Abstract
The purpose of this study was to identify determinants of HIV and sexually transmitted infection (STI) testing and acquisition among female victims of intimate partner violence (IPV). Data were abstracted from intake and HIV/STI testing forms from a family justice center, to identify the socioeconomic and abuse characteristics associated with requesting and obtaining an HIV/STI test (n = 343) and acquisition of HIV/STIs (n = 111). Multiple logistic regression using forward selection was used to identify predictors of HIV/STI testing and acquisition. Females experiencing greater risk of lethality were at higher odds of requesting an HIV/STI test; however, risk of lethality did not predict the receipt of an HIV/STI test. A history of sexual assault was associated with higher odds of acquiring HIV/STIs in the past year. Interventions are needed to facilitate HIV/STI testing among female victims of IPV, especially those with higher risk of lethality and a history of sexual assault.
Keywords: battered women, domestic violence, intervention/treatment, homicide, sexual assault, sexuality
There is a growing body of research identifying health disparities in the acquisition of HIV and other sexually transmitted infections (STIs) among female victims of intimate partner violence (IPV) worldwide. In a systematic review and meta-analysis assessing the association between HIV and IPV among women in 16 countries, authors noted a moderate statistically significant relationship between multiple forms of IPV including physical, sexual, and psychological violence and HIV infection (Li et al., 2014). Although the exact strength of the relationship between IPV and HIV and other STIs has not been well established, it appears that in the United States, women who report recent IPV are between 1.5 and 6 times at greater odds of ever having an STI than their nonabused counterparts (Gonzalez-Guarda, Peragallo, Urrutia, Vasquez, & Mitrani, 2008; Li et al., 2014). Variation in the conditions where women live, work, play, and love (i.e., social determinants) likely play a role in influencing the large range of risk of HIV/STIs identified among victims of IPV.
Various pathways linking IPV and HIV/STIs have been delineated. These include (a) an increase in sexual risk behaviors among both victims and perpetrators of IPV such as, having unprotected sex, multiple sex partners, and having sex under the influence of alcohol or drugs; (b) physiological and psychological consequences of violence that facilitate HIV transmission, such as being immune compromised; (c) forced sex with an infected partner; and (d) the inability of victims to negotiate condom use and other safer sexual practices because of lack of control over sexual decision making (Campbell et al., 2008). The overlap between IPV and HIV/STIs calls for public health approaches that more closely target these intersecting risks for women.
HIV/STI testing and counseling have been identified as key public health strategies to reduce HIV/STI-related health disparities among high-risk populations (Granich, Gilks, Dye, De Cock, & Williams, 2009). Despite the growing body of research documenting the disproportionate risk that victims of IPV face in acquiring HIV/STIs, and recent calls for the integration of HIV and IPV services, there is a paucity of research identifying factors that influence HIV/STI testing behaviors in this population (Campbell et al., 2008; Gielen et al., 2007; Interagency Federal Working Group, The White House, 2013). In addition, the vast majority of research describing the incidence of HIV and STIs among women experiencing IPV has relied on self-reported data, likely overlooking women who are asymptomatic. This article reports findings from a community-academic partnership that provided HIV/STI testing services to women seeking social services for IPV at a family justice center and conducted research to identify determinants of HIV/STI testing (Aim 1) and acquisition (Aim 2) in this population.
Background
Social Determinants of Health Framework
The World Health Organization’s (Marmot et al., 2008) Social Determinants of Health Framework sheds light on the social production of health. According to this framework, an individual’s socioeconomic position plays a central role in determining his or her health and well-being. The socioeconomic and political context influences, and is influenced by, the socioeconomic positions of groups. Marginalized and oppressed groups often characterized according to gender, race/ethnicity, education, and income have limited access to power, which, in turn, influences intermediary determinants of health, such as material circumstances, behaviors, and psychosocial and biological factors that influence health inequities (Marmot et al., 2008). In the context of health disparities related to HIV/STIs among victims of IPV, we posit that abuse characteristics such as the type of IPV (i.e., physical, sexual, psychological) and the risk of lethality (i.e., dangerousness of IPV) serve as additional key social determinants that influence an individual’s need and access to HIV/STI testing (Aim 1) and risk of acquiring HIV/STIs (Aim 2). This approach is aligned with the Social Determinants of Health Framework, in that, it addresses how an individual’s vulnerability to negative health outcomes can be linked to differential exposures to violence (Marmot et al., 2008). An adapted framework that incorporates a focus on the influence of socioeconomic and abuse vulnerabilities among female victims of IPV related to their likelihood of HIV/STI testing and acquisition is depicted in Figure 1.
Figure 1.
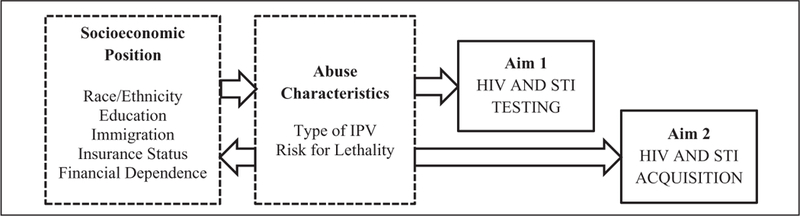
Determinants of HIV and STI testing and acquisition among female victims of IPV explored in this study. Note. STI = sexually transmitted infection; IPV = intimate partner violence.
