.20±0.40*** | |
| 0-39 | 83.00±0.70 | 92.50±0.40*** | |
| 40-54 | 82.00±0.70 | 89.10±0.60*** | |
| 55-69 | 83.5±0.9 | 87.9±0.9** | |
| 70-84 | 79.5±1.4 | 79.2±1.9 | |
| 85+ | 38.4±10.3 | 72.3±4.1*** | |
| 94-03 | 12-Mo RS | ||
| All | 96.40±0.10 (41349) | 97.60±0.10 (34004)*** | |
| 0-39 | 97.60±0.20 (5629) | 99.00±0.10 (8467)*** | |
| 40-54 | 96.70±0.20 (12223) | 98.30±0.10 (10653)*** | |
| 55-69 | 96.60±0.20 (12738) | 96.90±0.20 (7462) | |
| 70-84 | 95.40±0.30 (9324) | 95.90±0.40 (5924) | |
| 85+ | 96.50±0.10 (1435) | 97.70±0.10 (1468)*** | |
| 60-Mo RS | |||
| All | 88.10±0.20 | 92.50±0.20*** | |
| 0-39 | 90.7±0.40 | 96.50±0.20*** | |
| 40-54 | 89.00±0.30 | 94.10±0.30*** | |
| 55-69 | 88.90±0.40 | 91.80±0.40*** | |
| 70-84 | 85.80±0.70 | 87.30±0.80 | |
| 85+ | 89.40±0.20 | 93.20±0.20*** | |
| 120-Mo RS | |||
| All | 85.70±0.30 | 90.60±0.30*** | |
| 0-39 | 87.8±0.5 | 95.20±0.30*** | |
| 40-54 | 86.20±0.40 | 92.10±0.30*** | |
| 55-69 | 87.2±0.5 | 89.4±0.5** | |
| 70-84 | 82.80±1.10 | 85.8±1.1 | |
| 85+ | 70.70±4.60 | 66.30±5.90 | |
| 04-13 | 12-Mo RS | ||
| All | 96.50±0.10 (77685) | 97.70±0.10 (61332)*** | |
| 0-39 | 97.50±0.20 (7095) | 99.20±0.10 (11799)*** | |
| 40-54 | 96.60±0.10 (18837) | 98.60±0.10 (18229)*** | |
| 55-69 | 96.40±0.10 (28831) | 97.60±0.10 (17095)*** | |
| 70-84 | 96.50±0.20 (18996) | 96.30±0.30 (11027) | |
| 85+ | 95.10±0.80 (3926) | 91.60±0.80 (3182)** | |
| 60-Mo RS | |||
| All | 89.40±0.20 | 93.20±0.20*** | |
| 0-39 | 91.80±0.40 | 96.90±0.20*** | |
| 40-54 | 90.30±0.30 | 95.30±0.20*** | |
| 55-69 | 89.50±0.30 | 93.20±0.30*** | |
| 70-84 | 87.70±0.60 | 88.60±0.60 | |
| 85+ | 83.40±2.50 | 77.70±2.40 | |
| 120-Mo RS | |||
| All | 84.90±0.40 | 90.80±0.37*** | |
| 0-39 | 88.10±0.59 | 95.15±0.35*** | |
| 40-54 | 86.40±0.52 | 93.40±0.35*** | |
| 55-69 | 87.80±0.54 | 91.60±0.56*** | |
| 70-84 | 83.00±1.30 | 87.80±0.76** | |
| 85+ | 73.00±8.20 | 62.00±7.50 | |
Abbreviations: Mo, month; RS, relative survival; SEM, standard error of the mean.
P < 0.01;
P < 0.001;
P < 0.0001.
Melanoma survival by SES and race
White patients exhibited a markedly higher 12-month RSR than Black patients for four decades (94.5% vs. 79.5% from 1974 to 1983, 96.40% vs. 86.60% from 1984 to 1993, 96.90% vs. 87.30% from 1994 to 2003, 97.00% vs. 87.90% from 2004 to 2013; P < 0.0001 for each decade; Figure 5B and Table S1). A similar tendency over time was observed in the 60-month and 120-month survival rates (Table S1). The high-poverty group consistently exhibited the lowest 12-, 60-, and 120-month RSRs, whereas the low-poverty group consistently showed the highest survival rates (Figure 5C, Table S2). All SES groups showed improvement in survival rate across the four decades; the three SES groups exhibited markedly larger differences in survival rate in the fourth decade than in the first three decades. Similarly widening gaps in the 60- and 120-month survival rates were found (Table S2). Notably, the distribution of the SES groups differed between races: more White than Black patients were classified as low-poverty individuals (64.1% vs. 35.5%), and more Black than White patients were classified as medium-poverty individuals (64.2% vs. 34.3%; Figure S2; Table S3). The disparity in survival between White and Black patients reflected the difference in survival between the low- and medium-poverty groups. A similar trend was indicated in the Kaplan-Meier survival analysis for the three SES groups over the four decades. Higher poverty was always associated with shorter survival (Figure 5C).
