Abstract
Spermatogonial stem cells (SSCs) are the most primitive spermatogonia in the testis and have an essential role to maintain highly productive spermatogenesis by self-renewal and continuous generation of daughter spermatogonia that differentiate into spermatozoa, transmitting genetic information to the next generation. Since the 1950s, many experimental methods, including histology, immunostaining, whole-mount analyses, and pulse-chase labeling, had been used in attempts to identify SSCs, but without success. In 1994, a spermatogonial transplantation method was reported that established a quantitative functional assay to identify SSCs by evaluating their ability to both self-renew and differentiate to spermatozoa. The system was originally developed using mice and subsequently extended to nonrodents, including domestic animals and humans. Availability of the functional assay for SSCs has made it possible to develop culture systems for their ex vivo expansion, which dramatically advanced germ cell biology and allowed medical and agricultural applications. In coming years, SSCs will be increasingly used to understand their regulation, as well as in germline modification, including gene correction, enhancement of male fertility, and conversion of somatic cells to biologically competent male germline cells.
Keywords: spermatogonial stem cell, germline stem cell, germ cell transplantation, germline modification, transgenesis, spermatogonium, stem cell culture, stem cell niche, infertility treatment, gene therapy, cryopreservation, transdifferentiation
Introduction
Spermatogenesis plays a pivotal role in the continuity of the male germline by producing haploid spermatozoa that fertilize eggs and eventually produce progeny for the next generation. Mammalian spermatogenesis is a highly productive and coordinated process, which is subdivided into three successive phases based on functional considerations: the proliferative phase (spermatogonia), in which cells undergo continuous, successive divisions, the meiotic phase (spermatocytes) in which genetic material is recombined, and the differentiation or spermiogenesis phase, in which spermatids transform into spermatozoa. The high productivity of spermatogenesis relies primarily on the proliferation of spermatogonia, which occurs in the mitotic spermatogonial compartment of the seminiferous tubule [1]. However, the life-long maintenance of spermatogenesis is dependent on the biological competence of the extremely rare spermatogonial stem cells (SSCs), which are capable of self-renewal and production of daughter cells to generate terminally differentiated cells, spermatozoa. Since the 1950s, a tremendous effort with rodent models, using histological approaches, whole-mount analyses, and isotope pulse-chase monitoring, had been made to understand SSCs [2], but a means to unequivocally identify SSCs was the major hurdle. SSCs were believed to be the least differentiated spermatogonia, called type Asingle (As) spermatogonia, which remain as single cells on the basement membrane of the seminiferous tubule. Germ cells, including spermatogonia, undergo incomplete cell division during differentiation, and when As spermatogonia undergo differentiation, they generate type Apaired (Apr) spermatogonia, which are interconnected by an intercellular bridge. If they remain in the undifferentiated state, As spermatogonia generate two As spermatogonia without an intercellular bridge. This mitotic pattern is called a symmetric self-renewal division. Subsequent cell divisions of the Apr spermatogonia generate Aaligned-4, Aaligned-8, and Aaligned-16 (Aal), which will differentiate to type A1 spermatogonia. The As, Apr, and Aal spermatogonia are called undifferentiated spermatogonia, and the undifferentiated spermatogonia population is heterogeneous. The As spermatogonum has been designated an SSC, and their number is calculated to be as low as 0.03% of total adult testis cells [3]. The small number of SSCs and the inability to unequivocally identify them has greatly hindered our ability to understand the biology of SSCs, the complexity of spermatogenesis, and regulation of the male germline. In this chapter, we provide an overview of the advancement in our knowledge regarding SSCs and the male germline, since the development of the spermatogonial transplantation method in 1994 [4, 5], which was a major breakthrough for basic research on SSCs, for clinical applications and in agriculture.
Spermatogonial stem cell transplantation
Development of spermatogonial stem cell transplantation method
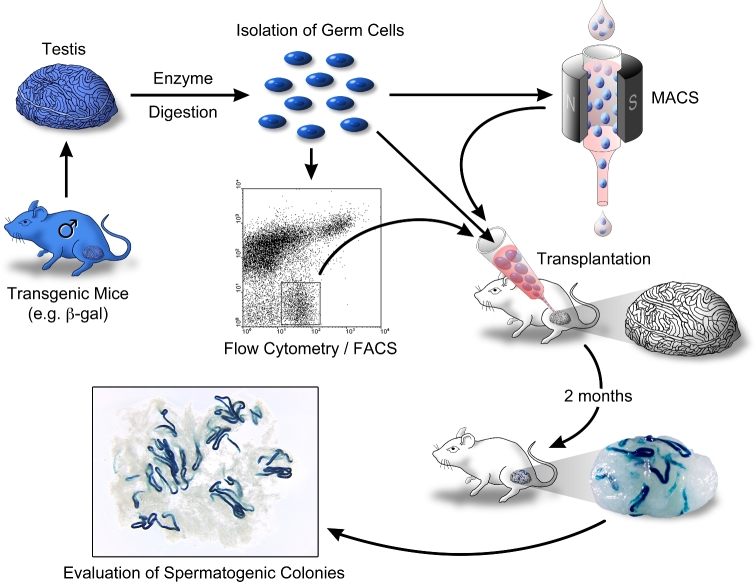
A technique for microinjection of donor germ cells into seminiferous tubules of infertile recipient males was first reported using mice in 1994 to identify SSCs by their biological function [4, 5]. In the initial approach, testis cell suspensions from transgenic mice expressing a reporter gene, lacZ encoding β-galactosidase, were used to unequivocally identify donor cells in recipient testes after transplantation by staining with X-gal (5-Bromo-4-chloro-3-indolyl-β-D-galactoside) (Figure 1). When donor testicular cells from fertile males are injected into the lumen of the seminiferous tubules of an infertile recipient male, some donor germ cells migrate toward the seminiferous tubule periphery passing through the tight junction of Sertoli cells, which form the blood–testis barrier. Because spermatogenesis is not present in the recipient males, donor germ cells can more readily penetrate the epithelial layer of Sertoli cells and reach the basal lamina surrounded by the peritubular myoid cells. Two types of infertile mice can be used for recipients. One type can be prepared by injection of Busulfan, an alkylating agent used for cancer chemotherapy, which will eliminate endogenous germ cells, including SSCs. The second type of recipients are specific mutant mice lacking spermatogenesis, such as White-spotting (W) mouse strains that have mutations in the Kit gene that encodes a receptor tyrosine kinase responsible for proliferation of primordial germ cells (PGCs) in the fetus and spermatogonia in postnatal testes [4]. In addition, immature testes before forming the blood–testis barrier of Sertoli cells, which occurs between 10 and 16 days postpartum in the mouse, are excellent recipients resulting in a significant improvement of the colonization efficiency [6, 7].
Figure 1.
Outline of spermatogonial transplantation method and quantitative assay for SSCs. Single-cell suspension prepared from testes of transgenic mice expressing a reporter gene (e.g., β-galactosidase) by enzymatic digestion is injected into the seminiferous tubules of an infertile recipient mouse. Cells from in vitro culture or cells fractionated by FACS or MACS can be used for a donor cell population. Two months after transplantation, donor-derived spermatogenesis can be detected in the recipient testis as blue colonies. Because each colony of spermatogenesis is developed from a single SSC, the number of colonies represents the number of SSCs in the donor cell suspension. The length of each colony demonstrates the degree of SSC expansion. Modified from [199].
After microinjection into infertile recipient testes, the donor germ cells colonize the basement membrane of the recipient seminiferous tubules and regenerate spermatogenesis. Donor cell-derived spermatozoa appear by 2 months after transplantation. The donor-derived spermatozoa are morphologically normal and are able to fertilize eggs, resulting in production of fertile progeny carrying the donor male haplotype. This proves that donor-derived spermatozoa are functionally normal [4]. Furthermore, the reconstituted spermatogenesis continues during the remaining life of the recipient male. The spermatogenesis-reconstituting cells fulfill the biological criteria for a stem cell, both the ability to self-renew and differentiate into the appropriate terminal cell type; therefore, the spermatogonial transplantation technique has made it possible to unequivocally identify SSCs in any donor-cell population based on their biological function and established the second functional assay for stem cells following the previously established bone marrow transplantation system for hematopoietic stem cells (HSCs) [8].
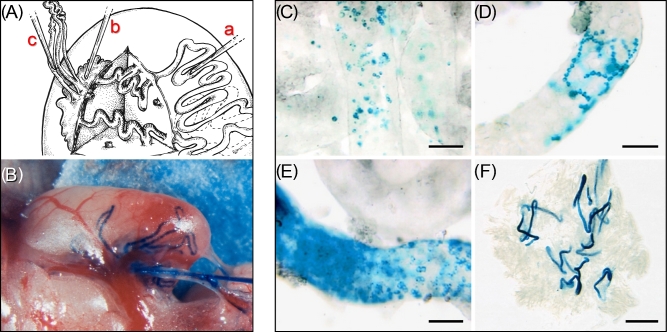
Distributing donor cells to many areas of seminiferous tubules is critical to maximize colonization efficiency of transplanted SSCs. Because all seminiferous tubules access the rete testis, microinjecting donor cells into the rete testis followed by filling of many seminiferous tubules is the most efficient way to achieve this goal. Three ways to inject donor cells have been developed [9]. The first method is to inject donor cells directly into the seminiferous tubule using a micropipette, which was the first method reported [5] (Figure 2Aa). Donor germ cells introduced are forced into the rete testis from the injected tubule and can then enter other seminiferous tubules. The second method is to insert a micropipette directly into the rete testis and inject donor cells, which fill the rete and flow into the seminiferous tubules (Figure 2Ab). When injection pressure is increased too rapidly or is too high, some leakage around the insertion site of the rete testis may occur. The third method is to insert a micropipette into one of the efferent ducts and thread it into the rete testis in a retrograde direction (Figure 2Ac and B). This method is the most accurate to control the injection volume because less cell suspension can leak from the insertion site of the micropipette, and seminiferous tubule filling of 70 to 90% can be achieved routinely.
Figure 2.
Spermatogonial transplantation methods and regeneration process of donor-derived spermatogenesis. (A) Three cell-injection methods into a recipient testis are shown. The micropipette can be inserted directly into the seminiferous tubules (a), into the rete testis (b), or into an efferent duct (c). (B) A micropipette was inserted through an efferent duct into rete testis. Seminiferous tubules of a recipient testis were beginning to fill by injecting donor cells with dye (trypan blue). Modified from [9]. (C–F) Regeneration process of donor-derived spermatogenesis from transplanted SSCs expressing β-galactosidase. (C) One week after transplantation, some blue donor cells were observed on the basement membrane. (D) Two weeks after transplantation, spreading interconnected spermatogonia were observed. (E) Two months after transplantation, dark blue colonies with complete spermatogenesis were identified. Donor-derived spermatogenic colonies continued to grow at the extremities. (F) Donor SSCs-derived spermatogenic colonies were identified as blue stretches of tubules under lower magnification by 2 months after transplantation. Each blue colony in the recipient testis is developed from a single donor SSCs. The testes were stained with X-gal. Scale bars: (C–E) 100 μm, (F) 2 mm. Modified from [10].
Regenerative spermatogenesis from spermatogonial stem cells
The regeneration process of donor-derived spermatogenesis from transplanted SSCs has been investigated using transgenic mice expressing the β-galactosidase reporter gene [10]. During the first week following donor cell transplantation, some donor germ cells reach and colonize the basement membrane (Figure 2C). After 2 weeks, spreading interconnected spermatogonia appear, indicating the donor cells begin proliferating laterally on the basement membrane (Figure 2D). About 1 month following transplantation, donor-derived spermatocytes appear in the adluminal compartment of the seminiferous tubules. By 2 months after transplantation, the recipient seminiferous tubules are filled by donor germ cells, and donor spermatozoa can be identified. The complete spermatogenesis established by donor cells forms identifiable colonies, and the area of donor-derived spermatogenesis continues to extend laterally along recipient seminiferous tubules (Figure 2E and F). Although the process of spermatogenesis from type A spermatogonia to mature spermatozoa in mice is 35 days [1], nearly twice as long as necessary to differentiate into donor spermatozoa following transplantation [10]. The reason for the difference of 35 days versus 2 months remains unclear, but the migration and colonization processes from the lumen to the basement membrane are likely involved in the time lag to produce mature spermatozoa following transplantation. Furthermore, the time required for differentiation from an SSC to A1 spermatogonium is not known and not counted in the 35 days; therefore, this differentiation time may account for a significant part of the additional 1 month for transplanted SSCs to produce spermatozoa.
Quantitative functional assay for spermatogonial stem cells
Controlling the injection volume of a donor cell suspension transplanted to a recipient testis has made it possible to establish a quantitative analysis of SSCs. When β-galactosidase-expressing SSCs are transplanted, donor-derived spermatogenesis can be unequivocally identified as blue colonies after staining with X-gal in the recipient testes 2 months after transplantation (Figure 1). These spermatogenic colonies are each derived from a single donor cell [11–13], and the colony number does not change from 1–4 months, whereas the length of colonies increases [10]. Thus, while the number of blue colonies represents the number of SSCs, which successfully colonized recipient testes, in donor cell suspensions, the area of blue colonies represents the proliferative ability of each SSC colonized, both of which can be quantified by an imaging analysis [11]. In addition to β-galactosidase, any visible reporter gene product, such as green fluorescent protein (GFP) or other fluorescent proteins, can be used to identify spermatogenic colonies derived from donor SSCs in recipient testes.
In a previous whole mount analysis of seminiferous tubules, the estimated quantity of As spermatogonia was 0.03% of all germ cells in an adult testis [3]. If all As spermatogonia are considered SSCs, the SSC number in an adult mouse testis was calculated to be approximately 35 000. Using the estimated number, the colonization efficiency of SSCs in adult recipient testes is 4.25% (functional value (colony number)/SSC number from morphological readout) [14]. On the other hand, the colonization efficiency of SSCs based on the transplantation assay has been estimated to be approximately 12.5% (functional value/SSC number from functional readout), and the functional SSC number estimated to be 3000, which represents 0.01% of all seminiferous tubule cells [15]. The functional assessment of SSC number in the adult testis suggests that all As spermatogonia are not functional SSCs that are able to colonize the basement membrane and regenerate long-term spermatogenesis; therefore, the 4.25% value likely underestimates the colonization efficiency, and the calculation using this efficiency overestimates the absolute number of total SSCs. The reason for the low colonization efficiency following transplantation is not clear, but spontaneous differentiation and apoptosis before reaching the basal lamina and the necessity to migrate through the blood–testis barrier between Sertoli cells in the opposite direction of normal spermatogenesis are possible contributing reasons. Although the molecular mechanism of the homing process of donor SSCs through the blood–testis barrier is largely unknown, several molecules have been tentatively identified as important, including integrin β1 (ITGB1), chemokine (C-X-C motif) ligand 12 (CXCL12), RAC1, and claudins (CLDNs) [16, 17]. Because the number of functional SSCs is extremely low in testes, improving the colonization efficiency of SSCs is important in many applications and therapeutic uses of SSCs, and elucidation of the mechanism of the homing process should increase colonization efficiency.
Functional assay for spermatogonial stem cell potential
The spermatogonial transplantation technique can be used to identify progenitor cells of SSCs. In mice, the first SSCs arise from a subpopulation of gonocytes, also called prospermatogonia, a few days after birth. Gonocytes are immature germ cells and follow PGCs in male germ cell development. By 11.5 dpc (days post coitum), PGCs migrate into the fetal gonad from the proximal epiblast, where they arise at 6.5 dpc, and differentiate to gonocytes at approximately 13.5 dpc. Subsequently, the gonocytes become mitotically inactive and remain in the center of the seminiferous tubules until birth. When neonatal and fetal gonocytes (14.5 dpc∼) are transplanted into seminiferous tubules of adult recipient testes, donor-derived spermatogenesis can be reconstituted [4, 6, 18, 19]. This indicates that the donor gonocytes can give rise to SSCs in the mature testis environment. Furthermore, not only PGCs, but also epiblast cells can reconstitute spermatogenesis when transplanted into immature W mouse testes before the blood–testis barrier of Sertoli cells is formed, and produced spermatozoa [20]. Although adult recipient testes were not able to support the conversion of PGCs to SSCs [19], the immature testis environment did enable the differentiation process from PGCs to SSCs, including proper epigenetic modification. Indeed, normal fertile progeny were produced by microinsemination using donor-derived spermatids or spermatozoa from as early as 8.5-dpc PGCs [20]. This indicates that the transplantation technique can be used for not only a functional assay to identify SSCs, but also for assessing developmental potential of earlier differentiation steps to produce SSCs, when immature recipient testes are used.
Derivation of functional spermatozoa from pluripotent stem cells in vitro is an attractive approach to study germ cell development and restore fertility. A series of stepwise studies of the developmental process from early embryonic cells to PGCs eventually lead to generation of functionally normal spermatozoa from embryonic stem (ES) cells and induced pluripotent stem (iPS) cells in the mouse [21, 22]. In this study, epiblast-like cells were initially generated from pluripotent stem cells, and then further differentiation to PGC-like cells was induced in culture. The PGC-like cells were transplanted into immature W mouse testes to generate SSCs. In the recipient testes, donor PGC-like cell-derived spermatogenesis occurred, and spermatozoa were collected from the recipient seminiferous tubules. Microinsemination using the spermatozoa successfully generated offspring transmitting the donor haplotype. The progeny were fertile, and no abnormalities were observed [22]. Although an in vitro differentiation system to produce functional haploid germ cells from PGC-like cells from pluripotent stem cells has been reported [23], the procedure is complex and the applicability to all mouse strains is not clear. Therefore, the transplantation procedure is still the most effective and reliable approach to generate functional spermatozoa from PGCs or PGC-like cells.