Determinants of HIV/STI Testing for Victims of IPV
Strategies that increase access to safe and confidential HIV/STI testing for female victims of IPV are needed. Researchers have found that although victims of IPV have higher rates of HIV testing than nonabused women, HIV testing in this population remains low (Etudo, Metheny, Stephenson, & Kalokhe, 2017; Nasrullah, Oraka, Breiding, & Chavez, 2013; Rountree, Chen, & Bagwell, 2016). For example, in one study examining HIV testing in a large sample of nonpregnant women in 15 U.S. states/territories, 53% of women ever experiencing IPV reported being tested for HIV as compared with 33% among nonabused women. Yet, only about half of female victims of IPV have ever sought out testing (Nasrullah et al., 2013). Integrating HIV testing within existing IPV services, such as domestic violence shelters and other social agencies, has been recommended as a strategy for increasing testing among this vulnerable population (Interagency Federal Working Group, The White House, 2013). Nevertheless, few studies have reported on predictors of HIV/STI testing among victims accessing IPV services. This information is vital to developing interventions that promote the uptake of HIV/STI testing in settings serving victims of IPV.
Previous research on HIV/STI testing behaviors in the United States has also documented certain predictors of testing. Individuals who are younger in age, African American, unmarried, and caretakers of children have been overrepresented among testers (Rountree, Chen, Brown, & Pomeroy, 2009; Robinson, Sanders, & Boyd, 2012; Tucker, Wenzel, Elliott, Hambarsoomian, & Golinelli, 2003). However, because researchers conducting these studies did not stratify their samples according to abuse experiences, it is unknown whether these predictors are also applicable for victims of IPV.
Determinants of HIV/STI Acquisition Among Victims of IPV
A few studies have been conducted to identify predictors of HIV/STI acquisition among victims of IPV accessing services for IPV. Researchers have estimated that approximately one in three women in domestic violence agencies report acquiring an STI during their abusive relationship (Wingood, DiClemente, & Raj, 2000). A history of sexual assault, having an unfaithful partner, sexual risk behaviors, and fear of negotiating condom use have been found to be associated with a history of STI among victims of IPV accessing social services (Mittal et al., 2013; Wingood et al., 2000). Nevertheless, these studies are limited by the sole reliance on self-reported history of HIV/STIs. Given that not all abused women have access to testing and obtain it, it is likely that these figures underestimate the true problem.
There is also limited research on how abuse determinants, such as the type and lethality of IPV, influence HIV/STI risk. Although sexual assault is an established risk factor for HIV, little is known about how other forms of abuse contribute to this risk (Welch & Mason, 2007). Emerging evidence suggests that physical IPV has an additional effect on risk of HIV/STIs, even when considering the overlap of physical and sexual violence (Spiwak, Afifi, Halli, Garcia-Moreno, & Sareen, 2013). In fact, in a review of 40 years of published research (1966–2006), researchers documented consistent evidence that physical IPV is associated with sexual risk-taking behaviors, self-reported history of STIs, and the negative health outcomes of these (Coker, 2007). However, less is known about the impact that IPV has on HIV/STI acquisition when testing is made available to victims and how the lethality of this IPV influences these risks.
Aims of the Study
This study aimed to fill various gaps in the literature. First, we aimed to identify determinants associated with requesting and receiving an HIV/STI test at a social service agency serving female victims of IPV (Aim 1). To address this aim, we explored the influence of socioeconomic position (race/ethnicity, education, insurance status, immigration, financial dependence on the abuser) and abuse characteristics (type of IPV [physical, psychological, sexual], risk of lethality). To our knowledge, this is the first study to document predictors of HIV/STI testing among victims of IPV by offering access to testing. Second, we aimed to identify determinants of HIV/STI acquisition among female victims receiving testing (Aim 2). This study aimed to overcome limitations to exclusive use of self-reported STI histories by providing free HIV/STI testing, and adding the results from these tests to self-reported data.
Method
Design
A secondary analysis was used to address the two aims of the study. For the first aim, a chart review was conducted in the social service agency where the study took place over a 6-month period (July 2014 to December 2014; N = 343). The charts contained information about client characteristics, socioeconomic position, abuse characteristics, and HIV/STI testing. For the second aim of the study, the HIV/STI test results performed for clients over a 1-year period (July 2014 to September 2015; N = 132) were abstracted from consented clients’ HIV/STI testing forms and linked to data from chart reviews. Institutional review board approval was granted prior to the implementation of any study-related procedures.
Sample and Setting
The study took place in a family justice center for victims of IPV, sexual assault, and human trafficking in South Florida with a strong community–academic partnership with a local university, the Partnership for Domestic Violence Prevention (Gonzalez-Guarda, Cummings, Becerra, Fernandez, & Mesa, 2013). The family justice center approach is one that aims to bring together multisector partnerships that allow for comprehensive and wraparound services (e.g., legal, social, and mental health services) for victims at one place, thus providing a “one stop shop” for victims with multiple needs (Gwinn, Strack, Adams, & Lovelace, 2007). The vast majority of clients who access services related to IPV are from racial and ethnic minority groups (65% Hispanic, 22% Black, 11% Other), and about half are primarily Spanish speaking (Lawson, Laughon, & Gonzalez-Guarda, 2012). Although HIV/STI services were available to all clients, to be eligible for the study, clients needed to identify as female, a victim of IPV, and 18 years or older. There were no exclusion criteria applied.
