Key Points
Question
Is electronic cigarette (e-cigarette) use associated with marijuana use in adolescents and young adults?
Findings
In this systematic review and meta-analysis, the odds of past or current marijuana use among youth who used e-cigarettes were 3.5 times higher than for those who denied e-cigarette use; this association was significant in both cross-sectional and longitudinal studies. Studies conducted in adolescents aged 12 to 17 years (vs young adults aged 18 to 24 years) showed a stronger association between e-cigarette and marijuana use.
Meaning
These findings suggest that clinical and regulatory approaches to managing e-cigarette use among youth amid the current trend of marijuana legalization should consider the significant association between e-cigarette and marijuana use.
This systematic review and meta-analysis of longitudinal and cross-sectional studies examines the association between electronic cigarette use and marijuana use in people aged 10 to 24 years.
Abstract
Importance
Use of electronic cigarettes (often called e-cigarettes) has increased considerably among young people in the past 5 years. Use of e-cigarettes has been associated with higher rates of marijuana use, which is associated with several adverse health outcomes in youth.
Objective
To characterize and quantify the association between e-cigarette and marijuana use among youth using a meta-analysis.
Data Sources
PubMed, Embase, and Web of Science & ProQuest Dissertations and Theses were searched from inception to October 2018. A gray-literature search was also conducted on conference abstracts, government reports, and other sources.
Study Selection
Included studies compared rates of marijuana use among youth aged 10 to 24 years who had used e-cigarettes vs those who had not used e-cigarettes. Two reviewers independently assessed studies for inclusion; disagreements were discussed with a third reviewer and resolved by consensus.
Data Extraction and Synthesis
Data were extracted by 2 independent reviewers following Meta-analyses of Observational Studies in Epidemiology (MOOSE) reporting guidelines and pooled using a random-effects analysis. The Newcastle-Ottawa Scale was used to assess data quality and validity of individual studies.
Main Outcomes and Measures
Adjusted odds ratios (AORs) of self-reported past or current marijuana use by youth with vs without past or current e-cigarette use.
Results
Twenty-one of 835 initially identified studies (2.5%) met selection criteria. The meta-analysis included 3 longitudinal and 18 cross-sectional studies that included 128 227 participants. Odds of marijuana use were higher in youth who had an e-cigarette use history vs those who did not (AOR, 3.47 [95% CI, 2.63-4.59]; I2, 94%). Odds of marijuana use were significantly increased in youth who used e-cigarettes in both longitudinal studies (3 studies; AOR, 2.43 [95% CI, 1.51-3.90]; I2, 74%) and cross-sectional studies (18 studies; AOR, 3.70 [95% CI, 2.76-4.96]; I2, 94%). Odds of using marijuana in youth with e-cigarette use were higher in adolescents aged 12 to 17 years (AOR, 4.29 [95% CI, 3.14-5.87]; I2, 94%) than young adults aged 18 to 24 years (AOR, 2.30 [95% CI, 1.40-3.79]; I2, 91%).
Conclusions and Relevance
This meta-analysis found a significant increase in the odds of past or current and subsequent marijuana use in adolescents and young adults who used e-cigarettes. These findings highlight the importance of addressing the rapid increases in e-cigarette use among youths as a means to help limit marijuana use in this population.
Introduction
Use of electronic nicotine-delivery systems (ENDS), specifically electronic cigarettes (also known as e-cigarettes), among young people between the ages of 10 and 24 years has increased substantially in the past 5 years.1 In fact, more than one-third of high school seniors in the United States report e-cigarette use in the past year.2 While ENDS have been hypothesized to contain fewer harmful emissions than traditional cigarettes, research has shown that they are not without risk, and ENDS aerosols often contain high levels of nicotine, heavy metals, and carcinogens.3,4 In addition, recent studies have shown a strong association between ENDS use and subsequent use of alcohol, marijuana, and other drugs.5,6,7
Most individuals with substance use disorders initiate substance use before the age of 18 years, and more than 95% do so before the age of 25 years.8 Adolescents and young adults, whose brains are still developing, are more vulnerable than older adults to the addictive properties of nicotine, alcohol, marijuana, and other drugs.9 While the current understanding of harmful long-term effects of nicotine use on the developing human brain, including decreased memorization and attention capacity, still mostly relies on preclinical trials,10,11 the evidence of harmful long-term effects of adolescent marijuana use is more robust.12 For instance, longitudinal studies have shown that marijuana use during adolescence is associated with reduced cognitive abilities, motivation, satisfaction with life, and life achievement, as well as significantly greater rates of mental health disorders, such as depression, anxiety, and schizophrenia.13,14
On the one hand, several governments around the world are moving forward with legislation aimed at containing rates of ENDS use among youth.15 On the other hand, a strong global trend toward legalization and decriminalization of marijuana is increasing access to this substance.16 The effects of these policies on rates of ENDS and marijuana use among youth remain controversial,17 but the rapidly increasing prevalence of ENDS use in this population, and the possibility that this could lead to increases in comorbid substance use among youth, including marijuana use, is concerning.6 More precise estimates of the risk of current or subsequent marijuana use in youth with ENDS use could inform development and implementation of public policies aiming to delay initiation and reduce rates of marijuana use among young people.
We conducted a systematic review of the literature and meta-analysis to characterize and quantify the association between ENDS and marijuana use among adolescents and young adults. We hypothesized that the odds of using marijuana would be significantly higher among youth with ENDS use (vs no use) and that this association would be stronger in adolescents vs young adults and youth with dual ENDS and cigarette use vs use of ENDS only.
Methods
Data Sources and Search Strategy
This meta-analysis is in accordance with proposed reporting set forth in Meta-Analysis and Systematic Review of Observational Studies in Epidemiology (MOOSE)18 and the Enhancing the Quality and Transparency of Health Research (EQUATOR) Reporting Guidelines.19 PubMed, Embase, Web of Science, and ProQuest Dissertations & Theses databases were searched for potential studies. In addition, conference abstracts, proceedings, and reports from the past 10 years (2008-2018) from major substance use and tobacco prevention associations and conferences in the United States and international locations were searched for relevant sources. Finally, targeted searches of systematic reviews and summary reports on the health effects of e-cigarettes3,20 were conducted, yielding 1 additional relevant review, which was searched for relevant studies.21
The database search strategy (eMethods in the Supplement) was developed in consultation with a medical reference librarian and was adapted from a recently published meta-analysis looking at the association between ENDS and tobacco cigarette use among adolescents.22 When available, we used controlled vocabularies, such as medical subject headings (MeSH) on PubMed and Embase subject headings (Emtree) on Embase. Key terms included ENDS, e-cigarette, vaping, marijuana, alcohol, prescription drug misuse, illicit drug use, and substance abuse. We chose not to include any terms limiting participant age, language, type of substance used, study design, or year of publication in the search strategy, to minimize unintentional exclusions. Final PubMed, Embase, and Web of Science & ProQuest searches were conducted on October 8, 2018. Identified studies were imported and compiled using Covidence Software (Veritas Health Innovation).