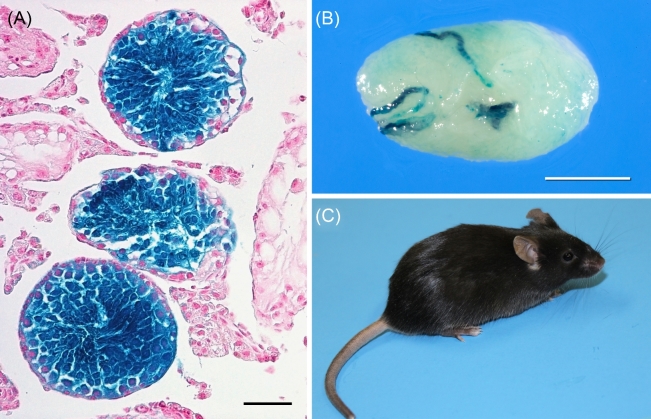
Cryopreservation of spermatogonial stem cells
The transplantation technique has demonstrated that SSCs can be cryopreserved for a long period in liquid nitrogen by a protocol commonly used for somatic cells [24]. SSCs thawed after a 14-year storage in liquid nitrogen retain the ability to regenerate spermatogenesis following transplantation, and the spermatozoa recovered generated normal progeny by microinsemination [25] (Figure 3). Because SSCs have the ability to self-renew and expand in number, cryopreservation of SSC-containing cell populations provides a potentially immortal lifespan for germlines of individual males. Although semen cryopreservation can be used to preserve the germline of certain economically, biologically, or scientifically valuable males, including livestock breeds or endangered animal species, semen cryopreservation represents a resource limited by the number of spermatozoa in the sample, and the cryopreservation protocols must be developed for each species. Cryopreservation methods for all mammalian SSCs examined are identical and basically the same procedures used for somatic cells [24, 26–31]; therefore, cryopreserving SSCs is more suitable for preservation of male germlines and the only method applicable for prepubertal males and in those species where specific techniques have not been developed for cryopreservation of spermatozoa.
Figure 3.
Restoration of spermatogenesis and generation of viable progeny by cryopreserved SSCs. (A) SSCs cryopreserved for 14 years reconstituted spermatogenesis in recipient testes. Cryopreserved donor SSCs were prepared from transgenic mice expressing β-galactosidase. (B) Colonies of spermatogenesis generated by cryopreserved SSCs in a recipient testis following transplantation. (C) Intracytoplasmic sperm injection (ICSI)-derived progeny using spermatozoa isolated from a recipient testis transplanted cryopreserved SSCs. Scale bars: (A) 50 μm, (B) 2 mm. Modified from [25].
A critically important aspect of SSC cryopreservation is that SSCs retain all the potential recombination possibilities during meiotic divisions, whereas the genetic variation of spermatozoa preserved is limited by the number of spermatozoa present in the sample. Furthermore, SSCs are able to self-renew in culture; thus, providing a potentially unlimited source of any individual male's genetic program and the variability contained within that program. Although long-term culture techniques are available for only a few species at present, techniques for many of the valuable species, including human, livestock, or endangered animals, are certain to be developed in the future.
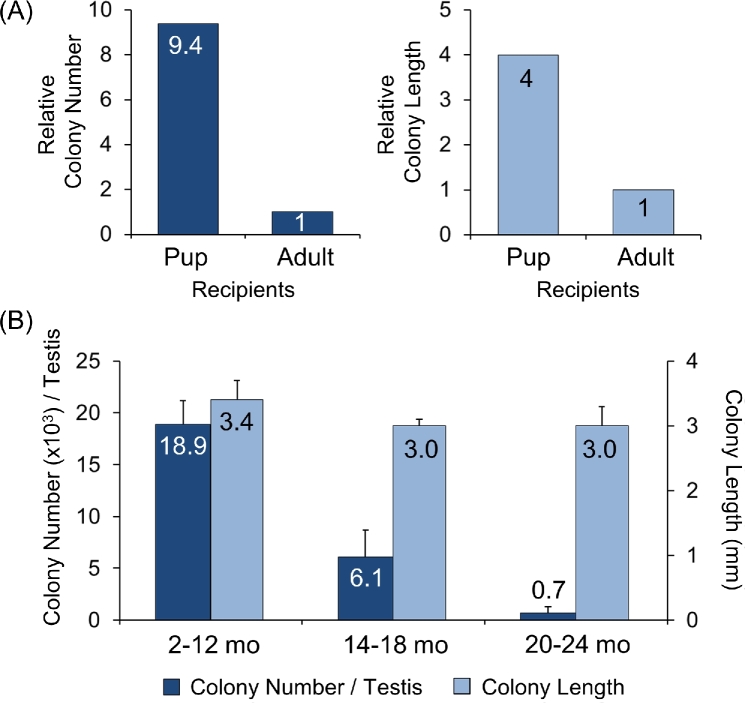
Spermatogonial stem cell niche
Self-renewal and differentiation of stem cells must be precisely regulated, and intrinsic and extrinsic factors are involved. The surrounding microenvironment of stem cells is called the stem cell niche, which provides extrinsic factors for maintaining stem cell competence [32]. The testis cell transplantation technique was originally developed for SSC transplantation and evaluation but is also valuable to investigate the biological function of the SSC niche. When SSCs from adult mice were transplanted into infertile pups and adult recipient testes, the number of spermatogenic colonies generated in pup testes was about 10 times greater than in adult testes [6]. In addition, the length of colonies generated was four times longer in pup testes than in adult testes (Figure 4A). These findings indicate that the SSC niche in pups is more accessible and supportive of transplanted SSCs than that in adults. Conversely, aged testes are less supportive of transplanted SSCs. Although some male mice can maintain spermatogenesis and are fertile until old age (over 2-years-old), the number of SSCs begins to decrease after the first year and is generally very low by 2 years of age. Although the SSC number in old males is low, the colony length generated by transplanted SSCs from young and old males is the same [33, 34] (Figure 4B). In contrast, SSCs from young males rarely colonized and regenerated spermatogenesis in atrophic aged testes of 2-year-old mice [34]. In addition, serial transplantation of SSCs into young recipient males demonstrated that the SSC number and the SSC activity of the transplanted SSCs did not change up to 32 months, during which time SSCs were serially transplanted eight times, every 3 months into young recipients [33]. These serial transplantation experiments indicate that the young SSC niche extends the competency of SSC beyond the normal life span of the mouse. Thus, aging of the SSC niche is the critical factor for maintenance of SSCs, and dysfunction of the SSC niche results in the decreased number of SSCs in old males.
Figure 4.
Developmental effect of the stem cell niche on SSC activity. Donor SSCs from adult testes were transplanted into pup or adult recipient mice. (A) The colony number and length of donor-derived spermatogenesis generated in recipient testes were analyzed 2 months after transplantation. The colony number and length in pup recipient testes were 9.4-fold and 4-fold greater than those in adult recipient testes, respectively [6]. This result indicated that the SSC niche in immature testes is more accessible and supportive for transplanted SSCs. (B) The colony number (SSC number) and the length of colony generated by SSCs from young to old donor males. The SSC number progressively decreased as the males aged, but the colony length from young and old males was not significantly different [33].
These experiments demonstrate that the transplantation assay can be used to evaluate the biological impact of the SSC niche in recipient testes. Components of the stem cell niche comprise neighboring cells, soluble factors, and extracellular matrices. The neighboring cells include Sertoli cells, peritubular myoid cells, Leydig cells, potentially other interstitial cells, and spermatogonia. In particular, Sertoli cells play a critical role in establishing the SSC niche, because they produce glial cell line-derived neurotrophic factor (GDNF) and fibroblast growth factor 2 (FGF2), which are the primary and secondary critical soluble factors for self-renewal and expansion of SSCs in vivo and in vitro [35–39]. Moreover, the number of Sertoli cells influences the number of niches accessible for colonization of transplanted SSCs in mice [40]. Following SSC transplantation, the number of spermatogenic colonies derived from donor SSCs was significantly increased 3-fold in recipient testes with an ∼50% increase in Sertoli cell numbers compared with normal recipient mice. In addition to GDNF and FGF2, insulin-like growth factor 1 (IGF1), CXCL12, and colony-stimulating factor 1 (CSF1) are candidate SSC niche factors, because they enhance expansion or survival of SSCs [37, 41–43]. Using the transplantation assay, it has been shown that CSF1 selectively increases the number of SSCs in vitro relative to the number of spermatogonia and other germ cells in the culture. It is important to identify the sources of these factors to fully understand the function of the niche. Like GDNF and FGF2, it has been demonstrated that IGF1 and CXCL12 are expressed in Sertoli cells [41, 42, 44]. Although CSF1 is expressed in Leydig cells and myoid cells [43], a recent study has shown that CSF1 is also produced from specialized peritubular macrophages in addition to vascular-associated macrophages and vascular smooth muscle cells [45]; thus, some cells expressing CSF1 are closely associated with the basement membrane and undifferentiated spermatogonia, including the SSC. Furthermore, in addition to Sertoli cells, it has been shown that peritubular myoid cells and vascular smooth muscle cells express GDNF [46, 47], and that premeiotic germ cells express FGF2 [48]. Based on the distribution of cell sources to produce these critical factors for SSC self-renewal, further investigation to clarify the roles of individual factors and functional interaction of each factor will be critical to fully understand the SSC niche.
Restoration of fertility by transplantation
There are a number of congenital disorders leading to impairment of spermatogenesis, which result in male infertility; however, the exact mechanism of many disorders is still unclear [49]. As seen in age-related degeneration of spermatogenesis, which can be caused by defects or dysfunction of either germ cells or their microenvironment, congenital disorders in spermatogenesis can also result from either germ cells or surrounding cells.
Spermatogonial transplantation can be used to elucidate the mechanism of genetic defects in spermatogenesis and to restore fertility in infertile males. The first proof of principal was from infertile mice with congenital mutations of the Steel (Sl) locus and W locus. The Sl locus encodes KIT-ligand (KITL) and the W locus encodes KIT. Several mutations in the Sl locus have been identified, and mice with the Sld mutation do not express the membrane-bound form of KITL on Sertoli cells and have no spermatogenesis. When testis cells from adult Sld mice were transplanted into wild-type recipients, donor-derived spermatogenesis was reconstituted [50]. This indicates the Sld germ cells including SSCs are normal, and stimulation by membrane-bound form of KITL is required for progression of spermatogenesis. Importantly, the SSC niche of Sld mice is functional, because the Sld SSCs were able to survive until puberty. KIT is expressed at a low level on undifferentiated spermatogonia, and the expression is induced in differentiating spermatogonia, which stimulates their proliferation and differentiation [51]. The W mutant mice have a congenital mutation of KIT and show impaired spermatogenesis. When testis cells from adult Wv mice, which have a defect in the tyrosine kinase domain, were transplanted into wild-type recipients, no donor-derived spermatogenesis was reconstituted, indicating that spermatogonial activation through KIT is necessary for progression of spermatogenesis. Conversely, when SSCs from wild-type mice were transplanted into the Wv mouse testes, complete spermatogenesis could be reconstituted [4]. These results indicated that the microenvironment for spermatogenesis in the Wv testis is normal. This was confirmed by transplantation of SSCs from Sld mutant mice into testes of Wv mutant mice, which resulted in normal spermatogenesis and produced fertile progeny from the donor Sld SSCs [52]. The transplantation assay between mutant and wild-type mice is a powerful approach to elucidate the mechanism of impaired spermatogenesis of mutant mice and the function of mutated genes, because the assay can clarify the self-renewal or differentiation ability of SSCs, as well as the function of their niche, or differentiation environments. Although species differences in gene function may exist, spermatogonial transplantation of mice provides a valuable model for studying male infertility in humans.
The transplantation of Sertoli cells into the seminiferous tubule can provide an approach to restore fertility in some infertile males. Sld mice are infertile due to a congenital defect of the membrane-bound KIT ligand on Sertoli cells, and transplantation of wild-type Sertoli cells into the seminiferous tubules of Sld mice initiates spermatogenesis [53]. In addition, transplantation of Sertoli cells from infertile W mice testes into infertile Sld recipient mice restored endogenous spermatogenesis and fertility, demonstrating that functional transplantation of Sertoli cells is feasible [54]. These studies demonstrate an alternative approach to restore fertility in infertile males by transplantation of the appropriate milieu for spermatogenesis. A major drawback of this approach is low colonization efficiency of donor Sertoli cells [53]. Because recipient Sertoli cells form intact seminiferous tubules with tight junctions, penetration of donor Sertoli cells into the epithelial sheets is likely inefficient; therefore, elimination of endogenous Sertoli cells could improve colonization efficiency of donor Sertoli cells [55]. Moreover, transplantation of xenogeneic Sertoli cells in addition to xenogeneic SSCs into immunocompromised mice would reconstitute the SSC niche for foreign species and their differentiation milieu resulting in reconstitution of spermatogenesis, which could be used for xenogeneic spermatogenesis in mice (see below).
Application of spermatogonial transplantation method to nonmouse systems
Spermatogonial stem cell transplantation in rats
The spermatogonial transplantation technique developed in the mouse has been extended to many other species, including rats, dogs, goats, sheep, pigs, cattle, and monkeys [56–66] (Table 1). The transplantation method for rats is essentially the same procedure as for mice. Donor germ cells are injected into infertile recipient rat testes through the efferent duct [57, 67, 68]. Recipient males can be prepared by injection of Busulfan to deplete endogenous germ cells, although the injection dose of Busulfan must be reduced for recipient rats because they are more sensitive to the drug than mice. There are no infertile rat strains with congenital mutations, like W mice, that are suitable for recipient males. After Busulfan treatment in rat, some endogenous spermatogenesis remains, but complete removal of endogenous germ cells is not necessary because residual endogenous spermatogenesis is helpful to maintain a healthy testicular microenvironment to enhance donor spermatogenesis [68]. When testicular cells from wild-type rats or transgenic rats expressing β-galactosidase were transplanted into recipient testes, progeny with the donor haplotype were produced in the recipient from the allogeneic combinations [67, 68].
Table 1.
Germ cell transplantation in various mammalian species.§
| Donor | Recipient | Colonization | Spermatogenesis | Offspring (transgenesis) |
|---|---|---|---|---|
| Intraspecies transplantation (syngeneic/allogeneic transplantation) | ||||
| Mouse | Mouse | + | + | + (+) |
| Rat | Rat | + | + | + (+) |
| Dog | Dog | + | +1,2 | – |
| Goat | Goat | + | +1 | + (–3) |
| Sheep | Sheep | + | +2 | + (–) |
| Pig | Pig | + | +1,2 | –3 |
| Cattle | Cattle | + | +2 | – |
| Macaque | Macaque | + | +1,2 | –3 |
| Interspecies transplantation (xenotransplantation) | ||||
| Mouse | Rat | + | + | – |
| Rat | Mouse | + | + | + |
| Hamster | Mouse | + | + | – |
| Rabbit | Mouse | + | – | – |
| Cat | Mouse | + | – | – |
| Dog | Mouse | + | – | – |
| Pig | Mouse | + | – | – |
| Cattle | Mouse | + | – | – |
| Horse | Mouse | + | – | – |
| Marmoset | Mouse | + | – | – |
| Baboon | Mouse | + | – | – |
| Macaque | Mouse | + | – | – |
| Human | Mouse | + | – | – |
§See text for references and detail.
1Generation of transgenic sperm by viral transduction to donor cells
2Generation of allogenic sperm
3Production of embryo with donor haplotype
Modification of spermatogonial transplantation method for nonrodent animals
The procedures for spermatogonial transplantation in nonrodents require modification because of the species-specific anatomy of the testis, particularly size and rete testis structure. While three methods to inject donor germ cells were developed in the mouse system, direct injection of donor SSCs into the rete testis by ultrasound guidance or surgical dissection has been shown to be a feasible approach in nonrodents, such as farm animals and companion animals [58, 59, 62, 63, 69, 70] (Table 1). For preparation of recipients, Busulfan injection or local irradiation of testes can be used in nonrodent species. Although appropriate injection timing and doses for Busulfan or irradiation protocols must be determined in each species, complete removal of endogenous germ cells is not essential, and like rats, residual endogenous spermatogenesis could help to maintain a healthy testicular microenvironment to enhance donor spermatogenesis. In addition, it has been shown that immature males before onset of spermatogenesis without pretreatment can be used as recipients in pig, goat, and cattle [58, 59, 71–73].
In nonrodent animals, transgenic strains that express a reporter gene are not available, and there are no spermatogenesis-impaired males with congenital mutations suitable for recipients. Therefore, proving regeneration of donor-derived spermatogenesis following transplantation is no easy task, because recipients can produce both donor- and recipient-derived spermatozoa. To demonstrate donor-derived sperm production in recipients, viral transduction was employed to genetically label donor SSCs. Using lentivirus vector or adeno-associated virus vector, transgenic sperm were successfully detected by genotyping of ejaculates in pig, goat, dog, and Rhesus monkey [66, 72, 74, 75]. It should be pointed out, however, that semen samples might contain somatic cells and the virus vector-mediated approach cannot rule out the possibility of transduction into endogenous germ cells or somatic cells by residual intact virus particles. Another approach to confirm donor-derived spermatogenesis is detection of donor-specific microsatellite DNA in semen samples, which has been employed in dog, sheep, cattle, and Rhesus monkey [61, 66, 71, 76]. Again, this approach alone cannot distinguish between DNA coming from somatic cells versus sperm of donor origin; therefore, production of embryo by in vitro fertilization or micro insemination using the sperm or, ideally, generation of progeny is evidently required for demonstration of complete donor-derived spermatogenesis. So far, progeny with donor SSC haplotype were successfully generated in goat and sheep [73, 76], while production of embryo using donor-derived sperm were demonstrated in pig, goat, and Rhesus monkey (Table 1). Taken together, although generation of progeny derived from donor SSCs is crucial to unequivocally demonstrate feasibility of spermatogonial transplantation in nonrodent animals, these studies demonstrate that spermatogonial transplantation techniques are applicable to nonrodent species.