Procedures
When clients first sought services at the agency, they completed an intake process with a trained advocate. During this process, advocates completed a standardized intake form and service referral form. These forms documented factors about the individual, his or her relationship, characteristics of the abuse, and services sought at the family justice center, including HIV and STI testing. Clients who expressed a desire to obtain an HIV and/or STI test were referred to an on-site certified HIV counselor. For clients who were eligible to participate in Aim 2, written informed consent was collected at the same time that informed consent for the HIV test was collected. Study team members emphasized that the client’s decision whether or not to participate in the study did not have an influence on his or her ability to access HIV testing or any other services. The HIV counselor collected additional data required by the local health department for HIV testing, conducted a rapid HIV test (Oraquick) using a finger prick, and collected a urine specimen, which was tested for chlamydia and gonorrhea by the local health department laboratory. The HIV counselor communicated directly with the client regarding the test results. These results were linked to the data collected during the intake process for the purposes of this study, and with participant consent.
Measures
Control variables.
The client’s age (years) and previous experience with receiving an HIV or STI test (yes/no; if yes, then date) were abstracted from the intake form and used as control variables.
Socioeconomic position.
Self-identified information related to socioeconomic position was abstracted from the intake forms. This included self-identified race/ethnicity (Hispanic, Black, non-Hispanic White, and Other), education (less than high school, high school or higher), immigration status (immigrant vs. U.S. born), and access to health insurance (yes/no). Many of the clients did not report their monthly income. Consequently, we abstracted information regarding whether they were financially dependent on the abuser (yes/no).
Abuse characteristics.
The intake form also collected self-identified exposure to physical, sexual, and psychological abuse by their intimate partner. These were coded as three separate, dichotomous (yes/no) variables. A danger assessment was also completed for each client as part of the intake process (Campbell, Webster, & Glass, 2009). The danger assessment contains a 20-item instrument, which has been shown to predict risk of lethality among victims of IPV. Clients respond to a series of questions assessing the dangerousness of specific abusive acts (e.g., Does he ever try to choke you? Does he threaten to kill you?). Responses (yes/no) are weighted to calculate a total score (range = 0–39). Scores are categorized into variable danger (<8), increase danger (8–13), severe danger (14–17), or extreme danger (>18). The reliability for the danger assessment was acceptable (α = .75 for Aim 1 and α = .80 for Aim 2). Finally, for participants of Aim 2, information regarding their lifetime history of sexual assault, regardless of the relationship to the perpetrator, was also collected as part of the HIV/STI testing process.
HIV/STI testing.
Clients completing an intake were asked whether they were interested in receiving an HIV and/or STI test on site (yes/no). An HIV/STI testing log was also kept to document the number of individuals who requested to get tested and received a test. Three mutually exclusive categorical outcomes were generated from these data: (a) clients who did not request an HIV and/or STI test, (b) clients who requested an HIV and/ or STI test, but did not receive one; and (c) clients who requested an HIV and/or STI test, and obtained one.
HIV/STI acquisition.
HIV/STI acquisition was assessed through three different means. First, a positive HIV test was considered when one had a reactive rapid HIV test on site (Oraquick), and then a positive confirmatory Western Blot, which was conducted through the local health department. Second, a positive STI was considered when one tested positive for chlamydia or gonorrhea via a urine specimen that was collected on site and examined by the local health department laboratory. Third, self-reported past-year histories of STIs were also collected from individuals being tested. Finally, positive cases of HIV and STIs identified through on-site HIV/STI testing were added to self-reported STI past-year histories to identify all participants who had detected HIV or STIs in the past 12 months.
Analysis
Descriptive statistics were used to describe the sample and identify the frequency of requesting HIV/STI testing, receiving one, and HIV/STI acquisition. Descriptive results for the danger assessment scores were summarized using means and standard deviations as well as categories of risk. In the regression models, danger assessment was treated as a continuous variable to utilize all available information and maximize power to identify significant associations. Determinants of requesting/receiving an HIV/STI test (Aim 1) were assessed using multinomial logistic regression. The dependent variable categories included not requesting/receiving an HIV/STI test (the referent), requesting but not receiving an HIV/STI test, or receiving an HIV/STI test. Charts from 532 clients were reviewed for Aim 1. Determinants of acquiring HIV/STI in the past year (Aim 2) were assessed using multivariable logistic regression. Model covariates for both models were added using forward selection with a p = .1 cutoff. Race/ethnicity and education were included in the models, regardless of statistical significance as forced demographic variables. The social determinants of immigration, financial dependence on the abuser, and physical/sexual/psychological abuse by an intimate partner were not included in the final models because they did not meet this cutoff.
Participants who had been tested in the past 3 months (n = 86) were excluded from the multivariable model in Aim 1 to avoid including women whose decision to test was based on having a recent test. Individuals who were missing testing information (n = 52) or covariate data (n = 51) were also excluded from analyses, resulting in a final sample size of 343 for Aim 1. One hundred thirty-one individuals who received HIV/STI testing consented to participate in Aim 2. Individuals with missing test results (n = 3) or covariate data (n = 17) were excluded from analyses, resulting in a final sample size of 111 for Aim 2.
Results
Sample Characteristics
The characteristics of participants included in the analyses for Aim 1 (N = 323) and Aim 2 (N = 111), a subset of Aim 1, are summarized in Table 1. Both samples were largely comprised of Hispanic (62%, 67%, respectively) and immigrant (both 59%) females. The majority of participants reported physical (67%, 70%, respectively), sexual (37%, 36%, respectively), and psychological abuse (both 61%) by an intimate partner, and 29% of those assessed for Aim 2 reported being sexually assaulted by anyone at some point in their life (this variable was not collected for Aim 1). The risk of lethality was high, with a mean score on the danger assessment above 15 for both samples, and more than half categorized as being in severe or extreme danger of being killed by their partner (Campbell et al., 2009). Of those analyzed for Aim 1, just more than half (53%) requested an HIV and/or STI test, and less than one third received one (33%). Of the women included in the analysis for Aim 2 (n = 111), one tested positive for HIV, seven (6%) tested positive for one or more STIs (six cases of chlamydia, one case of gonorrhea), and an additional nine (8%) reported that they acquired an STI in the past 12 months. A summary of the participant characteristics and bivariate analysis of associations according to aim are summarized in Table 2.
