Abstract
Background
Supraglottic jet oxygenation and ventilation (SJOV) can effectively maintain adequate oxygenation in patients with respiratory depression, even in apnea patients. However, there have been no randomized controlled clinical trials of SJOV in obese patients. This study investigated the efficacy and safety of SJOV using WEI Nasal Jet tube (WNJ) for obese patients who underwent hysteroscopy under intravenous anesthesia without endotracheal intubation.
Methods
A single-center, prospective, randomized controlled study was conducted. The obese patients receiving hysteroscopy under intravenous anesthesia were randomly divided into three groups: Control group maintaining oxygen supply via face masks (100% oxygen, flow at 6 L/min), the WNJ Oxygen Group with WNJ (100% oxygen, flow: 6 L/min) and the WNJ SJOV Group with SJOV via WNJ [Jet ventilator working parameters:100% oxygen supply, driving pressure (DP) 0.1 MPa, respiratory rate; (RR): 15 bpm, I/E; ratio 1:1.5]. SpO2, PETCO2, BP, HR, ECG and BIS were continuously monitored during anesthesia. Two-Diameter Method was deployed to measure cross sectional area of the gastric antrum (CSA-GA) by ultrasound before and after SJOV in the WNJ SJOV Group. Episodes of SpO2 less than 95%, PETCO2 less than 10 mmHg, depth of WNJ placement and measured CSA-GA before and after jet ventilation in the WNJ SJOV Group during the operation were recorded. The other adverse events were collected as well.
Results
A total of 102 patients were enrolled, with two patients excluded. Demographic characteristics were similar among the three groups. Compared with the Control Group, the incidence of PETCO2 < 10 mmHg, SpO2 < 95% in the WNJ SJOV group dropped from 36 to 9% (P = 0.009),from 33 to 6% (P = 0.006) respectively,and the application rate of jaw-lift decreased from 33 to 3% (P = 0.001), and the total percentage of adverse events decreased from 36 to 12% (P = 0.004). Compared with the WNJ Oxygen Group, the use of SJOV via WNJ significantly decreased episodes of SpO2 < 95% from 27 to 6% (P = 0.023), PETCO2 < 10 mmHg from 33 to 9% (P = 0.017), respectively. Depth of WNJ placement was about 12.34 cm in WNJ SJOV Group. There was no significantly difference of CSA-GA before and after SJOV in the WNJ SJOV Group (P = 0.234). There were no obvious cases of nasal bleeding in all the three groups.
Conclusions
SJOV can effectively and safely maintain adequate oxygenation in obese patients under intravenous anesthesia without intubation during hysteroscopy. This efficient oxygenation may be mainly attributed to supplies of high concentration oxygenation to the supraglottic area, and the high pressure jet pulse providing effective ventilation. Although the nasal airway tube supporting collapsed airway by WNJ also plays a role. SJOV doesn’t seem to increase gastric distension and the risk of aspiration. SJOV can improve the safety of surgery by reducing the incidence of the intraoperative involuntary limbs swing, hip twist and cough.
Trial registration
Chinese Clinical Trial Registry. Registration number, ChiCTR1800017028, registered on July 9, 2018.
Keywords: Jet ventilation, Supraglottic, Obesity, Anesthesia, Gastric antrum, Ultrasound, Hysteroscopy
Background
It is estimated that more than 100,000 patients receive hysteroscopy each year in China. Usually, hysteroscopy is accomplished under intravenous (IV) anesthesia or sedation without endotracheal intubation, primarily with IV propofol and remifentanil [1]. Endoscopic sedation and analgesia by propofol/remifentanil have been significantly increased during the past 10 years [2]. Remedial oxygenation by the jaw lift or pressurized mask ventilation is usually performed to manage anesthesia/sedation mediated respiratory depression, especially in obese patients. Supraglottic jet oxygenation and ventilation (SJOV) is aimed at oxygenation and ventilation in patient with depressed respiration or apnea, and have been demonstrated effective in difficult airway management without significant complications [3]. However, it is unclear whether SJOV can be used effectively and safely to maintain adequate oxygenation/ventilation in obese patients during hysteroscopy under intravenous sedation. The efficacy and safety of SJOV via nasopharyngeal approach in the obese patients needs further elucidated, although recent case reports [4, 5] and several clinical trials [6–8] delineated effectiveness of SJOV maintaining oxygenation in the non-obese patients. The Wei Nasal Jet Tube (WNJ, Well Lead Medical Co. Ltd., Guangzhou, China. number: 20170501) with an inner diameter of 5.0 mm, outer diameter of 7.5 mm, and a length of 18 cm is a newly invented nasal tube [9]. Here, we conducted a single-blind, prospective, randomized controlled study, and hypothesized SJOV using WNJ can reduce adverse events of hypoxia and hypoventilation in obese patients under IV anesthesia with propofol and remifentanil during hysteroscopy, without tracheal intubation.
Methods
Ethics, consent and permissions
This study was approved by the local Ethics Committee of Peking University People’s Hospital (No. 2018PHB036–01). Informed written consent was obtained from the obese patients who underwent hysteroscopy between July and September 2018. This study adhered to the Consolidated Standards of Reporting Trials (CONSORT) guidelines.