Study Selection
To be included in this review, a study had to compare rates of marijuana use among youth with vs without a history of ENDS use. Studies could be cross-sectional or longitudinal, and the mean or median age of study participants needed to be between 10 and 24 years. The use of ENDS was defined as current (in the past month) and/or ever, and ENDS products with or without flavoring were included. Similarly, marijuana use was defined as current and/or ever use of marijuana products consumed by inhalation or ingestion. Studies were required to provide actual or calculable adjusted odds ratios of the association between ENDS use and co-occurring marijuana use (in cross-sectional studies) or subsequent marijuana use (in longitudinal studies). In 1 case, provision of relevant unpublished data, which included adjusted odds ratios, allowed inclusion of the study.23
All titles and abstracts obtained through the literature search (835 studies) were reviewed independently by 2 of 3 co-authors (N.C., J.W.J., and/or R.S.) to determine suitability for full-text screening. All 3 reviewers have been trained in public health research methods. Each article selected for full-text screening was then screened individually by 2 of 3 coauthors (N.C., J.W.J., and/or R.S.) for ultimate inclusion in the review and meta-analysis. At each stage, any discrepancy between reviewers concerning inclusion suitability was resolved by discussion among the 3 reviewers until unanimous consensus was reached. Reasons for exclusion included participants older than 24 years, the absence of a participant group that did not use ENDS, and the measurement of marijuana vaping without mention of nicotine vaping in participants reporting use of e-cigarettes (eFigure 1 in the Supplement).
Data Extraction
Individual study data were extracted by a coauthor (J.W.J., R.S., or N.C.) and subsequently verified by a second coauthor. Data extracted for each study included study design and type; survey method; geographic location of study sample; sample size; age of study participants; ENDS use; marijuana use; comorbid cigarette, alcohol, and drug use; covariates accounted for in adjusted models; and adjusted odds ratios (AORs) with 95% CIs. If studies lacked clear indication of adjustment for confounders, study authors were contacted for clarification. Additionally, authors who did not report odds ratios were contacted if the results they did report suggested that a relevant measure of association, although not published, had likely been calculated. When 2 or more studies presented with an overlapping population, exposure (ENDS use), and outcome (marijuana use), the study with the largest sample size (or the most recent analysis, in the case of equal-sized samples) was retained.
Risk of Bias Assessment
Risk of bias was assessed using the Newcastle-Ottawa Scale for observational studies.24 Studies were evaluated by 2 of 3 coauthors (N.C., J.W.J., and/or R.S.) and received a score of up to 6 points for cross-sectional studies and up to 9 points for longitudinal studies based on participant selection, study comparability, and assessment of the outcome of interest (marijuana use). Any disagreement was resolved by consensus between coauthors (N.C., J.W.J., and R.S.).
Statistical Analysis
The summary effect of ENDS use on marijuana use was calculated using a random-effects model. Several subgroup analyses based on clinically relevant factors were also conducted. Forest plots and measures of observed heterogeneity (I2 statistic) were generated for all summary and subgroup analyses.
A first subgroup analysis compared cross-sectional studies, limited to a strict determination of association without temporal ordering, to longitudinal studies, which could offer insights on temporal ordering of ENDS and marijuana use (and minimize the risk for reverse causation). A second subgroup analysis was conducted on studies divided by mean or median participant age (<18 years vs ≥18 years). This analysis was conducted in light of neurophysiologic differences between younger and older youths that have been shown to have a characteristic effect on risk-taking behaviors, impulse control, and susceptibility to substance use.9,25 We chose to have a cut point at 18 years because this separated studies that were conducted on middle school or high school students (the younger group) from studies that were generally conducted on college students (the older group). A third subanalysis compared youths with and without co-occurring use of conventional cigarettes or other forms of tobacco, since youths with dual or poly–tobacco use may have different substance use risk profiles than youth with ENDS-only use.5 A fourth subanalysis divided studies by publication year to account for the arrival of rechargeable, higher-technology, and often youth-friendly ENDS called pod mods, which became popular around 2015.26 We chose 2017 as a divider between older and newer studies because many studies published in 2017 or beyond used study data collected after the arrival of pod mods–type ENDS. A regional subgroup analysis by continent was conducted (North America, Europe, and other continents), given differences in prevalence, regulation, and taxation of ENDS between different continents.27 Finally, an Egger test was performed to assess the risk for publication bias and small study effects. All analyses were conducted using Stata computational software version 14.2 (StataCorp).
Results
Of 835 potentially relevant studies identified through the database search and 4 through the gray-literature search, 158 reports appeared potentially eligible after title and abstract screening. After exclusion of 137 studies through full-text screening, including 3 studies with overlapping data sets,28,29,30 21 studies were found to be eligible5,6,7,23,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47 and were included in the qualitative and quantitative syntheses. All studies were observational; there were 3 longitudinal studies6,7,45 representing 14 364 participants and 18 cross-sectional studies5,23,31,32,33,34,35,36,37,38,39,40,41,42,43,44,46,47 representing 113 863 participants in total. Summary characteristics of included studies are shown in Table 1.
Table 1. Summary Characteristics of Included Studies.