Table 1.
Participant Characteristics for Aim 1 (N = 343) and Aim 2 (N = 111).
| Variable | Aim 1 M (SD) or % (N) (N = 343) |
Aim 2 M (SD) or % (N) (N = 111) |
|---|---|---|
| Age | 34.69 (10.08) | 33.14 (9.98) |
| Race/ethnicity | ||
| Hispanic | 61.8 (212) | 66.7 (74) |
| Black | 29.5 (101) | 33.3 (37) |
| Other | 8.8 (30) | a |
| Less than high school education | 31.5 (108) | 37.8 (42) |
| Health insurance | 49.3 (169) | 43.0 (46) |
| Previous HIV test | 73.2 (251) | 70.0 (77) |
| Immigrant | 59.2 (202) | 58.6 (65) |
| Financial dependence on abuser | 32.9 (104) | 34.3 (35) |
| Physical abuse by intimate partner | 66.9 (228) | 70.0 (77) |
| Sexual abuse by intimate partner | 36.7 (125) | 35.5 (39) |
| Psychological abuse by intimate partner | 60.6 (206) | 60.9 (67) |
| Sexual assault by anyone | NC | 28.8 (32) |
| Risk of lethality, M (STD) | 15.28 (7.49) | 15.92 (8.02) |
| Risk of lethality category, % (n) | ||
| Variable (<8) | 15.2 (52) | 13.5 (15) |
| Increase (8–13) | 26.8 (92) | 25.2 (28) |
| Severe (14–17) | 20.1 (69) | 20.7 (23) |
| Extreme (18+) | 37.9 (130) | 40.5 (45) |
Note. Participants with missing covariates were excluded from the analysis. NC = not collected for Aim 1 portion of study; STD = sexually transmitted disease.
N = 5 omitted from the analysis/model due to small group size.
Table 2.
HIV Test Request/Receipt (Aim I) and HIV/STI (Aim 2) by Participant Characteristics and Bivariate Analyses of Associations.
| Variable | Aim 1 (N = 343) |
Aim 2 (N = 111) |
|||||
|---|---|---|---|---|---|---|---|
| Did Not Request an HIV Test (n = 160) M (SD) or % (N) |
Requested an HIV Test, Not Received (n = 70) M (SD) or % (N) |
Received an HIV Test (n = 113) M (SD) or % (N) |
P | Did Not Acquire HIV/STI (n = 95) M (SD) or % (N) |
Acquired HIV/ STI (n = 16) M (SD) or % (N) |
P | |
| Age, M (SD) | 35.59 (10.47) | 36.00 (9.85) | 32.61 (9.39) | .0283 | 33.26 (9.73) | 32.50 (1 1.66) | .7786 |
| Race/ethnicity, n (%) | |||||||
| Hispanic | 46.7 (99) | 21.7 (46) | 31.6 (67) | .5990 | 89.2 (66) | 10.8 (8) | .1,330 |
| Black | 44.6 (45) | 19.8 (20) | 35.6 (36) | 78.4 (29) | 21.6 (8) | ||
| Other | 53.3 (16) | 13.3(4) | 33.3 (10) | ||||
| High school education or more, n (%) | |||||||
| No | 48.1 (52) | 18.5 (20) | 33.3 (36) | .8358 | 78.6 (33) | 21.4 (9) | .1076 |
| Yes | 46.0 (108) | 21.3 (50) | 32.8 (77) | 89.9 (62) | 10.1 (7) | ||
| Health insurance, n (%) | |||||||
| No | 39.1 (68) | 24.7 (43) | 36.2 (63) | .0137 | 82.0 (50) | 18.0 (1 1) | .3082 |
| Yes | 54.4 (92) | 16.0 (27) | 29.6 (50) | 89.1 (41) | 10.9 (5) | ||
| Previous HIV test, n (%) | |||||||
| No | 50.0 (46) | 10.9 (10) | 39.1 (36) | .0303 | 97.0 (32) | 3.0(1) | .0525 |
| Yes | 45.4 (114) | 23.9 (60) | 30.7 (77) | 80.5 (62) | 19.5 (15) | ||
| Immigrant, n (%) | |||||||
| No | 45.3 (63) | 18.7 (26) | 36.0 (50) | .6071 | 82.6 (38) | 17.4 (8) | .4545 |
| Yes | 47.0 (95) | 21.8 (44) | 31.2 (63) | 87.7 (57) | 12.3 (8) | ||
| Financial dependence on | abuser, n (%) | ||||||
| No | 48.1 (102) | 18.4 (39) | 33.5 (71) | .3007 | 83.6 (56) | 16.4 (1 1) | .2823 |
| Yes | 43.3 (45) | 26.0 (27) | 30.8 (32) | 91.4 (32) | 8.6 (3) | ||
| Physical abuse by intimate partner, n (%) | |||||||
| No | 53.1 (60) | 15.0 (17) | 31.9 (36) | .1363 | 81.8 (27) | 18.2 (6) | .4807 |
| Yes | 43.4 (99) | 23.2 (53) | 33.3 (76) | 87.0 (67) | 13.0 (10) | ||
| Sexual assault by intimate partner, n (%) | |||||||
| No | 49.1 (106) | 18.1 (39) | 32.9 (71) | .2872 | 83.1 (59) | 16.9 (12) | .3490 |
| Yes | 42.4 (53) | 24.8 (31) | 32.8 (41) | 89.7 (35) | 10.3 (4) | ||
| Psychological abuse by intimate partner, n (%) | |||||||
| No | 44.8 (60) | 21.6 (29) | 33.6 (45) | .8137 | 93.0 (40) | 7.0 (3) | .0834 |
| Yes | 48.1 (99) | 19.4 (40) | 32.5 (67) | 80.6 (54) | 19.4 (13) | ||
| Sexual assault by anyone | |||||||
| No | NC | NC | NC | NC | 91.1 (72) | 8.9 (7) | .0126 |
| Yes | NC | NC | NC | NC | 71.9 (23) | 28.1 (9) | |
| Risk of lethality, M (SD) | 14.88 (7.30) | 16.97 (7.03) | 14.81 (7.93) | .1095 | 15.62 (7.93) | 17.69 (8.56) | .3401 |
| Risk of lethality category, % (n) | |||||||
| Variable (<8) | 48.1 (25) | 13.5(7) | 38.5 (20) | .1742 | 86.7 (13) | 13.3 (2) | .1519 |