Study design
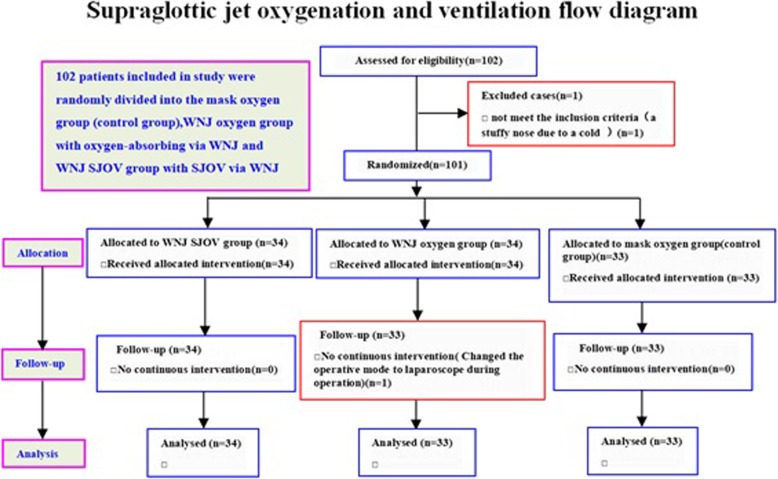
Patients were randomized to the mask oxygen group (Control Group) maintaining oxygen absorption via face mask (100% oxygen, flow at 6 L/min), the WNJ oxygen group with WNJ (100% oxygen, flow at 6 L/min) and the WNJ SJOV group with SJOV via WNJ [Jet ventilator working parameters:100% oxygen supply, driving pressure (DP) 0.1 MPa, respiratory rate (RR): 15 bpm, I/E ratio 1:1.5]. The Sample Size was calculated by SAS, considering at least a 90 and 60% reduction in patients with SpO2 reduction in WNJ SJOV group and WNJ oxygen group compared to that in control group by the preliminary test. With a standard deviation of 0.8, and bilaterally equal to 0.05, or even 0.2 (power = 0.8), estimated value of each group should be 34 cases (n = 2(μα + μβ)2σ2/δ2 with 20% shedding rate). The randomization was performed by random number table from the SPSS23.0, and the blinding was completed by one medical student and two anesthesiologists. Patients were labeled with WNJ SJOV, WNJ or Control by One anesthesiologist, and the other anesthesiologist administered the intravenous anesthesia and maintained oxygenation. The flow diagram of this study was shown in Fig. 1.
Fig. 1.
Supraglottic jet oxygenation and ventilation flow diagram. A total of 102 patients with BMI > 30 receiving hysteroscopy were randomly divided into three groups: the mask oxygen group (control group) maintaining oxygen absorption via face mask (N = 33), the WNJ oxygen group maintaining oxygen absorption via WNJ(N = 33) and the WNJ SJOV group maintaining SJOV via WNJ(N = 34). One patient in the control group was excluded because of stuffy nose due to a cold(N = 1). The other patient in WNJ oxygen group was abandoned intervention due to change of the operative mode during operation(N = 1)
Patients
In-patients receiving routine hysteroscopy under IV anesthesia with propofol and remifentanil were recruited. Inclusion criteria were as follows: (1) 18 yrs. < age < 65 yrs.; (2) BMI > 30 kg/m2; (3) Fasting for 8 h and no water for 4 h before surgery; (1) ASA class: I-II classes. Exclusion criteria were as follows: (1) Epistaxis; (2) Nasal stenosis; (3) Long-term use of anticoagulants; (4) Rhinitis episodes; (5) Severe reflux disease; (6) History of severe respiratory, cardiovascular and cerebrovascular diseases.
Anesthesia
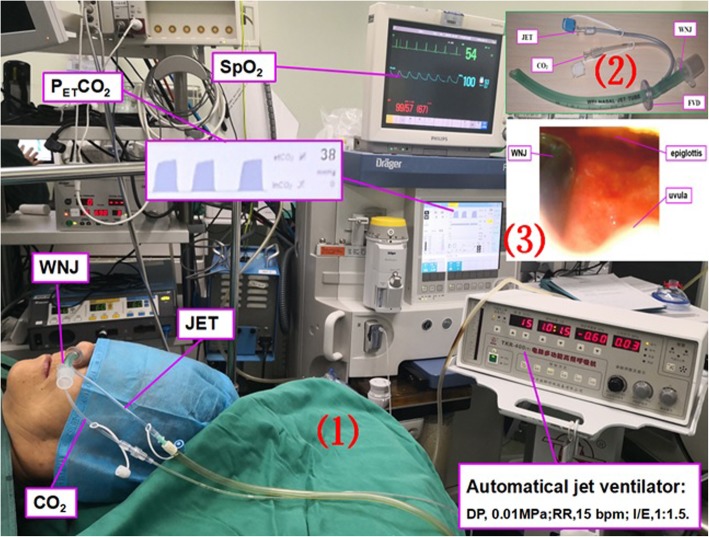
Induction of anesthesia was conducted by IV injection of propofol (1.5–2 mg/kg) and remifentanil (0.5 μg/kg). Anesthesia was maintained by continuous IV infusion of propofol (3-5 mg/kg/h) and remifentanil (0.05–0.08μg/kg/ min). After anesthesia induction, the face mask in control group, the WNJ in WNJ oxygen group and WNJ SJOV group were placed appropriately straightway. Before putting WNJ into the unobstructed nostril of patients, a paraffin oil cotton swab was used to clear the nasal cavity and about 1 ml lidocaine ointment was smeared on the tip of WNJ (the depth was equivalent to the distance from the alar to the ipsilateral earlobe [3]. The jet catheter of the WNJ was connected to an automated jet ventilator-TKR-400 (Well Lead Medical Equipment Ltd. Guangzhou, China.) (Fig. 2). Bispectral index (BIS) was maintained at 45–60 [additional propofol (0.3–0.5 mg/kg) was given with one bolus infusion if needed] and SpO2 was maintained above 95%. A dose of ephedrine (3–6 mg) was administered as needed in order to maintain the mean arterial pressure above 55 mmHg. Remedial measures were executed immediately in the setting of oxygen saturation (SpO2) < 95%, including adjusting the WNJ position (1 cm deep or shallow) in the WNJ SJOV group and the WNJ oxygen group, and taking jaw-lift maneuver in the three groups. Mask pressurized ventilation was used to provide oxygen only when SpO2 < 90% happened in all the three groups.
Fig. 2.