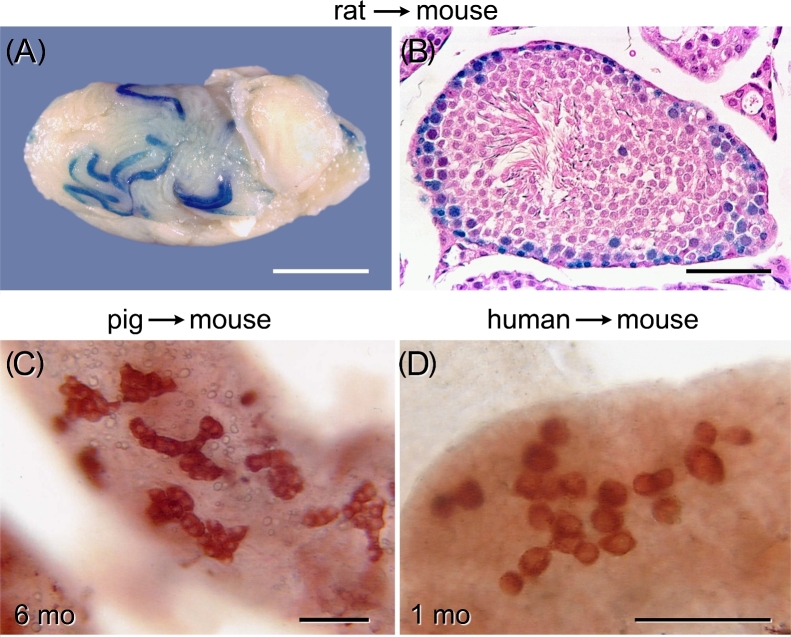
Xenotransplantation using immunocompromised mice
Autologous, syngeneic, and allogeneic donor/recipient combinations have been used in spermatogonial transplantation in intraspecies experimental settings [60, 62, 66, 77]. The first interspecies spermatogonial transplantation was performed injecting rat donor cells into mouse testes. Following transplantation of rat testis cells into the seminiferous tubules of immunocompromised mice treated with Busulfan, rat spermatogenesis was established in the recipient mouse testes [78] (Figure 5A and B). The rat spermatozoa, which developed in the recipient mouse testes, were morphologically and functionally normal, because the rat spermatozoa generated normal progeny by microinsemination into rat oocytes [79]. Conversely, mouse SSCs also colonized rat testes and reconstituted mouse spermatogenesis following transplantation [57, 67]. Complete spermatogenesis from transplanted SSCs has been obtained in other combinations between rodents, such as hamster-to-mouse [80]. This finding suggests that xenogeneic spermatogenesis could be reconstituted by transplantation of SSCs from a phylogenetically closely related species. Although the differentiation time from type A spermatogonia to mature spermatozoa is different among species (30–75 days in most mammals), the causal factors are not clear. The rat-to-mouse spermatogonial transplantation experiments demonstrated that the timing of germ cell differentiation during spermatogenesis is controlled by the germ cell genotype [78]. While development of type A spermatogonia to spermatozoa takes 35 days in mice, rats require 52 days [1]. Surprisingly, rat spermatogenesis in mouse seminiferous tubules progresses at the slower rate of rat spermatogenesis, although mouse Sertoli cells provide the support and nourishment for the rat germ cell differentiation, indicating that the endogenous program of the germ cells regulates species-specific timing of differentiation during spermatogenesis [81].
Figure 5.
Xenogeneic spermatogenesis and spermatogonial colonization in immunocompromised mouse testes. (A) Four months after transplantation of rat testis cells expressing β-galactosidase, rat spermatogenesis was regenerated in the recipient mouse testis (blue stretches of tubules). The testis was stained with X-gal. (B) Histological analysis of rat spermatogenesis in the immunocompromised mouse testis 4 months after transplantation. The testis was stained with X-gal plus hematoxylin and eosin. (C) Colonies of porcine spermatogonia were identified in recipient testes 6 months after transplantation of porcine testis cells. (D) Colonies of human spermatogonia were identified in recipient testes 1 month after transplantation of human testis cells. Donor germ cells in the seminiferous tubules were identified by species-specific antibody staining and appear red (C, D). Scale bars: (A) 2 mm, (B–D) 50 μm. Modified from [27, 29, 78].
To extend the xenogeneic spermatogonial transplantation approaches into mammalian species other than rodents, including rabbits, cats, dogs, pigs, cattle, horses, marmosets, baboon, macaques, and humans, germ cells from those species were transplanted into Busulfan-treated immunocompromised male mice [26–30, 82–84]. However, complete spermatogenesis from donor nonrodent SSCs did not develop (Table 1). Although differentiation of donor-derived spermatogonia did not occur in the recipient testes, colonies of donor germ cells from all nonrodent mammals examined were formed on the basal lamina (Figure 5C and D).The germ cell colonies persisted in the recipient testes for 1–12 months, indicating that the colonies contained germ cells that can survive and proliferate in the seminiferous tubules of immunocompromised mice for long periods [26–30, 82, 83]. The germ cell colonies formed in the recipient testes likely contain SSCs or undifferentiated spermatogonia due to their long-lived nature, and therefore the colony-forming spermatogonia in immunocompromised mice testes are often considered to represent SSCs. Because no functional assay for nonrodent SSCs has been yet developed, the xenogeneic transplantation system with immunocompromised mice has been used as a facultative method for assessment of nonrodent SSC activity, although interpretation of experimental results has to be cautious.
Assuming that the colony-forming cells are nonrodent SSCs, the xenogeneic transplantation experiments demonstrate that factors produced in the microenvironments of the colony-formed area, likely mouse SSC niche, are able to support survival and proliferation of SSCs from nonrodent species and the exogenous factors are conserved among mammalian species, while differentiation factors must be species-specific. When nonrodent xenogeneic SSCs are transplanted into mouse testes, Sertoli cell transplantation from the same species as the donor SSCs may overcome the block in differentiation of xenogeneic donor SSCs in the mouse microenvironment. Successful colonization of xenogeneic Sertoli cells would re-establish the necessary microenvironment for foreign species spermatogenesis in immunocompromised mice. Such reconstitution system can be used as a functional assay for nonrodent SSCs. At present, the SSC characteristics of nonrodent mammals are largely unknown because there is no functional assay to unequivocally identify them. Therefore, it is extremely important to develop functional assays for nonrodent SSCs in which both self-renewal and differentiation can be evaluated, which will allow a definitive conclusion on whether the colony-forming cells in the mouse testes are nonrodent SSCs.
Identity of spermatogonial stem cells
The number of SSC in the seminiferous tubules of adult mouse testes is only 0.01% [15]. Therefore, identification of the phenotype of SSCs is critical to investigate SSCs at the single-cell level in the context of tissue sections or whole mount analyses. Several methods to enrich SSCs from postnatal testes were developed, including differential plating, density-gradient centrifugation, experimental surgical cryptorchidism, and antibody-based selection [18, 50, 85]. Among the methods for antibody-based selection to isolate particular subpopulations from a mixed cell population, fluorescence activated cell sorting (FACS) has proved to be the most precise to identify stem cell populations from a variety of tissues [86]. An approach using FACS together with a functional transplantation assay was initially developed to identify HSCs. After considerable effort, the unique cell surface phenotype of murine HSCs was successfully determined, although mouse HSCs are less than 0.01% of the cells in bone marrow [87]. Utilizing a similar experimental approach, the cell surface phenotype of SSCs in mice and rats was determined. When the testicular cell population of isolated testes is divided based on expression of cell surface molecules by flow cytometric analysis, each fraction can be isolated by FACS and subjected to the spermatogonial transplantation assay. Two months after transplantation of each cell fraction, recipient testes are analyzed to count donor-derived spermatogenic colonies (Figure 1). The number of spermatogenic colonies generated by different cell populations indicates the number of SSCs in that population of cells. By repeating this process, the antigenic profile of SSCs in mice has been determined to be integrin α6 (ITGA6)+ ITGB1+ thymus cell antigen 1 (THY1)+ CD9+ GDNF family receptor α1 (GFRA1)+ epithelial cell adhesion molecule (EPCAM)+ CD24+ E-cadherin (CDH1)+ melanoma cell adhesion molecule (MCAM)+ KIT− major histocompatibility complex class I (MHC-I)− [85, 88–92]. A combination of multiple cell surface markers can identify a uniform cell population of undifferentiated spermatogonia enriched for SSCs [90]. While unfractionated adult testis cells generated 0.8–1.6 colonies per 105 cells transplanted, the THY1+ ITGA6+ KIT− MHC-I− cells isolated from cryptorchid testes generated approximately 350 colonies [18, 90], indicating that the THY1+ ITGA6+ KIT− MHC-I− cell population has a 300-fold higher SSC concentration than unfractionated adult testis cells. Accurate determination of the antigenic profile of SSC-enriched cell populations by FACS lead to subsequent development of simpler and quicker methods to enrich SSCs, such as magnetic activated cell sorting (MACS) [18, 93]. Other than antibody staining for cell surface molecules, FACS can be used for cell fractionation based on cellular activity, such as efflux pump activity, mitochondrial activity, cell-cycle, and intracellular enzymatic activity, which all have been used for HSC identification [90, 94–97]. Fractionation by these parameters is useful for nonrodent and nonhuman animals, because the availability of antibodies for those species is limited.
To identify SSC-specific gene expression, transgenic mice in which a reporter gene, such as GFP, or a site-specific recombinase, such as Cre, is inserted downstream of the promoter of a gene of interest, have been used. Several genes expressed in undifferentiated spermatogonia, including Pou5f1 (Oct-3/4), Neurogenin 3 (Ngn3), Nanos2, inhibitor of DNA binding 4 (Id4), Bmi1, Pax7, and telomerase reverse transcriptase (Tert) have been investigated [98–105]. Following identification of genetically marked cells in the testes by flow cytometry, the cells can be isolated by FACS and transplanted into recipient testes to determine the SSC activity. Although no SSC-specific molecules have been identified, this approach could allow better fractionation of undifferentiated spermatogonia and would be useful to characterize each spermatogonia subpopulation based on the SSC activity. Although As spermatogonia have been thought to be SSCs for a long time, recent live image studies using GFP-labeled Ngn3 spermatogonia by whole mount analysis suggest that fragmentation of Aal spermatogonia resulted in generation of Apr or As spermatogonia occurred. Furthermore, the Apr and As spermatogonia reinitiate formation of Aal spermatogonia [106]. Because no specific molecular marker for As, Apr, and Aal spermatogonia has been identified, their individual SSC activity cannot directly be assessed. However, the whole mount study suggests that some nonstem cell undifferentiated spermatogonia might revert to stem cells. To support this, KIT-expressing type A1 spermatogonia have been shown to possess SSC potential [107]. It is not clear, however, that these reversion pathways from differentiating spermatogonia to SSCs contribute to normal spermatogenesis; therefore, the biological significance of this phenomenon remains to be determined. In any event, if a molecular marker specifically expressed in SSCs could be identified, the SSC behavior in the testis will be able to be clarified in future. Because even in a single cohort of Aal spermatogonia, gene expression patterns in individual spermatogonia appeared to be different [108], Aal spermatogonia may contain a few SSCs. If individual spermatogonia within an Aal spermatogonia syncytium could be isolated, it would be possible to examine whether a single cohort of Aal spermatogonia contain SSCs by the transplantation assay. Functional activity of SSCs combined with whole mount analysis, flow cytometry, and live imaging is necessary to fully elucidate SSCs at molecular, cellular, and population levels.
Spermatogonial stem cell culture
Mouse
The first long-term maintenance of murine SSCs in culture was demonstrated in 1998 [109]. In this study, unfractionated testicular cells from neonatal and adult transgenic mice expressing β-galactosidase were cultured for up to 4 months on STO (SIM mouse embryo-derived thioguanine and ouabain resistant) feeder cells, which have been routinely used for mouse ES cell cultures, in a regular 10% fetal bovine serum (FBS)-supplemented medium. To determine whether SSCs were maintained in culture, the stem cell activity of cultured cells was examined by the transplantation assay [109]. In recipient testes transplanted cultured cells derived from neonatal testis, donor-derived spermatogenic colonies were identified, demonstrating that SSCs could be maintained in culture at least 4 months [109]. However, no expansion of SSCs was observed, and the number of surviving SSCs was very low. Therefore, the effect of several cytokines, including FGF2, leukemia inhibitory factor (LIF), and KITL, on SSC survival was investigated. FGF2 and KITL stimulate PGC proliferation [110, 111], while LIF is essential for self-renewal of mouse ES cells [112, 113], but none of these factors supported an increase in SSC number [114]. Although a large number of SSCs were lost after 1 week in culture, a beneficial effect of GDNF on SSC maintenance was demonstrated in this short-term culture experiment [114]. Originally, GDNF was identified as a neurotrophic factor [115], but a seminal study reported in 2000 demonstrated that GDNF is a critical regulator of fate determination of undifferentiated spermatogonia in mice [36]. In this study, GDNF-overexpressing mice showed abnormal proliferation of spermatogonia, whereas hemizygous GDNF-knock-out mice gradually lost spermatogonia, resulting in seminiferous tubules lined only by Sertoli cells. In both cases, the males became infertile due to impaired spermatogenesis. This result indicated that GDNF controls spermatogonial proliferation and differentiation in a dose-dependent manner [36]. Subsequently, a positive effect of GDNF on SSC self-renewal was demonstrated by overexpression of GDNF in Sertoli cells by electroporation of a GDNF-expression vector [116]. As seen in the GDNF-overexpressing transgenic mice, expansion of undifferentiated spermatogonia occurred. In addition, the transplantation assay demonstrated an increase in SSC number in the transfected testes [116]. However, GDNF supplementation did not result in proliferation of SSCs in the culture conditions employed; therefore, whether GDNF was directly stimulating proliferation of SSCs or indirectly regulate the SSC number in testes was not clear [114].
The first report of in vitro expansion of SSCs was in 2003 culturing gonocytes, precursor of SSCs, from newborn mice of genetic background ICR or BDF1 (C57BL/6 x DBA/2). The gonocytes enriched by a differential plating were cultured on mouse embryonic fibroblasts (MEFs) feeders in a serum-supplemented proprietary StemPro-34 (Gibco)-based medium, which contained the original StemPro-34 supplement plus 16 individual compounds and FBS with a cytokine mixture of GDNF, FGF2, LIF, and epidermal growth factor (EGF) [117]. Using the enriched culture media, quiescent gonocytes resumed proliferation and formed grape-like clusters. They continuously proliferated and expressed several spermatogonial markers such as ITGA6, ITGB1, and EPCAM. Although SSCs in seminiferous tubules are believed to be subpopulation of As spermatogonia presenting as single cells, continuously proliferating spermatogonial cells in culture formed cellular aggregates, which did not look like typical As spermatogonia that appear as individual, isolated cells in the seminiferous tubule. However, the transplantation assay unequivocally demonstrated that the aggregated cells possessed SSC activity, and the recipient mice generated progeny with the donor haplotype by micro insemination. The grape-like proliferating cells generated ∼12 colonies per 105 cells transplanted [117], which is similar to the stem cell activity of neonatal gonocytes purified by FACS or MACS that generated 17–22 colonies per 105 cells transplanted [18]. The continuously proliferating cells were named GS (germline stem) cells; however, formation of grape-like cluster did not occur, when gonocytes from C57BL/6 or 129/Sv mice were cultured in the same culture condition [117]. Interestingly, GS cells developed from DBA/2 genetic background spontaneously transformed to pluripotent stem cells, which were designated multipotent GS (mGS) cells, with characteristics similar to ES cells, although the appearance occurred only about once in 30 testes [118]. Because spontaneous transformation of SSCs to pluripotent cells in normal mouse testes is extremely rare, this unique characteristic of GS cells suggests that they might not be identical to normal SSCs. In fact, GS cells could proliferate in an anchorage independent manor, indicating attaching to basement membrane is not absolutely required for continuous proliferation [119]. These unique characteristics of GS cells are likely acquired during the developmental process or long-term cultivation. GS-like cell lines, which retain SSC activity and spontaneously acquire pluripotency potential, have also been established from adult testes using similar StemPro-34-based culture conditions [120–122]. Therefore, although SSCs are unipotent stem cells in the testis, the transformation capability of GS cells into pluripotent stem cells makes them a valuable tool to investigate and understand pluripotent characteristics of the germline. Furthermore, although an SSC population was never maintained in the testes of homozygous GDNF-knock-out mice [123], FGF2-dependent GS cells could be established in the absence of GDNF [124]. It is important to clarify the origin of FGF2-dependent GS cells and the presence of similar FGF2-dependent spermatogonia in normal or GDNF-knock-out mouse testes. Because FGF2 is a potent mitogen for PGCs, and the FGF2-dependent GS cells express the KIT receptor-like PGCs, it is quite valuable to investigate whether they can generate pluripotent stem cells as seen in PGCs or GS cells cultured with GDNF.
