Music is fundamental to the human species in ways that reach beyond entertainment or pastime. In Musicophilia, Oliver Sacks noted that music can “calm us, animate us, comfort us, thrill us, or serve to organize and synchronize us at work or play, [but] it may be especially powerful and have great therapeutic potential for patients with a variety of neurological conditions.” For stroke patients with Broca aphasia, for example, the neural connections that allow ordinary speech are damaged; patients know what they want to communicate but are unable to verbalize their thoughts. Standard medical treatments are limited, but patients working with a music therapist can learn to express themselves through song, which can translate into improved speech potentially through the utilization of neural pathways more heavily relied on during singing.1
The number of stories and viral videos attesting to the promise of music therapy in clinical applications has grown substantially in recent years. Yet even with decades of practical application, we do not fully understand how music and music therapy achieve these beneficial effects, or how to optimize them for the individual patient. We now have the opportunity to connect our rapidly increasing insights from neuroscience with the clinical experience of applying music therapy in practice.
As individuals, we—soprano Renée Fleming and National Institutes of Health (NIH) Director Francis Collins—share a love of singing, playing, and composing music and a fascination with the intersection of music and neuroscience. As representatives of the John F. Kennedy Center for the Performing Arts and the NIH and in association with the National Endowment for the Arts, we launched the Sound Health: Music and the Mind initiative, beginning with an NIH workshop in January 2017 in which music therapists, experts in the neuroscience of music, and supporters of biomedical research and the arts gathered to discuss the current state of the field and identify future research needs.
The workshop made clear that neuroscientists are now using brain imaging techniques in new and innovative ways to address fundamental questions about how humans perceive and create music and are beginning to catalog what effects music can have structurally and functionally on the developing, adult, and aged brain. Meanwhile, music therapists have generated evidence for the therapeutic effects of active engagement with music for an ever-growing list of indications. Future goals are now to connect the effects of music on the brain with mechanistic insights from biomarkers and other approaches to elucidate how music therapy interventions may be working and enhance their efficacy and generalizability. Building on this foundation, the Kennedy Center will host a public kick-off event for the partnership on June 2 and 3, 2017, including a National Symphony Orchestra concert, performances inspired by music therapy approaches, and discussions about the underlying science and recent advances in understanding.
Processing music is one of the most cognitively demanding tasks our brains undertake, and creating and performing music is even more complex. We are just beginning to understand what neural processes underlie the effects of active music making, and a better appreciation of these processes would likely enhance understanding of brain responses to other stimuli and tasks. There is already compelling evidence that in children, music training assists development of language skills, auditory processing, and educational achievement compared with untrained peers,2–4 and anecdotally, many top professionals across different disciplines have musical training in their background.
At the level of fundamental neuroscience, musicians have notable differences in gray matter thickness of the ventral premotor cortex compared with that of nonmusicians, and the extent of these differences is related to the age at onset of intense musical training.5 On a functional level measurable by imaging techniques, music engages the brain in expansive and specific ways. The degree of overlap between brain activity induced by music and that associated with other functional domains such as language hints at how the benefits of music training transfer to those other domains.6 But just as music engagement with large expanses of the brain may be crucial to its effects, certain parts of the brain appear to be specifically tuned for music. There is an area within the auditory cortex that appears to respond only to music and not to other auditory stimuli.7 If music were not important to our species, why would human brains have evolved a “music room” to receive and interpret it?
Given music’s effect on the brain, it is natural to examine how music can best be used in health care settings. The inception of the music therapy field itself evolved from the treatment of posttraumatic stress disorder in veterans returning from World War II, but the field has been growing ever since. Music therapy is now used to improve health outcomes in pediatric cancer, autism, Alzheimer disease, chronic pain, and Parkinson disease, to name a few applications. In just the last 10 years, there have been more than 100 systematic reviews on the topic, including 10 Cochrane analyses. Individual cases have reported compelling results, but relatively few large- scale clinical trials have been conducted. The largest of these trials have yielded mostly inconclusive results, possibly because of the heterogeneity of affected individuals, interventions, and responses. Research requires standardized interventions while music therapy likely requires interventions tailored to the individual. More defined biological targets and biomarkers could facilitate assessment of the degree of target engagement by music therapy and could be useful in interpreting outcomes.
Music therapy has the potential to benefit substantially from the explosion of multidisciplinary cooperation and advances in technology that are happening in neuroscience, like those emerging from the BRAIN Initiative in the United States. The expansion of this knowledge is bidirectional; the music and music therapy communities are likely to contribute as much as they benefit and can be valuable partners participating in the development and validation of new tools exploring the brain and emotion. Neuroscientists working with musicians have developed magnetic resonance imaging- compatible cellos and keyboards, which have allowed for imaging of brain function during musical performances and improvisation. As an interesting example, we have already learned that improvisation yields widespread changes in activity across many neural networks compared with rote performance.8 Advances like these promise to provide mechanistic clues as to how music therapy may be working and how its efficacy can be improved.