(1) The scene of supraglottic jet oxygenation and ventilation (SJOV) via WNJ with or without spontaneous breathing. SJOV could maintain oxygen saturation and carbon dioxide exhalation. PETCO2 = End-tidal carbon dioxide partial pressure; SpO2 = pulse oxygen saturation;DP = driving pressure;RR = respiratory rate; I/E ratio = inhalation/exhalation ratio. (2) Wei Nasal Jet tube (WNJ), which has two channels built inside the tube wall for jet ventilation and the end-tidal pressure of CO2 monitoring, respectively. FVD = fixed valve of depth. (3) The position of the WNJ into the laryngopharynx observed by nasal fiberoptic scope. The depth of placement of the WNJ was about equivalent to the distance from the alar to the ipsilateral earlobe. The best site for WNJ insertion under fiber bronchoscope was between the epiglottis and uvula
Intraoperative monitoring
We continuously monitored following parameters during the anesthesia: pulse SpO2, End-tidal carbon dioxide partial pressure (PETCO2), mean blood pressure (MBP), heart rate (HR), electrocardiogram (ECG) and BIS. SpO2 < 95% and PETCO2 < 10 mmHg were considered hypoxic adverse event and hyperventilation, respectively [10]. Two-Diameter Method was used to measure antral cross-sectional area of gastric antrum (CSA-GA) by ultrasound [Vivid, GE MEDICAL SYSTEMS CO.,LTD, China] with patients in the supine position before and after SJOV in the WNJ SJOV group, using the sagittal plane measurement at the xiphoid process level, with the help of the anatomical markers (the superior mesenteric artery,the left liver lobe and abdominal aorta) (Fig. 3). The diameter of antero-posterior and cranio-caudal antral was expressed as AP and CC, respectively, with a π of 3.1416 during CSA = (AP × CC × π)/4. Stomach volume was estimated and calculated by estimated stomach volume (ESV) = 27.0 + 14.6 × CSA-1.28 × age (yrs) [11, 12].
Fig. 3.
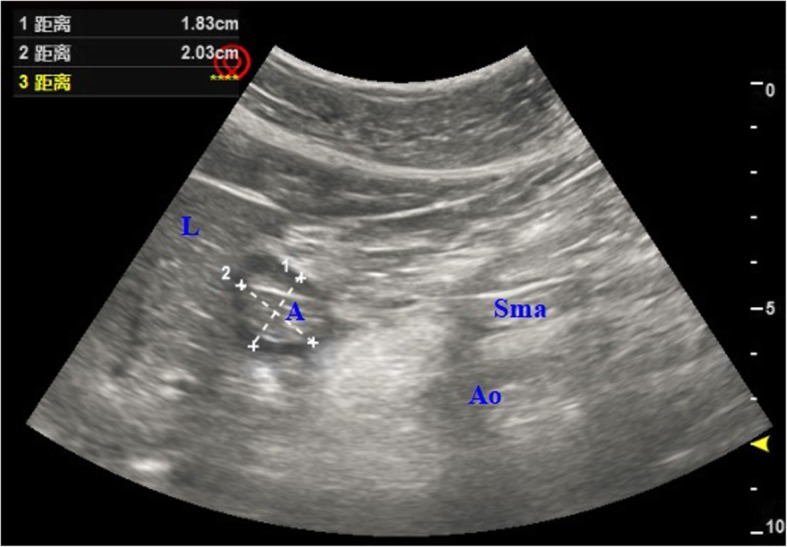
Two-Diameter Method was carried out to measure antral CSA by ultrasound before and after SJOV in the WNJ SJOV group. GA = Gastric antrum, Ao = aorta, Sma = superior mesenteric artery, L = liver. The antero-posterior (AP) antral diameter was expressed as dotted line 1,The cranio-caudal (CC) antral diameter was represented by dotted line 2,and π was 3.1416 during CSA = (AP × CC × π)/4
Episodes of SpO2 less than 95% and PETCO2 less than 10 mmHg during the operation were recorded. The other adverse events such as hip twist, cough, nasal bleeding and remedial interventions such as jaw-lift, pressure mask, depth of WNJ placement were also noted. Types and time of surgery, recovery time of anesthesia, dose of anesthetics, measured CSA-GA before and after jet ventilation in the WNJ SJOV group were also recorded.
Statistical analysis
The measurement data was expressed as mean ± SD and the count data was presented as the number and percentage. Kruskal-wallis single factor ANOVA test was used to compare the difference of time of surgery, recovery time of anesthesia, dosage of anesthetics between different groups. The data about depth of WNJ placement between the WNJ SJOV and the WNJ oxygen groups was analyzed by Wilcoxon rank sum test. Independent sample t-test was used for comparing the CSA-GA and ESV before and after jet ventilation in the WNJ SJOV group. Categorical variables as the cases of SpO2 less than 95%, PETCO2 less than 10 mmHg, hip twist, nasal bleeding, and patients requiring jaw-lift, pressured mask ventilation, as well as other perioperative adverse reactions were all analyzed withchi-square test and Fisher’s exact test. All data was analyzed with SPSS23.0 statistical software (SPSS Inc., Chicago, IL, USA). A value of p < 0.05 was considered the difference was statistically significant.
Results
A total of 102 patients were enrolled. One patient in the control group was excluded because of stuffy nose due to catching a cold, and another patient in WNJ oxygen group was removed because of change of the operative mode during operation. All the patients tolerated the hysteroscopy well. There were no serious adverse events (i.e. aspiration, laryngospasm, nasal bleeding post operation, barotrauma and death).
Clinical characteristics of study population
The clinical characteristics of patients was represented in Table 1. Age, height, weight, BMI, ASA classification, airway-related parameters, (including mouth opening degree, thyromental distance, neck circumference, Mallampati class), snore history, and obstructive sleep apnea hypoventilation syndrome (OSAHS) were compared. Data of the surgical and anesthesia procedure, adverse events and remedial interventions were analyzed in Table 2.
Table 1.