| Source | Region and Country | Study Design | Study Period | Population | School Grade or Age of Study Participants | Sample Size, No. | Exposure to Electronic Cigarettes | Marijuana Use Outcome |
|---|---|---|---|---|---|---|---|---|
| Audrain-McGovern et al,7 2018 | California, United States | Prospective, longitudinal (baseline and 24-mo follow-up) | 2013-2015 | Students from 10 public high schools | Mean (SD), 14.6 (0.4) y | 2668 | Ever | Ever or past 30-d marijuana use |
| Azagba,32 2018 | Canada | Cross-sectional | 2014-2015 | Secondary data analysis of the 2014-2015 Canadian Student Tobacco and Alcohol and Drugs Survey | Grades 9-12 | 23 429 | Past 30 d, dual use | Past 30-d marijuana use |
| Bluestein,33 2017 | United States | Retrospective, cross-sectional | 2013-2014 | Secondary data analysis of the Population Assessment of Tobacco and Health Study, wave 1 | Range, 18-24 y | 8954 | Ever or past 30 d | Ever marijuana use |
| Camenga et al,34 2014 | Connecticut and New York, United States | Cross-sectional | 2010-2011 | Secondary data analysis of a student survey conducted in 4 high schools | Grades 9-12 | 1556 | Past 30 d | Past 30-d marijuana use |
| Cohn et al,35 2015 | United States | Retrospective, cross-sectional | 2013 | Secondary data analysis from Legacy Young Adult Cohort, wave 4 | Mean (SD), 20.9 (2.0) y | 1609 | Ever or past 30 d | Past 30-d marijuana use |
| Conway et al,36 2018 | United States | Retrospective, cross-sectional | 2013-2014 | Secondary data analysis of Population Assessment of Tobacco and Health Study, wave 1 | Range, 12-17 y | 13 617 | Ever | Ever marijuana use |
| Curran et al,5 2018 | United States | Cross-sectional | 2015 | Secondary data analysis of the National Youth Risk Behavior Survey | Grades 9-12 | 15 624 | Past 30 d, dual use | Ever or past 30-d marijuana use |
| Dai et al,6 2018 | United States | Retrospective, longitudinal | 2013-2015 | Secondary data analysis of Population Assessment of Tobacco and Health Study, wave 1 and 2 | Range, 12-17 y | 10 364 | Ever | Marijuana use 1-y follow-up |
| Dautzenberg et al,37 2015 | France | Cross-sectional | 2013 | Secondary data analysis from 2013 Paris Sans Tabac surveys | Range, 12-19 y | 2279 | Ever | Ever marijuana use |
| Dunbar et al,23 2017 | California, United States | Retrospective, cross-sectional | 2014 | Secondary data analysis from wave 7 of the CHOICE project cohort | Mean (SD), 17 (0.7) y | 2488 | Past year, dual use | Past-year marijuana use |
| Fotiou et al,38 2015 | Greece | Cross-sectional | 2014 | 2014 Health Behavior in School-aged Children study | Mean (SD), 15 (0) y | 435 | Ever | Ever marijuana use |
| Kong et al,39 2017 | Russia | Cross-sectional | 2015 | Survey of high school students | Range, 15-18 y | 716 | Ever | Ever marijuana use |
| Kristjansson et al,40 2017 | West Virginia, United States | Cross-sectional | 2015 | School survey conducted in 15 middle schools in 3 counties | Grades 6-8 | 5553 | Ever | Ever marijuana use |
| McCabe et al,31 2017 | United States | Cross-sectional | 2014 | Secondary data analysis of Monitoring the Future study | Grades 12a | 7711 | Past 30 d | Past 30-d marijuana use |
| Milicic and Leatherdale,41 2017 | Ontario and Alberta, Canada | Prospective cross-sectional | 2012-2015 | Ongoing cohort study in schools (the COMPASS Study) | Grades 9-12 | 39 837 | Past 30 d | Ever or past 30-d marijuana use |
| Saddleson et al,42 2015 | New York, United States | Cross-sectional | 2013 | Internet survey from a convenience sample of students at 4 colleges and universities | Mean (SD), 19.0 (1.3) y | 1292 | Ever or past 30 d | Past-year marijuana use |
| Sutfin et al,43 2013 | North Carolina, United States | Cross-sectional | 2009 | Survey of students from 8 colleges | Mean (SD), 20.5 (2.9) y | 4444 | Ever | Past 30-d marijuana use |
| Tavolacci et al,44 2016 | France | Cross-sectional | 2014-2015 | Multicenter study on 2 major campuses | Mean (SD), 20.8 (3.6) y | 1134 | Ever or past 30 d | Past 30-d marijuana use |
| Unger et al,45 2016 | California, United States | Retrospective, longitudinal | 2014-2015 | Secondary data analysis of longitudinal survey of Hispanic young adults | Mean (SD), 22.7 (0.4) y | 1332 | Past 30 d | Past 30-d marijuana use |
| White et al,46 2015 | Australia and New Zealand | Cross-sectional | 2014 | Youth Insights survey of year 10 students | Range, 14-15 y | 2855 | Ever, dual use | Ever marijuana use |
| Williams and White,47 2018 | Victoria, Australia | Cross-sectional | 2014 | Australian Secondary Students’ Alcohol and Drug Survey | Range, 12-17 y | 3158 | Ever | Ever marijuana use |
Most students were aged 18 years and older.
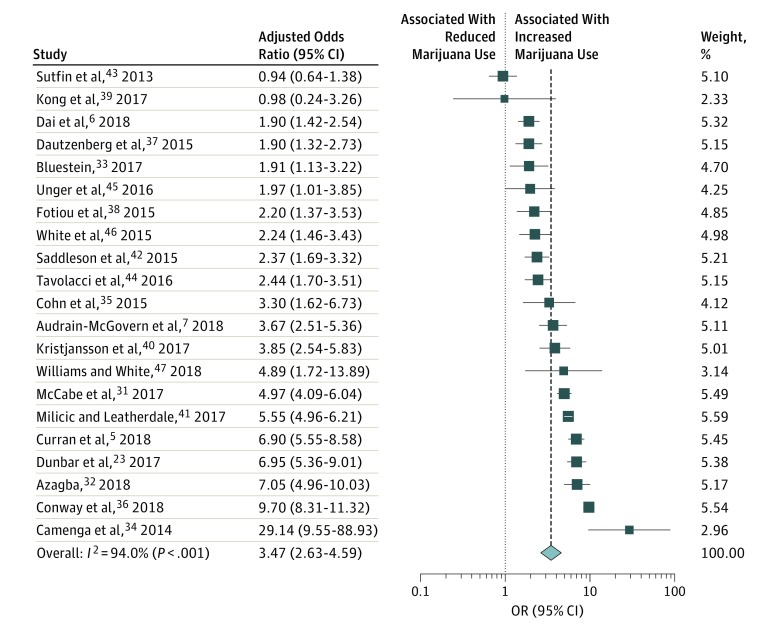
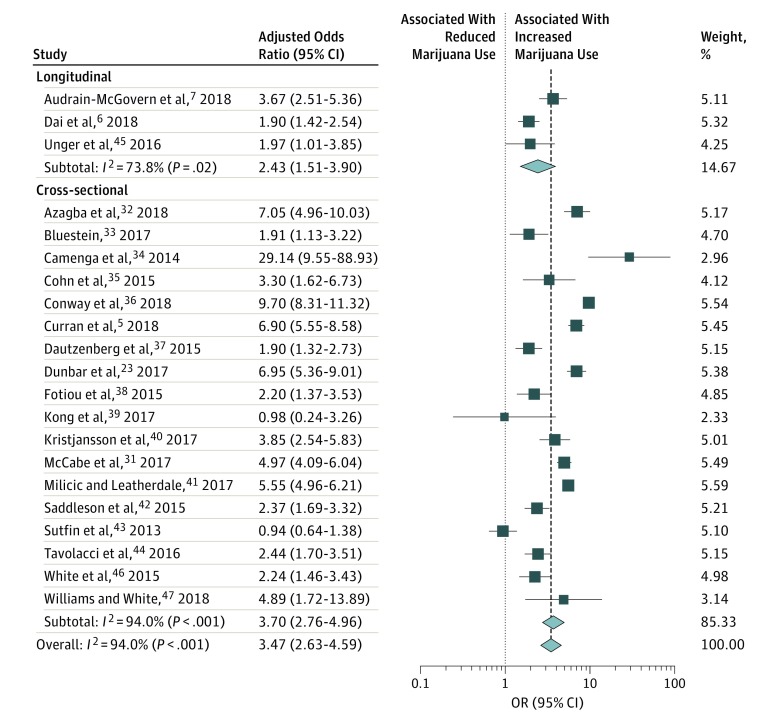
Pooling of data from all studies (Figure 1) suggested that ENDS use is associated with an increased risk of marijuana use (AOR, 3.47 [95% CI, 2.63-4.59]; I2, 94%). Subgroup analysis by study type (Figure 2) revealed significantly increased odds of marijuana use in both longitudinal (3 studies6,7,45; AOR, 2.43 [95% CI, 1.51-3.90]; I2, 73.8%) and cross-sectional studies (18 studies5,23,31,32,33,34,35,36,37,38,39,40,41,42,43,44,46,47; AOR, 3.70 [95% CI, 2.76-4.96]; I2, 94%).