Figure 5.

Relative survival rates according to sex (A, D, G, J), races (C, F, I, L) and according to SES/county-level poverty rates (B, E, H, K) including male (orange), female (blue); White (orange), Black (blue); SES/county-level poverty rates in low-poverty (orange), medium poverty (blue) and high poverty (black) for patients with melanoma at eighteen SEER sites from 1974 to 2013.
Comparison of survival between cutaneous melanoma and mucosal melanoma
Cutaneous melanoma exhibited improved survival over the four decades, whereas mucosal melanoma showed survival rates mainly decreased from 1974 to 2013 (Figure 6, Tables S4, S5). In addition, cutaneous melanoma showed a markedly higher 12-month RSR, compared with mucosal melanoma from 1974 to 2013 (94.70% vs. 75.60% from 1974 to 1983; 96.50% vs. 80.60% from 1984 to 1993; 97.10% vs. 77.30% from 1994 to 2003; 97.20% vs. 74.80% from 2004 to 2013; Tables S4, S5). A similar tendency was found for 60- and 120-month survival rates. Owing to a small number of cases in each age group, the differences in survival data for the two types of melanoma between different age groups are not discussed.
Figure 6.
Trends in Kaplan-Meier survival analysis for patients with two types melanoma at eighteen SEER sites in 1974-1983 (orange), 1984-1993 (blue), 1994-2003 (black) and 2004-2013 (gray) respectively according to age group (total and ages 0-39, 40-54, 55-69, 70-84 and 85+ years; (A-F) for cutaneous melanoma, while (G-L) for mucosal melanoma).
In addition, the medium-poverty group showed higher survival rates in cutaneous melanoma in the four decades, whereas the low-poverty group showed higher survival rates in mucosal melanoma (owing to the considerably small number of patients in the high-poverty group, they were not included in this study; Figures S1, S3). In addition, both types of melanoma showed a similar trend in survival to that of all types of melanoma by sex and race. However, the difference in changes in SES and race was more apparent in mucosal melanoma than in all other types of melanoma (Figure S3).
Discussion
In a word, not only the melanoma incidence but also the RSRs for melanoma increased in each decade from 1974 to 2013. However, no improvement in the survival rate for mucosal melanoma was observed in the latter three decades; and the survival rates were higher in the second decade than in the first decade, indicating the urgent need for the development of effective treatments to improve this situation.
In this study, melanoma incidence per 100,000 was markedly higher in males than in females. Evidence strongly indicates that exposure to ultraviolet radiation from the sun is an important pathogenic factor for malignant melanoma [11]. Compared with females, males exhibited greater exposure to sunlight, which could be the main reason males showed higher incidence than did females. In addition, long hair, which leaves less skin exposed to sunlight, could also slightly affect the lower incidence of cutaneous melanoma in female patients. Meanwhile, the incidence of mucosal melanoma in females is higher than that in males probably because lesions in females are more inclined to arise in the genital tracts [12].
Slightly improving long-term survival in both sexes was observed, with survival in females being superior to that in males. The higher survival in females than males may be attributed to the typical presentation of thinner lesions in females [13-15]. The distribution of the anatomic origin of cutaneous melanomas differs between males and females: females have a higher percentage of extremity melanomas, whereas males have a higher percentage of truncal melanomas. The axial location of melanoma has been associated with worse prognosis [16]. The sex differences revealed in the current study may be related to hormonal effects on the prognosis of melanoma as well.
Compared with Blacks and other races, Whites exhibited markedly higher incidence in either cutaneous or mucosal melanoma during the four decades; this difference may be attributed to the lightness of skin of White. With respect to SES, the low-poverty group showed the highest incidence, whereas the high-poverty group exhibited the lowest incidence; the reason may be that Whites mostly comprise the low-poverty population. Meanwhile, the high survival rate of Whites may be attributed to most Whites being in the low-poverty group, allowing them to be equipped with better medical care and earlier diagnosis of the disease, compared with the other races. Thinner lesions may also be associated with better survival in Whites [12]. With regard to patients with cutaneous melanoma, the medium-poverty group showed the highest survival, which was directly related to income level [12].