General information of patients in the three groups and the surgical types. The differences among the three groups and between each two groups were not statistically significant(p > 0.05)
| Characteristic (mean ± SD) | mask oxygen(I) (N = 33) | WNJ oxygen (II) (N = 33) | WNJ SJOV (III) (N = 34) |
|---|---|---|---|
| Age (yr.) | 44.7 ± 11.65 | 44.1 ± 12.86 | 43.8 ± 15.22 |
| Height (cm) | 155.6 ± 5.56 | 154.4 ± 7.23 | 156.3 ± 8.23 |
| Weight (kg) | 80.3 ± 6.05 | 79.2 ± 10.34 | 80.5 ± 5.17 |
| BMI (kg.m−2) | 33.18 ± 2.87 | 33.23 ± 3.22 | 32.97 ± 2.36 |
| mouth opening(I)(II)(III)(IV) | (32)(1)(0)(0) | (33)(0)(0)(0) | (33)(1)(0)(0) |
| thyromental Distance(I)(II)(III) | (27)(5)(1) | (28)(5)(0) | (30)(4)(0) |
| neck circumference(I)(II)(III) | (11)(19)(3) | (13)(18)(2) | (10)(20)(4) |
| mallampati class (I)(II)(III)(IV) | (8)(23)(2)(0) | (7)(22)(4)(0) | (8)(22)(4)(0) |
| Snore history [n (%)] | 11 (33%) | 13 (39%) | 13 (38%) |
| OSAHS [n (%)] | 0 (0%) | 0 (0%) | 1 (3%) |
| ASA(I)(II) | (28)(5) | (30)(3) | (30)(4) |
| surgical types of hysteroscopy | |||
| TCRP [n(%)] | 4 (12) | 5 (15) | 6 (18) |
| TCRM [n(%)] | 6 (18) | 5 (15) | 6 (18) |
| TCRS [n(%)] | 11 (33) | 12 (36) | 11 (32) |
| TCRA [n(%)] | 12 (36) | 11 (33) | 11 (32) |
BMI body mass index; Mouth opening(I/II/III/IV):I > 4.0 cm, II 2.5–3.0 cm, III 1.2–2.0 cm, and IV < 1.0 cm; Thyromental distance (I/II/III): I > 6.5 cm, II 6–6.5 cm, and III < 6 cm; Neck circumference(I/II/III): I < 35 cm, II 35–41 cm, and III > 41 cm; OSAHS obstructive sleep apnea hypoventilation syndrome, SJOV supraglottic jet oxygenation and ventilation, WNJ Wei nasal jet tube, TCRP transcervical polyp resection, TCRM transcervical hysteroscopy fibroid resection, TCRS transcervical resection of septa, TCRA transcervical resection of adhesions
Table 2.
Data about the procedure, drugs dosage, adverse events and remedial interventions. Compared with the mask oxygen or WNJ oxygen groups, the use of SJOV via WNJ during the surgery significantly decreased the total percentage of adverse events and surgical time, cases of SpO2 < 95% and PETCO2 < 10 mmHg, and the application rate of jaw-lift
| Monitored variables [n (%)] | mask oxygen(I) (N = 33) | WNJ oxygen (II) (N = 33) | WNJ SJOV (III) (N = 34) | P-Value (I VS II) | P-Value (I VS III) | P-Value (II VS III) | P |
|---|---|---|---|---|---|---|---|
| Surgical time (min) | 24.28 ± 10.18 | 23.19 ± 9.72 | 22.56 ± 5.91 | 0.053 | 0.013 | 0.053 | 0.027 (Kruskal-wallis) |
| Anesthesia recovery (min) | 14.73 ± 5.59 | 13.22 ± 3.73 | 13.97 ± 4.12 | 0.068 | 0.217 | 0.866 | 0.061 (Kruskal-wallis) |
| WNJ placement depth (cm) | – | 12.22 ± 0.54 | 12.34 ± 0.47 | – | – | 0.087a | – |
| Propofol dose (mg) | 207.01 ± 62.85 | 212.57 ± 51.44 | 225.01 ± 48.63 | 1.000 | 0.002 | < 0.001 | < 0.001 (Kruskal-wallis) |
| Remifentanil dose (μg) | 32.28 ± 6.18 | 33.02 ± 8.27 | 33.21 ± 4.97 | 0.059 | 0.244 | 0.196 | 0.079 (Kruskal-wallis) |
| Ephedrine dose (mg) | 5.14 ± 1.03 | 5.23 ± 1.16 | 5.25 ± 1.10 | 0.516 | 0.417 | 0.975 | 0.022 (Kruskal-wallis) |
| Total adverse events | 12 (36) | 13 (39) | 4 (12) | 1.000 | 0.004 | 0.002 | 0.013 |
| Intra-operation | |||||||
| SpO2 < 95% | 11 (33) | 9 (27) | 2 (6) | 0.789 | 0.006 | 0.023 | 0.017 |
| PETCO2 < 10 mmHg | 12 (36) | 11 (33) | 3 (9) | 1.000 | 0.009 | 0.017 | 0.019 |
| Jaw-lift | 11 (33) | 10 (30) | 1 (3) | 1.000 | 0.001 | 0.003 | 0.004 |
| Mask pressurized ventilation | 5 (15) | 3 (9) | 0 (0) | 0.708 | 0.025 | 0.114 | 0.071 |
| Oropharyngeal tube | 2 (6) | 0 (0) | 0 (0) | 0.492 | 0.239 | – | 0.126 |
| Nasal bleeding | 0 (0) | 1 (3) | 2 (6) | 1.000 | 0.493 | 1.000 | 0.369 |
| Cough | 3 (9) | 1 (3) | 1 (3) | 0.613 | 0.356 | 1.000 | 0.420 |
| Laryngospasm | 0 (0) | 0 (0) | 0 (0) | – | – | – | – |
| Aspiration | 0 (0) | 0 (0) | 0 (0) | – | – | – | – |
| Hip twist | 2 (6) | 1 (3) | 0 (0) | 1.000 | 0.239 | 0.493 | 0.348 |
| Bradycardia | 9 (27) | 8 (24) | 4 (12) | 1.000 | 0.132 | 0.217 | 0.254 |
| Tachycardia | 2 (6) | 1 (3) | 0 (0) | 1.000 | 0.239 | 0.493 | 0.348 |
| Hypertension | 5 (15) | 4 (12) | 1 (3) | 1.000 | 0.105 | 0.197 | 0.221 |
| Hypotension | 1 (3) | 1 (3) | 3 (9) | 1.000 | 0.614 | 0.614 | 0.453 |
| Post-operation | |||||||
| Nausea or Vomiting | 1 (3) | 2 (6) | 1 (3) | 1.000 | 1.000 | 0.614 | 0.761 |
| Pharyngalgia | 2 (6) | 3 (9) | 3 (9) | 1.000 | 1.000 | 1.000 | 0.881 |
| Xerostomia | 2 (6) | 3 (9) | 4 (12) | 1.000 | 0.427 | 0.709 | 0.488 |
| Nasal bleeding | 0 (0) | 0 (0) | 0 (0) | – | – | – | – |
| Barotrauma | 0 (0) | 0 (0) | 0 (0) | – | – | – | – |
SpO2: pulse oxygen saturation; PETCO2: End-tidal carbon dioxide partial pressure; SJOV:supraglottic jet oxygenation and ventilation; WNJ: Wei nasal jet tube
Primary outcome
Adverse events of hypoxia and hypoventilation
The majority of patients had shown good wave form and good values of PETCO2 during SJOV. Compared with the Control Group, the incidence of PETCO2 < 10 mmHg,SpO2 < 95% in the WNJ SJOVgroup dropped from 36 to 9% (P = 0.009), from 33 to 6% (P = 0.006) respectively, and the application rate of jaw-lift decreased from 33 to 3% (P = 0.001), and the total percentage of adverse events decreased from 36 to 12% (P = 0.004). Compared with the WNJ Oxygen Group, the use of SJOV via WNJ significantly decreased episodes of SpO2 < 95% from 27 to 6% (P = 0.023), PETCO2 < 10 mmHg from 33 to 9% (P = 0.017), respectively. There were no significant differences in episodes of SpO2 < 95% and PETCO2 < 10 mmHg between the WNJ Oxygen Group and the Control Group (P = 0.789 and P = 1.000). (Table 2).