| Increase (8–13) | 52.2(48) | 16.3 (15) | 31.5 (29) | 92.9 (26) | 7.1 (2) | ||
| Severe (14–17) | 40.6 (28) | 24.6 (17) | 34.8 (24) | 91.3 (21) | 8.7 (2) | ||
| Extreme (18+) | 45.4 (59) | 23.8 (31) | 30.8 (40) | 77.8 (35) | 22.2 (10) | ||
Note. N = 5 omitted from the analysis/model due to small group size; participants with missing covariates were excluded from the analysis; p values resulting bivariate analyses (multinomial model for Aim 1; logistic model for Aim 2, with only the single characteristic as an independent variable). STI = sexually transmitted infection; NC = not collected.
Determinants of HIV/STI Testing
Requesting HIV/STI testing but not receiving it.
Participants with health insurance had lower odds of requesting an HIV/STI test (adjusted odds ratio [AOR] = 0.40,p < .01; Table 3). Participants with a history of past year HIV/STI testing (AOR = 2.55, p < .05) and greater risk of lethality (AOR = 1.05, p < .05) were at greater odds of requesting testing. Age, race/ethnicity, and education did not predict requesting HIV/STI testing (p > .05).
Table 3.
Determinants of Requesting and Receiving an HIV/STI Test (Aim 1, N = 343) and Acquiring HIV/STIs (Aim 2, N = 111).
| Requesting Test | Receiving Test | Acquiring HIV/STI | |
|---|---|---|---|
| (Aim 1) | (Aim 1) | (Aim 2) | |
| Predictor | AOR (95% CI)a | AOR (95% CI)a | AOR (95% CI)b |
| Age | 1.02 (0.99–1.05) | 0.97 (0.95–0.999)* | NAc |
| Race/ethnicity (ref. = Hispanic) | |||
| Black | 0.89 (0.44–1.80) | 1.19 (0.66–2.15) | 2.15 (0.67–6.93) |
| Other | 0.50 (0.15–1.65) | 1.27 (0.52–3.11) | —d |
| Less than high school education | 1.41 (0.73–2.72) | 1.20 (0.70–2.07) | 0.34 (0.11–1.09) |
| Health insurance | 0.40 (0.21–0.74)** | 0.59 (0.35–0.999)* | NAc |
| Previous HIV test | 2.55 (1.16–5.60)* | 0.80 (0.46–1.39) | NAc |
| Sexual assault by anyone | NAc | NAc | 4.64 (1.46–14.76)** |
| Risk of lethality | 1.05 (1.001–1.09)* | 1.00 (0.97–1.03) | 1.04 (0.97–1.12) |
Note. Participants with missing covariates were excluded from the analysis. CI = confidence interval; STI = sexually transmitted infection; AOR = adjusted odds ratio.
Multinomial logistic regression with no test requested or received as the referent.
Multivariable logistic regression.
Variable not included using forward selection with a p = .1 cutoff.
N = 5 omitted from the analysis/model due to small group size.
p < .05.
p < .01.
Receiving HIV/STI testing.
Participants of older age (AOR = 0.97, p < .05) and with health insurance (AOR = 0.59, p < .05) were at lower odds of receiving an HIV/STI test on site. Race/ethnicity, education, previous HIV test, and risk of lethality did not predict receiving an HIV/STI test on site (p > .05).
Determinants of HIV/STI Acquisition
Participants with a history of sexual assault were more than 4 times at greater odds of acquiring HIV/STI in the past year (AOR = 4.64, p < .01). Race/ ethnicity, education, and risk of lethality did not predict HIV/STI acquisition (p > .05).
Discussion
This study examined determinants of HIV/STI testing and acquisition among racially and ethnically diverse female victims of IPV, a group disproportionately affected by HIV and other STIs (Campbell et al., 2008; Gielen et al., 2007). An adapted Social Determinants of Health Framework (Marmot et al., 2008) was used to explore the influence of socioeconomic position and abuse characteristics on likelihood of HIV/STI testing and acquisition. Secondary data from a large family justice center in South Florida were obtained and linked to HIV/STI testing behaviors, and outcomes after a free and confidential HIV/STI testing service were established on site. This allowed researchers to assess predictors of HIV/STIs among victims using two data sources—self-reported history of HIV and STIs in the past 12 months and biological data obtained from the HIV/STI test results. To our knowledge, this is one of the first studies to explore predictors of HIV/STI testing and acquisition at a social service agency for victims of IPV who have access to testing. Findings from this study provide important implications for designing and promoting the use of HIV/STI services for victims of IPV.