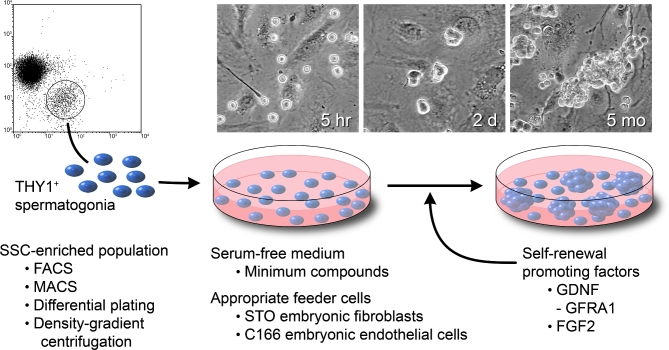
Identification of essential extrinsic factors for self-renewal of SSCs is crucial not only to establish long-term culture conditions for SSCs but also to elucidate the competency of SSCs [93]. One approach to accomplish this is cultivation of SSCs under a defined culture system and subsequent transplantation to evaluate the SSC activity of cultured SSCs following stimulation with various candidate factors. For this purpose, a culture system consisting of a spermatogonial population enriched for SSCs, a serum-free medium containing minimum compounds, and a mitotically inactive STO feeder cells, has been developed, which was originally described for hepatic stem/progenitor cells [125]. When THY1+ undifferentiated spermatogonia from pups were cultured on STO feeders in a serum-free defined medium consisting of alpha MEM basal medium containing bovine serum albumin (BSA), insulin, transferrin, selenium, putrescine, 2-mercaptoethanol, free fatty acids, HEPES, and antibiotics, the immature germ cells formed morula-like, tightly packed clumps, which continuously proliferated (Figure 6). The THY1+ undifferentiated spermatogonia from DBA background mice continuously proliferated in a GDNF-dependent manner and generated spermatogenic colonies following transplantation, indicating they contained SSCs [37]. Although the STO cells, like primary MEFs, produce LIF, SCF, and EGF [126, 127], these factors did not show any beneficial effect on SSC proliferation [18]. On the other hand, THY1+ undifferentiated spermatogonia from non-DBA/2 mouse strains, such as C57BL/6 or 129/Sv, did initially formed clumps, but ceased proliferation and disappeared within a few weeks [37]. However, addition of a small amount of FGF2 (1 ng/mL) or soluble GFRA1 allowed slow but continuous proliferation of SSCs from non-DBA/2 mouse strains [37]. GFRA1 is a GDNF-binding subunit of the GDNF receptor complex that consists of RET receptor tyrosine kinase and GFRA1, a glycosil phosphatidylinositol-anchored molecule. Free soluble GFRA1 and GDNF bind in the culture medium, and the GDNF/GFRA1 complex directly and more intensely stimulates RET activation [128]. Adding both factors, FGF2 and GFRA1, with GDNF in the medium, allowed THY1+ undifferentiated spermatogonia from all mouse strains examined to proliferate indefinitely in this defined culture condition [37]. The proliferating cells were THY1+ ITGA6+ GFRA1+ CDH1+ EPCAM+, and their SSC activity was 200–400 colonies per 105 cell transplanted, which is equivalent to freshly isolated undifferentiated spermatogonia from postnatal testes [18, 37, 93, 129], indicating that the clump-forming cells in the serum-free condition are phenotypically and functionally identical to SSC-enriched undifferentiated spermatogonia, which represent a heterogeneous mixture of SSCs (a smaller portion) and progenitors (a greater portion). When the clump cells were transplanted into infertile males, the recipients produced progeny carrying the donor SSC haplotype. In this culture condition, the clump cells maintained stem cell activity and doubled every 5.6 days for more than 6 months [37].
Figure 6.
Long-term in vitro proliferation of SSCs. A SSC-enriched population can be obtained by FACS, MACS, differential plating, or density-gradient centrifugation. The SSC-enriched population is placed on appropriate feeder cells (STO feeders for mouse SSCs, C166 feeders for rabbit SSCs) in a serum-free defined medium supplemented with self-renewal promoting factors (GDNF, FGF2, GFRA1, etc.). Microscopic images of germ-cell clump formation and continuous proliferation are shown. Three images are 5 h, 2 days, and 5 months after in vitro culture of mouse THY1+ undifferentiated spermatogonia isolated from pup testes by MACS. The clump-forming cells retain SSC competency equivalent to undifferentiated spermatogonia in the testis. Modified from [37].
The culture system can be improved by reducing the atmosphere oxygen concentration. Compared with an air atmosphere (21% O2), a 10% O2 atmosphere significantly enhanced self-renewing proliferation of SSCs in culture. Following 15-day culture under a 10% O2 atmosphere, the number of SSCs increased 1.5-fold [129]. In addition, a beneficial effect of a reduced O2 condition on cultured SSCs has been confirmed in a long-term culture [130]. One of the most dramatic effects of a low O2 condition appeared on proliferation of SSCs from W infertile mouse testes, which contain very few undifferentiated spermatogonia. A long-term culture of clump-forming undifferentiated spermatogonia from Wv/Wv mice could be established only in a 10% O2 atmosphere [129]. This improved culture condition is important because the undifferentiated spermatogonia number is extremely low in Wv/Wv testes, and it was impossible to enrich them by regular antibody-based enrichment such as FACS or MACS. However, even without an enrichment step, a 10% O2 condition could support proliferation of Wv/Wv undifferentiated spermatogonia and establish a long-term culture. Furthermore, the functional transplantation assay proved the Wv/Wv clump-forming gem cells contain SSCs [129].
Rat
Two rat SSC culture systems have been developed by modification of the mouse SSC culture conditions [131, 132]. One of these conditions is essentially the same as the mouse SSC culture system consisting of serum-free medium, STO feeders, and the same growth factors, GDNF, FGF2, and GFRA1 [131]. Rat undifferentiated spermatogonia were enriched by MACS with an antibody for rat EPCAM [133] and cultured on STO feeder cells in a serum-free defined medium with an increased concentration of several components (BSA, insulin, transferrin, selenium, putrescine, 2-mercaptoethanol, and free fatty acids) and reduced osmolality. Like mouse SSCs, rat undifferentiated spermatogonia formed clumps and proliferated indefinitely in a GDNF-dependent manner. FGF2 and GFRA1 were also supportive. The cultured cells generated spermatogenic colonies in the testes of Busulfan-treated recipient rats following transplantation, and offspring were successfully produced by mating with female rats. These results clearly indicated that the clump-forming cells derived from rat undifferentiated spermatogonia contain rat SSCs that are able to self-renew and generate functionally normal spermatozoa [131]. An important finding is that GDNF is the key growth factor for the formation and proliferation of clump-forming cells, including rat SSC, and FGF2 supports their continuous proliferation.
The second long-term culture condition for rat SSCs consists of MEF feeder cells and a serum-free medium containing the proprietary B27 supplement minus vitamin A (Gibco), supplemented with GDNF and FGF2 [132]. The culture medium was StemPro-34-based GS cell medium, but serum was replaced with B27 supplement, a serum-free supplement developed for supporting neural cell cultures [134]. Although the original B27 supplement contains vitamin A, B27 minus vitamin A was used for rat SSC culture because vitamin A is a potent differentiation factor for spermatogonia. When the B27 supplement minus vitamin A replaced serum in the StemPro-34-based GS cell medium, rat spermatogonia enriched for SSCs by FACS continuously proliferated [132]. Serum-supplemented GS medium was initially used, but the number of rat germ cells progressively decreased after each subculture due to overgrowth of fibroblasts [132]. This is reminiscent of a dramatic decrease of SSC numbers that occurred when mouse SSCs were cultured with a combination of serum and testicular somatic cells [18]. Interestingly, a subsequent study showed that a serum-free DMEM/F12 medium supplemented with B27 minus vitamin A seemed better than the StemPro-34-based medium for rat SSC culture [135]. Likewise, B27 supplementation and removal of FBS in the GS medium improved the cell proliferation rate of mouse GS cells, although FBS appeared to be necessary for initial derivation of mouse GS cell lines on primary MEF feeder cells [136]. Rat pluripotent stem cell lines have not been developed from cultured rat SSCs in the GS medium.
Rabbit
The in vitro culture techniques and the functional transplantation assay have revealed that the extrinsic factors for self-renewal of murine and rat SSCs are identical; however, those for nonrodent SSCs are not clear. The first long-term culture of nonrodent clump-forming germ cells with SSC potential was for rabbit [137]. Mice and rats diverged phylogenetically approximately 11 million years ago [138], while rabbits diverged from rodents about 60–70 million years ago [139]. Thus, cultivation of rabbit SSCs could provide a valuable foundation for development of other nonrodent SSC cultures. When rabbit germ cells were transplanted into mouse testes, putative rabbit SSCs colonized and proliferated for several months, although no spermatogonial differentiation occurred [26]. This indicates that exogenous factors to support long-term maintenance and proliferation of rabbit SSCs exist in mouse seminiferous tubules, and GDNF and FGF2 are logical candidates for those factors. In the presence of GDNF and FGF2, STO feeder cells could not support clump formation and proliferation of rabbit primitive spermatogonia; however, C166 feeder cells, a yolk-sac-derived endothelial cell line, did support clump formation and proliferation of rabbit germ cells in the serum-free medium used for rodent SSCs [137]. The proliferation of rabbit germ cell clumps was dependent on GDNF, but FGF2 was not required for continuous proliferation. The possibility of a role for FGF2 on the initiation phase of cultivation cannot be ruled out. The rabbit clump-forming cells expressed several undifferentiated spermatogonial markers identified for rodents, including promyelocytic leukaemia zinc finger (PLZF), POU5F1, GFRA1, RET, THY1, CD9, and ITGA6 in addition to evolutionally conserved germ cell-specific protein DEAD-box polypeptide 4 (DDX4, also known as VASA) [137]. To demonstrate that the clump-forming germ cells on C166 feeder cells were rabbit SSCs, functional characterization was necessary. Because an assay to evaluate rabbit SSC activity that includes both self-renewal and differentiation capability to produce functional sperm has not been established, the clump-forming germ cells on C166 feeder cells were transplanted into immunocompromised mouse testes, which is the most reliable method to evaluate SSC potential for nonrodent SSCs [26–30, 82, 83]. After genetic labeling of the clump cells to avoid any misinterpretation, they were transplanted into mouse testes. Although no donor-derived spermatogenesis occurred, the rabbit clump-forming germ cells colonized and proliferated in the recipient testes for at least 6 months. Furthermore, they retained their undifferentiated spermatogonial phenotype during this period. Therefore, it is very likely that the transplanted clump-forming cells cultured on C166 feeders contained rabbit SSCs. However, to unequivocally prove that they are rabbit SSCs, a transplantation assay using rabbit testes is required, because demonstration of biological competency in vivo is the gold standard for identification of stem cells in any type of tissue.
In the transplantation experiments using immunocompromised recipient mice for nonrodent SSCs, at least two issues must be carefully addressed. First, donor-derived cells must be unequivocally identified in recipient testes and should be distinguished from recipient cells. Although donor-cell specific antibodies can be used for whole-mount analyses [26–29], a possibility of cross-reaction by antibodies always persists. In particular, when the specificity of the antibody is not high or colonized cell number is low, the judgment will be difficult. Therefore, genetic labeling of donor cells by introducing a reporter gene is preferable to avoid any misinterpretation. In the rabbit study, the clump-forming germ cells were labeled with the β-galactosidase or GFP gene using lentivirus vectors before transplantation [137]. By X-gal staining, β-galactosidase-expressing donor rabbit cells could be readily identified as blue cells on the basement membrane in recipient mice. The second critical issue is characterization of colonized cells, because some types of somatic cells also can colonize the testis [26, 27, 53]. If the colonies have developed from transplanted SSCs, such colonies should consist of primitive spermatogonia or self-renewing SSCs. By flow cytometry, GFP-expressing rabbit donor cells in the recipient testes were identified and shown to retain the undifferentiated spermatogonial phenotype for 6 months [137].
Development of long-term cultivation techniques for SSCs derived from nonrodent species except rabbit have not been successful. Thus, the approach of this rabbit experiment, including development of a culture condition and assessment of transplanted cultured germ cells for a long-period, serves as a model of initial assessment for SSC activity of cultured germ cells from other nonrodent species, including domestic animal and human SSCs.
Domestic animals
The long-term culture of SSCs or undifferentiated spermatogonia from domestic animals, other than rabbits, is still in its infancy [140]. When freshly isolated testicular cells from domestic animals, including dogs, pigs, cattle, and horses, were transplanted into immunocompromised mouse testes, colonies of undifferentiated spermatogonia likely derived from putative SSCs were identified. Cryopreserved testis cells also resulted in colonization following transplantation. However, after short-term culture of the testis cells, the colonizing cells appeared to be primarily fibroblasts, and donor spermatogonia could not be unequivocally identified [26, 27]. Although xenogeneic transplantation experiments using fresh germ cells suggest that mouse and other domestic animals share the survival and mitogenic factors for putative SSCs, research to evaluate culture conditions for each domestic animal species is required [18, 37, 114, 129, 131, 132, 141]. Culture conditions that have been evaluated include enrichment methods for spermatogonia, modification in composition of medium (basal medium, serum, supplements for serum-free medium, etc.), various types of feeder cells (MEFs, same species-derived primary cells, established cell lines, etc.), appropriate growth factor combinations (GDNF, FGF2, LIF, EGF, etc.), and different physical conditions (temperature, oxygen concentration, etc.). Using this approach, a canine short-term culture that allowed lentiviral gene transfer into canine SSCs was developed [75]. The genetically modified SSCs were transplanted into canine recipients, which were previously irradiated to destroy endogenous spermatogenesis, and the donor cells produced genetically modified spermatozoa for 4 months. In addition, a culture condition that allows survival of bovine undifferentiated spermatogonia for 2 months has been reported [142]. However, colonization of neither murine nor bovine recipient testes following transplantation was reported for these cells; therefore, it is unclear whether the cultured cells contained functional bovine SSCs or undifferentiated spermatogonia. Currently, no long-term culture system capable of supporting proliferation and maintenance of SSCs that can reconstitute donor-derived spermatogenesis in recipient immunocompromised mouse testes or the same species recipient testes has been reported for domestic animals [140, 143]. Because long-term culture systems are crucial to investigate the biology of domestic animal SSCs and to use these cells in practical applications, such as germline modification, further studies are critical.
Human
In vitro expansion of human SSCs is of great clinical value, and a number of studies on culture of human germ cells have been reported [144–150], but conclusive demonstration of the existence of human SSCs is challenging. Most culture conditions that have been used are modified from the GS cell culture system. In these conditions, two types of cell aggregates appeared after cultivation of human testis cell suspensions. One type had a round shape, while the second type had flattened morphology consisting of tightly attached cells, which appeared similar to ES cells [144]. The round aggregates expressed several spermatogonial markers, including PLZF, GFRA1, ubiquitin carboxyl-terminal hydrolase L1 (UCHL1), and G protein-coupled receptor 125 (GPR125); therefore, they were considered to be primitive spermatogonia [144, 151]. Following transplantation to immunocompromised mouse testes only single donor cells were identified [144, 151]. Because cellular identity of these colonized cells in the recipients was not examined, further characterization to determine whether they are human primitive spermatogonia will be required.
The absence of a functional assay system to identify unequivocally human SSCs has resulted in considerable controversy regarding interpretation of human SSC culture experiments [84, 152–154]. Although the cellular identity of human SSCs in the cultures was determined based on expression of SSC markers previously identified in rodent SSCs, recent studies have clearly demonstrated that several putative markers used for identifying human SSCs are expressed in nongerm cells of primary and cultured human testis cells [152, 153]. In particular, it has been shown that PLZF, GFRA1, UCHL1, GPR125, and ITGA6, which were used to identify human SSCs in previous studies, are expressed in many testicular somatic cells. Therefore, in either culture experiments or transplantation experiments, detection of several putative human spermatogonial markers, such as PLZF, GFRA1, UCHL1, GPR125, and ITGA6, is not reliable to identify human spermatogonia. A possible approach to avoid the problem would be the identification of reliable human SSC-specific markers. Determining molecular signatures by various omics studies of human undifferentiated spermatogonia would be helpful for identification, which would facilitate detection and characterization of cultured human SSCs and colonized donor cells in recipient testes [155–158].
Several reports indicated that ES-like cells appeared by culturing human testicular cells under GS cell culture conditions [144, 159] or ES cell culture conditions [160, 161]. Although the ES-like colonies are believed to be derived from SSCs or primitive germ cells, gene expression analysis suggested that their origin is mesenchymal cells [162, 163], indicating that the ES-like colonies formed in the culture conditions may not be SSC-derived cells. In conclusion, while several reports proposed that human SSCs or SSC-derived pluripotent cells could be continuously cultured over months, these published reports remain controversial regarding the functionality of the stem cells; therefore, further rigorous evaluation is required. Development of a definitive functional assay to evaluate the competency of human SSCs will be essential to acceptance of any published techniques.
Regulation of self-renewal and fate determination
In vivo and in vitro studies have established GDNF as the primary extrinsic factor stimulating self-renewal of mouse SSCs in a dose-dependent manner. A high concentration of GDNF promotes proliferation of undifferentiated spermatogonia, and a low concentration of GDNF induces spermatogonial differentiation [36, 37, 116, 136]. Not surprisingly, expression of the GDNF receptor, which consists of GFRA1 and RET, on SSCs is also critical for their fate determination. In particular, GFRA1 is high in As spermatogonia, which contain SSCs, but the expression decreases in Apr and Aal spermatogonia [164]. Although knock-out mice homozygous for Gdnf, Gfra1, or Ret are neonatal lethal, the effect on spermatogenesis of deficiencies of any of these genes on spermatogenesis can be investigated by analyzing testes grafted into mature mice. When normal neonatal testes are grafted to the back/flank of castrated male nude mice, the grafted testes initiate spermatogenesis and eventually generate functional spermatozoa [165, 166]. When neonatal testes of homozygous Gdnf, Gfra1, or Ret knock-out mice were grafted into recipient mice, no spermatogonial proliferation occurred, but spermatogonial differentiation was initiated. Therefore, the grafted testes eventually showed a Sertoli cell-only phenotype because spermatogonia did not proliferate [123]. Collectively, these results clearly indicated that the GDNF-RET signaling pathway plays the central role for regulation of fate determination, self-renewal or differentiation, of murine SSCs, although other exogenous factors have a role.