The incidence of mucosal melanoma remained low and stable, but the survival rate was decreasing for the latter three decades. Therefore, the etiology and treatment of mucosal melanoma, require close attention. However, risk factors for mucosal melanoma have not been clearly determined. Mucosal melanomas are rare tumors and can be easily misdiagnosed during clinical examination and imaging. Biopsy, histopathological examination, and immunohistochemistry are thus recommended for a conclusive diagnosis. TakagiM et al. reported that oral mucosal melanoma can be behind with oral pigmentation [17]. Pathological changes such as oral pigmentation can be increased by cigarette smoking, which may be related to oral mucosal melanoma [18]. Mucosal melanoma seems to be a particularly aggressive subtype of melanoma. Only 9% of patients with cutaneous melanoma involve regional lymph nodes when diagnosed, whereas in mucosal melanoma, the percentage is considerably higher (21% in head and neck mucosal melanoma, 61% in anorectal mucosal melanoma, and 23% in vulvovaginal mucosal melanoma) [12]. Some patients with mucosal melanoma have been diagnosed with multifocal disease [19]. In addition, a considerable number of patients have been diagnosed with advanced mucosal melanoma [12,20]. Thus, regional lymph node involvement, multifocal disease, failure of early diagnosis, and other unknown factors have been associated with poor survival in patients with mucosal melanoma.
Surgical therapy is widely recognized as the mainstream treatment for mucosal melanoma, apart from radiotherapy of oral melanomas. Numerous therapies that have been proven effective for achieving higher survival rates have emerged. In a clinical trial, patients with stage III melanoma who received PD-1 inhibitor pembrolizumab achieved a 12-month recurrence-free survival rate of 75.4%, whereas the placebo group achieved 61% [21]. BRAF-targeted strategies and PD-1-blocking immunotherapy have also been more effective than currently approved options for patients with high-risk resectable melanoma [22]. In addition, Postow MA et al. found that radiotherapy may reduce the rate of local recurrence of mucosal melanoma, and novel immunotherapeutic agents like agents targeted to the oncogenic pathways of KIT and BRAF exhibited significant advances in the treatment of metastatic disease of mucosal melanoma [20,23].
Thus, analysis of the incidence and survival of melanoma, including mucosal melanoma, in the past four decades indicates changes in the clinical outcomes of melanoma; the need to increase the survival rate of patients with mucosal melanoma is emphasized as well. This study may provide more information on the latest incidence and survival rates related to melanoma, as well as guide the formulation of healthcare acts and clinical management programs to reconcile survival disparities between age groups, sexes, SES groups, and races, thereby improving the clinical management of melanoma. In short, analyzing the incidence and survival of melanoma including mucosal melanoma in the past four decades illustrated us that the changes of clinical outcomes of melanoma, and more importantly highlighted the urgency of improving the survival rate of patients with mucosal melanoma. Furthermore, the study may help us get more acquainted with the latest incidence and survival of melanoma, help make better healthcare acts and clinical management programs to balance the survival disparities between ages, sexes, SES groups, and races demonstrated in this study, and thereupon ameliorate the clinical management of melanoma.
Acknowledgements
This research was funded by the National Natural Science Foundation of China (81872308, 81500030) and the Natural Science Foundation of Guangdong Province (2017A030313573, 2016A030313272, and 2016A030313277).
Disclosure of conflict of interest
None.
Supporting Information
References
- 1.Melanoma research gathers momentum. Lancet (London, England) 2015;385:2323. doi: 10.1016/S0140-6736(15)61087-X. [DOI] [PubMed] [Google Scholar]
- 2.Rastrelli M, Tropea S, Rossi CR, Alaibac M. Melanoma: epidemiology, risk factors, pathogenesis, diagnosis and classification. In Vivo. 2014;28:1005–11. [PubMed] [Google Scholar]
- 3.Situm M, Buljan M, Kolic M, Vucic M. Melanoma-clinical, dermatoscopical, and histopathological morphological characteristics. Acta Dermatovenerol Croat. 2014;22:1–12. [PubMed] [Google Scholar]