Just more than half of the female victims (53%) accessing services at the family justice center for IPV requested an HIV/STI test. The relatively low rate of interest in HIV/STI testing among victims of IPV has also been documented by others (Nasrullah et al., 2013; Rountree et al., 2016). There are various possible explanations for the low interest in HIV/STI testing in this population. First, female victims may not have felt that they were psychologically ready to take on the stressful experience of HIV/STI testing. The HIV/STI testing processes can be very stressful for women because they fear the results (Draucker et al., 2015; Williams, Gonzalez-Guarda, & Ilias, 2017). Victims may have decided against exposing themselves to another potential source of trauma at this time. Second, female victims may not have necessarily linked their IPV experience to an increased risk of HIV/STI. In fact, qualitative research with IPV victims has identified lack of knowledge regarding HIV transmission and risk as a barrier to testing (Draucker et al., 2015). Third, there is a possibility that victims of IPV accessed HIV/STI in a follow-up visit at the family justice center or elsewhere and, hence, are not captured in these data. Finally, additional barriers previously documented among minority women, such as stigma and fatalism, may have also served as deterrents to requesting HIV/STI testing (Eastwood et al., 2015). In fact, stigma and fatalism have been documented to have a negative influence on HIV testing uptake across the globe (Kelly, Weiser, & Tsai, 2016; Obermeyer & Osborn, 2007).
It is important to note that although 53% of clients requested a test, only 33% received one. The socioeconomic and abuse characteristics from the adapted Social Determinants of Health Framework appeared to play a role. In fact, individuals with insurance were less likely to request an HIV/STI test and receive one. This may have been because victims of IPV with insurance were more likely to receive testing through health care settings. Researchers investigating the influence of insurance coverage and HIV testing have found that insurance coverage increases HIV testing rates, especially for high-risk populations in the United States (Sood, Wagner, & Wu, 2015). However, it is important to note that victims of IPV both in the United States and across the globe may have limited access to health care that results from their partner’s controlling behavior, especially as it relates to reproductive and sexual health (Silverman & Raj, 2014). There are also additional sociocultural and political barriers, such as medical mistrust and immigration status that may limit access to HIV/STI among victims of IPV in both formal and informal health care settings, particularly among ethnic minority women (Stockman, Hayashi, & Campbell, 2015).
This gap between requesting an HIV/STI test and receiving one suggests that multiple implementation factors, including agency-level factors, may have been at play. For example, the HIV/STI counselors may not have been available at the moment the request was made because they were with another client or away from the office. Another possibility is that a decision to not receive an HIV/STI test was made by the client or the advocate because of competing demands during the visit. For example, the client may have a higher priority safety need such as obtaining a protective order that was prioritized over HIV/STI testing. There may have also been language barriers between the client and the counselor, or high levels of distress deemed by the client and counselor as the wrong timing for HIV/STI testing. Finally, it is possible that the added cost and challenges to providing HIV/STI testing in a family justice center does not provide an additional benefit over referral services to more traditional health care settings for HIV/STI testing, such as an STI clinic or primary care office. More research is needed to go beyond the client-specific data examined in this study to explore the organizational factors that influence the implementation of HIV/STI testing for this high-risk population and the cost effectiveness of offering this service at a family justice center.
There was one case of HIV, six cases of chlamydia, and one case of gonorrhea identified through the HIV/STI testing service. In total, seven (6%) participants tested positive for one or more STIs and an additional nine (8%) reported that they acquired an STI in the past 12 months. The only determinant of HIV/STI acquisition from the adapted Social Determinants of Health Framework was abuse characteristics, specifically a history of lifetime sexual assault. Surprisingly, race/ethnicity, and risk of lethality were not predictive of HIV/STI acquisition. This may have been because the sample was already at an increased risk of HIV/STI related to their abuse histories, which may have “washed out” effects of socioeconomic determinants on HIV/STI. Although clients experiencing higher levels of lethality were more likely to request testing, they did not necessarily receive one. Therefore, the sample on which the analysis was based to predict HIV/STI acquisition may not have adequately represented the variance in danger levels present in female victims of IPV. As reported in the sample characteristics, the women included in this study experienced severe risk of lethality. Future research should reexamine the influence of risk of lethality on HIV/STI outcomes among groups of women with a broader range of lethality risk.
There are additional limitations to this study that warrant attention. The analysis of this study was based on data that were collected for social service purposes. Consequently, the quality of data collection cannot be ensured, and some participants could not be included in the analysis due to missing data. We were also limited with regard to what social determinants of health could be examined as predictors. Second, the predictors included in this study were all based on self-reported data. Given the stigma regarding both IPV and HIV, it is likely that social desirability played a role in experiences that were reported. The influence of community attitudes and norms around IPV and HIV testing on these behaviors should be examined in future research. In addition, we were unable to collect information regarding participants’ current HIV status, due to potential legal implications that may arise having this information recorded in their file. As such, we could not control for HIV status in our analyses. In addition, although we were able to test for HIV/STI and document acquisition, we also relied on self-reported histories of STIs in the past 12 months. Consequently, there is a possibility that participants who were classified as not having a history of an STI may have had undetected cases. Finally, the results from this study can only be generalized to women in South Florida seeking services for IPV. More research is needed to identify predictors of HIV/STI testing and acquisition among victims not formally seeking help.