Figure 1. Marijuana Use in Youth With e-Cigarette Use in Individual Studies.
Figure 2. Marijuana Use in Youth With e-Cigarette Use by Study Design in Individual Studies.
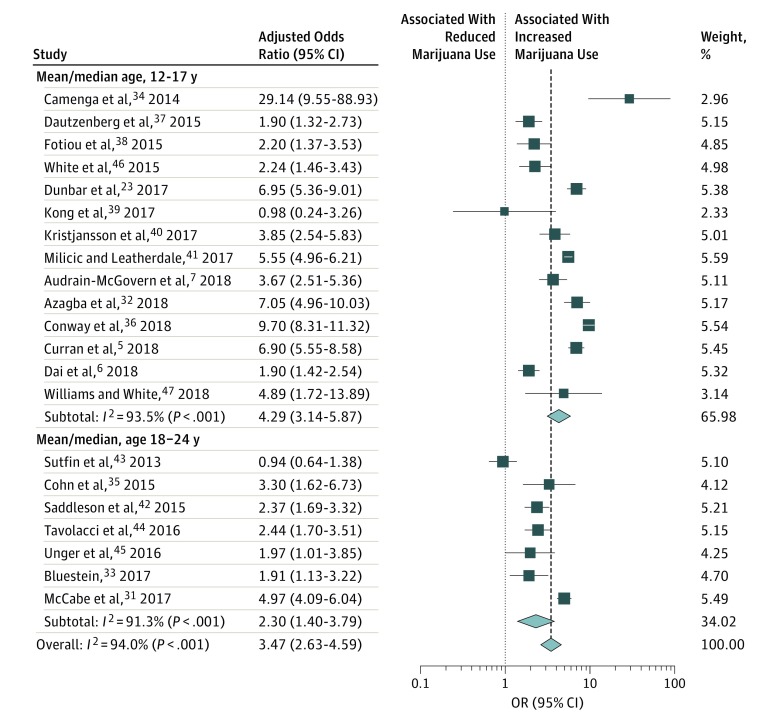
Subgroup analyses by age (Figure 3) showed a stronger association between ENDS use and marijuana use in studies with participants with a mean or median age younger than 18 years (14 studies5,6,7,23,32,34,36,37,38,39,40,41,46,47; AOR, 4.29 [95% CI, 3.14-5.87]; I2, 93.5%) vs studies with participants with a mean or median age 18 years and older (7 studies31,33,35,42,43,44,45; AOR, 2.30 [95% CI, 1.40-3.79]; I2, 91%). Subgroup analysis by single use of ENDS vs dual use of both ENDS and cigarettes or other tobacco products (eFigure 2 in the Supplement) revealed a stronger association between ENDS and marijuana use in studies with youths with dual use (4 studies5,23,32,46; AOR, 5.39 [95% CI, 3.53-8.24]; I2, 87.6%) than in studies with youths with single use (17 studies6,7,31,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47; AOR, 3.10 [95% CI, 2.22-4.34]; I2, 94.6%).
Figure 3. Marijuana Use in Youth With e-Cigarette Use by Mean/Median Participant Age in Individual Studies.
The pooled AOR for the association between ENDS use and marijuana use was higher for North American studies (15 studies5,6,7,23,31,32,33,34,35,36,40,41,42,43,45; AOR, 4.03 [95% CI, 2.97-5.49]) than for European studies (4 studies37,38,39,44; AOR, 2.12 [95% CI, 1.70-2.65]). There were only 2 non-European, non–North American studies (from Australia and New Zealand; 2 studies46,47; AOR, 2.84 [95% CI, 1.41-5.76]), and they had a pooled AOR with a 95% CI that overlaps with the 95% CIs of the pooled AOR for the North American and European studies.
Studies published in 2017 or later (12 studies5,6,7,23,31,32,33,36,39,40,41,47; AOR, 4.57 [95% CI, 3.47-6.03]) revealed a stronger association between ENDS use and marijuana use than studies that were published before 2017 (9 studies34,35,37,38,42,43,44,45,46; AOR, 2.39 [95% CI, 1.67-3.40]). Measures of association and risk of bias for each of the 21 selected studies are shown in Table 2. Quality ratings ranged from 3 to 5 points (of 6 points) for cross-sectional studies and 6 to 8 points (of 9 points) for longitudinal studies. The Egger test was nonsignificant, suggesting that a small study effect was unlikely.