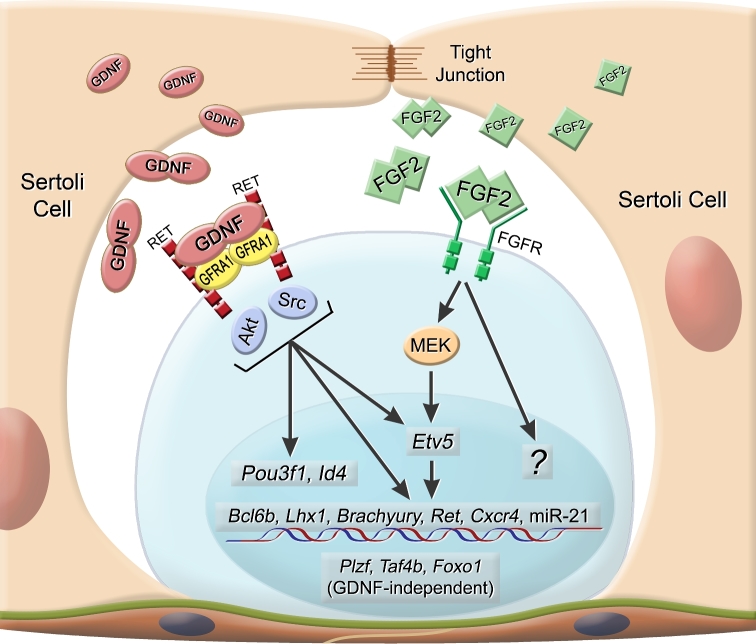
To understand the molecular mechanism of self-renewal in mouse SSCs, elucidation of GDNF-RET signal transduction is essential, and identification of the target effector molecules is crucial. Using the serum-free culture system for mouse SSCs, several GDNF-responsive genes including B cell CLL/lymphoma 6B (Bcl6b), LIM homeobox 1 (Lhx1), ets variant 5 (Etv5), Pou3f1 (Oct-6), and Brachyury were identified by transcriptome analysis, and knock-down of each gene led to a reduction of stem cell activity [167–169]. Culturing SSCs with specific kinase inhibitors revealed that Src family kinases and Akt are critical for the effect [170]. Other in vitro experiments with SSCs also showed that proliferation of SSCs is dependent on the two signaling pathways [171, 172]. Among the GDNF-responsive genes, Etv5 is a key factor because Etv5 upregulates Ret, Bcl6b, Brachyury, chemokine (C-X-C motif) receptor 4 (Cxcr4), a receptor for CXCL12, and microRNA-21 (miR-21), which prevents apoptosis of SSCs [169, 173, 174] (Figure 7). Although Etv5 is expressed in spermatogonia and Sertoli cells [175], the endogenous expression in spermatogonia is indispensable for SSC competence [173]. Since development of SSC cultivation methods, the number of GDNF-responsive molecules supporting SSC self-renewal has increased dramatically, and they now include microRNAs, long noncording RNAs, and phosphorylated proteins [174, 176, 177]. Identifying important pathways, target genes and elucidating the functional interaction between these molecules will be an exciting focus of future studies.
Figure 7.
Molecular mechanisms of mouse SSC self-renewal. After GDNF binds to a ligand binding receptor GFRA1, the complex activates RET receptor tyrosine kinase following activation of Akt and Src-family kinases. The GDNF stimuli induces expression of many genes in SSCs, including transcription factor-encoding genes, Etv5, Bcl6b, Lhx1, Brachyury, Ret, Cxcr4, Pou3f1, and Id4. These transcriptional factors are involved in SSC self-renewal. Plzf, Taf4b, and Foxo1 also play important roles on SSC self-renewal, but their expression is not regulated by GDNF. FGF2 is the second critical factor for SSC self-renewal, which induces Etv5 expression through MEK activation. Etv5 appears to be a key molecule, because this transcription factor upregulates other GDNF-inducing genes. MicroRNA-21 (miR-21) expression is regulated by Etv5 and inhibits apoptosis in SSCs. GDNF and FGF2 are produced from Sertoli cells in the testis. Modified from [156].
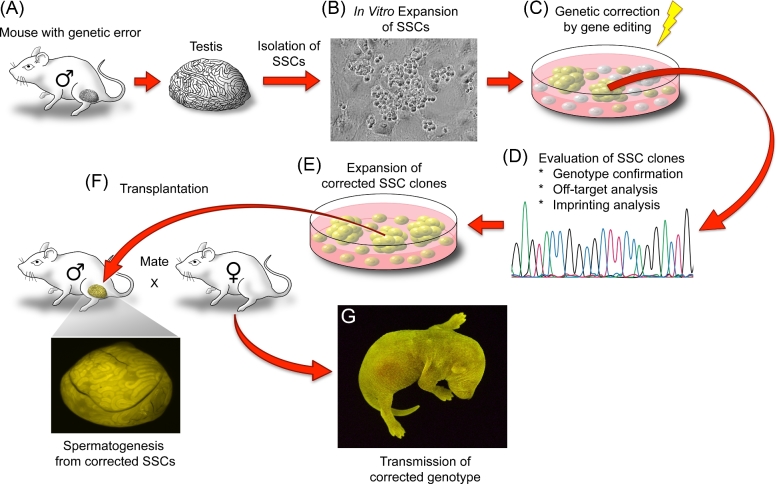
In addition, gene expression analyses of newly isolated, undifferentiated spermatogonia, as well as cultured germ cells enriched for SSCs and lineage-tracing experiments have identified several genes, such as Bmi1, Pax7, and Id4, which are expressed in long-term self-renewing As spermatogonia in testes [98, 104, 178, 179]. Several lines of evidence show that Id4 is a critical factor for SSC maintenance. For example, ID4 is expressed in As, but not Apr and Aal, and the spermatogonial transplantation of Id4+ spermatogonia demonstrated that the Id4bright population possessed higher SSC activity than the Id4dim population. Because Id4 expression is regulated by GDNF, identification of the Id4 downstream pathway in SSCs will be critical. Using knock-out mice in loss of function analyses has also revealed several additional factors, such as Plzf, TATA-box binding protein associated factor 4b (Taf4b), Nanos2, forkhead box O1 (Foxo1), and RB transcriptional corepressor 1 (Rb1) that are essential for SSC self-renewal or maintenance in testes [102, 180–183]. Because expressions of several of these factors, including Plzf, Taf4b, and Foxo1, are not upregulated by GDNF [184], SSC self-renewal and fate decision are likely regulated by both GDNF-responsive factors and non-GDNF responsive factors (Figure 7).
In addition to GDNF, FGF2 is an important factor for SSC self-renewal, since SSCs from C57Bl/6 mice or 129/Sv mouse strains required FGF2 for self-renewal in culture [37, 93]. Furthermore, in humans, gain-of-function mutations in FGFR2 lead to Apert syndrome, in which growth advantaged SSCs increase in number in aged males and result in the mutant phenotype [38, 185, 186], indicating that FGFs are positive regulators of SSC proliferation. Interestingly, studies using GS cells showed that Bcl6b, Lhx1, Etv5 were also upregulated by MEK (MAP2K1) activation following FGF2 stimulus [187], indicating that FGF2, in addition to GDNF, plays an important role in GDNF-responsive gene expression. However, in the serum-free culture system, the target molecules of FGF2 in SSCs have little overlap with genes regulated by GDNF, indicating that FGF2 plays a distinct role on SSC self-renewal [48]. Because FGF2 alone cannot support SSC self-renewal, the role of FGF2 on SSC self-renewal must be defined in the context of a GDNF stimulus. Further detailed elucidation of the self-renewal mechanism of mouse SSCs is central to understanding the fate determination process and would serve as a foundation for establishing the universal self-renewal mechanism in other mammals.
Germline modification and gene therapy using spermatogonial stem cells
In the adult body, germ cells are the only cells that can transmit genetic information to subsequent generations. In mammals, female germ cells do not increase in number following birth; however, in the male, germ cells continue to divide and represent a renewable source of the genetic code, which will be modified through meiosis during spermatogenesis and produce a large array of recombined genotypes in spermatozoa. Access to this renewable source is represented by SSCs; therefore, an enormously valuable application of the techniques described above is for germline modification [188]. The first transgenic animals using SSCs were created by transduction of mouse SSCs using a retrovirus vector containing the β-galactosidase gene [189]. Subsequent development of long-term culture systems has allowed a variety of techniques to be used for genetic modification of SSCs, resulting in generation of not only knock-out mice by homologous recombination [190], but also transchromosomic mice [191] and gene-edited mice using the TALEN or, in particular, the CRISPR/Cas9 system [192, 193]. In rats, similar to the mouse system, the first SSC-based transgenic rats were generated using a lentiviral vector [194, 195]. Subsequently, gene editing of rat SSCs by the CRISPR/Cas9 system has also been developed [196].
A number of genetic mutations causing genetic disorders in human have been identified, and germline gene editing may be considered for therapy to correct these genetic defects. Although recent reports of gene editing in human preimplantation embryos using CRISPR/Cas9 are controversial [197], once a stable culture system for human SSCs has been developed, the ethics of research designed to generate spermatozoa from gene-edited human SSCs will require serious discussion. Using eggs, gene-editing studies have revealed that off-target effects and mosaicisms are two major problems, but cultured SSCs can avoid these concerns because off-target SSC clones can be identified, and the proper targeted SSCs selected to produce corrected spermatozoa (Figure 8).
Figure 8.
Outline of germline gene therapy by SSCs. (A) SSCs are isolated from the testis of a mouse with a genetic error. (B) SSCs are expanded in culture. (C) The genetic error is corrected by a gene edition technique (ZFN, TALEN, or CRISPR/Cas9) and the corrected SSC clones are selected (yellow). (D) Genetic and epigenetic analysis of each SSC clone is carried out to confirm there is no error in the genome sequences and proper epigenetic modifications. (E) Corrected SSC clones are expanded in culture. (F) Following transplantation into infertile recipient testes, spermatozoa from the corrected SSCs are produced. (G) Progeny with the corrected gene are generated by mating to a wild-type female or micro insemination into a wild-type oocyte.
Clinical applications and future directions
Transplantation of SSCs from immature males before puberty can produce functional spermatozoa, and SSCs can be cryopreserved for over 14 years [24, 25]. Thus, one of potential clinical applications using human SSCs is in prepubertal boys undergoing chemotherapy or radiation treatment for cancer [198, 199] (Figure 9). Germ cells including SSCs are very sensitive to chemotherapeutic agents and radiation, and about 80% of childhood cancers can now be cured. Currently, it is estimated that approximately 1 in 5000 males of reproductive age are infertile or severely subfertile as a result of treatment for childhood cancer [200]. While adults can cryopreserve semen before cancer therapies for future use in artificial insemination or in vitro fertilization, prepubertal boys cannot use this option, because functional spermatozoa have not developed. Instead, cryopreservation of a testicular biopsy obtained before cancer treatment begins containing SSCs is an option for prepubertal boys. After cancer treatment, autologous spermatogonial transplantation by testicular cells recovered from the cryopreserved tissues can be used to establish spermatogenesis [201]. Once efficient culture methods to allow in vitro expansion of human SSCs have been developed, the number of SSCs can be greatly increased before cryopreservation or transplantation, which improves recovery of spermatogenesis in recipient testes (Figure 9).
Figure 9.
Clinical application of SSCs and spermatogonial transplantation. In a prepubertal patient with cancer, a testis biopsy containing SSCs can be taken before cancer treatment with chemotherapy or irradiation. The biopsy containing SSCs or SSCs after in vitro expansion could be cryopreserved. After successful cancer treatment, the SSCs would be autologously transplanted to the patient's testes to restore fertility. For a patient carrying a genetic defect, the defective gene could be corrected in SSCs during culture (see Figure 8). The SSCs with the corrected gene could be transplanted into the testes of the patient. Modified from [198, 199].
For this therapeutic approach, potential contamination by malignant cells in donor cell suspensions must be avoided, and purification of human SSCs before transplantation is a feasible solution. Identification of the unique surface phenotype of human SSCs will allow both enrichment of human SSCs and elimination of cancer cells before transplantation [155]. THY1 and EPCAM have been identified as useful cell surface markers to enrich putative SSCs in human. In addition, human SSCs do not express MHC-I, CD45, and CD49e (integrin α5), while leukemic cells strongly express these cell surface molecules. By staining donor cell suspensions with fluorochrome-conjugated antibodies against these cell surface molecules, contamination of tumorigenic cells in donor cell suspension could be avoided by FACS [202]. In addition, culture techniques for selective human SSC expansion, would facilitate removal of any potential cancer cells prior to transplantation.
There has been increasing interest in reprogramming a somatic cell, particularly a somatic stem cell, into a germline cell, represented by either a one-cell egg or an SSC. The ability to convert a somatic cell of any type to a germ cell would be a revolutionary advance. Reprogramming a somatic cell to an SSC, in some ways, appears the most direct or simplest, since it does not initially involve meiosis. In many reprogramming experiments, an adult somatic cell is converted into an iPS cell, and then differentiates into an oocyte or SSC (or SSC-like cell) via epiblast-like cells and PGC-like cells [22, 203, 204]. However, these experiments contain numerous steps, are difficult, and have a low efficiency. The specificity and power of the spermatogonial transplantation system allows one to transplant many cells, and if there are a few SSCs present, they are the only cells that will continuously proliferate and differentiate in the seminiferous tubules of the recipient testis and generate spermatozoa.
Instead of generating iPS cells, another approach would be a direct reprogramming of adult somatic cells into SSCs. For example, skin hair follicle cells can be used for an initial cell population, because the bulge of the follicle contains stem cells, which can be isolated and grown in vitro. A potential sequence for converting hair bulge cells to functional germ cells is diagrammed in Figure 10. The bulge cells can be isolated by dissecting the hair follicles and establishing a culture. A variety of techniques or systems can be used to convert or reprogram the cultured bulge cells to SSCs. Following reprogramming events, some cells will be converted to SSCs, and when these cells are cultured and transplanted to a recipient testis, the seminiferous tubules will determine which if any of these cells have been reprogrammed. The power of this system is that tens of thousands of the somatic cells can be exposed to reprogramming factors or environments, and if only a few are reprogrammed, the seminiferous tubule of the recipient mouse will select them and produce a colony of spermatogenesis. As many as one million cells can be transplanted into a single testis, and the colonizing efficiency of an SSC is approximately 1 in 10 following transplantation (see above). Since 10 to 20 recipient testes can be injected in a single day, the spermatogonial transplantation system provides a highly efficient system from which to select a very few functional SSCs from many potentially reprogrammed cells. Changes along the reprogramming pathway can be analyzed following establishment of the process. Understanding the reprograming process from a somatic cell of any type into an SSC would be an enormous advance that would allow not only a window into the biological differences between somatic cells and germline cells, but also provide a powerful approach to elucidate germ cell development. Studies to reprogram somatic cells into SSCs are an enormously important future direction and would provide a major advance to the germ cell field.
Figure 10.
Proposed protocol for reprogramming of somatic cells to become germline stem cells, SSCs. (A) Three-dimensional diagram of skin. The hair bulge contains stem cells for all the skin appendages. (B) Image of mouse skin culture. When skin is cultured, primarily bulge cells continuously proliferate. By introducing various reprogramming factors, for example, transcription factors, epigenetic modifiers, soluble factors (including growth factors) and micro RNAs, hair bulb cells can be converted to SSCs. (C) Image of SSCs in culture as they would appear following reprogramming. The original cells taken from the skin of the mouse have a GFP-reporter system (e.g., a Ddx4-Cre gene and a floxed-stop Gfp gene) that is not active in skin cells but is expressed in germline cells including SSCs; thus, reprogrammed cells will fluoresce if they are SSCs in culture, as will all cells derived from the fluorescent SSC. To prove the bulge cells have been reprogrammed to SSCs, the cells will be transplanted into the testis of a recipient mouse. Any cells in culture that have become SSCs will produce a colony of spermatogenesis in the recipient male, which will be fluorescent. (D) Testis with fluorescent colonies of spermatogenesis in the seminiferous tubules. Mating to a wild-type female will produce fluorescent pups from these spermatozoa. (E) Fluorescent pups of the type that would be produced from spermatozoa that were reprogrammed from somatic cells with a GFP marker. Modified from [37].
Acknowledgment
We thank James Hayden, RBP, FBCA, for assistance in preparation of figures.
Footnotes
Grant Support: This work was supported by a Grant-in-Aid for Challenging Exploratory Research (No. 25660255) of Japan Society for the Promotion of Science (HK), National Institute of Child Health and Human Development Grant HD 052728 (RLB), and the Robert J. Kleberg, Jr and Helen C. Kleberg Foundation (RLB).