Secondary outcome
Incidence of the nasal bleeding, cough and hip twist
There were three cases of nasal bleeding (a small amount of blood attached WNJ) during operation in this study. One occurred in WNJ oxygen group, the other two cases happened in WNJ SJOV group. On the second day after surgery, these three patients had no other symptoms except feeling slight dry and itching in the throat.
There were no significant differences in the cough and hip twist among three groups (P = 0.420 and P = 0.348). However, compared with the Control Group, SJOV could slightly decrease the incidence of cough from 9 to 3% (P = 0.356) and hip twist from 6 to 0% (P = 0.239) (Table 2).
Incidence of the nausea or vomiting, pharyngalgia, and xerostomia after surgery, changes of CSA-GA and ESV
There were no significant differences in the nausea or vomiting, pharyngalgia and xerostomia among three groups after surgery (P = 0.761, P = 0.488 and P = 0.881).(Table 2). The changes of the CSA-GA and ESV were not significant before and after supraglottic jet ventilation in the WNJ SJOV Group (P = 0.234 and P = 0.777). (Table 3).
Table 3.
Two-Diameter Method was used to measure CSA-GA by ultrasound. Stomach volume was estimated and calculated by ESV = 27.0 + 14.6 × CSA-1.28 × age (years). Compared with before jet ventilation, CSA-GA and ESV after jet ventilation had not been increased in the WNJ SJOV group (p > 0.05)
| Monitored variables | Before WNJ SJOV (N = 34) | After WNJ SJOV (N = 34) | P-Value (before VS after) |
|---|---|---|---|
| CSA-GA (cm2) | 3.32 ± 0.59 | 3.34 ± 0.56 | 0.234 |
| ESV (ml) | 18.78 ± 6.68 | 18.89 ± 6.59 | 0.777 |
CSA-GA cross sectional area of the gastric antrum, ESV Estimated stomach volume, SJOV supraglottic jet oxygenation and ventilation, WNJ Wei nasal jet tube
Propofol dosage
Compared with the Control Group and the WNJ Oxygen Group, respectively, the dosage of propofol in the WNJ SJOV Group increased significantly (P = 0.002, P < 0.001).
Discussion
Hysteroscopy is one of the most common procedures in gynecology [1]. Involuntary limbs swing and hip twist should be avoided during hysteroscopy surgery [13], considering that it not only increases potential risk of uterine perforation but adding extra burden to operation. Therefore, sufficient depth of anesthesia and analgesic intensity is required. Admittedly, intraspinal anesthesia can provide adequate analgesia and satisfactory patient cooperation, but it is not conducive to rapid postoperative recovery of patients [14]. With the application of propofol and remifentanil in clinical practice, short IV anesthesia is possible and can be easily accepted by surgeons and patients. At present, IV anesthesia becomes a trend in hysteroscopy [1]. Majholm, an obstetrician and gynecologist in Denmark, believed that although the time of hysteroscopy surgery under non-intubation IV anesthesia was similar to that under intraspinal anesthesia or intubation general anesthesia, the length of hospital stay reduced and patients’ satisfactions were improved [15]. However, while providing satisfactory anesthesia and rapid patients’ recovery, anesthesiologists must guarantee a difficult task, that is adequate oxygenation and ventilation of patients. Therefore, the key to anesthesia management in hysteroscopy surgery is how to balance the short time, analgesic intensity and anesthesia depth with airway safety of patients. Shallow anesthesia is unable to meet surgery needs, however, deep anesthesia may lead to significant airway collapse. When the depth of anesthesia is sufficient for the operation, supplemental oxygen was proved to be an effective intervention measure to improve oxygenation and ventilation. These common measures include nasal catheter, mask, jaw-lift, or pressurized mask ventilation, which require the patient to maintain an autonomous breathing. Usually, pressurized mask ventilation is used as the last attempt in the settings of non-artificial airway assisted-ventilation [2]. However, this ventilation mode is easy to make stomach flatulence, and increase the risk of gastric reflux and aspiration [16]. Obesity is a multisystem, chronic, proinflammatory disorder, and specific care is needed for airway management [17]. Leakage is likely to occur when airway pressure is more than 20cmH2O for the patients with obesity under intravenous general anesthesia using laryngeal mask, and ventilation and oxygenation are affected. When the airway pressure exceeds 25cmH2O, it is easy to increase gastric distension and the risk of aspiration [18].
Transnasal humidified rapid insufflation ventilatory exchange (THRIVE) is a new approach to enhance oxygenation [19]. THRIVE has the advantage of increasing oxygen concentration, removing carbon dioxide from the ineffective chamber, and maintaining positive airway pressure, thus improving lung compliance and reducing upper airway obstruction [20]. However, in terms of upper airway obstruction, jet ventilation, which was developed in 1967, has the same enhanced oxygenation advantage as THRIVE, although they work in different ways [21, 22].