We are just beginning to understand at a clinical level how music can elicit strong effects in the brain. Music gives individuals the “chills” by triggering a targeted release of dopamine in the striatum9; the common characterization of music as “powerful” reveals a widespread acceptance of this concept. A better understanding of the intersection of music and neuroscience would only add to the “magic” of these experiences. We hope that, through the Sound Health initiative, we can galvanize broad public interest in the scientific investigation of music and the brain from both a fundamental knowledge and health standpoint. Brain scans and wellness outcomes demonstrate that music can be more than entertainment. Through this initiative we seek to shine a light on this field of research and amplify this message to the public. The stage is set for an acceleration of understanding and application, and we invite clinicians, scientists, and the public to lend their voices to the choir.
Soprano Renée Fleming with National Institutes of Health (NIH) postdoctoral fellow David Jangraw during a recent visit to the NIH.
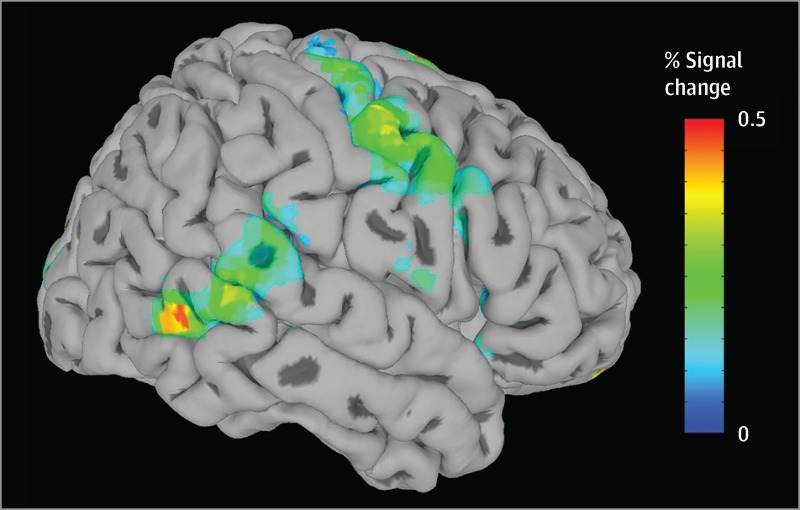
Functional magnetic resonance imaging (MRI) scan of coauthor Renée Fleming imagining herself singing an excerpt of “River Songs” (a medley by Dave Grusin). The colors indicate an increase in fMRI signal, commonly interpreted as increased brain activity. Areas where a statistically significant increase in activity was not observed are shown in gray. Darker gray regions indicate indentations in the cortex. Like speaking and overt singing, imagined singing activates motor regions and auditory-motor integration regions, but this silent rehearsal did not excite primary auditory regions. Imagined singing also activates regions in the inferior frontal cortex, believed to play a role in musical syntax and motor preparation, and the amygdala, commonly implicated in studies of emotion and arousal. These results from one individual are similar to those seen in larger studies of singers. Image courtesy of David Jangraw, National Institute of Mental Health, NIH.
Contributor Information
Francis S. Collins, National Institutes of Health, Bethesda, Maryland.
Renée Fleming, John F. Kennedy Center for the Performing Arts, Washington, DC..
Conflict of Interest Disclosures
The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
References
- 1.Schlaug G. Musicians and music making as a model for the study of brain plasticity. Prog Brain Res. 2015;217:37–55. doi: 10.1016/bs.pbr.2014.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hallam S. The power of music: its impact on the intellectual, social and personal development of children and young people. IntJ Music Educ. 2010;28 (3):269–289. doi: 10.1177/0255761410370658 [DOI] [Google Scholar]
- 3.The Arts and Human Development: Learning Across the Lifespan. National Endowment for the Arts in partnership with US Dept of Health and Human Services. https://www.arts.gov/sites/default/files/TheArtsAndHumanDev.pdf 2011. Accessed April 5, 2017.
- 4.Moreno S, Bialystok E, Barac R, et al. Short-term music training enhances verbal intelligence and executive function. PsycholSci. 2011;22(11):1425–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bailey JA, Zatorre RJ, Penhune VB. Early musical training is linked to gray matter structure in the ventral premotor cortex and auditory-motor rhythm synchronization performance. J Cogn Neurosci. 2014;26(4):755–767. [DOI] [PubMed] [Google Scholar]
- 6.Patel AD. Why would musical training benefit the neural encoding of speech? the OPERA hypothesis. Front Psychol. 2011;2:142. doi: 10.3389/fpsyg.2011.00142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Norman-Haignere S, Kanwisher NG, McDermott JH. Distinct cortical pathways for music and speech revealed by hypothesis-free voxel decomposition. Neuron. 2015;88(6):1281–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Limb CJ, Braun AR. Neural substrates of spontaneous musical performance: an FMRI study of jazz improvisation. PLoS One. 2008;3(2):e1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salimpoor VN, Benovoy M, Larcher K, Dagher A, Zatorre RJ. Anatomically distinct dopamine release during anticipation and experience of peak emotion to music. Nat Neurosci. 2011;14(2):257–262. [DOI] [PubMed] [Google Scholar]