References
- 1. Russell LD, Ettlin RA, Sinha Hikim AP, Clegg ED. Histological and Histopathological Evaluation of the Testis. Clearwater, FL: Cache River Press; 1990:1–58. [Google Scholar]
- 2. Meistrich ML, van Beek, MEAB. Spermatogonial stem cells. In: Desjardins C, Ewing LL (eds.), Cell and Molecular Biology of the Testis. New York: Oxford University Press; 1993:266–295. [Google Scholar]
- 3. Tegelenbosch RA, de Rooij DG. A quantitative study of spermatogonial multiplication and stem cell renewal in the C3H/101 F1 hybrid mouse. Mutat Res 1993; 290(2):193–200. [DOI] [PubMed] [Google Scholar]
- 4. Brinster RL, Avarbock MR. Germline transmission of donor haplotype following spermatogonial transplantation. Proc Natl Acad Sci USA 1994; 91(24):11303–11307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brinster RL, Zimmermann JW. Spermatogenesis following male germ-cell transplantation. Proc Natl Acad Sci USA 1994; 91(24):11298–11302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shinohara T, Orwig KE, Avarbock MR, Brinster RL. Remodeling of the postnatal mouse testis is accompanied by dramatic changes in stem cell number and niche accessibility. Proc Natl Acad Sci USA 2001; 98(11):6186–6191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brinster CJ, Ryu BY, Avarbock MR, Karagenc L, Brinster RL, Orwig KE. Restoration of fertility by germ cell transplantation requires effective recipient preparation. Biol Reprod 2003; 69(2):412–420. [DOI] [PubMed] [Google Scholar]
- 8. Eaves CJ. Hematopoietic stem cells: concepts, definitions, and the new reality. Blood 2015; 125(17):2605–2613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ogawa T, Arechaga JM, Avarbock MR, Brinster RL. Transplantation of testis germinal cells into mouse seminiferous tubules. Int J Dev Biol 1997; 41:111–122. [PubMed] [Google Scholar]
- 10. Nagano M, Avarbock MR, Brinster RL. Pattern and kinetics of mouse donor spermatogonial stem cell colonization in recipient testes. Biol Reprod 1999; 60(6):1429–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dobrinski I, Ogawa T, Avarbock MR, Brinster RL. Computer assisted image analysis to assess colonization of recipient seminiferous tubules by spermatogonial stem cells from transgenic donor mice. Mol Reprod Dev 1999; 53(2):142–148. [DOI] [PubMed] [Google Scholar]
- 12. Zhang X, Ebata KT, Nagano MC. Genetic Analysis of the clonal origin of regenerating mouse spermatogenesis following transplantation. Biol Reprod 2003; 69(6):1872–1878. [DOI] [PubMed] [Google Scholar]
- 13. Kanatsu-Shinohara M, Inoue K, Miki H, Ogonuki N, Takehashi M, Morimoto T, Ogura A, Shinohara T. Clonal origin of germ cell colonies after spermatogonial transplantation in mice. Biol Reprod 2006; 75(1):68–74. [DOI] [PubMed] [Google Scholar]
- 14. Ogawa T, Ohmura M, Yumura Y, Sawada H, Kubota Y. Expansion of murine spermatogonial stem cells through serial transplantation. Biol Reprod 2003; 68(1):316–322. [DOI] [PubMed] [Google Scholar]
- 15. Nagano MC. Homing efficiency and proliferation kinetics of male germ line stem cells following transplantation in mice. Biol Reprod 2003; 69(2):701–707. [DOI] [PubMed] [Google Scholar]
- 16. Kanatsu-Shinohara M, Takehashi M, Takashima S, Lee J, Morimoto H, Chuma S, Raducanu A, Nakatsuji N, Fässler R, Shinohara T. Homing of mouse spermatogonial stem cells to germline niche depends on beta1-integrin. Cell Stem Cell 2008; 3(5):533–542. [DOI] [PubMed] [Google Scholar]
- 17. Takashima S, Kanatsu-Shinohara M, Tanaka T, Takehashi M, Morimoto H, Shinohara T. Rac mediates mouse spermatogonial stem cell homing to germline niches by regulating transmigration through the blood-testis barrier. Cell Stem Cell 2011; 9(5):463–475. [DOI] [PubMed] [Google Scholar]
- 18. Kubota H, Avarbock MR, Brinster RL. Culture conditions and single growth factors affect fate determination of mouse spermatogonial stem cells. Biol Reprod 2004; 71(3):722–731. [DOI] [PubMed] [Google Scholar]
- 19. Ohta H, Wakayama T, Nishimune Y. Commitment of fetal male germ cells to spermatogonial stem cells during mouse embryonic development. Biol Reprod 2004; 70(5):1286–1291. [DOI] [PubMed] [Google Scholar]
- 20. Chuma S, Kanatsu-Shinohara M, Inoue K, Ogonuki N, Miki H, Toyokuni S, Hosokawa M, Nakatsuji N, Ogura A, Shinohara T. Spermatogenesis from epiblast and primordial germ cells following transplantation into postnatal mouse testis. Development 2005; 132(1):117–122. [DOI] [PubMed] [Google Scholar]
- 21. Ohinata Y, Ohta H, Shigeta M, Yamanaka K, Wakayama T, Saitou M. A signaling principle for the specification of the germ cell lineage in mice. Cell 2009; 137(3):571–584. [DOI] [PubMed] [Google Scholar]
- 22. Hayashi K, Ohta H, Kurimoto K, Aramaki S, Saitou M. Reconstitution of the mouse germ cell specification pathway in culture by pluripotent stem cells. Cell 2011; 146(4):519–532. [DOI] [PubMed] [Google Scholar]
- 23. Zhou Q, Wang M, Yuan Y, Wang X, Fu R, Wan H, Xie M, Liu M, Guo X, Zheng Y, Feng G, Shi Q et al. Complete meiosis from embryonic stem cell-derived germ cells in vitro. Cell Stem Cell 2016; 18(3):330–340. [DOI] [PubMed] [Google Scholar]
- 24. Avarbock MR, Brinster CJ, Brinster RL. Reconstitution of spermatogenesis from frozen spermatogonial stem cells. Nat Med 1996; 2(6):693–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wu X, Goodyear SM, Abramowitz LK, Bartolomei MS, Tobias JW, Avarbock MR, Brinster RL. Fertile offspring derived from mouse spermatogonial stem cells cryopreserved for more than 14 years. Hum Reprod 2012; 27(5):1249–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dobrinski I, Avarbock MR, Brinster RL. Transplantation of germ cells from rabbits and dogs into mouse testes. Biol Reprod 1999; 61(5):1331–1339. [DOI] [PubMed] [Google Scholar]
- 27. Dobrinski I, Avarbock MR, Brinster RL. Germ cell transplantation from large domestic animals into mouse testes. Mol Reprod Dev 2000; 57(3):270–279. [DOI] [PubMed] [Google Scholar]
- 28. Nagano M, McCarrey JR, Brinster RL. Primate spermatogonial stem cells colonize mouse testes. Biol Reprod 2001; 64(5):1409–1416. [DOI] [PubMed] [Google Scholar]
- 29. Nagano M, Patrizio P, Brinster RL. Long-term survival of human spermatogonial stem cells in mouse testes. Fertil Steril 2002; 78(6):1225–1233. [DOI] [PubMed] [Google Scholar]
- 30. Hermann BP, Sukhwani M, Lin CC, Sheng Y, Tomko J, Rodriguez M, Shuttleworth JJ, McFarland D, Hobbs RM, Pandolfi PP, Schatten GP, Orwig KE. Characterization, cryopreservation, and ablation of spermatogonial stem cells in adult rhesus macaques. Stem Cells 2007; 25(9):2330–2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Izadyar F, Matthijs-Rijsenbilt JJ, den Ouden K, Creemers LB, Woelders H, de Rooij DG. Development of a cryopreservation protocol for type A spermatogonia. J Androl 2002; 23:537–545. [PubMed] [Google Scholar]
- 32. Oatley JM, Brinster RL. The germline stem cell niche unit in mammalian testes. Physiol Rev 2012; 92(2):577–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ryu BY, Orwig KE, Oatley JM, Avarbock MR, Brinster RL. Effects of aging and niche microenvironment on spermatogonial stem cell self-renewal. Stem Cells 2006; 24(6):1505–1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhang X, Ebata KT, Robaire B, Nagano MC. Aging of male germ line stem cells in mice. Biol Reprod 2006; 74(1):119–124. [DOI] [PubMed] [Google Scholar]
- 35. Mullaney BP, Skinner MK. Basic fibroblast growth factor (bFGF) gene expression and protein production during pubertal development of the seminiferous tubule: follicle-stimulating hormone-induced Sertoli cell bFGF expression. Endocrinology 1992; 131(6):2928–2934. [DOI] [PubMed] [Google Scholar]
- 36. Meng X, Lindahl M, Hyvonen ME, Parvinen M, de Rooij DG, Hess MW, Raatikainen-Ahokas A, Sainio K, Rauvala H, Lakso M, Pichel JG, Westphal H et al. Regulation of cell fate decision of undifferentiated spermatogonia by GDNF. Science 2000; 287(5457):1489–1493. [DOI] [PubMed] [Google Scholar]
- 37. Kubota H, Avarbock MR, Brinster RL. Growth factors essential for self-renewal and expansion of mouse spermatogonial stem cells. Proc Natl Acad Sci USA 2004; 101(47):16489–16494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Martin Laura A, Assif N, Gilbert M, Wijewarnasuriya D, Seandel M. Enhanced fitness of adult spermatogonial stem cells bearing a paternal age-associated FGFR2 mutation. Stem Cell Rep 2014; 3(2):219–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Chen S-R, Liu Y-X.. Regulation of spermatogonial stem cell self-renewal and spermatocyte meiosis by Sertoli cell signaling. Reproduction 2015; 149(4):R159–R167. [DOI] [PubMed] [Google Scholar]
- 40. Oatley MJ, Racicot KE, Oatley JM. Sertoli Cells Dictate Spermatogonial Stem Cell Niches in the Mouse Testis. Biol Reprod 2011; 84(4):639–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kanatsu-Shinohara M, Inoue K, Takashima S, Takehashi M, Ogonuki N, Morimoto H, Nagasawa T, Ogura A, Shinohara T. Reconstitution of mouse spermatogonial stem cell niches in culture. Cell Stem Cell 2012; 11(4):567–578. [DOI] [PubMed] [Google Scholar]
- 42. Yang QE, Kim D, Kaucher A, Oatley MJ, Oatley JM. CXCL12-CXCR4 signaling is required for the maintenance of mouse spermatogonial stem cells. J Cell Sci 2013; 126(4):1009–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Oatley JM, Oatley MJ, Avarbock MR, Tobias JW, Brinster RL. Colony stimulating factor 1 is an extrinsic stimulator of mouse spermatogonial stem cell self-renewal. Development 2009; 136(7):1191–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pitetti J-L, Calvel P, Zimmermann C, Conne B, Papaioannou MD, Aubry F, Cederroth CR, Urner F, Fumel B, Crausaz M, Docquier M, Herrera PL et al. An Essential Role for Insulin and IGF1 Receptors in Regulating Sertoli Cell Proliferation, Testis Size, and FSH Action in Mice. Mol. Endocrinol. 2013; 27(5):814–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. DeFalco T, Potter Sarah J, Williams Alyna V, Waller B, Kan Matthew J, Capel B. Macrophages Contribute to the Spermatogonial Niche in the Adult Testis. Cell Reports 2015; 12(7):1107–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chen S-R, Liu Y-X.. Myh11 -Cre is not limited to peritubular myoid cells and interaction between Sertoli and peritubular myoid cells needs investigation. Proc Natl Acad Sci USA 2016; 113(17):E2352–E2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Chen L-Y, Willis WD, Eddy EM. Targeting the Gdnf Gene in peritubular myoid cells disrupts undifferentiated spermatogonial cell development. Proc Natl Acad Sci USA 2016; 113(7):1829–1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Zhang Y, Wang S, Wang X, Liao S, Wu Y, Han C. Endogenously produced FGF2 is essential for the survival and proliferation of cultured mouse spermatogonial stem cells. Cell Res 2012; 22(4):773–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Matzuk MM, Lamb DJ. The biology of infertility: research advances and clinical challenges. Nat Med 2008; 14(11):1197–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Shinohara T, Avarbock MR, Brinster RL. Functional analysis of spermatogonial stem cells in Steel and cryptorchid infertile mouse models. Dev Biol 2000; 220(2):401–411. [DOI] [PubMed] [Google Scholar]
- 51. Yoshinaga K, Nishikawa S, Ogawa M, Hayashi S, Kunisada T, Fujimoto T. Role of c-kit in mouse spermatogenesis: identification of spermatogonia as a specific site of c-kit expression and function. Development 1991; 113:689–699. [DOI] [PubMed] [Google Scholar]
- 52. Ogawa T, Dobrinski I, Avarbock MR, Brinster RL. Transplantation of male germ line stem cells restores fertility in infertilemice. Nat Med 2000; 6(1):29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Shinohara T, Orwig KE, Avarbock MR, Brinster RL. Restoration of spermatogenesis in infertile mice by sertoli cell transplantation. Biol Reprod 2003; 68(3):1064–1071. [DOI] [PubMed] [Google Scholar]
- 54. Kanatsu-Shinohara M, Miki H, Inoue K, Ogonuki N, Toyokuni S, Ogura A, Shinohara T. Germline niche transplantation restores fertility in infertile mice. Hum Reprod 2005; 20(9):2376–2382. [DOI] [PubMed] [Google Scholar]
- 55. Shinomura M, Kishi K, Tomita A, Kawasumi M, Kanezashi H, Kuroda Y, Tsunekawa N, Ozawa A, Aiyama Y, Yoneda A, Suzuki H, Saito M et al. A novel Amh-Treck transgenic mouse line allows toxin-dependent loss of supporting cells in gonads. Reproduction 2014; 148(6):H1–H9. [DOI] [PubMed] [Google Scholar]
- 56. Jiang FX, Short RV. Male germ cell transplantation in rats: apparent synchronization of spermatogenesis between host and donor seminiferous epithelia. Int J Androl 1995; 18(6):326–330. [DOI] [PubMed] [Google Scholar]
- 57. Ogawa T, Dobrinski I, Brinster RL. Recipient preparation is critical for spermatogonial transplantation in the rat. Tissue Cell 1999; 31(5):461–472. [DOI] [PubMed] [Google Scholar]
- 58. Honaramooz A, Megee SO, Dobrinski I. Germ cell transplantation in pigs. Biol Reprod 2002; 66(1):21–28. [DOI] [PubMed] [Google Scholar]
- 59. Honaramooz A, Behboodi E, Blash S, Megee SO, Dobrinski I. Germ cell transplantation in goats. Mol Reprod Dev 2003; 64(4):422–428. [DOI] [PubMed] [Google Scholar]
- 60. Herrid M, Vignarajan S, Davey R, Dobrinski I, Hill JR. Successful transplantation of bovine testicular cells to heterologous recipients. Reproduction 2006; 132(4):617–624. [DOI] [PubMed] [Google Scholar]
- 61. Kim Y, Turner D, Nelson J, Dobrinski I, McEntee M, Travis AJ. Production of donor-derived sperm after spermatogonial stem cell transplantation in the dog. Reproduction 2008; 136(6):823–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Izadyar F, DenOuden K, Stout T, Stout J, Coret J, Lankveld DP, Spoormakers TJ, Colenbrander B, Oldenbroek JK, VanderPloeg KD, Woelders H, Kal HB et al. Autologous and homologous transplantation of bovine spermatogonial stem cells. Reproduction 2003; 126(6):765–774. [PubMed] [Google Scholar]
- 63. Schlatt S, Rosiepen G, Weinbauer GF, Rolf C, Brook PF, Nieschlag E. Germ cell transfer into rat, bovine, monkey and human testes. Hum Reprod 1999; 14(1):144–150. [DOI] [PubMed] [Google Scholar]
- 64. Mikkola M, Sironen A, Kopp C, Taponen J, Sukura A, Vilkki J, Katila T, Andersson M. Transplantation of normal boar testicular cells resulted in complete focal spermatogenesis in a boar affected by the immotile short-tail sperm defect. Reprod Domest Anim 2006; 41(2):124–128. [DOI] [PubMed] [Google Scholar]
- 65. Rodriguez-Sosa JR, Silvertown JD, Foster RA, Medin JA, Hahnel A. Transduction and transplantation of spermatogonia into the testis of ram lambs through the extra-testicular rete. Reprod Domest Anim 2009; 44(4):612–620. [DOI] [PubMed] [Google Scholar]
- 66. Hermann Brian P, Sukhwani M, Winkler F, Pascarella Julia N, Peters Karen A, Sheng Y, Valli H, Rodriguez M, Ezzelarab M, Dargo G, Peterson K, Masterson K et al. Spermatogonial stem cell transplantation into rhesus testes regenerates spermatogenesis producing functional sperm. Cell Stem Cell 2012; 11(5):715–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Zhang Z, Renfree MB, Short RV. Successful intra- and interspecific male germ cell transplantation in the rat. Biol Reprod 2003; 68(3):961–967. [DOI] [PubMed] [Google Scholar]
- 68. Ryu BY, Orwig KE, Avarbock MR, Brinster RL. Stem cell and niche development in the postnatal rat testis. Dev Biol 2003; 263(2):253–263. [DOI] [PubMed] [Google Scholar]
- 69. Honaramooz A, Behboodi E, Hausler CL, Blash S, Ayres S, Azuma C, Echelard Y, Dobrinski I. Depletion of endogenous germ cells in male pigs and goats in preparation for germ cell transplantation. J Androl 2005; 26(6):698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Oatley JM, Tibary A, de Avila DM, Wheaton JE, McLean DJ, Reeves JJ. Changes in spermatogenesis and endocrine function in the ram testis due to irradiation and active immunization against luteinizing hormone-releasing hormone. J Anim Sci 2005; 83(3):604–612. [DOI] [PubMed] [Google Scholar]
- 71. Stockwell S, Herrid M, Davey R, Brownlee A, Hutton K, Hill JR. Microsatellite detection of donor-derived sperm DNA following germ cell transplantation in cattle. Reprod Fertil Dev 2009; 21(3):462–468. [DOI] [PubMed] [Google Scholar]