Jostrand from Sweden first introduced the technology of using 60 to 100 breaths per minute, which was called high frequency positive pressure ventilation (HFPPV) [23]. Klein studied the HFPPV and renamed the system as high frequency jet ventilation (HFJV) [24]. Since then, HFJV has become a technique to maintain ventilation. The application of this technique enables rapid pulsation gas to enter the respiratory tract through a narrow jet tube under low pressure [25, 26]. HFJV has three characteristics [27–29], open system, high-frequency (> 60 bpm) and low tidal volume. Transtracheal jet ventilation (TTJV) is one of the popular methods of emergency airway management in the ASA guide, but barotrauma is a severe complication that damper the excitement to use it [30–32]. The characteristics of supraglottic jet ventilation (SJV) are that can be used as the ventilation of emergency airway, and auxiliary oxygenation of difficult airway, with more open ventilating system, less complications, and low requirement for spontaneous breathing [33]. Advantages of WNJ are jetting ventilation via side hole, releasing gas from the main hole and surrounding upper airway space, and reduction of barotrauma.
In addition to observing chest fluctuation, PETCO2 can also be monitored [34] [Fig. 2(2)]. In this study, we successfully applied SJOV via WNJ to decrease the episodes of hypoxia and hypoventilation for the patients receiving hysteroscopy surgery under IV anesthesia by propofol and remifentanil. This efficient oxygenation may be accomplished primarily by jet ventilation, though nasal airway tube supporting collapsed airway also plays a role. Additionally, SJOV was seemed to improve the safety of surgery by reducing the incidence of the intraoperative involuntary limbs swing and hip twist, cough, and stomach flatulence.
The scene of SJOV via WNJ was shown in Fig. 2(1). With or without spontaneous breathing, both oxygenation and carbon dioxide exhalation were well maintained. The depth of placing the WNJ was equivalent to the distance from the alar to the ipsilateral earlobe. Meanwhile, we located the front-end of WNJ by fibro bronchoscope and found that the best site for WNJ oxygenation was between epiglottis and uvula in the WNJ SJOV Group. The distance was about 12.34 cm [Fig. 2(3)]. Oxygenation effect can be maintained better in the WNJ SJOV Group than that in the WNJ Oxygen Group, although the same WNJs were used for the patients in both groups. Accordingly, we believe the role of maintaining oxygenation was mainly jet ventilation rather than propping up the collapsed airway with or without spontaneous respiration. For obese patients, it was usually difficult to perform hysteroscopy surgery under general IV anesthesia without intubation and maintain proper intensity of spontaneous breathing without respiratory depression under the guarantee of surgical safety. Therefore, WNJ SJOV had more advantages in enhancing oxygenation than WNJ alone.
Theoretically, SJV can make the WNJ front end swing, which may cause damage to the throat soft tissue. However, we did not find such kind of swing under the fiberoptic bronchoscopy. The possible reasons were that the curved part of the nasal cavity of WNJ weakened the airflow impact, and the jet ventilation through the WEJ side hole reduced the airflow and the airflow pressure. SJV via WNJ (WNJ SJV) could provide adequate ventilation, although it is less effective than transtracheal jet ventilation (TTJV). However, WNJ SJV could significantly reduce the complications of TTJV, such as barotrauma. WNJ SJV within 25 min did not increase incidence of postoperative laryngopharyngeal pain, cough and ability of discharge of sputum, suggesting that this technique may not produce inflammatory reaction caused by damage of airway mucosa and throat soft tissue.
Although the mechanisms about the respiratory depressant effect of propofol have not been fully explained, it is clear that propofol causes the respiratory depressant effect in a dose-dependent manner [35]. When mask/nasopharyngeal tube oxygen is used to maintain oxygenation under propofol sedation, propofol dosage is often reduced involuntary due to respiratory depressant, which will increase the incidence of the intraoperative involuntary limbs swing, hip twist and cough. The respiratory depressant effect may be not worried with/without spontaneous respiration during SJOV via WNJ to maintain oxygenation under propofol sedation. The short duration of hysteroscopy and the small total dosage of propofol which did not lead to the difference in anesthesia recovery, although there were differences in the dosage of propofol among the three groups.
Although it had been reported that SJV can maintain 1 h oxygenation, but it was not suitable for longer time application [8]. Appropriate use time and whether it will cause airway mucosal inflammation remains to be observed in large-sample multi-center randomized controlled trials in the future. Previous anesthesiologists criticize that this methods may not be sensitive enough to monitor gastric volume and extension by ultrasound. The CSA-GA in the evaluation of gastric flatulence may seemed to have poor quantitative accuracy, but it could provide some qualitative reference value in clinical application, so making efforts to explore this field was required in the future work.
The shortcomings of this trial are reflected in the small sample size, which cannot fully reflect the real situation of adverse reactions. The position of the patient during ultrasound examination is not the optimal position.
Conclusions
SJOV can effectively and safely maintain adequate oxygenation in obese patients under intravenous anesthesia without intubation during hysteroscopy. This efficient oxygenation may be mainly attributed to supplies of high concentration oxygen to the supraglottic area, and the high pressure jet pulse providing effective ventilation. Although the nasal airway tube supporting collapsed airway by WNJ also plays a role. SJOV doesn’t seem to increase gastric distension and the risk of aspiration. SJOV can improve the safety of surgery by reducing the incidence of the intraoperative involuntary limbs swing, hip twist and cough.
Acknowledgements
We thank Dr. Xin Yang, Dr. Xudong Liang and Dr. Yi Li from department of gynaecology, Peking University people’s hospital for their understanding, support and cooperation in this clinical trial, and for making some pertinent suggestions.
