Abstract
A 40-year-old-man with chronic history of refractory palmoplantar psoriasis presented with new onset of well-demarcated oval erythematous asteatotic plaques on bilateral shins after starting guselkumab therapy. Histopathology revealed chronic spongiotic dermatitis consistent with a diagnosis of nummular dermatitis. This case highlights a previously unreported adverse event to guselkumab therapy.
Keywords: Dermatitis, guselkumab, IL23, nummular, palmoplantar psoriasis, psoriasis, Th17
Case Report
A 40-year-old otherwise healthy man initially presented to the dermatology clinic nine years prior when he developed a generalized pustular eruption, subungual pustules with widespread nail dystrophy, and hyperkeratotic well-demarcated scaly plaques on his right heel. The patient reported a remote history of childhood psoriasis and no family history of skin disease. Biopsy was performed at initial presentation on the right mid-back showing neutrophilic dermatitis with subcorneal pustules consistent with pustular psoriasis. Subsequent biopsies of his heel were consistent with palmopustular psoriasis. The patient was treated with short course of cyclosporine and his trunk involvement improved but his acral lesions persisted.
For the next several years, the patient continued to have recalcitrant palmoplantar disease with nail involvement. He was tried on numerous treatments including topical and intralesional steroids, psoralen and UVA therapy, oral systemics, including cyclosporine, soriatane, and isotretinoin. Eventually, the patient was started on biologic therapy with ustekinumab, which provided the patient with some relief. A repeat biopsy was performed, which showed features consistent with initial diagnosis of palmoplantar psoriasis. Despite combination therapies with PUVA, acitretin, and ustekinumab, the patient continued to have painful pustular lesions on the fingertips and heel. He was then switched to guselkumab and had noticeable improvement.
After three months of guselkumab therapy, the patient retuned with a new pruritic well-demarcated erythematous asteatotic plaques on his bilateral shins (Fig. 1). Biopsy of the left upper shin showed chronic spongiotic dermatitis with psoriasiform epidermal hyperplasia, foci of spongiosis, hypergranulosis, parakeratosis, and perivascular lymphohistiocytic infiltrates consistent with nummular dermatitis (Fig 2). The patient had no other changes in medications or medical history at the time of rash onset. Lesions similar to these had never before been present.
Figure 1:

Bilateral well-demarcated oval well-demarcated erythematous asteatotic plaques on bilateral shins.
Figure 2:
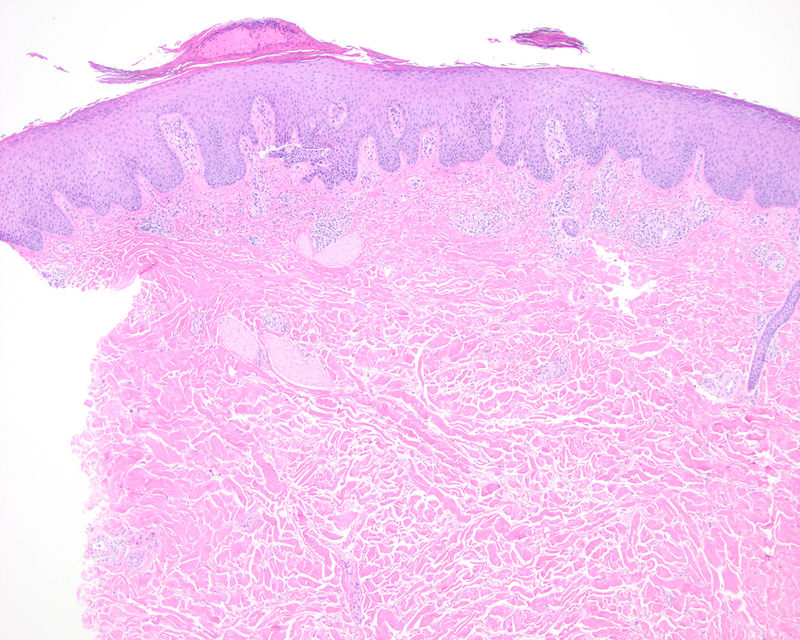
Punch biopsy of left lower shin of lesion demonstrates chronic spongiotic dermatitis with psoriasiform epidermal hyperplasia, foci of spongiosis, hypergranulosis, parakeratosis, and perivascular lymphohistiocytic infiltrates (H&E, 4x).