- 72. Zeng W, Tang L, Bondareva A, Honaramooz A, Tanco V, Dores C, Megee S, Modelski M, Rodriguez-Sosa JR, Paczkowski M, Silva E, Wheeler M et al. Viral transduction of male germline stem cells results in transgene transmission after germ cell transplantation in pigs. Biol Reprod 2013; 88:(27):21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Honaramooz A, Behboodi E, Megee SO, Overton SA, Galantino-Homer H, Echelard Y, Dobrinski I. Fertility and germline transmission of donor haplotype following germ cell transplantation in immunocompetent goats. Biol Reprod 2003; 69(4):1260–1264. [DOI] [PubMed] [Google Scholar]
- 74. Honaramooz A, Megee S, Zeng W, Destrempes MM, Overton SA, Luo J, Galantino-Homer H, Modelski M, Chen F, Blash S, Melican DT, Gavin WG et al. Adeno-associated virus (AAV)-mediated transduction of male germ line stem cells results in transgene transmission after germ cell transplantation. FASEB J. 2008; 22(2):374–382. [DOI] [PubMed] [Google Scholar]
- 75. Harkey MA, Asano A, Zoulas ME, Torok-Storb B, Nagashima J, Travis A. Isolation, genetic manipulation, and transplantation of canine spermatogonial stem cells: progress toward transgenesis through the male germ-line. Reproduction 2013; 146(1):75–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Herrid M, Olejnik J, Jackson M, Suchowerska N, Stockwell S, Davey R, Hutton K, Hope S, Hill JR. Irradiation enhances the efficiency of testicular germ cell transplantation in sheep. Biol Reprod 2009; 81(5):898–905. [DOI] [PubMed] [Google Scholar]
- 77. Kanatsu-Shinohara M, Ogonuki N, Inoue K, Ogura A, Toyokuni S, Honjo T, Shinohara T. Allogeneic offspring produced by male germ line stem cell transplantation into infertile mouse testis. Biol Reprod 2003; 68(1):167–173. [DOI] [PubMed] [Google Scholar]
- 78. Clouthier DE, Avarbock MR, Maika SD, Hammer RE, Brinster RL. Rat spermatogenesis in mouse testis. Nature 1996; 381(6581):418–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Shinohara T, Kato M, Takehashi M, Lee J, Chuma S, Nakatsuji N, Kanatsu-Shinohara M, Hirabayashi M. Rats produced by interspecies spermatogonial transplantation in mice and in vitro microinsemination. Proc Natl Acad Sci USA 2006; 103(37):13624–13628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Ogawa T, Dobrinski I, Avarbock MR, Brinster RL. Xenogeneic spermatogenesis following transplantation of hamster germ cells to mouse testes. Biol Reprod 1999; 60(2):515–521. [DOI] [PubMed] [Google Scholar]
- 81. França LR, Ogawa T, Avarbock MR, Brinster RL, Russell LD. Germ cell genotype controls cell cycle during spermatogenesis in the rat. Biol Reprod 1998; 59(6):1371–1377. [DOI] [PubMed] [Google Scholar]
- 82. Kim Y, Selvaraj V, Dobrinski I, Lee H, McEntee MC, Travis AJ. Recipient preparation and mixed germ cell isolation for spermatogonial stem cell transplantation in domestic cats. J Androl 2006; 27(2):248–256. [DOI] [PubMed] [Google Scholar]
- 83. Oatley JM, Reeves JJ, McLean DJ. Biological activity of cryopreserved bovine spermatogonial stem cells during in vitro culture. Biol Reprod 2004; 71(3):942–947. [DOI] [PubMed] [Google Scholar]
- 84. Langenstroth D, Kossack N, Westernstroer B, Wistuba J, Behr R, Gromoll J, Schlatt S. Separation of somatic and germ cells is required to establish primate spermatogonial cultures. Hum Reprod 2014; 29(9):2018–2031. [DOI] [PubMed] [Google Scholar]
- 85. Shinohara T, Avarbock MR, Brinster RL beta1- and alpha6-integrin are surface markers on mouse spermatogonial stem cells. Proc Natl Acad Sci USA 1999; 96(10):5504–5509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Grompe M. Tissue stem cells: new tools and functional diversity. Cell Stem Cell 2012; 10(6):685–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Oguro H, Ding L, Morrison Sean J. SLAM family markers resolve functionally distinct subpopulations of hematopoietic stem cells and multipotent progenitors. Cell Stem Cell 2013; 13(1):102–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Tokuda M, Kadokawa Y, Kurahashi H, Marunouchi T. CDH1 is a specific marker for undifferentiated spermatogonia in mouse testes. Biol Reprod 2007; 76(1):130–141. [DOI] [PubMed] [Google Scholar]
- 89. Shinohara T, Orwig KE, Avarbock MR, Brinster RL. Spermatogonial stem cell enrichment by multiparameter selection of mouse testis cells. Proc Natl Acad Sci USA 2000; 97(15):8346–8351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Kubota H, Avarbock MR, Brinster RL. Spermatogonial stem cells share some, but not all, phenotypic and functional characteristics with other stem cells. Proc Natl Acad Sci USA 2003; 100(11):6487–6492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Kanatsu-Shinohara M, Toyokuni S, Shinohara T. CD9 is a surface marker on mouse and rat male germline stem cells. Biol Reprod 2004; 70(1):70–75. [DOI] [PubMed] [Google Scholar]
- 92. Kanatsu-Shinohara M, Morimoto H, Shinohara T. Enrichment of mouse spermatogonial stem cells by melanoma cell adhesion molecule expression. Biol Reprod 2012; 87(6):139. [DOI] [PubMed] [Google Scholar]
- 93. Kubota H, Brinster RL. Culture of rodent spermatogonial stem cells, male germline stem cells of the postnatal animal. Methods Cell Biol 2008; 86:59–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Lo KC, Brugh VM 3rd, Parker M, Lamb DJ. Isolation and enrichment of murine spermatogonial stem cells using rhodamine 123 mitochondrial dye. Biol Reprod 2005; 72(3):767–771. [DOI] [PubMed] [Google Scholar]
- 95. Kanatsu-Shinohara M, Mori Y, Shinohara T. Enrichment of mouse spermatogonial stem cells based on aldehyde dehydrogenase activity. Biol Reprod 2013; 89(6):140. [DOI] [PubMed] [Google Scholar]
- 96. Kanatsu-Shinohara M, Kato-Itoh M, Ikawa M, Takehashi M, Sanbo M, Morioka Y, Tanaka T, Morimoto H, Hirabayashi M, Shinohara T. Homologous recombination in rat germline stem cells. Biol Reprod 2011; 85(1):208–217. [DOI] [PubMed] [Google Scholar]
- 97. Kanatsu-Shinohara M, Morimoto H, Shinohara T. Enrichment of mouse spermatogonial stem cells by the stem cell dye CDy11. Biol Reprod 2016; 94:(13):13, 1-10. [DOI] [PubMed] [Google Scholar]
- 98. Komai Y, Tanaka T, Tokuyama Y, Yanai H, Ohe S, Omachi T, Atsumi N, Yoshida N, Kumano K, Hisha H, Matsuda T, Ueno H. Bmi1 expression in long-term germ stem cells. Sci Rep 2015; 4(1):6175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Ohmura M, Yoshida S, Ide Y, Nagamatsu G, Suda T, Ohbo K. Spatial analysis of germ stem cell development in Oct-4/EGFP transgenic mice. Arch Histol Cytol 2004; 67(4):285–296. [DOI] [PubMed] [Google Scholar]
- 100. Ohbo K, Yoshida S, Ohmura M, Ohneda O, Ogawa T, Tsuchiya H, Kuwana T, Kehler J, Abe K, Scholer HR, Suda T. Identification and characterization of stem cells in prepubertal spermatogenesis in mice. Dev Biol 2003; 258:209–225. [DOI] [PubMed] [Google Scholar]
- 101. Yoshida S, Takakura A, Ohbo K, Abe K, Wakabayashi J, Yamamoto M, Suda T, Nabeshima Y. Neurogenin3 delineates the earliest stages of spermatogenesis in the mouse testis. Dev Biol 2004; 269(2):447–458. [DOI] [PubMed] [Google Scholar]
- 102. Sada A, Suzuki A, Suzuki H, Saga Y. The RNA-binding protein NANOS2 is required to maintain murine spermatogonial stem cells. Science 2009; 325(5946):1394–1398. [DOI] [PubMed] [Google Scholar]
- 103. Chan F, Oatley MJ, Kaucher AV, Yang QE, Bieberich CJ, Shashikant CS, Oatley JM. Functional and molecular features of the Id4+ germline stem cell population in mouse testes. Genes Dev 2014; 28(12):1351–1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Aloisio GM, Nakada Y, Saatcioglu HD, Peña CG, Baker MD, Tarnawa ED, Mukherjee J, Manjunath H, Bugde A, Sengupta AL, Amatruda JF, Cuevas I et al. PAX7 expression defines germline stem cells in the adult testis. J Clin Invest 2014; 124(9):3929–3944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Pech MF, Garbuzov A, Hasegawa K, Sukhwani M, Zhang RJ, Benayoun BA, Brockman SA, Lin S, Brunet A, Orwig KE, Artandi SE. High telomerase is a hallmark of undifferentiated spermatogonia and is required for maintenance of male germline stem cells. Genes Dev 2015; 29(23):2420–2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Hara K, Nakagawa T, Enomoto H, Suzuki M, Yamamoto M, Simons BD, Yoshida S. Mouse spermatogenic stem cells continually interconvert between equipotent singly isolated and syncytial states. Cell Stem Cell 2014; 14(5):658–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Barroca V, Lassalle B, Coureuil M, Louis JP, Le Page F Testart J, Allemand I, Riou L, Fouchet P. Mouse differentiating spermatogonia can generate germinal stem cells in vivo. Nat Cell Biol 2009; 11(2):190–196. [DOI] [PubMed] [Google Scholar]
- 108. Zheng K, Wu X, Kaestner KH, Wang PJ. The pluripotency factor LIN28 marks undifferentiated spermatogonia in mouse. BMC Dev Biol 2009; 9(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Nagano M, Avarbock MR, Leonida EB, Brinster CJ, Brinster RL. Culture of mouse spermatogonial stem cells. Tissue Cell 1998; 30(4):389–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Matsui Y, Zsebo K, Hogan BL. Derivation of pluripotential embryonic stem cells from murine primordial germ cells in culture. Cell 1992; 70(5):841–847. [DOI] [PubMed] [Google Scholar]
- 111. Resnick JL, Bixler LS, Cheng L, Donovan PJ. Long-term proliferation of mouse primordial germ cells in culture. Nature 1992; 359(6395):550–551. [DOI] [PubMed] [Google Scholar]
- 112. Smith AG, Heath JK, Donaldson DD, Wong GG, Moreau J, Stahl M, Rogers D. Inhibition of pluripotential embryonic stem cell differentiation by purified polypeptides. Nature 1988; 336(6200):688–690. [DOI] [PubMed] [Google Scholar]
- 113. Williams RL, Hilton DJ, Pease S, Willson TA, Stewart CL, Gearing DP, Wagner EF, Metcalf D, Nicola NA, Gough NM. Myeloid leukaemia inhibitory factor maintains the developmental potential of embryonic stem cells. Nature 1988; 336(6200):684–687. [DOI] [PubMed] [Google Scholar]
- 114. Nagano M, Ryu BY, Brinster CJ, Avarbock MR, Brinster RL. Maintenance of mouse male germ line stem cells in vitro. Biol Reprod 2003; 68(6):2207–2214. [DOI] [PubMed] [Google Scholar]
- 115. Lin LF, Doherty DH, Lile JD, Bektesh S, Collins F. GDNF: a glial cell line-derived neurotrophic factor for midbrain dopaminergic neurons. Science 1993; 260(5111):1130–1132. [DOI] [PubMed] [Google Scholar]
- 116. Yomogida K, Yagura Y, Tadokoro Y, Nishimune Y. Dramatic expansion of germinal stem cells by ectopically expressed human glial cell line-derived neurotrophic factor in mouse Sertoli cells. Biol Reprod 2003; 69(4):1303–1307. [DOI] [PubMed] [Google Scholar]
- 117. Kanatsu-Shinohara M, Ogonuki N, Inoue K, Miki H, Ogura A, Toyokuni S, Shinohara T. Long-term proliferation in culture and germline transmission of mouse male germline stem cells. Biol Reprod 2003; 69(2):612–616. [DOI] [PubMed] [Google Scholar]
- 118. Kanatsu-Shinohara M, Inoue K, Lee J, Yoshimoto M, Ogonuki N, Miki H, Baba S, Kato T, Kazuki Y, Toyokuni S, Toyoshima M, Niwa O et al. Generation of pluripotent stem cells from neonatal mouse testis. Cell 2004; 119(7):1001–1012. [DOI] [PubMed] [Google Scholar]
- 119. Kanatsu-Shinohara M, Inoue K, Lee J, Miki H, Ogonuki N, Toyokuni S, Ogura A, Shinohara T. Anchorage-independent growth of mouse male germline stem cells in vitro. Biol Reprod 2006; 74(3):522–529. [DOI] [PubMed] [Google Scholar]
- 120. Guan K, Nayernia K, Maier LS, Wagner S, Dressel R, Lee JH, Nolte J, Wolf F, Li M, Engel W, Hasenfuss G. Pluripotency of spermatogonial stem cells from adult mouse testis. Nature. 2006; 440(7088):1199–1203. [DOI] [PubMed] [Google Scholar]
- 121. Ko K, Tapia N, Wu G, Kim JB, Bravo MJ, Sasse P, Glaser T, Ruau D, Han DW, Greber B, Hausdorfer K, Sebastiano V et al. Induction of pluripotency in adult unipotent germline stem cells. Cell Stem Cell 2009; 5(1):87–96. [DOI] [PubMed] [Google Scholar]
- 122. Seandel M, James D, Shmelkov SV, Falciatori I, Kim J, Chavala S, Scherr DS, Zhang F, Torres R, Gale NW, Yancopoulos GD, Murphy A et al. Generation of functional multipotent adult stem cells from GPR125+ germline progenitors. Nature 2007; 449(7160):346–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Naughton CK, Jain S, Strickland AM, Gupta A, Milbrandt J. Glial cell-line derived neurotrophic factor-mediated RET signaling regulates spermatogonial stem cell fate. Biol Reprod 2006; 74(2):314–321. [DOI] [PubMed] [Google Scholar]
- 124. Takashima S, Kanatsu-Shinohara M, Tanaka T, Morimoto H, Inoue K, Ogonuki N, Jijiwa M, Takahashi M, Ogura A, Shinohara T. Functional differences between GDNF-dependent and FGF2-dependent mouse spermatogonial stem cell self-renewal. Stem Cell Rep 2015; 4(3):489–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Kubota H, Reid LM. Clonogenic hepatoblasts, common precursors for hepatocytic and biliary lineages, are lacking classical major histocompatibility complex class I antigen. Proc Natl Acad Sci USA 2000; 97(22):12132–12137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Schmitt RM, Bruyns E, Snodgrass HR. Hematopoietic development of embryonic stem cells in vitro: cytokine and receptor gene expression. Genes Dev 1991; 5(5):728–740. [DOI] [PubMed] [Google Scholar]
- 127. Wei X, Jia Y, Xue Y, Geng L, Wang M, Li L, Wang M, Zhang X, Wu X. GDNF-expressing STO feeder layer supports the long-term propagation of undifferentiated mouse spermatogonia with stem cell properties. Sci Rep 2016; 6(1):36779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Paratcha G, Ledda F, Baars L, Coulpier M, Besset V, Anders J, Scott R, Ibanez CF. Released GFRalpha1 potentiates downstream signaling, neuronal survival, and differentiation via a novel mechanism of recruitment of c-Ret to lipid rafts. Neuron 2001; 29(1):171–184. [DOI] [PubMed] [Google Scholar]
- 129. Kubota H, Avarbock MR, Schmidt JA, Brinster RL. Spermatogonial stem cells derived from infertile Wv/Wv mice self-renew in vitro and generate progeny following transplantation. Biol Reprod 2009; 81(2):293–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Helsel AR, Oatley MJ, Oatley JM. Glycolysis-optimized conditions enhance maintenance of regenerative integrity in mouse spermatogonial stem cells during long-term culture. Stem Cell Rep 2017; 8(5):1430–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Ryu BY, Kubota H, Avarbock MR, Brinster RL. Conservation of spermatogonial stem cell self-renewal signaling between mouse and rat. Proc Natl Acad Sci USA 2005; 102(40):14302–14307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Hamra FK, Chapman KM, Nguyen DM, Williams-Stephens AA, Hammer RE, Garbers DL. Self renewal, expansion, and transfection of rat spermatogonial stem cells in culture. Proc Natl Acad Sci USA 2005; 102(48):17430–17435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Ryu BY, Orwig KE, Kubota H, Avarbock MR, Brinster RL. Phenotypic and functional characteristics of spermatogonial stem cells in rats. Dev Biol 2004; 274(1):158–170. [DOI] [PubMed] [Google Scholar]
- 134. Brewer GJ, Torricelli JR, Evege EK, Price PJ. Optimized survival of hippocampal neurons in B27-supplemented neurobasal, a new serum-free medium combination. J Neurosci Res 1993; 35(5):567–576. [DOI] [PubMed] [Google Scholar]
- 135. Wu Z, Falciatori I, Molyneux LA, Richardson TE, Chapman KM, Hamra FK. Spermatogonial culture medium: an effective and efficient nutrient mixture for culturing rat spermatogonial stem cells. Biol Reprod 2009; 81(1):77–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Kanatsu-Shinohara M, Miki H, Inoue K, Ogonuki N, Toyokuni S, Ogura A, Shinohara T. Long-term culture of mouse male germline stem cells under serum-or feeder-free conditions. Biol Reprod 2005; 72(4):985–991. [DOI] [PubMed] [Google Scholar]
- 137. Kubota H, Wu X, Goodyear SM, Avarbock MR, Brinster RL. Glial cell line-derived neurotrophic factor and endothelial cells promote self-renewal of rabbit germ cells with spermatogonial stem cell properties. FASEB J 2011; 25(8):2604–2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Catzeflis FM, Dickerman AW, Michaux J, Kirsch JAW. DNA Hybridization and Rodent Phylogeny. New York: Springer Verlag; 1993:159–172. [Google Scholar]
- 139. Novacek MJ. Mammalian phylogeny: shaking the tree. Nature 1992; 356(6365):121–125. [DOI] [PubMed] [Google Scholar]