Abbreviations
- Ao
aorta
- AP
Antero-posterior
- ASA
American Society of Anesthesiologists
- BIS
Bispectral index
- BMI
body mass index
- CC
cranio-caudal
- CONSORT
Consolidated standards of reporting trials
- CSA-GA
Cross sectional area of the gastric antrum
- DP
Driving pressure
- ECG
Electrocardiogram
- ESV
Estimated stomach volume
- FVD
Fixed valve of depth
- GA
Gastric antrum
- HFJV
High frequency jet ventilation
- HR
Heart rate
- I/E ratio
Inhalation/exhalation ratio
- IV
Intravenous
- L
Liver
- MBP
Mean blood pressure
- OSAHS
Obstructive sleep apnea hypoventilation syndrome
- PETCO2
End-tidal carbon dioxide partial pressure
- RR
Respiratory rate
- SJOV
Supraglottic jet oxygenation and ventilation
- SJV
Supraglottic jet ventilation
- Sma
Superior mesenteric artery
- SpO2
Pulse oxygen saturation
- TCRA
Transcervical resection of adhesions
- TCRM
Transcervical hysteroscopy fibroid resection
- TCRP
Transcervical polyp resection
- TCRS
Transcervical resection of septa
- THRIVE
Transnasal humidified rapid insufflation ventilatory exchange
- TTJV
Transtracheal jet ventilation
- WNJ
Wei Nasal Jet tube
Authors’ contributions
Study conception: YF, HL, HW. Study design: YF, HL. Study conduct: YF, HL, QL. Data analysis: HL,YH, LS. Data interpretation: HW, YH, LS, QL. Drafting of the manuscript: YF, HL. All authors approved the final version of the manuscript.
Funding
The authors declare that they have no funding.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Ethical approval has been confirmed from the Ethics Committee of Peking University People’s Hospital (ref approval number: No. 2018PHB036–01). Informed written consent was obtained from the obese patients who underwent hysteroscopy between July and September 2018.
Consent for publication
Not applicable.
Competing interests
Huafeng Wei is the inventor of the WEI Nasal Jet Tube (WEI NASAL JET or WNJ), which was used to generate SJOV in this study. The University of Pennsylvania has been granted following patients: International Patent Number PCT/US/70253, 2013.; U.S.A. Patent Number 61779379, 2013, 9669182B2, 2017; China Patent Number 201380044238.8, 2018; European Patent Number 2863976, 2018; Japan Patent Number P6343287, 2018; Australia Patent Number 2013344546, 2018. Dr. Wei is also a paid consult form Well Lead company which make and commercialize the WNJ. The other authors have no potential competing interests to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hansheng Liang, Email: doctorlianghsh@sina.com.
Yuantao Hou, Email: houyuantao2013@163.com.
Liang Sun, Email: heimingway1984@163.com.
Qingyue Li, Email: liqy04534@163.com.
Huafeng Wei, Email: weih@uphs.upenn.edu.
Yi Feng, Email: fengyimzk@163.com.
References
- 1.Sloth SB, Schroll JB, Settnes A, et al. Systematic review of the limited evidence for different surgical techniques at benign hysterectomy: a clinical guideline initiated by the Danish health authority. Eur J Obstet Gynecol Reprod Biol. 2017;216(2):169–177. doi: 10.1016/j.ejogrb.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 2.Mazanikov M, Udd M, Kylänpää L, et al. Patient-controlled sedation with propofol and remifentanil for ERCP: a randomized, controlled study. Gastrointest Endosc. 2011;73(2):260–266. doi: 10.1016/j.gie.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Wei HF. A new tracheal tube and methods to facilitate ventilation and placement in emergency airway management. Resuscitation. 2006;70:438–444. doi: 10.1016/j.resuscitation.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 4.Xie P, Li Q, Wei H, et al. Supraglottic jet oxygenation and ventilation saved a patient with 'cannot intubate and cannot ventilate' emergency difficult airway. J Anesth. 2017;31(1):144–147. doi: 10.1007/s00540-016-2279-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dziewit JA, Wei H. Supraglottic jet ventilation assists intubation in a Marfan's syndrome patient with a difficult airway. J Clin Anesth. 2011;23:407–409. doi: 10.1016/j.jclinane.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 6.Qin Y, Li LZ, Su DS, et al. Supraglottic jet oxygenation and ventilation enhances oxygenation during upper gastrointestinal endoscopy in patients sedated with propofol: a randomized multicentre clinical trial. Br J Anaesth. 2017;119(1):158–166. doi: 10.1093/bja/aex091. [DOI] [PubMed] [Google Scholar]
- 7.PENG J, YE J, ZHAO Y, et al. Supraglottic jet ventilation in difficult airway management. J Emerg Med. 2012;43:382–390. doi: 10.1016/j.jemermed.2011.06.145. [DOI] [PubMed] [Google Scholar]
- 8.Wu CN, Ma WH, Wei JQ, et al. Laryngoscope and a new tracheal tube assist lightwand intubation in difficult airways due to unstable cervical spine. PLoS One. 2015;10(3):e0120231. doi: 10.1371/journal.pone.0120231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.LEVITT C, WEI H. Supraglotic pulsatile jet oxygen ventilation during deep propofol sedation for upper gastrointestinal endoscopy in a morbidly obese patient. J Clin Anesth. 2014;26:157–159. doi: 10.1016/j.jclinane.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 10.Athayde RAB, Oliveira Filho JRB, Lorenzi Filho G, et al. Obesity hypoventilation syndrome: a current review. J Bras Pneumol. 2018;44(6):510–518. doi: 10.1590/s1806-37562017000000332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van de Putte P, Vernieuwe L. When fasted is not empty: a retrospective cohort study of gastric content in fasted surgical patients. Br J Anaesth. 2017;118(3):363–371. doi: 10.1093/bja/aew435. [DOI] [PubMed] [Google Scholar]
- 12.Van de Putte P, Vernieuwe L, Perlas A. Term pregnant patients have similar gastric volume to non-pregnant females: a single-centre cohort study. Br J Anaesth. 2019;122(1):79–85. doi: 10.1016/j.bja.2018.07.025. [DOI] [PubMed] [Google Scholar]