Discussion
Guselkumab is a fully human IgG1 λ monoclonal antibody. It binds to the p19 subunit of IL-23. Inhibition of IL-23 in turn adversely affects Th17 cells which are dependent on IL-23 for their maintenance. In global phase 2 and 3 studies, guselkumab has shown efficacy and safety in patients with moderate-severe plaque psoriasis and received in FDA indication in 2017. It is currently used off-label for the treatment of palmoplantar psoriasis and has shown to have efficacy in several case reports and case series(Terui et al., 2018). There have been no case reports to our knowledge of nummular dermatitis from guselkumab.
Evidence from molecular studies supports the involvement of IL-23 in palmoplantar psoriasis and palmoplantar pustulosis(Murakami et al., 2011, Torii et al., 2011). Further, reductions in serum concentrations of IL-17A and IL-17F can alleviate the phenotypic manifestations of plaque psoriasis and palmoplantar psoriasis. By antagonizing IL-23p19, this inflammatory pathway is disrupted and therefore is a viable biological therapy for these immune-mediated skin conditions. In a recent study of 49 patients conducted by Terui et. al. in 2018, guselkumab was used to treat palmoplantar pustulosis. Onset of clinical response within two weeks of therapy with a trend towards improvement until week 24(Terui et al., 2018).
The cytokine signaling profile of nummular dermatitis has not been well characterized. There have been several case reports of drug-induced nummular dermatitis with interferon alfa-2b plus ribavirin and isotretinoin but not reported in guselkumab or biologic therapies(Bettoli et al., 1987, Moore et al., 2004). This case highlights an unusual presentation of nummular dermatitis in a patient with recalcitrant palmoplantar psoriasis on guselkumab. Guselkumab shows current promise as a therapeutic potential for palmoplantar psoriasis. Greater awareness of dermatologic side effects to biologic therapies may lead to improved surveillance and treatment of these side effects and potentially prevent switching or discontinuation of effective therapies.
Acknowledgments:
AT was supported by the National Psoriasis Foundation.
Funding sources: Dr Kiuru’s involvement in this case report was in part supported by the National Cancer Institute, National Institutes of Health through grant K12CA138464.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to declare.
References
- Bettoli V, Tosti A & Varotti C (1987). Nummular eczema during isotretinoin treatment. J Am Acad Dermatol 16, 617. [DOI] [PubMed] [Google Scholar]
- Moore MM, Elpern DJ & Carter DJ (2004). Severe, generalized nummular eczema secondary to interferon alfa-2b plus ribavirin combination therapy in a patient with chronic hepatitis C virus infection. Arch Dermatol 140, 215–7. [DOI] [PubMed] [Google Scholar]
- Murakami M, Hagforsen E, Morhenn V, Ishida-Yamamoto A & Iizuka H (2011). Patients with palmoplantar pustulosis have increased IL-17 and IL-22 levels both in the lesion and serum. Exp Dermatol 20, 845–7. [DOI] [PubMed] [Google Scholar]
- Terui T, Kobayashi S, Okubo Y, Murakami M, Hirose K & Kubo H (2018). Efficacy and Safety of Guselkumab, an Anti-interleukin 23 Monoclonal Antibody, for Palmoplantar Pustulosis: A Randomized Clinical Trial. JAMA Dermatol 154, 309–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torii K, Furuhashi T, Saito C, Kato H, Nishioka A, Nishida E, Shintani Y & Morita A (2011). Increased peripheral Th17 in patients with pustulosis palmaris et plantaris. Arch Dermatol Res 303, 441–4. [DOI] [PubMed] [Google Scholar]