- 4.Luke JJ, Ott PA. PD-1 pathway inhibitors: the next generation of immunotherapy for advanced melanoma. Oncotarget. 2015;6:3479–92. doi: 10.18632/oncotarget.2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adams S, Lin J, Brown D, Shriver CD, Zhu K. Ultraviolet radiation exposure and the incidence of oral, pharyngeal and cervical cancer and melanoma: an analysis of the SEER data. Anticancer Res. 2016;36:233–7. [PubMed] [Google Scholar]
- 6.Marcus DM, Marcus RP, Prabhu RS, Owonikoko TK, Lawson DH, Switchenko J, Beitler JJ. Rising incidence of mucosal melanoma of the head and neck in the United States. J Skin Cancer. 2012;2012:231693. doi: 10.1155/2012/231693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scarbrough PM, Akushevich I, Wrensch M, Il’yasova D. Exploring the association between melanoma and glioma risks. Ann Epidemiol. 2014;24:469–74. doi: 10.1016/j.annepidem.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang GB, Barnholtz-Sloan JS, Chen Y, Bordeaux JS. Risk and survival of cutaneous melanoma diagnosed subsequent to a previous cancer. Arch Dermatol. 2011;147:1395–402. doi: 10.1001/archdermatol.2011.1133. [DOI] [PubMed] [Google Scholar]
- 9.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures the public health disparities geocoding project. Am J Public Health. 2003;93:1655–71. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156:471–82. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 11.Koh HK, Kligler BE, Lew RA. Sunlight and cutaneous malignant melanoma: evidence for and against causation. Photochem Photobiol. 1990;51:765–79. [PubMed] [Google Scholar]
- 12.Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer. 1998;83:1664–78. doi: 10.1002/(sici)1097-0142(19981015)83:8<1664::aid-cncr23>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 13.Arce PM, Camilon PR, Stokes WA, Nguyen SA, Lentsch EJ. Is sex an independent prognostic factor in cutaneous head and neck melanoma? Laryngoscope. 2014;124:1363–7. doi: 10.1002/lary.24439. [DOI] [PubMed] [Google Scholar]
- 14.Liu W, Dowling JP, Murray WK, McArthur GA, Thompson JF, Wolfe R, Kelly JW. Rate of growth in melanomas: characteristics and associations of rapidly growing melanomas. Arch Dermatol. 2006;142:1551–8. doi: 10.1001/archderm.142.12.1551. [DOI] [PubMed] [Google Scholar]
- 15.Richard MA, Grob JJ, Avril MF, Delaunay M, Thirion X, Wolkenstein P, Souteyrand P, Dreno B, Bonerandi JJ, Dalac S, Machet L, Guillaume JC, Chevrant-Breton J, Vilmer C, Aubin F, Guillot B, Beylot-Barry M, Lok C, Raison-Peyron N, Chemaly P. Melanoma and tumor thickness: challenges of early diagnosis. Arch Dermatol. 1999;135:269–74. doi: 10.1001/archderm.135.3.269. [DOI] [PubMed] [Google Scholar]
- 16.Balch CM, Karakousis C, Mettlin C, Natarajan N, Donegan WL, Smart CR, Murphy GP. Management of cutaneous melanoma in the United States. Surg Gynecol Obstet. 1984;158:311–8. [PubMed] [Google Scholar]
- 17.Takagi M, Ishikawa G, Mori W. Primary malignant melanoma of the oral cavity in Japan. With special reference to mucosal melanosis. Cancer. 1974;34:358–70. doi: 10.1002/1097-0142(197408)34:2<358::aid-cncr2820340221>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 18.Axell T, Hedin CA. Epidemiologic study of excessive oral melanin pigmentation with special reference to the influence of tobacco habits. Scand J Dent Res. 1982;90:434–42. doi: 10.1111/j.1600-0722.1982.tb00760.x. [DOI] [PubMed] [Google Scholar]
- 19.Verschraegen CF, Benjapibal M, Supakarapongkul W, Levy LB, Ross M, Atkinson EN, Bodurka-Bevers D, Kavanagh JJ, Kudelka AP, Legha SS. Vulvar melanoma at the M. D. Anderson Cancer Center: 25 years later. Int J Gynecol Cancer. 2001;11:359–64. doi: 10.1046/j.1525-1438.2001.01043.x. [DOI] [PubMed] [Google Scholar]
- 20.Postow MA, Hamid O, Carvajal RD. Mucosal melanoma: pathogenesis, clinical behavior, and management. Curr Oncol Rep. 2012;14:441–8. doi: 10.1007/s11912-012-0244-x. [DOI] [PubMed] [Google Scholar]
- 21.Adjuvant Therapy for Melanoma Prolongs RFS. Cancer Discov. 2018;8:666–667. doi: 10.1158/2159-8290.CD-NB2018-047. [DOI] [PubMed] [Google Scholar]
- 22.Melanoma drugs effective as adjuvants. Cancer Discov. 2017;7:OF7. doi: 10.1158/2159-8290.CD-NB2017-131. [DOI] [PubMed] [Google Scholar]
- 23.Ballester Sanchez R, de Unamuno Bustos B, Navarro Mira M, Botella Estrada R. Mucosal melanoma: an update. Actas Dermosifiliogr. 2015;106:96–103. doi: 10.1016/j.ad.2014.04.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.