- 13.Cai HL, Pan LY, Wang SF, et al. Discussion on operative skills in the embolization of hydrosalpinx by hysteroscopic placement of a microcoil. Medicine. 2019;98(11):e14721. doi: 10.1097/MD.0000000000014721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Munmany M, Gracia M, Nonell R, et al. The use of inhaled sevoflurane during operative hysteroscopy is associated with increased glycine absorption compared to intravenous propofol for maintenance of anesthesia. J Clin Anesth. 2016;31:202–207. doi: 10.1016/j.jclinane.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 15.Majholm B, Bartholdy J, Clausen HV, et al. Comparison between local anaesthesia with remifentanil and total intravenous anaesthesia for operative hysteroscopic procedures in day surgery. Br J Anaesth. 2012;108(2):245–253. doi: 10.1093/bja/aer337. [DOI] [PubMed] [Google Scholar]
- 16.An X, Ye H, Chen J, Lu B. Effect of positive end-expiratory pressure on overlap between internal jugular vein and carotid artery in mechanically ventilated patients with laryngeal mask airway (LMA) insertion - a prospective randomized trial. Med Sci Monit. 2019;25:2305–2310. doi: 10.12659/MSM.913595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Petrini F, Di Giacinto I, Cataldo R, et al. Perioperative and periprocedural airway management and respiratory safety for the obese patient: 2016 SIAARTI consensus. Minerva Anestesiol. 2016;82(12):1314–1335. [PubMed] [Google Scholar]
- 18.Wang H, Gao X, Wei W, et al. The optimum sevoflurane concentration for supraglottic airway device blockbuster™ insertion with spontaneous breathing in obese patients: a prospective observational study. BMC Anesthesiol. 2017;17(1):156. doi: 10.1186/s12871-017-0449-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.George S, Humphreys S, Williams T, et al. Transnasal Humidified Rapid Insufflation Ventilatory Exchange in children requiring emergent intubation (Kids THRIVE): a protocol for a randomised controlled trial. BMJ Open. 2019;9(2):e025997. doi: 10.1136/bmjopen-2018-025997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hermez LA, Spence CJ, Payton MJ, et al. A physiological study to determine the mechanism of carbon dioxide clearance during apnoea when using transnasal humidified rapid insufflation ventilatory exchange (THRIVE) Anaesthesia. 2019;74(4):441–449. doi: 10.1111/anae.14541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Toussaint M, Gonçalves M, Chatwin M. Effects of mechanical insufflation-exsufflation on the breathing pattern in stable subjects with duchenne muscular dystrophy: a step in a wrong direction. Respir Care. 2019;64(2):235–236. doi: 10.4187/respcare.06495. [DOI] [PubMed] [Google Scholar]
- 22.Philips R. deSilva B, Matrka L.Jet ventilation in obese patients undergoing airway surgery for subglottic and tracheal stenosis. Laryngoscope. 2018;128(8):1887–1892. doi: 10.1002/lary.27059. [DOI] [PubMed] [Google Scholar]
- 23.Altun D, Çamcı E, Orhan-Sungur M, et al. High frequency jet ventilation during endolaryngeal surgery: Risk factors for complications. Auris Nasus Larynx. 2018;45(5):1047–1052. doi: 10.1016/j.anl.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 24.Buchan T, Walkden M, Jenkins K, et al. High-frequency jet ventilation during cryoablation of small renal tumours. Cardiovasc Intervent Radiol. 2018;41(7):1067–1073. doi: 10.1007/s00270-018-1921-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bialka S, Copik M, Rybczyk K, et al. Assessment of changes of regional ventilation distribution in the lung tissue depending on the driving pressure applied during high frequency jet ventilation. BMC Anesthesiol. 2018;18(1):101. doi: 10.1186/s12871-018-0552-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abedini A, Kiani A, Taghavi K, et al. High-frequency jet ventilation in nonintubated patients. Turk Thorac J. 2018;19(3):127–131. doi: 10.5152/TurkThoracJ.2018.17025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Engstrand J, Toporek G, Harbut P, et al. Stereotactic CT-guided percutaneous microwave ablation of liver tumors with the use of high-frequency jet ventilation: An accuracy and procedural safety study. AJR Am J Roentgenol. 2017;208(1):193–200. doi: 10.2214/AJR.15.15803. [DOI] [PubMed] [Google Scholar]
- 28.Mowes A, de Jongh BE, Cox T, et al. A translational cellular model to study the impact of high- frequency oscillatory ventilation on human epithelial cell function. J Appl Physiol (1985) 2017;122(1):198–205. doi: 10.1152/japplphysiol.00400.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barry RA, Fink DS, Pourciau DC, et al. Effect of increased body mass index on complication rates during laryngotracheal surgery utilizing jet ventilation. Otolaryngol Head Neck Surg. 2017;157(3):473–477. doi: 10.1177/0194599817698679. [DOI] [PubMed] [Google Scholar]
- 30.Mokra D, Kosutova P, Balentova S, et al. Effects of budesonide on the lung functions, inflammation and apoptosis in a saline-lavage model of acute lung injury. J Physiol Pharmacol. 2016;67(6):919–932. [PubMed] [Google Scholar]
- 31.Wheeler CR, Smallwood CD, O'Donnell I, et al. Assessing initial response to high-frequency jet ventilation in premature infants with hypercapnic respiratory failure. Respir Care. 2017;62(7):867–872. doi: 10.4187/respcare.05264. [DOI] [PubMed] [Google Scholar]
- 32.Carpi MF. High-frequency jet ventilation in preterm infants: Is there still room for it? Respir Care. 2017;62(7):997–998. doi: 10.4187/respcare.05647. [DOI] [PubMed] [Google Scholar]
- 33.Yang ZY, Meng Q, Wei HF, et al. Supraglottic jet oxygenation and ventilation during colonoscopy under monitored anesthesia care: a controlled randomized clinical trial. Eur Rev Med Pharmacol Sci. 2016;20:1168–1173. [PubMed] [Google Scholar]
- 34.Liang H, Hou Y, Wei H, Feng Y. Supraglottic jet oxygenation and ventilation assisted fiberoptic intubation in a paralyzed patient with morbid obesity and obstructive sleep apnea: a case report. BMC Anesthesiol. 2019;19(1):40. doi: 10.1186/s12871-019-0709-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Doğanay F, Ak R, Alışkan H, et al. The effects of intravenous lipid emulsion therapy in the prevention of depressive effects of propofol on cardiovascular and respiratory systems: An experimental animal study. Medicina (Kaunas). 2018;55(1):1–10. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.