The findings from this article have important implications for the integration of HIV/STI testing in social service agencies. As previously mentioned, one case of HIV and seven cases of STIs were identified through the 12-month testing period for this study. Given the individual and public health consequences associated with HIV/STIs, it is important to implement strategies to identify, counsel, and treat HIV/STIs in this population. Offering free, rapid, and confidential HIV/STI testing and counseling for victims of IPV appears to be a promising approach, which is supported by both victims and providers (Draucker et al., 2015; Williams et al., 2017). However, less than half of the clients seeking services for IPV requested testing, and an even smaller proportion received one. Organizational and client-provider factors appear to play a key role in the success of implementing HIV/STI testing in social agencies serving victims of IPV. The influence of these should be further explored through research and tracked and monitored in the implementation of HIV/STI testing. More research is also needed to identify strategies to promote HIV/STI testing in this population, and when these may be appropriate (e.g., when to offer testing for victims). In doing so, special attention should be paid to finding a balance between trauma-informed strategies that consider the psychosocial well-being of female victims of IPV with population-based strategies aimed at protecting the public’s health.
Acknowledgments
The authors would also like to acknowledge the additional support from the Coordinated Victim Assistance Center, Miami Dade County Community Action and Human Services Department, and the University of Miami Adolescent Counseling and Testing Service at the Miller School of Medicine.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the Center of Excellence for Health Disparities Research: El Centro, National Center on Minority Health and Health Disparities (NIMHD) (grant P60MD002266).
Author Biographies
Rosa M. Gonzalez-Guarda, PhD, MPH, RN, FAAN, is an associate professor at Duke University School of Nursing. Her research focuses on understanding and addressing intersecting behavioral and mental health disparities among Hispanic immigrants and the prevention of gendered-based violence. She has expertise in community-engaged research approaches, culturally tailored interventions, and efforts to diversify the health disparities scientific workforce.
Jessica R. Williams, PhD, MPH, APHN-BC, is an assistant professor at the University of North Carolina at Chapel Hill School of Nursing. Her primary research interests focus on (a) improving health outcomes among those affected by gender-based violence and (b) improving the role of the health care system in identifying and responding to gender-based violence with a particular focus on elucidating disparities that exist in this process. Her work is facilitated through the application of community engagement methodology and dissemination and implementation science.
Weston Williams, PhD, MHS, is a senior statistical analyst at Public Health Analytic Consulting Services, Inc. His research focus is on the design and analysis of HIV prevention and treatment adherence program evaluations and studies in epidemiology. He has more than 10 years consulting experience providing analytic and statistical support to government agencies, universities, and nonprofit organizations.
Dalia Lorenzo, MPH, is a project manager at the University of Miami School of Nursing and Health Studies’ Center of Excellence in Precision Medicine and Population Health. She completed her MPH and MBA at the University of Miami. She has previously worked as a research coordinator for University of Miami School of Nursing and Health Studies’ National Institutes of Health (NIH)/National Center on Minority Health and Health Disparities (NIMHD)–funded Center of Excellence for Health Disparities Research, which advances the science of reducing health disparities in the areas of HIV/AIDS and other sexually transmitted infections, substance abuse, family and intimate partner violence (IPV), and associated mental and physical health conditions.
Cherelle Carrington, LCSW, is a doctoral student at Florida International University Robert Stempel College of Public Health and Social Work. Her research interests focus on (a) assessing psychological treatment for women who have experienced IPV utilizing single-case design methodology and (b) relationship interventions with a focus on African American couples.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Campbell JC, Baty M, Ghandour RM, Stockman JK, Francisco L, & Wagman J (2008). The intersection of intimate partner violence against women and HIV/AIDS: A review. International Journal of Injury Control and Safety Promotion, 15, 221–231. doi: 10.1080/17457300802423224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JC, Webster DW, & Glass N (2009). The danger assessment: Validation of a lethality risk assessment instrument for intimate partner femicide. Journal of Interpersonal Violence, 24, 653–674. doi: 10.1177/0886260508317180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker AL (2007). Does physical intimate partner violence affect sexual health? A systematic review. Trauma, Violence, & Abuse, 8, 149–177. doi: 10.1177/1524838007301162 [DOI] [PubMed] [Google Scholar]
- Draucker CB, Johnson DM, Johnson-Quay NL, Kadeba MT, Mazurczyk J, & Zlotnick C (2015). Rapid HIV testing and counseling for residents in domestic violence shelters. Women Health, 55, 334–352. doi: 10.1080/03630242.2014.996726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eastwood EA, Fletcher J, Quinlivan EB, Verdecias N, Birnbaum JM, & Blank AE (2015). Baseline social characteristics and barriers to care from a special projects of national significance women of color with HIV study: A comparison of urban and rural women and barriers to HIV care. AIDS Patient Care STDS, 29(Suppl. 1), S4–S10. doi: 10.1089/apc.2014.0274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etudo O, Metheny N, Stephenson R, & Kalokhe AS (2017). Intimate partner violence is linked to less HIV testing uptake among high-risk, HIV-negative women in Atlanta. AIDS Care, 29, 953–956. doi: 10.1080/09540121.2016.1271936 [DOI] [PubMed] [Google Scholar]
- Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, & O’Campo P (2007). HIV/AIDS and intimate partner violence: Intersecting women’s health issues in the United States. Trauma, Violence, & Abuse, 8, 178–198. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Guarda RM, Cummings AM, Becerra M, Fernandez MC, & Mesa I (2013). Needs and preferences for the prevention of intimate partner violence among Hispanics: A community’s perspective. The Journal of Primary Prevention, 34, 221–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Guarda RM, Peragallo N, Urrutia MT, Vasquez EP, & Mitrani VB (2008). HIV risks, substance abuse, and intimate partner violence among Hispanic women and their intimate partners. Journal of the Association of Nurses in AIDS Care, 19, 252–266. [DOI] [PubMed] [Google Scholar]
- Granich RM, Gilks CF, Dye C, De Cock KM, & Williams BG (2009). Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: A mathematical model. The Lancet, 373, 48–57. [DOI] [PubMed] [Google Scholar]
- Gwinn C, Strack G, Adams S, & Lovelace R (2007). The family justice center collaborative model. The Saint Louis University Public Law Review, 27, 79–120. [Google Scholar]
- Interagency Federal Working Group, The White House. (2013). Addressing the intersection of HIV/AIDS, violence against women and girls, & gender–related health disparities. Retrieved from https://www.hivlawandpolicy.org/resources/addressing-intersection-hivaids-violence-against-women-and-girls-gender-related-health
- Kelly JD, Weiser SD, & Tsai AC (2016). Proximate context of HIV stigma and its association with HIV testing in Sierra Leone: A population-based study. AIDS and Behavior, 20, 65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson SL, Laughon K, & Gonzalez-Guarda RM (2012). Predictors of health care use among a predominantly Hispanic, urban sample of individuals seeking IPV services. Hispanic Health Care International, 10, 28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue EE, & Ehiri JE (2014). Intimate partner violence and HIV infection among women: A systematic review and meta-analysis. Journal of the International AIDS Society, 17(1), Article 18845. doi: 10.7448/ias.17.1.18845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M, Friel S, Bell R, Houweling TA, Taylor S, & Commission on Social Determinants of Health. (2008). Closing the gap in a generation: Health equity through action on the social determinants of health. The Lancet, 372. 1661–1669. [DOI] [PubMed] [Google Scholar]
- Mittal M, Stockman JK, Seplaki CL, Thevenet-Morrison K, Guido J, & Carey MP (2013). HIV risk among women from domestic violence agencies: Prevalence and correlates. Journal of the Association of Nurses AIDS Care, 24, 322–330. doi: 10.1016/j.jana.2012.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasrullah M, Oraka E, Breiding MJ, & Chavez PR (2013). HIV testing and intimate partner violence among non-pregnant women in 15 US states/territories: Findings from behavioral risk factor surveillance system survey data. AIDS and Behavior, 17, 2521–2527. doi: 10.1007/s10461-013-0493-1 [DOI] [PubMed] [Google Scholar]
- Obermeyer CM, & Osborn M (2007). The utilization of testing and counseling for HIV: A review of the social and behavioral evidence. American Journal of Public Health, 97, 1762–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson KT, Sanders SA, & Boyd JL (2012). High-risk HIV minorities in the United States: Who gets tested and where? American Journal of Health Behaviors, 36, 348–359. doi: 10.5993/ajhb.36.3.6 [DOI] [PubMed] [Google Scholar]
- Rountree MA, Chen L, & Bagwell M (2016). HIV-testing rates and testing locations among women who have experienced intimate partner violence: Data from the centers for disease control behavioral risk factor surveillance system, 2006. Violence Against Women, 22, 399–414. doi: 10.1177/1077801215603487 [DOI] [PubMed] [Google Scholar]
- Rountree MA, Chen L, Brown A, & Pomeroy EC (2009). HIV testing rates and testing locations, by race and ethnicity. Health & Social Work, 34, 247–255 [DOI] [PubMed] [Google Scholar]
- Silverman JG, & Raj A (2014). Intimate partner violence and reproductive coercion: Global barriers to women’s reproductive control. PLoS Medicine, 11(9), e1001723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sood N, Wagner Z, & Wu Y (2015). The impact of insurance on HIV testing. American Journal of Health Economics, 1, 515–536. [Google Scholar]
- Spiwak R, Afifi TO, Halli S, Garcia-Moreno C, & Sareen J (2013). The relationship between physical intimate partner violence and sexually transmitted infection among women in India and the United States. Journal of Interpersonal Violence, 28, 2770–2791. doi: 10.1177/0886260513487992 [DOI] [PubMed] [Google Scholar]
- Stockman JK, Hayashi H, & Campbell JC (2015). Intimate partner violence and its health impact on ethnic minority women. Journal of Women’s Health, 24, 62–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS, Wenzel SL, Elliott MN, Hambarsoomian K, & Golinelli D (2003). Patterns and correlates of HIV testing among sheltered and low-income housed women in Los Angeles County. Journal of Acquired Immune Deficiency Syndrome, 34, 415–422. [DOI] [PubMed] [Google Scholar]
- Welch J, & Mason F (2007). Rape and sexual assault. British Medical Journal, 334, 1154–1158. doi: 10.1136/bmj.39211.403970.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JR, Gonzalez-Guarda RM, & Ilias V (2017). Trauma-informed decision-making among providers and victims of intimate partner violence during HIV testing: A qualitative study. Journal of the Association of Nurses in AIDS Care, 28, 819–831. doi: 10.1016/j.jana.2017.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ, & Raj A (2000). Identifying the prevalence and correlates of STDs among women residing in rural domestic violence shelters. Women & Health, 30(4), 15–26 [DOI] [PubMed] [Google Scholar]