- 140. González R, Dobrinski I. Beyond the mouse monopoly: studying the male germ line in domestic animal models. ILAR J 2015; 56(1):83–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Hamra FK, Schultz N, Chapman KM, Grellhesl DM, Cronkhite JT, Hammer RE, Garbers DL. Defining the spermatogonial stem cell. Dev Biol 2004; 269(2):393–410. [DOI] [PubMed] [Google Scholar]
- 142. Oatley MJ, Kaucher AV, Yang Q-E, Waqas MS, Oatley JM. Conditions for long-term culture of cattle undifferentiated spermatogonia. Biol Reprod 2016; 95(14):1–10. [DOI] [PubMed] [Google Scholar]
- 143. Honaramooz A, Yang Y. Recent advances in application of male germ cell transplantation in farm animals. Vet Med Int 2011; 2011:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Sadri-Ardekani H, Mizrak SC, van Daalen SK, Korver CM, Roepers-Gajadien HL, Koruji M, Hovingh S, de Reijke TM, de la Rosette JJ, van dV, de Rooij DG, Repping S et al. Propagation of human spermatogonial stem cells in vitro. JAMA. 2009; 302:2127–2134. [DOI] [PubMed] [Google Scholar]
- 145. Lim JJ, Sung SY, Kim HJ, Song SH, Hong JY, Yoon TK, Kim JK, Kim KS, Lee DR. Long-term proliferation and characterization of human spermatogonial stem cells obtained from obstructive and non-obstructive azoospermia under exogenous feeder-free culture conditions. Cell Prolif 2010; 43:405–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Kokkinaki M, Djourabtchi A, Golestaneh N. Long-term culture of human SSEA-4 positive spermatogonial stem cells (SSCs). J Stem Cell Res Ther 2011; S2:003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Guo Y, Liu L, Sun M, Hai Y, Li Z, He Z. Expansion and long-term culture of human spermatogonial stem cells via the activation of SMAD3 and AKT pathways. Exp Biol Med (Maywood) 2015; 240:1112–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Conrad S, Azizi H, Hatami M, Kubista M, Bonin M, Hennenlotter J, Renninger M, Skutella T. Differential gene expression profiling of enriched human spermatogonia after short- and long-term culture. BioMed Res Int 2014; 2014:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Koruji M, Shahverdi A, Janan A, Piryaei A, Lakpour MR, Gilani Sedighi MA. Proliferation of small number of human spermatogonial stem cells obtained from azoospermic patients. J Assist Reprod Genet 2012; 29:957–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. He Z, Kokkinaki M, Jiang J, Dobrinski I, Dym M. Isolation, characterization, and culture of human spermatogonia. Biol Reprod 2010; 82:363–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Sadri-Ardekani H, Akhondi MA, van der Veen F, Repping S, van Pelt AM. In vitro propagation of human prepubertal spermatogonial stem cells. JAMA 2011; 305:2416–2418. [DOI] [PubMed] [Google Scholar]
- 152. Kossack N, Terwort N, Wistuba J, Ehmcke J, Schlatt S, Schöler H, Kliesch S, Gromoll J. A combined approach facilitates the reliable detection of human spermatogonia in vitro. Hum Reprod 2013; 28:3012–3025. [DOI] [PubMed] [Google Scholar]
- 153. Zheng Y, Thomas A, Schmidt CM, Dann CT. Quantitative detection of human spermatogonia for optimization of spermatogonial stem cell culture. Hum Reprod 2014; 29:2497–2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Medrano JV, Rombaut C, Simon C, Pellicer A, Goossens E. Human spermatogonial stem cells display limited proliferation in vitro under mouse spermatogonial stem cell culture conditions. Fertil Steril 2016; 106:1539–1549.e8. [DOI] [PubMed] [Google Scholar]
- 155. Valli H, Sukhwani M, Dovey SL, Peters KA, Donohue J, Castro CA, Chu T, Marshall GR, Orwig KE. Fluorescence- and magnetic-activated cell sorting strategies to isolate and enrich human spermatogonial stem cells. Fertil Steril 2014; 102:566–580.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Wu X, Schmidt JA, Avarbock MR, Tobias JW, Carlson CA, Kolon TF, Ginsberg JP, Brinster RL. Prepubertal human spermatogonia and mouse gonocytes share conserved gene expression of germline stem cell regulatory molecules. Proc Natl Acad Sci USA 2009; 106:21672–21677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Neuhaus N, Yoon J, Terwort N, Kliesch S, Seggewiss J, Huge A, Voss R, Schlatt S, Grindberg RV, Schöler HR. Single-cell gene expression analysis reveals diversity among human spermatogonia. Mol Hum Reprod 2017; 23:79–90. [DOI] [PubMed] [Google Scholar]
- 158. von Kopylow K, Schulze W, Salzbrunn A, Spiess AN. Isolation and gene expression analysis of single potential human spermatogonial stem cells. Mol Hum Reprod 2016; 22:229–239. [DOI] [PubMed] [Google Scholar]
- 159. Mizrak SC, Chikhovskaya JV, Sadri-Ardekani H, van Daalen S, Korver CM, Hovingh SE, Roepers-Gajadien HL, Raya A, Fluiter K, de Reijke TM, de la Rosette JJ, Knegt AC et al. Embryonic stem cell-like cells derived from adult human testis. Hum Reprod 2010; 25:158–167. [DOI] [PubMed] [Google Scholar]
- 160. Kossack N, Meneses J, Shefi S, Nguyen HN, Chavez S, Nicholas C, Gromoll J, Turek PJ, Reijo-Pera RA. Isolation and characterization of pluripotent human spermatogonial stem cell-derived cells. Stem Cells 2009; 27:138–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Golestaneh N, Kokkinaki M, Pant D, Jiang J, DeStefano D, Fernandez-Bueno C, Rone JD, Haddad BR, Gallicano GI, Dym M. Pluripotent stem cells derived from adult human testes. Stem Cells Dev 2009; 18:1115–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Chikhovskaya JV, van Daalen SK, Korver CM, Repping S, van Pelt AM. Mesenchymal origin of multipotent human testis-derived stem cells in human testicular cell cultures. Mol Hum Reprod 2014; 20:155–167. [DOI] [PubMed] [Google Scholar]
- 163. Chikhovskaya JV, Jonker MJ, Meissner A, Breit TM, Repping S, van Pelt AM. Human testis-derived embryonic stem cell-like cells are not pluripotent, but possess potential of mesenchymal progenitors. Hum Reprod 2012; 27:210–221. [DOI] [PubMed] [Google Scholar]
- 164. Nakagawa T, Sharma M, Nabeshima YI, Braun RE, Yoshida S. Functional hierarchy and reversibility within the murine spermatogenic stem cell compartment. Science. 2010328:62–67;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Honaramooz A, Snedaker A, Boiani M, Schöler H, Dobrinski I, Schlatt S. Sperm from neonatal mammalian testes grafted in mice. Nature 2002; 418:778–781. [DOI] [PubMed] [Google Scholar]
- 166. Shinohara T, Inoue K, Ogonuki N, Kanatsu-Shinohara M, Miki H, Nakata K, Kurome M, Nagashima H, Toyokuni S, Kogishi K, Honjo T, Ogura A. Birth of offspring following transplantation of cryopreserved immature testicular pieces and in-vitro microinsemination. Hum Reprod 2002; 17:3039–3045. [DOI] [PubMed] [Google Scholar]
- 167. Oatley JM, Avarbock MR, Telaranta AI, Fearon DT, Brinster RL. Identifying genes important for spermatogonial stem cell self-renewal and survival. Proc Natl Acad Sci USA 2006; 103:9524–9529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Wu X, Oatley JM, Oatley MJ, Kaucher AV, Avarbock MR, Brinster RL. The POU domain transcription factor POU3F1 is an important intrinsic regulator of GDNF-induced survival and self-renewal of mouse spermatogonial stem cells. Biol Reprod 2010; 82:1103–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Wu X, Goodyear SM, Tobias JW, Avarbock MR, Brinster RL. Spermatogonial stem cell self-renewal requires ETV5-mediated downstream activation of brachyury in mice. Biol Reprod 2011; 85:1114–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Oatley JM, Avarbock MR, Brinster RL. Glial cell line-derived neurotrophic factor regulation of genes essential for self-renewal of mouse spermatogonial stem cells is dependent on Src family kinase signaling. J Biol Chem 2007; 282:25842–25851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Braydich-Stolle L, Kostereva N, Dym M, Hofmann MC. Role of Src family kinases and N-Myc in spermatogonial stem cell proliferation. Dev Biol 2007; 304:34–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Lee J, Kanatsu-Shinohara M, Inoue K, Ogonuki N, Miki H, Toyokuni S, Kimura T, Nakano T, Ogura A, Shinohara T. Akt mediates self-renewal division of mouse spermatogonial stem cells. Development 2007; 134:1853–1859. [DOI] [PubMed] [Google Scholar]
- 173. Tyagi G, Carnes K, Morrow C, Kostereva NV, Ekman GC, Meling DD, Hostetler C, Griswold M, Murphy KM, Hess RA, Hofmann M-C, Cooke PS. Loss of Etv5 decreases proliferation and RET levels in neonatal mouse testicular germ cells and causes an abnormal first wave of spermatogenesis. Biol Reprod 2009; 81:258–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Niu Z, Goodyear SM, Rao S, Wu X, Tobias JW, Avarbock MR, Brinster RL. MicroRNA-21 regulates the self-renewal of mouse spermatogonial stem cells. Proc Natl Acad Sci USA 2011; 108:12740–12745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Chen C, Ouyang W, Grigura V, Zhou Q, Carnes K, Lim H, Zhao GQ, Arber S, Kurpios N, Murphy TL, Cheng AM, Hassell JA et al. ERM is required for transcriptional control of the spermatogonial stem cell niche. Nature 2005; 436:1030–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Li L, Wang M, Wang M, Wu X, Geng L, Xue Y, Wei X, Jia Y, Wu X. A long non-coding RNA interacts with Gfra1 and maintains survival of mouse spermatogonial stem cells. Cell Death Dis 2016; 7:e2140–e2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Chen J, Cai T, Zheng C, Lin X, Wang G, Liao S, Wang X, Gan H, Zhang D, Hu X, Wang S, Li Z et al. MicroRNA-202 maintains spermatogonial stem cells by inhibiting cell cycle regulators and RNA binding proteins. Nucleic Acids Res 2017; 45:4142–4157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Helsel AR, Yang Q-E, Oatley MJ, Lord T, Sablitzky F, Oatley JM. ID4 levels dictate the stem cell state in mouse spermatogonia. Development 2017; 144:624–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Sun F, Xu Q, Zhao D, Degui Chen C. Id4 Marks spermatogonial stem cells in the mouse testis. Sci Rep 2015; 5:624–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Falender AE, Freiman RN, Geles KG, Lo KC, Hwang K, Lamb DJ, Morris PL, Tjian R, Richards JS. Maintenance of spermatogenesis requires TAF4b, a gonad-specific subunit of TFIID. Genes Dev 2005; 19:794–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Costoya JA, Hobbs RM, Barna M, Cattoretti G, Manova K, Sukhwani M, Orwig KE, Wolgemuth DJ, Pandolfi PP. Essential role of Plzf in maintenance of spermatogonial stem cells. Nat Genet 2004; 36:653–659. [DOI] [PubMed] [Google Scholar]
- 182. Buaas FW, Kirsh AL, Sharma M, McLean DJ, Morris JL, Griswold MD, de Rooij DG, Braun RE. Plzf is required in adult male germ cells for stem cell self-renewal. Nat Genet 2004; 36:647–652. [DOI] [PubMed] [Google Scholar]
- 183. Hu Y-C, de Rooij DG, Page DC. Tumor suppressor gene Rb is required for self-renewal of spermatogonial stem cells in mice. Proc Natl Acad Sci USA 2013; 110:12685–12690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Song H-W, Wilkinson MF. Transcriptional control of spermatogonial maintenance and differentiation. Semin Cell Dev Biol 2014; 30:14–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Goriely A, McVean GA, Rojmyr M, Ingemarsson B, Wilkie AO. Evidence for selective advantage of pathogenic FGFR2 mutations in the male germ line. Science 2003; 301:643–646. [DOI] [PubMed] [Google Scholar]
- 186. Goriely A, McVean GA, van Pelt AM, O’Rourke AW, Wall SA, de Rooij DG, Wilkie AO. Gain-of-function amino acid substitutions drive positive selection of FGFR2 mutations in human spermatogonia. Proc Natl Acad Sci USA 2005; 102:6051–6056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Ishii K, Kanatsu-Shinohara M, Toyokuni S, Shinohara T. FGF2 mediates mouse spermatogonial stem cell self-renewal via upregulation of Etv5 and Bcl6b through MAP2K1 activation. Development 2012; 139:1734–1743. [DOI] [PubMed] [Google Scholar]
- 188. Brinster RL. Germline stem cell transplantation and transgenesis. Science 2002; 296:2174–2176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189. Nagano M, Brinster CJ, Orwig KE, Ryu BY, Avarbock MR, Brinster RL. Transgenic mice produced by retroviral transduction of male germ-line stem cells. Proc Natl Acad Sci USA 2001; 98:13090–13095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Kanatsu-Shinohara M, Ikawa M, Takehashi M, Ogonuki N, Miki H, Inoue K, Kazuki Y, Lee J, Toyokuni S, Oshimura M, Ogura A, Shinohara T. Production of knockout mice by random or targeted mutagenesis in spermatogonial stem cells. Proc Natl Acad Sci USA 2006; 103:8018–8023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Shinohara T, Kazuki K, Ogonuki N, Morimoto H, Matoba S, Hiramatsu K, Honma K, Suzuki T, Hara T, Ogura A, Oshimura M, Kanatsu-Shinohara M et al. Transfer of a mouse artificial chromosome into spermatogonial stem cells generates transchromosomic mice. Stem Cell Rep 2017; 9:1180–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Sato T, Sakuma T, Yokonishi T, Katagiri K, Kamimura S, Ogonuki N, Ogura A, Yamamoto T, Ogawa T. Genome editing in mouse spermatogonial stem cell lines using TALEN and double-nicking CRISPR/Cas9. Stem Cell Rep 2015; 5:75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Wu Y, Zhou H, Fan X, Zhang Y, Zhang M, Wang Y, Xie Z, Bai M, Yin Q, Liang D, Tang W, Liao J et al. Correction of a genetic disease by CRISPR-Cas9-mediated gene editing in mouse spermatogonial stem cells. Cell Res 2015; 25:67–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Hamra FK, Gatlin J, Chapman KM, Grellhesl DM, Garcia JV, Hammer RE, Garbers DL. Production of transgenic rats by lentiviral transduction of male germ-line stem cells. Proc Natl Acad Sci USA 2002; 99:14931–14936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Ryu BY, Orwig KE, Oatley JM, Lin CC, Chang LJ, Avarbock MR, Brinster RL. Efficient generation of transgenic rats through the male germline using lentiviral transduction and transplantation of spermatogonial stem cells. J Androl 2007; 28:353–360. [DOI] [PubMed] [Google Scholar]
- 196. Chapman KM, Medrano GA, Jaichander P, Chaudhary J, Waits AE, Nobrega MA, Hotaling JM, Ober C, Hamra FK. Targeted germline modifications in rats using CRISPR/Cas9 and spermatogonial stem cells. Cell Rep 2015; 10:1828–1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Bosley KS, Botchan M, Bredenoord AL, Carroll D, Charo RA, Charpentier E, Cohen R, Corn J, Doudna J, Feng G, Greely HT, Isasi R et al. CRISPR germline engineering—the community speaks. Nat Biotechnol 2015; 33:478–486. [DOI] [PubMed] [Google Scholar]
- 198. Brinster RL. Male germline stem cells: from mice to men. Science 2007; 316:404–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Kubota H, Brinster RL. Technology insight: In vitro culture of spermatogonial stem cells and their potential therapeutic uses. Nat Clin Pract Endocrinol Metab 2006; 2:99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Ginsberg JP, Carlson CA, Lin K, Hobbie WL, Wigo E, Wu X, Brinster RL, Kolon TF. An experimental protocol for fertility preservation in prepubertal boys recently diagnosed with cancer: a report of acceptability and safety. Hum Reprod 2010; 25:37–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Ginsberg JP, Li Y, Carlson CA, Gracia CR, Hobbie WL, Miller VA, Mulhall J, Shnorhavorian M, Brinster RL, Kolon TF. Testicular tissue cryopreservation in prepubertal male children: an analysis of parental decision-making. Pediatr Blood Cancer 2014; 61:1673–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Dovey SL, Valli H, Hermann BP, Sukhwani M, Donohue J, Castro CA, Chu T, Sanfilippo JS, Orwig KE. Eliminating malignant contamination from therapeutic human spermatogonial stem cells. J Clin Invest 2013; 123:1833–1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Hayashi K, Ogushi S, Kurimoto K, Shimamoto S, Ohta H, Saitou M. Offspring from oocytes derived from in vitro primordial germ cell-like cells in mice. Science 2012; 338:971–975. [DOI] [PubMed] [Google Scholar]
- 204. Ishikura Y, Yabuta Y, Ohta H, Hayashi K, Nakamura T, Okamoto I, Yamamoto T, Kurimoto K, Shirane K, Sasaki H, Saitou M. In vitro derivation and propagation of spermatogonial stem cell activity from mouse pluripotent stem cells. Cell Rep 2016; 17:2789–2804. [DOI] [PubMed] [Google Scholar]