Table 2. Measures of Association and Risk of Bias of Included Studies.
| Source | Covariates | Newcastle-Ottawa Scale | Adjusted Odds Ratio (95% CI) | |||
|---|---|---|---|---|---|---|
| Study Selection Subscore | Study Comparability Subscore | Outcomes Subscore | Quality Rating Summary Score | |||
| Audrain-McGovern et al,7 2018 | Age, sex, race/ethnicity, parental education, family history of combustible cigarette and drug use, peer combustible cigarette and marijuana use, Temperament and Character Inventory impulsivity subscale, and Center for Epidemiologic Studies Depression Scale | 3 | 1 | 2 | 6 | 3.67 (2.51-5.36) |
| Azagba,32 2018 | Sex, grade level, socioeconomic status, living area, and region of residence | 2 | 1 | 0 | 3 | 7.05 (4.95-10.03) |
| Bluestein,33 2017 | Sex, race, education level, household income, and the total number of tobacco products used | 3 | 2 | 0 | 5 | 1.91 (1.13-3.22) |
| Camenga et al,34 2014 | Sex, grade, and race | 2 | 1 | 0 | 3 | 29.14 (9.54-88.92) |
| Cohn et al,35 2015 | Age, sex, race/ethnicity, and educational attainment | 2 | 1 | 0 | 3 | 3.30 (1.61-6.73) |
| Conway et al,36 2018 | Age, sex, race/ethnicity, lifetime mental health (internalizing and externalizing) symptoms, and sensation seeking | 3 | 1 | 0 | 4 | 9.70 (8.31-11.31) |
| Curran et al,5 2018 | Age, sex, and race/ethnicity | 2 | 2 | 0 | 4 | 6.90 (5.55-8.57) |
| Dai et al,6 2018 | Sensation seeking, ever use of cigarettes, drinking, nonmedical use of prescription drugs and other illicit drugs, and demographic characteristics (sex, race and/or ethnicity, grade performance, parental education, and region) | 4 | 2 | 2 | 8 | 1.90 (1.42-2.53) |
| Dautzenberg et al,37 2015 | Age, smoking status of best friend, smoking status of sibling, ever smoked a cigarette, ever smoked shisha, smoking status, private school vs public, and parental message of prohibition | 2 | 2 | 0 | 4 | 1.90 (1.32-2.72) |
| Dunbar et al,23 2017 | Age, sex, mother's education level, nuclear family status, intervention group, and smokeless tobacco use | 2 | 2 | 0 | 4 | 6.95 (5.36-9.01) |
| Fotiou et al,38 2015 | Sex, life satisfaction, cigarette smoking, cannabis use, and presence of peers who smoke tobacco | 2 | 2 | 0 | 4 | 2.20 (1.37-3.53) |
| Kong et al,39 2017 | Age, sex, ethnicity, family structure, highest degree of mother and father, substance use, antisocial behaviors, stress coping scale, and school clustering | 2 | 2 | 0 | 4 | 0.98 (0.24-3.26) |
| Kristjansson et al,40 2017 | Age, sex, family structure, race, and each parent education | 2 | 2 | 0 | 4 | 3.85 (2.54-5.84) |
| McCabe et al,31 2017 | Age, sex, race/ethnicity, parental education, college plans, urbanicity, and geographical region | 2 | 1 | 0 | 3 | 4.97 (4.09-6.04) |
| Milicic and Leatherdale,41 2017 | Sex and school clustering | 2 | 2 | 0 | 4 | 5.55 (4.96-6.20) |
| Saddleson et al,42 2015 | Age, sex, race/ethnicity, institution, tobacco smoking, school ability, other tobacco use in the past 30 d, and beliefs about e-cigarette harm | 1 | 2 | 0 | 3 | 2.37 (1.69-3.32) |
| Sutfin et al,43 2013 | Sex, sensation seeking, current binge drinking, current marijuana use, lifetime illegal drug use, and e-cigarette harm perception | 1 | 2 | 0 | 3 | 0.94 (0.64-1.38) |
| Tavolacci et al,44 2016 | Age, university, student job holder, study grant holder, curriculum, and academic year | 1 | 2 | 0 | 3 | 2.44 (1.70 -3.51) |
| Unger et al,45 2016 | Age, sex, and other substance abuse | 3 | 2 | 2 | 7 | 1.97 (1.01-3.85) |
| White et al,46 2015 | Age, sex, school deprivation, income/allowance, smoking status, parental smoking behavior, close friends’ smoking behavior, use of tobacco products other than cigarettes (eg, chewing tobacco and cigars) in the past 30 d, ever use of marijuana, and ever engagement in binge drinking | 2 | 2 | 0 | 4 | 2.24 (1.46-3.43) |
| Williams and White,47 2018 | Age, sex, socioeconomic status, school level clustering, and education sector | 2 | 2 | 0 | 4 | 9.00 (1.72-13.89) |
Discussion
This study revealed that ENDS use was significantly associated with marijuana use in a large sample of adolescents and young adults pooled from 21 independent observational studies. While most included articles were cross-sectional, 3 longitudinal studies were included, and these suggested a temporal association between ENDS use and subsequent marijuana use. Subgroup analyses revealed that the association was stronger in youths who were younger and who combined ENDS and cigarette or tobacco use. The analyses also revealed regional and temporal variations: North American studies and studies published since 2017 showed stronger associations between ENDS use and marijuana use than European studies and studies published before 2017 did.
The findings of increased concurrent and subsequent marijuana use in youths with ENDS use can be interpreted in the context of what is already known about the association between tobacco cigarette use and subsequent marijuana use. In fact, a systematic review of the literature published by Ramo and colleagues48 in 2012 showed that tobacco use among youths is strongly and independently associated with current and subsequent use of marijuana. Among 24 longitudinal studies included in the review, 70% of associations between tobacco and subsequent marijuana use were statistically significant, with odds ratios ranging from 1.6 to 8.6 for the increased likelihood of using marijuana in those that had used tobacco (vs those who had not) during adolescence and early adulthood.48
The finding of increased marijuana use with ENDS use in younger vs older youths is consistent with developmental assumptions that a younger, less-developed brain is more vulnerable to substance use and addiction.49 In fact, both nicotine and marijuana directly affect neural pathways involved with pleasure and reward and may increase the brain’s long-term sensitivity to other psychoactive substances and drug-seeking behaviors throughout adulthood.50 While tobacco and nicotine products are considered legal in most parts of the world, nicotine use, especially during adolescence, should be discouraged because of risks of several negative long-term outcomes, including a chronic decrease in attention and memorization capacity.10,51 Exposure to nonnicotine components contained in ENDS aerosols is also a concern. While the long-term health outcomes of using newer ENDS devices is not yet well understood, e-cigarette liquids contain several known toxins.4 Chronic exposure accruing over a lifetime for individuals who initiate use early is a particular concern. It is well established that the younger the age at onset of substance use, the higher the likelihood of developing a substance use disorder later in life.52,53 In this sense, these findings, which show a significant association between 2 psychoactive substances that have long-term deleterious effects on the brain, have important public health implications: addressing ENDS use and doing so early may be an effective way of delaying onset of marijuana use.
The 3 longitudinal studies included in this review suggest that ENDS use typically predates use of marijuana. While the number of longitudinal studies included in the meta-analysis was small, this finding yields high clinical relevance. In fact, recent surveys and epidemiological studies have shown that ENDS are often the first psychoactive substance used by youths, and based on epidemiological evidence, many of these youth would have been assessed as having never used nicotine or other substances.54 The use of ENDS may sensitize the reward and pleasure center of the brain and increase the odds of using other forms of nicotine and other psychoactive substances.5 While it is possible that youths who are substance naive and initiate substance use through ENDS would have gravitated toward other substances with the passage of time, the possibility of delaying onset of substance use by reducing use of ENDS in youths could have important benefits—notably by decreasing the burden of substance use on a population level.55
We found a stronger association between ENDS and marijuana use in youths with dual use of ENDS and other forms of tobacco than in youths with use of ENDS only. While ENDS were initially designed to help adults with chronic cigarette smoking habits quit smoking or use a less harmful alternative form of nicotine delivery, a recent systematic review of the literature has highlighted that, when used by adolescents, ENDS are associated with a significant increase in the odds of using cigarettes and other forms of tobacco.22 This association is both cross-sectional and longitudinal, whereby youth with ENDS-only use have an increased risk of using traditional cigarettes in the future.56 The concurrent use of several nicotine or tobacco products has not only been associated with higher rates of substance use and substance use disorders,57 poly–tobacco use has also been associated with increased risk of high-risk substance use behaviors in youth.58 While co-occurring mental health disorders are common and may be a factor,31 the effect of nicotine in individuals who are susceptible and have a still-developing brain should not be dismissed, and prevention and intervention efforts in youths should consider ENDS in the broader context of nicotine and tobacco use.
The subgroup analysis by region suggested that the association between ENDS use and marijuana use may be stronger in North American vs European countries. Marijuana use is much more common in North America, while cigarette use is more prevalent in most European countries59; this discordant epidemiology may be the basis of this finding, whereas youths in Europe may be less inclined to use marijuana whether they have used ENDS or not. In addition, large variations in public policies, laws surrounding sales (including legal age of purchase of ENDS and tobacco products), and taxation practices in North America and Europe may also contribute.15 Neither the European Union nor the US federal government has placed an excise tax on ENDS, although constituent member states can and do tax it at varying levels. While this falls beyond the scope of this review, it is likely that certain jurisdictions have already put in place successful protective policies and practices to limit the outcomes of ENDS use in youths. With further research, promising regional initiatives could be identified and replicated.
Finally, we conducted a subgroup analysis for studies published before 2017 vs in 2017 or later. The time separation with this method is imperfect, since most studies published in 2017 or later still used data that was collected before 2017, and there was some overlap in data collection dates between the 2 subgroups. However, more recent studies had a higher pooled AOR than older studies, which could be a reflection of the rapidly evolving landscape of ENDS products.60 In North America, the rise of companies manufacturing small, high-technology types of ENDS with refillable cartridges (pod mods) could have contributed to increases in rates of use of ENDS with high levels of nicotine.26 Given the susceptibility of the adolescent brain to psychoactive substances, such as nicotine, which may increase vulnerability to other substances as well, this shift in ENDS products over time may have played a role in the stronger association between ENDS and marijuana use found in more recent studies. Altogether, efforts to contain ENDS use should be mindful of rapidly changing products, which may have different effects on youths.
Limitations
This study had several limitations. First, all of the included studies were observational and adjusted for different sets of confounders. This could have led to overinflated odds ratios in the case of underadjusted models and could have contributed to the high level of heterogeneity seen between studies. Second, most included studies were cross-sectional and did not provide information about the temporal association between nicotine exposure through ENDS use and subsequent changes in marijuana use, although the 95% CIs for the AORs of the cross-sectional and longitudinal subgroups were overlapping. Conducting a new meta-analysis of longitudinal studies would be a useful next step, once a greater number of such studies become available. Third, to increase the number of included studies, we considered any use of marijuana, be it ever, in the past year, or currently or daily, to be a marijuana-positive outcome. This again could have contributed to the high level of heterogeneity found in this study and renders the clinical implications of the findings more difficult to interpret (ie, daily vs monthly use of marijuana use does not carry the same level of risk in youths). Fourth, although there were several studies from Europe and North America, no studies from Asia met criteria for inclusion in this meta-analysis, which limits the generalizability of the findings. Finally, there was a high level of heterogeneity between included studies (I2,94% for the pooled AOR). Nonetheless, owing to the observational design of the studies included in the meta-analysis, and since many of the studies used large, nationally representative samples or cohorts, we considered the risk of publication bias to be of lesser concern than if this meta-analysis had included primarily experimental studies.
Conclusions
To our knowledge, this study is the first meta-analysis to summarize the evidence to date about the association between ENDS use and marijuana use among youths. We found a significant increase in the odds of using marijuana in youths who had used ENDS in both cross-sectional and longitudinal studies. This study suggests that, in addition to potential harms of using ENDS alone and an increased risk of using other forms of nicotine or tobacco, ENDS use is significantly associated with use of at least 1 other addictive psychoactive substance: marijuana. These findings should be taken into account in the design of public policies aiming to restrict access to ENDS for minors. This study also opens the door to other similar meta-analyses looking at the association between ENDS use and use of alcohol or other drugs.
eMethods. Detailed Database Search Strategy
eFigure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Diagram of Study Selection
eFigure 2. Marijuana Use in Youth with e-Cigarette-only Use and Dual e-Cigarette and Tobacco Use in Individual Studies
References
- 1.Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the field: use of electronic cigarettes and any tobacco product among middle and high school students—United States, 2011-2018. MMWR Morb Mortal Wkly Rep. 2018;67(45):-. doi: 10.15585/mmwr.mm6745a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnston LD, Miech RA, O’malley PM, Bachman JG, Schulenberg JE, Patrick ME Monitoring the future national survey results on drug use, 1975-2018: overview, key findings on adolescent drug use. http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2018.pdf. Published 2019. Accessed February 11, 2019.
- 3.US Department of Health and Human Services E-cigarette use among youth and young adults: a report of the Surgeon General. 2016:298. https://e-cigarettes.surgeongeneral.gov/documents/2016_SGR_Full_Report_non-508.pdf. Accessed June 3, 2018.
- 4.Rubinstein ML, Delucchi K, Benowitz NL, Ramo DE. Adolescent exposure to toxic volatile organic chemicals from e-cigarettes. Pediatrics. 2018;141(4):e20173557. doi: 10.1542/peds.2017-3557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Curran KA, Burk T, Pitt PD, Middleman AB. Trends and substance use associations with e-cigarette use in US adolescents. Clin Pediatr (Phila). 2018;57(10):1191-1198. doi: 10.1177/0009922818769405 [DOI] [PubMed] [Google Scholar]
- 6.Dai H, Catley D, Richter KP, Goggin K, Ellerbeck EF. Electronic cigarettes and future marijuana use: a longitudinal study. Pediatrics. 2018;141(5):e20173787. doi: 10.1542/peds.2017-3787 [DOI] [PubMed] [Google Scholar]
- 7.Audrain-McGovern J, Stone MD, Barrington-Trimis J, Unger JB, Leventhal AM. Adolescent e-cigarette, hookah, and conventional cigarette use and subsequent marijuana use. Pediatrics. 2018;142(3):e20173616. doi: 10.1542/peds.2017-3616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality The TEDS report: age of substance use initiation among treatment admissions aged 18 to 30. https://www.samhsa.gov/data/sites/default/files/WebFiles_TEDS_SR142_AgeatInit_07-10-14/TEDS-SR142-AgeatInit-2014.pdf. Published 2017. Accessed November 10, 2017. [PubMed]
- 9.Squeglia LM, Gray KM. Alcohol and drug use and the developing brain. Curr Psychiatry Rep. 2016;18(5):46. doi: 10.1007/s11920-016-0689-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goriounova NA, Mansvelder HD. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb Perspect Med. 2012;2(12):a012120. doi: 10.1101/cshperspect.a012120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goriounova NA, Mansvelder HD. Nicotine exposure during adolescence alters the rules for prefrontal cortical synaptic plasticity during adulthood. Front Synaptic Neurosci. 2012;4:3. doi: 10.3389/fnsyn.2012.00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Volkow ND, Swanson JM, Evins AE, et al. . Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: a review. JAMA Psychiatry. 2016;73(3):292-297. doi: 10.1001/jamapsychiatry.2015.3278 [DOI] [PubMed] [Google Scholar]
- 13.Meier MH, Caspi A, Ambler A, et al. . Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci U S A. 2012;109(40):E2657-E2664. doi: 10.1073/pnas.1206820109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bagot KS, Milin R, Kaminer Y. Adolescent initiation of cannabis use and early-onset psychosis. Subst Abus. 2015;36(4):524-533. doi: 10.1080/08897077.2014.995332 [DOI] [PubMed] [Google Scholar]
- 15.Kennedy RD, Awopegba A, De León E, Cohen JE. Global approaches to regulating electronic cigarettes. Tob Control. 2017;26(4):440-445. doi: 10.1136/tobaccocontrol-2016-053179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chadi N, Weitzman ER, Levy S. understanding the impact of national and state medical marijuana policies on adolescents. Curr Addict Rep. 2018;5(2):93-101. doi: 10.1007/s40429-018-0191-1 [DOI] [Google Scholar]
- 17.Cerdá M, Wall M, Feng T, et al. . Association of state recreational marijuana laws with adolescent marijuana use. JAMA Pediatr. 2017;171(2):142-149. doi: 10.1001/jamapediatrics.2016.3624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stroup DF, Berlin JA, Morton SC, et al. . Meta-analysis of observational studies in epidemiology: a proposal for reporting: Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008-2012. doi: 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Academies of Sciences Engineering and Medicine Public health consequences of e-cigarettes: health and medicine division. http://nationalacademies.org/hmd/Reports/2018/public-health-consequences-of-e-cigarettes.aspx. Published 2018. Accessed June 2, 2018.
- 21.Glasser AM, Collins L, Pearson JL, et al. . overview of electronic nicotine delivery systems: a systematic review. Am J Prev Med. 2017;52(2):e33-e66. doi: 10.1016/j.amepre.2016.10.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soneji S, Barrington-Trimis JL, Wills TA, et al. . Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788-797. doi: 10.1001/jamapediatrics.2017.1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dunbar MS, Tucker JS, Ewing BA, et al. . Frequency of e-cigarette use, health status, and risk and protective health behaviors in adolescents. J Addict Med. 2017;11(1):55-62. doi: 10.1097/ADM.0000000000000272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Published 2013. Accessed December 18, 2018.
- 25.Staff J, Schulenberg JE, Maslowsky J, et al. . Substance use changes and social role transitions: proximal developmental effects on ongoing trajectories from late adolescence through early adulthood. Dev Psychopathol. 2010;22(4):917-932. doi: 10.1017/S0954579410000544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barrington-Trimis JL, Leventhal AM. Adolescents’ use of “pod mod” e-cigarettes—urgent concerns. N Engl J Med. 2018;379(12):1099-1102. doi: 10.1056/NEJMp1805758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rose A, Filion KB, Eisenberg MJ, Franck C. Electronic cigarettes: a comparison of national regulatory approaches. Can J Public Health. 2015;106(6):e450-e453. doi: 10.17269/CJPH.106.5043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Demissie Z, Everett Jones S, Clayton HB, King BA. Adolescent risk behaviors and use of electronic vapor products and cigarettes. Pediatrics. 2017;139(2):e20162921. doi: 10.1542/peds.2016-2921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McCabe SE, West BT, McCabe VV. Associations between early onset of e-cigarette use and cigarette smoking and other substance use among US adolescents: a national study. Nicotine Tob Res. 2018;20(8):923-930. doi: 10.1093/ntr/ntx231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Silveira ML, Conway KP, Green VR, et al. . Longitudinal associations between youth tobacco and substance use in waves 1 and 2 of the Population Assessment of Tobacco and Health (PATH) study. Drug Alcohol Depend. 2018;191:25-36. doi: 10.1016/j.drugalcdep.2018.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCabe SE, West BT, Veliz P, Boyd CJ. E-cigarette use, cigarette smoking, dual use, and problem behaviors among U.S. adolescents: results from a national survey. J Adolesc Health. 2017;61(2):155-162. doi: 10.1016/j.jadohealth.2017.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Azagba S. E-cigarette use, dual use of e-cigarettes and tobacco cigarettes, and frequency of cannabis use among high school students. Addict Behav. 2018;79:166-170. doi: 10.1016/j.addbeh.2017.12.028 [DOI] [PubMed] [Google Scholar]
- 33.Bluestein M. Exploring associations between the use of psychoactive substances and e-cigarettes in a nationally representative sample of young adults. https://digitalcommons.library.tmc.edu/dissertations/AAI10275505/. Published January 2017. Accessed December 17, 2018.
- 34.Camenga DR, Kong G, Cavallo DA, et al. . Alternate tobacco product and drug use among adolescents who use electronic cigarettes, cigarettes only, and never smokers. J Adolesc Health. 2014;55(4):588-591. doi: 10.1016/j.jadohealth.2014.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cohn A, Villanti A, Richardson A, et al. . The association between alcohol, marijuana use, and new and emerging tobacco products in a young adult population. Addict Behav. 2015;48:79-88. doi: 10.1016/j.addbeh.2015.02.005 [DOI] [PubMed] [Google Scholar]
- 36.Conway KP, Green VR, Kasza KA, et al. . Co-occurrence of tobacco product use, substance use, and mental health problems among youth: findings from wave 1 (2013-2014) of the Population Assessment of Tobacco and Health (PATH) study. Addict Behav. 2018;76:208-217. doi: 10.1016/j.addbeh.2017.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dautzenberg B, Berlin I, Tanguy M-L, Rieu N, Birkui P. Factors associated with experimentation of electronic cigarettes among Parisian teenagers in 2013. Tob Induc Dis. 2015;13:40. doi: 10.1186/s12971-015-0065-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fotiou A, Kanavou E, Stavrou M, Richardson C, Kokkevi A. Prevalence and correlates of electronic cigarette use among adolescents in Greece: a preliminary cross-sectional analysis of nationwide survey data. Addict Behav. 2015;51:88-92. doi: 10.1016/j.addbeh.2015.07.021 [DOI] [PubMed] [Google Scholar]
- 39.Kong G, Idrisov B, Galimov A, Masagutov R, Sussman S. Electronic cigarette use among adolescents in the Russian Federation. Subst Use Misuse. 2017;52(3):332-339. doi: 10.1080/10826084.2016.1225766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kristjansson AL, Mann MJ, Smith ML. Prevalence of substance use among middle school-aged e-cigarette users compared with cigarette smokers, nonusers, and dual users: Implications for primary prevention. Subst Abus. 2017;38(4):473-476. doi: 10.1080/08897077.2017.1343218 [DOI] [PubMed] [Google Scholar]
- 41.Milicic S, Leatherdale ST. The associations between e-cigarettes and binge drinking, marijuana use, and energy drinks mixed with alcohol. J Adolesc Health. 2017;60(3):320-327. doi: 10.1016/j.jadohealth.2016.10.011 [DOI] [PubMed] [Google Scholar]
- 42.Saddleson ML, Kozlowski LT, Giovino GA, et al. . Risky behaviors, e-cigarette use and susceptibility of use among college students. Drug Alcohol Depend. 2015;149:25-30. doi: 10.1016/j.drugalcdep.2015.01.001 [DOI] [PubMed] [Google Scholar]
- 43.Sutfin EL, McCoy TP, Morrell HER, Hoeppner BB, Wolfson M. Electronic cigarette use by college students. Drug Alcohol Depend. 2013;131(3):214-221. doi: 10.1016/j.drugalcdep.2013.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tavolacci M-P, Vasiliu A, Romo L, Kotbagi G, Kern L, Ladner J. Patterns of electronic cigarette use in current and ever users among college students in France: a cross-sectional study. BMJ Open. 2016;6(5):e011344. doi: 10.1136/bmjopen-2016-011344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Unger JB, Soto DW, Leventhal A. E-cigarette use and subsequent cigarette and marijuana use among Hispanic young adults. Drug Alcohol Depend. 2016;163:261-264. doi: 10.1016/j.drugalcdep.2016.04.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.White J, Li J, Newcombe R, Walton D. Tripling use of electronic cigarettes among New Zealand adolescents between 2012 and 2014. J Adolesc Health. 2015;56(5):522-528. doi: 10.1016/j.jadohealth.2015.01.022 [DOI] [PubMed] [Google Scholar]
- 47.Williams T, White V. What factors are associated with electronic cigarette, shisha-tobacco and conventional cigarette use? findings from a cross-sectional survey of Australian adolescents? Subst Use Misuse. 2018;53(9):1433-1443. doi: 10.1080/10826084.2017.1411367 [DOI] [PubMed] [Google Scholar]
- 48.Ramo DE, Liu H, Prochaska JJ. Tobacco and marijuana use among adolescents and young adults: a systematic review of their co-use. Clin Psychol Rev. 2012;32(2):105-121. doi: 10.1016/j.cpr.2011.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gray KM, Squeglia LM. Research review: what have we learned about adolescent substance use? J Child Psychol Psychiatry. 2018;59(6):618-627. doi: 10.1111/jcpp.12783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Casey BJ, Jones RM. Neurobiology of the adolescent brain and behavior: implications for substance use disorders. J Am Acad Child Adolesc Psychiatry. 2010;49(12):1189-1201. doi: 10.1016/j.jaac.2010.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Campos MW, Serebrisky D, Castaldelli-Maia JM. Smoking and cognition. Curr Drug Abuse Rev. 2016;9(2):76-79. doi: 10.2174/1874473709666160803101633 [DOI] [PubMed] [Google Scholar]
- 52.Moss HB, Chen CM, Yi HY. Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug Alcohol Depend. 2014;136:51-62. doi: 10.1016/j.drugalcdep.2013.12.011 [DOI] [PubMed] [Google Scholar]
- 53.Hingson RW, Heeren T, Winter MR. Age at drinking onset and alcohol dependence: age at onset, duration, and severity. Arch Pediatr Adolesc Med. 2006;160(7):739-746. doi: 10.1001/archpedi.160.7.739 [DOI] [PubMed] [Google Scholar]
- 54.Dutra LM, Glantz SA. E-cigarettes and national adolescent cigarette use: 2004-2014. Pediatrics. 2017;139(2):e20162450. doi: 10.1542/peds.2016-2450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Levy SJ, Williams JF; Committee on Substance Use and Prevention . Substance use screening, brief intervention, and referral to treatment. Pediatrics. 2016;138(1):e20161211. doi: 10.1542/peds.2016-1211 [DOI] [PubMed] [Google Scholar]
- 56.Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, Williams RJ. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob Control. 2017;26(1):34-39. doi: 10.1136/tobaccocontrol-2015-052705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cavazos-Rehg PA, Krauss MJ, Spitznagel EL, Grucza RA, Bierut LJ. Youth tobacco use type and associations with substance use disorders. Addiction. 2014;109(8):1371-1380. doi: 10.1111/add.12567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sutter ME, Everhart RS, Miadich S, Rudy AK, Nasim A, Cobb CO. Patterns and profiles of adolescent tobacco users: results from the Virginia Youth survey. Nicotine Tob Res. 2018;20(suppl_1):S39-S47. doi: 10.1093/ntr/nty032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.de Looze M, Ter Bogt TFM, Raaijmakers QAW, Pickett W, Kuntsche E, Vollebergh WAM. Cross-national evidence for the clustering and psychosocial correlates of adolescent risk behaviours in 27 countries. Eur J Public Health. 2015;25(1):50-56. doi: 10.1093/eurpub/cku083 [DOI] [PubMed] [Google Scholar]
- 60.Padon AA, Maloney EK, Cappella JN. Youth-targeted e-cigarette marketing in the US. Tob Regul Sci. 2017;3(1):95-101. doi: 10.18001/TRS.3.1.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Detailed Database Search Strategy
eFigure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Diagram of Study Selection
eFigure 2. Marijuana Use in Youth with e-Cigarette-only Use and Dual e-Cigarette and Tobacco Use in Individual Studies